Immediate on‐site interpretation of fine‐needle aspiration smears
advertisement

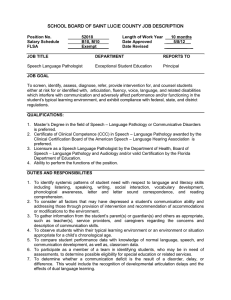
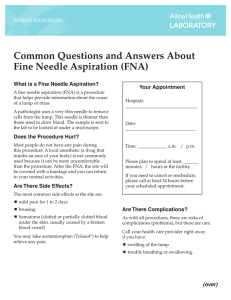
CANCER 319 CYTOPATHOLOGY Immediate On-Site Interpretation of Fine-Needle Aspiration Smears A Cost and Compensation Analysis Lester J. Layfield, M.D. Joel S. Bentz, M.D. Evelyn V. Gopez, M.D. Department of Pathology, University of Utah School of Medicine, Salt Lake City, Utah. Address for reprints: Joel S. Bentz, M.D., Department of Pathology, University of Utah School of Medicine, 50 North Medical Drive, Salt Lake City, UT; Fax: (801) 585-3831. Received December 13, 2000; revision received March 16, 2001; accepted March 22, 2001. © 2001 American Cancer Society BACKGROUND. A significant body of literature exists supporting the cost effectiveness of fine-needle aspiration (FNA) cytology in the work-up of patients with potential neoplastic disease. Several authorities have stated that immediate, onsite smear evaluation by cytopathologists optimizes diagnostic accuracy and minimizes the technique’s insufficiency rate. This favorable effect on FNA diagnostic accuracy is most pronounced for deep body sites, where FNA is guided by computed tomography (CT), ultrasound, bronchoscopy, or endoscopy. Little data exist regarding whether compensation from Medicare is adequate to support the pathologist in this endeavor compared with other potentially more remunerative activities, including routine surgical pathology sign-out, nongynecologic cytopathology sign-out, and frozen section consultation. METHODS. The authors studied a series of 142 fine-needle aspirates with immediate, on-site evaluations performed under a variety of clinical settings. These included bronchoscopic, endoscopic, ultrasound-guided, and CT-guided biopsies along with palpation-directed biopsies performed by either cytopathologists or clinicians. For these aspirates, total pathologist attendance time was calculated and correlated with guidance technique, target organ, location where aspirate was performed, and nature of aspirator. Fifty frozen section evaluations were timed similarly. For comparison purposes, cytopathologists’ costs were calculated using the 80th percentile pay level of an associate professor with full-time clinical duties. Medicare rate schedules were used to calculate compensation. Including salary and benefits, the pathologist cost was approximately $88.83 per hour. RESULTS. On average, an intraprocedural FNA evaluation for a CT-guided biopsy required 48.7 minutes, an ultrasound-guided biopsy required 44.4 minutes of pathologist time, an endoscopic procedure required 56.2 minutes, a bronchoscopic procedure required 55.3 minutes, a clinic aspirate performed by a pathologist required 42.5 minutes, and a clinic FNA performed by a clinician required 34.7 minutes. The average frozen section required 15.7 minutes of pathologist time for performance and interpretation. With the exception of FNA performed in clinic by the cytopathologist, time costs exceeded compensation by $40 –50 per procedure. Clinic aspirates performed by a clinician and immediately evaluated by a pathologist resulted in a deficit of approximately $18 over actual time cost. CONCLUSIONS. From the current data, it appears that intraprocedural consultations by cytopathologists for CT-guided, ultrasound-guided, bronchoscopic, or endoscopic procedures are compensated insufficiently by current Medicare compensation schedules using the CPT code 88172 for on-site evaluation. Only when the cytopathologist personally performs the aspirate and immediately interprets it (CPT codes 88172 and 88170) does the Medicare payment adequately compensate for professional services. Cancer (Cancer Cytopathol) 2001;93:319 –322. © 2001 American Cancer Society. KEYWORDS: fine-needle aspiration, immediate interpretation, compensation, work load. 320 CANCER (CANCER CYTOPATHOLOGY) October 25, 2001 / Volume 93 / Number 5 F ine-needle aspiration (FNA) is used widely as the initial technique to obtain a tissue diagnosis in patients suspected of harboring a neoplastic process. FNA has been shown to be cost effective for the work-up of patients with suspected neoplasms in a wide variety of body sites, is considerably less expensive than alternate biopsy techniques, and it is associated with lower patient morbidity rates compared with open biopsy.1–7 Authorities on FNA have stated that immediate, on-site smear evaluation optimizes the technique’s diagnostic accuracy by reducing the rate of specimen inadequacy and aids in the timely procurement of additional material for special studies when needed.8,9 This beneficial effect is most prominent for FNA guided by computed tomography (CT), ultrasound, or other imaging techniques, for which the cost of repeating the study is relatively high. Little data exist documenting the time expenditures and costs associated with immediate, on-site smear evaluation and the associated prolonged attendance by cytopathologists at these procedures. Whereas some institutions have intraprocedural specimens prepared and interpreted by cytotechnologists or brought to the cytopathology laboratory for cytopathologist review, other institutions require on-site attendance by cytopathologists for smear preparation and interpretation. We studied the time commitments and costs associated with this latter approach at a university hospital and its associated clinics for FNAs performed at a variety of body sites using a range of guidance techniques. We correlated the cost of this time expenditure with Medicare compensation rates. In addition, comparison was made with time expenditure and Medicare compensation for the comparable activity of frozen section preparation and evaluation. MATERIALS AND METHODS One hundred forty-two consecutive fine-needle aspirates requiring cytopathologist involvement during the aspiration and immediate, on-site interpretations were studied for time utilization. These aspirates were obtained from a variety of body sites (Table 1) and were guided by a variety of imaging techniques (Table 2). The majority were performed by radiologists or clinicians, although a substantial minority were performed by cytopathologists (Table 2). All FNAs were associated with on-site, immediate microscopic evaluation, resulting in assessment of adequacy and a written preliminary cytologic diagnosis. Pathologist time was measured in minutes from the time the pathologist left the office to the time the pathologist returned to the office after the aspiration procedure and interpretation. Fifty consecutive frozen sections were timed sim- TABLE 1 Sites of Fine-Needle Aspiration in This Study Site No. of patients Head and neck Thyroid Lung Pancreas/biliary Liver Breast Axillary lymph nodes Bone/soft tissue Skin Chest Retroperitoneal Abdomen Eye Lymph node Site not given 17 29 23 8 14 11 3 8 3 6 3 12 1 3 4 TABLE 2 Guidance Techniques Used in This Study for Fine-Needle Aspiration Technique No. of patients Computerized tomography Ultrasound Endoscopy Bronchoscopy Intraoperative Hospital room palpable Clinic pathologist palpable Clinician palpable Outlying clinic 58 17 9 7 2 6 19 14 10 ilarly for comparison. Elapsed time for frozen section was calculated as the time from arrival of the frozen section specimen in the pathology laboratory to the telephonic reporting of a diagnosis to the operating room. For ease of comparison, costs for pathologist involvement were calculated using the 80th percentile salary level for an associate professor of pathology published from national data.10 This salary was converted to an hourly rate using a full-time service commitment of 50 hours a week and 48 weeks per year. An hourly cost of $88.83 per hour was calculated to include salary and associated benefits. The Medicare rate schedule effective in Utah for the CPT codes 88170 ($65.16) and 88172 ($32.88) was used to calculate compensation. Time studies for routine surgical pathology were performed by measuring with a stop watch the actual time required to evaluate the glass slides and dictate a report for CPT codes 88305, 88307, and 88309. This quantification was performed on 25 cases for each CPT code with an average of four pathologists. Like Cost Analysis of On-Site FNA Assistance/Layfield et al. TABLE 3 Average Time Expenditure by Cytopathologist for On-Site FineNeedle Aspiration Evaluation by Guidance Technique Guidance technique Time expenditure (minutes) Pathologist cost ($) Computerized tomography Ultrasound Endoscopy Bronchoscopy Intraoperative Hospital room palpable Clinic pathologist palpable Clinician palpable Outlying clinic palpable 48.7 44.4 56.2 55.3 55.0 46.7 42.5 34.7 44.4 72.10 65.73 83.20 81.87 81.43 69.13 62.92 51.37 65.73 the cytology compensation estimates, the Medicare rate schedule for CPT codes 88305 ($50.00), 88307 ($92.75), and 88309 ($127.75) was used. RESULTS The average time expenditure by cytopathologists associated with each guidance technique and site are given in Table 3 along with the associated cost for the cytopathologist’s time. CT-guided biopsies required approximately 49 minutes of cytopathologist time, ultrasound-guided biopsies required 44 minutes, endoscopic biopsies required 56 minutes, and bronchoscopic biopsies required 55 minutes. Aspiration of palpable lesions performed by clinicians but immediately interpreted by a pathologist required an average of 35 minutes of pathologist attendance. Aspirates of palpable lesions performed and interpreted by cytopathologists required 42 minutes of pathologist time. In contrast, the average frozen section required 16 minutes for performance and interpretation. The cost of on-site cytologic interpretation generally exceeded compensation by $40 –50 (Table 3). Only when pathologists personally performed the aspirates did compensation cover costs (Table 3). In comparison, compensation covered the total costs of frozen section examination in this study. On average, the professional time was 4.1 minutes for an 88305 procedure, 7.7 minutes for an 88307 procedure, and 17.5 minutes for an 88309 procedure. Hence, hourly compensation for signing out surgical pathology cases with a mixture of 50% 88305, 20% 88307, and 30% 88309, was $638. DISCUSSION FNA has been proven as an accurate, cost-effective technique for the diagnosis of patients with palpable and nonpalpable lesions at a variety of body sites.1–7,10 FNA is most accurate when immediate assessment for specimen adequacy is performed and a differential 321 diagnosis constructed so that additional material can be acquired for special studies when needed.8,9 Although these studies have demonstrated the economies associated with the use of FNA over other biopsy techniques, we are unaware of any studies evaluating time expenditures by cytopathologists involved in immediate, on-site evaluation of smears obtained by needle aspiration. The expenses to the pathology department associated with immediate, on-site interpretation and the associated prolonged attendance by cytopathologists have not been estimated to our knowledge. Using an 80th percentile salary for an associate professor of pathology ($88.83 per hour), we found that the Medicare reimbursement rate (88172) for onsite evaluation undercompensated this activity by an average of $40 –50 per patient. Only when the cytopathologist actually performed the aspirate and interpreted it in the clinic did Medicare compensation (88172 and 88170) cover the costs of cytopathologists’ time expenditure. Immediate consultation by pathologists is substantially undercompensated compared with routine surgical pathology, for which a pathologist can generate approximately $638 per hour. Hence, from a purely economic standpoint, a pathologist’s time is spent better signing out surgical patients than performing immediate, on-site evaluation of FNA specimens. Medicare reimbursement for frozen section evaluation adequately covers cost expenditures for this service. From these data, it appears that academic pathology departments and private practice groups are subsidizing immediate, on-site evaluation of FNAs by approximately $40 –50 per patient. This untoward economic impact may lead cytopathologists to de-emphasize on-site evaluation or defer such services to cytotechnologists in an attempt to alleviate the unfavorable economic impact. An alternative to the practice of immediate, onsite interpretation by pathologists is the use of cytotechnologists to screen patients and submit only difficult cases for pathologist review. Although this may be appropriate in some institutions, it results in cytotechnologists rendering diagnoses of malignancy, albeit preliminary. At our institution, preliminary onsite assessments are similar to frozen section results, in that therapeutic decisions may be enacted immediately based on these results. Hence, these diagnoses require the review of a pathologist. At institutions where therapeutic decisions are not based on immediate assessment but are delayed until final pathologist review, the use of cytotechnologists would appear to be a reasonable alternative if sufficient cytotechnologists are available. 322 CANCER (CANCER CYTOPATHOLOGY) October 25, 2001 / Volume 93 / Number 5 Preliminary, rapid, on-site diagnosis can be of marked clinical importance, in that it assures the presence of diagnostic material, allowing invasive and potentially morbid procedures to be terminated as soon as diagnostic material is obtained. This increases the safety of the procedure as well as optimizing utilization of procedure rooms and imaging facilities. In addition, it allows rapid institution of therapy in critically ill patients. Examples of conditions in which immediate diagnosis and rapid initiation of therapy may be critical include spinal cord compression by lymphoma (treatable by radiation therapy) and lung masses due to aggressive, infectious organisms. Further studies are necessary to confirm these findings. If subsequent studies support our data, then Medicare compensation rates should be re-evaluated and increased to provide adequate support for this clinically valuable service. In addition, codes like 99358 for prolonged attendance may help alleviate the negative economic impact on pathologists of prolonged attendance at image-guided FNAs. REFERENCES 1. 2. Frable WJ. Needle aspiration of the breast. Cancer 1984;53: 671– 6. Silverman JF, Lannin D, O’Brien K, Norris HT. The triage role of fine needle aspiration biopsy of palpable breast masses: diagnostic accuracy and cost-effectiveness. Acta Cytol 1987;31:731– 6. 3. Kaminsky DB. Aspiration biopsy in the context of the new Medicare fiscal policy. Acta Cytol 1986;28:333– 6. 4. Lannin DR, Silverman JF, Pories WJ, Walker C. Cost-effectiveness of fine-needle biopsy of the breast. Ann Surg 1986; 203:474 – 80. 5. Layfield LJ, Glasgow BJ, Cramer H. Fine-needle aspiration in the management of breast masses. In: Rosen PP, Pechner RE, editors. Pathology annual 1989, part 2. Norwalk: Appleton and Lange, 1989:23– 62. 6. Zarbo RJ, Howanitz PJ, Bachner P. Interinstitutional comparison of performance in breast fine-needle aspiration cytology: a Q-probe quality indicator study. Arch Pathol Lab Med 1991;115:743–50. 7. Layfield LJ, Chrischilles EA, Cohen MB, Bottles K. The palpable breast nodule. A cost-effectiveness analysis of alternate diagnostic approaches. Cancer 1993;72:1642–51. 8. Langlois SLP. Imaging methods for guidance of aspiration cytology. In: Orell SR, Sterrett GF, Walters MNI, Whitaker D, editors. Manual and atlas of fine needle aspiration cytology, 3rd ed. London: Churchill Livingstone, 1999:30. 9. Tao LC. Guides to clinical aspiration biopsy. Lung, pleura and mediastinum. Tilde S. Kline (ed). New York: IgakuShoin, 1988:9. 10. Rimm DL, Stastny JF, Rimm EB, Ayer S, Frable WJ. Comparison of the costs of fine-needle aspiration and open surgical biopsy as methods for obtaining a pathologic diagnosis. Cancer Cytopathol 1997;81:51– 6.