1810
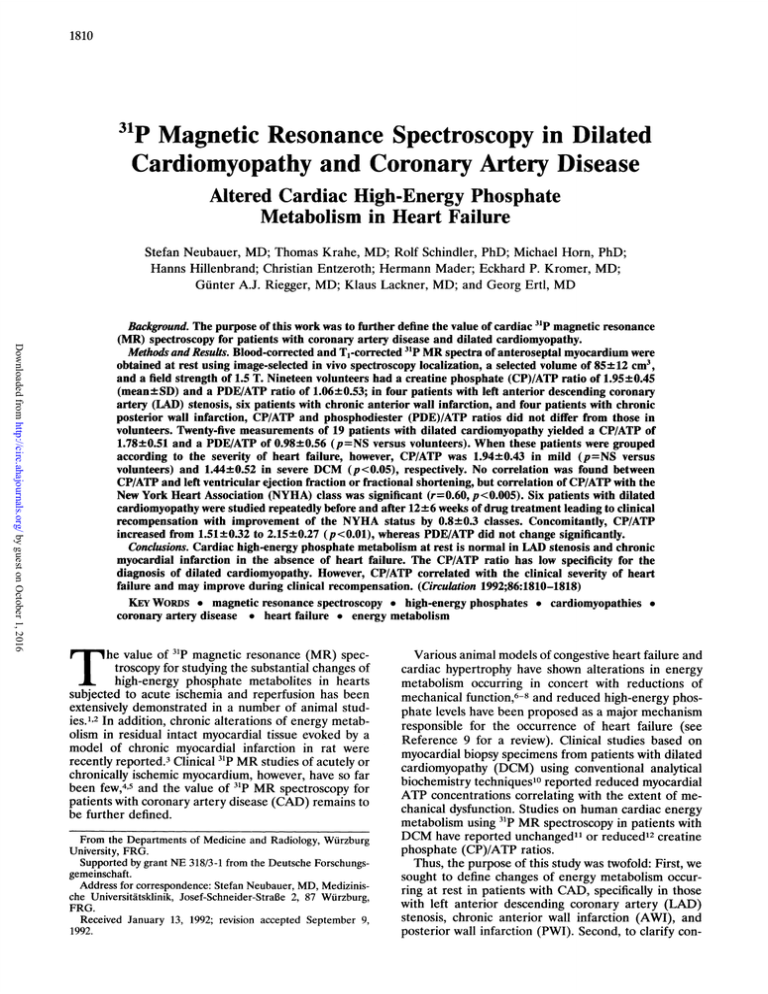
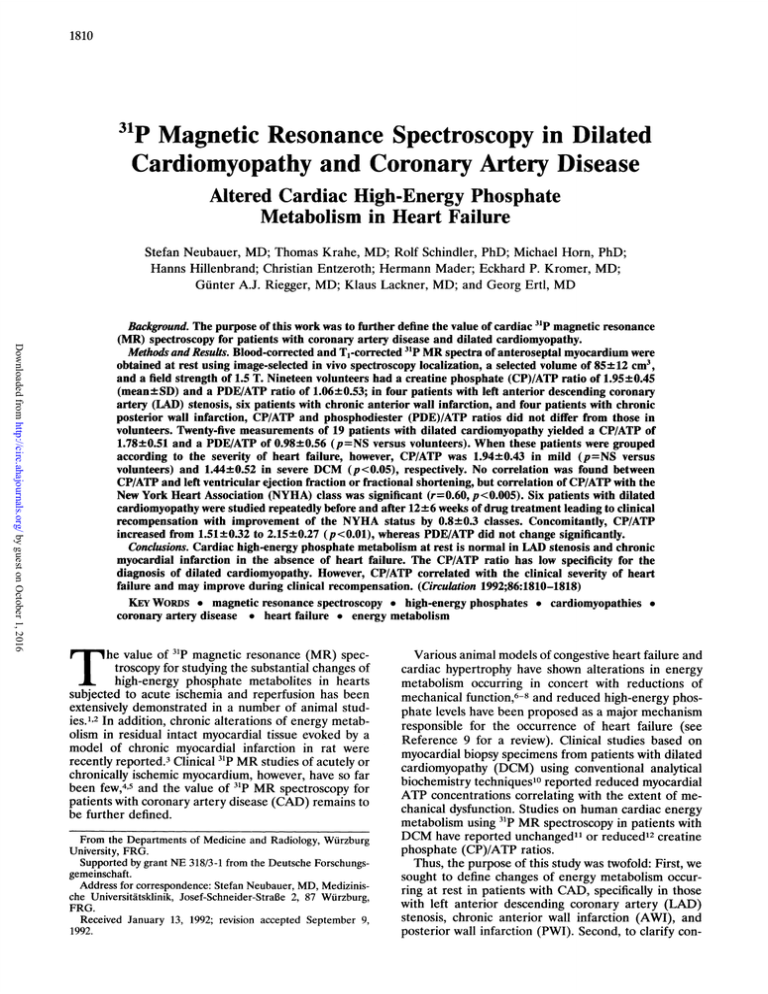
31p Magnetic Resonance Spectroscopy in Dilated
Cardiomyopathy and Coronary Artery Disease
Altered Cardiac High-Energy Phosphate
Metabolism in Heart Failure
Stefan Neubauer, MD; Thomas Krahe, MD; Rolf Schindler, PhD; Michael Horn, PhD;
Hanns Hillenbrand; Christian Entzeroth; Hermann Mader; Eckhard P. Kromer, MD;
Gunter A.J. Riegger, MD; Klaus Lackner, MD; and Georg Ertl, MD
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Background. The purpose of this work was to further define the value of cardiac 3'P magnetic resonance
(MR) spectroscopy for patients with coronary artery disease and dilated cardiomyopathy.
Methods and Results. Blood-corrected and Tl-corrected 3`P MR spectra of anteroseptal myocardium were
obtained at rest using image-selected in vivo spectroscopy localization, a selected volume of 85± 12 cm3,
and a field strength of 1.5 T. Nineteen volunteers had a creatine phosphate (CP)/ATP ratio of 1.95±0.45
(mean± SD) and a PDE/ATP ratio of 1.06+0.53; in four patients with left anterior descending coronary
artery (LAD) stenosis, six patients with chronic anterior wall infarction, and four patients with chronic
posterior wall infarction, CP/ATP and phosphodiester (PDE)/ATP ratios did not differ from those in
volunteers. Twenty-five measurements of 19 patients with dilated cardiomyopathy yielded a CP/ATP of
1.78+0.51 and a PDE/ATP of 0.98±0.56 (p=NS versus volunteers). When these patients were grouped
according to the severity of heart failure, however, CP/ATP was 1.9490.43 in mild (p=NS versus
volunteers) and 1.44+0.52 in severe DCM (p<0.05), respectively. No correlation was found between
CP/ATP and left ventricular ejection fraction or fractional shortening, but correlation of CP/ATP with the
New York Heart Association (NYHA) class was significant (r=0.60, p<0.005). Six patients with dilated
cardiomyopathy were studied repeatedly before and after 12±6 weeks of drug treatment leading to clinical
recompensation with improvement of the NYHA status by 0.8±0.3 classes. Concomitantly, CP/ATP
increased from 1.51±0.32 to 2.1590.27 (p<0.01), whereas PDE/ATP did not change significantly.
Conclusions. Cardiac high-energy phosphate metabolism at rest is normal in LAD stenosis and chronic
myocardial infarction in the absence of heart failure. The CP/ATP ratio has low specificity for the
diagnosis of dilated cardiomyopathy. However, CP/ATP correlated with the clinical severity of heart
failure and may improve during clinical recompensation. (Circulation 1992;86:1810-1818)
KEY WORDs * magnetic resonance spectroscopy * high-energy phosphates * cardiomyopathies
coronary artery disease * heart failure * energy metabolism
T he value of 31p magnetic resonance (MR) spectroscopy for studying the substantial changes of
high-energy phosphate metabolites in hearts
subjected to acute ischemia and reperfusion has been
extensively demonstrated in a number of animal studies.1'2 In addition, chronic alterations of energy metabolism in residual intact myocardial tissue evoked by a
model of chronic myocardial infarction in rat were
recently reported.3 Clinical 31p MR studies of acutely or
chronically ischemic myocardium, however, have so far
been few,45 and the value of 31p MR spectroscopy for
patients with coronary artery disease (CAD) remains to
be further defined.
From the Departments of Medicine and Radiology, Wurzburg
University, FRG.
Supported by grant NE 318/3-1 from the Deutsche Forschungsgemeinschaft.
Address for correspondence: Stefan Neubauer, MD, Medizinische Universitatsklinik, Josef-Schneider-StraBe 2, 87 Wurzburg,
FRG.
Received January 13, 1992; revision accepted September 9,
1992.
Various animal models of congestive heart failure and
cardiac hypertrophy have shown alterations in energy
metabolism occurring in concert with reductions of
mechanical function,6-8 and reduced high-energy phosphate levels have been proposed as a major mechanism
responsible for the occurrence of heart failure (see
Reference 9 for a review). Clinical studies based on
myocardial biopsy specimens from patients with dilated
cardiomyopathy (DCM) using conventional analytical
biochemistry techniques'0 reported reduced myocardial
ATP concentrations correlating with the extent of mechanical dysfunction. Studies on human cardiac energy
metabolism using `P MR spectroscopy in patients with
DCM have reported unchanged1" or reduced'2 creatine
phosphate (CP)/ATP ratios.
Thus, the purpose of this study was twofold: First, we
sought to define changes of energy metabolism occurring at rest in patients with CAD, specifically in those
with left anterior descending coronary artery (LAD)
stenosis, chronic anterior wall infarction (AWI), and
posterior wall infarction (PWI). Second, to clarify con-
Neubauer et al Energy Metabolism in CAD and DCM
1811
TABLE 1. Characteristics of Patients With Coronary Artery Disease
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Time
Age
after MI
Angiography/ventriculography
Sex
Patient
Diagnosis
(years)
M
20
LAD
67
...
LAD 90%, Rd1 95%, Rd2 95%, Cx 90%, RCA 100%, EF 56%
62
M
21
LAD
...
Left main 60%, LAD 70%, Cx 70%, RCA 95%, EF 53%
M
LAD
66
...
LAD 95%, Cx 60%, RCA 70% EF 54%
45
M
...
LAD 95%, EF 89%
50
LAD
58
M
7
54
6 Years
LAD 100%, ant. hypokinesia, EF 68%
AWI
M
3 Weeks
LAD 70%, left posterolat. 70%, ant. hypokinesia, EF 75%
11
AWI
62
M
14
61
2 Weeks
LAD 100%, Cx 95%, RCA 100%, ant./inf. hypokinesia, EF 30%
AWI
M
24
54
2 Weeks
LAD 95%, interm. 80%, Rm, 95%, RCA 80%, ant. hypokinesia, EF 89%
AWI
M
30
2 Weeks
LAD 95%, ant. akinesia, EF 42%
AWI
55
M
63
3 Weeks
LAD 95%, anteroseptal hypokinesia, EF 83%
36
AWI
M
5 Months
4
54
Cx 100%, RCA 95%, inf. hypokinesia, EF 58%
PWI
M
5
50
2 Weeks
RCA 100%, Cx 30%, inf. akinesia, EF 55%
PWI
M
19
56
4 Weeks
Cx 100%, inf. hypokinesia, EF 54%
PWI
M
46
6 Weeks
Cx 100%, inf. akinesia, EF 56%
PWI
67
MI, myocardial infarction; LAD, left anterior descending coronary artery; AWI, anterior wall infarction; PWI, posterior wall infarction;
Rdl, Rd2, first and second diagonal branch of LAD; Cx, circumflex artery; RCA, right coronary artery; EF, ejection fraction; ant., anterior;
posterolat., posterolateral; inf., inferior; interm., intermediate; Rmj, first marginal branch of Cx.
flicting results from other groups, we evaluated whether
31P MR is a sensitive technique for the detection of
DCM. Furthermore, we examined whether alterations
of energy metabolism in DCM correlate with the clinical severity of heart failure, as estimated by the New
York Heart Association (NYHA) classification independent of functional parameters, and whether depressed energy metabolism can improve with medical
therapy leading to clinical recompensation.
Methods
Characteristics of Volunteers and Patient Groups
All studies were approved by the Ethics Committee of
the University of Wurzburg. Nineteen volunteers with a
mean age of 24±2 years (range, 20-29 years) served as
a control group. All volunteers were apparently healthy
individuals with no signs of heart disease at rest and
during exercise. The 33 patients (mean age, 54 years;
range, 28-67 years) were divided into 14 with CAD and
19 with DCM. Those with CAD (Table 1) were further
subdivided as follows.
Four patients (all men; mean age, 63 years; range,
58-67 years; LAD group) had an LAD stenosis of
270%. Three of four reported a typical history of chest
pain. All patients received nitrates and acetylsalicylic
acid, three received a P-blocking agent, two received a
Ca21 channel blocker, two an angiotensin-converting
enzyme (ACE) inhibitor, one digitalis, and one a diuretic. The LAD lesion was demonstrated by coronary
angiography by an independent cardiologist. This group
was examined to visualize energy metabolism at rest in
myocardium supplied by a highly stenotic coronary
artery. Patients in this group were allowed to have
significant stenoses of the circumflex (Cx) and/or right
coronary artery (RCA) in addition to the LAD lesion
but were not included if left ventriculographic and/or
ECG evidence of previous infarction was found.
Six patients (all men; mean age, 58 years; range,
54-63 years; AWI group) were examined who had a
previous anterior wall myocardial infarction (between 2
weeks and 6 years previously). In all patients, this was
evidenced by anterior wall motion abnormalities upon
left ventriculography. In addition, in every patient,
previous serum chemistry changes (creatine kinase
[CK]-MB) and/or ECG findings indicated the presence
of myocardial infarction. All patients received nitrates,
four received a Ca2' channel blocker, three a p-blocker,
three acetylsalicylic acid, three a diuretic agent, one an
ACE inhibitor, and one digitalis. The LAD lesion
responsible for the AWI was demonstrated by coronary
angiography. This group was examined to visualize
energy metabolism in scar tissue and in residual myocardium immediately adjacent to the infarct scar. Patients in this group were allowed to have significant
stenosis of the Cx and/or RCA in addition to the LAD
lesion and were also allowed to have other wall motion
abnormalities in addition to the anterior hypokinesis or
akinesis.
Four patients (all men; mean age, 57 years; range,
50-67 years; PWI group) were examined who had a
previous posterior wall myocardial infarction (between
2 weeks and 5 months previously). In all patients, this
was evidenced by inferior wall motion abnormalities
upon left ventriculography. In addition, in every patient,
previous serum chemistry changes (CK-MB) and/or
ECG findings indicated the presence of infarction. All
patients received nitrates, three received acetylsalicylic
acid, two a P-blocker, and two a diuretic agent. The
RCA or Cx lesion responsible for the PWI was demonstrated by coronary angiography. Because this group
was examined to visualize energy metabolism in residual
intact myocardium in a region remote from the infarct
scar, patients were included only if normal LAD morphology and normal anterior wall motion was found.
None of the patients with CAD (LAD, AWI, or PWI)
had any clinical signs of heart failure.
Table 2 shows characteristics of the 19 patients with
DCM. Seventeen were men, two women; mean age was
51+± 10 years (range, 28-64 years). The presumed
pathogenesis of DCM was alcoholic in seven, postmyocarditis in three, and idiopathic in nine. In all patients,
left ventricular (LV) fractional shortening (FS) averag-
1812
Circulation Vol 86, No 6 December 1992
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
TABLE 2. Characteristics of Patients
Dilated Cardiomyopathy
Age
Patient
Cause
(years) Sex
37
M
6
Alcoholic
30
M
8
Myocarditis
M
40
10
Idiopathic
F
47
17
Myocarditis
51
M
23
Idiopathic
56
M
26
Idiopathic
49
M
28
Alcoholic
M
59
32
Myocarditis
F
55
33
Idiopathic
64
M
38
Alcoholic
M
40
28
Idiopathic
63
44
Alcoholic
M
50
M
51
Idiopathic
63
M
54
Idiopathic
M
53
75
Alcoholic
52
M
78
Idiopathic
51
M
Alcoholic
84
56
Alcoholic
M
98
M
56
109
Idiopathic
With
FS
(%)t
11
38
8
30
18
II-III
46 (rn)
16
II-III
II
19 (mn)
8
27
13
II-III
41
58 (in)
II-III
6
III
...
II
60
30
12
III-IV
...
5
Ill-IV 32
42
14
II-III
20
27
II
24
40
lI-IlI
III-IV 18
8
II
40
15
8
III-IV 17 (rn)
17
13
TI-IIl
34
III
23
NYHA, New York Heart Association; EF, ejection fraction; FS,
fractional shortening.
*By radiocontrast left ventriculography or radionuclide scan (in).
NYHA
class
III
III
EF
(%)*
20
tBy echocardiography.
ing 16+9% was determined echocardiographically in
the parasternal long-axis view close to the time of
spectroscopy (c2 days). In 17 of 19 patients, LV ejection fraction (EF) averaging 33±14% was determined
by radiocontrast left ventriculography13 or radionuclide
scan.4 In all DCM patients, the presence of CAD was
ruled out by demonstrating normal coronary anatomy in
the presence of LV dysfunction by coronary angiography. In addition, none of the DCM patients had chest
pain or signs of myocardial infarction on ECG readings.
At the day of spectroscopy, the clinical status of each
patient was evaluated by an independent cardiologist
before spectroscopy was performed, and patients were
graded according to the NYHA classification for heart
failure. At the time of study, 16 patients received a
diuretic, 16 received digitalis, 16 an ACE inhibitor, two
a class I (mexiletine and propafenone) and one a class
III (amiodarone) antiarrhythmic drug, and two acetylsalicylic acid. Table 3 describes NYIHA classes and
treatment regimen of six patients with DCM who were
studied before and 12±6 weeks (range, 3-20 weeks)
after drug therapy. The mean age of this subgroup was
54±11 years (range, 37-64 years). All patients received
diuretics and ACE inhibitors, five received digitalis, and
four were treated with 50 mg/day of the ,3-blocker
metoprolol. In all patients, the clinical status improved
by at least 0.5 NYHA classes (mean, 0.8±0.3) during
treatment. Serial measurements of LV function were
not made.
MR Data Acquisition and Processing
Measurements were taken with a 1.5-T (resonance
frequencies, 63.83 MHz for 'H, 27.16 MHz for 31p)
TABLE 3. Characteristics of Patients With Dilated
Cardiomyopathy During Treatment
NYHA/heart rate
(bpm)
Time
interval
Before
After
Treatment
Patient
(weeks)
18
6
Dig, diu, ACEI, p-bl
11/88
111/100
11
17
Diu, ACEI, ,B-bl
II-III/90 11/85
20
Dig, diu, ACEI
32
111/95
11/85
13
38
III-IV/90 II-III/90 Dig, diu, ACEI
3
Dig, diu, ACEI, 1B-bl
54
II-III/80 11/80
9
98
Dig, diu, ACEI, ,-bl
II-III/90 11/65
NYHA, New York Heart Association; bpm, beats per minute;
dig, digitalis; diu, diuretic; ACEI, ACE inhibitor; 8-bl, (8-blocker.
whole-body Philips Gyroscan MR system with an effective bore size of 65 cm. A single custom-made 15-cmdiameter surface coil tunable to 'H and 31p (doubletuned coil) served as both transmitter and receiver coil.
To minimize motion artifacts, subjects were examined in
prone position with the chest wall lying above the
surface coil.
Before each measurement, shimming on the proton
signal was performed, yielding line widths of <0.7 ppm
(<45 Hz) for H20; spectroscopy was not performed if
'H line width could not be reduced below 0.7 ppm.
Localization was then carried out by the image-selected
in vivo spectroscopy (ISIS) technique.'3 First, nine
Tl-weighted, spin-echo multislice 'H images of the
heart were recorded with a pulse repetition time (TR)
equal to one RR interval, an echo time of 30 msec, and
a slice thickness of 15 mm, confirming the correct
position of the surface coil relative to the heart. On the
basis of these scout images, the ISIS volume was positioned over the anteroseptal region of the heart, as
illustrated by an example shown in Figure 1. Volume
size for spectroscopy ranged from 46 to 117 cm3 (mean,
84+12 cm3). Adiabatic pulses were used and yielded flip
angles of 1800 throughout the selected volume. The
acquisition was ECG triggered. TR was equal to two RR
intervals, 15 or 24 seconds; correspondingly, the number
of averages was 1,024, 128, or 96; 32%, 36%, and 24% of
measurements in volunteers, CAD patients, and DCM
patients, respectively, were performed with a short TR
(two RR intervals). Total scan time/spectrum was :32
minutes, and total patient examination time was 45-60
minutes. For the six patients with DCM studied sequentially, the same TR was used for both examinations.
CP/ATP ratios were corrected for partial saturation
based on T, measurements in volunteers as previously
described14: Tls of y-ATP, CP, and phosphodiester
(PDE) were 5.4±0.5, 6.1±0.5, and 5.0±+1.0 seconds,
respectively. This assumes that T,s do not change in the
presence of cardiac disease. The quality of volume
selection by ISIS was tested in phantom experiments in
which a cube (volume, 64 ml) filled with hypophosphoric
acid (H3P02) was placed in a cylinder (15 cm in diameter and height) containing orthophosphoric acid
(H3P04). When the ISIS volume was localized within
the cube containing H3P02 and TR was varied from 2 to
20 seconds, the H3P04 resonance area was reduced by
91.3% (TR, 2 seconds) to 91.9% (TR, 20 seconds)
compared with nonlocalized spectra. Thus, localized
spectra were contaminated by signal from surrounding
Neubauer et al Energy Metabolism in CAD and DCM
1813
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
FIGURE 1. Typical example of a transverse 'Hmagnetic resonance image of a patient with coronary artery disease demonstrating
how the image-selected in vivo spectroscopy volume was placed into the anteroseptal portions of the heart. RA, right atrium; RV
right ventricle; LA, left atrium; LV, left ventricle; R, right; L, left.
volume by <10% regardless of TR. 3P spectra were
processed with zero shift, direct current correction
(30%), exponential multiplication (7 Hz), and individual phase correction. Peak areas for 2,3 -diphosphoglycerate (2,3-DPG), PDE, CP, [y-P], [a-P], and [P-PJATP
(Figure 2) were obtained by Lorentzian line fits in the
time domain as previously described14 using 400 iterations. Preliminary work indicated that peak areas differed by <3% after 300 iterations were applied. For
comparison of spectra from different subjects, the CP/
[y-P]ATP ratio and PDE/[y-PJATP ratio were calculated. Because of bandwidth limitations of the transmitter, we chose to use the [y-P] instead of the [,8-P]
resonance of ATP. The CP/ATP ratio is regarded as an
index of the energetic state of the heart (see Reference
9 for review); furthermore, it has been suggested that
changes of the PDE/ATP ratio may indicate cardiomyocyte membrane damage in DCM.11
When ISIS is used as a single-volume technique, all
`P spectra exhibit resonances corresponding to 2,3DPG. We therefore corrected spectra for blood contamination. `P spectra of venous blood freshly drawn from
19 volunteers (temperature, 37°C; TR, 2.4 seconds;
number of acquisitions, 1,032) gave a [y-P]ATP/2,3DPG area ratio of 0.11±0.02 (SD), corresponding to a
molar ratio of 0.22. Literature values reported using
routine chemistry are somewhat higher (0.30±0.02,
SEM).'5,16 The PDE/2,3-DPG area ratio in blood was
0.19±0.03. Thus, for blood correction, the [y-P]ATP
resonance area of cardiac spectra was reduced by 11%
of the 2,3-DPG resonance area, and the PDE resonance
was reduced by 19% of the 2,3-DPG area. The average
[y-P]ATP/2,3-DPG ratio in all cardiac spectra was
0.73+0.41 and was 0.87±0.44 in volunteers 0 75-0.48
in CAD, and 0.68±0.41 in DCM (p=NS, volunteers
versus CAD and DCM, respectively), indicating that the
degree of blood contamination tended to be greater in
DCM but was not significantly different.
Statistical Analysis
CP/ATP and PDE/ATP ratios calculated for each
metabolite were averaged to yield mean±SD values.
Data from the various groups and subgroups were
compared by factorial ANOVA17 with statistically significant differences detected by Scheffe's F test. The
correlations among CP/ATP ratios and NYHA class,
EF, and FS were analyzed by linear regression analysis.'7 Changes of heart rate and high-energy phosphate
ratios during treatment in patients with DCM were
compared by paired t test.17 Calculations were aided by
the StatView SE+Graphics Professional, Graphic, Statistics Utility (BrainPower Inc., Calabasas, Calif.). Values of p<0.05 were considered significant.
Results
Volunteers
Figure 2A shows a typical "P spectrum from a
volunteer. The average ratio of T1- and blood-corrected
CP/ATP was 1.95+0.45, and PDE/ATP was 1.06±0.53
(Figure 3). Values without blood correction were CP/
ATP, 1.64±0.26 and PDE/ATP, 1 17±0.45; thus, blood
correction increased the CP/ATP ratio by 19% and
decreased the PDE/ATP ratio by 9%. On the basis of
31p metabolite ratios measured in blood from volunteers, we calculated that, on average, 17+8% of the
ATP resonance area and 28±17% of the PDE reso-
Circulation Vol 86, No 6 December 1992
1814
B
A
3-ATP
a
,-~ ~,
(;;- ) 13
5
C
0
1
~~
-5
-10
-13
-23
-25 (;PM) 13
5
0
-5
-10
-15
-23
T
-25
D
1
FIGURE 2. Cardiac 31P magnetic resonance spectra from a volunteer (panel
A) andfrom patients with LAD stenosis
(panel B), chronic anterior (panel C),
and chronic posterior wall infarction
(panel D). Compared with the volunteer, none of thepatient spectra appearto
be grossly altered apart from various
degrees of blood contamination. CP, creatine phosphate; PDE, phosphodiesters;
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
213 DPG,
2,3-dohosphoglycerate.
IfW WW
1
(pnM)
10
5
0
-5
-10
-15
-23
-25
(pprM)
10
5
0
nance area could be attributed to blood contamination
of the ISIS volume.
Coronary Artery Disease
Examples of 31P spectra from one patient with LAD
stenosis, one with AWI, and one with PWI are shown in
Figures 2B-2D. Compared with the volunteer, none of
the spectra appear to be grossly altered apart from
various degrees of blood contamination. Mean T,- and
blood-corrected metabolite ratios are given in Figure 3.
The figure demonstrates that neither the CP/ATP nor
the PDE/ATP ratio showed any significant change in
patients with CAD, although there may be a slight
tendency for reduced CP/ATP in AWI and PWI. Thus,
no significant abnormalities of energy metabolism at
rest could be detected in patients with LAD stenosis,
AWI, and PWI.
Dilated Cardiomyopathy
Figure 4 (left panel) shows the spectrum of a 37-year
old patient with DCM who was in NYHA class Ill heart
failure. In this spectrum, the CP/ATP ratio is reduced
(1.56), and the PDE/ATP ratio is elevated (2.26). Figure
3 gives mean values of Ti- and blood-corrected metabolite ratios for all 25 measurements of 19 patients with
DCM. The CP/ATP ratio showed a trend toward a
decrease (1.78 +0.51) but was not significantly different
from volunteers (1.95 ±0.45). The PDE/ATP ratio
(0.98±0.56) was similar to values from volunteers
(1.06±0.53). Thus, as a group including all clinical
stages, patients with DCM could not be distinguished
from volunteers on the basis of 31P MR data. When
patients were grouped according to the clinical severity
-5
-10
-15
-20
-25
of heart failure, however, a different picture evolved. As
depicted in Figure 3, CP/ATP ratios were unchanged
(1.94+0.43) in patients with mild (NYHA <III) but
significantly reduced (1.44+0.52; p<0.05) in severe
(NYHA 2111) DCM. Figure 5 shows that the CP/ATP
ratio decreased progressively in relation to the severity
of heart failure; CP/ATP values were 2.14±0.32 (n=9),
1.71±0.46 (n=8), 1.61±0.31 (n=4), and 1.26±0.68
(n=4) for NYHA classes II, 11-111, III, and III-IV,
respectively. Furthermore, linear regression between
NYHA class and CP/ATP was highly significant
(r=0.60,p<0.005). In contrast, the PDE/ATP ratio bore
no correlation with the clinical severity of heart failure
(Figures 3 and 5), and linear regression was not significant (r=0.16, p=0.43). Similarly, we failed to detect a
significant correlation between the indexes of LV performance (EF and FS) and CP/ATP or PDE/ATP
ratios. Linear regression yielded CP/ATP=0.009EF+
1.38 (r=0.25, p=0.34); CP/ATP=-0.OO1FS+1.68
(r=0.02, p=0.94); PDE/ATP=0.007EF+0.79 (r=0.17,
p=0.52); and PDE/ATP= -0.004FS +1.06 (r=0.07,
p=0.76). Correlations did not improve when EF values
>40% or FS values >20% were excluded from the
regression.
Finally, a subgroup of six patients with DCM was
examined sequentially before and after 12±6 weeks of
drug therapy (see "Methods" and Table 3). The six
patients improved by 0.8±0.3 NYHA classes during
treatment. Figure 4 shows spectra of a patient before
and after therapy. The increase of CP/ATP and the
decrease of PDE/ATP occurring with therapy are apparent. Figure 6 shows the changes of CP/ATP and
PDE/ATP during treatment. The initial CP/ATP ratio
Neubauer et al Energy Metabolism in CAD and DCM
1815
0L
0~
+10
-10
-20
+10
-20 ppm
-10
0
FIGURE 4. 3'P magnetic resonance spectra of a patient with
dilated cardiomyopathy before (left panel) and 18 weeks after
(right panel) treatment with digitalis, diuretics, ACE inhibitors, and P-blockers. As the clinical status was improvedfrom
New York HeartAssociation class III to II, creatine phosphate
(CP)IATP ratio was increased, and in this case, phosphodiesters (PDE)IATP was reduced. Also, in this case, 2,3diphosphoglycerate (2/3 DPG) was decreased after therapy,
indicating reduced signal from blood. For all patients, however, the amount of blood contamination was similar before
and after therapy. -y, [y-P]ATP; a, [a-P]ATP.
9n .
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
1.5
0.0
0
ATITT
T
LI-
0,5
0.0
VL
LAD
AWI
PWM
DCM
DCMn
DCMs
FIGURE 3. Bar graphs showing mean creatine phosphate
(CP)lATP (top panel) and phosphodiesters (PDE)IATP
(bottom panel) ratios of volunteers (Vol) and patient groups.
LAD, left anterior descending coronary artery stenosis; AWI,
chronic anterior wall infarction; PWI, chronic posterior wall
infarction; DCM, dilated cardiomyopathy; DCMm and
DCMs, mild and severe DCM, respectively. Data are
mean +SD.
was 1.51±0.32 and increased in all six patients after
therapy to a value of 2.15±0.27; this increase was
statistically significant (p<0.01). The PDE/ATP ratio
was 1.14±0.76 before and 0.94+0.56 after treatment;
there was a decrease in four and an increase in two
patients; changes with therapy were not significant.
Thus, in patients with DCM, the CP/ATP ratio but
not the PDE/ATP ratio was inversely correlated to the
severity of heart failure and could be improved by
chronic drug therapy. Only the more severe cases of
DCM showed abnormal CP/ATP, which bore no correlation with parameters of LV function.
Discussion
Volunteers
In this report, we measured cardiac anteroseptal
CP/ATP and PDE/ATP ratios using ISIS as a singlevolume technique. CP/ATP values obtained for volunteers (T,-corrected, 1.64±0.26 [SD]) are comparable to
results reported from other groups. Uncorrected CP/
ATP was 1.55±0.20 (SD),18 1.33±0.19 (SEM),"1
1.6±0.4 (SD),5 and 1.58±1.69.19 TI-corrected CP/ATP
was 1.72+0.15 (SEM)4 or 1.64±0.08 (SEM).12 After
spectra were corrected for the presence of blood, the
volunteer CP/ATP ratio increased to 1.95+±0.45, i.e., by
19%. Reported blood20,21 and blood- and Tl-corrected
CP/ATP ratios are 1.71±0.12 (SEM),20 1.5+0.2 (SD),2'
1.80±0.06 (SEM),12 and 2.0±0.4 (SD).22 These values
are all comparable and are also close to numbers
reported for blood-perfused animal hearts.23-25 Thus,
although our volunteer group was not age-matched,
there are no indications that an age dependence of the
CP/ATP ratio exists that could influence our findings.
Few studies have reported on the PDE/ATP ratio, and
the available data show considerable scatter: 1.76±0.22
(SEM),12 0.29±0.08 (SEM),1" 0.84+0.08 (SEM),26 or
1.06±0.53 (SD), as reported here. The reasons for
substantially differing PDE/ATP ratios in these studies
remain unclear at present, although a partial explanation may be varying acquisition delays.'2 From our
measurements of the PDE/2,3-DPG ratio in blood, we
calculate that 26% of the cardiac PDE peak arose from
blood contamination, and thus, only 74% of the PDE
3OT
2.5f
2.0
LL
0
CL)
3-OT
.
a
;
2.5+
0
11
0
all
0
1.5
2Dl
0
8.1
0
01.
0
I-
011
a
11
0
a
1.0
1.1 1.5'
W
*
1'+ '' ;T~ ~ ~ ~ 1
CL1.
01
0.51
01
0,
II
n-rn
m
m-IV
0
0.1
B
11-m
m
m-Wv
FIGURE 5. Scatterplots showing creatine phosphate (CP)I
ATP (left panel) and phosphodiesters (PDE)IATP (right
panel) in patients with dilated cardiomyopathy graded according to the New York Heart Association (NYHA) classification. For each NYMI4 class, raw and mean data are shown.
Correlation between the NYHA grade and CPIATP was
highly significant (r=0.60; p<0.005).
1816
Circulation Vol 86, No 6 December 1992
2.5
2.0 I
U
FIGURE 6. Graphs showing creatine phosphate
(CP)IATP (left panel) and phosphodiesters PDE/
ATP (right panel) ratios before and after 12±6 weeks
of drug therapy in six patients with dilated cardiomyopathy. There was a significant increase of CP/ATP
from 1.51±0.32 to 2.15±0.27 (*p<0.01).
C.
[L
1.5
1.0
L
pc.01
-
0.5
0.0
before
[
after therapy
bor
before
p=NSatrh
after thearapy
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
signal originated from heart muscle. Therefore, PDE/
ATP ratios may also vary depending on the degree of
blood contamination. Because all published values were
obtained at 1.5-2 T, the well-described field dependence of PDE27,28 should not be a major factor influencing PDE/ATP ratios.
Coronary Artery Disease
In patients with LAD stenosis, we studied energy
metabolism of myocardium supplied by a highly stenotic
coronary artery at rest. Normal metabolite ratios indicate that alterations of energy metabolism do not occur
under these conditions. This is in agreement with the
findings of Weiss et al,4 who reported normal CP/ATP
in anterior myocardium supplied by a stenotic LAD. In
addition, these authors demonstrated that the CP/ATP
ratio decreased significantly during exercise. We also
found normal CP/ATP and PDE/ATP in patients with
AWI and PWI. In AWI, because of a relatively large
selected volume (up to 114 cm3), we obtained signal
from residual myocardium adjacent to the infarct zone
and from scar tissue. Since myocardial scar tissue presumably contains little or almost no ATP, however, the
acquired signal most likely arose almost exclusively from
residual intact myocardium. In PWI patients, spectra
from residual intact myocardium remote from the infarct scar were acquired. Normal metabolite ratios in
AWI and PWI patients indicate that energy metabolism
at rest is unaltered in residual myocardium. It remains
to be determined whether such patients will show
altered energy metabolism during exercise. To date,
there are no other studies examining anterior wall 31P
spectra after PWI. One study by Bottomley et al5 has
reported reduced CP/inorganic phosphate (Pi) and increased Pi/ATP ratios in some spectra obtained from
patients examined 5-9 days after AWI. In our spectra,
we were unable to resolve the Pi resonance from the
overlapping 2,31-DPG resonances and thus could not
evaluate changes of the Pi resonance. Hardy et al'2 have
reported reduced CP/ATP (1.53+±0.07 versus 1.80±0.06
in volunteers, SEM) in patients with congestive heart
failure resulting from severe multivessel CAD (presumably patients who had myocardial infarctions months to
years before), but none of our patients with myocardial
infarction and normal CP/ATP ratios had signs of
failure. Systematic sequential studies of the changes in
energy metabolism after myocardial infarction in conjunction with invasive and noninvasive evaluation of
altered hemodynamics (remodeling) are needed to further clarify these points.
Dilated Cardiomyopathy
In this study, we report that as a group including all
clinical stages, the CP/ATP ratio in patients with DCM
tended to be lower (1.78±0.51, SD) but was not significantly decreased compared with volunteers (1.95±
0.45). When patients were subdivided according to the
clinical severity of heart failure, however, the CP/ATP
ratio was progressively- reduced. There was no significant change in patients with mild heart failure, but there
was a marked reduction of CP/ATP in advanced stages
of heart failure. CP/ATP ratios showed a highly significant correlation with the NYHA class (p<0.005). No
correlation could be detected between measurements of
LV function (FS, EF) and CP/ATP or PDE/ATP ratios.
The presence of a correlation of CP/ATP with the
clinical status in the absence of a correlation with direct
functional indexes may be related to the fact that not all
DCM patients with low EFs immediately develop the
full clinical syndrome of heart failure. The clinical
syndrome of severe heart failure is characterized by
neurohumoral activation, and it is likely that this was
the case in DCM patients with severe heart failure,
whereas DCM patients with discrete signs of heart
failure have only slightly elevated catecholamine, renin,
and vasopressin levels.29,30 Changes in high-energy
phosphate metabolism of the heart may therefore be
dependent in part on the full clinical syndrome of
congestive heart failure, including neurohumoral activation and sodium and water retention. Our findings are
in line with the few reports available on this issue.
Hardy et al'2 reported reduced CP/ATP (1.41+0.12
versus 1.80±0.06 in volunteers, SEM) in patients with
DCM and overt cardiac failure; these authors also were
unable to demonstrate a correlation of LVEF and
CP/ATP or PDE/ATP. Reduced CP/ATP ratios have
also been described by Luyten et a122 (0.56±0.16, SD)
and Rajagopalan et a131 (0.9) in patients with severe
DCM. In the first study available on human DCM,
Whitman et a132 reported on an infant with severe DCM
in whom the CP/ATP ratio increased from 1.3 to 2.0
upon intravenous infusion of glucose. Similar to our
findings, in patients with DCM not classified for the
severity of heart failure, Schaefer et all' found a trend
toward a decrease of the CP/ATP ratio (0.70±0.12
versus 0.89±0.08 in volunteers, SEM), which was not
significant. Reduced CP/ATP is probably linked to the
Neubauer et al Energy Metabolism in CAD and DCM
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
presence of heart failure by a common mechanism
nonspecific for DCM: In patients with aortic stenosis or
aortic incompetence, Conway et a121 reported reduced
CP/ATP (1.10+0.32, SD) in the presence but normal
CP/ATP (1.56+0.15) in the absence of heart failure.
CP/ATP was also reduced (1.53±0.07 versus 1.80±0.06
in volunteers, SEM) in cardiac failure resulting from
ischemic heart disease.12
To the best of our knowledge, this is the first report
on patients with DCM and clinical heart failure that
demonstrates changes of the CP/ATP ratio during medical treatment leading to clinical recompensation. We
found that concomitantly with the improvement of
NYHA class (by 0.8±0.3 classes), the CP/ATP ratio
increased from 1.51+0.32 to 2.15+0.27 (p<0.05). This
indicates that cardiac energy metabolism improved in
parallel with the clinical status. The most likely explanation of improved high-energy phosphate metabolism
is an improved hemodynamic milieu with reductions in
both preload and afterload, probably caused by ACE
inhibition and diuretics. Purely speculatively, there may
also be a direct beneficial effect of either the ACE
inhibitor and/or the a-blocker; both classes of agents
have been shown to protect cardiac energy metabolism
during metabolic stress.33,34 Controlled studies with
larger patient numbers are needed to further elucidate
these points.
We do not believe that changes in energy metabolism
are an artifact of changes in selected spectroscopic
volumes: Spectra were corrected for the presence of
blood, and in addition, the ATP/2,3-DPG ratio of
cardiac spectra was 0.53±0.19 before and 0.46+0.25
(p=NS) after therapy, indicating that the percentage of
selected volume contaminated by blood was similar
before and after treatment. Thus, we assume that
spectral changes observed with treatment were a result
of intrinsic metabolic recovery of myocardial tissue. At
the time of spectroscopy, heart rate was slightly, although significantly, higher before (91±+7 beats per
minute) than after (82±9 beats per minute) treatment
(p<0.05). Thus, changes in CP/ATP may result in part
from reduced work load after therapy. Experimentally,
however, blood-perfused hearts show little variation of
high-energy phosphate ratios with changing work load
conditions.35
Our findings do not allow us to discriminate whether
the observed changes of CP/ATP in severe DCM are a
cause for or only an epiphenomenon of heart failure.
However, a number of studies using various models of
cardiac hypertrophy and failure3,7,8,36,37 have uniformly
demonstrated reduced CP/ATP ratios occurring simultaneously with the depression of cardiac contractile
function, suggesting an essential role for energy metabolism in the development of heart failure. One mechanism for reduced CP/ATP in heart failure is probably
depletion of the total creatine pool: Nascimben et a138
reported a 57% reduction of total creatine in patients
with DCM.
In our study, no significant alterations of the PDE/
ATP ratio were observed in patients with DCM. This is
in agreement with Hardy et a112 but in disagreement
with others who observed increased PDE/ATP.1,26 We
could not reproduce the correlation of PDE/ATP and
LVEF reported by Auffermann et al.26 Although increased PDE/ATP ratios were attributed to increased
1817
membrane damage,39 Luyten et a122 recently showed
that increased PDE/ATP was entirely attributable to
increased blood contamination of spectra in DCM. We
could not reproduce this finding, because PDE/ATP
ratios were not elevated in DCM. Our findings indicate
that the PDE/ATP ratio is not a useful parameter for
characterizing patients with DCM.
Limitations
Using ISIS as a single-volume technique, we had to
use relatively large selected volumes for the spectroscopy protocol. Multiple voxel techniques, currently unavailable for all but a few clinical MR systems, allow for
smaller selected volumes and, thus, better spatial resolution with, possibly, determination of endocardial/
epicardial gradients of energy metabolism as well as
determination of intracellular Pi and pH.2240 Also, at
present, the technique does not allow absolute quantification of CP and ATP. Thus, although CP/ATP ratios
were unchanged after myocardial infarction and in mild
DCM, we would not be able to detect simultaneous
proportional reductions of both CP and ATP. Possible
solutions to overcome this problem may be on the way.41
Furthermore, we varied the ISIS volume between 46
and 114 ml; using computer simulation, Lawry et a142
have shown that, in an ISIS experiment, the degree of
contamination from signal outside the selected volume
may depend on the size of the selected volume itself.
We selected the ISIS volume to include as much heart
muscle as possible and cannot exclude the possibility
that such effects might constitute an error source. It
should also be mentioned that all spectra were obtained
at rest, and establishment of routine exercise standards
should greatly enhance the sensitivity of the technique
for detecting diseased myocardium.4,43 Finally, the approach of blood-correcting spectra, which is at present
taken by most groups using cardiac 31p MR spectroscopy, may have certain limitations: first, blood 31p_
observable metabolites may undergo changes with disease states44; second, the Pi resonance is included in the
area of the 2,3-DPG peaks, and if Pi is increased in
DCM, overcorrection of the CP/ATP ratio might occur;
third, the blood ATP/2,3-DPG ratio may change with
the degree of oxygen saturation45 and may, thus, vary
depending on the degree of right versus left chamber
blood contamination. Although we would not expect
any of these factors to profoundly change our results, an
exact evaluation is problematic at present.
In summary, we found unchanged myocardial highenergy phosphate metabolism at rest in patients with
CAD. Alterations in energy metabolism do occur
in advanced but not in mild cases of DCM; such
changes correlate with the severity of heart failure and
can be improved with treatment leading to clinical
recompensation.
References
1. Clarke K, O'Connor AJ, Willis RJ: Temporal relation between
energy metabolism and myocardial function during ischemia and
reperfusion. Am J Physiol 1987;253:H412-H421
2. Hollis DP, Nunnally RL, Taylor GJ, Weisfeld ML, Jacobus WE:
Phosphorus nuclear magnetic resonance studies of heart physiology. J Magn Reson 1978;29:319-330
3. Neubauer S, Horn M, Gaudron P, Hu K, Laser M, Voll J, Tian R,
Ingwall JS, Ertl G: Susceptibility of chronically infarcted heart to
1818
4.
5.
6.
7.
8.
9.
10.
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
Circulation Vol 86, No 6 December 1992
hypoxia and reoxygenation: A 31p NMR study. (abstract) Circulation 1991;84(suppl II):II-27
Weiss RG, Bottomley PA, Hardy CJ, Gerstenblith G: Regional
myocardial metabolism of high-energy phosphates during isometric exercise in patients with coronary artery disease. N Engl J Med
1990;323:1593-1600
Bottomley PA, Herfkens RJ, Smith LS, Bashore TM: Altered
phosphate metabolism in myocardial infarction: P-31 NMR spectroscopy. Radiology 1987;165:703-707
Bittner V, Reeves RC, Digerness SB, Caulfield JB, Pohost GM:
Myocardial phosphocreatine depletion after chronic adriamycin
exposure. Proc 7th Annu Meet SMRM 1988;1:275
Markiewicz W, Wu SS, Parmley WW, Higgins CB, Sievers R,
James TL, Wikman-Coffelt J, Jasmin G: Evaluation of the hereditary Syrian hamster cardiomyopathy by 31P nuclear magnetic resonance spectroscopy: Improvement after acute verapamil therapy.
Circ Res 1986;59:597-604
Ingwall JS, Atkinson DE, Clarke K, Fetters JK: Energetic correlates of cardiac failure: Changes in the creatine kinase system in
the failing myocardium. Eur Heart J 1990;2(suppl C):108-115
Ingwall JS: On the hypothesis: Cardiac failure is due to decreased
energy reserve. (in press)
Bashore TM, Magorien DJ, Letterio J, Shaffer P, Unverferth DV:
Histologic and biochemical correlates of left ventricular chamber
dynamics in man. JAm Coll Cardiol 1987;9:734-742
Schaefer S, Gober JR, Schwartz GG, Twieg DB, Weiner MW,
Massie B: In vivo phosphorus-31 spectroscopic imaging in patients
with global myocardial disease. Am J Cardiol 1990;65:1154-1161
Hardy CJ, Weiss RG, Bottomley PA, Gerstenblith G: Altered
myocardial high-energy phosphate metabolites in patients with
dilated cardiomyopathy. Am Heart J 1991;122:795-801
Ordidge RJ, Connelly A, Lohman JAB: Image-selected in vivo
spectroscopy (ISIS): A new technique for spatially selective NMR
spectroscopy. J Magn Reson 1985;66:283-294
Neubauer S, Krahe T, Schindler R, Hillenbrand H, Entzeroth C,
Horn M, Bauer WR, Stephan T, Lackner K, Haase A, Ertl G:
Direct measurement of spin-lattice relaxation times of phosphorus
metabolites in human myocardium. Magn Reson Med (in press)
Minakami S, Suzuki C, Saito T, Yoshikawa H: Studies on erythrocyte glycolysis: I. Determination of the glycolytic intermediates
in human erythrocytes. J Biochem 1965;58:543-550
Beutler E: The erythrocyte, in Williams WJ, Beutler E, Erslev AJ,
Lichtman MA (eds): Hematology, ed 3. New York, McGraw-Hill
Book Co Inc, 1983, pp 283-284
Zar JH: BiostatisticalAnalysis. Englewood Cliffs, NJ, Prentice Hall,
1974, pp 130-181
Blackledge MJ, Rajagopalan B, Oberhaensli RD, Bolas NM, Styles
P, Radda G: Quantitative studies of human cardiac metabolism by
31P rotating-frame NMR. Proc Natl Acad Sci U S A 1987;84:
4283-4287
Grist TM, Kneeland JB, Rilling WR, Jesmanowicz A, Froncisz W,
Hyde JS: Gated cardiac MR imaging and P-31 MR spectroscopy in
humans at 1.5 T. Radiology 1989;170:357-361
Sakuma H, Takeda K, Tagami T, Kinosada Y, Nakagawa T, Okamoto S, Konishi T, Nakano T: P-31 MR spectroscopy in hypertrophic cardiomyopathy with correction of blood contamination:
Comparison with T1-201 myocardial perfusion imaging. Proc 10th
Annu Meet SMRM 1991;1:75
Conway MA, Allis J, Ouwerkerk R, Niioka T, Rajagopalan B,
Radda GK: Detection of low phosphocreatine to ATP ratio in
failing hypertrophied human myocardium by 31p magnetic resonance spectroscopy. Lancet 1991;338:973-976
Luyten PR, de Roos A, Oosterwaal LJMJ, Doornbos J, den Hollander JA: PCr/ATP ratio and pH values in dilated and hypertrophic cardiomyopathy patients determined by 31P NMR heart
spectroscopy. Proc 10th Annu Meet SMRM 1991;1:74
Camacho SA, Lanzer P, Toy BJ, Gober J, Valenza M, Botvinick
EH, Weiner MW: In vivo alterations of high-energy phosphates
and intracellular pH during reversible ischemia in pigs: A 31P
magnetic resonance spectroscopy study. Am Heart J 1988;116:
701-708
Guth BD, Martin JF, Heusch G, Ross J: Regional myocardial
blood flow, function and metabolism using phosphorus-31 nuclear
magnetic resonance spectroscopy during ischemia and reperfusion
in dogs. JAm Coll Cardiol 1987;10:673-681
Robitaille PM, Lew B, Merkle H, Sublett E, Lindstrom P, From
AHL, Garwood M, Bache B, Ugurbil K: Transmural metabolite
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
distribution in regional myocardial ischemia as studied with 31P
NMR. Magn Reson Med 1989;10:108-118
Auffermann W, Chew W, Wolfe CL, Tavares NJ, Parmley WW,
Semelka RC, Donnelly T, Chatterjee K, Higgins CB: Normal and
diffusely abnormal myocardium in humans: Functional and metabolic characterization with P-31 MR spectroscopy and cine MR
imaging. Radiology 1991;179:253-259
Hardy CJ, Bottomley PA, Roemer PB, Redington RW: Rapid 31p
spectroscopy on a 4 T whole-body system. Magn Reson Med 1988;
8:104-109
Bates TE, Williams SR, Gadian DG: Phosphodiesters in the liver:
The effect of field strength on the 31P signal. Magn Reson Med
1989;12:145-150
Dzau VJ, Colucci WS, Williams GH, Hollenberg NK: Relation of
renin-angiotensin-aldosterone to clinical state in congestive heart
failure. Circulation 1981;63:645-651
Francis GS, Benedict C, Johnstone DE, Kirlin PC, Nicklas J, Liang
C, Kubo SH, Rudin-Toretsky E, Yusuf S: Comparison of neuroendocrine activation in patients with left ventricular dysfunction
with and without congestive heart failure. Circulation 1990;82:
1724-1729
Rajagopalan B, Blackledge MJ, McKenna WJ, Bolas N, Radda
GK: Measurement of phosphocreatine to ATP ratio in normal and
diseased human heart by 31P magnetic resonance spectroscopy
using the rotating frame-depth selection technique. Ann N YAcad
Sci 1987;508:321-332
Whitman GR, Chance B, Bode H, Maris J, Haselgrove J, Kelley R,
Clark BJ, Harken AH: Diagnosis and therapeutic evaluation of
pediatric cardiomyopathy using 31P-NMR. JAm Coil Cardiol 1985;
5:745-749
Rahusen FD, van Gilst WH, Robillard GT, Dijkstra K, Wildevuur
CRH: Captopril improves recovery of adenosine triphosphate during reperfusion of the ischemic isolated rat heart: A 31-phosphorus-nuclear magnetic resonance study. Basic Res Cardiol 1988;83:
540-549
Nakazawa M, Katano Y, Imai S, Matsushita K, Ohuchui M: Effects
of /- and d-propranolol on the ischemic myocardial metabolism of
the isolated guinea pig heart as studied by 31P-NMR. J Cardiovasc
Pharmacol 1982;4:700-704
Ligeti L, Osbakken MD, Clark BJ, Schnall M, Bolinger L, Subramanian H, Leigh JS, Chance B: Cardiac transfer function relating
energy metabolism to workload in different species as studied by
31P NMR. Magn Reson Med 1987;4:112-119
Buser PT, Auffermann W, Wu ST, Jasmin G, Parmley WW, Wikman-Coffelt J: Dobutamine potentiates amrinone's beneficial
effects in moderate but not in advanced heart failure: 3`P-MRS in
isolated hamster hearts. Circ Res 1990;676:747-753
Shimamoto N, Goto N, Tanabe M, Imamoto T, Fujiwara S, Hirata
M: Myocardial energy metabolism in the hyperthyroid hearts of
spontaneously hypertensive rats. Basic Res Cardiol 1982;77:
359-371
Nascimben L, Pauletto P, Pessina AC, Reis I, Ingwall JS:
Decreased energy reserve may cause pump failure in human
dilated cardiomyopathy. Circulation 1991;84(suppl lI):II-563
Katz AM, Freston JW, Messineo FC, Herbette LG: Membrane
damage and the pathogenesis of cardiomyopathies. J Mol Cell
Cardiol 1985;17(suppl 2):11-20
Bottomley PA, Weiss RG, Hardy C, Gerstenblith G: 31P NMR
stress testing in patients with coronary disease: Evidence for myocardial PCr/Pi changes. Proc 10th Annu Meet SMRM 1991;2:577
Bottomley PA, Hardy CJ, Roemer PB: Phosphate metabolite imaging and concentration measurements in human heart by nuclear
magnetic resonance. Magn Reson Med 1990;14:425-434
Lawry TJ, Karczmar GS, Weiner MW, Matson GB: Computer
simulation of MRS localization techniques: An analysis of ISIS.
Magn Reson Med 1989;9:299-314
Conway MA, Radda GK: Nuclear magnetic resonance spectroscopic investigations of the human myocardium. Trends Cardiovasc
Med 1991;1:300-304
Horn M, Neubauer S, Schmidt M, Kadgien M, Schnackerz K, Ertl
G: 31P-MR spectroscopy of human blood and serum: Results from
volunteers and patients with congestive heart failure and diabetes
mellitus. Proc 1Oth Annu Meet SMRM 1991;1198
Ouwerkerk R, van Echteld CJA, Staal GEJ, Rijksen G: Intracellular free magnesium and phosphorylated metabolites in hexokinase- and pyruvate kinase-deficient red cells measured using 31PNMR spectroscopy. Biochim Biophys Acta 1989;1010:294-303
31P magnetic resonance spectroscopy in dilated cardiomyopathy and coronary artery
disease. Altered cardiac high-energy phosphate metabolism in heart failure.
S Neubauer, T Krahe, R Schindler, M Horn, H Hillenbrand, C Entzeroth, H Mader, E P
Kromer, G A Riegger and K Lackner
Downloaded from http://circ.ahajournals.org/ by guest on October 1, 2016
Circulation. 1992;86:1810-1818
doi: 10.1161/01.CIR.86.6.1810
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1992 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/86/6/1810
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/