Biomaterials 32 (2011) 8712e8721
Contents lists available at ScienceDirect
Biomaterials
journal homepage: www.elsevier.com/locate/biomaterials
Effects of chitosan-nanoparticle-mediated tight junction opening on the oral
absorption of endotoxins
Kiran Sonaje a,1, Kun-Ju Lin b, c,1, Michael T. Tseng d, Shiaw-Pyng Wey b, Fang-Yi Su a, Er-Yuan Chuang a,
Chia-Wei Hsu a, Chiung-Tong Chen e, **, Hsing-Wen Sung a, *
a
Department of Chemical Engineering, National Tsing Hua University, Hsinchu 30013, Taiwan, ROC
Department of Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan, ROC
Department of Nuclear Medicine and Molecular Imaging Center, Chang Gung Memorial Hospital, Taoyuan, Taiwan, ROC
d
Department of Anatomical Sciences and Neurobiology, University of Louisville, Louisville, KY, USA
e
Institute of Biotechnology and Pharmaceutical Research, National Health Research Institutes, Zhunan, Miaoli, Taiwan, ROC
b
c
a r t i c l e i n f o
a b s t r a c t
Article history:
Received 19 July 2011
Accepted 29 July 2011
Available online 8 September 2011
Recently, we reported a pH-responsive nanoparticle (NP) system shelled with chitosan (CS), which could
effectively increase the oral absorption of insulin and produce a hypoglycemic effect, presumably due to
the CS-mediated tight junction (TJ) opening. It has been often questioned whether CS can also enhance
the absorption of endotoxins present in the small intestine. To address this concern, we studied the effect
of CS NPs on the absorption of lipopolysaccharide (LPS), the most commonly found toxin in the
gastrointestinal tract. To follow their biodistribution by the single-photon emission computed tomography/computed tomography, LPS and insulin were labeled with 99mTc-pertechnetate (99mTc-LPS) and
123
iodine (123I-insulin), respectively. The 99mTc-LPS was ingested 1 h prior to the administration of the
123
I-insulin-loaded NPs to mimic the physiological conditions. The confocal and TEM micrographs show
that the orally administered CS NPs were able to adhere and infiltrate through the mucus layer, approach
the epithelial cells and mediate to open their TJs. The radioactivity associated with LPS was mainly
restricted to the gastrointestinal tract, whereas 123I-insulin started to appear in the urinary bladder at 3 h
post administration. This observation indicates that the insulin-loaded in CS NPs can traverse across the
intestinal epithelium and enter the systemic circulation, whereas LPS was unable to do so, probably
because of the charge repulsion between the anionic LPS in the form of micelles and the negatively
charged mucus layer. Our in vivo toxicity study further confirms that the enhancement of paracellular
permeation by CS NPs did not promote the absorption of LPS. These results suggest that CS NPs can be
used as a safe carrier for oral delivery of protein drugs.
Ó 2011 Elsevier Ltd. All rights reserved.
Keywords:
Chitosan
Tight junction
Endotoxin
Insulin
Paracellular transport
1. Introduction
Despite the advances in the development of drug delivery
technologies, successful oral administration of protein drugs has
remained to be an elusive goal. After oral administration, protein
drugs encounter several difficulties such as rapid pre-systemic
denaturation/degradation and poor absorption in the small intestine [1]. Therefore, a delivery system is needed to enhance the
bioavailability of such drugs. An ideal delivery system for oral
* Corresponding author. Tel.: þ886 3 574 2504; fax: þ886 3 572 6832.
** Corresponding author.
E-mail addresses: ctchen@nhri.org.tw (C.-T. Chen), hwsung@che.nthu.edu.tw
(H.-W. Sung).
1
The first two authors (K. Sonaje and K. J. Lin) contributed equally to this work.
0142-9612/$ e see front matter Ó 2011 Elsevier Ltd. All rights reserved.
doi:10.1016/j.biomaterials.2011.07.086
administration of protein drugs should reversibly increase the
permeability of the mucosal epithelium to improve the absorption
of protein drugs and provide the intact drugs to the systemic
circulation [2].
In a recent study, we reported a pH-responsive nanoparticle
(NP) system shelled with chitosan (CS) for oral delivery of insulin
via the paracellular pathway [3,4]. CS, a cationic polysaccharide, can
adhere to the epithelial surface to impart transient opening of the
tight junctions (TJs) between contiguous cells [5]. The results
obtained in a diabetic rat model indicated that CS NPs could
effectively increase the intestinal absorption of insulin and produce
a slower, but prolonged hypoglycemic effect [6]. However, it has
been often argued whether CS can also enhance the absorption of
unwanted toxins present in the small intestine [7].
The gastrointestinal (GI) tract is normally exposed to a number
of chemical and bacterial toxins. Some chemical toxins such as
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
thallium and lead can enter the systemic circulation with or
without the disruption of cell membrane integrity. Fortunately,
these chemical toxins are not normally present in the intestine,
unless ingested accidentally [8].
On the other hand, the enteric bacteria produce two kinds of
toxins, exotoxins and endotoxins [9]. Exotoxins are the proteins
secreted by living bacteria [10]. Since the majority of the orally
ingested bacteria are killed by the acidic environment in the
stomach, the intestine is seldom exposed to exotoxins. Additionally,
the proteolytic enzymes present in the GI tract can further
neutralize such exotoxins [9]. In contrast, endotoxins are the
negatively charged components (lipopolysaccharide, LPS) from the
cell wall of gram-negative bacteria; they are released in the GI tract
by the disintegrating or dead bacteria [11]. Thus, LPS is the major
bacterial toxin present in the GI tract at all times [12]. If delivered to
the systemic circulation, LPS triggers a systemic inflammatory
response that can progress to endotoxic shock and sometimes
death [13]. Therefore, it is essential to study the effect of CS NPs on
the absorption of LPS.
To follow their biodistribution, we used 99mTc-pertechnetate
99m
Tc) to label LPS (99mTc-LPS) and 123iodine (123I) to label insulin
(
123
( I-insulin). Employing a rat model, the 99mTc-LPS was orally
administered 1 h before the ingestion of the 123I-insulin-loaded NPs
to mimic the natural conditions, in which LPS is present in the small
intestine. The biodistribution of the orally administered LPS was
studied using the single-photon emission computed tomography
(SPECT)/computed tomography (CT) and confocal laser scanning
microscopy (CLSM). The activity of epithelial TJ opening by CS NPs
was investigated by transmission electron microscopy (TEM).
Additionally, the in vivo toxicity of the orally administered LPS was
examined in mice.
2. Materials and methods
2.1. Preparation and characterization of CS NPs
CS (MW 80 kDa) with a degree of deacetylation of approximately 85% was
acquired from Koyo Chemical Co. Ltd. (Japan), while poly(g-glutamic acid) (g-PGA)
(MW 60 kDa) was purchased from Vedan Co. Ltd. (Taichung, Taiwan). The insulinloaded NPs were prepared by an ionic-gelation method, using the positivelycharged CS and the negatively charged g-PGA in the presence of bovine insulin
[4,6,14,15]. The prepared NPs were washed three times with deionized (DI) water
and collected by centrifugation at 8000 rpm for 50 min. The collected NPs were
redispersed in DI water and stored at 4 C until used. The mean particle size and zeta
potential value of the prepared NPs were measured using a Zetasizer (Nano ZS,
Malvern Instruments Ltd., Worcestershire, UK); their insulin loading efficiency and
content were calculated as reported previously [4,6].
2.2. Evaluation of the micelle-forming characteristics of LPS
LPS is an amphiphilic molecule, composed of a hydrophilic oligosaccharide chain
with varying length and a hydrophobic portion known as lipid A [11,16], which may
form micelles in an aqueous environment. To confirm this possibility, different
concentrations of LPS (Escherichia coli, serotype 0111:B4, Sigma-Aldrich, St. Louis,
MO, USA) were suspended in phosphate buffered saline (PBS, pH 7.4). The formation
of micelles was validated by measuring the particle size and zeta potential of the
resulting suspensions using the Zetasizer.
2.3. Animal studies
Animal studies were performed in compliance with the “Guide for the Care and
Use of Laboratory Animals” prepared by the Institute of Laboratory Animal
Resources, National Research Council, and published by the National Academy Press,
revised in 1996.
2.3.1. Biodistribution study
The biodistribution of LPS and the insulin-loaded in CS NPs was studied in rats
(male Wistar, 200250 g) using the SPECT/CT. In the study, LPS was radiolabeled
with 99mTc (emitting 140 keV photons) using a stannous chloride (SnCl2) method
[17]; the labeling efficiency of 99mTc to LPS was determined by the instant thin layer
chromatography (ITLC) [18]. The insulin was radiolabeled with 123I (emitting
159 keV photons) using an iodogen-tube (Pierce Iodination Tubes, Thermo Fisher
8713
Scientific, Rockford, IL, USA) method, as per the manufacturer’s instructions. The
123
I-insulin was separated from the free-form 123I using a centrifugal dialysis device
(MWCO: 3 kDa, Amicon Ultra 4, Millipore, Billerica, MA, USA); its labeling efficiency
was determined by a reversed-phase HPLC system equipped with a gamma counter
[19]. The obtained 123I-insulin was then used to prepare test NPs as described above.
In the biodistribution study, rats were fed with 99mTc-LPS alone or together with
the 123I-insulin-loaded CS NPs (n ¼ 3 in each studied group). For the group receiving
both LPS and test NPs, the 99mTc-LPS was administered 1 h before the ingestion of
the 123I-insulin-loaded NPs. The detailed protocol used in the image acquisition was
previously described by our group [18,20]. Animal images were acquired using
a dual modality system (NanoSPECT/CT, Bioscan Inc., Washington DC, USA), which is
capable of detecting two kinds of isotopes simultaneously at a relatively high spatial
resolution (approximately 0.6 mm).
Animals were kept under the controlled temperature (37 C) and anesthesia
(1.5% isoflurane in 100% oxygen) during imaging. Dual isotope dynamic SPECT
images were acquired at 30-min intervals up to 24 h after the administration of test
samples. Additional CT images were collected for anatomical references and used to
investigate the details of radiotracer distribution in rats. The co-registered dynamic
scintigraphy and CT images were displayed and analyzed using the PMOD v2.9
image analysis software (PMOD Technologies Ltd., Zurich, Switzerland).
The quantitative analysis of SPECT images was performed to evaluate the
distribution of 99mTc-LPS and 123I-insulin within the peripheral tissue/plasma (PP)
compartment. The PP compartment was defined as the whole body (WB) excluding
the gastrointestinal (GI) tract and urinary bladder. To calculate the percentage of
initial dose (% ID) within each region, the corresponding contours were manually
drawn on the co-registered dynamic SPECT and reference CT images. The biodistribution data were expressed as % ID using the following formula:
% ID ¼
decay corrected total radioactivity in the target region
100%
ingested counts
(1)
2.3.2. Ultra-structural examination of TJ opening by CS NPs
The opening of epithelial TJs by CS NPs was examined using TEM. In the study, CS
was labeled with quantum dot (QD, CdSe) according to a method reported in the
literature [21]. Briefly, carboxyl QD (40 mL, 0.6 nM, QdotÒ ITKÔ, Invitrogen, USA) was
activated in the presence of 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC,
60 mL, 50 mM) and N-hydroxysuccinimide (NHS, 30 mL, 25 mM) for 15 min under
gentle stirring. The resulting NHS-activated QD was covalently linked to the primary
amines on CS (QD-CS) at pH 6.0. The reaction was carried out under gentle mixing
for 4 h. The final QD-CS conjugate was purified by the centrifugal spin filtration and
then resuspended in DI water.
QD-CS NPs were then prepared using the method described above. The QD-CS
NPs (1 mg/mL, 1 mL) were orally administered to the overnight-fasted ICR mice
(33e40 g, n ¼ 3). Animals were sacrificed 3 h later and the intestinal segments were
dissected and washed three times with isotonic saline. The dissected intestinal
segments were then fixed in 4% paraformaldehyde (PFA), cut into smaller pieces and
silver-intensified using a commercial silver enhancer kit (Sigma-Aldrich) [22]. After
silver-enhancing QD-CS, tissue samples were post-fixed in 1% osmium tetroxide and
dehydrated in a graded series of ethanol. Subsequently, the dehydrated samples
were infiltrated with and embedded in Spurr resin with overnight polymerization at
70 C to prepare the tissue-embedded TEM blocks. Sections (1 mm in thickness) were
made and stained with toluidine blue and then observed under a light microscope.
To demonstrate the enhancement of paracellular transport by CS NPs, tissues
samples were stained with lanthanum nitrate [23]. For this, the PFA-fixed tissue
samples were washed with s-Collidine buffer and treated with 2% lanthanum nitrate
for 2 h at room temperature [23,24]. After washing with s-Collidine and PBS, the
tissue samples were processed for TEM as detailed above. Ultrathin sections were
then cut with a diamond knife and loaded onto TEM grids. The sections were
examined by a Philips CM10 electron microscope (Philips Electron Optics B.V.) at
accelerating voltage of 60 kV.
2.3.3. Intestinal absorption of FITC-LPS and Cy3-insulin-loaded NPs
The FITC (fluorescein isothiocyanate) labeled LPS (FITC-LPS) and Cy3 (Cyanine-3)
labeled insulin (Cy3-insulin) were used to visualize their intestinal absorption
characteristics using CLSM (TCS SL, Leica, Germany). The FITC-LPS was obtained
from Sigma-Aldrich, whereas the Cy3-insulin was synthesized as per a method
described in the literature [4,14]. Briefly, Cy3 NHS ester (GE Healthcare, Pittsburgh,
PA, USA) dissolved in DMSO (dimethyl sulfoxide, 1 mg/mL, 1 mL) was slowly added
into an aqueous solution of insulin (1% w/v in 0.01 N HCl, 4 mL) and stirred overnight
at 4 C. To remove the unconjugated Cy3, the synthesized Cy3-insulin was dialyzed
in the dark against 5 L of 0.01 N HCl and replaced on a daily basis until no fluorescence was detected in the dialysis medium. The resultant Cy3-insulin was
lyophilized in a freeze dryer. Fluorescent NPs were then prepared for the subsequent
in vivo CLSM study according to the procedure described above.
FITC-LPS (2 mg/mL, 0.5 mL) alone or in combination with a mucolytic agent (Nacetylcysteine) were administered to the overnight-fasted rats (male Wistar, n ¼ 3 in
each studied group). To study the effects of CS NPs on the absorption of LPS, the Cy3insulin-loaded NPs (2 mg/mL, 0.5 mL) were orally administered 1 h after the
8714
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
ingestion of the FITC-LPS (2 mg/mL, 0.5 mL). Rats were sacrificed 3 h later and
intestinal segments were then dissected and washed three times with isotonic
saline. The isolated intestinal segments were fixed using the methanol-Carnoy’s
fixative and processed for paraffin-embedding. The embedded sections were dewaxed, hydrated and stained with Alexa-633-labeled wheat-germ-agglutinin and
SYTOX blue (Invitrogen, Carlsbad, CA, USA) to visualize the mucus and nuclei,
respectively. Finally, the stained sections were examined under CLSM.
2.3.4. In vivo toxicity study
LPS is a well-known inflammatory agent; therefore, a study was performed to
evaluate whether CS NPs can promote the toxicity of the orally administered LPS.
Animals (male ICR mice) were randomly divided into four groups (n ¼ 6 for each
studied group). The experimental groups received once-daily oral doses of LPS
(5 mg/kg) with or without CS NPs (10 mg/kg) for 7 consecutive days; the group
without any treatment was used as a control. Additionally, a group receiving intraperitoneal (IP) LPS (5 mg/kg) served as a reference for the extent of toxicity produced
by the systemic LPS. All animals were fed with normal chows and water ad libitum.
Animals were observed carefully for the onset of any signs of toxicity and monitored
for changes in body weight. At the end of the treatment period, animals were
anaesthetized (tribromoethanol, IP, 240 mg/kg) and blood samples were collected
via cardiac puncture for the determination of alanine aminotransferase (ALT) and
aspartate aminotransferase (AST) using a FUJI DRI-CHEM 3500s serum-chemistry
analyzer. After sacrificed, internal organs of each animal were harvested and
observed grossly. For histological examinations, specimens of liver were fixed in 10%
phosphate buffered formalin, embedded in paraffin, sectioned and stained with
hematoxylin and eosin (H&E).
2.4. Statistical analysis
Comparison between groups was analyzed by the one-tailed Student’s t-test
(SPSS, Chicago, Ill). All data are presented as a mean value with its standard deviation indicated (mean SD). Differences were considered to be statistically significant when the p values were less than 0.05.
3. Results and discussion
The efficacy of oral delivery of protein drugs is often limited
because of their inherent instability in the GI tract. Additionally, the
high molecular weight of this class of drugs coupled with their
hydrophilic nature significantly restricts their transcellular
permeation [1]. Thus, enhancement of the paracellular permeation
is an alternative for oral absorption of protein drugs [25]. CS is
a well-known mucoadhesive agent with the capability of transiently and reversibly opening epithelial TJs [26]. Formulating CS
into NPs has the advantages over the traditional tablet or powder
formulations, as NPs can readily infiltrate into the mucus layer and
deliver the protein drugs to the actual site of absorption (i.e., the TJs
between epithelial cells). CS is generally regarded as a safe material
for drug delivery. However, its effects on the absorption of
unwanted toxins remain to be understood.
3.1. Characteristics of CS NPs
The prepared CS NPs had a mean particle size of 253.2 4.8 nm
with a zeta potential of 28.2 1.3 mV; their insulin loading efficiency and content were 72.4 3.9% and 17.9 2.1%, respectively
(n ¼ 6 batches). The as-prepared NPs are pH-responsive: they were
stable in the pH range of 2.0e7.0; beyond this range, the particles
became unstable and disintegrated. Similar characteristics were
found for the NPs prepared with QD-CS or FITC-CS.
3.2. Micelle-forming characteristics of LPS
Due to its amphiphilic nature, LPS may form micelles in an
aqueous environment when above its critical micelle concentration
(CMC) [12]. The reported CMC values for LPS vary from 10 nM to
1.6 mM, depending on the source of LPS [16]. It has been suggested
that the aggregated form (i.e., micelles) of LPS predominates in the
range of concentration usually found in the intestinal lumen
[8,12,27]. To evaluate the micelle-forming characteristics of LPS, we
measured the size and zeta potential of the aqueous suspensions of
LPS at different concentrations. As shown in Table 1, with an
increase in concentration, the size of LPS micelles increased
significantly (P < 0.05). The LPS micelles were negatively charged at
all concentrations, which could be due to the two phosphate groups
present on the LPS structure. In the concentration used in the
subsequent animal study (2 mg/mL), LPS formed micelles with an
average size of 220.5 7.6 nm and a zeta potential of 8.5 1.7 mV.
3.3. Biodistribution and absorption of the orally administered LPS
The biodistribution and intestinal absorption of the orally
administered LPS was investigated by the SPECT/CT. In the study,
99m
Tc was used to label LPS and its labeling efficiency was determined by the ITLC. It was found that more than 99% of 99mTc was
successfully conjugated onto LPS (Fig. 1a). The SPECT/CT images of
the orally administered 99mTc-LPS are shown in Fig. 1b. As shown,
after oral administration of LPS alone, the radioactivity (99mTc-LPS)
propagated from the stomach, small intestine and then to the large
intestine with time. Overall, the 99mTc-labeled LPS appeared to be
restricted within the GI tract, with no detectable radioactivity
present in the PP compartment. These results were in agreement
with the findings reported in the literature that the orally administered LPS was not able to be absorbed into the systemic circulation in rabbits [27,28]. Mucus is a viscoelastic gel layer that protects
tissues that would otherwise be exposed to the external environment [29]. The mucus layer has been shown to act as a physical
barrier to the enteric bacteria and hinders their access to the
underlying epithelium [30]. However, the protective function of the
mucus layer against LPS is still unknown.
To understand how the intestinal epithelium prevents the
absorption of LPS, we investigated the absorption of FITC-LPS in rats
using CLSM. In the study, the FITC-LPS was orally administered in
the absence/presence of a mucolytic agent (N-acetylcystein). In the
absence of the mucolytic agent, the epithelial mucus layer was
intact; the administered FITC-LPS was found to be restricted
outside the mucus layer (Fig. 2, upper panels). This is probably due
to the charge repulsion between the negatively charged mucus [31]
and the anionic LPS in the form of micelles. Additionally, the
intestinal mucus is rich in LPS-binding proteins [32], which might
contribute to the inability of LPS to penetrate through the mucus
layer. In contrast, in the presence of the mucolytic agent, the
thickness of the mucus layer decreased significantly, and the
administered FITC-LPS was able to infiltrate through the mucus and
access the epithelium surface. This led to the absorption of LPS into
the systemic circulation, as indicated by its presence on the basolateral side of intestinal villi (Fig. 2, lower panels).
The epithelium lining on the GI tract provides a regulated,
selectively permeable barrier between the external environment
(the intestinal lumen) and the systemic circulation. It transports
nutrients, ions and fluid transcellularly, but prevents the entry of
toxins, antigens and microorganisms [9]. The paracellular route is
restricted by the presence of TJs at the apical poles of enterocytes
that limit the passage of macromolecules [33]; its permeability
generally depends on the regulation of intercellular TJs by using an
intestinal permeation enhancer such as CS [5].
Table 1
Particle size, distribution and zeta potential of the micelles formed in aqueous LPS
suspensions at different concentrations (n ¼ 5).
LPS Concentration
(mg/mL)
0.2
2.0
10.0
Particle Size
(nm)
Polydispersity
Zeta Potential
(mV)
135.3 3.2
220.5 7.6
545.8 14.1
0.2 0.0
0.5 0.1
0.7 0.1
9.8 2.5
8.5 1.7
4.8 1.2
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
8715
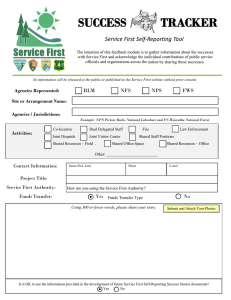
Fig. 1. (a) Scan of the radioactivity of 99mTc-LPS, developed on an instant thin layer chromatography (ITLC) plate; (b) biodistribution of 99mTc-LPS observed in a rat model after oral
ingestion.
3.4. Ultra-structural examination of TJ opening by CS NPs
The ability of CS in enhancing the permeability of model drug
compounds across Caco-2 cell monolayers has been investigated in
numerous studies [5,26]; however, it’s in vivo activity has never
been investigated. Fig. 3a shows photomicrographs of a silverenhanced intestinal segment of an ICR mouse after being treated
with QD-CS NPs. The silver-enhancement procedure enlarges QD
Fig. 2. Confocal images showing the intestinal absorption of FITC-LPS (green) after its oral administration in the absence/presence of a mucolytic agent (N-acetylcystein). In the
presence of the mucolytic agent, the mucus layer (red) became thinner, and FITC-LPS was observed underneath the epithelium (indicated in the superimposed image by the white
arrows), an indication of the intestinal absorption of LPS. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
8716
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
by selective deposition of metallic silver, making them easily
identifiable by light microscopy [34]. As shown, the orally administered NPs were able to adhere and infiltrate into the mucus layer
and approach the surface of epithelial cells. However, we were not
able to tell whether the epithelial TJs were opened, due to the lack
of electron density in their intercellular spaces.
For this reason, the same tissue samples after being treated with
QD-CS NPs were incubated with an aqueous lanthanum.
Lanthanum is an electron-dense element with a hydrated radius of
0.4 nm and has been widely used to stain the cell surfaces for TEM
examination [24]. It has been reported that the width of TJs, when
fully opened, is less than 20 nm [25]. For the control sample (that
without being treated with QD-CS NPs), the TJs were intact and the
lanthanum staining was restricted on the mucosal surface (Fig. 3b).
In contrast, lanthanum was able to penetrate into the paracellular
spaces for the experimental sample, suggesting that the TJs were
indeed opened by QD-CS NPs. These results support our hypothesis
that CS NPs could infiltrate through the epithelial mucus layer and
thus may deliver the loaded drugs near the opened TJs to promote
their intestinal absorption. However, it is also essential to consider
the effects of CS-mediated TJ opening on the transport of endotoxins (i.e., LPS) present in the small intestine.
3.5. Effects of the insulin-loaded CS NPs on the biodistribution and
absorption of LPS
In the study, insulin was radiolabeled by 123I with an efficiency
of about 80%, determined by the reversed-phase HPLC; the freeform 123I was removed using a centrifugal dialysis device.
Following oral administration in rats, effects of CS NPs on the biodistribution and absorption of 99mTc-LPS and 123I-insulin (the
loaded drug) were studied using the dual isotope dynamic SPECT/
CT. To mimic the physiological conditions, the 99mTc-LPS was
ingested 1 h prior to the administration of the 123I-insulin-loaded
NPs. As shown in Fig. 4a, the radioactivity associated with LPS was
mainly limited to the GI tract throughout the entire course of the
study, whereas 123I-insulin started to appear in the urinary bladder
at 3 h post administration. These results suggest that the insulinloaded in CS NPs can traverse across the intestinal epithelium
Fig. 3. (a) Photomicrograph of a silver-enhanced intestinal section showing the mucoadhesion and infiltration of QD-CS NPs (black dots) after oral administration, area defined by
a rectangle is shown at a higher magnification in the inset; (b) TEM micrographs of the control intestinal segment incubated with a lanthanum solution; and (c) permeation of
lanthanum through the opened paracellular space (indicated by the blue arrows) in mice treated with QD-CS NPs. (For interpretation of the references to colour in this figure legend,
the reader is referred to the web version of this article.)
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
8717
Fig. 4. (a) Biodistribution of 99mTc-LPS and 123I-insulin in rats orally treated with 99mTc-LPS followed by 123I-insulin-loaded NPs; (b) reconstructed 3D images showing the whole
body (WB) and gastrointestinal tract/urinary bladder (GIT/UB) regions together with their sagittal and coronal views: the plasma/peripheral tissue (PP) compartment is defined as
the WB region (blue contour) excluding the GIT/UB (yellow contour); and (c) % initial dose (% ID) of 99mTc-LPS and 123I-insulin observed in the PP compartment. (For interpretation
of the references to colour in this figure legend, the reader is referred to the web version of this article.)
8718
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
Fig. 5. Schematic drawing of intestinal villi and confocal images showing the intestinal villi retrieved from rats fed with FITC-LPS (green) followed by the administration of Cy3insulin-loaded NPs. The white arrows indicate the absorbed insulin (purple) underneath the epithelium, while FITC-LPS (pointed by the blue arrows) was mainly restricted outside
the mucus layer (red). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 6. Changes in (a) body weight and (b) serum levels of aspartate transaminase and alanine transaminase in mice treated with LPS alone via the intra-peritoneal route (IP LPS) or
the oral route (oral LPS) or in combination with CS NPs (oral LPS þ CS NPs). The group without receiving any treatment was used as a control. *statistical significance at a level of
P < 0.05.
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
8719
Fig. 7. Photomicrographs of the liver sections obtained in the toxicity study: (a) the control group; (b) the group treated with LPS intraperitoneally (IP LPS); (c) the group orally
treated with LPS alone (oral LPS); and (d) the group orally treated with LPS followed by CS NPs (oral LPS þ CS NPs). The black arrows indicate foci of necrotic cells.
and enter the systemic circulation; in contrast, LPS was unable to do
so, hence retaining primarily within the intestinal lumen.
To quantify the amount of 99mTc-LPS and 123I-insulin within the
PP compartment, contours of the WB and the GI tract/urinary
bladder were manually drawn on an averaged SPECT/CT image. The
dynamic 99mTc-LPS SPECT/CT images superimposed with the region
contours in the sagittal and coronal views are presented in Fig. 4b.
The radioactivity counts of 99mTc-LPS and 123I-insulin within the PP
compartment were calculated and normalized to their initially
ingested doses (% ID). As shown in Fig. 4c, the radioactivity of
Fig. 8. Schematic illustrations showing the selective barrier function of the mucus layer, preventing the oral absorption of anionic LPS in the form of micelles, while allowing the
positively-charged CS NPs to infiltrate through.
8720
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
123
I-insulin in the PP compartment increased with time and
reached to its maximum value (w8% ID) by 6 h post administration,
while no measurable 99mTc-LPS was observed throughout the
study. These results suggest that the absorption enhancement by CS
NPs was specific for the loaded insulin only. To determine a specific
reason for this observation, we used the FITC-LPS and Cy3-insulinloaded NPs to repeat the study, examining by CLSM.
Fig. 5 shows the CLSM images acquired from a rat ingested with
the FITC-LPS followed by the administration of the Cy3-insulinloaded NPs. As shown, the Cy3-insulin was able to infiltrate through
the mucus layer and was observed underneath the epithelium. In
contrast, the FITC-LPS was still restricted outside the mucus layer.
3.6. In vivo toxicity study
LPS is a potent inflammatory agent, which plays an important
role in the pathogenesis of endotoxic shock [35]. One of the most
frequently reported symptoms of endotoxic shock is the hepatocyte
necrosis [13,36]. To study whether CS NPs can induce in vivo
toxicity in the presence of LPS, the changes in body weight and two
of the liver function indicators (ALT and AST) were evaluated. As
expected, the daily injections of LPS via the IP route led to decrease
in body weight and a significant increase in the level of AST
(P < 0.01, Fig. 6a and b). In contrast, the group receiving oral LPS
followed by CS NPs did not show any significant changes in body
weight and levels of liver function indicators, as compared to the
control (p > 0.05). The histological examination of liver sections
was performed. In the group treated with LPS via the IP route, the
liver section showed broad hemorrhagic necrosis, hepatocyte
swelling and degeneration (Fig. 7b). In contrast, the liver sections
retrieved from the groups receiving LPS via the oral route (Fig. 7c
and d) were similar to the control (Fig. 7a). These results further
confirm that the paracellular permeation enhancement by CS NPs
did not promote the intestinal absorption of LPS.
The aforementioned findings suggest that CS NPs can adhere
and infiltrate into the mucus; the infiltrated NPs become unstable
and disintegrate near the epithelial cell surface due to their pHsensitivity (Section 3.1) and thus release the loaded insulin. The
released insulin could then enter the systemic circulation due to the
CS-mediated TJ opening (Section 3.4). In contrast, the anionic LPS in
the form of micelles are repelled by the negatively charged mucus
layer lining on the intestinal epithelium, consequently preventing
LPS from entering the systemic circulation (Fig. 8).
In our previous report, an in vivo toxicity study was performed
to determine whether oral administration of CS NPs was safe [4].
The animals were treated with a daily dose of CS NPs for 14 days. No
significant differences in clinical signs and body weight between
the experimental group and the untreated control group were
found. The measured hematological and biochemical parameters
for both studied groups were within the normal ranges. Moreover,
no pathological changes were observed in the histological sections
of the liver and kidney. These results indirectly pointed out that CS
NPs did not promote the absorption of any toxins from the GI tract.
4. Conclusions
The results obtained in the study indicate that CS NPs could
adhere and infiltrate through the mucus layer, mediate to open the
epithelial TJs, and enhance the paracellular delivery of the loaded
insulin. However, the enhancement of paracellular permeation by
CS NPs did not promote the intestinal absorption of LPS; this
observation was further confirmed in our in vivo toxicity study. On
the basis of these results, it can be concluded that the CS NPs can be
used as a safe carrier for oral delivery of protein drugs.
Acknowledgement
This work was supported by a grant from the National Science
Council (NSC 99-2120-M-007-006), Taiwan, Republic of China.
References
[1] Khafagy el S, Morishita M, Onuki Y, Takayama K. Current challenges in noninvasive insulin delivery systems: a comparative review. Adv Drug Deliv
Rev 2007;59:1521e46.
[2] Carino GP, Mathiowitz E. Oral insulin delivery. Adv Drug Deliv Rev 1999;35:
249e57.
[3] Sonaje K, Lin KJ, Wang JJ, Mi FL, Chen CT, Juang JH, et al. Self-assembled phsensitive nanoparticles: a platform for oral delivery of protein drugs. Adv
Funct Mater 2010;20:3695e700.
[4] Sonaje K, Lin YH, Juang JH, Wey SP, Chen CT, Sung HW. In vivo evaluation of
safety and efficacy of self-assembled nanoparticles for oral insulin delivery.
Biomaterials 2009;30:2329e39.
[5] Smith J, Wood E, Dornish M. Effect of chitosan on epithelial cell tight junctions. Pharm Res 2004;21:43e9.
[6] Sonaje K, Chen YJ, Chen HL, Wey SP, Juang JH, Nguyen HN, et al. Enteric-coated
capsules filled with freeze-dried chitosan/poly(g-glutamic acid) nanoparticles
for oral insulin delivery. Biomaterials 2010;31:3384e94.
[7] Junginger HE, Verhoef JC. Macromolecules as safe penetration enhancers for
hydrophilic drugs a fiction? Pharm Sci Technolo Today 2000;3:346e58.
[8] Lu FC, Kacew S. Basic toxicology: fundamentals, target organs, and risk
assessment. Chapter 2: Absorption, distribution, and excretion of toxicants. 5th
ed. PA, USA: Taylor & Francis; 2009. p. 1528.
[9] Walker RL, Owen RL. Intestinal barriers to bacteria and their toxins. Annu Rev
Med 1990;41:393e400.
[10] Macpherson AJ, Geuking MB, McCoy KD. Immune responses that adapt the
intestinal mucosa to commensal intestinal bacteria. Immunology 2005;115:
153e62.
[11] Gutsmann T, Schromm AB, Brandenburg K. The physicochemistry of endotoxins in relation to bioactivity. Int J Med Microbiol 2007;297:341e52.
[12] Piazza M, Colombo M, Zanoni I, Granucci F, Tortora P, Weiss J, et al. Uniform
lipopolysaccharide (LPS)-loaded magnetic nanoparticles for the investigation
of LPS-TLR4 signaling. Angew Chem Int Ed Engl 2011;50:622e6.
[13] Li G, Liu Y, Tzeng NS, Cui G, Block ML, Wilson B, et al. Protective effect of
dextromethorphan against endotoxic shock in mice. Biochem Pharmacol
2005;69:233e40.
[14] Lin YH, Sonaje K, Lin KM, Juang JH, Mi FL, Yang HW, et al. Multi-ion-crosslinked nanoparticles with pH-responsive characteristics for oral delivery of
protein drugs. J Control Release 2008;132:141e9.
[15] Sonaje K, Lin KJ, Wey SP, Lin CK, Yeh TH, Nguyen HN, et al. Biodistribution,
pharmacodynamics and pharmacokinetics of insulin analogues in a rat model:
oral delivery using pH-Responsive nanoparticles vs. subcutaneous injection.
Biomaterials 2010;31:6849e58.
[16] Yu L, Tan M, Ho B, Ding JL, Wohland T. Determination of critical micelle
concentrations and aggregation numbers by fluorescence correlation spectroscopy: aggregation of a lipopolysaccharide. Anal Chim Acta 2006;556:
216e25.
[17] Rosenbaum JT, Hendricks PA, Shively JE, McDougall IR. Distribution of radiolabeled endotoxin with particular reference to the eye: concise communication. J Nucl Med 1983;24:29e33.
[18] Chen MC, Wong HS, Lin KJ, Chen HL, Wey SP, Sonaje K, et al. The characteristics, biodistribution and bioavailability of a chitosan-based nanoparticulate
system for the oral delivery of heparin. Biomaterials 2009;30:6629e37.
[19] Sodoyez JC, Sodoyez-Goffaux F, Guillaume M, Merchie G. [123I]Insulin
metabolism in normal rats and humans: external detection by a scintillation
camera. Science 1983;219:865e7.
[20] Lin KJ, Liao CH, Hsiao IT, Yen TC, Chen TC, Jan YY, et al. Improved hepatocyte
function of future liver remnant of cirrhotic rats after portal vein ligation:
a bonus other than volume shifting. Surgery 2009;145:202e11.
[21] Bagalkot V, Zhang L, Levy-Nissenbaum E, Jon S, Kantoff PW, Langer R, et al.
Quantum dot-aptamer conjugates for synchronous cancer imaging, therapy,
and sensing of drug delivery based on bi-fluorescence resonance energy
transfer. Nano Lett 2007;7:3065e70.
[22] Liang RQ, Li W, Li Y, Tan CY, Li JX, Jin YX, et al. An oligonucleotide microarray
for microRNA expression analysis based on labeling RNA with quantum dot
and nanogold probe. Nucleic Acids Res 2005;33. e17.
[23] Friend DS, Gilula NB. Variations in tight and gap junctions in mammalian
tissues. J Cell Biol 1972;53:758e76.
[24] Flynn AN, Itani OA, Moninger TO, Welsh MJ. Acute regulation of tight junction
ion selectivity in human airway epithelia. Proc Natl Acad Sci USA 2009;106:
3591e6.
[25] Salama NN, Eddington ND, Fasano A. Tight junction modulation and its relationship to drug delivery. Adv Drug Deliv Rev 2006;58:15e28.
[26] Smith JM, Dornish M, Wood EJ. Involvement of protein kinase C in chitosan
glutamate-mediated tight junction disruption. Biomaterials 2005;26:3269e76.
[27] Beatty WL, Meresse S, Gounon P, Davoust J, Mounier J, Sansonetti PJ, et al.
Trafficking of Shigella lipopolysaccharide in polarized intestinal epithelial
cells. J Cell Biol 1999;145:689e98.
K. Sonaje et al. / Biomaterials 32 (2011) 8712e8721
[28] Ravin HA, Rowley D, Jenkins C, Fine J. On the absorption of bacterial endotoxin
from the gastro-intestinal tract of the normal and shocked animal. J Exp Med
1960;112:783e92.
[29] Cone RA. Barrier properties of mucus. Adv Drug Deliv Rev 2009;61:
75e85.
[30] Johansson MEV, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The
inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of
bacteria. Proc Natl Acad Sci USA 2008;105:15064e9.
[31] Atuma C, Strugala V, Allen A, Holm L. The adherent gastrointestinal mucus gel
layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver
Physiol 2001;280:G922e9.
[32] Vreugdenhil AC, Snoek AM, Greve JW, Buurman WA. Lipopolysaccharidebinding protein is vectorially secreted and transported by cultured intestinal
[33]
[34]
[35]
[36]
8721
epithelial cells and is present in the intestinal mucus of mice. J Immunol 2000;
165:4561e6.
Ward PD, Tippin TK, Thakker DR. Enhancing paracellular permeability by
modulating epithelial tight junctions. Pharm Sci Technolo Today 2000;3:346e58.
Mortensen LJ, Oberdorster G, Pentland AP, Delouise LA. In vivo skin penetration of quantum dot nanoparticles in the murine model: the effect of UVR.
Nano Lett 2008;8:2779e87.
Illyes G, Kovacs K, Kocsis B, Baintner K. Failure of oral E. coli O83 lipopolysaccharide to influence intestinal morphology and cell proliferation in rats:
short communication. Acta Vet Hung 2008;56:1e3.
Bertok L. Effect of bile acids on endotoxin in vitro and in vivo (physicochemical defense). Bile deficiency and endotoxin translocation. Ann N Y Acad
Sci 1998;851:408e10.