TRS-ActiveCare Drug Prior Authorization & Quantity Limits
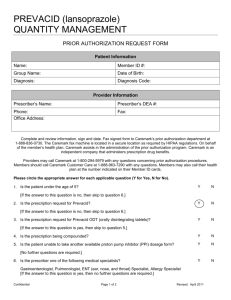
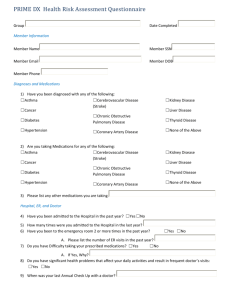
advertisement

TRS-ActiveCare Prior Authorization, Quantity Limit and Step Therapy List Certain prescription drugs are subject to step therapy requirements, prior authorization requirements and quantity limits. These programs are in place to ensure appropriate use of these medications. Prior Authorization Your doctor needs to get prior authorization for the drugs listed below before your prescription benefit plan administered by Caremark will cover them. Anti-Obesity Medications Adipex-P Bontril PDM Diethylpropion Qsymia Xenical Belviq Bontril SR Phendimetrazine ER/SR Regimex (benzphetamine) Contrave Benzphetamine Didrex Phentermine Suprenza Attention Deficit Hyperactivity Disorder (ADHD) and Narcolepsy Medications (Prior Authorization Required for 19 Years and Older) Adderall Adderall XR Concerta Daytrana Desoxyn Dexedrine Focalin Products LiQuadd/ProCentra Metadate Products Methylin Products Quillivant XR Susp Ritalin Products Strattera Vyvanse Dextroamphetamine Products Evekeo GLP-1 Agonists Bydureon Tanzeum Byetta Trulicity Victoza Narcolepsy Medications Nuvigil Provigil Xyrem Oral/Intranasal Fentanyl Medications Abstral Actiq Lazanda Onsolis Testosterone Topical/Buccal Medications Androderm Axiron Striant Fentora Subsys Fortesta Topical Acne Medications (Prior Authorization Required for 35 Years and Older) Atralin Fabior Tazorac Veltin Avita Retin-A Tretinoin Ziana Differin Retin-A Micro Tretin-X Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Quantity Limits The drugs listed below have limits based on U.S. Food and Drug Administration (FDA)approved prescribing information, approved medical guidelines and/or the average utilization quantity for the drugs. The limits listed below affect only the amount of medication that the prescription benefit plan pays for, not whether you can get a greater quantity. The final decision about the amount of medication you receive remains between you and your doctor. Note: Some of the quantity limits have a prior authorization available if you exceed the drug’s limit. Those drugs with a prior authorization available are noted in chart below. If your doctor has determined that a greater amount is appropriate, your doctor should call Caremark toll-free at 1800-294-5979 to request prior authorization for a larger quantity. The prior authorization line is for your doctor’s use only. Antiemetic Medications Quantity Limit With Post Limit Prior Authorization Aloxi 1 vial (5 mL) per 15 days Anzemet Tablets 3 tabs per 15 days Cesamet 18 per 30 days Emend 115 mg injection 1 vial per 15 days Emend 125 mg 1 cap per 15 days Emend 150 mg injection 1 vial per 15 days Emend 40 mg 3 caps per 180 days Emend 80 mg 2 caps per 15 days Emend Bi-Pak 1 bi-pak per 15 days Emend Tri-Pak 1 tri-pak per 15 days Granisol (Granisetron) Oral Solution 30 mL per 15 days Kytril (Granisetron) 1 mg tab 6 per 15 days Kytril (Granisetron) injection 1 mL per 15 days Marinol (dronabinol) 60 per 30 days Sancuso 1 patch per 15 days Zofran (Ondansetron) 24 mg tab 1 per 15 days Zofran (Ondansetron) 2 mg/mL injection 10 mL per 15 days Zofran (Ondansetron) 4 and 8 mg ODT 12 per 15 days Zofran (Ondansetron) 4 and 8 mg tabs 12 per 15 days Zofran (Ondansetron) oral solution 100ml per 15 days Zuplenz 4 and 8 mg films 12 per 15 days Antiemetic Medications Anzemet Injection 5 mL per15 days Antimigraine Medications Quantity Limit With Post Limit Prior Authorization Alsuma (sumatriptan) injection 12 per 30 days Amerge (naratriptan) 12 per 30 days Axert 12 per 30 days Frova 18 per 30 days Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Imitrex (sumatriptan) 20 mg nasal spray Imitrex (sumatriptan) 5 mg nasal spray Imitrex (sumatriptan) injection Imitrex (sumatriptan) tabs Maxalt/Maxalt MLT (rizatriptan) tabs Relpax Sumavel Treximet Zomig (zolmitriptan) nasal spray Zomig/Zomig ZMT (zolmitriptan) tabs 12 per 30 days 24 per 30 days 12 per 30 days 12 per 30 days 18 per 30 days 12 per 30 days 12 per 30 days 9 per 30 days 12 per 30 days 12 per 30 days Antimigraine Medications Migranal NS 8 mL per 30 days Erectile Dysfunction Medications Caverject Cialis 10 mg/20 mg Edex Levitra Muse Staxyn Stendra Viagra 8 per 30 days 8 per 30 days 8 per 30 days 8 per 30 days 8 per 30 days 8 per 30 days 8 per 30 days 8 per 30 days Erectile Dysfunction Medications Quantity Limit With Post Limit Prior Authorization Cialis 2.5 mg/5 mg 8 per 30 days Influenza Medications Quantity Limit With Post Limit Prior Authorization Relenza 40 caps per 180 days Tamiflu 45 mg and 75 mg caps 14 per 180 days Tamiflu 30 mg caps 28 per 180 days Tamiflu oral suspension 180 mL per 180 days Pain/Stadol Medications Quantity Limit With Post Limit Prior Authorization Stadol NS 5mL per 30 days Sedative/Hypnotic Medications Doral Estazolam Flurazepam Halcion Restoril 15 per 30 days 15 per 30 days 15 per 30 days 10 per 30 days 15 per 30 days Sedative/Hypnotic Medications Quantity Limit With Post Limit Prior Authorization Ambien (zolpidem) 15 per 30 days Ambien CR (zolpidem) 15 per 30 days Lunesta (eszopiclone) 15 per 30 days Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Sonata (zaleplon) 15 per 30 days Toradol/Sprix Medications Sprix Toradol 5 bottles per 30 days 20 tabs per 30 days Step Therapy You are required to try a specific drug before your prescription benefit plan will cover one of the drugs listed below. Your doctor may call Caremark to request prior authorization for these drugs. Atypical Antipsychotics Abilify Invega Seroquel (Brand Only) Fanapt Latuda Seroquel XR Minocycline ER Brand Only Solodyn Ximoni Geodon (Brand Only) Saphris Generic Step Therapy Step 1: You may have to try one Drug Class Condition Treated** or two* of these generic medications first: Step 2: Before you can try one of these brand drugs: These preferred select brand drugs do not require use of a generic first: Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 ACE Inhibitors/Angiotensin II Receptor Antagonists (ARBs)/ Direct Renin Inhibitors/ Combinations High Blood Pressure amlodipine-benazepril Tekturna/Tekturna HCT Benicar/Benicar HCT Preferred select brand not available in class benazepril/benazepril HCTZ candesartan/candesartan HCTZ captopril/captopril HCTZ enalapril/enalapril HCTZ eprosartan fosinopril/fosinopril HCTZ irbesartan/irbesartan HCTZ lisinopril/lisinopril HCTZ losartan/losartan HCTZ moexipril/moexipril HCTZ quinapril/quinapril HCTZ *Please note. A member’s Plan determines whether one or two generics must be tried first. ramipril telmisartan/telmisartan HCTZ trandolapril trandolapril-verapamil ext-rel valsartan/valsartan HCTZ Acne/Topical benzoyl peroxide Acanya Skin clindamycin solution Azelex clindamycin-benzoyl peroxide erythromycin solution erythromycin-benzoyl peroxide sodium sulfacetamide sulfacetamide-sulfur Benign Prostatic Hyperplasia-Alpha blockers alfuzosin ext-rel Cardura XL Preferred select brand not Prostate doxazosin Rapaflo available in class tamulosin terazosin Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Benign Prostatic Hyperplasia5 Alpha Reductase Inhibitors/Combinations finasteride Avodart available in class Prostate Bisphosphonates/Combinations alendronate Atelvia Osteoporosis ibandronate Binosto risedronate 150 mg Fosamax Plus D COX-2 Inhibitors/Nonsteroidal Anti-Inflammatory (NSAIDs)/ Combinations celecoxib Cambia diclofenac sodium/misoprostol Nalfon Pain and Inflammation diclofenac sodium Voltaren Gel diclofenac sodium solution Zipsor ibuprofen Zorvolex *Please note. A member’s Plan determines whether one or two generics must be tried first. Preferred select brand not Preferred select brand not available in class Preferred select brand not available in class meloxicam naproxen (additional generic NSAIDs available) Fibrates gemfibrozil Fenoglide Preferred select brand not High Triglycerides fenofibrate Triglide available in class amlodipine-atorvastatin Crestor (excluding 40 mg) atorvastatin Simcor Preferred select brand not available in class fluvastatin Vytorin fenofibric acid HMG-CoA Reductase Inhibitors (HMGs or Statins)/Combinations High Cholesterol lovastatin niacin ext-rel pravastatin simvastatin Ophthalmic/Prostaglandins latanoprost Travatan Z Glaucoma travoprost Zioptan Preferred select brand not available in class Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Proton Pump Inhibitors (PPIs) lansoprazole Dexilant Stomach Acid omeprazole Nexium omeprazole-sodium bicarbonate capsule Prilosec Packets *Please note. A member’s Plan determines whether one or two generics must be tried first. pantoprazole Preferred select brand not available in class Zegerid Powder for Oral Susp rabeprazole Selective Serotonin Agonists/ Combinations Migraine naratriptan Alsuma rizatriptan Axert sumatriptan Frova zolmitriptan Relpax Preferred select brand not available in class Sumavel Dosepro Treximet Serotonin Norepinephrine Reuptake Inhibitors (SNRIs) Depression duloxetine Fetzima venlafaxine/venlafaxine ext-rel Khedelza Preferred select brand not available in class Pristiq Selective Serotonin Reuptake Inhibitors (SSRIs) Depression citalopram Brintellix escitalopram Pexeva fluoxetine Viibryd Preferred select brand not available in class fluvoxamine/fluvoxamine ext-rel paroxetine/paroxetine ext-rel sertraline Sleeping Agents eszopiclone Edluar Insomnia/Sleep Problems zaleplon Silenor zolpidem/zolpidem ext-rel Zolpimist Preferred select brand not available in class zolpidem ext-rel Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614 Urinary Antispasmodics oxybutynin/oxybutynin ext-rel Enablex Overactive Bladder/Incontinence tolterodine/tolterodine ext-rel Gelnique trospium/trospium ext-rel Myrbetriq *Please note. A member’s Plan determines whether one or two generics must be tried first. Preferred select brand not available in class Vesicare Log in to www.caremark.com to check coverage and copay information for a specific drug. Discuss this information with your doctor or health care provider. This information is not a substitute for medical advice or treatment. Talk to your doctor or health care provider about this information and any health-related questions you have. Caremark assumes no liability whatsoever for the information provided or for any diagnosis or treatment made as a result of this information. This document contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with Caremark. This list is subject to change. There may be additional plan restrictions. Please consult your plan for further information. 106-T31719a 071614