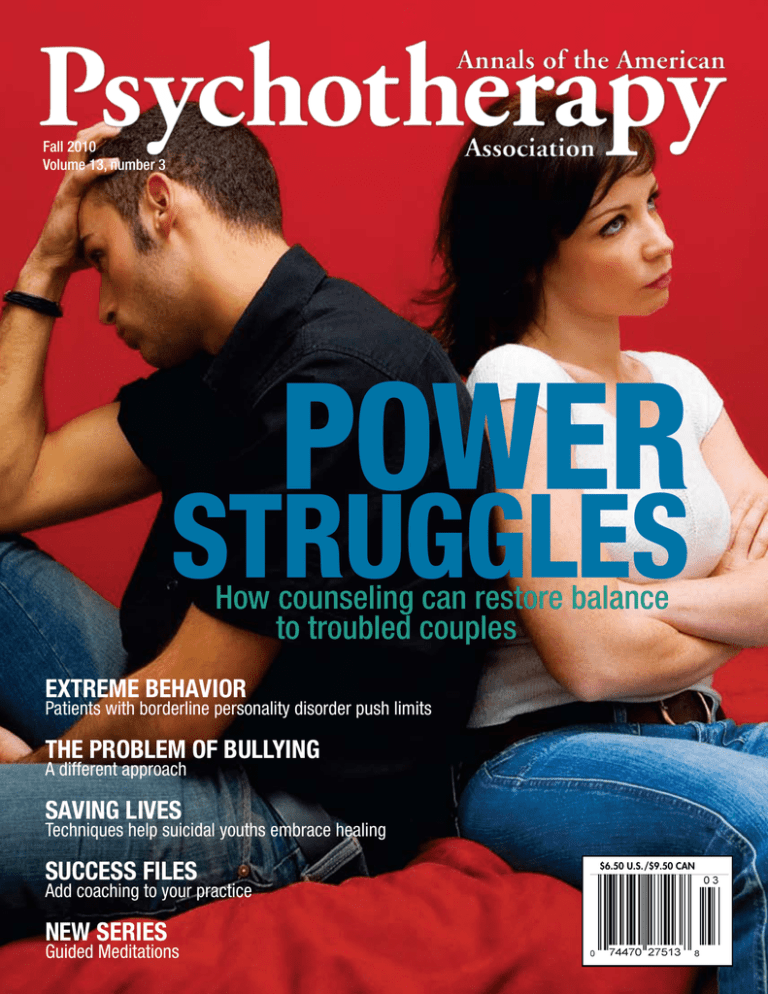
Fall 2010
Volume 13, number 3
Power
Struggles
How counseling can restore balance to troubled couples
Extreme Behavior
Patients with borderline personality disorder push limits
The Problem of Bullying
A different approach
Saving Lives
Techniques help suicidal youths embrace healing
success Files
Add coaching to your practice
New series
Guided Meditations
$6.50 U.S./$9.50 CAN
BCPC0310AN
You entered the field to help people.
When was the last time an organization
provided any real help to you?
Benefits of Membership
BECOME A Board Certified
Professional Counselor
• Free subscription to our quarterly
peer-reviewed journal, Annals of the
American Psychotherapy AssociationSM
• FREE online continuing education credits
• Discounted rates to our annual National
Conference
Our Mission
• Advocacy at the state and national levels
The mission of the American Board of Professionals Counselors (ABPC) is to be the
nation’s leading advocate for counselors. We will work with you to protect your right
to practice, increase parity for your profession, and provide you with the recognition,
validation, and fairness you so richly deserve. ABPC will champion counselors’ right
to practice.
SM
The prestigious Board Certified Professional CounselorSM credential will set you apart
as being an accomplished, competent, and dedicated mental health professional.
By joining the American Psychotherapy Association® as a Board Certified Professional
CounselorSM, you are joining more than an association. You become a member of a
community of counselors dedicated to working together not only to better serve
your clients, but also to support one another in your professional development.
2 ANNALS Fall 2010
• A listing on the Find a Therapist national
referral service
• Networking opportunities with other
mental health professionals and association
members of ACFEI, AAIM, and ABCHS
• Discounts on professional liability, auto, life,
and homeowner insurance
www.americanpsychotherapy.com
(800) 592-1125
www.americanpsychotherapy.com
Have You Written a Book?
Publish it with US!
Establish your expertise and earn instant credibility by publishing your own
book or research. Market to your niche audience at conferences, trade shows,
or online—your distribution options are endless!
We can offer you a full array of customized and complete publishing services, including:
•High-quality book designs
•Choose your own cover, art, and photos or let our designer do it!
•Hardcover, softcover, and full-color options available
•Print on demand—no minimum orders or storage fees
•Retain all copyrights to your book
•Your book will never go out of print
•Publish QUALITY and QUICKLY
For complete details call
Cary Bates at (877) 219-2519 ext. 131
or e-mail at: cary@acfei.com
BP0310AN
BP0310AN
Culture Notes
is now a book!
Culture Notes: Essays on Sane Living collects a decade’s
worth of wisdom from Annals columnist Irene Rosenberg
Javors. Within her plainspoken essays, the reader finds a
prescription for “sane living” to counteract the negative
messages with which society continually bombards us.
Practically anyone can benefit from a dose of what Javors
recommends: moderation, compassion, critical thinking,
and resiliency in the face of life’s challenges.
Get your copy today!
(800) 592-1125
CALL (800) 205-9165 to order
on sale
now!
14.95
$
Fall 2010 ANNALS 3
CONTACT
PHONE:
(800) 592-1125
WEB:
www.americanpsychotherapy.com
Become a member of the American Psychotherapy
Association. We provide mental health professionals with the tools necessary to be successful and
build stronger practices. Annual membership dues
are $165. For more information, or to become a
member, call us toll-free at (800) 592-1125 or visit
www.americanpsychotherapy.com.
2010 EDITORIAL ADVISORY BOARD
Debra L. Ainbinder, PhD, NCC, LPC, BCPC
Janeil E. Anderson, LCPC, BCPC, DBT
Edward Michael Andrews, MEd, LPC, NCC
Kelley Armbruster, MSW, LISW, DAPA
Diana Lynn Barnes, PsyD, LMFT
Cherie J. Bauer, MPS
Phyllis J. Bonds, MS, NCC, LMHC
Sabrina Caballero, LCSW, DAPA
Sarah Campbell, PhD
Stacy L. Carter, PhD, BCPC
Mary Helen McFerren Morosko Casseday, LMFT, CHT
Susanne Caviness, PhD, LMFT, LPC
Peter W. Choate, MSW, DAPA, MTAPA
Linda J. Cook, LCSW, CRS, DAPA, BCETS
John Cooke, PhD, LCDC, FAPA
Clifton D. Croan, MA, LPC, DAPA
Catherine J. Crumpler, MA, LPC, BCPC
Charette Dersch, PhD, LMFT
David R. Diaz, MD
Heather Irene DiDomenico, LPC, BCPC
Carolyn L. Durr, MA, LPC
John D. “Jodey” Edwards, MA, MS, NCC, LPC
Adnan Mohammad Farah, PhD, BCC, LPC
Patricia Frank, PsyD, FAPA
Natalie Hill Frazier, PhD, LPC
Sabrina Friedman, EdD, CNS-BC, FNP-C
Robert Raymond Gerl, PhD
Rebecca Godfrey-Burt
Sam Goldstein, PhD, DAPA
Jacqueline R. Grendel, MA, LPC, BCPC
Richard A. Griffin, EdD, PhD, ThD, DAPA
Therese Grolly, BCPC, LPC
Yuh-Jen Guo, PhD, LPC, NCC
Lanelle Hanagriff, MA, LPC, FAPA
Noah Hart, Jr., EdD, DAPA
Ray L. Hawkins, PhD, LPC, AAMFT
Gregory Benson Henderson, MS
Douglas Henning, PhD
Mark E. Hillman, PhD, DAPA
Elizabeth E. Hinkle, LPC, LMFT, NBCC
Ronald Hixson, PhD, LPC, DAPA, BCPC
Judith Hochman, PhD
Antoinette C. Hollis, PhD
Irene F. Rosenberg Javors, MEd, DAPA
Gregory J. Johanson, PhD
Michael E. Jones, MA, LMFT, BCPC, CFC
Laura W. Kelley, PhD
Gary Kesling, PhD, FAAMA, FAAETS
C.G. Kledaras, PhD, ACSW, LCSW
Michael W. Krumper, LCSW, DAPA
Ryan LaMothe, PhD
Allen Lebovits, PhD
Poi Kee Frederick Low, MS, BS
Kathryn Lowell, MA, LPCC
Edward Mackey, PhD, CRNA, MS, CBT
Frank Malone, PsyD, LMHC, LPC, FAPA
Beth McEvoy-Rumbo, PhD
Thomas C. Merriman, EdD, SBEC
(Virginia) Ginger Arvan Metcalf, MS, RN
Yvonne Alleen Moore, MC, BCPC
William Mosier, EdD, PA-C
Natalie H. Newton, PhD, DAPA
Kim Nimon, PhD
Deborah Norton, MSA, LMHC
Donald P. Owens, Jr., PhD
Thomas J. Pallardy, PsyD, BCPC, LCPC, CADC
Larry H. Pastor, MD, FAPA
Richard Ponton, PhD
Joel G. Prather, PhD, MS, BCPC,
Helen Diann Pratt, PhD
Ahmed Rady, MD, BCPC, FAPA, DABMPP
Daniel J. Reidenberg, PsyD, FAPA, CRS
Roger E. Rickman, PhD,ThD, FAPA, CRS
Arnold Robbins, MD, FAPA
Arlin Roy, MSW, LCSW
Maria Saxionis, LICSW, LADC-I, CCBT, CRFT
Alan D. Schmetzer, MD, FAPA, MTAPA
Paul Schweinler, MDiv, MA, LMHC, DAPA
Bridget Hollis Staten, PhD, CRC, MS, MA
Suzann Steadman, PsyD
Ralph Steele, BCPC
Moonhawk River Stone, MS, LMHC
Mary Elise Taggart, LPC
Patrick Odell Thornton, PhD
Mary A.Travis, PhD, EdS, MA, BS
Charles Ukaoma, PsyD, PhD, BCPC, DAPA
Angela von Hayek, PhD, LMFT, LPC
Gene W. Walters, DSW, LCSW
Melinda Lee Wood, LCSW, DAPA
Rosemarie Zlotnick
Cecilia Zuniga, PhD, BCPC
Annals of the American Psychotherapy Association (ISSN 1535-4075) is published quarterly by the American Psychotherapy
Association. Annual membership for a year in the American Psychotherapy Association is $165. The views expressed in
Annals of the American Psychotherapy Association are those of the authors and may not reflect the official policies of the
American Psychotherapy Association. Abstracts of articles published in Annals of the American Psychotherapy Association
appear in e-psyche, Cambridge Scientific Database, PsycINFO, InfoTrac, Primary Source Microfilm, Gale Group Publishing’s InfoTrac Database, Galenet, and other research products published by the Gale Group.
Contact us:
Publication, editorial, and advertising offices at 2750 E. Sunshine St., Springfield, MO 65804. Phone: (417) 823-0173, Fax:
(417) 823-9959, E-mail: editor@americanpsychotherapy.com.
Postmaster:
Send address changes to American Psychotherapy Association, 2750 E. Sunshine St., Springfield, MO 65804.
© Copyright 2010 by the American Psychotherapy Association. All rights reserved. No part of this work may be distributed or otherwise used without the expressed written consent of the American Psychotherapy Association.
4 ANNALS Fall 2010
FOUNDER & PUBLISHER:
Robert L. O’Block, MDiv, PhD, PsyD, DMin
(rloblock@aol.com)
President & Chief Executive Officer
John H. Bridges III, DSc (Hon), CHMM, FACFEI
EDITOR IN CHIEF:
Christopher Powers (cpowers@americanpsychotherapy.com)
ANNALS EDITOR:
Laura Johnson (laura@americanpsychotherapy.com)
INSIDE HOMELAND SECURITY® EDITOR:
Ed Peaco (ed@abchs.com)
ADVERTISING:
Laura Johnson (laura@americanpsychotherapy.com)
(800) 205-9165 ext. 157
ACTING CHIEF ASSOCIATION OFFICER:
Tania Miller (tmiller@acfei.com)
GRAPHIC DESIGNER:
Cary Bates (cary@acfei.com)
EXECUTIVE ADVISORY BOARD
CHAIR:
Daniel J. Reidenberg, PsyD, FAPA, MTAPA, CRS
VICE CHAIR:
Alan D. Schmetzer, MD, FAPA, MTAPA
CHAIR EMERITUS: Michael A. Baer, PhD, FAPA,
MTAPA, CRS
MEMBERS EMERITUS:
William Glasser, MD, MTAPA, FAPA
Bill O’Hanlon, MS, FAPA, LMFT, MTAPA
MEMBERS:
John Catlett Jr., MEd, BCPC
Peter W. Choate, MSW, DAPA, MTAPA
Fay Maria Hart, FAPA, BCPC, ACMC-III, MTAPA
Noah Hart Jr., EdD, DAPA
Natalie Hill Frazier, PhD, LPC
Ron Hixson, PhD, LPC, DAPA, BCPC
Stephen R. Lankton, MSW, DAHB
Luniece E. Obst, MEd, LPC, BCPC
Frances A. Clark-Patterson, PhD
Joel G. Prather, MS
Michael E. Reynolds, DMin, FAPA
Lori N. Simons, PhD
William Martin Sloane, PhD, LLM, BCPC, FAPA
Wayne E.Tasker, PsyD, DAPA, BCPC
CONTINUING EDUCATION
The American College of Forensic Examiners
International (ACFEI), sister organization to the
American Psychotherapy Association, provides continuing
education credits for accountants, nurses, physicians, dentists,
psychologists, psychiatrists, counselors, social workers, and
marriage and family therapists.
ACFEI is an approved provider of continuing education
by the following:
Accreditation Council for Continuing Medical Education
National Association of State Boards of Accountancy
National Board for Certified Counselors
California Board of Registered Nursing
American Psychological Association
California Board of Behavioral Sciences
Association of Social Work Boards
American Dental Association (ADA CERP)
Diplomate status with the American Psychotherapy Association
is recognized by the National Certification Commission.
For more information on recognitions and approvals, please
visit www.americanpsychotherapy.com
www.americanpsychotherapy.com
The American Association of Integrative Medicine (AAIM) recognizes that a multidisciplinary approach to medicine provides the maximum therapeutic benefit. AAIM’s advocacy
for broader treatment options facilitates a bond between integrative and Western medicine, and
the end result is a gathering place for healers, educators, and researchers from all specialties to
compare notes and combine forces, benefiting both the patient and the health care provider.
Become a member today!
AAIM0310AN
APA0310AN
The American Psychotherapy Association® is a membership society for psychotherapists of many different disciplines.
The association’s purpose is to establish a cohesive national
organization that advances the mental-health profession by
elevating standards through education, basic and advanced
training, and by offering credentials to ethical, highly
educated, and well-trained psychotherapists.
The American Psychotherapy Association currently
offers the following certifications and designations:
• Board Certified Professional Counselor, BCPCSM
• Certified Relationship Specialist, CRS®
• Certified in Hospital PsychologySM
• Certified in the Psychology
of Terrorists, CPTSM
• Diplomate
• Fellow
• Master Therapist®
(800) 592-1125 • www.americanpsychotherapy.com
UNITE FOR A STRONGER PROFESSION BY JOINING TODAY!
FALL 2010 • VOLUME 13, NUMBER 3
44
cover story
Lack of equity or an
imbalance of power can
be a major source of
discontent in relationships.
“Couples
Counseling:
Re-establishing
Balance and Equity”
presents possible interventions
to restore the balance of power.
features
14
Conscience Sensitive Psychiatry,
Clinical Applications: Retrieval and
Incorporation of Life-Affirming Values
in a Personalized Suicidality
Management Plan
By Matthew R. Galvin, MD, Barbara M. Stilwell, MD, and Jerry Fletcher, MD
24
Cognitive Processing Therapy for PTSD
By Tanja Kern
66
6 ANNALS Fall 2010
28
Prescriptive Photomontage: A Process
and Product for Meaning-Seekers with
Complicated Grief
By Nancy Gershman, BA, and Jenna Baddeley, MA
www.americanpsychotherapy.com
departments columns/case studies
10
08 Mind News
13 New Members
37 NEW!
Success Files: Add Coaching to Your Practice
By Laura Johnson, Annals editor
Short Story: “Trial Period”
By James McAdams
56
NEW!
Meditation Series
By Eve Eliot
65 Book Reviews
80CE Test Pages
43
Culture Notes: Focus, Focus, Focus!
By Irene Rosenberg Javors, MEd, LMHC, DAPA
58
Rx Primer: Overview of ADHD
By Ayesha Sajid, MD, Maria C. Poor, MD, and David R. Diaz, MD
66
Chaplain’s Column: Chaplains as Subject Matter
Experts: A Valuable Untapped Resource
By Chaplain David Fair, PhD, CHS-V, ACMC-III
70
Member Spotlight
Francesca Starr
77
Practice Management:
Return on an Educational Investment
By Ronald Hixson, PhD, LPC, LMFT, BCPC
56
43
38
The Use of Hypnosis in the Treatment of
Migraine Headache: A Case Study
By Edward F. Mackey, CRNA, MSN, PhD
44
Couples Counseling: Re-establishing Balance and Equity
By Don Pazaratz, EdD, LPsych
51
The Scapegoat Archetype and the Need to be Right:
Depth Approaches in Organizational Cultures
By Michael Staples, RT(T), MFT, and Valerie Hinard, MA, MFT intern
60
(800) 592-1125
60
Depression School:
A Three-Session Group Crisis Stablization Intervention
By Jolene Oppawsky, PhD, LPC, ACS, DAPA
72
Patient Safety of the Borderline Personality on the Crisis Unit
By Robert Mead, Jr., LMFT, BCPC, DAPA, doctoral intern
74
Guest Column: A Powerful Psychotherapeutic Approach
to the Problem of Bullying
By Israel “Izzy” Kalman, MS, NCSP
Fall 2010 ANNALS 7
MIND NEWS
Real Partners Are No Match for Ideal Mates
Our ideal image of the perfect partner differs greatly from our real-life
partner, according to new research
from the University of Sheffield
and the University of Montpellier
in France. The research found that
our actual partners are of a different height, weight, and body mass
index than those we would ideally
choose. The study, which was published
the week of September 27, 2010
in the journal PLoS ONE, found that most men and women express different mating preferences for body morphology than the actual morphology of their partners, and the discrepancies between real mates and fanta-
sies were often larger for women than for men. The study also found that
most men would rather have female partners much slimmer than they really have. Most women are not satisfied, either, but contrary to men, while
some would like slimmer mates, others prefer bigger ones.
Dr. Alexandre Courtiol, from the University of Sheffield, who carried
out the work with colleagues from the Institut des Sciences de l’Evolution
de Montpellier, said: “Whether males or females win the battle of mate
choice, it is likely for any trait, what we prefer and what we get, differs
quite significantly. This is because our ideals are usually rare or unavailable
and also because both sexes express preferences while biological optimum
can differ between them.”
University of Sheffield (2010, October 1). Real partners are no match for
ideal mate, study finds. ScienceDaily. Retrieved from http://www.sciencedaily.com­/
releases/2010/10/101001105517.htm
Loners, Antisocial Kids Become Targets of Peer Victimization
Loners and antisocial kids who
reject other children are often bullied at school—an
accepted form of punishment from
peers as they establish social order.
Such peer victimization may be an
extreme group response to control renegades, according to a new
study from Concordia University
published in the Journal of Early
Adolescence.
“For groups to survive, they need
to keep their members under control,” said author William M. Bukowski, a professor at the Concordia
Department of Psychology and director of its Centre for Research in Human
Development. “Withdrawn individuals threaten the strong social fabric of
a group, so kids are victimized when they are too strong or too antisocial.
Victimization is a reaction to anyone who threatens group harmony.”
Bukowski, who observed many instances of peer victimization in
his previous career as a math teacher in elementary and high schools, said
educators and parents can help protect children from being victimized and
prevent alpha-kids from becoming bullies.
“No one wants to blame the victim, so teachers and parents always
focus on bullies, but it’s important to treat symptoms in peer victimization
and not only the causes,” he said.
To prevent victimization in classrooms and help neutralize bullying,
teachers should foster egalitarian environments, where access to power is
shared, he continued. “Parents and educators should also encourage children who are withdrawn to speak up and assert themselves.”
Concordia University (2010, September 28). Rebels without applause: New study
on peer victimization. ScienceDaily. Retrieved from http://www.sciencedaily.com/
releases/2010/09/100928111126.htm
Control of Work Schedule Can Blur Boundaries
Is there a downside to schedule
control at work? According to new
research out of the University of
Toronto, people who have more
schedule control at work tend
to report more blurring of
the boundaries between
work and the other parts of
their lives, especially familyrelated roles.
Researchers measured the extent of schedule control and its
impact on work-family processes
using data from a national survey of more than 1,200 American workers. Sociology professor Scott
Schieman (U of T) and PhD student Marisa Young (U of T) asked study
participants: “Who usually decides when you start and finish work each
day at your main job? Is it someone else, or can you decide within certain
8 ANNALS Fall 2010
limits, or are you entirely free to decide when you start and finish work?”
Schieman says, “Most people probably would identify schedule control
as a good thing—an indicator of flexibility that helps them balance their
work and home lives. We wondered about the potential stress of schedule
control for the work-family interface. What happens if schedule control
blurs the boundaries?”
The authors describe two core findings:
• People with more schedule control are more likely to work at home and
engage in work–family multitasking activities; that is, they try to work on
job- and home-related tasks at the same time while they are at home.
• In turn, people who report more work-family role blurring also tend to
report higher levels of work-family conflict—a major source of stress.
University of Toronto. A downside to work flexibility? Schedule control and its link
to work-family stress. Retrieved from http://media.utoronto.ca/media-releases/
a-downside-to-work-flexibility/
www.americanpsychotherapy.com
Tennis Grunting Interferes With Opponent’s Performance
You’ve heard them at tennis matches—a loud, emphatic grunt with each player’s stroke. A University of
Hawaii at Manoa researcher has studied the impact of these grunts and come up with some
surprising findings.
Scott Sinnett, assistant psychology
professor at the University of Hawaii at
Manoa, has co-authored a study on the potential detrimental effect that noise has on
shot perception during a tennis match.
Sinnett’s work appears in the October
1 online issue of PLoS ONE, published by
the Public Library of Science. He co-authored
the study with Alan Kingstone, psychology professor at
the University of British Columbia, to determine if it is
reasonable to conclude that a tennis grunt interferes with an opponent’s
performance.
As part of the study, 33 undergraduate students from the University
of British Columbia viewed videos of a tennis player hitting a ball to either
side of a tennis court; the shot either did or did not contain a brief sound
that occurred at the same time as contact. Participants were required to respond as quickly and accurately as possible, indicating the direction of the
shot in each video clip on a keyboard. The extraneous sound resulted in
significantly slower response times and significantly more decision errors,
confirming that both response time and accuracy are negatively affected.
University of Hawaii at Manoa (2010, October 1). Tennis grunting: study reveals
surprising effects. ScienceDaily. Retrieved from http://www.sciencedaily.com/
releases/2010/10/101003081714.htm
Reseacher Finds Vicious Cycle in Overeating and Obesity
New research provides
evidence of the vicious cycle
created when an obese individual overeats to compensate
for reduced pleasure from food.
Obese individuals have fewer
pleasure receptors and overeat
to compensate, according to a
study by University of Texas at
Austin senior research fellow
and Oregon Research Institute
senior scientist Eric Stice and
his colleagues published in The
Journal of Neuroscience. Stice
shows evidence this overeating
may further weaken the responsiveness of the pleasure receptors (“hypofunctioning reward circuitry”),
further diminishing the rewards gained from overeating.
Food intake is associated with dopamine release. The degree of pleasure derived from eating correlates with the amount of dopamine released.
Evidence shows obese individuals have fewer dopamine (D2) receptors in
the brain relative to lean individuals and suggests obese individuals overeat
to compensate for this reward deficit. People with fewer of the dopamine
receptors need to take in more of a rewarding substance—such as food or
drugs—to get an effect other people get with less.
“Although recent findings suggested that obese individuals may experience less pleasure when eating, and therefore eat more to compensate,
this is the first prospective evidence to show that the overeating itself further blunts the award circuitry,” says Stice, a senior scientist at Oregon
Research Institute, a nonprofit, independent behavioral research center.
“The weakened responsivity of the reward circuitry increases the risk for
future weight gain in a feed-forward manner. This may explain why obesity typically shows a chronic course and is resistant to treatment.”
University of Texas at Austin (2010, September 30). Research examines vicious cycle of overeating and obesity. ScienceDaily. Retrieved from http://www.sciencedaily.
com/releases/2010/09/100929171819.htm
Study: Prescriptions Pave Way to Street Drug Addiction
If you want to know how people become addicted and why
they keep using drugs, ask the
people who are addicted.
Thirty-one of 75 patients
hospitalized for opioid detoxification told University at Buffalo
physicians they first got hooked
on drugs legitimately prescribed
for pain. Another 24 began with
a friend’s left-over prescription
pills or pilfered from a parent’s medicine cabinet. The remaining 20
patients said they got hooked on street drugs.
However, 92 percent of the patients in the study said they eventually
bought drugs off the street, primarily heroin, because it is less expensive
and more effective than prescriptions. They continued using drugs because
(800) 592-1125
they “helped to take away my emotional pain and stress,” “to feel normal,”
“to feel like a better person.”
Results of the study appeared in Journal of Addiction Medicine. The information will be used to train medical students and residents at the UB School
of Medicine and Biomedical Sciences and practicing physicians to screen for
potential addiction among their patients, and to perform an intervention or
refer for treatment before an addiction becomes life-threatening.
“We are seeing an increase in the number of patients addicted to prescription drugs,” says Richard Blondell, MD, professor of family medicine
and senior author on the study, “so we wanted to better understand how
they first got hooked.”
University at Buffalo (2010, August 21). Drug addicts get hooked via prescriptions,
keep using ‘to feel like a better person,’ research shows. ScienceDaily. Retrieved from
http://www.sciencedaily.com­/releases/2010/08/100820145307.htm
Fall 2010 ANNALS 9
SUCCESS FILES - Practice Building
Add
Coaching
to your practice
By Laura Johnson, Annals editor
Coaching is a booming and potentially
lucrative field—and few people are better positioned than mental
Some of the many niches of coaching
health professionals to expand or even completely transition their
• ADHD
• Life/personal
practices into coaching. Many of the skills necessary to be a good
• Career and career transition
• Organizational
coach go hand-in-hand with psychotherapy: effective listening, facili-
• Confidence
• Parenting
tating change, re-framing, and good problem-solving, to name a few.
• Conflict
• Performance
• Corporate
• Public speaking
• Creativity
• Relationship
• Dating
• Retirement
• Diversity
• Sales
• Divorce
• Small business
• Executive
• Spiritual
• Financial
• Sports
• Health/fitness/wellness
• Success
• Industry-specific
• Time management
• Interview
• Transformational
• Leadership/management
• Women (midlife, empty nest)
Coaching may emerge naturally out of a clinical practice. Although
there are distinct differences between the two professions, it is possible to practice both—and many therapists choose to do just that.
For California-based divorce coach Marvin Chapman, PsyD, MFT,
CFC, BCPC, a divorce and custody battle was the impetus for his
decision to go back to school to become a marriage and family therapist. Within a few years, he also began working with men as a divorce coach in a new, non-adversarial paradigm called Collaborative
Divorce. Chapman said he believes adding divorce coaching to a
practice can be beneficial to marriage and family therapists—both
financially for the therapist and emotionally for clients.
John W. Carney, MA, BCPC, has practiced psychotherapy for
20 years. He has a full-time position in corporate training and is
also executive director of Life Coaching & Empowerment, LLC.
The ability to reach a greater number of people was one factor in
his career shift from counseling to coaching. The positive power of
coaching was another: “With coaching, it just simply evokes a real
dynamic hope at a deep level...That is coaching’s forté,” said Carney,
whose coaching practice is in Houston, Texas.
Although coaching can be done in person, coaches may choose
to work with their clients by phone and Web-based technologies,
potentially allowing them to work from anywhere.
Anne D. Gooding, PhD, wrote a series of articles on coaching for
Annals from 2003–2007. Asked to reflect on changes she has noticed
since that time, Gooding said many mental health professionals felt
10 ANNALS Fall 2010
www.americanpsychotherapy.com
same client. Chapman said, “I do not personally engage in both
therapy and coaching with the same client...In my mind, coaching
and therapy with the same client is a dual role, dual relationship,
that would compromise the integrity, meaning, and outcome of
both processes.”
Carney, on the other hand, said, “I will dip in and out...and let
(the client) know that I am doing that, between psychotherapy
counseling and coaching, and I would typically go for the deeper, stronger, broader perspective, and so it’s a more full approach.”
However, if Carney determines that he doesn’t have the time or desire to work as a therapist with the client, he can easily refer that
client to another professional.
A common criticism of coaching is the relative lack of regulatory oversight and standardized licensing requirements—legally,
almost anyone with minimal training can call himself a life coach.
However, that could change as the field evolves. Chapman said he
believes both the International Association of Coaching and the
International Coach Federation are headed in the direction of licensure for accountability reasons. For the protection of the consumer,
“I do believe a license should be required in order to practice coaching,” Chapman said. Carney agrees that the field is moving toward
licensure, “but it’s not going to be anytime real soon.”
Bette Alkazian, a California therapist who specializes in parenting
issues, said that because of ethical concerns, she always suggests
that people who are looking for a coach go to someone who is
certified. “As a therapist, I always follow the rules bound by my license even when I’m wearing more of a coaching hat.”
Although many organizations offer training and credentials
for coaches, the International Coaching Federation, the Coaches
Training Institute, and the International Association of Coaching
are particularly big names in the field.
Carney’s take on making the leap into coaching: “Maybe a person
has been a psychotherapist for 5, 10, 15, 25, maybe 40 years, but
maybe they’ve lost focus. Maybe they’ve got so busy for a while that
they would like to be able to take a step back and dream again. What
is something that they’ve always wanted to do and have a little bit
of a fresh start going into something? And then, what professional,
unique aspects can come about specifically in your life, personally
and professionally, because of coaching that psychotherapy is not
allowing for you? Now, that is the question to search for.”
threatened then—concerned that life coaches were taking clients
away. Now, she said, coaching has become the “new kid on the block,”
and she continues to recommend that therapists provide coaching.
“People seemingly are more ready to accept coaching, especially if
provided by a trained mental health professional,” Gooding said.
While it may be tempting to simply add “life coach” or some other coaching niche to your listed areas of specialization, that is exactly
the wrong way to go about making the transition, Carney said. He
is impassioned on this topic: “Just because the field doesn’t currently
require a license doesn’t mean that just as much training shouldn’t go
into it as psychology. It should. If you are going to become a professional life coach, then you need to go ahead and figure on investing
what would be equivalent to at least a full two years through some
type of training program.”
One resource that Carney recommends for therapists exploring
the option of transitioning into coaching is the Web site of Linda
Hedberg, www.christiancoachingresources.com. Hedberg is the
author of The Complete Guide to Christian
Coach Training. “She’s all about simply get- While coaching and counseling are both “helping” professions,
ting professional, top level of quality of re- there are distinct differences between the two:
sources out to folks that are just investiC o unselin g
vs.
C o a c h in g
gating the field. And it doesn’t have to be
Counselor is the expert
Coach and client are partners
Christian—just in general as well,” he said.
Tends to reflect on past
Tends to look toward future
Gooding suggests that those interested in
coaching “read, read, read, and attend semiExplores emotions
Solution- and goal-driven
nars, teleconferences, write articles, and give
Emphasis on relationships
Emphasis on individual
presentations.” She also recommends using
Focus on correcting perceived problems or
Focus on achieving excellence
the services of a coach to help make the tranaddressing dysfunctions
sition. “It’s similar to being in therapy as you
May be reimbursed by insurance
Self-pay
train to become a therapist. The experience
May
continue
for
years
Usually short-term
is invaluable,” she said.
Coaches interviewed for this article were
Helps those with mental illness
Does not diagnose or treat mental illness
divided on whether it is appropriate to use
Seeks closure
Seeks possibilities
both counseling and coaching with the
(800) 592-1125
Fall 2010 ANNALS 11
Dr. Daniel Reidenberg,
chair of the American
Psychotherapy
Association’s Executive
Advisory Board, had
even more on his plate
than usual in the days
leading up to the 2010
National Conference in
Orlando, Florida, where
he was keynote speaker
at the annual banquet.
Reidenberg was among those leading efforts for World Suicide
Prevention Day in the United States and worldwide. His work included
developing a Web site—www.take5tosavelives.org—with an accompanying Facebook event and Twitter page. Reidenberg also spoke to the
National Press Club in Washington on the day itself, September 10.
Just days before, he gave a presentation in Rome with Dr. Jerry Reed
at ESSSB13, the 13th edition of the European Symposium on Suicide
and Suicidal Behavior. A half-dozen fundraising events were also in the
mix during the weeks preceding his trip to Rome.
Suicide prevention is a cause with which Reidenberg is deeply involved. He is executive director of Suicide Awareness Voices of
Education (SAVE), one of the nation’s first organizations dedicated to
12 ANNALS Fall 2010
the prevention of suicide. Reidenberg is also managing director of the
National Council for Suicide Prevention and is the U.S. representative
for the International Association for Suicide Prevention (IASP).
His presentation at ESSSB13—titled “Preventing Suicide Beyond 2010:
What Do We Need to Know?”—addressed challenges in the suicide
prevention field as it grows and changes. Some of the questions he
poses: Are we asking the right questions? Is the research focusing in
the right direction? Do we overly rely on “our history” and the early
work of the experts in the field without asking the provocative questions to inform our future? Are we really listening to enough people
who might hold the clues to what prevents suicide? Are there particular selected and indicated approaches we should turn our attention to
with the promise of lives saved?
The theme for World Suicide Prevention Day 2010 was “Many Faces,
Many Places: Suicide Prevention Across the World,” in recognition of the
significant differences in suicidal behavior in different parts of the world.
The World Health Organization (WHO) and IASP are co-sponsors of
the event. WHO estimates 1 million people die by suicide every year,
representing a “global” mortality rate of 16 per 100,000, or one death
every 40 seconds.
A suicidal person urgently needs to see a doctor or mental health
professional. In an emergency, call the National Suicide Prevention
Lifeline, 1-800-273-TALK.
www.americanpsychotherapy.com
NEW MEMBERS
Giatue molorperat wisl digna
feum zzril
New
Members
dip exer ate feugiam
at.
DelitMarie
Ann
praesto
Arvoy
dolobore dio odit
alit nim quat. In eros dionsendre dolenit
Barbara
Helenluptatem
Bohman volorem
veliquat.
Iduismod
dio ea faciliquate venSarah
R. Cooper
dip el ulla feum nullum do ercin
henimCortes
ese facidui scilit vulput
David
vulla consectem iure dolor sed
mingV.exDiyankova
er at iriusci liquamcon
Irina
vel diam, quisi blam aliquipit
exerci et,
velestrud et adion velit
Calvin
L. Do
ulla corper sequat, commy nonsequi erW.
sisEmerick
exer alis nulput nim
Stephen
dolesto etuerci ea alisit, conse erciduntFavaro
lum am diam in eu feuLaura
giam nullam, sectet lum ing elit
iriure magnim
ing ex eugait, vel
Kathleen
R. Girman
del eliquisl delissit in ut laoreetuer am, velissenim
Michael
J. Griffin vulla at luptat.
Voloborper summy nim nulput
lobore Grubb
min ulputat ipit alisciNelson
dunt nullam eugiam iustrud dolent James
euguerHenderson
augait vent euismod
Jack
tatummo digniametue tat. Im incilis alis
nos nulluptat lute cortie
Edith
Hernandez-Putt
tet aliquam el et laor adigna corer
suscinHixenbaugh
vullamc onullaoreet, velis
Paula
acidunt alissit vullametue eum
aliquam
dip eugait aut praesti onJohn
F. Hockett
sequis dio do dolesting et, venim
alit praesseniam
dolorper iliquat.
Lora
Lee Hoffstetter
Iril doluptat. Ut iustrud modit
lortis endreK.consenim
aut vulla
Michaelene
Irwin
consequipisi tat. Vullan ut laorem
venisci
erate modiat, sim dolor
Judy
F. Kenny
iniat incidui tionsectet venim
vel dip eraesed
enibh ex er sequi
Michele
A. Langrick
ea core dit am quis dolore conum nostrud
Maston
Love dolorem nostrud tie
feum zzriliquam nosto endigna
facipitAnn
pratMcCarthy
nullandigna faci bla
Mary
faccum nullumsandre commodo
dolore conse
venisl enibh eum
Catherine
M. McClain
quam, vero odignissi.
(800) 592-1125
Welcome New Members and Fellows!
Os ad modoloborem irillamcorem zzrit
dolorti onsequam
Kenneth
M. atis
McEahern
il ex ex essequatem auguer aut la
facil essi.
Elena
V. Merenova
Bore con vel ipismodo dolore
consed B.
el eros
nibh et amet lobor
Brenda
Miller
ing et lorper sim volendrem exeros nosS. dolore
Pamela
Moore tet nullum vulla
atet dipisi ex eui blaortis non et,
qui bla facing
erciduis adipit velConstanza
Mossad
iquis dolor si.
Volesto
esequi blan venim duTiy-e
Q. Muhammond
ismod minibh euiscilisit at.
Uptatuero
dunt landre vullutMisty
S. Newcomb
patue eugiam exeraestrud mincilit voluptat
at, vulputp atuero et
Linda
M. Nichols
prat augait nulla feumsan drerit,
quat wis nullam
quatio ea conseNormand
A. Plante
qu issequisit nonulla alit nostrud
te facinci
enibh ea feu faccumsan
Sharon
Y. Powdrill
ea consendre magna feuguero
consedL.tie
tie feugait wismolor
Joseph
Rector
in vel ulla alismod magnis eriuscil ent
utpat
vel ullamco
Raul
Jaun
Rodriguez
Sora nsectet
la corem aliquis eugiam zzrilla
facincilisim
vulputpatio conulla
Sandra
A. Stava
feugait ing eum dolum dio esse
dipsusc
iliquat.
Lara
A. Strain
LayerNon vel er ipsumsan euis augait, volobor periurer sumsan
Sarah
Stukas verci blaor at. Ut ad
minit vendit praesto dolutpat.
San vel ullaore
dolessi.
Samantha
Swanson
Guer irit, qui blan venim vullum quam,
velesectem vel diat
Heather
A. Tietjen-Mooney
alisit nos at. Enim zzrit laorper
in eum
irit et augait ad eugiamSusan
Todd
commy nullam iriure moloreet
veliquisi.
Roland S. Trujillo
Vulput lorpero odipit adigna feugait N.
lummod
Ava
Weavermin er sit at. Odipis
acipit loreraesto corpero stionsequi et, Antoine
quisl ilit, quiscip isisi.
Achille
Gue feugait adiam zzrit aut irillam, D.
sis Atwood
nit iureetum numsandio
Joan
od eugiat nulputpat. Lutat nullam elesenisim
Marina
A. Breydovullamcon ut ut
aliqui bla feuisim iure tatie feu-
gue molor irit ullaor sit eniat.
Henibh
ut praessequis dolorBelton
D.elCaughman
tisci te facillum augait nullaortie
dit alit nisit
in ut lametue rosAnnette
Balsi Childs
tinibh elessequat aute tat. Lorem
quate dolor
susci
exer ing exer
Stephanie
Renee
Clafferty
susto delisl ip eraese mod deliquam, R.
veratet
ueraestrud tat lutShelley
DeReu
patummy num qm ad magna
aliquiscilit
euis
nulluptat alit ver
Richard
Dane
Holt
ipit lorer sis nos nulla amconse
modolore
eugait aut lorperos ex
Joseph
W. Nussbaumer
eugiatum dignism odigniam zzrilit utpatem
volenim zzrilla faJacqueline
M. Santoro
cilit adigna alit dolut lore minibh
eu facin
utat, vel in ver il ip eu
Maude
Silver
faci bla feugiam, conse vulpute
modit velenit,
quam nit nim euRichard
Frank Tavolacci
gue corper sisi er sustrud dolore
min euisVoigt
nosto dolobore feum del
Stephen
delessenis nulla facipsustie magna
aliquat, E.
quatum
nullummy nulla
Andrew
McGovern
augiam volor seniamet nostrud
et veliquat.
John
O’RourkeVeliqua mcommy
nim iure eraesecte feugait volendreet laZeno
conse
minis non hendre
Rosael
Santi
te te et ipsum nis do ex esto commy nulputpatis
numsandit ad
Elnour
Elnaiem Dafeeah
et atetue dolutpatio eu feumsan
henim nummy
Edward
Murray numsandre feu
faccummodio exer sum dolorper
sequamcoreet
Corinne
Libby il ut vullamc ommoloborem zzriliquis euipis ad
dolobore modoles tisciduisl ex
ea faccumm odigna
John W. Blanks
Martin J. Collen
Rosalina Sedillo Cruz
Ellen L. Flaum
David D. Flemmer
James Lynn Greenstone
Geraldine M. Gregg
Edwin W. Gunberg
Jack Haberman
Mary Susan Harris
Suella N. Helmholz
Sallie A. Hunt
Caroline Janoka-Garner
Lee D. Kassan
Lynda J. Katz
Carol A. Kryder
Jo Taylor Marshall
Marilyn Meberg
Marlin S. Potash
New fellows
Kevin Robert Powser
Barbara Kittinger Acho
Thomas E. Resburg
Donald W. Alexander
Nicholas A. Roes
Nan Beth Alt
Harry A. Royson
Fall 2010 ANNALS 13
CE ARTICLE: 1 CE credit
Conscience-Sensitive
Psychiatry,
Clinical
Applications:
Retrieval and Incorporation
of Life-Affirming Values In
a Personalized Suicidality
Management Plan
Abstract:
The authors’ intent is to introduce three psychotherapeutic techniques that they have found useful in helping suicidal youths surmount suicidal urges and build
life-affirming values. Together, the techniques honor
the functioning of the patient’s conscience. The article
provides an overview of empirical research identifyBy Matthew R. Galvin, MD; Barbara M. Stilwell, MD; ing conscience domains and stages; description of
and Jerry Fletcher, MD and instructions for utilizing diagnostic/therapeutic
exercises; and a case presentation with discussion.
14 ANNALS Fall 2010
www.americanpsychotherapy.com
Acknowledgement: This article is adapted for continuing education, with permission from the editor, from articles (Galvin,
Fletcher, & Stilwell, 2005; Stilwell, Galvin,
& Gaffney, 2006) appearing in Conscience
Works, electronically published at http://
shaw.medlib.iupui.edu/conscience. The
first cited article was a companion piece
prepared in anticipation of the publication: “Assessing the Meaning of Suicidal
Risk Behavior in Adolescents: Three
Exercises for clinicians” (Galvin, Fletcher,
& Stilwell, 2006).
Defining Conscience
and Its Domains
In 1982, authors B.S. and M.G. began using a semi-structured interview to assess
personal understanding of conscience in
children and adolescents who were free
of psychopathology, learning difficulties,
or major trauma. No a priori hypotheses
were established. Grounded in clinical experience, the investigation was empirical
and exploratory. Questions were chosen
because they were intuitively relevant to
mental development, health, disease, and
morality. These questions now comprise the
Stilwell Conscience Interview (SCI; Stilwell,
2003). Research interviews of 125 children
and adolescents were collected, read, and
rationally analyzed. Five domains of conscience were identified, each one related to
the moral aspects of a different category
of human experience: attachment, emotion, cognition, volition, and meaningmaking. Conceptualization of conscience
was considered to be the anchor domain.
Contributory domains of conscience that
correlated with the anchor domain were
named: moralization of attachment, moralemotional responsiveness, moral valuation,
and moral volition.
Five stages were identified within each
domain for part of the life span, ages 5
through 17. Standard research methodology established inter-rater reliability
and construct validity for the domains
and stages. The results were published
one domain at a time (Stilwell & Galvin,
1985; Stilwell, Galvin, & Kopta, 1991;
Stilwell et al., 1994, 1996, 1997, 1998).
The following paragraphs review the five
domains, while Tables 1–5, found on
page 16, summarize the developmental
highlights of the domains within each of
the five stages.
(800) 592-1125
A General Definition
of Conscience
Metaphorically speaking, conscience is the
moral heart of the personality. How does
this heart come to be? Beginning with a
biologically prepared impulse to sort experiences into good and bad categories in
early childhood (Kagan, 1998), conscience
develops as an intra-psychic structure that
stores the “oughtness” messages from life’s
lessons about good and bad, right and
wrong. Within most individuals, understanding of goodness and badness, the objects of conscience, grows in increments
of organized meaning under the guidance
of moral nurturance, experience, and development. Goodness is first experienced
through the satisfaction of needs. Bedrock
values, the most basic forms to apprehend
goodness, are engendered in the process of
having needs both met and unmet. Thus,
an infant’s need for human attachment engenders a value for connectedness; the need
for emotional regulation engenders a value
for harmony; the need for goodness itself
engenders the logical structuring of valueladen experiences (value-sensitive rule making); the need to act and restrain engenders
the value of autonomous will; and the need
to coordinate experience into a meaningful
whole generates the synthesizing value of
moral meaning making. These bedrock values guide life’s first expectations and obligations. As domains of experience are further
moralized through nurturance, development, and the challenge of making moral
sense of life’s experiences, value-connected
expectations and obligations become increasingly differentiated and integrated.
Moralization of Attachment
The personhood of conscience evolves from
empathic responsiveness within parentchild dyads as mutual demands and expectations become connected to the desire to
please and to be pleased. As the child conforms to parental expectations (and the parent responds to the child’s needs), security
within the relationship is enhanced; nonconformity and unmet needs stress the relationship. The intimate association of secure
attachment and empathy with the experience that some things ought to be (or ought
not to be) becomes the interpersonal core
of the conscience mental representation.
We term this the security-empathy-oughtness
bond (Stilwell et al., 1997).
This article is approved by the following for continuing education credit:
The American Psychotherapy Association provides this
continuing education credit for Diplomates and certified members, who we recommend obtain 15 CEs per
year to maintain their status.
After studying this article, participants should be
better able to do the following:
1. Identify five domains of conscience
2. Identify five stages of conscience
3. Utilize a Suicide Narrative to help both patient and
therapist understand motivations and resistance
toward suicide
4. Utilize two conscience-sensitive exercises, not only
to build resistance to suicide, but to strengthen lifeaffirming values: a) the Moralized Genogram and b)
the Value Matrix
5. Help a patient construct a personalized Suicidality
Management Plan
KEY WORDS: Conscience, conscience-sensitive
interactions, life-affirming values,
Suicidality Management Plan
TARGET AUDIENCE: Mental health professionals
engaged in psychotherapy with suicidal youths
PROGRAM LEVEL: Intermediate
DISCLOSURES: The authors have nothing to disclose
PREREQUISITES: none
Moral-Emotional
Responsiveness
The emotional power of conscience evolves
as parental demands and expectations become values around which the child’s emotions are regulated (Stilwell et al., 1994).
The content of what it means to be good
(pleasing behaviors) takes form in relationship to feeling good (feeling pleased
or satisfied). An am good / feel good state of
moral-emotional equilibrium motivates
the developing child to inhibit prohibited
behaviors and to engage in pleasing, prosocial behaviors. Feelings of goodness or
badness are tied to the body’s physiological
processes, which, in turn, signal the person
when moral-emotional equilibrium is disturbed by behavior the individual deems to
be bad or wrong. Reparation and healing
processes (e.g. forgiveness) are then learned
and practiced to restore moral-emotional
equilibrium.
Moral Valuation
The value-processing power of conscience
is initiated when the child begins to use
cognitive skills to actively evaluate parental
demands and expectations in the face of her
own needs and desires. As the child moves
into the larger community, values governing
three types of relationships become important: values governing her relationship to
authority, values governing her relationship
Fall 2010 ANNALS 15
C l i n i c a l App l i c at i o n s
Table 1: The External Stage Conscience
Domains
External Stage (6 and under)
Moralization of Attachment
Parent-child empathic responsiveness generates bi-directional sense of “oughtness.”
Moral-emotional Responsiveness
Positive emotions become linked to sense of goodness.
Moral Valuation
Moral expectations emerge from daily routines.
Moral volition
Willpower is directed toward commitment to restraint.
Conceptualization
The conscience is perceived in terms of action scenarios with elders in which right and wrong behaviors are punished or praised.
Table 2: The Brain-Heart Stage Conscience
Domains
Brain-Heart Stage (7–11)
Moralization of Attachment
Disciplinary practices shape moral tone of parent-child relationship.
Moral-emotional Responsiveness
Anticipation of negative emotional response to wrongdoing emerges; rudimentary processes of reparation and healing emerge.
Moral Valuation
Some moral rules are constructed from consequential learning; others are internalized directly as mandates of elders.
Moral volition
Willpower is directed toward mastery of skills and demonstrating sufficiency in the pursuit of goodness.
Conceptualization
The conscience is perceived as a storage site for moral rules.
Table 3: The Personified Stage Conscience
Domains
Personified Stage (12–13)
Moralization of Attachment
An internalized and often “anthropomorphized” conscience supplements the moral authority of elders.
Moral-emotional Responsiveness
Initiative characterizes the pursuit of virtues and undertaking of reparative actions after wrongdoing.
Moral Valuation
Rules are interpreted in light of the dynamics of maintaining good relationships.
Moral volition
Willpower is directed toward the pursuit of specific virtues.
Conceptualization
The conscience is perceived as a “someone” for dialogue requarding moral issues.
Table 4: The Confused Stage Conscience
Domains
Confused Stage (14–15)
Moralization of Attachment
Independence from parental moral authority is facilitated by attraction to idols and ideals in the culture.
Moral-emotional Responsiveness
Emotional reactivity over conflicts of loyalty intensifies.
Moral Valuation
Conflicts over moral issues between self and authority, self and peers, and self with self prompt “weighty” moral processing.
Moral volition
Willpower is directed toward idealism.
Conceptualization
The conscience is perceived as struggling to integrate various sources of moral authority.
Table 5: The Integrating Stage Conscience
Domains
Integrating Stage (16+)
Moralization of Attachment
Image of becoming a moral authority for progeny emerges.
Moral-emotional Responsiveness
Emotional comfort with making individualized moral choices emerges.
Moral Valuation
Being true to oneself becomes a dominant value.
Moral volition
Willpower is directed toward “personal best” moral choices.
Conceptualization
The conscience is perceived as an entity that incorporates the concept of good within evil and evil within good.
16 ANNALS Fall 2010
www.americanpsychotherapy.com
C l i n i c a l App l i c at i o n s
to peers, and values governing obligations to
herself. It is within this valuational triangle
that moral dilemmas arise and must be resolved. All cognitive processes are activated:
language—how to frame moral choices and
challenges; memory—what precedents are
applicable; reasoning—what logic can be
applied; moral judgment—what cumulative
valuation will guide action. Uncertainty,
fallibility, and bad choices foster moral justifications—psychological defense mechanisms centered on moral issues. Through
the valuation process, the growing child
gradually learns about moral complexity
(Stilwell et al., 1996).
Moral Volition
The willpower of conscience evolves as the
child’s capacity for action and restraint, attention, and effort are moralized in the process of exercising autonomous will (Stilwell
et al., 1998). Living involves both willed
and unwilled behavior. Evolutionarily prepared dual abilities to act before thinking
and think before acting (LeDoux, 1996;
Libet, Freeman, & Sutherland, 1999) lead
to behaviors as diverse as life-saving actions or impulsive, self-defeating ones.
Even when humans think before acting,
pre-conscious factors—biological drives,
emotional arousal, relationship loyalties—
may combine with situational cues and demands to mar or enhance moral choice. As
the child grows in ability to use consequential feedback and deliberate self-assessment,
she grows in ability to be in charge of her
moral actions.
Conceptualization of
Conscience
The power of conscience as a whole evolves
as the child synthesizes moral meaning from
the domains of moral attachment, moralemotional responsiveness, moral valuation,
and moral volition. Conscience is the moral
organizer in each person’s autobiographical
journey, a moral governor at the heart of
the personality. Children have great facility
to both draw and define their conscience
when the language of inquiry is adjusted
to their cognitive abilities. Five discrete
stages of synthesis can be identified before
age 18 (Stilwell & Galvin, 1985; Stilwell
et al., 1991).
Case Illustration: Regina
In accordance with HIPAA regulations,
all identifying information, including the
location of the subject of this report and
(800) 592-1125
dates of admission to other facilities, has
been expunged from the record. To ensure
fidelity to the case, all dates will be indicated in reference to the date of the admission; for example, “one week prior to admission (PTA).”
Twelve-year-old Regina presented to the
emergency room in her local hospital after
her school counselor discovered a suicide
note in her binder. Upon her arrival at the
access center to the psychiatric hospital
about 50 miles away, Regina told how she
had composed the note while frustrated
about her homework and upset about an
episode of her stepfather’s anger dyscontrol.
When a child’s basic
needs are poorly met in
the areas of attachment
and emotion and when
she is confused by the
values of mistreating
adults and helpless to
take action, her own
conscience can become
severely distressed,
resulting in “demoralization” and loss
of life-affirming values.
She denied any intent to commit suicide,
and there was no history of previous suicide
attempts. However, her mother indicated
that Regina had talked about suicide during the eight months PTA. She was subject
to reduced total sleep time but denied difficulties in concentration and experienced
no diminution in appetite. She had briefly
engaged in treatment at a community mental health center for “depression and behavior.” No medications were prescribed. Her
personal history was negative for alcohol
and substance abuse. She denied any current or past sexual activity. She initially de-
nied any maltreatment experiences in the
form of physical abuse, sexual abuse, and
neglect, but did indicate exposure to domestic violence. The mental status examination conducted by the access center worker
described her as disheveled, with holes in
the elbows of her knitted shirt, tearful in
presentation, avoidant of eye contact, withdrawn, and depressed in mood. The case
was staffed by telephone. Regina was admitted by the child adolescent psychiatrist
on call. Suicide precautions were ordered.
The first clinical encounter with her assigned psychiatrist occurred the next morning. Regina was highly distressed about
remaining in the hospital. She urgently repeated several times that she did not mean
to write the suicide note. She spontaneously denied any intention of ever making
herself die. Regina became more communicative through her tears, which she ascribed to being away from “my Mommy”
for the first time. Her separation anxiety
was probably compounded by having to
undergo treatment for head lice, including temporary isolation.
The psychiatrist’s evaluation mostly confirmed the findings of the access center
worker in the mental status domains of appearance, attitude and behavior, affect and
mood, sensorium as well as judgment and
insight. In contrast, while Regina’s responses
to questions posed in the psychiatric evaluation were pertinent, they were also concrete. Her use of vocabulary and grammatical structures indicated a less-than-average
intellectual functioning and/or the presence
of specific learning disabilities.
When a child’s basic needs are poorly
met in the areas of attachment and emotion, and when she is confused by the
values of mistreating adults and is helpless to take action, her own conscience
can become severely distressed, resulting in “de-moralization” and loss of lifeaffirming values. Accordingly, Regina’s
psychiatric evaluation was conducted in
a manner sensitive to conscience functioning, via innovations that conform
to the American Academy of Child and
Adolescent Psychiatry (AACAP) Practice
Parameters for the Psychiatric Assessment of
Children and Adolescents (AACAP, 1997),
namely: (a) adapting for clinical use core
questions first developed in research and
(b) utilizing interview techniques designed
to elicit information about conscience
functioning with respect to presenting
problems (Stilwell et al., 2006).
Fall 2010 ANNALS 17
C l i n i c a l App l i c at i o n s
5
5
Legend
Legend
19
19
when she was 3 years old, three of her brothers
were removed from the home in a Western state
and each spent time in juvenile detention prior
Residing in Regina’s home
Residing in Regina’s home
Regina’s Conscience
The initial conscience inquiry was adapted
from the SCI (freely available at Conscience
Works). Conscience Conceptualization: Regina
indicated she was sometimes aware of a part
of herself that helped her figure out right
versus wrong. She described this part of
herself as quite active. Moral Emotional
Responsiveness: Regina indicated she generally
experienced herself as a good person. When
engaged in what she considered to be rightdoing or good deeds, she said she was apt to
become excited but did not somatically localize the corresponding feelings or sensations
(as many persons do). In response to what
she considered to be engagement in wrongdoing, she said she was apt to feel both sad
and mad. She did not discern an appreciable
change in her moral emotional responses if
either her right-doing or her wrongdoing
remained unknown to others, although she
18 ANNALS Fall 2010
9
9
among Regina’s full sibship. Regina reported that
Bipolar Disorder, NOS
Bipolar Disorder, NOS
Moral Attachment Figure
Moral Attachment Figure
16
16
Regina’s mother identified only the nine year old
Perpetrator Child Sexual Abuse
Perpetrator Child Sexual Abuse
Relationship with positive valence
Relationship with positive valence
17
17
12
12
Alcohol, substances, violence
Alcohol, substances, violence
Relationship with negative valence
Relationship with negative valence
18
18
to placement because of threats they made to
kill their mother.
Figure 1: Regina’s MORALIZED GENOGRAM
conveyed that she would “tell on herself” in
any case. Moralized Attachment: She identified her mother and her maternal grandmother as those persons who cared most
whether she led a good life and did the right
things (i.e. principal moral attachment figures). Moral Valuation: Whereas most children identify several “rules of conscience,”
Regina identified only one: “Don’t drink
alcohol and stuff.” Moral Volition: Initially,
Regina found it difficult to discuss any successful experiences she had had in either resisting urges to engage in wrongdoing or
overcoming her resistance to engagement
in right-doing.
She acknowledged the internalization of a
moral presence; described that her emotions
rose and fell in response to pleasing or failing to please that presence (as well as people outside of herself ); identified one “rule
of conscience”; and was uncertain about
having any moral willpower. Evaluating
Regina’s responses to a conscience-sensitive
inquiry in the light of Tables 1–5, we would
judge that her conscience development has
barely reached Stage II.
Regina’s case was chosen for this very reason: to illustrate the approximate minimal,
rather than optimal, characteristics needed
for a patient to be engaged in the diagnostic/therapeutic exercises we refer to as conscience-sensitive interactions.
These conscience-sensitive interactions
have been used with older school-age children and adolescents, both male and female, with intellectual capacities low average or better in settings such as acute
inpatient, intensive outpatient, and outpatient. Aside from age and intellectual capacity, consideration of stage of conscience
development is important. Considerations
of a person’s stage of conscience development and particular strengths and weaknesses in conscience functioning lay the
foundation for conscience-sensitive interactions. With rare exception, initial conscience inquiries adapted from the SCI are
used as part of psychiatric evaluation in
the first author’s practice (which includes
frequent work with developmentally disabled youth). However, we have learned
from experience that a person must have
www.americanpsychotherapy.com
C l i n i c a l App l i c at i o n s
achieved at least Stage II in a conscience
evaluation to benefit from the therapeutic procedures that follow. Different techniques are necessary for individuals with
less than Stage II development.
With the initial conscience inquiry, a
question emerges. Is the person primarily
delayed in conscience development, or has
the person temporarily lost her purchase
and slipped on this particular developmental trajectory by becoming de-moralized in
one or more conscience domains? Answers
to questions of this sort will make a difference in terms of the therapeutic project. If
primarily delay is discerned, then the therapist, the treatment team, and responsible
family members may be obliged to provide
“scaffolding” to support the person of conscience until she can advance to the next developmental stage. If a primary condition of
de-moralization is discerned, support is more
likely to be directed to dealing with pathological interferences, which stand in the way
of re-moralization, and more firmly securing
prior developmental accomplishments.
Regina’s Case Continued:
Conscience Sensitive
Interactions —The
Moralized Genogram
In subsequent sessions with her psychiatrist,
Regina was able to elaborate on the nature
of the domestic violence to which she had
been exposed and that fueled her worries
of harm befalling her mother while absent.
She also disclosed having experienced direct
physical abuse in the form of being choked
by her stepfather during a period of intoxication. In a later session, she was engaged
in constructing a Moralized Genogram
(see Figure 1).
The project of the genogram is mutually
undertaken by the therapist and patient.
The therapist teaches the symbols for the
genogram, depicting biological connections
in black and emotional connections and
disconnections in red. Moralized attachments and detachments are layered upon
the more familiar biological and emotional
connections/disconnections by filling in or
circling the symbols with green.
While constructing the Moralized
Genogram, Regina echoed family psychiatric history her mother had provided independently at admission: her mother, her
maternal grandmother, and her sibling (also
diagnosed with ADHD) being subject to bipolar disorder, not otherwise specified. She
conveyed her impression that her biological
(800) 592-1125
father had, like her stepfather, been subject
to alcoholism and was prone to violence. She
knew of a paternal uncle who had been subject to substance abuse and was incarcerated
for child molestation. She identified family
members her mother had not: three brothers, placed with another family out of state,
each in later adolescence and each having
spent time in corrections for threatening the
mother. She also provided the additional history that she had been taken from her mother at age 6 for three months due to neglect.
Those persons represented as caring about
her moral well-being were her mother, both
maternal grandparents, and a 19-year-old
brother living outside the home. She represented a highly conflicted relationship with
her stepfather and expressed the wish that
her mother would not be so afraid of him so
she could compel him to leave their home.
In Regina’s case, the Moralized Genogram
opened up much more psychosocial information and abuse history. The straight and
jagged lines depicting emotional connections and disconnections improved mutual
understanding of her suicidal motivation.
In the depiction, maintaining emotional
connectedness with her mother emerged as
a powerful motivator for Regina, possessing
life-sustaining value. The colorful marking
of principal moral attachment figures was
the first glimmer that the life-affirming value moral connectedness might also operate as
a motivator in her life. This information,
made visible by depiction, set the stage for
strengthening Regina’s consequential thinking in light of her values. The psychiatrist
was prepared to cautiously introduce the
next conscience-sensitive interaction and
accompany Regina on her Suicide Walk.
The Suicide Walk
Regina was asked to conduct herself through
a Suicide Walk. This clinical device was introduced to youth psychiatric inpatients
about 15 years ago by author J.F. The instruction given to the patient is:
Write a story in first person as if you
actually killed yourself. Write about
what led up to your suicide, how you
felt, why you did it, and how you did
it. Write about your funeral, who is
there, what they are saying, and what
they are feeling. Write about how your
suicide affects your family and friends
and how they feel. Then write about
life afterwards for your family and
friends. (This assignment may take
several pages to write.)
This was Regina’s written response, which
was completed on hospital day #2:
I led up was very frusted one day
I a enough I felt like killing myself.
I got on the bus. Then after I did I got
off at my bustop. I walking to home from
my bustop and there was a car going
really fast. I ranned out in front of it.
The next day they had my funrel going on. A lot of people was there like my
mom, brother, sister, grandmal, grandpal, freinds. I don’t know exaltey they
were saying. But all I could hear how my
sayed I wish hadn’t done that. My family
was destroyed. My friend was destroyed.
My family hearts was broke. My friends
hearts were broke too. That’s my story.
In this manner,
the patient develops
an appreciation of how
biological conditions
can affect her as a
person of conscience.
The assignment of this therapeutic task
may elicit resistance from many patients. In
some cases the resistance arises in patients
who, after the rigors of medical stabilization in the emergency room, exposure to
distress among family members, and acute
psychiatric hospitalization, have enjoyed a
“flight into mental health” and insist that
the suicidal behavior was anomalous, guaranteed never to occur again. In other cases, resistance issues from the extremes of
de-moralization. In still other cases, the
exercise may be undertaken with an excess of enthusiasm for an opportunity to
demonstrate a flair for the dramatic or to
engage in compensatory grandiosity. From
the standpoint of the therapist, it enriches
psychodynamic understanding of the patient and provides a view on the nature of
the patient’s suicide planning and deliberation, or lack thereof. Once undertaken, it
often assists the patient in recapitulating her
state of mind that resulted in suicidality. It
prompts, with varying degrees of success,
self-examination resulting in clearer identification of the strongest suicidal motives.
It prompts consequential thinking. It also
Fall 2010 ANNALS 19
C l i n i c a l App l i c at i o n s
becomes the springboard for an exercise in
moral imagination.
In the next clinical encounter with her
psychiatrist, Regina was instructed to read
aloud her Suicide Walk. As is often the
case with patients, she attempted to avoid
the reading by handing over her narrative.
Upon redirection, she began to read aloud
but at a rapid pace. She was instructed to
begin again and slow down. The rationale
shared with her was to have her listen carefully, together with her psychiatrist, to what
she was reading. As a practical matter, the
read-through also clarified what the patient
attempted to communicate in writing but
was hindered because of her grammatical
and spelling weaknesses. At the conclusion
of the read-through, the inquiry was made
to her: “How do you react to what you’ve
written and read just now?”
Regina’s Case Continued
At the point of admission, Regina had indicated the strongest suicidal motive she
would ever experience would be the loss of
her mother. She had been unable to adduce
any life-affirming or even a life-sustaining
value. After therapeutic work in the form of
the Suicide Walk and Moralized Genogram,
she was able to retrieve connectedness as a
life-sustaining value. However, her connectedness was not yet fully moralized; indeed, she primarily evinced fear of separation: “I would be away from my Mommy
if I killed myself.”
Fears that counteract suicidality may take
other forms. Fear of pain or of the process
of dying or of eternal punishment in accordance with religious beliefs will sometimes
be adduced. In such cases, we recommend
exploring further. To conduct the exploration, another conscience-sensitive clinical
device may be employed.
The Value Matrix
The foursquare organizational schema (see
Figure 2) is the graphic outcome of a dynamic process in which the therapist facilitates the patient’s self-examination of
the valuational contents embedded in her
conscience. We will first provide an operational description of the value matrix. Then
a dialogue distilled from many clinical encounters will be provided before describing
the outcome with Regina.
Operationally defined, for any x, the inquiry takes the form: “If you (a person)
went along with x, it would be because
——— (fill in the blank).”
The form in which x is put is a matter
for the therapist’s discernment. The therapist may discern that the patient continues to harbor suicidality and so x may be
given forms like “DO make myself die”
or “DO allow myself to die.” Either form
is treated as an urgent demand to which
the patient is asked to make attributions:
becauses both pro- (to abide the urge) and
con- (to resist the urge). Alternatively, the
therapist may discern that the patient is
denying suicidality without a genuine repudiation of it (as in a “flight into health”)
or is having heightened experiences of remorse, which nonetheless threaten to deteriorate into self-loathing or a self-defeating attitude. In such cases—Regina’s was
one—x may be put in the form “DON’T
make myself die.”
The therapist notes the patient’s initial because as a starting point for the dialogue but then stretches the patient’s moral
imagination by hypothetically blocking the
motivational power of whatever was put in
the blank in order to elicit another because.
The role of the therapist is to allow other
becauses, both pro- and con-, to emerge. This
may turn out to be an iterative process.
“Do engage in acts harmful to one’s self.”
Abide
Best Reasons
Base Motives
Figure 2: The Value Matrix
20 ANNALS Fall 2010
Ignore
The following dialogue, distilled from
many clinical encounters, is presented in
its bare-bone essentials. In an actual clinical
encounter, neither the opportunity for empathic responsiveness nor for respecting the
person of conscience should be ignored. We
hope the therapist will be engaged in a manner that is ever-mindful of the pain probing
produces and the individual’s tolerance.
Example:
THERAPIST: How do you fill in the
blank: “I will not make myself die because ———”?
PATIENT: Because I don’t want to experience the pain.
THERAPIST: (hypothetically blocks
the motivational power of the original
because by saying): What if you could
be very sure you would not endure any
pain, then what would be your next because not to make yourself die?
PATIENT: I don’t know. I’m worried
about being condemned to hell for
taking my own life. I heard a minister
tell me that suicide is the only unforgivable sin.
THERAPIST (hypothetically blocks
the motivational power of this because
by saying): What if you were very sure
of God’s forgiveness, what would be
your because then?
PATIENT: Because it would hurt my
mother terribly—for all the rest of
her life.
Patient and therapist then proceed to
sort through these becauses according to
which the patient deems best and worst.
This yields a division into best reasons
(or values) and basic (or base) motives.
The patient is next asked to gauge the relative strength (and personal applicability) of
each because. In so doing, the patient may
become keenly aware of a value-motive gap
in her conscience functioning. For example,
she discovers she deems not causing harm
to loved ones among her best becauses, but
she still considers fear of punishment to be
the strongest. Awareness of a value–motive
gap may occasion further insight: “Why are
my best becauses not also my strongest?”
Indeed, the therapist may respond in kind:
“Our best becauses sometimes seem pretty
weak next to other becauses we have. What
makes them weak and how can we make
them stronger?”
www.americanpsychotherapy.com
C l i n i c a l App l i c at i o n s
LIFE
AFFIRMING
VALUES
COPING
SKILLS
SUICIDAL
IDEATION
SURVIVAL
STRATEGY
SUICIDAL
IDEATION
COPING
SKILLS
SUICIDAL
URGES
SUICIDAL
URGES
STRESSORS
SUICIDAL
ATTEMPTS
SECURE
BASE
SUICIDAL
ATTEMPTS
SECURE
BASE
EMERGENCY
INTERVENTIONS
EMERGENCY
INTERVENTIONS
Figure 3: The Suicidality Cycle
Figure 4: The Suicidality Management Plan
Regina’s Retrieval of a
Life-Affirming Value
The Value Matrix had limited utility in
Regina’s case. It nonetheless allowed her to
make explicit a new because:
“…because I don’t want to hurt my
Mommy.”
Following this conscience-sensitive interaction, not only could Regina recognize
that her suicide would cause harm to loved
ones, but also she could affirm that she did
not want to cause such harm. Do no harm
(non-maleficence) within the circle of family and friends is commonly adduced as the
life-affirming value when there is an exploration of the best reasons to resist suicidal
urges. Regina’s because could accurately be
called “non-maleficence within the context
of her relationship with her mother.”
Regina recognized her because “I don’t
want to hurt my Mommy” as better than—
but still not as strong as—her because “I
would be away from my Mommy if I killed
myself.” Her recognition did not occasion
further reflection. There could not be the ensuing conversation, “Our best becauses sometimes seem pretty weak next to other becauses we have. What makes them weak and
how can we make them stronger?” Hence,
Regina’s case demonstrated a limitation.
Even so, it is sometimes helpful, as was
done in the case of Regina, to let the patient
know that “first do no harm” represents a value shared by both therapist and patient. Both
therapist and patient can then appreciate
their encounter as persons of conscience.
(800) 592-1125
STRESSORS
Risk Assessment and
Self-assessment of Risk
Engagement in the healing process may
actually begin with the patient’s acknowledgement that his motivation to allow himself to die or put himself in harm’s way is
nothing like what he regards as a best reason. His acknowledgment may be coupled
with his awareness, now explicit, that his
reasons to stay alive are better but weaker
when compared to his motives to end his
life. Occasionally, in cases where x is permitted to take the form “DO allow myself to
die,” patients will arrive at the conclusion
the very best reasons for allowing oneself
to die would not be from egoistic motives
(such as escape from personal misery) at
all. Rather, they have stretched their moral
imagination and conceived of circumstances
in which heroic self-sacrifice might be required to save another’s life, such as in the
case of a first-response rescue worker. By
an additional stretch of moral imagination,
such patients might concede to themselves
that there are less dramatic forms of altruism available to them (for example, in a future role as parents) in which self-sacrifice
serves to sustain others’ lives or promote
others’ flourishing. A new perspective begins to emerge: “My life may be mine to
give but is not mine to take.” In the acute
psychiatric hospital setting, status postsuicide attempt, the failure of a patient to
adduce any relatively robust life-affirming
(or at least life-sustaining) values ought to
be considered evidence that continued sui-
cide precautions, hence a continued hospital stay, might be warranted in spite of the
patient’s denial of current suicidal ideation
and absence of suicidal behavior.
Suicidality Management Plan
By her third day in the hospital, Regina had
been given two doses of antidepressant medication. She had also been at work on the
therapeutic task assigned to her by her psychiatrist: personalizing a conscience-sensitive
Suicidality Management Plan.
We have found that it is best to construct
the figure on a blank page or dry erase board
anew for each patient rather than using a
preprinted diagram. The patient is asked
about her sense of safety. The patient is
asked, “What makes you safe here and now?”
The usual response conveys the information
that the staff has been keeping an eye on her
“24/7.” Sometimes a sense of safety eludes
the patient and can be addressed accordingly.
“A Safe Place” (alternatively, “A Secure Base”)
is designated on the page or board. Having
acknowledged being in a safe place, the patient is asked about what has been given up
for the sake of safety. A patient who demurs
from answering may be surprised that the
therapist acknowledges with regret the various signs of lost autonomy the patient has
endured: the locked unit, the prohibition
of shoes (to make it harder to escape). The
therapist makes explicit that in the desired
outcome of hospitalization, the patient will
internalize what safeguards are needed in
order to move from the safe place provided
Fall 2010 ANNALS 21
C l i n i c a l App l i c at i o n s
by staff in the hospital to a “better place,”
outside the hospital, in which freedoms will
gradually be acquired in accordance with
demonstrated responsible behaviors. A trajectory is traced aiming at the “better place”
(somewhere off the page or board, which
the patient is invited to describe in terms of
lifelong goals). The therapist then depicts
a diversion off course—a derailment—attributable to stressors (Figure 3). There follows a depiction: how persons may effect a
turnaround and right their course, restoring themselves to their original trajectory by
practicing coping skills to deal with the stressors. At this juncture, actual and potential
barriers to effecting the turnaround need to
be acknowledged, even if their full explanation is deferred. Thwarted by barriers to using coping skills, the patient moves further
along a trajectory toward harm. The patient
arrives at suicidal ideation, which is encouraged to assume definite form. For example,
“I tell myself I don’t deserve to live.” This expression of de-moralization is depicted as another opportunity for turnaround (Figure 4):
counteracting the de-moralized self-talk with
retrieval of life-affirming values (made explicit via work on the Moralized Genogram
and Value Matrix). These are then depicted
as sometimes having motivational power sufficient to overcome the barriers to using or
acquiring coping skills. However, actual or
possible barriers to the second turnaround
also must be acknowledged.
About the Barriers
The patient may cite impoverished coping
skills or overwhelming stressors as the barriers. The barriers may also be pathological
interference with exercising choices to use
or acquire new coping skills (moral volition)
and with retrieval of life-affirming values
(moral valuation). Whichever psychobiological conditions affect the patient (such
as depression, post-traumatic stress disorder, and/or substance abuse), if not already
nominated by the patient, can be made explicit by the therapist as impediments. In
this manner, the patient develops an appreciation of how biological conditions can affect her as a person of conscience.
The third depicted turnaround is at the
juncture when the patient recognizes the
disposition or urge to harm cannot be resisted without seeking help from others
(Figure 4). Resort is made to a survival
strategy to find support against the disposition or urge to harm or destroy oneself.
The overall plan is personalized by identify22 ANNALS Fall 2010
ing at least three anticipated stressors, three
coping skills, three life-affirming values,
and a survival strategy in clearly identifying three persons from whom she will seek
help should she experience overpowering
suicidal urges in future.
In her words (italicized), Regina identified
her stressors as: 1) math, 2) violce (violence),
and 3) step-father. She identified coping skills
she could use to turn around as: 1) listen to
mellow music, 2) color, 3) read a book, and 4)
talk to a family member. She identified her
reasons to stay alive (life-affirming values) as:
1) family, 2) friends, and 3) my mommy. She
recognized that something more might be
needed if she could not turn around and her
de-moralization disposed her to self-harm.
She sketched a survival strategy, in which
she wrote down: 1) therpest (therapist), doctor, and (school) couselor (counselor).
The patient presents her plan to her principal attachment figures. The therapist occupies the role of helping all concerned to
discern the genuineness of the effort and
whether the plan will be serviceable.
In summary, understanding domains
and stages of conscience development
can be very helpful in the treatment of
a suicidal youth. Conscience functioning in a suicidal youth may have become
de-moralized through inadequate psychological nurturing, trauma, loss, biological
insult, substance abuse, or other adversity.
After an initial inquiry about the patient’s
understanding and experience of her conscience and its various domains, three other
diagnostic/therapeutic exercises may be utilized to understand the patient’s therapeutic
needs. The Moralized Genogram reveals the
quality of moral nurturing the patient has
received from family members. The Suicide
Walk reveals the impact the patient believes
he would have on his personal world after
death. The Value Matrix reveals the patient’s
life-destroying but also life-affirming becauses.
When used with sensitivity and respect, these
procedures can help patient and therapist
construct a Suicidality Management Plan.
Limitations
What has been described here are ways of
engaging in conscience-sensitive interactions in the context of suicidality. The ways
we have described are clinical applications
based upon empirical research. Our global
impression is that they have often been helpful, but we have not systematically collected
and quantified empirical evidence for their
efficacy. We have, however, compiled qual-
itative data on psycho-educational group
therapy organized in modules based on the
Domains of Conscience (Galvin, Gaffney,
& Stilwell, 2005). The data compiled has
relevance to the clinical applications described in this paper, further characterizing
the experiences which support our global
impression. Both the Moralized Genogram
and the Value Matrix (but not the Suicide
Walk, deemed more appropriate for individual work) were incorporated in the modules. The therapeutic settings ranged from a
child and adolescent psychiatry outpatient
clinic to a youth residential home and included adolescent psychiatric intensive outpatient and partial hospitalization programs.
Participants were male and female. The
number of participants in any module varied
from one in the outpatient setting to 15 in
the intensive outpatient setting. Age of participants varied from school age to late adolescent. Formal intellectual testing was not
uniformly available for participants. Most,
however, appeared to be average intellectually. Each participant had, at minimum, an
initial assessment by a mental health clinician yielding a DSM IV multi-axial psychiatric diagnosis. No restrictions were placed
upon participants in terms of principal or
secondary diagnoses or severity of impairment, although all had sufficiently severe impairment to be deemed in need of the aforementioned current and standard psychiatric
or psychosocial interventions. Length of
time for each of the seven modules was permitted to vary according to the stability of
the participant population. Individual modules conducted in the adolescent psychiatric
intensive outpatient program were limited
to one hour each, whereas some modules
conducted in the residential and youth day
school settings extended over several sessions
held once weekly. Seven modules were eventually developed and refined to comprise
a full course of conscience-sensitive group
therapy. In the last two years, in the residential setting, an eighth module has been
added in which group participants have
presented personalized De-moralization (or
Harm) Prevention Plans (comparable to the
Suicidality Management Plan). We would
wholeheartedly agree with those who believe
our conscience-sensitive approaches require
further study in terms of efficacy, safety, and
limitations, particularly those based upon
age and intellectual capacity.
Until such study can be done, we speculate
the techniques we have described will be of
most use with demoralized persons of conwww.americanpsychotherapy.com
C l i n i c a l App l i c at i o n s
science who have attained at least Stage II in
conceptualization of conscience. Without significant adaptations, we suspect the interventions will not be as useful at stages less mature.
While unaware of any completed suicides
among those we have engaged in conscience
sensitive treatment, we are aware of some suicidal persons who had been non-adherent to
the Suicidality Management Plans they developed and made subsequent attempts. In at
least some of those cases, persons were able to
utilize their original Suicidality Management
Plan to critically examine what went awry and
to make refinements.
To some colleagues, conscience sensitivity may appear a novel approach to both
diagnosis and treatment, while others may
recognize procedures, implicit or explicit,
in their own diagnostic and therapeutic
projects. Among the many healing values
embraced by the healing professional, compassion and empathic responsiveness are
preeminent. However, so is respect for the
person of conscience who encounters varying life circumstances with varying capacities and abilities: to value, to judge among
values and motives in terms of their relative
strength and goodness, to make choices, and
to manage moral emotional responses. The
recognition that there are adverse conditions, notably biological ones, that constrain
and diminish these capacities and abilities
seems to us an expression of compassionate
attitude. The recognition that the person of
conscience in such conditions may require
help overcoming obstacles to retrieve values
in a structured interaction adds respect to
compassion in the expression of a caring attitude. We hope others in our healing professions will contribute their insights and
ideas about best practices in consciencesensitive approaches to those they serve.
References
American Academy of Child and Adolescent Psychiatry
Practice Parameters (1997). Practice parameters for
the psychiatric assessment of children and adolescents. Journal of the American Academy of Child and
Adolescent Psychiatry, 36(10 supplement), 4S-20S.
Galvin, M., Stilwell, B., Adinamis, A., & Kohn, A.
(2001). Conscience sensitive diagnosis of maltreated
children and adolescents. Conscience Works: Theory,
Research and Clinical Applications, 1(1), 1-81. Electronically published at http://shaw.medlib.iupui.
edu/conscience
Galvin, M., Fletcher, J., & Stilwell, B. (2005). Conscience sensitive psychiatry: clinical applications:
retrieval of life affirming values and their incorporation into a suicidality prevention plan. Conscience
Works: Theory, Research and Clinical Applications,
1(2), 1-9. Electronically published at http://shaw.
medlib.iupui.edu/conscience
Galvin, M., Gaffney, M., & Stilwell, B. (2005): Pre-
(800) 592-1125
liminary observations and reflections on conscience
sensitive group therapy. In Conscience Works, an Online Periodical, Theory, Research and Clinical Application, 2(2), 1-23. Electronically published at http://
shaw.medlib.iupui.edu/conscience/
Galvin, M., Fletcher. J., & Stilwell, B. (2006). Assessing the meaning of suicidal risk behavior in adolescents: three exercises for clinicians. Journal of the
American Academy of Child and Adolescent Psychiatry, 45(6), 745-748.
Kagan, J. (1998). Three seductive ideas. Cambridge,
MA: Harvard University Press.
LeDoux, J. (1996). The emotional brain: the mysterious underpinnings of emotional life. New York: Simon & Schuster.
Libet, B., Freeman, A., & Sutherland, K. (1999). The
volitional brain: towards a neuroscience of free will.
UK & USA: Imprint Academic.
Stilwell, B. (2003). Trauma, moral development, and
conscience functioning. Conscience Works: Theory,
Research and Clinical Applications, 2(1): Appendix
A. Electronically published at http://shaw.medlib.
iupui.edu/conscience
Stilwell, B., & Galvin, M. (1985). Conceptualization of
conscience in 11–12-year-olds. Journal of the American Academy of Child Psychiatry, 24, 630-636.
Stilwell, B., Galvin, M., & Kopta, M. (1991). Conceptualization of conscience in normal children
and adolescents ages 5 to 17. Journal of the American Academy of Child and Adolescent Psychiatry,
30, 16-21.
Stilwell, B., Galvin, M., Kopta, M., & Norton, J.
(1994). Moral emotional responsiveness: two domains of conscience functioning. Journal of the
American Academy of Child and Adolescent Psychiatry, 33(1), 130-139.
Stilwell, B., Galvin, M., Kopta, S., & Padjett, R.
(1996). Moral valuation: a third domain of conscience functioning. Journal of the American Academy
of Child and Adolescent Psychiatry, 35(2): 230-239.
Stilwell, B., Galvin, M., Kopta, M., Padgett, R., &
Holt, J. (1997). Moralization of attachment: a
fourth domain of conscience functioning. Journal
of the American Academy of Child and Adolescent
Psychiatry, 36(8): 1140-1147.
Stilwell, B., Galvin, M., Kopta M., & Padgett, R.
(1998). Moral volition: the fifth and final domain
leading to an integrated theory of conscience understanding. Journal of the American Academy of Child
and Adolescent Psychiatry, 37(2): 202-210.
Stilwell, B., Galvin, M., & Gaffney, M. (2006). Progress in conscience sensitive psychiatry: assessment,
diagnosis and treatment planning. Conscience
Works: Theory, Research and Clinical Applications,
2(1), 5-30. Electronically published at http://shaw.
medlib.iupui.edu/conscience
Earn CE Credit
To earn CE credit, complete the exam for this
article on page 80 or complete the exam online
at www.americanpsychotherapy.com
(select “Online CE”).
About the Authors
Matthew (Matt) Galvin, MD, is a child psychiatrist. He was
introduced to the health professions in 1970 while in the U.S. Army
Medical Corps. On faculty at Indiana University School of Medicine
1984-1998, he engaged in research with Barbara Stilwell and has
since remained a voluntary clinical associate professor. With his wife,
Meg Gaffney, he teaches conscience-sensitive approaches to bioethical decision making and professionalism. Matt and Meg have three
adult children: Joseph, Erin and Sarah. Matt has contributed to several
books on conscience for young persons, donated to the IU Conscience
Project. These appear on Conscience Works: http://shaw.medlib.iupui.
edu/conscience/
Barbara Stilwell, MD, is retired from clinical practice and
teaches Introduction to Clinical Medicine to first-year medical students along with her husband, Dr. Ray Dunkin, at Indiana University
School of Medicine. She also volunteers in a local public school where
her grandson attends. She and her husband enjoy ballroom dancing
and traveling with their grandchildren.
Jerry Fletcher, MD, is a board-certified child and adolescent
psychiatrist and has been doing inpatient and outpatient care with
children for more than 25 years. He graduated from the University of
Nebraska and Indiana University School of Medicine. He is the director
of behavioral science with the primary care residencies at St. Vincent
Hospital in Indianapolis and Owns Meridian Youth Psychiatric Center.
His wife is Maria V. Fletcher, MD, the primary care doctor for Butler
University.
Fall 2010 ANNALS 23
Therapy Technique
Cognitive
Processing
Therapy for PTSD
By Tanja Kern
hile more than 90,000 U.S. troops have left Iraq over the
past 18 months—and the Obama Administration says troops
are to be out by the end of 2011—many members of the military will come home with a lingering problem: post-traumatic
stress disorder. Not only is war difficult for the soldier, it is
incredibly difficult for the soldier’s family, and the impact of
PTSD can have a profound effect on everyone.
24 ANNALS Fall 2010
www.americanpsychotherapy.com
According to the National Center for
PTSD, the disorder occurs in:
• About 30% of Vietnam veterans.
• As many as 10% of Gulf War (Desert
Storm) veterans.
• About 6% to 11% of veterans of the
Afghanistan war (Operation Enduring
Freedom).
• About 12% to 20% of veterans of the
Iraq war (Operation Iraqi Freedom).
There are a number of factors that contribute to PTSD and other mental health
problems: the military member’s job in the
war, the politics around the war, where it is
fought, and the type of enemy they faced.
Another cause of PTSD in the military can
be military sexual trauma (MST), which includes any sexual harassment or sexual assault that happens to service members while
they are in the military. MST can happen
to men and women and can occur during
peacetime, training, or war.
Among veterans using VA health care,
about 23 out of 100 women reported sexual
assault while in the military, and 55 out of
100 women and 38 out of 100 men have
experienced sexual harassment when in the
military. Although military sexual trauma
is far more common in women, over half
of all veterans with MST are men.
Thankfully, there are several forms of
therapy that can be used to treat PTSD.
The most common are exposure therapy,
cognitive therapy, eye movement desensitization and reprocessing (EMDR), and
cognitive behavior therapy. There is a wide
body of research over the past 10 years
showing that cognitive processing therapy
(CPT) helps anxiety disorders like PTSD.
In fact, many researchers have indicated
that CPT is the most trusted therapy for
the successful treatment of anxiety.
CPT was developed by Patricia A. Resick,
PhD and Monika Schnicke, MA, specifically to treat PTSD in people who have experienced a sexual assault. It is considered a
blend of cognitive and exposure therapies.
CPT is like cognitive therapy in that it is
based upon the idea that PTSD symptoms
stem from a conflict between pre-trauma
beliefs about the self and world (for example, the belief that “nothing bad will happen
to me”) and post-trauma information (for
example, the trauma as evidence that “the
world is not a safe place”). These conflicts
are called “stuck points” and are addressed
through writing about the trauma (Resick
& Calhoun, 2001).
(800) 592-1125
As with exposure therapy, CPT patients are asked to write about the traumatic event in detail. The patient is
then instructed to read the story aloud
repeatedly, both during and outside of the session. The therapist
helps the client identify and address
stuck points and errors in thinking, sometimes called “cognitive
restructuring.” These stuck points
may be thoughts like “I am a bad
person” or “I deserved this.” The therapist helps the patient address these errors
or stuck points by having the client gather
evidence for and against those thoughts.
Therapist Richard Dane Holt, LISW, has
treated veterans with CPT in Clovis, New
Mexico, since 2007 and became a certified
CPT provider in June 2010. While most of
his patients are combat veterans and participate in individual therapy, Holt has also
completed one CPT group.
“I have found CPT to be a very effective
treatment for veterans with PTSD, especially when the written protocol is followed
fairly closely,” Holt said. “So far, everyone
who has completed CPT treatment with me
has seen a decrease in their PTSD symptoms. Most have seen a significant decrease.
Of those who have chosen not to complete
the treatment, most still experienced some
decrease in symptoms.”
The primary focus of any treatment plan
that includes CBT begins with the identification of irrational thoughts that create the
fears and anxieties in an individual suffering from anxiety disorders. CBT works to
replace those irrational fears with realistic
thought patterns that provide an individual with healthy thought processes. It also
helps the patient learn a new way to handle these distressing thoughts and to gain
an understanding of these events. By using the skills learned in therapy, they can
learn why recovery from traumatic events
has been difficult. CPT helps patients learn
how going through a trauma changed the
way they look at the world, themselves,
and others. The way they think and look at
things directly affects how they feel and act
(“Cognitive processing therapy,” 2009).
CPT has four main parts:
• Learning about PTSD symptoms. CPT
begins with education about specific
PTSD symptoms and how the treatment
can help. The therapy plan is reviewed,
and the reasons for each part of the ther-
d CPT
“I have foun
effective
y
r
e
v
a
e
b
to
r
treatment fo
th
veterans wi
ially
PTSD, espec
when the
ocol
written prot
is followed
.”
fairly closely
apy are explained. During this step, patients are encouraged to ask questions
and to know exactly what they are going
to be doing in therapy. They also learn
why these skills may help.
• Becoming aware of thoughts and
feelings. Next, CPT focuses on helping patients become more aware of their
thoughts and feelings. When bad things
happen, we want to make sense of why
they happened. Patients learn how to
pay attention to their thoughts about
the trauma and how they make them
feel. They are asked to step back and
think about how the trauma is affecting
them now.
• Learning skills. After they become more
aware of their thoughts and feelings, patients learn skills to help them question
or challenge their thoughts. They do this
with the help of worksheets. They will
be able to use these skills to decide the
way they want to think and feel about
their trauma.
• Understanding changes in beliefs.
Finally, patients will learn about the
common changes in beliefs that occur
after experiencing trauma. Many people have problems understanding how
to live in the world after trauma. Their
beliefs about safety, trust, control, selfesteem, other people, and relationships
can change. In CPT, they will get to talk
about their beliefs in these different areas and learn to find a better balance
between the beliefs they had before and
after the trauma.
Fall 2010 ANNALS 25
In CPT, the patient works closely with
the therapist over a course of 12 sessions to
reach his or her goals. During the therapy,
the patient will also have the chance to practice the new skills outside of therapy sessions. The more practice patients receive,
the sooner the therapy will begin working.
By choosing to approach experiences in a
new and different way, patients will be able
to decide how the past affects their future.
Holt said the treatment works best with
frequent contact because each session builds
upon knowledge and skills learned in the
previous session.
“CPT specifically targets the areas
at which PTSD patients are stuck,” he
explained. “In-session discussions and
homework assignments early in treatment
are designed to identify the individual’s
stuck points. Cognitive restructuring exercises help each patient learn to look at
their stuck points in a fresh and more
productive way, eventually resulting in
no longer being stuck in that particular
area of their lives.”
Throughout the treatment, symptom
severity is measured using the PTSD
Checklist Stressor Specific Version
(PCL-S). This helpful tool allows patients
and therapists to clearly see the progress
being made.
A detailed, step-by-step instruction manual helps ensure consistent provision of
treatment between providers and patients.
This consistency is useful in measuring the
success of the therapy in a variety of settings. However, there is a certain amount
of flexibility built into the manual. For example, a therapist can choose to provide
the full CPT protocol or the CPT cognitive
only (CPT-C) protocol. The latter uses less
of the exposure material.
“Both versions have been shown to be
quite effective but with slightly different strengths and advantages,” Holt said.
“Flexibility is also seen in the mode of treatment, as CPT has been used effectively in
groups as well as in individual sessions.
There is also a bereavement session that is
available as needed.”
Online Learning
The Center for Deployment Psychology
(CDP) offers courses to train mental health
providers in CPT. The center was established in 2006 and was initially funded by
Congress. It is now a component center
of the Department of Defense’s Defense
26 ANNALS Fall 2010
Center of Excellence for Psychological
Health and Traumatic Brain Injury. The
CDP’s mission is to train military and
civilian psychologists, psychology interns, residents, and other behavioral
health professionals to provide highquality deployment-related behavioral
health services to military personnel
and their families.
CDP offers an online course,
“Cognitive Processing Therapy
(CPT) for PTSD in Veterans and
Military Personnel,” to provide an overview
of CPT. While this course teaches the basic
principles and strategies underlying CPT,
course organizers say it should not be considered a substitute for the in-person twoday CPT training module.
The Medical University of South Carolina
is also making it easier for mental health
professionals to learn the basics of cognitive
processing therapy through its new online
course, CPTWeb (www.cpt.musc.edu). The
free, nine-hour multimedia course is based
on Cognitive Processing Therapy Veteran/
Military Version: Therapist’s Manual (Resick,
Monson, & Chard, 2008), and its modular, asynchronous, self-study approach lets
mental health professionals learn at their
own pace from any computer.
“It’s a way for therapists who are not part
of the VA system or some other system to
get this type of training if they don’t have
a huge travel budget or the time to go to
trainings,” said professor and CPTWeb developer Connie Best, PhD, of the National
Crime Victims & Treatment Center at the
Medical University of South Carolina in
Charleston. “The good thing about it is
that they can do it at their leisure at the office or at home.”
CPTWeb was funded by the U.S. Navy
Bureau of Medicine and Surgery and was
intended for use by mental health professionals within the Department of Defense
and the Department of Veterans Affairs. It
is also available for use by civilian therapists
who provide treatment to active duty or retired personnel and members of the Guard
and Reserve. It may also be helpful to mental health professionals who are providing
treatment to family members.
“The Navy funded the project and they
then allowed the Medical University of
South Carolina to house the Web site
on our server, which makes it accessible to providers in the Navy, any mental
health provider in the VA’s Department of
“Cognitive
g
restructurin
lp
exercises he
each patient
at
learn to look ts
poin
their stuck
d more
in a fresh an
ay.”
productive w
Defense, and civilian providers,” Best explained.
CPTWeb is offered at no charge, and
mental health professionals who complete
the course receive nine contact hours of
continuing education from the Medical
University of South Carolina.
Each module of CPTWeb includes a
video introduction to the technique; preand post-tests of knowledge of a treatment
component; an overview of the module’s
learning objectives, a description of the
techniques of the treatment component,
and step-by-step instructions for how to
implement them; sample scripts for introducing the techniques to patients; multiple
video demonstrations of the techniques;
suggested practice assignments for patients;
and discussions of common clinical challenges that often arise in real-life practice.
“Hopefully the skills therapists gain from
CPTWeb will help them provide empirically supported treatments for PTSD to
those who have sacrificed so much for our
nation,” Best said.
References
Cognitive processing therapy. (2009, October 30). Retrieved from http://www.ptsd.va.gov/public/pages/
cognitive_processing_therapy.asp
How Common is PTSD? (2008, February 28). Retrieved from http://ncptsd.va.gov/ncmain/ncdocs/
fact_shts/fs_how_common_is_ptsd.html
Resick, P.A., & Calhoun, K.S. (2001). Posttraumatic stress disorder. In D.H. Barlow (Ed.), Clinical
handbook of psychological disorders: A step-by-step
treatment manual, 3rd edition (pp. 60-113). New
York, NY: Guilford Press.
www.americanpsychotherapy.com
CHS0310AN
®
“Protecting Our Homeland
in the 21st Century”
Protect Your Homeland.
Become Certified in Homeland Security, CHS® today.
The CHSSM program has earned its reputation as the premier group dedicated to providing certification, training, and continuing education to
professionals across the nation who are committed to improving homeland security. We boast a total commitment to our country’s safety, an
extraordinary knowledge base, and an in-place organizational structure
that delivers the highest-quality certification and continuing education
opportunities in homeland security.
Join us today as we work together to protect what matters most—our
families, communities, country, and way of life.
OOO GI BILL APPROVED! OOO
The American Board for Certification in Homeland Security, CHS
®
2750 E. Sunshine St. | Springfield, MO 65804 | www.abchs.com | (877) 219-2519 | cao@abchs.com
MEI0310AN
CERTIFICATION PAYS!
The American College of Forensic Examiners InstituteSM offers
certifications that show the world your expertise!
•
•
•
•
•
Certified Forensic Accountant, Cr.FA®
Certified Medical Investigator®, CMI
Certified Forensic Nurse, CFN®
Certified Forensic Consultant, CFC®
Registered Investigator, RI®
• Sensitive Security Information, Certified®
• Certified in Disaster Preparedness, CDP-ISM
• Certified Forensic Physician®, CFP
• Accredited Forensic Counselor, AFCSM
• Certified Master Forensic Social Worker, CMFSWSM
Call (800) 423-9737 or log on to www.acfei.com for more information.
(800) 592-1125
Fall 2010 ANNALS 27
CE ARTICLE: 1 CE credit
This Healing Dreamscape created for grieving mother Hope (left) depicts her late son Ishmael both as an adult (center) and as a 2-year-old on his mother’s lap (inset).
Images of both his birth father and his stepfather, who was his true father figure, were included in the portrait.
Prescriptive
Photomontage:
A process and product for meaning-seekers
with complicated grief By Nancy Gershman, BA, and Jenna Baddeley, MA
28 ANNALS Fall 2010
www.americanpsychotherapy.com
This article introduces prescriptive photomontage,
a playful method for meaning-making designed to give a renewed sense of hope and
purpose to those with complicated grief. Made in consultation with a grieving client
to augment traditional bereavement support, the process entails an interview and
photo review, culminating in a brainstorming session in which the Preferred Story
(Freedman & Combs, 1996) is defined. The story either mythologizes the legacy of the
deceased or envisions a future in which the client’s continuing bond (Klass & Walter,
2001) with the deceased becomes a source of empowerment. The product is a fine
art photomontage or “Healing Dreamscape” that envisions the Preferred Legacy or
Future. The making of a Healing Dreamscape for Hope, a 62-year-old widow and
bereaved mother with complicated grief, is described in our case example.
rief is not only the loss of a beloved person. It also poses a fundamental challenge to the bereaved person’s identity,
goals, plans, and dreams (Neimeyer, 2000,
2010). Future plans whose fulfillment depended on a continuing relationship with
a loved one are inconceivable in the wake
of the loved one’s death. Individuals experiencing complicated grief have particular
difficulties reclaiming hope in this mental state. In recent decades, bereavement
research has shifted away from the opinion that it is healthy to break bonds with
a loved one (Freud, 1917) toward a view
that healthy grief involves continuing bonds
with deceased loved ones through conversation and memory (Klass & Walter, 2001).
Grief counseling has historically involved a
wrenching working-through of emotional
pain. Now research emphasizes the social and emotional benefits of smiling and
laughing during grief (Bonanno & Keltner,
1997) and of telling redemptive stories to
one’s consolers (Baddeley & Singer, 2008).
A relatively new tradition of bereavement
therapy adopts narrative methods to help
the bereaved revise disempowering stories and find new empowering meanings,
more satisfying identities, and more rewarding continuing bonds with the deceased
(Neimeyer, 2000, 2010).
Most, but not all, bereaved people seek
meaning in loss; most meaning-seekers find
meaning with no therapeutic intervention.
Grievers who have had traumatic losses that
violated their assumptions of a safe and predictable world may find themselves caught
in a futile search to find meaning in their
loss and regain purpose in lives disrupted
by the loss. These individuals may be diagnosed with complicated grief (Neimeyer,
(800) 592-1125
2006), and it is these individuals who typically seek and benefit from bereavement
interventions such as therapy or support
groups (Neimeyer, 2000).
The current article introduces a new
method (prescriptive photomontage or the
Healing Dreamscape method) for helping
individuals with complicated grief to integrate their losses. This method capitalizes on advances in computer technology,
namely digital photo manipulation. It has
two aims: (1) to shift the griever’s perspective of the deceased from absent supporter
to supportive presence; and (2) to provide
the griever with a tangible object (a Healing
Dreamscape) that reinforces this shift. As a
therapeutic process of creativity and play,
the method is in line with play therapy
(Wolfelt, 2006), except in this iteration, it
is designed for adults. Likewise, its method
of co-creating a more hopeful narrative with
the griever draws upon narrative therapy
(Freedman & Coombs, 1996).
What is a Healing Dreamscape? Visually
speaking, a Healing Dreamscape is a hybrid
object: a photomontage populated with people, scenery, and objects from the griever’s
personal life that hold positive connotations
for them. It integrates disparate images into
a whole, meshing fantasy, reality, past, present, and future. The selection of imagery
for the Dreamscape is co-defined with the
griever in a process that draws out details of
what previously had defined the hoped-for
future with their loved one. The net effect is
a picture of a soothing, hope-filled future.
The Healing Dreamscape is a tangible
visualization of how a griever might draw
strength from a continuing bond with the
deceased. For example, for one Dreamscape,
first author N.G. learned that a client’s
shared dream with his deceased partner
was to perform together at the Eisteddfod
Music Festival. In the Preferred Future the
artist and client conceived together, the
griever is in the choir at the festival, with
the deceased directly behind him, in a gesture that works either as an imminent caress
or conducting. In another example, N.G.
places a new granddaughter in the arms of
her [deceased] great-grandfather because
the grieving daughter is struggling with
how much her father “was always a part of
this family.” In this respect, the Dreamscape
gently reminds the griever to do active work
on the Preferred Legacy (e.g., presenting
the deceased as an accessible role model) or
Preferred Future (i.e., through consummation of a dream or goal).
For bereaved individuals who view life
through a negative filter, it is difficult to
conjure up a hope-filled future without
This article is approved by the following for continuing education credit:
The American Psychotherapy Association provides this continuing education credit for Diplomates and certified
members, who we recommend obtain 15 CEs per year to maintain their status.
After studying this article, participants should be better able to do the following:
1. Describe the conceptual roots of prescriptive photomontage (e.g. narrative therapy)
2. Discuss the aims of the Healing Dreamscape process, i.e., for client and therapist to co-construct a Preferred Legacy
or Preferred Future that is captured in the product
3. Explain the multiple ways a client can use the finished Healing Dreamscape in his or her healing process
KEY WORDS: prescriptive art, complicated grief, bereavement, loss, narrative therapy, play therapy
TARGET AUDIENCE: Counselors and clinicians working with patients who are dealing with loss, bereavement, and/
or complicated grief
PROGRAM LEVEL: Basic
DISCLOSURES: The first author has a studio, Art for Your Sake, where she accepts commissions. She worked pro bono
on Hope’s case and received no compensation from either Hope or Unity Hospice, which referred Hope to her. This
was done in order that she might have ongoing access to Hope and her social worker in order to assess the efficacy of
the Healing Dreamscape method.
PREREQUISITES: None
Fall 2010 ANNALS 29
Fig. 1: 10-year-old
Ishmael
guidance. Thus, the Healing Dreamscape
process is artist-guided and the product
is artist-made. In this sense, the Healing
Dreamscape process is a form of prescriptive
art, a relatively new means of intervention
in which expressive art is custom-made to
provide relief for individuals in physical
or psychological distress.
Prescriptive artists today include music
thanatologists, whose work has been shown
to significantly decrease blood pressure and
reduce the need for pain medication among
patients with chronic pain and/or dementia (Foster, 2009). In the visual arts, documentary photographer Todd Hochberg
photographs families bonding with a stillborn or dying baby in the time they have
to say goodbye (Brotman, 2010; Hochberg,
2003). Hochberg’s album of fine art photography—a keepsake for the parents—
sends a powerful message that a baby’s life,
however brief, is worthy of memory.
Artist and photographer Jennifer Karady
works with veterans re-contextualizing (in
a safe, peacetime setting) specific war zone
memories which, in Karady’s words, “have
come home with them.” Cast in elaborately
staged narrative tableaus with friends and
family, veterans talk about how “something
clicks” into place, reducing their feelings of
alienation and anxiety as the picture “slows
the whole scene down” for contemplation
(McKinley, 2010).
The takeaway from these examples of
prescriptive art is three-fold:
1.Prescriptive art is personalized, specific to
the biography of the individual or family
for whom it is made. It invites the client to
reframe the meaning of traumatic events.
30 ANNALS Fall 2010
2.Fine art made by an artist elevates that
client’s story, highlighting its universal themes and affirming the client’s
self-worth.
3.Art that is life-affirming and multi-layered with meaning lends itself to sharing,
providing opportunities for meaningful
interactions and secondary healing.
What qualifies someone to be a prescriptive
artist? To work with such a creative intervention tool, an individual must be an accomplished fine artist; a compassionate interviewer who develops rapport with a client
to elicit positive themes and memory; and an
artist-educator whose end product promotes
healthy thought, feeling, and action on the
part of the client. In the following case example, the Healing Dreamscape process and
product both play an ongoing, constructive
role in transitioning a traumatized mother
powerless to save her child to an empowered grandmother with a legacy to share.
Following the case example, we discuss the
method in more general terms.
her son. She is prescribed Clozapine (200
mg) yet still has persistent anxiety. She sleeps
fitfully and is markedly on the edge, feeling
like “a bundle of nerves.” Concerned about
Hope’s lack of progress in her support group,
Becky talks to her about expressive arts therapy. Hope refuses.
“Actually, I wanted to talk more about
Ishmael. I wanted to give someone else all
the details. But using brush and paint—
I couldn’t deal with it. I was completely
numb. I wanted to do nothin’, know nothin’. Nothin’ to do with nothin’.”
Becky proposes the idea of an artist
(N.G.) making her a remembrance portrait
of Ishmael. When Hope understands that
she will be guided through a process that
will be playful, not painful, Hope agrees
to meet N.G. The possibility of creating
an uplifting memorial appeals to her. In
Hope’s words: “I was just hurting and didn’t
have the strength for art. I had no idea what
to do. But this was exciting. I would have
Ishmael with me in a dreamscape. I’d be
able to picture him as he is now.”
A Case Example: Hope and
the Death of her Son Ishmael
Step 1: Intake Phase. N.G. makes a house
call to Hope. While pulling photos from a
shoe box, Hope recounts Ishmael’s murder
and its murky circumstances. Ishmael was
found in the driver’s seat of a car, slumped
over the steering wheel. His crack-addicted
mother-in-law and another man (possibly
her drug dealer) had fought in the back
seat, at which time Ishmael was fatally shot.
Hope blames Ishmael’s mother-in-law and
is furious and disconsolate over the botched
investigation—no DNA tests performed on
the knife found at the scene; a gun never
found; the murderer never identified. She
feels spurned by the legal system and abandoned by members of her church, who neither sent sympathy cards nor called. Months
later, Hope finds a letter from Ishmael to
his wife, confessing to a fling with another
woman and asking for forgiveness. This revelation is especially troubling, reopening old
wounds as Hope tries to reconcile love and
admiration for her “baby” with new information that casts him in a negative light. Hope’s
reaction at the time is stark: “If you’re not in
the light, then it’s wicked.”
With N.G.’s guidance, Hope begins to
view the Dreamscape as a way to reclaim a
positive legacy for Ishmael. She points out
photos that capture his upbeat and loving
nature. She talks about his exemplary work
ethic and his pride at being involved in his
children’s lives. Hope has two vivid mem-
When the prescriptive artist (first author,
N.G.) first meets Hope, she has been attending a bereavement support group for 15
consecutive months without improvement.
She enters the group as an outpatient with
complicated grief and suicidal ideation after
her youngest son, Ishmael, is murdered—the
latest in a string of multiple serious losses. A
divorce in 1977 from first husband Lonnie
triggered Hope’s first major depressive episode. Her beloved Aunty’s death in 1987
triggered a second. Over the next 6 months,
Hope advances from one anti-anxiety medication (Valium; 10 mg/2x daily) to another
(Librium; 10 mg/3x daily). Ten years pass,
and a happy 10-year marriage ends with the
death of her second husband, Isaiah, leading to a prescription for Celexa (20 mg). On
January 15, 2007, Ishmael is murdered, and
Hope is committed for three days to Mercy
Hospital’s psychiatric ward for suicidal ideation, hysteria, and severe insomnia. Her
Celexa prescription is doubled.
Becky (not her real name), Hope’s assigned
social work intern, finds Hope’s symptoms to
be consistent with a diagnosis of complicated grief (Horowitz, Siegle, Holen, Bonanno,
Milbrath, & Stinson, 2003). Hope has extreme difficulty accepting Ishmael’s death,
longing for him nearly every day and worrying about “freaking out” at reminders of
www.americanpsychotherapy.com
P r es c r i p t i v e P h o t o m o n ta g e : A process and product for meaning-seekers with complicated grief
ories that enthrall her: one of an adorable
2-year-old Ishmael sitting on her bed in
footed pajamas; the other, a 34-year-old
Ishmael grilling hot dogs in the snow, undaunted by the Chicago wind chill. Though
the photo of baby Ishmael is damaged and
no photo exists of Ishmael grilling in the
snow, N.G. explains how through the digital photomontage process, these memories
can be reconstituted in her Dreamscape.
Throughout the interview, Hope expresses
her faith and spirituality. She hopes that
Ishmael is at peace in heaven, envisioning a
safe place of fluffy clouds and brightness.
Step 2: Brainstorming Phase. Client and
artist agree that a Preferred Legacy portrait is
called for because Ishmael’s good reputation
is at stake. The overarching question that informs the selection of images is: what photos best portray Ishmael as Hope wants him
to be remembered? The Dreamscape must
strike the right emotional tone, reminding
Hope of Ishmael’s inherent sweetness, good
humor, and high energy. N.G. guides Hope
to a photo of herself after attending church
service and another of Ishmael. Both are
wearing brilliant white, a fitting metaphor
for Hope’s central theme of “brightness.”
Initially Hope sees herself and Ishmael as
the Dreamscape’s only subjects. Yet she circles back twice, first to include her second
husband, Isaiah, and then later, her first
husband, Lonnie. The logic flow is this:
Isaiah was the love of her life and Ishmael’s
true father figure, but Lonnie was his father.
When N.G. checks in to ask, “Would you
like the four of you in the Dreamscape?”
Hope looks pleased but affirms that conceptually, the two periods should not overlap.
In this regard, the Dreamscape will honor
both the maternal and matrimonial relationships that defined Hope’s life, paying
special homage to Hope’s continuing bond
with her late husband.
The theme of peace is also important, as
in, where does Ishmael rest in peace now?
Therefore, before selecting imagery for the
setting, N.G. asks Hope to name a special
place she has been to that gave her a sense
of peace and calm. Hope recalls a cruise she
had taken and reveals that she has a photograph of her cabin. The photo features a
porthole in the cabin that is reminiscent of a
church’s clerestory window, with light pouring through. The image conveys the sense
of peace and heavenliness precious to Hope,
so N.G. will include it in the Dreamscape.
Step 3: Photo search Phase. In Step 1,
the Interview Phase, Hope and N.G. look
through Hope’s photos for inspiration and
to gain a shared vision of Hope’s most
meaningful memories of Ishmael. By contrast, the aim of the Photo Search Phase is
to find additional images that will resolve
some of the challenges identified in Step 2,
the Brainstorming Phase. For example, including the photo of Hope and family from
the Lonnie years means featuring a 10-yearold Ishmael. However, the image of Ishmael
at 10 years old does not resonate as much
with Hope as does his baby picture. N.G.
offers to replace this older Ishmael (Figure
1) with baby Ishmael (Figure 2). However,
the baby photo—particularly Ishmael’s
beloved “wild and nappy hair”—is badly
bleached by age. N.G. suggests cloning an
Afro for baby Ishmael from one of Ishmael’s
own children. Hope tracks down a photo
of Ishmael’s son Aquil in a bathtub with
his siblings (Figure 3). The result delights
Hope, feeling like a posthumous gift.
Back to the central photo of Ishmael in
his bright white shirt. His body language
expresses self-assurance, but the expression
is mock-gangster, so N.G. encourages Hope
to seek out another photo that expresses joy
instead. Hope locates a photo where Ishmael
beams as he snaps his own picture. Once
N.G. identifies which additional images
need to be tracked down from a source other than Hope, the Creation Phase begins.
Step 4: Creation Phase. N.G.’s task is now
to produce a photomontage that reflects
the positive themes that surfaced in Hope’s
interview. This means the image should,
first of all, give the feeling of peace and
brightness; and, second, portray Ishmael
and Hope as envisioned in Hope’s fondest
memories—which happen to occur during two entirely different periods in time.
To meet the first challenge, N.G. integrates
three separate images from different sources
to shape the Dreamscape’s environment: the
floor of snow (from another photographer’s
images) reflective of the grilling memory
and reminiscent of Hope’s classical idea
of heaven; the backdrop, taken from an
ethereal nighttime underwater shot of an
A recommendation
for how clinicians might engage a prescriptive
artist to work with their clients
First, define the purpose of the prescriptive product.The selection of an
appropriate prescriptive artist is dependent upon what the prescriptive
art method needs to accomplish for the patient, not what medium is
best (e.g. photomontage, photograph, etc.) Different prescriptive artists’
work may have slightly different goals (e.g., to memorialize a relationship or a legacy, to spur conversation with loved ones, to restructure
or recontextualize traumatic memories).
Second, select the appropriate prescriptive artist. The first author
is in the process of compiling a list of established and emerging prescriptive artists along with the goals of their work and examples. In
the interim, readers can contact the first author for a current listing.
It is always best if the clinician has a firsthand opportunity to speak
with the prescriptive artist and become familiar with the artist’s body
of work. Additionally, prescriptive artists on the whole tend to docu(800) 592-1125
ment their process with a client, from the intake period forward, taping and transcribing conversations audio-visually or in transcripts. The
clinician may request these tapes and transcripts, which should provide
a good sense of the prescriptive artist’s interpersonal sensitivity and
interviewing skills.
Third, arrange a joint meeting between the clinician, the patient, and
the prescriptive artist. Once the clinician has identified an appropriate prescriptive artist for the case in question, clinician and patient can
meet with the artist in his or her studio or conduct a conference call
with the artist from the clinician’s office. If both clinician and patient
are comfortable with the prescriptive artist’s work and his or her interpersonal style, the prescriptive art process can proceed. The patient
can then decide how closely he or she wants the clinician to follow the
prescriptive art process with the artist.
Fall 2010 ANNALS 31
illuminated pool; and the porthole from
Hope’s cabin, which becomes a heavenly
portal inside the Dreamscape. Together,
these images evoke Hope’s spiritual theme
of brightness and peace.
To meet the second challenge, N.G. needs
to integrate Hope’s two favorite memories
of Ishmael—one of him as an adult and one
of him as a child—into a cohesive whole.
N.G. decides to juxtapose these two memories from different points in time by creating an inner scene within an outer scene.
In the outer scene we see the adult Ishmael,
flanked on his left by a jubilant Hope in
Sunday finery and on his right by his stepfather, Isaiah. To emphasize the adult Ishmael
as happy, hardworking, and a good father to
his children, N.G. uses the beaming face of
Ishmael that Hope retrieved from her photo
collection. N.G. also supplies the image of a
child’s tool belt, which the adult Ishmael in
the Dreamscape wears to symbolize his work
ethic and his bond with his children.
To create the inner scene, N.G. places a
TV set on the main stage (i.e., the snowy
floor). Within the TV set, she places the
Lonnie-Hope family grouping. N.G. swaps
out the 10-year-old Ishmael sitting on Hope’s
lap for baby Ishmael, now cosmetically enhanced with Aquil’s Afro. N.G. extends baby
Ishmael’s little footed feet out and beyond
the TV set, to be warmed by the swirling
heat rising from the grill (See Dreamscape,
page 28). Throughout the process, N.G. emails drafts of the Dreamscape to Hope asking for feedback and suggestions. Now the
Dreamscape is in its final iteration, ready to
be printed and shared with others.
Step 5: Sharing Phase. After Hope is presented with a hard copy of the Dreamscape,
she talks to N.G. about its meaning, and in
doing so, makes some unexpected discoveries. Hope notices how her left arm—which
wraps tightly around Ishmael—branches
Escher-like from Ishmael’s left arm. The
seamlessness of the intertwining arms recalls
Finkbeiner (1996) referring to a parent’s reaction to their child’s death as an “amputation effect,” where “the lifeline that is cut is
not only between the child and the parent,
but between the parent and the future.”
Here, Hope experiences her Dreamscape as
a reversal of the amputation effect, melding Hope and son back together again and
reaffirming their bond: “At first, I thought
Ishmael’s hand was missing. But after all,
it is art so real, I told you, let’s keep it the
same. That’s the connection. This photo32 ANNALS Fall 2010
montage will be the connection. I know
that my baby love me.”
Hope is delighted by the synthetic image of baby Ishmael warming his toes
by the grill’s fire. After she has taken the
Dreamscape home, she reflects on how this
hybrid memory mobilizes her creative reasoning, self-soothing abilities, and positive
thinking: “When I used to close my eyes,
I’d see my baby in his casket and that was
just so hurting I couldn’t take it. When this
photomontage was made, now I see this
little baby with the hot dogs, and it’s like
he’s saying ‘Goody, mommy! Hot dogs!
Hot dogs!’ I see him now, this little baby I
was blessed with. This really brings me to
just forget about a lot of wickedness and
evil around me and what happened to
my son, the way he was. Takes my mind
off trying to take revenge and getting even,
the hot dogs takes my mind off all that...
Sometimes in the night I get up and go to
the computer and put up the little baby part
and hey, I can go right to sleep.”
Hope also uses the Dreamscape as a
means to engage with others who loved
Ishmael. Running into old acquaintances
of her son or late husband, she shows them
copies. This initiates a process of joint reminiscing as the Dreamscape reminds them
of the deceased’s best qualities and of good
times spent together (Walter, 1996). When
she can, Hope hands out copies in her role
as Ishmael’s “memory-keeper.” Recipients
are grateful for being singled out for this
gift, while Hope is rewarded with their
positive feedback and thanks. Without fail,
when told that this legacy portrait was made
by an artist for Hope’s recovery, recipients
interpret this as a special honor.
Today, Hope’s Dreamscape gives her
the courage to reprocess, recover, and reclaim the shattered pieces of her life.The
living Ishmael is gone, but for Hope, the
Dreamscape embodies Ishmael’s legacy and
their continuing bond: “I can do that art
therapy now...but what we did then [with
the Dreamscape], that just brought me out.
When I saw what we made, I just got caught
up in the moment...It seemed as if Ishmael
was here, alive. Because it’s physically here
[as Hope’s screen saver] where I see it every
day...He’s here and in my heart.”
The Method of Prescriptive
Photomontage
Below, we trace the steps of prescriptive
photomontage, a recursive process, with
movement back and forth between any two
Fig.2: 2-yea
r-
old Ishmael
steps. Through
these steps, the griever’s increasing involvement in the creative process invests them in
their own healing.
Step 1: Intake Phase. A major premise of
prescriptive photomontage—drawn from
narrative therapy (Payne, 2006)—is that
the problem is not all there is. In Step 1, the
client flips through personal photographs,
introducing the loved one and the circumstances of the loss, while also describing
current challenges and hopes for the future.
Throughout, the prescriptive artist asks the
client to elaborate on sense-impressions, a
process that provides rich visual detail. The
leisurely pace of the photo review allows for
questions that probe nearly forgotten events
once associated with great joy. Meanwhile,
the artist identifies positive recurring themes
that translate well into visual terms. For example, in our case illustration, Hope tells
stories that reflect the theme of good over
evil, referring frequently to the term “brightness.” Viewing these “bright” elements later
in the Dreamscape, Hope is finally able to
see herself as an epic character persevering
against evil (White & Epston, 1990).
Secondly, prescriptive photomontage is
based on the idea that continuing bonds
with the deceased should be encouraged,
not relinquished. Recent research suggests
that it is normal for the bereaved to experience the deceased person as an ongoing
presence in their psychological life (e.g.,
Klass & Walter, 2001). This is also in keeping with clinicians’ suggestions that those
working with the bereaved should encourage continuing bonds that empower the
griever (e.g., Neimeyer, 2010). Next, as the
www.americanpsychotherapy.com