Intravascular ultrasonography versus digital subtraction angiography
advertisement

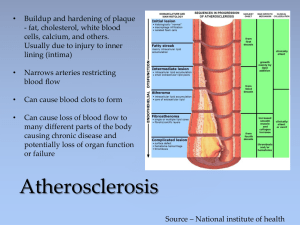
-~.-___~ --_-_--- --.. - ___..._ -_-_ .__ ..-.--_ _ -.- _- .--__ -_ Conventional angiography has generally been considered the gold standard in vivo method for assessing luminal diameter. luminal area and extent or severity of atherosclerotic disease. However. the accur.tcy of visual assessments of the physiologic significance of stenosis has been recently qucstioned (1). Even angiographic determination of left main coronary artery stenosis is subject to considerable error when compared with histologic deter ination (2). Although __- .--. From the Department of Medicine. Divihiun ofCardiology. Duke !_lni&~ sily Medical Center. Durham. North C;mGx~. Thk study wit\ pre\entcd in part at the 39th Annual Scientific Sesion of the American College 01 Cardiology. New Orleans. Louisiana. March IYYO. II WB\ cupported in part hy Na~ionaB Research Service Award Grant 5T37HL tJ71111fr~~rn the N;ttional Heart. Lung. and Blood Institute. National Institute\ of Health. Ht~the~da. Mar?/hnd. anuscripl received December !I. 19x9: revkd manuxript received March 7. 1990. accepted March 26. IYYO. Address forrenrints: Charles 9. Davidson. MD. Duke UntverGty Medical Center. Deparlmenl of Medicine. Diwsion of Cxdiolop. Box 31195. Durham. North Carolinlr 27710. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 _ ~~t~tomated q~aatitative angiography overcomes so limitations of visual assessment of coronary stenosis 63.4). its ability to define vessel morphology is limited. The feasibility of intravascular u~t~aso~o~raphy to provide real-time two-dimensional images of arteries and veins has recently been demonstrated in vitro and in vivo 6-9). Catheter-based ultrasonography is able to define intraluminal morphology including delineation of plaque characteristics. To date, this imaging approach has been shown to provide data regarding luminal diameter and area that are similar to those from pathologic sections of arterial Wall. animal models indicate that go ssel diameter and area by ultras compared with c~~~iper~de~iv tative ci~lea~~jo~raphy (101. owever. few data exist from humans in vivo. The purposes of this hu an in viva study were to graphic and digital subcompare catheter-based ultt ts of arterial lumen size traction angiographic measu 634 DAVIDSON ET AL. C’LTRASONOGRAPHY VERSUS ANGIOGRAPHY and to contrast the ability of the two techniques !esion morphology. to define Study patients. Twenty-one patients undergoing diagnostic cardiac catheterization were enrolled in the study according to a protocol that had been previously approved by the Institutional Review Board. There were I3 men and 8 women whose mean age was 55 + I9 years (range 24 to 83). Indication for catheterization was chest pain in 9 patients and valvular heart disease in 12. Ultrasound and digital subtraction images were obtained in 86 arterial segments that included 49 femoral, 3 renal, 5 iliac, 7 pulmonary and 22 aortic sites. Ultrasound images. The ultrasound transducer was a 20 MHz, 1.75 mm aperture, single piezoelectric crystal transducer bonded to a guide wire and housed within a 6F blunt-tipped or an 8F monorail over-the-wire catheter sheath (Boston Scientific CorporationlDiasonics). The transducer was mechanically rotated within the catheter at 1,800 rpm to provide cross-sectional images and was connected to an ultrasourrd diagnostic imaging console specifically designed for display of the two-dimensional images. The ultrasound beam was em:rted at a IO” forward look angle. The framing rate was I5 frames/s and the images were displayed on a video monitor on a 512 x 512 pixel matrix that discriminated 64 shades of gray. All images were recorded on 0.5 in. (I 27 cm) high fidelity videotape for subsequent off-line analysis. In vitro testing in our laboratory indicated that axial resolution and lateral resolution at a distance of 5 mm from the transducer tip were 0.39 and I .30 mm. respectively. Digital subtraction images. Images were recorded with an ADAC 4100-C digital radiography system interfaced to a General Electric-MPX L/U X-ray unit. Single plane anteriorposterior view images were acquired with use of a 9 in. (22.86 cm) image intensifier and fed into a 512 x 512 x 8 pixel matrix at 30 frames/s. All vessels of interest were centered to avoid pin-cushion distortion. R-wave-gated masked mode subtraction was performed after the procedure. All images were acquired and stored in digital format. TO ensure that ultrasound and digital images were acquired from the same arterial segment, a radiopaque graphic marker was placed on the patient at the point of ultrasound image acquisition. Subsequent quantitative and qrditative angiographic analyses were then performed at the corresponding marked segment. Hand injection of nonionic contrast medium was utilized for femoral and iliac artery radiographic images. Power hh3iOn Of 40 ml of nonionic contrast medium at 15 to 30 d/S was made for central aorta and pulmonary artery image acquisition. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 Quantitative data analysis. Ultrasound data analysis was performed by digitizing i computer and software titative measurements wer:: made for eter. Cross-sectional area ii~i%Sobtaine image displaying maximal arterial diameter ita the horizontal plane and maximal cross-sectional area was used for measurement. Diameter intraobserver variability for 10 i was r = 0.99. SFE = 0.03 mm and interobserver correlation was r = 0.99, sGk -; O.Gj server and int~r~~se~ver cm” and 0.99, SEE :- 0.08 Digital slrbtrcrctiott i’ng with a previously validat&, commercially available software program (I I, 12). A grid placed at the level of the artery was used for calibration. Absolute luminal diameter and crosssectional area were determined for the same seg artery that was imaged with intravascular ultrason QMalitat~ve analysis. Ultrasound images we tively evaluated by consensus agreement of tw for vessel morphology with use of a met suggested by Gussenhoven et al. (5). defined as intimal thickening with bright distal acoustic shadowing consistent with calcium, or Soft plaque lacked these characteristics and was repres as less dense echoes of thickened arterial wall. Data andysis. The correlation between angiographic an intravascular ultra nographic images was calculated wit linear regression. ata are expressed as mean values 2 SEE. Categoric data were analyzed with the chi-square test. Qime~siu~a~ correlates. The absolute luminal diameters for all (n = 86) arterial segments acquired by digital subtraction angiography and intravascular ultrasonography were closely related (r = 0.97, SEE = 1.83 mm). The linear correlation is described by the equation y = 0.85x + 2.7 (Fig. I). The correlation for arterial segments C IO mm in diameter (n = 53) was 0.87. SEE = I.25 mm, and for those IO to 40 mm (n = 32) it was 0.93, SEE = 2.40 mm. The arterial cross-sectional areas as visualized by both tcchniqaes were also closely related (r = 0.95, SEE = 0.65 cm’) and the correlation is described by the linear regression of y = 0.87x + 0.32 (Fig. 2). Angiographically determined cross-sectional area <I cm2 demonstrated a correlation coefficient of 0.93. SEE = 0. I4 cm’ and areas >1 cm* ex ted a correlation coefficient of 0.92, SEE = que correlates and lesion morphology (Table vascular ultrasonography identified 24 sites in which athemsclerotic plaque was present. In II (46%) of these 24 segments, the arterial lumen appeared to be ang~ogra~~ically normal. A representative example of a “normal” angiographic segment that demonstrated plaque on ultrasonogra- JACC Vol. 16. No. 3 September ~99~:~33-~ ihd Linear correlations of i~nii~~~ titative digital subtraction angiography M~trasono~~pby WM. ~travasc~iar The cot-t-elation of eecettrtic fo imeter derived by qwrn(DSAI and intravascular ared normal by intravascular ultrasonogra for detennittadotl of l~ttnit~~tl was simita arterial segments fr = 0.96, SEE = 0.82 ). The correlation toe graphically derived cross-sectional a tric plaque (n = 24) was 0.93, SEE regions excellent ~l~~i4e ia that for normal versus r = 0.96. subtraction angiography of femoral corresponding arterial right pranei = position T tally Figure 2. Linear correlation of luminal cross-sectional area derived by digital subtraction angiography (DSAI and intravascular ultrasonography (IVUS). Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 “silent” plaque is indicated by arrows. 636 DAVIDSON ET AL. ULTRASONOGRAPHY JACC Vol. 16, No. 3 September 1990:hJ3-6 VERSUS ANGlOGRAPHY these data without the potential confounding effects Of vasodilation inherent in the use of contrast agents. Thus. this new technique may more accurately determine arterial dimensions either during or after interventional therapy. Delineation of atherosclerotic plaque and vessel morphology. The two techniques were discordant in their ability to delineate the presence of atherosclerotic plaque. Although quantitative determinations were close@ related, on several occasions digital subtraction angiography failed to reveal focal areas of stenosis that were consistent with plaque by intravascular ultrasonography. It appears that intravascular ultrasonography may thus provide additional data regarding atherckclerotic plaque within arterial segments that are angiographically “silent.” In vitro studies utilizing intravascular ultrasonography indicate that plaque composition may be ascertained (5). Potential differentiation of cross-sectional lesion pathology such as thrombus, vasculitis or atheroma has important therapeutic implications. The potential advantages of this added delineation of vessel morphology are numerous in the setting of interventional therapy including angioplasty, atherectomy, stents or laser surgery. This morphologic definition may assist in selecting the most appropriate intervention based on lesion characteristics and guide additional treatment in complicated interventions where contrast angiography yields equivocal information. Although digital subtraction images were acquired with use of a single plane projection, the correlation between angiography and ultrasonography for eccentric lesions appeared similar to the correlation for insignificantly narrowed normal arterial segments with regard to absolute vessel diameter and cross-sectional area. This was also true in segments of calcific plaque, although there were only I I segments in which this type of plaque was identified by ultrasonography. It has recently been suggested that single plane angiography of the “worst view” is adequate in the vast majority of cases for evaluation of minimal lesion diameter and for measurement of percent area stenosis (13). These data are further supported by the ultrasound data provided in the current study. Because of potential arterial injury, catheter advancement into severe:y tortuous segments of arterial anatomy was not attempted. Although diameter and area correlation should b? similar in tortuous segments, eccentric catheter position within a large vessel couldadverselyaffectfar-field image quality and morphologic assessment. conclusions. Accurate determination of vessel diameter and area are readily obtainable by intravascular ultrasonog- Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 raphy. However, ultrasound provides additional deformation because vessel anatomy and plaque morphology are not adequately visualized by silhouette contrast a~g~og~a~~y. This imaging technique appears to be a useful adjunct to contrast angiography in diagnostic and i~te~ve~tio~a~ therapy of both peripheral arterial disease and coronary artery disease. I. Marcus ML. Skorton DJ. .JO~ISOII MR. Collins SM. RE. Visual estimates of percent diameter coronary stenosis: “a battered gold standard.” J Am Coil Cardiol 1988;1 I:882-5. Isner JM. Kishel J. Kent KM. Ronrn JA Jr. Ross AM. Roberts WC. Accuracy of angiographic determination of left maio coronary arlerial narrowing: angiographic-hislologic correlative analysis in 28 patients. Circulalion 1981 :b3: 1056~64. .3. Heiber JH. Serruys PW. Kooijman CJ. et ai. Assessment of short-, medium-. and lonpterm variations in arterial dimensions from compulerassisled quanlitation of coronary cineangiqrams. Circulation IYXS.71: 280-8. 4. Wilson RF, Marcus ML. White CW. Prediction of the physiologic significance of coronary arterial lesions by quanlicative lesion geometry in patients with limited coronary artery disease. Circulation 1987:75:723-32. 5. Gussenhoven EJ. Essed CE. LancCe CT. et al. Arterial wall chardcteristics determined by intravascular ultrasound imaging: an in vitro sludy. J Am Coil Cardiol 198Y:l4:947-52. b. Rndian NG. Kreis A. Brockway B, et al. Ultrasound angioscopy: real-lime. two-dimensional. intraluminal ultrasound imaging of blood vessels. Am J Cardiol 1988:62:4Y3-4. 7. Tobis JM. Mallery JA. Gessert J. et al. Intravascular ultrasound crosssectional arterial imaging before and after balloon angioplasty in vitro. Circulation IY89:8U:873-82. 8. Yock PG. Linker DT. Angelsen AJ. Two-dimensional intravascular ultrasound: technical development and initial clinical experience. J Am Sot Echo 1989:2:2%-304. Y. Hodgson JMcB. Gnham SP. Savakus AD. et al. Clinical percutaneous imaging of coronary anatomy using au over-the-wire ultrasound catheter system. Int J Card Imaging 1989:4:181-93. IO. Nissen SE. Grines CL. Gurley JC. ei al. Application of a uew phasedarray ultrasound imaging catheter in the assessment of vascular dimensions: in vivo comparison lo cinedngiot_traphy. Circulation 1990:81:660-6. II. Mancini GB. Simon SB. McGillem MJ. LeFree MT. Friedman HZ. Vogel RA. Automdted quantitative coronary arteriography: morphologic and physiologic validation in vivo of a rapid digital angiographic method. Circulation 1987:75:452-60. 12. Skehon TN. Kisslo KB. Mikat EM. Bashore TM. Accuracy of digital angiography for quantitation of normal coronary luminal segments in excised. perfused hearts. Am J Cardiol 1987359: 1261-5. 13. Lesperance J. Hudon G. White CW. Laurier J. Waters D. Comparison by quanlitalive angioeraphic assessmen of coronary stenoses of one view showing the severesl narrowing to two orthogonal views. Am J Cdrdiol 1989:64:462-5.