Characterization of stretch-activated cation current in coronary
advertisement

Am J Physiol Heart Circ Physiol
280: H1751–H1761, 2001.
Characterization of stretch-activated cation
current in coronary smooth muscle cells
XIN WU AND MICHAEL J. DAVIS
Department of Medical Physiology, Texas A & M University System
Health Science Center, College Station, Texas 77843
Received 20 September 1999; accepted in final form 29 November 2000
Wu, Xin, and Michael J. Davis. Characterization of
stretch-activated cation current in coronary smooth muscle
cells. Am J Physiol Heart Circ Physiol 280: H1751–H1761,
2001.—Stretch-activated ion currents were recorded from
vascular smooth muscle (VSM) after enzymatic isolation of
single cells from porcine coronary arterioles. Patch pipettes
were used to record whole cell current and control cell length.
Under voltage clamp in physiological saline solution, an
inward cation current (ICAT) was activated by 105–135%
longitudinal stretch. ICAT coincided with an increase in intracellular Ca2⫹ concentration. Under current clamp, membrane depolarization was induced by stretch. The magnitude
of ICAT varied from ⫺0.8 to ⫺6.9 pA/pF at a holding potential
of ⫺60 mV. ICAT was graded with stretch, inactivated on
release, and could be repeatedly induced. A potassium current (IK) activated in unstretched cells by depolarization was
also enhanced by stretch. In Ca2⫹-free bath solution, stretchinduced enhancement of IK was blocked, but ICAT was still
present. Hexamethyleneamiloride (50 M), a reputed inhibitor of mechanosensitive channels, blocked ICAT and the
stretch-induced increase in IK but not basal IK. Grammostolla spatulata venom (1:100,000) blocked basal IK,
blocked stretch-induced increases in IK, and blocked ICAT.
Iberiotoxin, a specific Ca2⫹-activated K⫹ channel blocker, did
not alter ICAT but blocked the stretch-induced increase in IK
and increased the magnitude of stretch-induced depolarization. We concluded that longitudinal stretch directly activates a cation current and secondarily activates a Ca2⫹activated K⫹ current in isolated coronary myocytes.
Although these two currents would partially counteract each
other, the predominance of ICAT at physiological potentials is
likely to explain the depolarization and contraction observed
in intact coronary VSM during pressure elevation.
mechanosensitive channels; vascular myogenic response; calcium-activated potassium channels
vascular smooth muscle
(VSM) in response to elevation of luminal pressure, or
stretch, is termed the myogenic response. This response is independent of neural, metabolic, hormonal,
and endothelial factors (5). The myogenic response is
important for local regulation of blood flow and capillary pressure and for generation of basal vascular tone.
ACTIVE FORCE DEVELOPMENT BY
Address for reprint requests and other correspondence: M. J.
Davis, Dept. of Medical Physiology, 336 Reynolds Medical Bldg.,
Texas A & M Univ. System Health Science Center, College Station,
TX 77843-1114.
http://www.ajpheart.org
However, the underlying cellular mechanisms are incompletely understood.
Myogenic contractions are associated with a sustained depolarization of smooth muscle (14, 15), bringing the membrane potential to threshold for opening
voltage-gated L-type Ca2⫹ channels (23). Ca2⫹ influx
through these channels is thought to initiate and/or
sustain contraction. Inhibition of the L-type channel
blocks the myogenic response in nearly all vascular
preparations (5). Although L-type Ca2⫹ channels can
be directly activated by stretch if single cells are pressurized through a patch pipette (20), the resulting
current is too small to account for stretch-induced
depolarization of VSM (21); moreover, stretch-induced
depolarization persists in the presence of L-type channel blockers (19, 26).
For these reasons, alternative mechanisms have
been proposed to account for stretch-induced depolarization, including 1) inhibition of a resting K⫹ conductance (15), 2) activation of a Cl⫺ conductance (22), and
3) activation of a nonselective cation conductance (18).
Although there is evidence to support each of these mechanisms, a cation channel is consistently activated by
whole cell stretch over a range of length changes that
would be experienced by VSM cells in vivo (4, 26, 31). The
characteristics of this channel, as studied in visceral (31)
and VSM cells (4, 26), appear to be appropriate to
produce depolarization and initiate Ca2⫹ influx (6).
However, the physiological importance of the cation
channel remains to be fully characterized. This is, in
part, due to the lack of a selective blocker (12) that
could be used to test its function in an intact vascular
preparation. The interaction of this current with other
mechanosensitive currents described in VSM (5) also
remains to be determined. Other currents could potentially augment or counteract the effect of cation channel
activation. Therefore, the purpose of this study was to
determine the interaction of whole cell currents activated
by longitudinal stretch of coronary smooth muscle cells.
METHODS
Cell isolation technique. Pigs (6–10 wk old, of either sex)
were sedated with telazol (4.4 mg/kg im) and xylazine
The costs of publication of this article were defrayed in part by the
payment of page charges. The article must therefore be hereby
marked ‘‘advertisement’’ in accordance with 18 U.S.C. Section 1734
solely to indicate this fact.
0363-6135/01 $5.00 Copyright © 2001 the American Physiological Society
H1751
H1752
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
(Rompun, 2.2 mg/kg im), anesthetized with pentobarbital
sodium (20 mg/kg iv), and administered heparin (1,000 U/kg
iv). Pigs were then intubated and ventilated with room air. A
left thoracotomy was performed, and the heart was electrically fibrillated, excised, and immediately placed in 4°C saline solution.
Arterioles (50- to 160-m inner diameter) were freshly
dissected from the pig heart and placed in a silastic-coated
Plexiglas chamber containing saline solution at 4°C. The
composition was (in mM) 145.0 NaCl, 4.7 KCl, 2.0 CaCl2, 1.17
MgSO4, 1.2 NaH2PO4, 5.0 glucose, 2.0 pyruvate, 0.02 EDTA,
and 3.0 MOPS (pH adjusted to 7.4 with NaOH), with bovine
serum albumin (BSA, 10 mg/ml; Amersham Life Science;
Arlington Heights, IL) added to maintain cell integrity. Dissected vessels (20–30 segments, 1 mm in length) were transferred to a tube of low-Ca2⫹ saline solution containing (in
mM) 144.0 NaCl, 5.6 KCl, 0.1 CaCl2, 1.0 MgCl2, 0.42
Na2HPO4, 0.44 NaH2PO4, 10 HEPES, 4.17 NaHCO3, and 1
mg/ml BSA (pH adjusted to 7.4 with NaOH) at room temperature for 10 min. The solution was aspirated and replaced
with low-Ca2⫹ saline solution containing 26 U/ml papain
(Sigma, St. Louis, MO) and 1 mg/ml dithioerythritol (Sigma).
The vessels were incubated for 30 min at 37°C with occasional agitation, after which fragments were transferred to
low-Ca2⫹ saline solution containing 1.95 FALGPA U/ml collagenase (Sigma), 1 mg/ml soybean trypsin inhibitor (Sigma),
and 75 U/ml elastase (Calbiochem, La Jolla, CA) for 25 min at
37°C. After further digestion, the remaining fragments were
rinsed two times in low-Ca2⫹ saline solution and gently
triturated using a fire-polished Pasteur pipette to release
single smooth muscle cells.
Patch-clamp techniques. Standard patch-clamp techniques
as devised by Hamill et al. (11) were used. Micropipettes for
whole cell recordings were pulled from 1.5-mm-outer diameter glass tubing (Corning 8161; Warner Instruments; Hamden, CT) on a programmable puller and fire polished. Pipette
resistances ranged from 1 to 3 M⍀. For conventional whole
cell recordings, pipettes were back filled with high-K⫹ pipette
solution (high K⫹) containing (in mM) 6.0 NaCl, 115 KCl, 10
HEPES, 1.15 NaH2PO4, 1.18 MgCl2, 2.0 CaCl2, 11 glucose,
and 10 EGTA [pH adjusted to 7.2 with KOH; free Ca2⫹
concentration ([Ca2⫹]) ⫽ 17 nM]. For perforated whole cell
recording, the pipettes also contained 240 g/ml amphotericin B. An EPC-7 amplifier (HEKA, Darmstadt-Eberstadt,
Germany) was used to record current, and Narishige MOseries hydraulic manipulators (Tokyo, Japan) were used for
fine control of the micropipettes. Analog-to-digital conversions were made using a TL-1 interface (Axon Instruments;
Foster City, CA) and stored on a Pentium computer for
subsequent analysis. Data were sampled at 5–10 kHz and
filtered at 1–2 kHz with the use of an 8-pole Bessel filter
(Frequency Devices, Haverhill, MA). Series resistances varied from 2 to 9 M⍀. Series resistance compensation was used
in whole cell recordings to improve voltage control. Current
records were analyzed by use of pCLAMP (version 6.0.3,
Axon Instruments). All experiments were performed at 22°C.
Suspensions of freshly dispersed smooth muscle cells were
studied in a recording chamber, suffused at a rate of 1.5
ml/min with physiological saline solution (PSS), on the stage
of an inverted microscope (Zeiss IM-405). PSS had the following composition (in mM): 136 NaCl, 5.9 KCl, 10 HEPES,
1.16 NaH2PO4, 1.2 MgCl2, 1.8 CaCl2, 18 glucose, 0.02 EGTA,
and 2 pyruvate (pH adjusted to 7.4 with NaOH). For Ca2⫹free PSS bath solution, Ca2⫹ was replaced with an equimolar
concentration of Na⫹. Cells harvested from the enzyme procedure were elongated (⬃100 m in length) with tapered
ends, refractile under phase optics, and contracted in solutions containing an elevated K⫹ concentration.
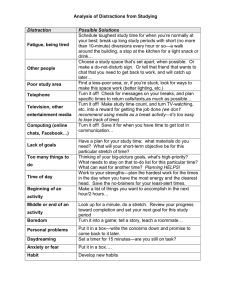
Cell stretch technique. Before they firmly attached to the
chamber bottom, individual cells were stretched with the use
of two patch pipettes. The first pipette (Fig. 1, pipette 1), also
used for intracellular recording, gently pressed one end of the
cell to the bottom of the experimental chamber. After establishment of a gigaseal, a sharp pulse of suction was applied to
the rear of the pipette to enter the whole cell recording mode.
A second “stretch” pipette (Fig. 1, pipette 2) was sealed to the
distal end of the cell in the cell-attached mode. The cell was
gently lifted off the chamber bottom by use of the stretch
pipette and slowly extended to its slack length as measured
on the video monitor. The inner tip diameter of this pipette
(Corning 7052; Garner Glass; Claremont, CA) was 3–5 m
after pulling and 2–3 m after heat polishing. The stretch
pipette was filled with the same solution used for superfusion. The position of the stretch pipette was controlled from a
computer-driven amplifier that powered a piezoelectric
translator attached to the pipette micromanipulator. Length
steps, typically in the shape of a trapezoid, were delivered by
the computer. The reference length (L) was designated as the
minimum length of the cell between the two pipettes when
Fig. 1. Cell stretch method. Pipette 1 was used for recording and to
gently hold one end of the cell. Pipette 2 was sealed to the cell near
its distal end, and its position was controlled using a piezoelectric
translator. The cell was never firmly attached to the chamber bottom. Pipette 3 was used to apply solutions and/or inhibitors. Pipette
1 contained high K⫹; pipettes 2 and 3 contained physiological saline
solution (PSS). L, reference length; ⌬L, change in length; Vm, membrane voltage. Bar in B is 15 m.
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
the slack in the cell was removed. Maximum length changes
to L ⫽ 130% corresponded to the magnitude of the transient
distention previously observed in isolated arterioles when
pressure was stepped over the entire myogenic range (7).
Length changes beyond this level were usually associated
with irreversible cell damage. During stretch protocols, the
controlling voltage to the piezoelectric manipulator was recorded as well as the signal of the responding current of the
cell (sampled at 20–400 Hz) with the use of LabView (National Instruments; Austin, TX). At the same time, the holding potential (HP), seal test, ramp or step voltage, and current changes were recorded using pCLAMP.
Fura 2 microfluorometry. Intracellular Ca2⫹ concentration
([Ca2⫹]i) was measured using a fura 2 microfluorometry
system (6). Cells were preloaded with the acetoxymethyl
ester of fura 2 (fura 2-AM; 10 M) for 10 min and then
superfused for at least 30 min with PSS before fluorescence
measurements were started. The ratio of 340/380 fluorescence was converted to [Ca2⫹]i using a standard method (10).
Minimum ratio (Rmin) was determined in 10 mM EGTA, and
maximum ratio (Rmax) was determined in 10 M Ca2⫹.
Solution changes. Solution changes and drug application
to individual cells were made with the use of a picospritzer
pipette before and during stretch (Fig. 1B, pipette 3). Cells at
the outflow end of the chamber were studied first and cells at
the inflow end last. Grammostolla spatulata spider venom
was obtained from Spider Pharm (Feasterville, PA). Iberiotoxin and apamin were obtained from Alomone Labs (Jerusalem, Israel). Tetraethylammonium (TEA), hexamethyleneamiloride (HMA), and all other chemicals were obtained from
Sigma.
Data analysis. We used data only from those experiments
in which the distal cell end did not pull away from the stretch
pipette and in which a stable gigaseal was maintained
throughout the stretch protocol. The high-resolution traces
from pCLAMP were used to determine current amplitude. In
most analyses, raw current values were normalized to cell
capacitance (an index of cell size) and expressed as current
density (in pA/pF). Whole cell capacitance ranged from 6 to
22 pF. Statistical comparisons were performed with repeated-measures analysis of variance (ANOVA) followed by post
hoc tests or with an independent two-tail t-test, as appropriate. Summary values are presented as means ⫾ SE. Values
of P ⬍ 0.05 were considered to be statistically significant.
When normalized current was plotted versus cell stretch, the
relationship was fit to the Boltzmann equation (I ⫽ {1 ⫹
exp[(L ⫺ L0.5)/k]}⫺1), where I is current, L0.5 is the length
producing 50% current activation, and k is the slope factor.
H1753
(n ⫽ 17). An example is shown in Fig. 2A, where the
duration of stretch was 15 s. In this case, the amplitude
of ICAT was nearly identical for both stretches. When
the interval between the two stimuli was ⬍20 s, the
amplitude of the second current was essentially unchanged in ⬇40% of the cells, decreased in ⬇50% of the
cells, and increased in the remainder of the cells. The
current could also be activated by a phasic stretch
stimulus (at the same frequency as the porcine arterial
pulse pressure). Sinusoidal stretch to 125% of L (at 1 or
2 Hz) activated ICAT, although the magnitude of the
current was more variable (Fig. 2B) than that observed
in response to a step change in length.
ICAT could be easily differentiated from artifacts due
to gigaseal breakdown. Seal breakdown would induce
RESULTS
An inward current is activated by whole cell stretch.
Longitudinal stretch typically induced an inward cation current, termed ICAT, at negative holding potentials (n ⫽ 285 cells from 112 animals). The magnitude
of ICAT varied from ⫺0.8 to ⫺6.9 pA/pF (HP ⫽ ⫺60 mV)
for length increases between 105 and 135% of L. ICAT
was reversible, and its amplitude increased monotonically with stretch. ICAT was noisier than the resting
membrane current, suggesting that it arose from a
channel. The delay in ICAT activation ranged from 20 to
1,000 ms after stretch. In most cells, ICAT could be
recorded for at least 90 s without substantial inactivation.
To examine the reproducibility of ICAT, two consecutive and identical stimuli were applied to the same cell
Fig. 2. Longitudinal stretch consistently induced an inward cation
current (ICAT). A: a single vascular smooth muscle (VSM) cell was
held at ⫺60 mV while being stretched to 120% of the reference length
(L) for 15 s. Inward ICAT is indicated by a downward deflection in the
current (I) density trace. B: ICAT was also induced by a 1-Hz sinewave stimulus. Trace is representative of 6 cells. C: gigaseal breakdown during stretch. Inward ICAT density (ICAT, ⫺2 to ⫺3.4 pA/pF)
was recorded after 2 successive stretches to 115 and 120% of L.
However, near the end of the second stretch (arrow), the seal broke
down, resulting in a large and noisy current (greater than ⫺15
pA/pF). The first inward ICAT recording reversed when stretch was
released, but the second current recording did not. Bath solution,
PSS; pipette solution, high K⫹. Holding potential (HP) ⫽ ⫺60 mV.
Acquisition rate ⫽ 80–120 Hz.
H1754
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
apparent changes in holding current, so seal resistance
was monitored periodically while recording whole cell
current during stretch. If the gigaseal broke down, the
resulting current became larger, noisier, and irreversible, as shown in Fig. 2C (note the lower gain for the
current recording compared with that used in Fig. 2,
A and B). In this cell, between ⫺2.0 and ⫺3.4 pA/pF of
inward ICAT was recorded after two successive
stretches to 115 and 120% of L. However, near the end
of the second stretch (see arrow), the seal broke down,
resulting in a large, artifactual and noisy current trace
(greater than ⫺15 pA/pF). The noisy current did not
inactivate when cell length was returned to control.
This response was typical of a cell that slipped from
under the recording pipette.
ICAT amplitude as a function of the magnitude of
stretch. Graded increases in the magnitude of stretch
were used to investigate whether the amplitude of ICAT
was proportional to the magnitude of stretch. With
cells stretched to 115, 120, 125, 130, or 135% of L, there
was a corresponding increase in the amplitude of ICAT.
An example is shown in Fig. 3A, in which length
changes to 120, 125, and 130% of L were imposed at
Fig. 3. Amplitude of ICAT was graded with increases in the magnitude of stretch. A: length changes to 120, 125, and 130% of L elicited
graded increases in inward ICAT density. B: the magnitude of ICAT
plotted as a function of L for the cell in A. Data were fit by a
Boltzmann equation with half-maximal stretch equal to 123.3% of L
and slope factor (k) ⫽ 1.8% above L. Bath solution, PSS; pipette
solution, high K⫹. HP ⫽ ⫺60 mV. Acquisition rate ⫽ 300 Hz.
Table 1. ICAT as a function of graded stretch
Group
n
A
B
1
2
3
4
5
3
3
5
8
6
⫺1.38 ⫾ 0.34
⫺1.56 ⫾ 0.21
⫺1.72 ⫾ 0.17
⫺2.16 ⫾ 0.18
⫺5.45 ⫾ 0.12
⫺1.43 ⫾ 0.19
⫺1.68 ⫾ 0.15
⫺2.34 ⫾ 0.12*
⫺3.81 ⫾ 0.13*
⫺5.74 ⫾ 0.19
C
⫺4.22 ⫾ 0.24*†
⫺5.53 ⫾ 0.11*†
Values are means ⫾ SE. Inward cation current (ICAT; in pA/pF) as
a function of graded stretch. Within each group, the same cell
experienced each level of stretch. Group 1, stretch to 105 ( A) and
then 110% (B) of reference length (L); group 2, stretch to 110 ( A) and
then 112.5% (B) of L; group 3, stretch to 115 ( A), 120 (B), and then
125% (C) of L; group 4, stretch to 120 ( A), 125 (B), and then 130% (C)
of L; group 5, stretch to 130 ( A) and then 135% (B) of L. Holding
potential (HP) ⫽ ⫺60 mV in all cases; n ⫽ no. of cells. * P ⬍ 0.05
compared with A. † P ⬍ 0.05 compared with B.
HP ⫽ ⫺60 mV. The duration of stretch was 6 s in each
case. The amplitude of the inward ICAT increased progressively with increasing stretch, and the entire data
set for this cell is plotted in Fig. 3B. A fit of the
Boltzmann equation to the data in Fig. 3B shows that
half-maximum inward ICAT was evoked by a stretch to
123.3% of L; k was 1.8% above L. It was difficult to
consistently analyze this relationship for individual
cells because most cells could not successfully be
stretched through the entire range of lengths. The
composite data set for 25 different cells is shown in
Table 1. The threshold for consistent, measurable ICAT
was a stretch to 115% of L, and 135% of L was usually
the maximum length change that could be imposed
without damage. This magnitude of stretch is consistent with that observed in isolated arterioles when
pressure is stepped through the entire range over
which the vessels respond myogenically (7).
Current-voltage relationship for ICAT. To determine
the whole cell current-voltage (I-V) relationship for
ICAT, voltage ramps from ⫺100 to ⫹60 mV (duration ⫽
200 ms, HP ⫽ ⫺60 mV, average of 3–5 ramps) were
applied before and during longitudinal cell stretch. We
used only data from ICAT recordings that were stable
during stretch (duration ⫽ 5–10 s). Figure 4A summarizes the I-V relationship of membrane currents before
and during 115% stretch (n ⫽ 5). Stretch produced a
248% increase in inward ICAT at ⫺70 mV and 20%
enhancement in outward current at ⫹60 mV. The difference current recorded before and after stretch is
shown in Fig. 4B. The I-V relationship of the difference
current was approximately linear between ⫺70 and
⫺10 mV, rectified inwardly at voltages negative to ⫺70
mV, and rectified outwardly at voltages positive to ⫺10
mV. The reversal potential of the stretch-induced current in this group of cells was ⫺18.2 ⫾ 3.2 mV (stretch
to 115% of L). The reversal potentials at other levels of
stretch, 105, 110, 115, and 120% of L, were not significantly different from this (Table 2). Membrane conductance increased from 0.3 ⫾ 0.04 to 1.0 ⫾ 0.07 nS at
⫺100 mV and from 1.5 ⫾ 0.05 to 1.8 ⫾ 0.04 nS at ⫹50
mV during stretch to 115% of L.
[Ca2⫹]i changes during ICAT recording. To test
whether longitudinal cell stretch induced an increase
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
H1755
Fig. 5. Time course of intracellular Ca2⫹ concentration ([Ca2⫹]i)
change relative to the change in stretch-evoked current density.
Trapezoidal stretch to 120% of L activated an inward ICAT at HP ⫽
⫺60 mV. A concomitant rise in [Ca2⫹]i occurred. In this cell, the
inward ICAT and [Ca2⫹]i declined slightly with time, while stretch
was maintained. When the cell was returned to its original L, the
current inactivated, but the decline in [Ca2⫹]i was delayed (complete
recovery is not shown). Test pulses from ⫺60 to ⫹50 mV (duration ⫽
400 ms) were delivered before, during, and after stretch to estimate
magnitude of outward K⫹ current (IK) density. Outward IK could be
recorded at ⫹50 mV in the absence of stretch, but the amplitude of
the current was increased during stretch. Perforated patch-clamp
mode with cell preloaded with fura 2-AM. Bath solution, PSS; pipette
solution, high K⫹ with amphotericin B. R340/380, ratio of 340- to
380-nm fluorescence.
Fig. 4. Current-voltage (I-V) relationship of stretch-induced current.
A: I-V plot of the average membrane current evoked by voltage ramp
from ⫺100 to ⫹60 mV (200-ms duration), with HP ⫽ ⫺60 mV.
Current density was recorded before (E) and during (F) stretch to
115% of L (n ⫽ 5). Each line is the average of 5 responses. B: I-V
curve of the difference current, i.e., obtained before and during
stretch. The reversal potential of the difference current was ⫺18.2 ⫾
3.2 mV for stretch to 115% of L. Bath solution, PSS; pipette solution,
high K⫹.
in [Ca2⫹]i concomitant with ICAT, global [Ca2⫹]i was
measured using fura 2 microfluorometry while current
recordings were performed in the perforated-patch,
whole cell mode. With cells bathed in PSS and high-K⫹
solution in the recording pipette, [Ca2⫹]i levels consistently increased in response to 120% stretch, as shown
in Fig. 5. The onset of the changes was normally
delayed 0.2–2 s after the change in length, and the
Table 2. Reversal potential of ICAT
as a function of stretch
Parameter
L, %
n
Erev, mV
105
4
⫺19.3 ⫾ 2.7
110
3
⫺18.8 ⫾ 3.5
115
5
⫺18.2 ⫾ 3.2
120
6
⫺20.1 ⫾ 3.1
Values are means ⫾ SE. Erev, reversal potential of net current,
determined as the difference in average of 3 voltage ramps before
and after stretch. HP ⫽ ⫺60 mV.
peak [Ca2⫹]i increase was delayed significantly with
respect to the peak ICAT. In the example shown in Fig.
5, an inward ICAT of approximately ⫺3 pA/pF was
evoked by stretch. This current activated over the
same time course in which [Ca2⫹]i increased from ⬇100
to a peak of 500 nM, followed by a plateau to ⬇300 nM.
Data for five cells showed an average increase in
[Ca2⫹]i to 278 ⫾ 35.8% of control levels in response to
a 120% stretch.
An outward K⫹ current is enhanced secondary to
stretch. An outward whole cell current was also enhanced during stretch, concomitant with the increase
in [Ca2⫹]i and ICAT. This is noted in the cell shown in
Fig. 5 by the current response to the three brief voltage
pulses (⫺60 to ⫹50 mV, duration ⫽ 400 ms) delivered
before, during, and after stretch. Although little outward current was evident at the holding potential
(HP ⫽ ⫺60 mV), 14.5 pA/pF of outward current were
evoked by the first depolarizing pulse. The amplitude
of this current increased to 20.2 pA/pF during the
application of a 120% stretch and then returned toward
control (to 16.2 pA/pF) after stretch was released. This
observation suggested that an outward Ca2⫹-dependent current might be enhanced secondary to ICAT.
To specifically test for the contribution of a K⫹ current, we analyzed the difference in the outward current
evoked by depolarizing pulses given before and during
stretch. Figure 6 shows an example of another cell
subjected first to 120% stretch and then to 125%
stretch, with paired voltage pulses delivered before and
during each step. As before, the magnitude of the
H1756
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
Fig. 6. Time course of the outward IK activated during stretch. A:
stretch to 120% and then to 125% of L, each stretch lasting 10 s. An
inward ICAT was activated by each stretch when HP was ⫺60 mV, as
noted by a sustained downward deflection in the current density
trace coinciding with each increase in stretch. Transient voltage
steps to ⫹50 mV (duration ⫽ 400 ms) elicited larger outward IK
superimposed on the inward ICAT. a–d: outward IK evoked by 4
successive voltage pulses, with a and c recorded before stretch and b
and d recorded during stretch. B: a higher-resolution trace (from
pCLAMP) of the outward IK elicited during voltage pulses c and d.
d-c, Difference current between c and d. An outward difference
current suggests that enhancement of IK occurred during stretch.
Bath solution, PSS; pipette solution, high K⫹.
outward current evoked by the pulse was larger during
the application of longitudinal stretch. For this cell, the
currents evoked by four voltage steps are labeled a–d,
where a and c are outward currents before stretch and
b and d are outward currents during stretch. The
amplitude of the outward current, termed IK, was significantly increased during both stretches. In Fig. 6A,
the recordings were digitized at 80 Hz, so the outward
IK traces are not clearly resolvable. Higher resolution
traces of the currents recorded during the voltage
pulses are shown in Fig. 6B (recorded in pCLAMP and
sampled at ⱖ2 kHz); the high-resolution traces were
used to measure outward IK amplitude in this and
subsequent analyses. Although there was no significant difference between the amplitudes of currents a
and c, the amplitudes of both b and d were larger than
their controls, and the amplitude of d (recorded during
125% stretch) was greater than that of b (recorded
during 120% stretch). The difference trace (d and c)
recorded during the larger stretch is shown in Fig. 6B.
The average results for these protocols are summarized in Table 3. For 18 cells studied, there were significant increases in the magnitude of IK during stretch
(compared with nonstretched controls), and the increase was significant for each length step studied
(120, 125, and 130% of L). Furthermore, the enhancement of IK was larger as the magnitude of the length
step increased (Table 3).
To test whether a Ca2⫹-activated K⫹ (KCa) channel
contributed to the outward component of current enhanced by cell stretch, several additional experimental
protocols were performed. First, the single-stretch protocol was repeated in Ca2⫹-free bath solution. Although ICAT could still be recorded in Ca2⫹-free bath
during stretch, the outward component of current no
longer increased with stretch (Fig. 7A, n ⫽ 7). This
result suggested that 1) ICAT is not carried primarily by
Ca2⫹, and 2) the outward component of ICAT was increased secondary to Ca2⫹ influx. Because TEA is
known to block various IK, the effect of TEA on ICAT
was tested during stretch with the cell bathed in PSS
(containing 1.8 mM Ca2⫹). TEA at 10 mM is a nonselective K⫹ channel inhibitor, whereas 1 mM TEA is
reported to have a more selective effect on KCa channels (24). Figure 7B shows an example of the protocol
used to test this idea. Two consecutive stretch stimuli
of the same magnitude were applied to the cell, the first
in PSS and the second in PSS containing 1 mM TEA. In
the absence of TEA, outward IK elicited by a depolarizing pulse was enhanced 22% (trace b vs. trace a) by
cell stretch (length ⫽ 130% of L). Addition of 1 mM
TEA (n ⫽ 8) to the superfusate reduced the outward IK
by 62 ⫾ 1% (trace d vs. trace c) before the second
stretch was applied, and, during the second stretch (to
130% of L), there was no significant increase in IK.
Importantly, the inward ICAT at HP ⫽ ⫺60 mV was
activated after each stretch (⫺5.4 ⫾ 0.3 pA/pF, n ⫽ 8),
and this current was unaffected by TEA (⫺5.5 ⫾ 0.2
pA/pF). IK recovered to the control level (trace f vs.
trace c) after washout of TEA. Qualitatively similar
results were also obtained using 10 mM TEA, which
had an even greater effect on basal outward IK (70 ⫾
1% inhibition of IK before stretch, n ⫽ 18) and on the
outward IK that was enhanced after stretch (98 ⫾
1.2%); 10 mM TEA was also without significant effect
on the inward ICAT recorded at HP ⫽ ⫺60 mV. The
data are summarized in Fig. 7C.
Table 3. Amplitude of IK as a function of stretch
L, %
Before stretch
During stretch
Change in IK
120
125
130
16.6 ⫾ 1.2 (8)
19.9 ⫾ 1.1 (8)*
2.8 ⫾ 0.2 (4)
17.1 ⫾ 1.4 (10)
21.6 ⫾ 1.7 (10)*
3.7 ⫾ 0.1 (4)†
16.4 ⫾ 1.4 (8)
22.7 ⫾ 1.6 (8)*
4.8 ⫾ 0.4 (4)†‡
Values are means ⫾ SE. Amplitude of K⫹ current (IK; in pA/pF) as
a function of stretch; nos. in parentheses are no. of cells. HP ⫽ ⫺60
mV; test pulse ⫽ ⫹50 mV. * P ⬍ 0.05, “before stretch” compared
with “during stretch.” † P ⬍ 0.05 compared with L ⫽ 120% (same
group of cells). ‡ P ⬍ 0.05 compared with 125% (same group of cells).
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
H1757
Iberiotoxin (IbTX; 100 nM), a specific inhibitor of
large-conductance KCa channels (24), inhibited basal
IK by 22% [n ⫽ 9, at time (t) ⫽ 2 min after application].
In the presence of IbTX, there was no significant increase in IK in response to 125% stretch, and the
stretch-induced enhancement in ICAT was unaffected
(Fig. 7C).
We also tested the effect of IbTX on the membrane
depolarization evoked by stretch. In current-clamp recording mode, the resting potential of unstretched
VSM cells averaged ⫺56.4 ⫾ 1.2 mV (n ⫽ 35). In
response to 130% longitudinal cell stretch, an average
depolarization of 11.6 ⫾ 1.6 mV (n ⫽ 6) was recorded
(Fig. 8). This depolarization was maintained for the
Fig. 7. Characteristics of the outward IK enhanced by stretch. A:
amplitude of the outward IK was not increased during stretch if the
cell was bathed in Ca2⫹-free ([Ca2⫹]o free, where [Ca2⫹]o is extracellular Ca2⫹ concentration) PSS. ICAT was still recorded in response to
stretch, as noted by a sustained downward deflection in the current
density trace coinciding with the L increase. Voltage steps from ⫺60
to ⫹50 mV during this time elicited an outward IK, the amplitude of
which was not noticeably enhanced during stretch. B: 2 stretches to
130% of L were used to test the effect of adding 1 mM tetraethylammonium (TEA) to the bath solution (PSS). Voltage steps from ⫺60 to
⫹50 mV revealed an increase in outward IK during stretch (trace b
vs. a). TEA caused a substantial decrease in outward IK at ⫹50 mV
before stretch (trace d vs. c), and, in the presence of TEA, outward IK
did not significantly increase during stretch (trace e vs. trace d).
There were no substantial differences in the amplitude of outward IK
with time in the absence of TEA and stretch (trace a vs. trace c vs.
trace f). Also, the amplitude of ICAT was similar between the 2
stretches in the presence of TEA. C: summary of effects of TEA (1
mM) and iberiotoxin (IbTX; 100 nM) on IK before and after stretch.
For TEA protocols, stretch was to 130% of L. For IbTX protocols,
stretch was to 125% of L. HP ⫽ ⫺60 mV; test pulse ⫽ ⫹50 mV; n ⫽
no. of cells. Bath solution, Ca2⫹-free PSS (A) and PSS (B and C);
pipette solution, high K⫹. * P ⬍ 0.05 vs. control.
Fig. 8. Stretch-induced depolarization was enhanced by Ca2⫹-activated K⫹ channel blockade. A: with the use of the current-clamp
configuration, longitudinal stretch to 130% of L induced a 17-mV
membrane depolarization from a resting potential near ⫺60 mV. B:
depolarization induced by stretch to 130% of L in another cell was
enhanced by addition of IbTX (100 nM) to the bath. In addition,
spontaneous fluctuations in the membrane potential recording were
reduced in the presence of IbTX (see portion of trace above the
dashed line). C: summary of effects of IbTX (100 nM) or apamin (200
nM) on membrane potential at rest and during stretch to 130% of L.
Nos. in parentheses indicate no. of cells. Bath solution, PSS; pipette
solution, high K⫹. * P ⬍ 0.05 vs. control group (no stretch). # P ⬍ 0.05
vs. stretch group.
H1758
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
duration of the stretch, although transient spikes often
appeared at the more positive potentials. The cell gradually repolarized 1–5 s after stretch was released.
IbTX (100 nM) had no significant effect on the resting
membrane potential of these cells (Fig. 8C), but after a
cell had been depolarized by stretch, application of
IbTX caused an additional depolarization. An example
of this effect is shown in Fig. 8B, where 130% stretch
produced a 17-mV initial depolarization and subsequent IbTX application produced an additional 7-mV
depolarization. Fluctuations in the membrane potential recording were typically reduced in the presence of
IbTX compared with control (Fig. 8, compare A and B).
The data are summarized in Fig. 8C. On average, the
additional depolarization produced by IbTX during
stretch was 5.1 mV.
We also tested the effects of apamin, an inhibitor of
small-conductance KCa channels (24), on this response.
Like IbTX, apamin (200 nM) had no significant effect
on the resting membrane potential (Fig. 8C). When
applied after cell stretch, apamin (200 nM) and IbTX
(100 nM) produced essentially the same response (additional depolarization of 5.9 mV) as IbTX alone. Thus
it is likely that apamin-sensitive KCa channels do not
play a role in stretch-induced depolarization, whereas
IbTX-sensitive KCa channels do.
Effects of putative mechanosensitive channel blockers. Although no highly selective blockers of mechanosensitive channels have been described to date, HMA is
reported to block stretch-activated single-channel cation currents in Xenopus oocytes (13), and G. spatulata
venom is reported to block mechanosensitive whole cell
cation currents in GH3 cells, Xenopus oocytes, and
chick heart cells (3, 16). We tested the effects of these
compounds on the inward and outward components of
stretch-activated current in coronary smooth muscle
cells.
Whole cell currents were elicited by voltage ramps
from ⫺100 to ⫹60 mV (200-ms duration, HP ⫽ ⫺60
mV) before, during, and after 120% cell stretch. The
average current evoked by three voltage ramps was
used for comparison. In the cell shown in Fig. 9A,
stretch induced an inward ICAT of ⫺1.8 pA/pF and a
24% increase in the outward IK at ⫹50 mV (trace b vs.
trace a). The inward ICAT was completely blocked by 50
M HMA (representative of 10 cells). In contrast to
TEA, HMA had no effect on the magnitude of the
outward IK at ⫹50 mV in the absence of stretch. However, stretch-induced increases in the outward IK were
blocked by HMA (trace e vs. trace d). The data for 10
cells are summarized in Fig. 9C.
In an additional series of experiments, G. spatulata
venom was applied at a concentration of 1:10,000 or
1:100,000 (dilutions of the crude extract in PSS, n ⫽ 6
for each). The stretch and recording protocol was identical to that used for HMA. In the cell shown in Fig. 9B,
120% stretch evoked ⫺2.2 pA/pF of inward ICAT at
HP ⫽ ⫺60 mV and increased the outward IK at ⫹50
mV by 21% (trace b vs. trace a). G. spatulata venom
(1:100,000) completely blocked ICAT and inhibited the
outward IK at ⫹50 mV by 52% in the absence of stretch
Fig. 9. Effect of putative mechanosensitive channel blockers on ICAT
and IK . A: 2 identical stretches to 120% of L evoked an inward ICAT
at ⫺60 mV and enhanced the outward IK at ⫹50 mV. Three voltage
ramps (from ⫺100 to ⫹60 mV, 200-ms duration) were delivered at
periodic intervals to measure IK, and the changes in IK (in C) are the
average of the 3 currents. ICAT was prevented by 50 M hexamethyleneamiloride (HMA) as indicated by the absence of inward ICAT at
⫺60 mV during HMA perfusion (for stretch 2). Stretch-induced
increases in IK did not occur in the presence of HMA (trace e vs. trace
d). HMA did not block control IK in the absence of stretch (trace d vs.
trace c or trace a). There were no substantial differences in the
amplitude of IK with time (trace a vs. trace c vs. trace f). B: same
protocol repeated in the presence of G. spatulata spider venom
(1:100,000). ICAT was blocked by the spider venom as indicated by the
absence of an inward ICAT evoked by stretch (for stretch 2). Stretchinduced increases in IK also did not occur in the presence of spider
venom (e vs. d), but the venom significantly blocked IK even in the
absence of stretch (d vs. c). C: summary of effects of HMA (50 M)
and G. spatulata venom (1:100,000) on ICAT and IK. For IK, test
pulse ⫽ ⫹50 mV. Nos. in parentheses indicate no. of cells. Stretch to
120% of L in all protocols. Bath solution, PSS; pipette solution, high
K⫹; HP ⫽ ⫺60 mV. * P ⬍ 0.05 vs. control.
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
(trace d vs. trace c). As before, stretch-induced increases in outward IK did not occur when ICAT was
blocked (trace e vs. trace d). At the higher concentration
of 1:10,000, G. spatulata venom blocked ICAT, although
this effect was not specific for ICAT because L-type Ca2⫹
currents were inhibited as well (data not shown). The
data for six cells are summarized in Fig. 9C.
DISCUSSION
To investigate the mechanism underlying myogenic
depolarization of VSM, whole cell currents were recorded from single coronary myocytes during longitudinal stretch. Stretch to 115–135% of control length
caused activation of an inward cation current, induced
membrane depolarization, and produced an increase in
global [Ca2⫹]i. The magnitude of ICAT ranged from
⫺0.8 to ⫺6.9 pA/pF (HP ⫽ ⫺60 mV), was graded with
stretch, inactivated on release of the stimulus, and
could be repeatedly induced. An outward IK was also
enhanced by stretch at depolarized potentials. In Ca2⫹free bath, ICAT could still be recorded, but the stretchinduced enhancement in IK was absent. The reputed
mechanosensitive channel blockers HMA and G. spatulata venom blocked stretch-induced increases in both
ICAT and IK, but G. spatulata venom also blocked basal
IK, suggesting it was not selective for mechanosensitive current. K⫹ channel blockers, including TEA and
IbTX, blocked the stretch-induced increase in IK and
increased the magnitude of the stretch-induced depolarization but did not alter ICAT. We concluded that
longitudinal stretch of coronary myocytes directly
activates an inward ICAT at the resting membrane
potential and secondarily activates a KCa channel. The
enhancement in IK may serve to counteract stretchinduced depolarization and thereby limit the magnitude and/or duration of a myogenic contraction.
Evidence for a depolarization-linked mechanism underlying myogenic tone derives from several lines of
experimentation. 1) Graded VSM depolarization occurs
as pressure in isolated small arteries and arterioles is
increased (17). 2) Smooth muscle strips (2) and single
myocytes depolarize in response to longitudinal stretch
(4, 26, 31), such that depolarization by 10–15 mV from
a resting potential of about ⫺55 mV would be sufficient
to increase the open probability of voltage-gated Ca2⫹
channels by severalfold (23). 3) The myogenic response
is blunted when the normal ion gradients across the
plasma membrane are altered so as to minimize the
extent of stretch-induced depolarization (5). 4) Ca2⫹
channel blockers attenuate myogenic tone in almost all
types of smooth muscle (5). Depolarization of smooth
muscle would activate Ca2⫹ entry and thereby enhance
contraction (14, 17). This is not the only mechanism
involved, however, because there is considerable evidence that Ca2⫹-independent pathways, e.g., protein
kinase C activation, are also important (5), perhaps for
long-term maintenance of contraction at high pressure.
The mechanism by which stretch is coupled to depolarization is controversial. Both the speed of the response and the change in membrane potential point to
H1759
a role for ion channels. One explanation is that depolarization is mediated by activation of a cation channel
promoting Na⫹/Ca2⫹ influx. Such channels have been
recorded in myocytes isolated from a number of smooth
muscles (4, 18, 25, 32). These channels typically exhibit
a relative permeability of K⫹ⱖ Na⫹ ⬎ Ca2⫹ and singlechannel conductance between 30 and 40 pS (for monovalent ions) (4, 18, 32). In the presence of Ca2⫹, they
often rectify (18, 32) and show reduced monovalent
conductance (18, 26), suggesting that a Ca2⫹-dependent inactivation mechanism exists. In terms of physiological relevance, it is important to note that stretchactivated whole cell currents and/or depolarizations
have now been recorded in pig coronary myocytes (4),
urinary bladder (30, 31), and rat mesenteric arterioles
(25, 26). The reversal potentials for whole cell currents
and their dependence on extracellular Na⫹ concentration are consistent with activation of a nonselective
cation channel rather than a pure Ca2⫹ conductance (4,
25, 26, 31).
Voltage-gated Ca2⫹ channels might also be modulated directly by stretch. L-type Ca2⫹ currents in rat
cerebral arterial myocytes, as recorded by use of the
conventional whole cell mode, are enhanced by inflating cells through a patch pipette (20, 21) and, in perforated-patch recordings, by hypoosmotic cell swelling
(20). Yet current flow through these channels is probably too small to account for stretch-induced depolarization (21), and stretch-induced depolarization persists in the presence of Ca2⫹ channel blockade (19, 26).
Stretch-induced depolarization might also be mediated by activation of Cl⫺ efflux if a mechanosensitive
Cl⫺ channel in smooth muscle responded to longitudinal stretch and if the Cl⫺ equilibrium potential of the
smooth muscle cell were more positive than the resting
membrane potential (22). These requirements have not
been thoroughly tested, but the reversal potential of
stretch-induced whole cell current appears to be independent of changes in extracellular Cl⫺ concentration
(4, 26). Although Cl⫺ channel blockers inhibit myogenic responsiveness (22), their actions may be explained by nonspecific effects on voltage-gated Ca2⫹
channels (9). Thus the evidence supporting a key role
for a Cl⫺ channel is not compelling at this time.
Inhibition of K⫹ efflux might also account for stretchinduced depolarization if one or more of the various K⫹
channels identified in smooth muscle were inhibited by
membrane stretch (5). Mechanosensitive K⫹ channels
have been identified in smooth muscle by use of singlechannel recording techniques, but the channels are
activated, rather than inactivated, by stretch (8). To
mediate stretch-induced depolarization, a putative
mechanosensitive IK must exhibit basal activity when
a vessel has resting vascular tone. Although some
isolated vessel data are consistent with this requirement (19), electrophysiological support is largely lacking. Voltage-dependent K⫹ (KV) channel blockers depolarize VSM cells in pressurized arterioles and
enhance myogenic tone (19), but the more likely candidate to mediate a stretch-sensitive IK is the largeconductance KCa (BK) channel (8). Wesselman et al.
H1760
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
(33) concluded that BK channels were necessary for
pressure-induced contraction of isolated mesenteric arteries because charybdotoxin, a relatively specific inhibitor, caused a decrease in myogenic index. However,
those experiments were performed in vessels precontracted with norepinephrine, which might have led to
basal BK channel activation. On the basis of the effect
of specific BK inhibitors on basal tone, it appears that
not all blood vessels have basal BK channel activity
that could potentially be inhibited by stretch (5).
A more likely role for K⫹ channels in myogenic
responsiveness is to counteract, rather than initiate,
myogenic tone. Indeed, because the conductance of BK
channels is so large and activation of only a few would
be necessary to substantially change smooth muscle
membrane potential, it has been proposed that stretchinduced depolarization could not be maintained unless
an endogenous inhibitor of the channels is produced
(15). There is evidence that 20-hydroxyeicosatetraenoic
acid (20-HETE), a cytochrome P-450 metabolite of arachidonic acid, may be one such substance (15). However, the use of (reputedly) selective inhibitors has
confirmed a role for 20-HETE only in some (33), not all
(1), vessels.
Data in the present study support the idea that a KCa
current is activated secondary to stretch-induced Ca2⫹
entry, whereas a cation channel underlies the depolarization controlling Ca2⫹ entry. The enhanced IK had
the following characteristics under the conditions of
our experiments: 1) it activated over a voltage range
appropriate for KV or KCa channels (Fig. 4), 2) its
activation coincided with the time course of stretchinduced [Ca2⫹]i increases (Fig. 5), 3) its enhancement
was prevented in Ca2⫹-free bath solution (Fig. 7), and
4) it was blocked by inhibitors of KCa channels (Figs. 7
and 8). These observations are all consistent with this
channel being a KCa channel. Importantly, its activation must have occurred secondary to that of the cation
channel, because IK was blocked when ICAT was
blocked, but not vice versa (Fig. 9). The idea that IK
counteracts stretch-induced depolarization is supported by our observation that stretch-induced depolarization was potentiated by the specific KCa channel
inhibitor IbTX (Fig. 8). Importantly, IbTX had no effect
on resting membrane potential, suggesting it blocked
only a component of current that was activated after
cell stretch (Fig. 8C). Our conclusions are consistent
with the findings of Wellner and Isenberg (31), who
reported that TEA caused a shift in reversal potential
of ICAT in bladder myocytes toward more positive values. In that study, stretch-enhanced outward IK was
also blocked by intracellular Ca2⫹ chelation (31). Collectively, these characteristics match those of a KCa
current.
Our data support the conclusion that a cation channel is activated by longitudinal stretch in coronary
arteries and arterioles, leading to membrane depolarization. The characteristics of the whole cell current
associated with this channel were as follows: 1) it was
reversibly and repeatedly activated by stretch (Fig. 2);
2) it showed graded increases in amplitude with in-
creasing stretch, up to 135% of control cell length (Fig.
3); 3) it activated over the same time course as stretchinduced depolarization (Figs. 2 and 8); and 4) it had a
reversal potential in PSS between ⫺15 and ⫺20 mV
(Fig. 4 and Table 2). These characteristics are nearly
identical to those for stretch-activated whole cell currents recorded in other smooth muscle cells (26, 31).
Furthermore, ICAT persisted in Ca2⫹-free bath solution
(Fig. 7) and in the presence of K⫹ channel blockers
(Figs. 7 and 8) and was blocked by inhibitors of mechanosensitive channels such as Gd3⫹ (28), HMA, and G.
spatulata venom (Fig. 9). Because the stretch-activated
current can be recorded at negative potentials after
extracellular Cl⫺ substitution (4), it is likely that current is carried predominantly by Na⫹ at negative potentials. At positive potentials, much of the current
must be carried by K⫹, because it can still be recorded
as the equilibrium potential for Na⫹ is approached.
The channel is likely to be Ca2⫹ permeable as well, as
is typical of other non-voltage-gated, mechanosensitive
channels (4, 18, 32). The observation that this current
sometimes decays markedly after stretch (16, 32) suggests a possible Ca2⫹-dependent inactivation mechanism that will make accurate determination of Na⫹-toCa2⫹ permeability ratio difficult.
Is activation of a nonselective cation channel necessary for initiation of the vascular myogenic response?
This question was not answered by the present experiments and cannot be answered at this time. There are
several reputed inhibitors of mechanosensitive channels used to block mechanotransduction in muscle (12).
Yet all of these compounds, including Gd3⫹, streptomycin antibiotics, and G. spatulata venom, also inhibit
voltage-gated Ca2⫹ channels. For example, Gd3⫹ inhibits ICAT in mesenteric artery and bladder myocytes (26,
31), inhibits stretch-induced depolarization of single
VSM cells, inhibits stretch-induced Ca2⫹ influx (6), and
blocks myogenic tone of arterioles (27, 29). However,
Gd3⫹ inhibits L-type channels in smooth muscle at
1,000-fold lower concentrations than required to inhibit mechanosensitive cation channels (28), so its
physiological effect on arterioles could be explained
simply by a downstream action on the L-type channel.
Thus circumstantial evidence linking stretch-induced
depolarization to activation of a nonselective cation
channel is growing, but the lack of a selective, highaffinity antagonist of that channel prevents definitive
testing of the hypothesis that its activation is required
for myogenic responsiveness.
We gratefully acknowledge Judy A. Davidson, Dr. William H.
Griffith, the laboratory of Dr. Lih Kuo, and Robert Gaffin for advice
and technical assistance.
This study was supported by National Heart, Lung, and Blood
Institute Grant HL-46502.
REFERENCES
1. Bakker ENTP, Kerkhof CJM, and Sipkema P. Signal transduction in spontaneous myogenic tone in isolated arterioles from
rat skeletal muscle. Cardiovasc Res 41: 229–236, 1999.
2. Bülbring E. Correlation between membrane potential, spike
discharge and tension in smooth muscle. J Physiol (Lond) 128:
200–221, 1955.
STRETCH-ACTIVATED CHANNELS IN VASCULAR MYOCYTES
3. Chen Y, Simasko SM, Niggel J, Sigurdson WJ, and Sachs
F. Ca2⫹ uptake in GH3 cells during hypotonic swelling: the
sensory role of stretch-activated ion channels. Am J Physiol Cell
Physiol 270: C1790–C1798, 1996.
4. Davis MJ, Donovitz JA, and Hood JD. Stretch-activated
single-channel and whole-cell currents in vascular smooth muscle cells. Am J Physiol Cell Physiol 262: C1083–C1088, 1992.
5. Davis MJ and Hill MA. Signaling mechanisms underlying the
vascular myogenic response. Physiol Rev 79: 387–423, 1999.
6. Davis MJ, Meininger GA, and Zawieja DC. Stretch-induced
increases in intracellular calcium in isolated vascular smooth
muscle cells. Am J Physiol Heart Circ Physiol 263: H1292–
H1299, 1992.
7. Davis MJ and Sikes PJ. Myogenic response of isolated arterioles: test for a rate-sensitive mechanism. Am J Physiol Heart
Circ Physiol 259: H1890–H1900, 1990.
8. Dopico AM, Kirber MT, Singer JJ, and Walsh JV Jr. Membrane stretch directly activates large conductance Ca2⫹-activated K⫹ channels in mesenteric artery smooth muscle cells.
Am J Hypertens 7: 82–89, 1994.
9. Doughty JM, Miller AL, and Langton PD. Non-specificity of
chloride channel blockers in rat cerebral arteries: block of the
L-type calcium channel. J Physiol (Lond) 507: 433–439, 1998.
10. Grynkiewicz G, Poenie M, and Tsien RY. A new generation
of Ca2⫹ indicators with greatly improved fluorescence properties.
J Biol Chem 260: 3440–3450, 1985.
11. Hamill OP, Marty A, Neher E, and Sigworth FJ. Improved
patch-clamp techniques for high-resolution current recording
from cells and cell-free membrane patches. Pflügers Arch 391:
85–100, 1981.
12. Hamill OP and Mcbride DW Jr. The pharmacology of mechanogated membrane ion channels. Pharmacol Rev 48: 231–252,
1996.
13. Hamill OP and Mcbride DW Jr. Rapid adaptation of single
mechanosensitive channels in Xenopus oocytes. Proc Natl Acad
Sci USA 89: 7462–7466, 1992.
14. Harder DR. Pressure-dependent membrane depolarization in
cat middle cerebral artery. Circ Res 55: 197–202, 1984.
15. Harder DR, Narayanan J, Gebremedhin D, and Roman
RJ. Transduction of physical force by the vascular wall: role of
phospholipase C and cytochrome P450 metabolites of arachidonic acid. Trends Cardiovasc Med 5: 7–14, 1995.
16. Hu H and Sachs F. Mechanically activated currents in chick
heart cells. J Membr Biol 154: 205–216, 1996.
17. Johnson PC. The myogenic response. In: Handbook of Physiology. The Cardiovascular System. Vascular Smooth Muscle. Bethesda, MD: Am. Physiol. Soc., 1980, sect. 2, vol. II, chapt. 15, p.
409–442.
18. Kirber MT, Walsh JV Jr, and Singer JJ. Stretch-activated
ion channels in smooth muscle: a mechanism for the initiation of
stretch-induced contraction. Pflügers Arch 412: 339–345, 1988.
H1761
19. Knot HJ and Nelson MT. Regulation of membrane potential
and diameter by voltage-dependent K⫹ channels in rabbit myogenic cerebral arteries. Am J Physiol Heart Circ Physiol 269:
H348–H355, 1995.
20. Langton PD. Calcium channel currents recorded from isolated
myocytes of rat basilar artery are stretch sensitive. J Physiol
(Lond) 471: 1–11, 1993.
21. McCarron JG, Crichton CA, Langton PD, Mackenzie A,
and Smith GL. Myogenic contraction by modulation of voltagedependent calcium currents in isolated rat cerebral arteries.
J Physiol (Lond) 498: 371–379, 1997.
22. Nelson MT, Conway MA, Knot HJ, and Brayden JE. Chloride channel blockers inhibit myogenic tone in rat cerebral arteries. J Physiol (Lond) 502: 259–264, 1997.
23. Nelson MT, Patlak JB, Worley JF, and Standen NB. Calcium channels, potassium channels, and voltage dependence of
arterial smooth muscle tone. Am J Physiol Cell Physiol 259:
C3–C18, 1990.
24. Nelson MT and Quayle JM. Physiological roles and properties
of potassium channels in arterial smooth muscle. Am J Physiol
Cell Physiol 268: C799–C822, 1995.
25. Ohya Y, Adachi N, Nakamura Y, Setoguchi M, Abe I, and
Fujishima M. Stretch-activated channels in arterial smooth
muscle of genetic hypertensive rats. Hypertension 31: 254–258,
1998.
26. Setoguchi M, Ohya Y, Abe I, and Fujishima M. Stretchactivated whole-cell currents in smooth muscle cells from mesenteric resistance artery of guinea-pig. J Physiol (Lond) 501:
343–353, 1997.
27. Sipkema P and Bakker ENTP. Inhibition of spontaneous
myogenic tone in isolated arterioles from rat skeletal muscle
(Abstract). FASEB J 12: A16, 1998.
28. Song JB and Davis MJ. Gadolinium blocks calcium channels
in coronary artery smooth muscle cells (Abstract). Biophys J 61:
A515, 1992.
29. Takenaka T, Suzuki H, Okada H, Hayashi K, Kanno Y, and
Saruta T. Mechanosensitive cation channels mediate afferent
arteriolar myogenic constriction in the isolated rat kidney.
J Physiol (Lond) 511: 245–253, 1998.
30. Wellner MC and Isenberg G. cAMP accelerates the decay of
stretch-activated inward currents in guinea-pig urinary bladder
myocytes. J Physiol (Lond) 482: 141–156, 1995.
31. Wellner MC and Isenberg G. Stretch effects on whole-cell
currents of guinea-pig urinary bladder myocytes. J Physiol
(Lond) 480: 439–448, 1994.
32. Wellner MC and Isenberg G. Properties of stretch-activated
channels in myocytes from the guinea-pig urinary bladder.
J Physiol (Lond) 466: 213–227, 1993.
33. Wesselman JPM, Schubert R, Vanbavel E, Nilsson H, and
Mulvany MJ. KCa-channel blockade prevents sustained pressure-induced depolarization in rat mesenteric small arteries.
Am J Physiol Heart Circ Physiol 272: H2241–H2249, 1997.