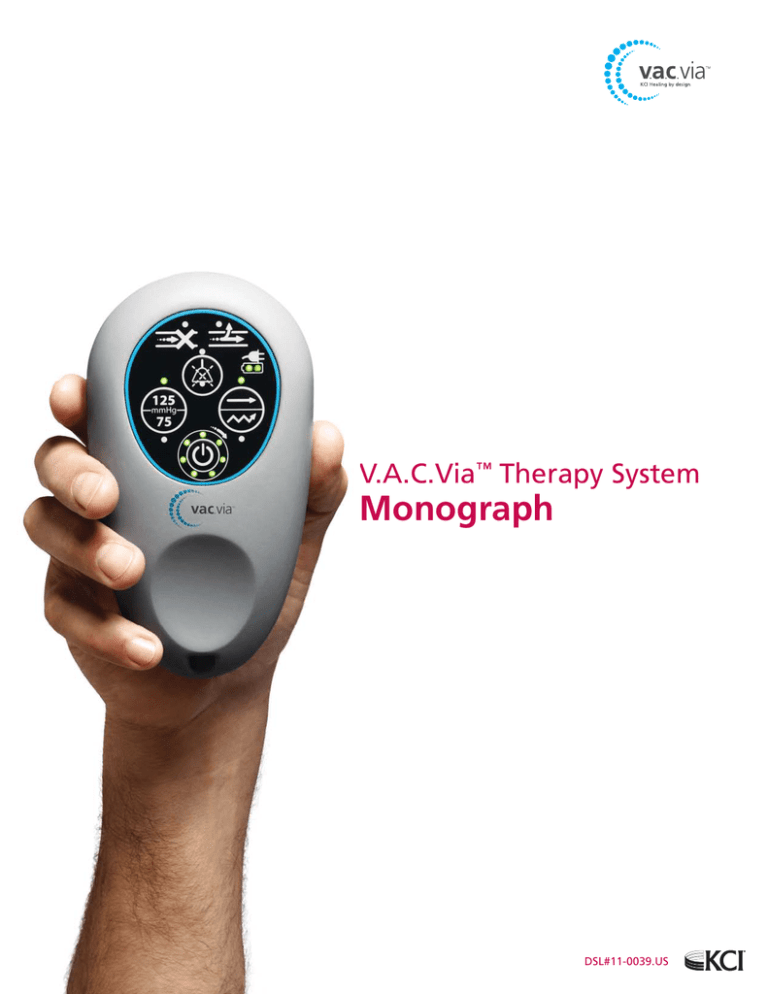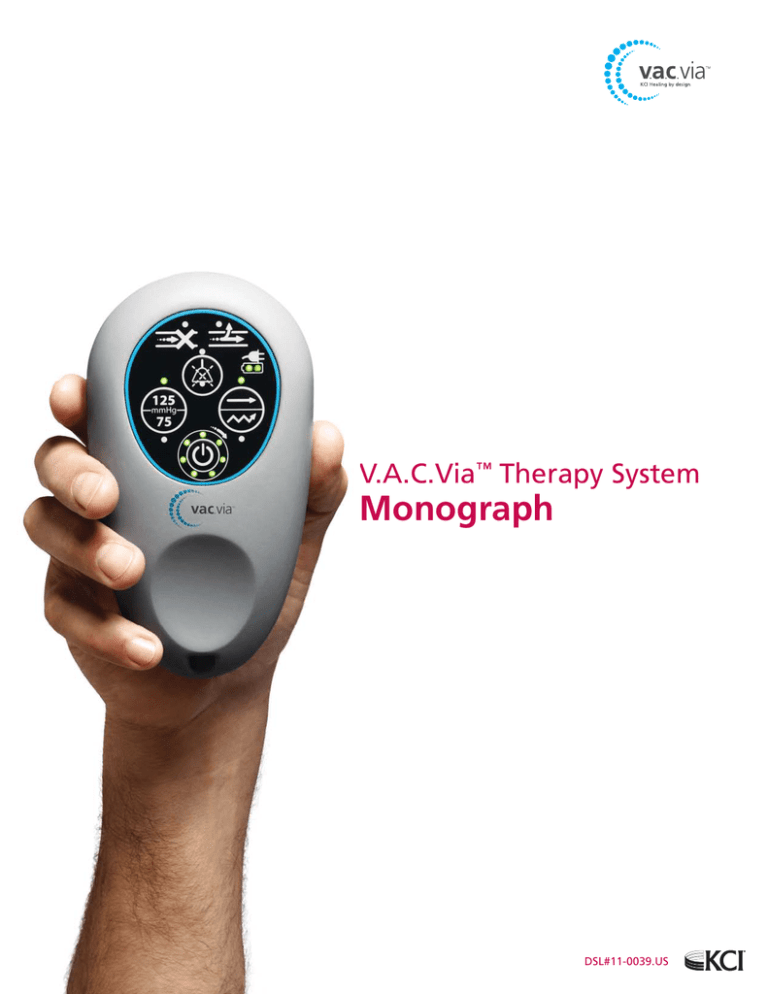
V.A.C.Via™ Therapy System
Monograph
DSL#11-0039.US
Table of Contents
Preface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2
Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
V.A.C.Via™ Therapy System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
V.A.C.Via™ Therapy System Product Description . . . . . . . . . . . . . . . . . . 3
Optimum Use Conditions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Safety Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Contraindications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Warnings and Precautions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Customer Preference Testing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6
Case Studies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Case Study 1: Dehiscence after open reduction internal fixation of tibial fracture . . 7
Case Study 2. Integra® Dermal Regeneration Template Placement . . . . . . . . . 8
Case Study 3. Free radial forearm flap transfer . . . . . . . . . . . . . . . . . . . 9
Key Evidence Supporting the Use of V.A.C.® Therapy Family of Products . . . . . . . 10
Acute Wounds . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Chronic Wounds . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 11
Cost Effectiveness of V.A.C.® Therapy . . . . . . . . . . . . . . . . . . . . . . . .
12
Cost-Effectiveness Analysis Studies . . . . . . . . . . . . . . . . . . . . . . . . 13
Early vs. Late Use of V.A.C.® Therapy . . . . . . . . . . . . . . . . . . . . . . . 13
Cost-Effectiveness Modeling . . . . . . . . . . . . . . . . . . . . . . . . . . . 13
Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18
V.A.C.Via™ Therapy System
Monograph
DSL#11-0039.US
Preface
The V.A.C.Via™ Therapy System is a small, portable and virtually silent addition to the V.A.C.® Therapy family of technologies (Figure 1).
This document provides a comprehensive introduction of the V.A.C.Via™ Therapy System and the role it plays on the wound healing continuum of care. This publication will:
•Describe the V.A.C.Via™ Therapy unit and its components
•Suggest optimum use conditions
•Review the V.A.C.® Therapy literature for wounds suitable for V.A.C.Via™ Therapy
•Describe clinical outcomes in various case studies
•Demonstrate potential cost savings such as:
- Reducing length of stay (LOS) based on immediate access to a V.A.C.® Therapy technology
- Transitioning patients sooner from acute to home care
- Reducing staff time associated with therapy unit operation and dressing changes
- Providing a “for sale” NPWT system that eliminates much of the administrative challenges (eg, indigent care) around a rental model
Figure 1: V.A.C.® Therapy Family of Products
2
V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
Introduction
The use of negative pressure wound therapy (NPWT) continues to
expand across the continuum of care, due to its positive effects
in healing a wide variety of wounds. Since the introduction of
V.A.C.® Therapy in 1997,1 the number of competing commercialized NPWT devices and dressing combinations has skyrocketed. To
date, there have been over 800 publications that have discussed
the use of commercial NPWT systems, with 97% (776/801) coming
from the use of V.A.C.® Therapy. Wound type, size, and severity,
as well as treatment cost, and patient mobility have become
important considerations when choosing an NPWT system. Given
increasing portability of personalized electronic devices (eg, cell
phones and computers), patients have come to expect similar
trends in medical device technologies.
V.A.C.® Therapy devices have traditionally been rented, which often
causes a delay in initiating therapy, due to the time required to
process rental and home care reimbursement paperwork. Faster
methods of procurement are now demanded to speed transition
from acute care to home care. For example, patients with splitthickness skin grafts (STSGs), who would benefit from immediate
application of V.A.C.® Therapy, could be immediately transitioned
to home care if a V.A.C.® Therapy System was available on site
in the hospital. What often happens is that patients are required
to stay in acute care while waiting for coverage for the V.A.C.®
Therapy System to be granted for home care use. Patients often
remain hospitalized for the single purpose of waiting to receive
V.A.C.® Therapy treatment, an issue that is increasingly being
challenged by hospital administrators.
These expanded needs of patients, clinicians and administrators
for more portable and immediately available therapy systems
prompted the creation of the V.A.C.Via™ Therapy System (Figure
2)—a next generation, ultra-lightweight, portable, single-patientuse V.A.C.® Therapy product. The V.A.C.Via™ Therapy System is an
integrated wound management system for use in acute, extended
and home care settings. It is intended to create an environment
that promotes wound healing by secondary or tertiary (delayed
primary) intention by preparing the wound bed for closure, reducing
edema, promoting granulation tissue formation and perfusion,
and by removing exudate and infectious material. It is indicated
for patients with chronic, acute, traumatic, sub-acute and
dehisced wounds, partial-thickness burns, ulcers (such as diabetic,
pressure or venous insufficiency), flaps and grafts.2
Figure 2: V.A.C.Via™ Therapy System
V.A.C.Via™ Therapy System
V.A.C.Via™ Therapy System Product Description
The V.A.C.Via™ Therapy System is equivalent to other V.A.C.®
Therapy Systems in terms of providing the same performance
specifications, mechanisms of action (Figure 3), and benefits of
traditional V.A.C.® Therapy. However, the V.A.C.Via™ Therapy Unit
is a single use, disposable V.A.C.® Therapy device designed to
be used for low exudating (<80 mL/day), small-to medium-sized
wounds, grafts and flaps in all care settings.
The V.A.C.Via™ Therapy delivers continuous subatmospheric
pressure (-75mmHg or -125mmHg) to the wound site via a small
or medium-sized V.A.C.® GranuFoam™ Spiral Dressing or Dynamic
Pressure Control™ (DPC) Therapy. DPC cycles the negative pressure
between 25mmHg to 75 or 125mmHg at the wound site in six
minute cycles as shown in Figure 4.
By sustaining the negative pressure above 0 mmHg between negative
pressure cycles, the level of discomfort is potentially eliminated
from the foam dressing expanding when negative pressure returns
to 0 mmHg; this also helps minimize possible dressing leaks that
can occur in the absence of negative pressure.
V.A.C.Via™ Therapy primarily differs from the other V.A.C.® Therapy
products in its compact size and 7–day therapy life. In addition,
it is available for sale rather than rental to allow for stocking in
hospital inventory for immediate use.
3
Provides a moist, closed wound healing environment
Cell Migration
and Proliferation
Macrostrain
(Draws wound
edges together)
Tissue Microstrain
(Promotes granulation
tissue formation)
Promotes Perfusion
Removes
Infectious Materials
Reduces Edema
Figure 3: Mechanism of Action of the V.A.C.® Therapy System of Products
The V.A.C.Via™ Therapy System is comprised of:
•A single-patient use NPWT unit
- Provides 7 days of V.A.C.® Therapy
- Operates under a rechargeable battery
- Weighs 0.7 lbs (0.032 kg)
- Simplified user interface
n Alarms for blockage and leaks
n Indicators for power and therapy life
-New Vortis™ Pump Technology (Figure 5) contained
inside the therapy unit makes it the quietest and
smallest V.A.C.® Therapy unit
•
A sterile single-use 250 mL disposable canister
•A sterile single-use dressing kit containing:
- Medium Spiral GranuFoam™ Dressing
(14.5 x 17 x 1.75 cm) or
Small Spiral GranuFoam™ Dressing
(7.7 x 11.2 x 1.75 cm)
- V.A.C.® Advanced Drape
- Interface pad and tubing set with foam quantity
record label
-3M™ Cavilon™ No-Sting Barrier Film (to help assure
dressing seal)
- Ruler (for wound measurement)
•A carrying case and lanyard that provide portability
options
A product comparison chart for the complete V.A.C.® Therapy
Upper Setting
-25mmHg
Figure 4: Dynamic Pressure Control™ Therapy
4
V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
Current V.A.C. Therapy System
®
V.A.C.Via Therapy System
550
450
400
350
300
250
200
150
™
100
Optimum Use Conditions
The V.A.C.Via™ Therapy System is expected to be used most
frequently in either of the following situations:
•As NPWT for low exudating (<80 mL/day), small-to medium-sized wounds, grafts and flaps in the acute care
setting (Figure 6).
•As a transition therapy for acute care patients who are
ready to be released to home care, and who require
continuation of NPWT at home. Depending on the
clinician’s
assessment
and
healthcare
agency
reimbursement guidelines, treatment may be continued
with additional V.A.C.Via™ Therapy Systems or from a
rental therapy unit. For example, in indigent hospital
paid placements, V.A.C.Via™ Therapy is an alternative
system that can provide a set number of therapy days
after the patient leaves the institution while eliminating
the risk of a lost rental therapy unit or unexpected days
billed.
Safety Information
The following safety information is that currently provided in all
V.A.C.® Therapy Systems. There is no safety information specific
to the V.A.C.Via™ Therapy System. Refer to complete safety
information as provided in V.A.C.Via™ Therapy Instructions for Use.
Clinical
Judgement
50
family of products is listed in Attachment 1.
Wound Exudate (mL)
Figure 5: Vortis Pump Technology
™
80 ml/day
Wound Volume (cm3)
Figure 6: V.A.C.® Therapy System Selection Criteria
Warnings and Precautions
As with any prescription medical device, failure to carefully read
and follow all instructions and safety information prior to use
may lead to improper product performance. The following table
(Table 1) summarizes all warnings and precautions that should be
considered when using the V.A.C.Via™ Therapy System.
Contraindications
The following are contraindications for the V.A.C.Via™ Therapy
System:
•Do not place foam dressings of the V.A.C.Via™ System
directly in contact with exposed blood vessels, anastomotic
sites, organs or nerves. Do not use on patients with:
- Malignancy in the wound
- Untreated osteomyelitis
- Non-enteric and unexplored fistulas
- Necrotic tissue with eschar present
NOTE: Refer to appropriate section in Instructions for Use
5
Table 1. Warnings and Precautions When Using the V.A.C.Via™ Therapy System
Warnings
Precautions
Therapy should be used with caution on patients who are at high risk of
bleeding complications (ie, weakened or friable blood vessels or organs in
or around the wound) or who are without adequate wound hemostasis
Standard precautions for infection control should always be applied to
reduce the risk of transmission of bloodborne pathogens
Therapy should not be used on exposed or superficial vessels (including
infected blood vessels) and organs in or around the wound
Continuous, rather than Dynamic Pressure Control™, is recommended
over unstable structures in order to help minimize movement and stabilize the wound bed
Therapy should be used with caution on patients who are receiving doses
of anticoagulants or platelet aggregation inhibitors that are thought to
increase the risk for bleeding
Continuous therapy is generally recommended for patients at increased
risk for bleeding, highly exudating wounds, fresh flaps and grafts, and
wounds with acute enteric fistulae
Therapy should not be used when sharp edges or bone fragments are
exposed; they must be eliminated or covered first
The size and weight of the patient should be considered when prescribing
V.A.C.® Therapy
Therapy should be used with caution on infected wounds, which may
require more frequent dressing changes than non-infected wounds
In the event a patient experiences autonomic dysreflexia (ie, sudden
changes in blood pressure or heart rate in response to stimulation of the
sympathetic nervous system), V.A.C.® Therapy should be discontinued to
help minimize sensory stimulation
Therapy should be used in conjunction with natural tissue, meshed nonadherent material, or bio-engineered tissue over tendons, ligaments, and
nerves
Therapy unit should not be taken into the MR environment; therapy
dressing can typically remain on patients with minimal risk
To minimize the risk of bradycardia, V.A.C.® Therapy should not be placed
in proximity to the vagus nerve
V.A.C.® Therapy is not recommended if enteric fistula effluent management
or containment is the sole goal of therapy
Therapy unit should not be taken into a hyperbaric oxygen chamber
The use of 3M™ Cavilon™ No Sting Barrier Film should be considered to
protect the periwound skin
Use of circumferential dressings should be avoided, except in the presence
of anasarca or excessively weeping extremities, where a circumferential
drape technique may be necessary to establish and maintain a seal
Table 2. Customer Preference Testing Results (n=110)
Customer Preference Testing
Customer Preference Testing was used to survey the initial
Wound Types
Number of Patients
V.A.C.Via™ Therapy placements. Both clinician and patients
Surgical wounds
34
™
Dehisced
wounds
24
were given surveys at the start and end of V.A.C.Via Therapy.
Traumatic wounds
10
The intent of the study was to determine which wound types the
Pressure ulcers
23
physicians were treating with this device, average wound
Diabetic ulcers
7
Chronic ulcers
3
dimensions and volume, levels of exudates and ease of use.
Venous leg ulcers
2
Table 2 summarizes the results from clinician questionnaires
Arterial ulcer
1
regarding wound types, initial wound dimensions, and level of
Unknown wounds
6
exudates. Ninety-four percent of physicians did not experience
Average Wound Dimensions
difficulties in placements of the V.A.C.Via™ Dressing. Reported
Length (cm)
7.7
difficulties were due to leaks caused by the dressing placement
Width (cm)
3.9
Depth (cm)
2.1
location: one dressing could not be placed on the patient’s left
Volume (cm3)
72.8
knee, 3 dressings in the coccyx region, and 3 in the rectal region.
Overall, the data reveal positive results for the use of V.A.C.Via™
Therapy in the treatment of wounds listed in Table 2.
6
V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
Levels of Exudate
Low
Moderate
High
64%
32%
4%
Case Studies
Clinical experience with the V.A.C.Via™ Therapy System is
reported in the following case studies.
Case Study 1: Dehiscence after open reduction internal
fixation of tibial fracture
A 71-year-old female presented with increasing pain of the lower extremity. Patient had suffered a grade IIIB tibial fracture for
which she underwent open reduction internal fixation (ORIF).
She subsequently developed a polymicrobial wound infection,
requiring plate replacement and multiple debridements. Patient
was placed on a 6-week course of IV antibiotics for osteomyelitis. (Figure 7 A-D). Medical history included peripheral vascular
disease (PVD) and type II diabetes. Following irrigation and
debridement, NPWT (V.A.C. ATS® Therapy) was initiated in
the wound to prepare it for STSG closure. After two days of
wound bed preparation, the NPWT dressing was removed and
an STSG was placed. A non-adherent layer (Adaptic® Nonadhering Dressing; Systagenix US, Quincy, MA) was cut slightly
larger than the STSG and placed over the skin graft. The V.A.C.Via™
Granufoam™ Spiral dressing was trimmed to the size of the nonadherent layer and placed over it. Pressure was initiated at -125
mmHg continuously and the patient was discharged home.
B) After two days of NPWT, an STSG was applied
On postoperative Day 6, the patient returned to the outpatient
clinic and the V.A.C.Via™ Therapy dressing was removed. There
was an approximately 100% graft take with good aesthetic results.
Figure 7. Case Study 1:
Dehiscence after open reduction of tibia fracture.
C) Application of V.A.C.Via™ Therapy System over STSG
A) Wound dehiscence at presentation
D) Wound on postoperative Day 6 after V.A.C.Via™ Therapy
dressing was removed
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual
results may vary depending on the patient’s circumstances and condition.
7
Case Study 2: Integra® Dermal Regeneration Template
Placement
A 71-year-old male patient presented for evaluation of scalp
reconstruction with diagnosis of melanoma Breslow thickness of 5.3mm and with a failed graft (Figure 8 A and B).
Wide local excision with sentinel node biopsy was performed
and bilaminate skin substitute (Integra® Dermal Regeneration
Template, Integra LifeSciences, Plainsboro, NJ) was used to
cover the defect (Figure 8 C-D). The patient’s medical
history included diabetes, PVD, and coronary artery
disease. A non-adherent layer (Adaptic® Non-adhering
Dressing; Systagenix US, Quincy, MA), cut slightly larger than the
Integra® graft, was applied over the skin substitute. A V.A.C.Via™
Therapy dressing was applied on top of the non-adherent
layer and pressure was initiated at -125 mmHg. The patient was
discharged home.
On postoperative Day 5, the patient returned to the outpatient
clinic for follow-up and removal of the V.A.C.Via™ Therapy
dressing. The Integra® graft appeared intact and viable. Following
availability of final pathology revealing clear margins, an STSG
was placed on post operative Day 24. A non-adherent layer and
V.A.C.Via™ Dressing were placed over the STSG. V.A.C.Via™
Therapy was discontinued 6 days post STSG with 100% take
of graft.
B) Excision of Integra® graft
In both instances, patient was discharged home with V.A.C.Via™
Therapy. Procedures were performed as outpatient and no
delays for V.A.C.® Therapy approvals were encountered.
C) Application of new Integra® graft
Figure 8. Case Study 2:
A) Integra® graft failure
D) Application of V.A.C.Via™ Therapy System over Integra®
As with any case study, the results and outcomes should not be interpreted as a guarantee or warranty of similar results. Individual
results may vary depending on the patient’s circumstances and condition.
8
V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
Case Study 3: Free radial forearm flap transfer
A 62-year-old male patient presented with a fracture to his left
leg due to a traffic accident while riding a bicycle. A free radial
forearm flap transfer was used to cover the defect. Treatment
of the donor site required multiple surgical interventions and
subsequent meshed STSG. A V.A.C.Via™ Therapy dressing was
applied at the donor site for 5 days, resulting in good healing of
the STSG (Figure 9 A-C).
Figure 9. Case Study 3:
A) Soft tissue findings after debridement before mesh-graft
coverage
B) Intraoperative after mesh-graft coverage
As with any case study, the results and outcomes should
not be interpreted as a guarantee or warranty of similar
results. Individual results may vary depending on the patient’s
circumstances and condition.
C) V.A.C.Via™ Therapy over mesh-graft coverage
9
Key Evidence Supporting the Use of the
V.A.C.® Therapy Family of Products
NPWT is a common method of actively bolstering STSGs in
difficult recipient beds. Adjunctive NPWT for 3-6 days has been
recommended over STSGs in cases of contoured surfaces,
exudative surfaces, surfaces subject to repeated motion, and
areas of compromised vascularity.12, 27 In addition, application
of NPWT prevents fluid collection beneath the graft, protects
the graft from outside contaminants and shear, and provides
positive contact between the bed and newly transplanted skin.
Pressure is distributed evenly over contoured surfaces, and the
pliability of the dressing allows limited movement of the recipient surface without compromising the graft.27 NPWT has also
As previously indicated, the V.A.C.Via™ Therapy Systems is
equivalent to other V.A.C.® Therapy System in terms of providing
the same performance specifications, mechanisms of action
and benefits of traditional V.A.C.® Therapy. A literature review
of V.A.C.® Therapy use was conducted based on the types of
wounds that would most likely be applicable to V.A.C.Via™
Therapy. Several published randomized controlled trials (RCTs)
and case series are provided for review and can be found in
Table 3.
Table 3. V.A.C.® Therapy Technology Key References
Wound Type
Number of Articles
Key References
Number of Articles
Key References
Acute Wounds
Zannis et al 2009 (PCT)
Siegel et al 2007 (CRS)
5
Yang et al 2006 (CRS)
6
Moues et al 2004 (RCT)
3
4
Surgical Wounds
109
General Trauma
17
Grafts
Machen et al 2007 (CSE)
8
Labler et al 2007 (CST)
7
9
Blume et al 2010 (RS)
Vidrine et al 2005 (CRS)
11
Moisidis et al 2004 (RCT)
12
Scherer et al 2002 (CSE)
10
58
13
Lavery et al 2008 (RCT-P)
Armstrong and Lavery 2005 (RCT)
15
Paola 2010 (RCT)
14
9
Diabetic Foot Amputations
Eginton et al 2003 (RCT)
16
Chronic Wounds
Pressure Ulcers
30
Wanner et al 2003 (RCT)
18
Ford et al 2002 (RCT)
19
Joseph et al 2000 (RCT)
Diabetic Foot
26
20
Chronic Leg
7
17
Blume et al 2008 (RCT)
Vuerstaek et al 2006 (RCT)
21
CRS: Comparative Retrospective Study; CSE: Case Series; PCT: Prospective Controlled Trial; RCT: Randomized Controlled Trial;
RCT-P: Post hoc Analysis of previously published RCT
Acute Wounds
The effectiveness of early, short-term NPWT in preparing acute
wounds for surgical closure is well documented.22-25 Applied
as a temporizing dressing, NPWT has been shown to downstage soft tissue coverage requirements on the ‘reconstructive
ladder.’24 The therapy has demonstrated reduced incidence
of acute wound infection in high-energy open fractures,26
compared to gauze dressings.
10 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
been shown to improve autograft survival as measured by
increased qualitative graft take11, and a reduction in secondary
procedures and number of repeated STSGs.10, 12, 28
An RCT by Armstrong and Lavery investigated the effects of
NPWT compared with standard moist wound care (control)
in complex wounds secondary to partial foot amputation in
diabetic patients.14 There were 162 patients who were randomly
assigned to NPWT (n=77) or control (n=85). All wounds were
treated until healing or completion of the 112-day treatment
period. The results showed that more patients healed in the
NPWT group compared to the control group (43 versus 33,
respectively; p=0.04) with faster rates of healing (p=0.005). The
NPWT group also reached 76-100% granulation faster than the
control group (42 days versus 84 days, respectively; p=0.002).
The authors concluded that NPWT was a safe and effective
treatment for complex diabetic foot wounds.14
In a more recent published RCT by Paola et al, the authors
evaluated the effectiveness of NPWT in improving graft takes
of diabetic foot wounds (Study I) and treatment for infected
open minor amputations (Study II).15 In Study I, 70 patients were
randomized to NPWT (n=35) or non-adherent gauze (n=35) for
coverage of their grafts. The findings revealed that complete
graft take was significantly better in the NPWT group than the
non-adherent gauze group (80% versus 68%, respectively;
p=0.05). In Study II, 130 diabetic patients were randomized to
NPWT (n=65) or standard modern wound dressings (n=65) for
treatment of their amputations. All patients received a vascular
assessment with transcutaneous oxygen pressure measurements.
NPWT patients achieved complete closure of the wound in
65±16 days compared to 98±45 days for standard wound
dressings (p=0.005). Also, the NPWT group developed wellvascularized granulation tissue over exposed bone significantly
faster than the standard wound dressing group (41±8 versus
59±18 days, respectively; p=0.03). Based on these outcomes,
use of NPWT resulted in faster wound bed preparation and
closure and better graft take rates as compared to standard
wound care.15
Chronic Wounds
Adjunctive NPWT has been shown to be effective in different
types of chronic wounds, including pressure ulcers (PrUs),
diabetic foot ulcers (DFUs), and venous leg ulcers (VLUs), by
removing exudate and infectious materials and promoting
granulation tissue formation.20, 29 In addition to irrigation and
debridement, mechanisms of action of V.A.C.® Therapy assist
physicians and clinicians in reducing ulcer size and preparing
the wound for closure. Short-term application of V.A.C.® Therapy
will be most effective in chronic wounds that have been
thoroughly debrided and converted to acute wounds. Furthermore, V.A.C.Via™ Therapy may benefit chronic wound patients
who could transition out of the hospital with the immediate
provision of an outpatient V.A.C.® Therapy device.
for treating diabetic patients with a stage II or III calcaneal,
dorsal, or plantar foot ulcer ≥2 cm2 in area.20 All wounds
were treated until ulcer closure or completion of the 112-day
treatment period. A greater percentage of foot ulcers attained
complete closure with V.A.C.® Therapy (73/169, 43.2%)
compared to AMWT (48/166, 28.9%; p=0.007) within the
treatment period. Based on Kaplan-Meier analyses, the median
time to complete ulcer closure was 96 days (95% CI, 75.0114.0) for V.A.C.® Therapy (p=0.001) and could not be determined for AMWT. Additionally, significantly fewer amputations
were reported for V.A.C.® Therapy patients compared to AMWT
patients (7/169 versus 17/166, respectively; p=0.035). These
findings showed that V.A.C.® Therapy is as safe as and more
efficacious than AMWT in the treatment of DFUs.20
In a prospective randomized trial by Joseph et al, V.A.C.® Therapy
was compared to traditional saline-wet-to-moist (WM) dressings
for the treatment of chronic wounds.19 Twenty-four patients
with 36 chronic wounds (mostly PrUs) were randomized to
receive either V.A.C.® Therapy or WM. Blinded, independent
wound evaluators measured wounds by volume displacement
of alginate impression molds and performed punch biopsies
for histology and culture. The results showed a significant
difference in volume with a change in depth of 66% for V.A.C.®
Therapy compared to 20% for WM (p<0.00001). Furthermore,
there was granulation tissue formation in 64% of the wounds
treated with V.A.C.® Therapy. The authors recommended that
V.A.C.® Therapy be applied to chronic, non-healing wounds
that are deep and complicated.
In the last RCT, Vuerstaek et al prospectively studied the
efficacy of V.A.C.® Therapy compared to conventional wound
care (control) for the treatment of venous leg ulcers.21 A total
of 60 patients (30 NPWT and 30 Control) were randomized;
the primary endpoint was time to complete healing. Data
revealed a significantly shorter time to achieve complete healing
using V.A.C.® Therapy with a median time of 29 days (95% CI,
25.5 to 32.5) for the V.A.C.® Therapy group as compared to 45
days (95% CI, 36.2 to 53.8) with control therapy (p=0.0001).
Additionally, wound bed preparation was significantly shorter
in the V.A.C.® Therapy group than the control group (7 days
versus 17 days, respectively; p=0.005). The authors recommended
that V.A.C.® Therapy “should be considered as the treatment of
choice for chronic leg ulcers owing to its significant advantages
in the time to complete healing and wound bed preparation
time compared with conventional wound care.”21
In the past 10 years, three different RCTs have been conducted
for DFUs, PrUs, and VLUs, respectively, comparing the use of
V.A.C.® Therapy versus the standard care for each wound type.
An RCT by Blume et al examined the safety and efficacy of V.A.C.®
Therapy compared with advanced moist wound therapy (AMWT)
11
Cost Effectiveness of V.A.C.® Therapy
Economic pressures continue to challenge the global healthcare
system. Wounds are a major source of patient morbidity and cost
to hospitals and community health providers, and wound care
costs are closely tied to the individual patient’s wound burden.30-35
In 2005, the US Centers for Medicare and Medicaid Services
(CMS) identified chronic wounds as an important issue for longterm study.36 Chronic wounds (eg, PrU) are difficult to heal and
often result in longer lengths of stay (LOS) than acute wounds
and require more skilled nursing visits and wound care supplies,
which drives up the cost of treatment.37, 38
In 2007, diabetes and its complications cost the US $174 billion;
$116 billion were in direct costs and $58.3 billion in indirect
costs, such as loss of productivity, disability, and premature
mortality.67 Diabetic foot problems impose a major economic
burden, and costs increase disproportionately to the severity of
the condition. The cost of care for patients with a foot ulcer is
5.4 times higher in the year after the first ulcer episode and 2.8
times higher in the second year compared with diabetic patients
without foot ulcers. Patients with DFUs require more frequent
emergency department visits, are more commonly admitted to
hospital, and require longer LOS.68
In 2008, more than 89 million US patients were treated for
wound-related conditions at a cost exceeding $25 billion.30 In
hospitals alone, an estimated 5 million patients have complex
chronic wounds that cost the US healthcare system more than
$20 billion.39 Of these chronic wounds, VLUs account for 80%
to 90% of all lower extremity ulcerations. It is estimated that
over 2.5 million people have VLUs, resulting in a loss of 2 million
workdays per year and at an estimated treatment cost of
greater than $2.5 billion per year.40 Furthermore, PrUs and their
prevention have become a challenge to both caregivers and
healthcare facilities. PrUs account for more than $1.3 billion in
healthcare costs per year. The prevalence of PrUs in acute care
is between 4% to 34%, with treatment estimates ranging from
$2,000 to $70,000, depending on severity,41 which is particularly
onerous to the facilities because the additional costs associated
with hospital-acquired PrUs are not reimbursed.
Healthcare systems continue to be challenged by a lack of
resources and supplies to effectively provide adequate healthcare
that results in effective outcomes. One of the major issues in the
US healthcare system today is a lack of incentives to manage
patients through the continuum of care. In 1983, US legislation
was enacted that established set payments per admission that
were based on the patient’s diagnosis-related group rather than
payments based on hospital days and services rendered.42 The
goal of the legislation was to encourage shorter LOS in the hospital
12 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
and more efficient care; however, the policymakers were concerned about possible growth in readmissions.43 In 2009, Jencks
reported that 19.6% of 11,855,702 Medicare beneficiaries who
had been discharged from a hospital were rehospitalized within
30 days, and 24% were rehospitalized within 90 days. Jencks
estimated that 10% of readmissions were planned. They also
estimated that the cost to Medicare of unplanned rehospitalizations
in 2004 was $17.4 billion.44, 45
Recent healthcare reforms are targeted at managing patient
outcomes through the continuum of care. In 2010, Morrison
reported that there are two big themes in the new US health
reform law, which include: 1) more people will be covered at
lower reimbursement and 2) there are changes coming that
will shift the game from payment for procedures to payment
for outcomes.46 This will allow healthcare reform laws to better
align with provider incentives and to reduce costs through
improvement of quality and care coordination. These reforms
will also institute value-based purchasing systems for hospitals,
voluntary bundled Medicare payment pilot projects, voluntary
pilot programs that allows qualifying hospital providers to form
accountable care organizations and share in Medicare cost
savings, and provides for financial penalties for hospitals with
excessive readmissions.47
Recently, President Barack Obama signed the Patient Protection
and Affordable Care ACT (PPACA) into law. This law will make
sweeping changes to the Medicare program to strengthen
program integrity by increasing the efficiency and quality of
medical services. Several provisions of the PPACA are consistent
with Medicare Payment and Advisory Commission (MedPAC)
recommendations to provide adequate incentives to produce
appropriate, high-quality care at an efficient price.48 For example,
PPACA will require the establishment of a national, voluntary
pilot program that will bundle physician and hospital payments
with the goal of improving patient care and reducing spending.49
Another provision establishes rewards for healthcare organizations that meet quality-of-care targets and reduce costs per
patient relative to a spending benchmark from the share of
the savings they achieve for the Medicare program.42, 49 The
Congressional Budget Office (CBO) estimates that this shared
savings program will save Medicare $4.9 billion over fiscal years
2010-2019.48
CMS is also looking into the Care Transitions Project within
the Quality Improvement Organization (QIO) 9th Statement of
Work. This project tasks QIOs in 14 states to coordinate care
and promote seamless transitions across care settings, including
from hospital to home, skilled nursing care, or home health care
agencies. It also targets the reduction of unnecessary readmissions
to hospitals that may increase risk or harm to patients as well
as Medicare costs. Measures arising from this work are geared
towards achieving goals of improved transitions of care and
greater coordination among providers. These measures should
be breaking down the traditional silos and shifting focus to the
continuum of care.50
p<0.0001), treatment days (5.1 versus 6.0 days, p=0.0498),
and ICU stays (5.3 versus 12.4 days, p<0.0001). These reductions translated into lower total costs ($32,175 versus $43,
956, p<0.0001) and variable costs ($15,805 versus $22, 891,
p<0.0001) with early intervention of NPWT for these traumatic
patients.23
Cost-Effectiveness Analysis Studies
Today, entities across the continuum of care use the methodology
of cost-effectiveness analysis (CEA) to structure the decision
making process of healthcare facilities when considering the
utilization of existing and new medical technologies.51 The
objective of CEA is to maximize health-related outcomes within
budget constraints. The major cost drivers for wound care include
time to healing, staff time, LOS in hospital, number of dressings,
rate of infections and long waiting time from diagnosis to
treatment.45 Only a small portion of costs involve technical
requirements to treat the wound. For instance, the cost of
materials (eg, dressings) typically accounts for 10-20% of the
total cost of treating a patient.36, 45
A third study by de Leon et al and Driver examined the effects
of early NPWT use on LOS in a long-term acute care setting.62, 63
This study retrospectively analyzed patients receiving NPWT early
(≤ 14 days of admission) and late (≥ 15 days of admission). The
findings demonstrated a reduction in mean LOS (35.4 versus
56.4 days, p<0.0001) and a 35% reduction in the mean time
to 50% wound closure (22 versus 34 days, p=0.0154) with early
NPWT use compared to late NPWT use. These data were also
associated with a reduction in total wound costs ($3,194 versus
$4,182, p=0.08) with early initiation of NPWT.
Several studies demonstrate that V.A.C.® Therapy can result in
fewer hospitalizations, emergent care incidents and complications,
reduced amputations, fewer dressing changes, decreased
personnel commitments, shorter hospitalization, and reduced
treatment times.5,7-9,37,66 By minimizing the factors that
contribute to direct and indirect wound care costs, V.A.C.®
Therapy has emerged as a cost-effective option for wound
healing through the continuum of care (Table 4). These economic
studies include several conducted on the benefits of early versus
late use of V.A.C.® Therapy
Early vs. Late Use of V.A.C.® Therapy
V.A.C.Via™ Therapy provides for early initiation of NPWT because
it can be stored on the shelf, thus avoiding extended delivery times.
Baharestani et al examined the impact of early versus late
initiation of NPWT on the LOS in home health care for patients
with Stage III or IV pressure ulcers or surgical wounds.54 The data
indicated that early intervention of NPWT was related to a reduction
in the overall length of home care services. For each day NPWT
initiation was delayed, nearly 1 day was added to the total length
of stay, potentially resulting in higher costs for wound care
treatment.54
A second study by Kaplan et al demonstrated the success using
NPWT early for the treatment of traumatic wounds.23 Trauma
patient records were retrospectively analyzed and divided into
early group (on day 1 or 2 of their hospital stay) or late group
(on day 3 or later). The results showed that early NPWT use was
associated with shorter hospital stays (10.4 versus 20.6 days,
Cost-Effectiveness Modeling
Currently, there are several economic studies that address the
costs associated with the use of NPWT in treating wounds.23, 31, 56, 59
Cost-effectiveness studies, such as Apelqvist et al56, Flack64 and
Schwien et al52, use economic models to compare the standard
medical costs of traditional wound care dressings with the costs
of using NPWT, including hospitalization and additional medical
procedures performed, and show total hospital savings between
$4,000 and $13,000 per patient episode. Patients with DFUs
run the risk of undergoing an amputation. Three published
studies have examined the clinical efficacy of V.A.C.® Therapy
versus traditional wound-care dressings. All three studies
showed V.A.C.® Therapy to be superior to traditional therapy.
Frykberg found V.A.C.® Therapy to reduce amputations by
5.8%;55 Blume displayed 6.1% fewer;20 and Armstrong showed
8.0% improvement.20 Amputations, in most cases, require
a readmission into an acute facility and cost the healthcare
system approximately $45,000 per case. In a recent study by
Driver et al comparing the costs of V.A.C.® Therapy versus
advanced moist wound therapy (AMWT), the authors found
that V.A.C.® Therapy reduced total inpatient costs by $3,364
per patient for DFU patients.68
V.A.C.® Therapy was shown by Page et al65 to reduce the risk
of readmission by 80% for patients with open wounds with
significant tissue defects when compared with saline-soaked
gauze. Additionally, Schwien et al retrospectively compared the
hospitalization rates for home-care patients with Stage III and
IV pressure ulcers treated with V.A.C.® Therapy versus other
wound care modalities. This study found that the hospitalization
rate due to wound complications was lower for patients treated
with V.A.C.® Therapy (5% versus 14%, p<0.01).52
13
Table 4: Literature Summary of V.A.C.® Therapy Cost-Effective studies
Wound Type
# of Patients
Costs Basis
Outcome
n=518 early group
(day 1 or 2)
n=1000 late group (day 3 or later)
2005
Early group patients had mean lower total ($32,175
vs $43,956; p<0.001) and variable costs ($15,805 vs
$22,891; p,0<001) than late group.
n=60 V.A.C.® Therapy
n=2,288 other
2003 & 2004
V.A.C.® Therapy patients had fewer hospital stays
(p≤0.05), fewer hospitalizations (p<0.01) and fewer
wound emergent care encounters (p≤0.01)
Traumatic Wounds
Kaplan et al (2009)
23
Pressure Ulcers
Schwien et al (2005)
52
Cost savings estimated $4,209 per episode
Philbeck et al (1999)
n=1032
1995 to 1998
Cost analysis showed a difference of $8,919 when
using NPWT (V.A.C.® Therapy) compared to MWT
Baharestani et al (2008)
n=65 early group (<30 days)
n=33 late group (>30 days)
2002 to 2004
Regression analysis indicated that for each day
NPWT initiation was delayed almost 1 day was
added to the total length of home care (β=0.96,
p<0.001)
n=12,795
2002-2003
Medicare patients had lower incidence of
amputations (p=0.0077)
53
54
Secondary Amputations
Frykberg and Williams
(2007)
55
56
Apelqvist et al (2008)
n=77 V.A.C.® Therapy
n=85 MWT
2005
Average direct cost per patient treated for 8 weeks:
$27,270 (V.A.C.® Therapy) versus $36,096 (MWT)
Average total cost to achieve healing: $25,954
(V.A.C.® Therapy) versus $38,809 (MWT)
57
Flack (2008)
Markov model
n=1000
NS
Demonstrated improved healing rates, more Quality
Adjusted Life years and an improved overall cost
of care $53,830 per person (V.A.C.® Therapy) and
$61,757 per person (AMWT dressings).
Markov model
n=1000
2008-2009
Experienced improved healing rates, more Quality
Adjusted Life years and an improved overall cost of
care €24,881 per patient/year (V.A.C.® Therapy) and
€28,855 per patient/year (Advanced Wound Care)
n=60 patients
2001-2003
Total wound care costs for hospitalized patients
were 25% to 30% lower for V.A.C.® Therapy
($3,881) versus stand wound care ($5,452)
n=54
NS
Mean hospitalization costs were €1,788 (V.A.C.®
Therapy) and €2,467 (conventional therapy)
p<0.043
n=352 early group (<7 days)
n=112 late group (>7 days)
2002-2004
Regression analysis indicated that for each day
NPWT initiation was delayed almost 1 day was
added to the total length of stay (β=0.97, p<0.001)
NS
Economic model estimates cost savings of over
$7,700 for treatment of dehisced chest wounds
with V.A.C.® Therapy compared to MWT dressings
1999-2001
Patients treated with NPWT showed a 70% reduction
in risk of complications, subsequent foot surgeries,
and hospital readmissions
Diabetic Foot Ulcer
58
Whitehead et al (2011)
Chronic Leg Ulcers
21
Vuerstaek et al (2006)
Full Thickness Wounds
59
Mouës et al (2005)
Surgical Wounds
54
Baharestani et al (2008)
60
Song et al (2006)
61
Page et al (2004)
n=47
NS: Not stated MWT: Moist Wound Treatment AMWT: Advanced Moist Wound Treatment
14 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
The Vuerstaek et al study of V.A.C.® Therapy versus Moist
Wound Therapy (MWT) revealed that total nursing time required to treat VLU’s was 40% lower for V.A.C.® Therapy
(232 minutes versus 386 minutes, p=0.001) (Figure 10).55
The V.A.C.Via™ System offers an even easier application than
our current V.A.C.® Therapy products. The V.A.C.Via™ System
has been developed to make the use of our NPWT systems
more intuitive for healthcare professionals and for patients.
Recently, KCI conducted an internal study comparing the
placement times between V.A.C.Via™ Therapy and InfoV.A.C.®
Therapy. This study concluded that V.A.C.Via™ Therapy takes
less than 10 minutes to complete product placement, a 19%
reduction in placement time compared to InfoV.A.C.® Therapy.
450
400
350
250
200
150
The economic model presented above illustrates the potential
cost effectiveness of the V.A.C.Via™ Therapy System on STSG.
Additional models can be constructed as clinical evidence is
reported for various wound types.
232
100
50
V.A.C.® Therapy (n=30)
Moist Wound
Therapy (n=30)
Hydrogels and Alginates
Nursing Time (Minutes)
Figure 10: Nursing time was reduced by 40% with V.A.C.®
Therapy versus MWT, Vuerstaek (2006)21
18.0%
A 10-year Retrospective Review of STSG Patients
Admitted to a Level 1 Trauma Center
16.0%
16.4%
14.0%
12.0%
10.0%
As previously indicated the process of obtaining home care
placement for medical devices is cumbersome and can take
days. Particularly in wounds, such as STSGs, that would benefit
from immediate application of NPWT, home care coverage for
the NPWT system is typically not granted until after the course
of treatment, if at all. Patients often remain hospitalized for
the single purpose of receiving NPWT treatment. Gabriel et al’s
results have also been inputted into a hypothetical model
(Table 6) to calculate savings per patient of $1,994.00 The total
potential savings from these two categories results in $3,532.15
per patient (Table 7).
386
40%
300
0
Blume et al25 retrospectively compared the survival outcomes of
STSGs between V.A.C.® Therapy and conventional therapy (eg,
cotton bolster, sterile compressive, and stainless steel gauze)
(Figure 11). Table 5 is a hypothetical economic model that uses
the superior clinical outcomes achieved by V.A.C.® Therapy in
reducing the number of repeat grafts to calculate savings of
$1538.15 per patient. Additionally, Gabriel et al conducted a
small study evaluating the impact of V.A.C.Via™ Therapy on
STSG patients.66 This study determined that using V.A.C.Via™
Therapy on STSG patients resulted in a reduction of at least one
hospital day per patient. Gabriel et al stated that an affordable,
for-sale disposable like V.A.C.Via™ Therapy may provide earlier
transition to the home.66
A Randomized Controlled Trial of Hospital Patients
with a Variety of Chronic Leg Ulcers
13.0%
8.0%
6.0%
4.0%
2.0%
0.0%
3.4%
V.A.C.® Therapy (n=87)
Conventional
Therapy (n=55)
% of Repeat Procedures
Figure 11: Percentage of failed STSG was reduced 13.0% (3.4%
versus 16.4%, p=0.006) with V.A.C.® Therapy versus conventional
therapy, Blume (2010)9
15
Table 5: V.A.C.Via™ Therapy hypothetical cost model (100 patient example) of repeated grafts based on Blume (2010)9
retrospective study (n=142; p=0.009).
Category
Conventional Therapy
(Assumed same as V.A.C.®
Therapy)
a
# of Patients
50
50
% of Repeat Grafts
3.5%
16.4%
# of Repeat Grafts
1.8
8.2
V.A.C.Via™ Therapy
Savings
Cost of Materials on Initial Graft
$24,750.00
$127.50
($24,662.50)
c
Cost of Repeat Graft
$29,691.00
$131,220.91
$101,529.91
Total Cost
$54,441.00
$131,348.41
$76,907.41
Cost per patient
$1,088.82
$2,626.97
$1,538.15
b
a
V.A.C.Via™ Therapy
Cotton bolster, sterile compressive, stainless steel gauze
V.A.C.Via™ Therapy cost: $495.00 per unit (includes $595.00 for the starter kit, with a $100 rebate); Cost of Conventional Therapy is $2.55
for dressings *50 Patients = $127.50.
b
Cost of a repeated graft is $16,000, and was calculated by averaging the cost of DRGs 573-578 based on publicly available 2008 HCUP data.
The following cost figures were averaged: DRG 573--$23,115; DRG 574--$12,578; DRG 575--$7,366; DRG 576--$29,100; DRG 577--$13,927;
DRG 578--$9,734. See http://hcupnet.ahrq.gov/. Cost of repeated graft per patient for V.A.C.Via™ Therapy is $16,495.00 ($16,000 + $495.00);
Cost of repeated graft per patient for Conventional Therapy is $16,002.55 ($16,000+2.55).
c
The above model uses selected study data to provide an illustration of estimates of costs for use of the V.A.C.Via™ Therapy System or conventional
therapy on STSGs. This model is an illustration and not a guarantee of actual individual costs, savings, outcomes or results. Results are based on
selected study data and may not be typical. Individual results may vary. The hospital and/or clinician is advised to use this model as an illustration
only to assist in an overall assessment of products and pricing.
Table 6: V.A.C.Via™ Therapy hypothetical cost model (100 patient example) of reduced LOS based on Gabriel et al (2011)66
prospective small pilot study (n=6).
Bolster Dressings
V.A.C.Via™ Therapy
Savings
Category
V.A.C.Via™ Therapy
a
# of Patients
50
50
Average LOS
4.6b
5.6a
c
Cost of LOS
$458,620.00
$558,320.00
$99,700.00
Cost per patient
$9,172.40
$11,166.40
$1,994.00
LOS for V.A.C.® Therapy was obtained from Blume (2010).9 Post-STSG LOS: 5.6 days.
a
LOS for V.A.C.ViaTM was calculated by reducing V.A.C.® Therapy LOS from 5.6 to 4.6 days based on Gabriel et al’s (2011)66 prospective small
pilot study (n=6). Gabriel stated that the purchase, versus rental, model of NPWT procurement was more cost-effective for this otherwise healthy
patient population, because hospital stay was reduced by at least one day per patient.
b
The average cost in 2008 for one day in an Acute facility is $1994, http://hcupnet.ahrq.gov/.
c
The above model uses selected study data to provide an illustration of estimates of costs for use of the V.A.C.Via™ Therapy System or conventional
therapy on STSGs. This model is an illustration and not a guarantee of actual individual costs, savings, outcomes or results. Results are based on
selected study data and may not be typical. Individual results may vary. The hospital and/or clinician is advised to use this model as an illustration
only to assist in an overall assessment of products and pricing.
Table 7: Total potential savings summary for V.A.C.Via™ Therapy
Reference
Category
Savings per Patient
Blume (2010)
Reduced Repeat Grafts vs. Conventional Therapy
$1,538.15
Gabriel (2010)
LOS Reduction vs. V.A.C.R THerapy
$1,994.00
Total Potential Savings
$3,532.15
16 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
Summary
This monograph provided a review of the literature on the use
of V.A.C.® Therapy over several wound types, as well as providing the V.A.C.® Therapy clinical and economic benefits. The
V.A.C.Via™ Therapy System is a simple, easy to use, virtually silent
device that has been developed as part of the wound healing
continuum
of
care.
V.A.C.Via™
Therapy
will
allow for transition of patients from the acute to the
homecare setting thereby improving their quality of care
and their quality of life. It should be considered as a first line
treatment for low exudating (<80 mL/day), small-to-mediumsized wounds, grafts and flaps.
In this age in which purchasing practices and policies should
ultimately support the founding principles of any healthcare
system, this “off the shelf” disposable product will help improve procurement efficiency and reduce costs associated with
duplication of administrative work, delays in delivery of a rental
unit, and may reduce the time needed to raise purchase orders.
Additional clinical research is still needed to fully understand
the scientific, medical and economic impact of the V.A.C.Via™
Therapy System in providing quality cost effective wound care.
17
References
(1) Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method
for wound control and treatment: clinical experience. Ann Plast Surg 1997
June 1;38(6):563-76.
(2) V.A.C.Via™Negative Pressure Wound Therapy System Instructions for
Use.
(3) Zannis J, Angobaldo J, Marks M et al. Comparison of fasciotomy
wound closures using traditional dressing changes and the vacuumassisted closure device. Ann Plast Surg 2009 April 1;62(4):407-9.
(4) Siegel HJ, Long JL, Watson KM, Fiveash JB. Vacuum-assisted closure
for radiation-associated wound complications. J Surg Oncol 2007 November 12;96(7):575-82.
(5) Yang CC, Chang DS, Webb LX. Vacuum-assisted closure for fasciotomy wounds following compartment syndrome of the leg. J Surg Orthop
Adv 2006 March 1;15(1):19-23.
(6) Moues CM, Van Den Bemd GJ, Heule F, Hovius SE. A prospective
randomized trial comparing vacuum therapy to conventional moist gauze
therapy. Presented at the 2nd World Union of Wound Healing Societies’
Meeting, July 8-13, 2004, Paris, France. 6. 7-8-2004.
(7) Machen MS. Management of traumatic war wounds using vacuumassisted closure dressings in an austere environment. Army Med Dept J
2007 January 1;17-23.
( 8) Labler L, Trentz O. The use of vacuum assisted closure (VAC) in soft tissue injuries after high energy pelvic trauma. Langenbecks Arch Surg 2007
September 1;392(5):601-9.
(9) Blume PA, Key JJ, Thakor P, Thakor S, Sumpio B. Retrospective evaluation of clinical outcomes in subjects with split-thickness skin graft: comparing V.A.C.® therapy and conventional therapy in foot and ankle reconstructive surgeries. Int Wound J 2010 December 1;7(6):480-7.
prospective, randomized trial of vacuum-assisted closure versus standard
therapy of chronic nonhealing wounds. Wounds 2000 May 1;12(3):60-7.
(20) Blume PA, Walters J, Payne W, Ayala J, Lantis J. Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced
moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial. Diabetes Care 2008 April 1;31(4):6316.
(21) Vuerstaek JD, Vainas T, Wuite J, Nelemans P, Neumann MH, Veraart
JC. State-of-the-art treatment of chronic leg ulcers: A randomized controlled trial comparing vacuum-assisted closure (V.A.C.) with modern
wound dressings. J Vasc Surg 2006 November 1;44(5):1029-38.
(22) Rinker B, Amspacher JC, Wilson PC, Vasconez HC. Subatmospheric
Pressure Dressing as a Bridge to Free Tissue Transfer in the Treatment of
Open Tibia Fractures. Plast Reconstr Surg 2008 May 1;121(5):1664-73.
(23) Kaplan M, Daly D, Stemkowski S. Early intervention of negative pressure wound therapy utilizing vacuum assisted closure in trauma patients:
impact on hospital length of stay and cost. Adv Skin Wound Care 2009
March 1;22(3):128-32.
(24) Stannard JP, Singanamala N, Volgas DA. Fix and flap in the era of
vacuum suction devices: What do we know in terms of evidence based
medicine? Injury 2010 May 12.
(25) DeFranzo AJ, Argenta LC, Marks MW et al. The use of vacuum-assisted closure therapy for the treatment of lower-extremity wounds with
exposed bone. Plast Reconstr Surg 2001 October 1;108(5):1184-91.
(26) Stannard JP, Volgas DA, Stewart R, McGwin G, Jr., Alonso JE. Negative pressure wound therapy after severe open fractures: a prospective
randomized study. J Orthop Trauma 2009 September 1;23(8):552-7.
(27) Schneider AM, Morykwas MJ, Argenta LC. A new and reliable method of securing skin grafts to the difficult recipient bed. Plast Reconstr Surg
1998 September 1;102(4):1195-8.
(10) Vidrine DM, Kaler S, Rosenthal EL. A Comparison of negative-pressure dressings versus Bolster and splinting fo the radial forearm donor site.
Otolaryngol Head Neck Surg 2005 September 1;133(3):403-6.
(28) Molnar JA, DeFranzo AJ, Marks MW. Single-stage approach to skin
grafting the exposed skull. Plast Reconstr Surg 2000 January 1;105(1):1747.
(11) Moisidis E, Heath T, Boorer C, Ho K, Deva AK. A prospective, blinded,
randomized, controlled clinical trial of topical negative pressure use in skin
grafting. Plast Reconstr Surg 2004 September 15;114(4):917-22.
(29) Lavery LA, Boulton AJ, Niezgoda JA, Sheehan P. A comparison of diabetic foot ulcer outcomes using negative pressure wound therapy versus
historical standard of care. Int Wound J 2007 June 1;4(2):103-13.
(12) Scherer LA, Shiver S, Chang M, Meredith JW, Owings JT. The vacuum
assisted closure device: A method of securing skin grafts and improving
graft survival. Arch Surg 2002 August 1;137(8):930-4.
( 30) Al-Benna S. A discourse on the contributions of evidence-based medicine to wound care. Ostomy Wound Manage 2010 June 1;56(6):48-54.
(13) Lavery LA, Barnes SA, Keith MS, Seaman JW, Jr., Armstrong DG. Prediction of healing for post-operative diabetic foot wounds based on early
wound area progression. Diabetes Care 2008 January 1;31(1):26-9.
(14) Armstrong DG, Lavery LA, Diabetic Foot Study Consortium. Negative pressure wound therapy after partial diabetic foot amputation:
a multicentre, randomised controlled trial. Lancet 2005 November
12;366(9498):1704-10.
(15) Paola LD, Carone A, Ricci S, Russo A, Ceccacci T, Ninkovic S. Use of
vacuum assisted closure therapy in the treatment of diabetic foot wounds.
J Diabet Foot Complications 2010 August 20;2(2):33-44.
(31) De Leon JM, Barnes S, Nagel M, Fudge M, Lucius A, Garcia B. Costeffectiveness of negative pressure wound therapy for postsurgical patients
in long-term acute care. Adv Skin Wound Care 2009 March 1;22(3):122-7.
(32) Horch RE, Nord D, Augustin M, Germann G, Leffler M, Dragu A.
[Economic aspects of surgical wound therapies]. Chirurg 2008 June
1;79(6):518-25.
(33) Nord D. [Cost-effectiveness in wound care]. Zentralbl Chir 2006 April
1;131(Suppl 1):S185-S188.
(34) Nord D. Efficacy and cost-efficiency in wound care. The German
V.A.C. experience. J Wound Technol 2008 June 1;(1):42-5.
(16) Eginton MT, Brown KR, Seabrook GR, Towne JB, Cambria RA. A prospective randomized evaluation of negative-pressure wound dressings for
diabetic foot wounds. Ann Vasc Surg 2003 November 1;17(6):645-9.
(35) Posnett J, Gottrup F, Lundgren H, Saal G. The resource impact of
wounds on health-care providers in Europe. J Wound Care 2009 April
1;18(4):154-61.
(17) Wanner MB, Schwarzl F, Strub B, Zaech GA, Pierer G. Vacuum-assisted wound closure for cheaper and more comfortable healing of pressure
sores: a prospective study. Scand J Plast Reconstr Surg Hand Surg 2003
January 1;37(1):28-33.
( 36) Centers for Medicare and Medicaid Services (CMS) H. MedCAC Meetings: Usual care of chronic wounds. 3-29-2005.
(18) Ford CN, Reinhard ER, Yeh D et al. Interim analysis of a prospective, randomized trial of vacuum-assisted closure versus the healthpoint
system in the management of pressure ulcers. Ann Plast Surg 2002 July
2;49(1):55-61.
(19) Joseph E, Hamori CA, Bergman S, Roaf E, Swann NF, Anastasi GW. A
18 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
(37) Black J, Baharestani MM, Cuddigan J et al. National Pressure Ulcer
Advisory Panel’s updated pressure ulcer staging system. Adv Skin Wound
Care 2007 May 1;20(5):269-74.
(38) Baharestani M, De Leon J, Mendez-Eastman S et al. Consensus Statement: A practical guide for managing pressure ulcers with negative pressure
wound therapy utilizing vacuum-assisted closure- understanding the treatment algorithm. Adv Skin Wound Care 2008 January 1;21(Suppl 1):1-20.
( 39) Rodrigues I, Megie MF. Prevalence of chronic wounds in Quebec home
care: an exploratory study. Ostomy Wound Manage 2006 May 1;52(5):468, 50, 52-7.
(40) McGuckin M, Kerstein MD. Venous leg ulcers and the family physician. Adv Wound Care 1998 November 1;11(7):344-6.
(41) Amlung SR, Miller WL, Bosley LM. The 1999 National Pressure Ulcer
Prevalence Survey: a benchmarking approach. Adv Skin Wound Care 2001
November 1;14(6):297-301.
(42) Rawlings RB, Stallings TJ, Riley JB, Jr., Brown TC, Jr. Health reform for
hospitals and health systems. McGuireWoods 2010 April 14.
(43) Epstein AM. Revisiting readmissions--changing the incentives for
shared accountability. N Engl J Med 2009 April 2;360(14):1457-9.
(44) Favole JA. Readmitted patients cost billions. Wall St J 2009 April 2.
(45) Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009 April
2;360(14):1418-28.
(46) Morrison I. Flip the switch. HHN Magazine 2010 July 5;Available at: URL: http://www.hhnmag.com/hhnmag_app/jsp/articledisplay.
jsp?dcrpath=HHNMAG/Article/data/07JUL2010/070510HHN_Weekly_
Morrison&domain=HHNMAG. AccessedJanuary 17, 2011.
(47) Health Care Reform. www nhha org 2011 January 17;Available at:
URL: http://nhha.org/nhha/healthcare_reform/index.php.
(48) Super N. What health care reform means to Medicare. (Presented at
Health Care Summit, August 30-31, 2010, Charleston, WV). 8-30-2010.
AARP.
(49) Davis PA, Hahn J, Morgan PC, Stockdale H, Stone J, Tilson S. Medicare provisions in PPACA (P.L. 111-148). Washington, D.C.: Congressional
Research Service; 2010 Apr 21. Report No.: R4116.
(50) Centers for Medicare and Medicaid Services (CMS) H. Roadmap for
quality measurement in the traditional medicare fee-for-service program.
Washington, D.C.: U.S. Department of Health and Human Services; 2009
Jan 1.
(51) Centre for Health Economics. Economic evaluation of health technologies. 4-19-2010. York, UK, The University of York.
(52) Schwien T, Gilbert J, Lang C. Pressure ulcer prevalence and the role
of negative pressure wound therapy in home health quality outcomes.
Ostomy Wound Manage 2005 September 1;51(9):47-60.
1;8(1):22-32.
(59) Moues CM, Van Den Bemd GJ, Meerding WJ, Hovius SE. An economic evaluation of the use of TNP on full-thickness wounds. J Wound
Care 2005 May 1;14(5):224-7.
(60) Song DH, Miller E, Keith M. A cost-effectiveness evaluation of vacuum-assisted closure* treatment for hospitalized dehisced chest wound
patients. Presented at the 2006 SAWC Meeting, April 30-May 3, San Antonio, TX , S146. 4-30-2006.
( 61) Page JC, Newswander B, Schwenke DC, Hansen M, Ferguson J. Retrospective analysis of negative pressure wound therapy in open foot wounds
with significant soft tissue defects. Adv Skin Wound Care 2004 September
1;17(7):354-64.
(62) De Leon JM, Nagel M, Fudge M et al. Early use of negative pressure
wound therapy in long-term acute care patients is associated with reduced
length of stay. Presented at the Third Congress of the World Union of
Wound Healing Societies, June 4-8, 2008, Toronto, Ontario. PF225. 6-42008.
(63) Driver VR, De Leon JM. Health economic implications for wound care
and limb preservation. J Manag Care Med 2008 January 1;11(1):13-9.
(64) Flack S, Apelqvist J, Keith M, Trueman P, Williams D. An economic
evaluation of VAC therapy compared with wound dressings in the treatment of diabetic foot ulcers. J Wound Care 2008 February 1;17(2):71-8.
( 65) Page JC, Newswander B, Schwenke DC, Hansen M, Ferguson J. Negative pressure wound therapy in open foot wounds with significant soft
tissue defects. Ostomy Wound Manage 2005 February 1;51(2A Suppl):9S14S.
(66) Gabriel A, Thimmappa B, Rubano C, Storm-Dickerson T. Ultra-light,
single-patient-use negative pressure wound therapy device as a bolster
over split-thickness skin grafts. (Abstract presented at: Symposium on Advanced Wound Care Spring Meeting, April 14-17, 2011, Dallas, TX). 1213-2010.
(67)American Diabetes Association. Economic costs of diabetes in the
U.S. In 2007. Diabetes Care 2008;31:596-615.
(68)Driver VR, Fabbi M, Lavery LA, Gibbons G. The costs of diabetic
foot: the economic case for the limb salvage team. J Vasc Surg 2010;52:
17S-22S.
(53) Philbeck TE, Jr., Whittington KT, Millsap MH, Briones RB, Wight DG,
Schroeder WJ. The clinical and cost effectiveness of externally applied
negative pressure wound therapy in the treatment of wounds in home
healthcare Medicare patients. Ostomy Wound Manage 1999 November
1;45(11):41-50.
(54) Baharestani MM, Houliston-Otto DB, Barnes S. Early versus late initiation of negative pressure wound therapy: examining the impact on home
care length of stay. Ostomy Wound Manage 2008 November 1;54(11):4853.
(55) Frykberg RG, Williams DV. Negative-pressure wound therapy and diabetic foot amputations: a retrospective study of payer claims data. J Am
Podiatr Med Assoc 2007 September 1;97(5):351-9.
(56) Apelqvist J, Armstrong DG, Lavery LA, Boulton AJ. Resource utilization and economic costs of care based on a randomized trial of vacuumassisted closure therapy in the treatment of diabetic foot wounds. Am J
Surg 2008 June 1;195(6):782-8.
(57) Flack SM, Apelqvist J, Trueman P, Keith MS, Williams DV. The costeffectiveness of vacuum assisted closure (V.A.C.) therapy for the treatment
of diabetic foot wounds. Presented at the ISPOR Twelfth Annual International Meeting, May 19-23, 2007, Arlington, VA. A62. 5-19-2007.
(58) Whitehead SJ, Forest-Bendien VL, Richard JL, Halimi S, Ha Van G,
Trueman P. Economic evaluation of Vacuum Assisted Closure Therapy for
the treatment of diabetic foot ulcers in France. Int Wound J 2011 January
19
Attachment 1: Comparison Chart of V.A.C.® Therapy Products
InfoV.A.C.®
Therapy System
ActiV.A.C.®
Therapy System
New V.A.C.Via™
Therapy System
Product acquisition
Daily rental
Covered under a DME HCPC Code
for NPWT; paid for by Patient’s
Third Party Payer
Purchased
Size of therapy unit
Wt: 2.7 kg/5.9 lbs; Dim: 23
cm/ 9.05" x 17 cm/6.69" x 17
cm/6.69"
Wt: 1.08 kg/2.4 lbs; Dim: 19.33
cm/7.6" x 15.2 cm/6" x 6.4
cm/2.5"
Wt: 0.5 kg/<1 lb; Dim: 17 cm/6.8”
x 6 cm/3.9” x 10 cm/2.4”
Portability of therapy unit
Hangs on IV pole or attached to
end of bed
Carrying case worn as belt
Carrying case with belt clip and/or
lanyard
Number of uses for therapy
device
Multiple patient use
Multiple patient use
Single patient use
Noise level of therapy unit
during operation
Low noise
Low noise
Virtually silent
Flow Rate
Dressing draw down; ~6L per
minute
Dressing draw down; ~6L per
minute
Dressing draw down; ~0.53L per
minute
Ease of use of therapy unit
Multiple steps interface
Multiple step interface
Single step interface
Ease of dressing application
GranuFoam and V.A.C. Drape
™
®
20 V.A.C.Via™ Therapy System Monograph | DSL#11-0039.US (3/11)
GranuFoam and V.A.C. Drape
™
®
All-in-One dressing package:
Enhanced V.A.C.® Drape, 3M™
Cavilion™ No Sting Barrier Film and
Spiral GranuFoam™ Dressing
21
V.A.C.Via™ Therapy System
Monograph
NOTE: Specific indications, contraindication, warnings, precautions and safety information exist for KCI
products and therapies. Please consult a physician and product instructions for use prior to application.
CAUTION: Federal law restricts this device to sale by or on the order of a physician
Follow local institutional protocols for infection control and waste disposal procedures. Local protocols should be based on the
applicable federal, state and/or local government environmental regulations.
©2011 KCI Licensing, Inc., All rights reserved. 3M and Tegaderm are trademarks of 3M Company. Unless otherwise indicated, all other trademarks
designated herein are proprietary to KCI Licensing, Inc., its affiliates and/or licensors. For US use only. DSL#11-0039.US • REV. 3/11• LIT# 29-A-208