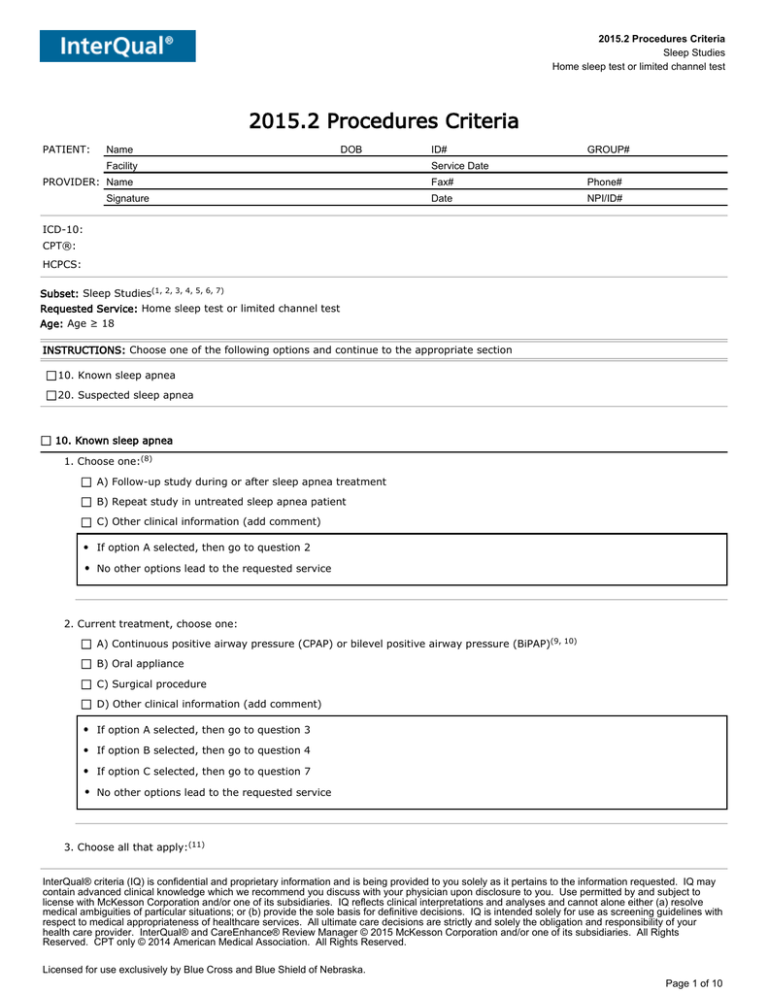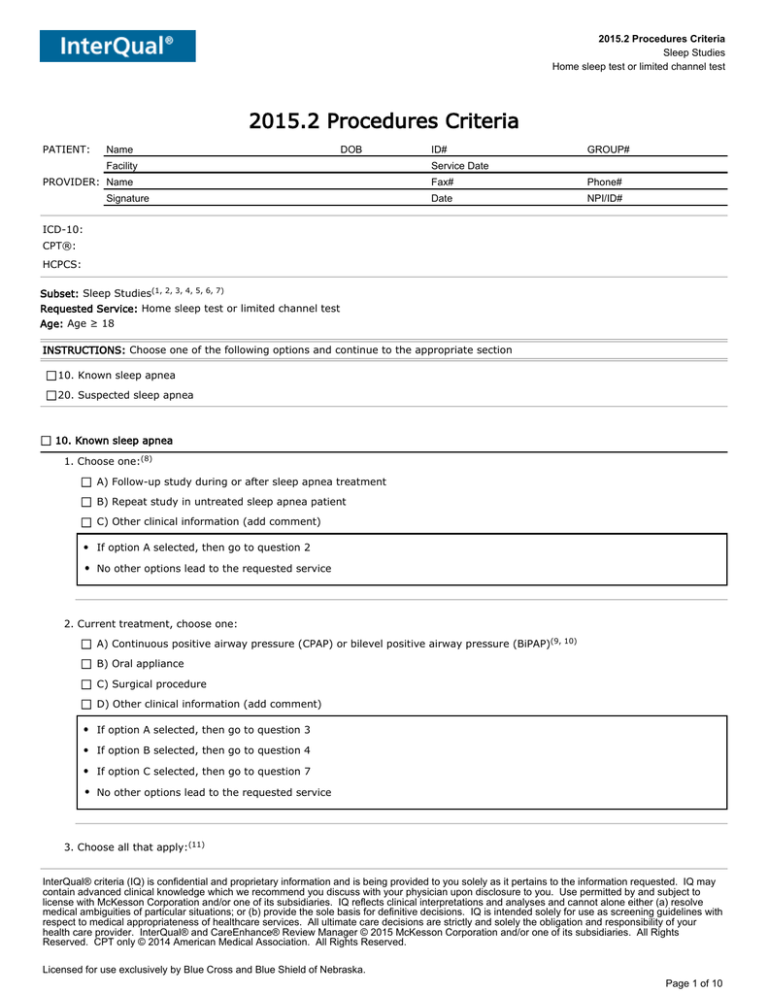
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
2015.2 Procedures Criteria
PATIENT:
Name
DOB
Facility
PROVIDER: Name
Signature
ID#
GROUP#
Service Date
Fax#
Phone#
Date
NPI/ID#
ICD-10:
CPT®:
HCPCS:
Subset: Sleep Studies(1, 2, 3, 4, 5, 6, 7)
Requested Service: Home sleep test or limited channel test
Age: Age ≥ 18
INSTRUCTIONS: Choose one of the following options and continue to the appropriate section
10. Known sleep apnea
20. Suspected sleep apnea
10. Known sleep apnea
1. Choose one:(8)
A) Follow-up study during or after sleep apnea treatment
B) Repeat study in untreated sleep apnea patient
C) Other clinical information (add comment)
If option A selected, then go to question 2
No other options lead to the requested service
2. Current treatment, choose one:
A) Continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP)(9, 10)
B) Oral appliance
C) Surgical procedure
D) Other clinical information (add comment)
If option A selected, then go to question 3
If option B selected, then go to question 4
If option C selected, then go to question 7
No other options lead to the requested service
3. Choose all that apply:(11)
InterQual® criteria (IQ) is confidential and proprietary information and is being provided to you solely as it pertains to the information requested. IQ may
contain advanced clinical knowledge which we recommend you discuss with your physician upon disclosure to you. Use permitted by and subject to
license with McKesson Corporation and/or one of its subsidiaries. IQ reflects clinical interpretations and analyses and cannot alone either (a) resolve
medical ambiguities of particular situations; or (b) provide the sole basis for definitive decisions. IQ is intended solely for use as screening guidelines with
respect to medical appropriateness of healthcare services. All ultimate care decisions are strictly and solely the obligation and responsibility of your
health care provider. InterQual® and CareEnhance® Review Manager © 2015 McKesson Corporation and/or one of its subsidiaries. All Rights
Reserved. CPT only © 2014 American Medical Association. All Rights Reserved.
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 1 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
10. Known sleep apnea (Continued...)
A) Continued or worsening or recurrent symptoms or findings
B) Weight loss or gain ≥ 10% body mass index (BMI)
C) Other clinical information (add comment)
If option B selected and option A not selected and option C not selected, then the rule is satisfied; you may stop here
(Outpatient)
No other options lead to the requested service
4. Choose all that apply:(12)
A) Final fit of appliance completed
B) Continued or worsening or recurrent symptoms or findings
C) Other clinical information (add comment)
If option A selected and option B not selected and option C not selected, then go to question 5
No other options lead to the requested service
5. Choose one:
A) Central sleep apnea or hypoventilation disorder(13, 14)
B) Obesity hypoventilation syndrome(15)
C) Co-existing sleep disorder(16)
D) Moderate to severe pulmonary disease(17)
E) Neuromuscular disease(17)
F) Heart failure (HF)(17)
G) Impaired dexterity or mobility(17)
H) Cognitive impairment(17)
I) None of the above, more choices
If option I selected, then go to question 6
No other options lead to the requested service
6. Home sleep test or limited channel test planned
Yes
No
If option Yes selected, then the rule is satisfied; you may stop here (Outpatient)
No other options lead to the requested service
7. Choose all that apply:
A) Moderate or severe preoperative sleep apnea(18)
B) Continued or worsening or recurrent symptoms or findings(19)
C) Other clinical information (add comment)
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 2 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
10. Known sleep apnea (Continued...)
If option A selected and option B not selected and option C not selected, then go to question 8
No other options lead to the requested service
8. Choose one:
A) Central sleep apnea or hypoventilation disorder(13, 14)
B) Obesity hypoventilation syndrome(15)
C) Co-existing sleep disorder(16)
D) Moderate to severe pulmonary disease(17)
E) Neuromuscular disease(17)
F) Heart failure (HF)(17)
G) Impaired dexterity or mobility(17)
H) Cognitive impairment(17)
I) None of the above, more choices
If option I selected, then go to question 9
No other options lead to the requested service
9. Home sleep test or limited channel test planned
Yes
No
If option Yes selected, then the rule is satisfied; you may stop here (Outpatient)
No other options lead to the requested service
20. Suspected sleep apnea
1. Choose one:
A) Symptoms or findings during sleep OR during sleep AND during the day
B) Unexplained excessive daytime sleepiness(20)
C) Other clinical information (add comment)
If option A selected, then go to question 2
If option B selected, then go to question 7
No other options lead to the requested service
2. Choose all that apply:(21)
A) Snoring
B) Gasping or choking
C) Irregular breathing pattern or witnessed apnea(22, 23)
D) Frequent awakenings(24)
E) Other clinical information (add comment)
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 3 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
20. Suspected sleep apnea (Continued...)
If 2 or more options A, B, C or D selected and option E not selected, then go to question 3
If the number of options selected is 1 and option E not selected, then go to question 6
No other options lead to the requested service
3. Choose one:
A) Suspected obstructive sleep apnea(8)
B) Suspected central sleep apnea or hypoventilation disorder(13, 14)
C) Suspected obesity hypoventilation syndrome(15)
D) Suspected or known co-existing sleep disorder(16)
E) Other clinical information (add comment)
If option A selected, then go to question 4
No other options lead to the requested service
4. Choose one:(17)
A) Moderate to severe pulmonary disease
B) Neuromuscular disease
C) Heart failure (HF)
D) Impaired dexterity or mobility
E) Cognitive impairment
F) Nondiagnostic or unsuccessful home sleep test or limited channel test
G) None of the above, more choices
If option G selected, then go to question 5
No other options lead to the requested service
5. Home sleep test or limited channel test planned
Yes
No
If option Yes selected, then the rule is satisfied; you may stop here (Outpatient)
No other options lead to the requested service
6. Choose all that apply:
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 4 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
20. Suspected sleep apnea (Continued...)
A) Excessive daytime sleepiness(20)
B) Fatigue(25)
C) Irritability or moodiness(26)
D) Morning headaches(27)
E) Decreased concentration or memory loss(28)
F) Increased neck circumference (> 17 inches in men or > 16 inches in women)(29)
G) Hypertension (HTN)(30)
H) Other clinical information (add comment)
If 1 or more options A, B, C, D, E, F or G selected and option H not selected, then go to question 3
No other options lead to the requested service
7. Choose all that apply:
A) Impairment of job performance
B) Safety compromised
C) Symptoms interfere with ADLs ≥ 8 weeks(28)
D) Other clinical information (add comment)
If 1 or more options A, B or C selected and option D not selected, then go to question 8
No other options lead to the requested service
8. Choose all that apply:(31)
A) Medical conditions considered and treated if indicated
B) Behavioral health disorder considered and treated if indicated
C) Medications deemed noncontributory
D) Substance use disorder excluded
E) Other clinical information (add comment)
If the number of options selected is 4 and option E not selected, then go to question 9
No other options lead to the requested service
9. Choose one:
A) Suspected obstructive sleep apnea(8)
B) Suspected central sleep apnea or hypoventilation disorder(13, 14)
C) Suspected obesity hypoventilation syndrome(15)
D) Suspected or known co-existing sleep disorder(16)
E) Other clinical information (add comment)
If option A selected, then go to question 10
No other options lead to the requested service
10. Choose one:(17)
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 5 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
20. Suspected sleep apnea (Continued...)
A) Moderate to severe pulmonary disease
B) Neuromuscular disease
C) Heart failure (HF)
D) Impaired dexterity or mobility
E) Cognitive impairment
F) Nondiagnostic or unsuccessful home sleep test or limited channel test
G) None of the above, more choices
If option G selected, then go to question 11
No other options lead to the requested service
11. Home sleep test or limited channel test planned
Yes
No
If option Yes selected, then the rule is satisfied; you may stop here (Outpatient)
No other options lead to the requested service
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 6 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
Notes
(1)
I/O Setting: Outpatient
(2)
These criteria include the following procedures:
Facility-based polysomnogram (PSG)
Home sleep test
Limited channel sleep test
Multiple sleep latency test (MSLT)
Polysomnogram (PSG)
(3)
A facility-based or attended polysomnogram (PSG) using a type I monitoring device is the gold standard for the diagnosis of sleeprelated breathing disorders, narcolepsy, idiopathic hypersomnia, parasomnia, and sleep-related movement disorders. These studies
include full sleep staging with electroencephalogram (EEG) and limb electromyelogram (EMG) for the detection of movement disorders.
In addition, electrooculogram (EOG), electrocardiogram (ECG), chin EMG, respiratory effort of the chest and abdominal wall, nasal
airflow, and pulse oximetry are monitored, and additional channels for continuous positive airway pressure, video, and other measures
can be utilized. A type II monitoring device is similar to the type I except that it may be performed in the home setting. The routine
use of type II devices is not currently recommended by the American Academy of Sleep Medicine (Jafari and Mohsenin, Clin Chest Med
2010, 31: 287-97; Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(4)
A facility-based polysomnogram (PSG) is necessary to titrate continuous positive airway pressure (CPAP) in a laboratory setting over a
2-night period. A split-night sleep study is a variation of the standard PSG in which the diagnostic PSG and CPAP titration are
completed in one night (Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(5)
A home sleep test is performed most commonly using a type III or IV portable monitor. A type III device monitors a minimum of four
channels that include respiratory movement and airflow, electrocardiogram (ECG) and heart rate, and oxygen saturation. A type IV
device monitors three channels that include arterial oxygen saturation and airflow or abdominal and chest wall movement.
A portable monitor is appropriate for the diagnosis of obstructive sleep apnea in patients with a high pretest probability of moderate to
severe disease and no major comorbid sleep or medical disorders that would compromise the quality of the test results (e.g., moderate
to severe pulmonary disease, heart failure, neuromuscular disease). Portable monitors may also be used to monitor a patient's
response to noncontinuous positive airway pressure treatments (e.g., oral appliances, upper airway surgery) (Fleetham et al., Can
Respir J 2011, 18: 25-47; Epstein et al., J Clin Sleep Med 2009, 5: 263-76; Collop et al., J Clin Sleep Med 2007; 3(7): 737-747;
Kushida et al., Sleep 2005; 28(4): 499-521).
(6)
Multiple sleep latency test (MSLT) is used to assist in the diagnosis of narcolepsy and idiopathic hypersomnia. The recording equipment
used during the MSLT consists minimally of electorencephalogram (EEG) (central and occipital), bilateral electrooculograms (EOG),
mental or submental electromyelogram (EMG), and electrocardiogram (ECG). The test quantifies excessive daytime sleepiness in the
controlled environment of a sleep laboratory. MSLT is performed following the polysomnogram (PSG) to quantify the time it takes a
patient to fall asleep and to determine if there are rapid eye movement episodes. Patients are given four or five opportunities to fall
asleep every two hours over the course of a day. It is recommended that patients have at least six hours of sleep prior to the MSLT
and that a split night sleep study (i.e., PSG and CPAP titration during the study period) not be done before the test.
(7)
InterQual® criteria are derived from the systematic, continuous review and critical appraisal of the most current evidence-based
literature and include input from our independent panel of clinical experts. The content is based on a variety of references which are
cited at specific criteria points throughout the subset.
(8)
Obstructive sleep apnea (OSA) is characterized by repetitive upper respiratory airway closure and increased resistance during sleep.
Multiple levels of the aerodigestive track may be involved and can include nasal, hypopharyngeal, nasopharyngeal, oropharyngeal, and
laryngeal contributors. OSA may be treated with positive airway pressure, oral appliances, or surgery (Freedman, Clin Chest Med 2010,
31: 187-201; McDaid et al., Sleep Med Rev 2009, 13: 427-36).
(9)
Sleep apnea should be re-evaluated when fatigue, daytime somnolence, or snoring persists. The American College of Physicians, the
American Academy of Sleep Medicine, and others agree that continuous positive airway pressure (CPAP) is the treatment of choice for
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 7 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
obstructive sleep apnea (OSA) and should be attempted in all patients (Qaseem et al., Ann Intern Med 2013; Aurora, Sleep 2010, 33:
1408-1413; Freedman, Clin Chest Med 2010, 31: 187-201; Epstein et al., J Clin Sleep Med 2009, 5: 263-76). CPAP has been shown to
be better than placebo and positional therapy in improving sleep-disordered breathing and rapid eye movement sleep across the
spectrum of disease severity (Freedman, Clin Chest Med 2010, 31: 187-201). PAP therapy does not cure OSA and symptomatology is
likely to recur after CPAP is discontinued.
(10)
Continuous positive airway pressure (CPAP) is the first-line treatment for patients with obstructive sleep apnea (Qaseem et al., Ann
Intern Med 2013; Epstein et al., J Clin Sleep Med 2009, 5: 263-76). Bilevel positive airway pressure (BiPAP) may be indicated for
patients who do not tolerate CPAP, when high pressure is needed for patients who experience difficulty with exhalation, or in patients
who have concomitant central hypoventilation (Kushida et al., Sleep 2006; 29(3): 375-380).
(11)
A follow-up polysomnogram may be appropriate to assess the impact of substantial weight change (e.g., greater than 10% of total
body weight) on continuous positive airway pressure (CPAP) requirements (Epstein et al., J Clin Sleep Med 2009, 5: 263-76). A patient
who experiences significant weight loss may have improvement or resolution of their sleep apnea symptoms and may be able to
discontinue CPAP after confirmation with a home sleep test. A patient with significant weight gain may require a titration study.
(12)
Oral appliances, including mandibular advancement devices, are indicated for the treatment of mild to moderate obstructive sleep
apnea in patients who prefer an oral appliance to continuous positive airway pressure (CPAP), cannot tolerate CPAP, do not improve
with CPAP, or are not an appropriate candidate for CPAP (Qaseem et al., Ann Intern Med 2013; Epstein et al., J Clin Sleep Med 2009,
5: 263-76; Kushida et al., Sleep 2006; 29(3): 375-380). All patients should undergo a follow-up sleep study after the final fitting of the
appliance to ensure optimal therapeutic efficacy (Epstein et al., J Clin Sleep Med 2009, 5: 263-76; Kushida et al., Sleep 2006; 29(3):
375-380).
(13)
Central sleep apnea is characterized by a cyclical or intermittent reduction or absence of respiratory effort. Central sleep apnea may be
idiopathic or associated with medical or neurological conditions, medications, or substance use. Treatment-emergent central sleep
apnea, previously referred to as complex sleep apnea, presents when central apnea or hypopnea appear after the initiation of positive
airway pressure treatment (International Classification of Sleep Disorders. 2014).
(14)
Sleep related hypoventilation disorders are characterized by insufficient ventilation that results in hypercapnia during sleep. The causes
of hypoventilation include genetic disorders, medication, medical conditions (e.g., lung disease, pulmonary vascular pathology, chest
wall disorder, muscle weakness, neurologic disorder (International Classification of Sleep Disorders. 2014).
(15)
2
Patients with obesity hypoventilation syndrome have a body mass index greater than 30 kg/m and experience hypercapnia that
causes hypoxemia when awake and asleep. They may also have co-existing sleep disordered breathing, most commonly obstructive
sleep apnea (International Classification of Sleep Disorders. 2014; Ioachimescu and Collop, Neurol Clin 2012, 30: 1095-136).
(16)
Patients with suspected obstructive sleep apnea (OSA) who have a co-existing sleep disorder (e.g., narcolepsy, idiopathic hypersomnia,
periodic limb movement disorder of sleep, parasomnias) should undergo facility-based polysomnogram, rather than a home sleep
test, to confirm the diagnosis of OSA (Collop et al., J Clin Sleep Med 2007; 3(7): 737-747).
(17)
Patients with significant comorbid medical conditions (e.g., moderate to severe pulmonary disease, neuromuscular disease, heart
failure) are generally not considered appropriate candidates for home sleep testing due to the inability to obtain accurate test results
(Fleetham et al., Can Respir J 2011, 18: 25-47; Epstein et al., J Clin Sleep Med 2009, 5: 263-76; Collop et al., J Clin Sleep Med 2007;
3(7): 737-747). Additionally, patients with cognitive impairment or impaired dexterity or mobility are not appropriate for an
unattended study and require a facility-based polysomnogram.
(18)
The success of surgical procedures (e.g., uvulopalatopharyngoplasty (UPPP), maxillomandibular advancement, tonsillectomy) for
obstructive sleep apnea is variable and does not consistently resolve sleep apnea symptoms. Patients with moderate to severe
pretreatment sleep apnea should undergo a follow-up polysomnogram to determine the efficacy of the procedure or the need for
additional treatment modalities (e.g., CPAP) (Aurora, Sleep 2010, 33: 1408-1413; Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(19)
Polysomnogram should be performed in patients who experience symptoms during use of their oral appliance or those who continue to
experience symptoms after a pharyngeal procedure in order to determine if additional treatment measures are needed (Epstein et al., J
Clin Sleep Med 2009, 5: 263-76).
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 8 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
(20)
Excessive daytime sleepiness is characterized by daytime sleepiness with inappropriate or irresistible naps throughout the day. Patients
may complain of the inability to function at optimum levels during the day, have difficulty concentrating, or may perform poorly at
work or school. This degree of sleepiness interferes with ADLs.
(21)
Often it is the patient's significant other who first recognizes an abnormal sleep pattern. They may witness gasping or choking,
irregular breathing, or even periods of apnea. Habitual snoring is a classic finding in obstructive sleep apnea, although it is not
universal. Furthermore, patients who snore may not have sleep apnea. Patients with sleep disruptions with or without daytime
symptoms should receive further evaluation.
(22)
An irregular breathing pattern, such as Cheyne-Stokes respiration, may be associated with moderate to severe heart failure and central
sleep apnea. Patients have apneic episodes followed by periods of hyperventilation that continually cycle during sleep.
(23)
Apnea occurs when a patient's breathing nearly or completely stops for periods of ten seconds or more.
(24)
Frequent awakenings during sleep which result in poor sleep quality are often seen in patients with obstructive and central sleep apnea
(Ioachimescu and Collop, Neurol Clin 2012, 30: 1095-136; Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(25)
Fatigue can be seen in varying degrees in both obstructive and central sleep apnea and is described as a lack of energy, poor
concentration, or tiredness (Ioachimescu and Collop, Neurol Clin 2012, 30: 1095-136).
(26)
Personality changes, such as new moodiness or irritability, may be a consequence of persistent sleep deprivation or chronic fragmented
sleep.
(27)
Morning headaches, which are often described as throbbing and frontal or temporal, typically resolve within one to two hours of
awakening and are suggestive of sleep apnea. Other etiologies of morning headaches should always be considered, including
intracranial masses and increased intracranial pressure. The morning headaches from sleep apnea result from prolonged periods of
hypercapnia and hypoxemia.
(28)
Patients may report the inability to function at optimum levels during the day, have difficulty concentrating, or have memory loss
(Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(29)
Increased neck circumference, defined as greater than 16 inches in women or 17 inches in men, may contribute to the development of
obstructive sleep apnea (Chung et al., Br J Anaesth 2012, 108: 768-75; Ioachimescu and Collop, Neurol Clin 2012, 30: 1095-136;
Epstein et al., J Clin Sleep Med 2009, 5: 263-76).
(30)
Hypertension (HTN) is associated with cardiovascular morbidity and there is increasing evidence that there is a significant relationship
between resistant hypertension and obstructive sleep apnea. Patients with HTN should undergo sleep testing if they exhibit nighttime
symptoms or if they remain hypertensive in spite of medical therapy (Khan et al., Int J Hypertens 2013, 2013: 193010; Epstein et al.,
J Clin Sleep Med 2009, 5: 263-76).
(31)
Patient history and physical examination should exclude other conditions that may cause excessive daytime sleepiness (e.g., poor sleep
habits, medical conditions, medication, drugs, alcohol, behavioral health disorders) (Harris et al., Neurol Clin 2012, 30: 1027-44).
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 9 of 10
2015.2 Procedures Criteria
Sleep Studies
Home sleep test or limited channel test
ICD-10-CM (circle all that apply): F51.8, G47.10, G47.30, G47.31, G47.33, G47.37, G47.39, G47.411, G47.419, G47.421, G47.429,
G47.50, G47.51, G47.52, G47.54, G47.61, G47.8, G47.9, I10, R06.3, R06.83, R06.89, R41.2, R41.3, R44.0, R44.1, R44.2, R44.3,
R45.4, R51, R53.83, Other___________
CPT® (circle all that apply): 95800, 95801, 95806, Other___________
HCPCS (circle all that apply): G0398, G0399, G0400, Other___________
Licensed for use exclusively by Blue Cross and Blue Shield of Nebraska.
Page 10 of 10