Technological Advances in the Management of Unruptured
Intracranial Aneurysms Fail to Improve Outcome in
New York State
Brad E. Zacharia, MD; Andrew F. Ducruet, MD; Zachary L. Hickman, MD;
Bartosz T. Grobelny, MD; Neeraj Badjatia, MD; Stephan A. Mayer, MD; Mitchell F. Berman, MD;
Robert A. Solomon, MD; E. Sander Connolly, Jr, MD
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Background and Purpose—Unruptured intracranial aneurysms (UIAs) are being identified more frequently and
endovascular coil embolization has become an increasingly popular treatment modality.
Our study evaluates patient outcomes with changing patterns of treatment of UIA.
Methods—We conducted a retrospective, longitudinal cohort study of 3132 hospital discharges for UIA identified from the
New York Statewide Database (SPARCS) in 2005 to 2007 and 2200 discharges from 1995 to 2000. The rates of
endovascular coiling and surgical clipping were examined along with hospital variables and discharge outcome.
Anatomic specifics of UIA were unavailable for analysis.
Results—The case rate for treatment of UIA doubled from 1.59 (1995 to 2000) to 3.45 per 100 000 (2005 to 2007,
P⬍0.0001) and increased in the case treatment rate for coiling of UIA (0.36 versus 1.98 per 100 000, P⬍0.0001).
Compared with the old epoch, there were more UIAs clipped at high-volume centers (55.8% versus 78.8%, P⬍0.0001)
but fewer coiled at high-volume centers (94.8% versus 84.5%, P⬍0.0001) in the new epoch. Coiling and increasing
hospital UIA treatment volume were associated with good discharge outcome. However, there was no significant
improvement in overall good outcome when comparing 1995 to 2000 versus 2005 to 2007 (79% versus 81%, P⫽0.168)
and a worsening of good outcomes for clipping (76.3% versus 71.7%, P⫽0.0132).
Conclusions—Despite coiling being associated with an increased incidence of good outcome relative to clipping of UIA,
the increase in coiling has failed to improve overall patient outcome. The shift in coiling venue from high-volume
centers to low-volume centers and decreasing microsurgical volume accompanied by a worsening in microsurgical
results contribute to this. This argues for greater centralization of care. (Stroke. 2011;42:2844-2849.)
Key Words: clipping 䡲 coiling 䡲 interventional neuroradiology 䡲 intracranial aneurysm 䡲 neurosurgery
U
nruptured intracranial aneurysms (UIAs) are relatively
common lesions, occurring in approximately 2% of the
general population, suggesting that ⬎15 million individuals
are affected in the United States alone.1–3 With increased use
of advanced brain imaging, incidental UIAs are being diagnosed with greater frequency.2 As such, an understanding of
evolving treatment paradigms for UIA is critical. In light of
2002, 2005, and 2009 results from the International Subarachnoid Aneurysm Trial (ISAT), a prospective, multicenter,
randomized study, major changes in treatment patterns
have occurred, favoring endovascular coiling over surgical
clipping for ruptured aneurysms amenable to both treatment modalities.4 – 6 Although the ISAT results are not
readily extrapolated to patients with UIA and no similar
prospective, randomized trial has been performed for UIA,
multiple studies demonstrate that an increasing percentage
of patients are undergoing endovascular coiling for the
treatment of UIA.7–16 Many of these studies have also
demonstrated improved outcomes in those patients undergoing endovascular versus surgical management. Nevertheless, overall outcome for UIA treatment remains largely
unchanged.7
Given our experience at a high-volume cerebrovascular
center, we hypothesize that a decentralization of endovascular
treatment of cerebral aneurysms to low-volume centers with
relatively less procedural experience and lack of comprehensive cerebrovascular programs may account for the
lack of improvement in observed outcomes despite an
increase in endovascular management. To this end, we
examined patient- and hospital-related factors after treatment of UIA using 8 years of New York State hospital
discharge data.
Received April 4, 2011; final revision received May 5, 2011; accepted May 6, 2011.
From the Department of Neurological Surgery (B.E.Z., A.F.D., Z.L.H., B.T.G., R.A.S., E.S.C.), THE Division of Critical Care Neurology (N.B.,
S.A.M.), and the Division of Neuroanesthesia (M.F.B.), Department of Anesthesiology, Columbia University, New York, NY.
Correspondence to Brad E. Zacharia, MD, Department of Neurological Surgery, Neurological Institute of New York, Columbia University Medical
Center, 710 W 168th Street, New York, NY 10032. E-mail Bez2103@columbia.edu
© 2011 American Heart Association, Inc.
Stroke is available at http://stroke.ahajournals.org
DOI: 10.1161/STROKEAHA.111.619767
2844
Zacharia et al
Trends in Unruptured Cerebral Aneurysm Treatment
2845
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Methods
Results
We reviewed data obtained from the New York Statewide Planning
And Research Cooperative System (SPARCS). SPARCS is a major
management tool assisting hospitals, agencies, and healthcare organizations with decision-making in relation to financial planning and
monitoring of inpatient and ambulatory surgery services and costs in
New York State. SPARCS currently collects patient-level details for
every hospital discharge, ambulatory surgery patient, and emergency
department admission in New York State as coded from admission
and billing records. This study was approved by the Institutional
Review Board of Columbia University Medical Center.
We used 1995 to 2000 and 2005 to 2007 SPARCS data to study
treatment trends for UIA and ruptured intracranial aneurysms before
and after the 2002 publication of the original ISAT study, although
the majority of our study focuses on UIA. The database records
diagnoses and procedures according to the International Classification of Diseases, 9th Revision17 and provides patient demographic
information and discharge destination. Using an accepted search
strategy, the following International Classification of Diseases, 9th
Revision–Clinical Modification codes were used for data query: 430
(subarachnoid hemorrhage), 437.3 (unruptured cerebral aneurysm),
39.51 (clipping of cerebral aneurysm), and 39.72 (endovascular
repair or occlusion of head and neck vessels). We analyzed solely the
primary procedure to parallel an intention-to-treat analysis. Temporal differences in discharge coding demanded a slightly altered initial
search strategy in the data set from 1995 to 2000, which has been
published previously by our group.10 The analysis involved patient
demographic variables (gender, race, age, ethnicity) and hospitalspecific characteristics, for example, admission source, percent
endovascular coiling, and treatment volume. New York State Census
data were used to calculate case rates for UIA treatment.
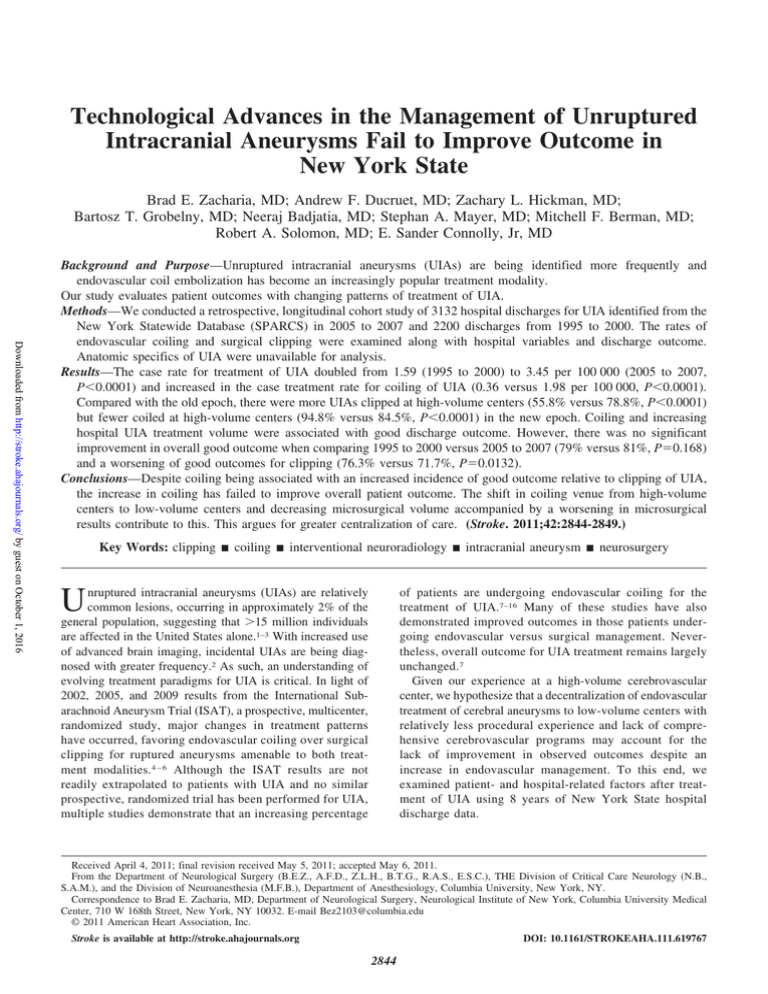
During the 6-year period from 1995 to 2000, there were 5656
patients and from 2005 to 2007 there were 4056 patients who
underwent surgical and or endovascular treatment with a
primary diagnosis of either a ruptured or unruptured intracranial aneurysm. When corrected for population changes, the
case rate for treatment from 1995 to 2000 was 5.04 per
100 000 compared with 7.02 per 100 000 in 2005 to 2007. In
the old epoch, 4917 patients underwent surgical clipping
versus 1894 in the most recent epoch for case treatment rates
of 4.38 and 3.27 per 100 000, respectively. In the old epoch,
739 patients underwent endovascular coiling versus 2162 in
the most recent epoch representing an almost 6-fold increase
in the case treatment rate from 0.66 to 3.74 per 100 000
(Figure 1A). The per annum rate of overall surgical clipping
(ruptured and unruptured) has decreased substantially from
819.5 cases in the old epoch to 631.3 in the new epoch.
When looking specifically at those patients with UIA, we
see similar trends in case treatment rates between the 2
epochs with an overall case treatment rate of 1.79 per 100 000
in the old epoch compared with 3.45 per 100 000 in the new
epoch (Figure 1B). Of those patients definitively treated for
UIA, 57% underwent endovascular coiling in the most recent
epoch versus 20.3% in the prior epoch (P⬍0.0001; Figure
1C). Compared with the old epoch, there were more UIAs
being surgically clipped in high-volume centers in the new
epoch (55.8% versus 78.8%, P⬍0.0001) but fewer were
undergoing endovascular coiling in high-volume centers
(94.8% versus 84.5%, P⬍0.0001; Figure 2A). This was a
trend that continued over the most current years 2005 to 2007
(89.8%, 81.5%, 80.9%, P⫽0.0006). The percent good outcome after treatment of UIA, however, did not show any
substantial improvement between the 2 epochs (79% versus
81%, P⫽0.168; Figure 2B). When directly comparing clipping, however, we note a decrease in the percent of good
outcomes (76.3% versus 71.7%, P⫽0.0132) between the old
and new epoch, whereas the outcome for coiling remained
relatively stable (89.7% versus 87.7%, P⫽nonsignificant;
Figure 2B).
We then focused attention on the most recent epoch (2005
to 2007) whose characteristics are shown in Table 1. No
significant interactions were found. Those patients undergoing surgical clipping were younger (53.4 versus 56.1 years,
P⬍0.0001), had a greater percentage of adverse outcomes
(28.3% versus 12.3%, P⬍0.0001), and had longer lengths of
stay (6.7 versus 3.6 days, P⬍0.0001) than those undergoing
coiling (Table 2). When comparing patients with UIAs
treated at high versus low-volume centers, we noted significant differences in mean age (55.4 versus 53.1 day,
P⫽0.0027), percent adverse outcome (17.4% versus 27%,
P⬍0.0001), length of stay (4.6 versus 6.6 days, P⬍0.0001),
and the percent definitively treated through endovascular
procedures (59.3% versus 47.5%, P⬍0.0001; Table 3). We
entered all clinically relevant patient and hospital variables
into a step-forward multivariate logistic regression model
(Table 4). We identified 3 independent predictors of good
discharge outcome following treatment of UIA: white race
(OR, 1.67; P⫽0.0007), treatment volume of the hospital (OR,
1.04 per additional 10 cases; P⬍0.0001), and definitive
Statistical Analysis
Outcome measures included in-hospital death and discharge outcome. Only discharge to home was considered a good outcome given
the predominantly elective nature of surgical treatment and minimal
premorbid disability. Mortality in all cases was defined as in-hospital
death. For each hospital treating unruptured cerebral aneurysms, we
calculated the procedural volume separately for surgical clipping and
endovascular therapy of UIA during the respective time period. For
univariate analysis, we dichotomized hospitals by case volume with
the 10 highest volume hospitals classified as high volume, whereas
case volume was used in a continuous manner for multivariate
analysis. The hospital-specific propensity to coil was calculated as a
percentage of UIA treated by endovascular coiling for each center.
Categorical variables and dichotomous outcomes were evaluated
with either the Pearson 2 test or Fisher exact test, and continuous
variables and outcomes were compared using a Student t test.
Wilcoxon rank sum was used for nonparametric data when appropriate. Generalized estimating equations with independent correlation matrix structures, good outcome as the dependent variable, and
hospital as the subject variable were used to allow observations to be
clustered by hospital. This is a standard statistical technique used
when other variables and characteristics of treatment that affect
outcome are thought to exist and expected to cluster within predetermined groups.15
All variables for treated patients from 2005 to 2007(n⫽2004) with
P⬍0.25 in univariate analysis entered into a multiple logistic
regression model along with those felt to be clinically relevant,
including hospital-related variables, age, gender, and race. Using
forward stepwise multiple logistic regression, a final model was
constructed leaving only variables achieving a statistical significance
of P⬍0.05. Interactions were tested for all clinically significant
variables in the multiple logistic regression model. Similar analysis
was performed for the group of patients treated 1995 to 2000, but our
study focused on the most recent epoch.
A P value of ⬍0.05 was considered significant for all analyses.
Trend data, statistical analyses, and linear regression were performed
using commercially available software (JMP, SAS Inc, Version 7).
2846
Stroke
October 2011
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Figure 1. A, Case treatment rate for clipping and coiling of intracranial aneurysms; (B) unruptured intracranial aneurysm case treatment
rate for clipping and coiling; (C) percent UIA coiled. UIA indicates unruptured intracranial aneurysm.
treatment by endovascular coiling (OR, 3.94; P⬍0.0001).
The association of higher treatment volume with good outcome is similar in the old epoch. Older age (OR 0.61 per
10-year increase in age; P⬍0.0001) and direct admission
from the emergency room (OR, 0.41; P⫽0.0004) were
associated with a propensity toward worse outcome in our
model. Surprisingly, as percent of patients with UIAs treated
by endovascular coiling increased at a given center, the risk
for poor outcome significantly increased (OR, 0.92 per 10%
additional coiling; P⫽0.05). Analysis was repeated for clipping and coiling cohorts separately and yielded similar results
(Table 4).
Additional analysis is included in the supplemental
(http://stroke.ahajournals.org).
Discussion
Although Food and Drug Administration-approved since
1995, the use of endovascular coiling truly began to blossom
within the past decade after the initial publication of ISAT in
20024 and with population-based data indicating improved
outcomes with endovascular management of UIA.13 Nevertheless, there remains significant clinical debate regarding the
ideal treatment modality for individual patients with both
aneurysmal subarachnoid hemorrhage and UIA. Specific
clinical and aneurysm characteristics may clearly indicate
when a patient is best served by a given treatment modality,
but often there will be equipoise in benefit between surgical
and endovascular treatment. In these instances, treatment
decisions are frequently based on operator availability and
local expertise. Thus, centers able to offer a comprehensive
neurovascular team approach with both surgical and endovascular capabilities are best equipped to make treatment
decisions based primarily on patient need.
In the present study, we reviewed all hospital discharges
from New York State between 2005 and 2007 involving
treatment for UIAs and made comparisons with data from
Figure 2. A, Percent of UIA treated at high-volume centers; (B) percent good outcome after treatment for UIA. UIA indicates unruptured
intracranial aneurysm.
Zacharia et al
Table 1.
Trends in Unruptured Cerebral Aneurysm Treatment
UIA Demographic Information for 2005 to 2007
Table 3. Univariate Analysis of High- Versus Low-Volume
Treatment Centers for UIA From 2005 to 2007
UIA Demographics 2005–2007
Admissions, no.
Unruptured Intracranial
Aneurysms
3132
Mean age, y
55.4⫾14.1
Female, no. (%)
2847
High Volume
2288 (73.1)
Admissions, no.
Race, no. (%)
Mean age, y
Low Volume
1619
385
55.4⫾12.7
53.1⫾13.2
White
2125 (67.8)
Black
398 (12.7)
Adverse outcomes, no. (%)
Asian
73 (2.3)
In-hospital deaths, no. (%)
6 (0.37)
Other
362 (12.7)
Length of stay (95% CI), d
4.6 (4.3–4.9)
Unknown
174 (5.6)
Endovascular procedures, no. (%) 960 (59.3)
281 (17.4)
P
N/A
0.0027
104 (27)
⬍0.0001
5 (1.3)
0.0427
6.6 (5.8–7.4) ⬍0.0001
183 (47.5)
⬍0.0001
UIA indicates unruptured intracranial aneurysm; N/A, not applicable.
Ethnicity
Hispanic
403 (12.9)
Non-Hispanic
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
unchanged (Figure 2B). As the technology driving endovascular coiling has been refined and training programs formalized, we would have expected an improvement in coiling
outcomes, yet they have remained stagnant over the past 10
years. Conversely, although one would anticipate stable
outcomes for surgical clipping, we have demonstrated a
significant decrement in outcome over this time period
(Figure 2B).
A possible explanation for the lack of improved outcomes
with greater use of coiling and coiling’s technical refinements
over time might be the fact that increasing numbers of
unruptured aneurysms are being coiled by less experienced
teams, thereby negating the advantages of this increasingly
sophisticated technology (Figure 2A). Although other studies
have investigated the role of regionalization in aneurysm
management and demonstrated improved outcomes at higher
volume centers for both open and endovascular management
2566 (81.9)
Unknown
163 (5.2)
Treated, no. (%)
2004 (64)
Endovascular treatment, no. (%)
1143 (57)
Adverse outcomes, no. (%)
666 (21.3)
In-hospital deaths, no. (%)
18 (0.6)
Length of stay (95% CI), d
4.5 (4.3–4.7)
UIA indicates unruptured intracranial aneurysm.
1995 to 2000. Since 1995, there has been a 6-fold increase in
the treatment of UIAs driven almost completely by coiling
(Figure 1B). Coil embolization of unruptured cerebral aneurysms has been the most significant advancement in the
treatment of these lesions since the advent of the operating
microscope, yet in the 15 years after its introduction, cumulative procedural morbidity after UIA treatment has remained
Table 2.
Univariate Analysis of UIA Clipping Versus Coiling and Between-Year Univariate Analysis
Clip and Coil
Admissions, no.
Mean age, y
Female, no. (%)
Clip
2005–2007
Coil
2005–2007
861
1143
53.4⫾11.7
56.1⫾13.5
⬍0.0001
856 (74.9)
NS
628 (72.9)
Race, no. (%)
P
2005
2006
2007
668
635
701
55.3⫾12.9
494 (74)
54.6⫾12.6
472 (74.3)
55.0⫾12.9
518 (73.9)
NS
NS
⬍0.0001
NS
White
610 (70.9)
839 (73.4)
472 (70.7)
464 (73.1)
513 (72.3)
67 (9.6)
Black
100 (11.6)
122 (10.7)
86 (12.9)
69 (10.9)
Asian
20 (2.3)
21 (1.8)
11 (1.7)
12 (1.9)
18 (2.6)
Other
92 (10.7)
95 (8.4)
57 (8.6)
51 (8)
79 (11.3)
Unknown
39 (4.5)
66 (5.8)
42 (6.3)
39 (6.1)
24 (3.4)
⬍0.0001
Ethnicity
P
NS
Hispanic
119 (13.8)
114 (10)
77 (11.5)
65 (10.2)
91 (13)
Non-Hispanic
686 (79.7)
1003 (87.8)
562 (84.1)
543 (85.5)
584 (83.3)
56 (6.5)
26 (2.3)
29 (4.3)
27 (4.3)
26 (3.7)
384 (57.5)
367 (57.8)
392 (55.9)
NS
Adverse outcomes, no. (%)
244 (28.3)
141 (12.3)
⬍0.0001 133 (19.9)
121 (19.1)
131 (18.7)
NS
In-hospital deaths, no. (%)
6 (0.7)
5 (0.4)
4 (0.6)
3 (0.4)
Unknown
Coiling, no. (%)
Length of stay (95% CI), d
6.7 (6.3–7.2)
High-volume center, no. (%) 659 (76.5)
NS
3.6 (3.3–4) ⬍0.0001
960 (84)
4 (0.6)
5.4 (4.9–5.9)
⬍0.0001 558 (84.3)
UIA indicates unruptured intracranial aneurysm; NS, nonsignificant.
NS
4.6 (4.1–5.1)
4.9 (4.4–5.4)
NS
507 (79.8)
554 (79)
NS
2848
Stroke
Table 4.
October 2011
Multivariate Analysis for Good Outcome After Treatment of UIA From 2005 to 2007
Overall
P
Clip
Coil
OR*
P
⬍0.0001
0.61
⬍0.0001
0.62
0.0026
0.65
0.0007
1.67
0.0004
1.88
0.0059
1.75
Treatment volume‡
⬍0.0001
1.04
⬍0.0001
1.11
0.0013
1.03
Coil versus clip
⬍0.0001
3.94
N/A
N/A
N/A
N/A
Age†
Race (white versus all other races)
OR*
P
OR*
Percent endovascular coiling§
0.05
0.92
N/A
N/A
NS
N/A
Admission from emergency department
0.0004
0.41
0.0306
0.57
0.0001
0.27
UIA indicates unruptured intracranial aneurysm; N/A, not applicable; NS, nonsignificant.
*OR of good discharge outcome.
†Per 10-y increase in age.
‡Per additional 10 cases.
§Per additional 10% coiling.
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
of cerebral aneurysm treatment,10,13,16,18,19 none has shown
the inverse regionalization trend that we observe with this
new technology. In the authors’ opinion, with the perceived
ease of coiling of UIA and attendant socioeconomic pressures, endovascular technology may continue to spread from
major academic centers to smaller community hospitals ill
equipped to provide comprehensive cerebrovascular care,
which may lead to inferior outcomes not only due to technical
shortcomings, but errors in judgment regarding who to treat
and how to treat them.
Given the more than doubling of the case rate for treatment
of UIAs over the past 10 years, however, the stagnation in
patient outcomes may also be, in part, an epiphenomenon of
expanding treatment indications. For instance, an increase in
the treatment of smaller previously uncoilable aneurysms
may be driving the increase in UIA treatment. Expanding
indications to lesions where safety is not well established may
also result in a wash-out of a possible inherent superiority of
endovascular coiling. Furthermore, because a greater percentage of aneurysm cases are being treated endovascularly, the
complexity of cases treated by surgical clipping has likely
increased substantially, yet case volume and ability to train
open cerebrovascular surgeons has suffered. Although endovascular treatment has become increasingly decentralized,
surgical management of unruptured aneurysms occurs increasingly at high-volume centers, but these same centers
exhibit erosion in their overall treatment volume and expertise (Figure 1A).
All analyses are generated from discharge data recorded
solely from New York State hospitals, and as such, the
validity of conclusions drawn from this study rests on the
accuracy of case-defining diagnostic codes. Numerous studies have pointed out the limitation of classification systems
such as the International Classification of Diseases, 9th
Revision.20,21 For instance, diagnostic codes may not fully
encompass the condition under study or the condition may be
spread across multiple diagnostic codes. Details about aneurysm size and location that might explain the rationale for
treatment or outcome are inherently lost. Only discharge
disposition (used as a surrogate for outcome) and in-hospital
mortality were available; thus, we were only able to track
events occurring up until the time of discharge. Thus, it is
possible, as has been previously demonstrated, that endovascular treatment may be associated with an increased risk of
recanalization and possibly aneurysmal rupture, an event that
would not be accounted for in our study.22 Additionally,
surgically clipped patients may recover more slowly than
patients undergoing endovascular interventions and this
would skew the outcome data in favor of coiling. Regardless,
although discharge to home does not always indicate a good
outcome, discharge status has been shown to correlate well
with modified Rankin Scale score23 and provides important
insight into differences within and between treatment modalities. In addition, it is impossible to control for all confounding variables. Clipped patients and those treated at a highervolume centers may have more comorbid disease, larger or
more complicated aneurysms, or more acute symptoms than
those treated endovascularly or vice versa. Additionally, we
could not account for number of aneurysms treated by each
surgeon per year in each center, which may confound our
analysis of high-volume centers. We included all available
potential risk factors for poor outcome in our multivariate
models, including age, gender, race, ethnicity, and admission source, but a myriad of other factors are not available
in the SPARCS data set, namely aneurysm location and
morphology.
Conclusions
Since 1995, in the absence of any published data expanding
indications, there has been a doubling the population-adjusted
treatment rate for UIA, almost completely driven by a 5-fold
increase in the rate of endovascular coiling. Our data,
although limited by lack of anatomic specifics of the treated
UIA, confirm that endovascular coiling is associated with an
increased incidence of good outcome relative to microsurgical clipping and the failure of the evolution in therapeutic
practice to improve overall patient outcome. Factors contributing to this failure appear to be the dramatic shift in coiling
venue from high-volume centers to low-volume centers
where outcomes are inferior, and decreasing microsurgical
volume, even in the busiest centers, accompanied by an
overall worsening in microsurgical results. Both factors argue
for greater centralization of care rather than further technological advances.
Zacharia et al
Trends in Unruptured Cerebral Aneurysm Treatment
Acknowledgments
Emilia Bagiella, PhD, Department of Biostatistics, Mailman School
of Public Health, Columbia University, assisted with the statistical
analyses and received financial compensation.
Sources of Funding
This study was internally funded by the Columbia University
Department of Neurological Surgery.
Disclosures
None.
References
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
1. Housepian EM, Pool JL. A systematic analysis of intracranial aneurysms from the autopsy file of the Presbyterian Hospital, 1914 to
1956. J Neuropathol Exp Neurol. 1958;17:409 – 423.
2. Wiebers DO, Whisnant JP, Huston J III, Meissner I, Brown RD Jr,
Piepgras DG, et al. Unruptured intracranial aneurysms: natural history,
clinical outcome, and risks of surgical and endovascular treatment.
Lancet. 2003;362:103–110.
3. Wiebers DO, Whisnant JP, O’Fallon WM. The natural history of
unruptured intracranial aneurysms. N Engl J Med. 1981;304:696 – 698.
4. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et
al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical
clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002;360:1267–1274.
5. Molyneux AJ, Kerr RS, Birks J, Ramzi N, Yarnold J, Sneade M, et al.
Risk of recurrent subarachnoid haemorrhage, death, or dependence and
standardised mortality ratios after clipping or coiling of an intracranial
aneurysm in the International Subarachnoid Aneurysm Trial (ISAT):
long-term follow-up. Lancet Neurol. 2009;8:427– 433.
6. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al.
International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical
clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival,
dependency, seizures, rebleeding, subgroups, and aneurysm occlusion.
Lancet. 2005;366:809 – 817.
7. Andaluz N, Zuccarello M. Recent trends in the treatment of cerebral
aneurysms: analysis of a nationwide inpatient database. J Neurosurg.
2008;108:1163–1169.
8. Bardach NS, Olson SJ, Elkins JS, Smith WS, Lawton MT, Johnston SC.
Regionalization of treatment for subarachnoid hemorrhage: a cost-utility
analysis. Circulation. 2004;109:2207–2212.
2849
9. Bardach NS, Zhao S, Gress DR, Lawton MT, Johnston SC. Association
between subarachnoid hemorrhage outcomes and number of cases treated
at California hospitals. Stroke. 2002;33:1851–1856.
10. Berman MF, Solomon RA, Mayer SA, Johnston SC, Yung PP. Impact of
hospital-related factors on outcome after treatment of cerebral aneurysms.
Stroke. 2003;34:2200 –2207.
11. Cowan JA Jr, Dimick JB, Wainess RM, Upchurch GR Jr, Thompson BG.
Outcomes after cerebral aneurysm clip occlusion in the united states: the
need for evidence-based hospital referral. J Neurosurg. 2003;99:947–952.
12. Hoh BL, Rabinov JD, Pryor JC, Carter BS, Barker FG II. In-hospital
morbidity and mortality after endovascular treatment of unruptured intracranial aneurysms in the united states, 1996 –2000: effect of hospital and
physician volume. AJNR Am J Neuroradiol. 2003;24:1409 –1420.
13. Johnston SC. Effect of endovascular services and hospital volume on
cerebral aneurysm treatment outcomes. Stroke. 2000;31:111–117.
14. Johnston SC, Selvin S, Gress DR. The burden, trends, and demographics
of mortality from subarachnoid hemorrhage. Neurology. 1998;50:
1413–1418.
15. Johnston SC, Zhao S, Dudley RA, Berman MF, Gress DR. Treatment of
unruptured cerebral aneurysms in California. Stroke. 2001;32:597– 605.
16. Solomon RA, Mayer SA, Tarmey JJ. Relationship between the volume of
craniotomies for cerebral aneurysm performed at New York State hospitals and in-hospital mortality. Stroke. 1996;27:13–17.
17. International Classification of Diseases: Clinical Modifications. 9th
Revision. US Department of Health and Human Services, Washington
DC; 1991.
18. Chyatte D, Porterfield R. Functional outcome after repair of unruptured
intracranial aneurysms. J Neurosurg. 2001;94:417– 421.
19. Taylor CL, Yuan Z, Selman WR, Ratcheson RA, Rimm AA. Mortality
rates, hospital length of stay, and the cost of treating subarachnoid
hemorrhage in older patients: institutional and geographical differences.
J Neurosurg. 1997;86:583–588.
20. Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using
International Classification of Diseases, Revisions 9 and 10. Stroke.
2005;36:1776 –1781.
21. Tirschwell DL, Longstreth WT Jr. Validating administrative data in
stroke research. Stroke. 2002;33:2465–2470.
22. Mitchell P, Kerr R, Mendelow AD, Molyneux A. Could late
rebleeding overturn the superiority of cranial aneurysm coil embolization over clip ligation seen in the international subarachnoid aneurysm trial? J Neurosurg. 2008;108:437– 442.
23. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke.
1988;19:1497–1500.
Downloaded from http://stroke.ahajournals.org/ by guest on October 1, 2016
Technological Advances in the Management of Unruptured Intracranial Aneurysms Fail
to Improve Outcome in New York State
Brad E. Zacharia, Andrew F. Ducruet, Zachary L. Hickman, Bartosz T. Grobelny, Neeraj
Badjatia, Stephan A. Mayer, Mitchell F. Berman, Robert A. Solomon and E. Sander Connolly,
Jr
Stroke. 2011;42:2844-2849; originally published online August 18, 2011;
doi: 10.1161/STROKEAHA.111.619767
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2011 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/42/10/2844
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/