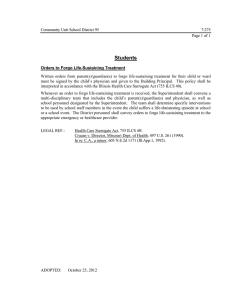
Withholding and Withdrawing Life
advertisement

Implementation Guidelines End-of-life care: Decision-making for withholding and withdrawing life-sustaining measures from adult patients Part 2 Ethical and Special Considerations Ethics Team Clinical Policy Unit Centre for Healthcare Improvement email: QHclinicalethics@health.qld.gov.au Table of Contents 1.0 2.0 3.0 4.0 5.0 INTRODUCTION .............................................................................4 1.1 Community expectations .................................................................................... 4 1.2 Autonomy and Obligation ................................................................................... 4 1.3 Principles for decision making and quality care at end of life ................................ 5 BEST INTERESTS ..........................................................................6 2.1 The Health Care Principle and General Principles ............................................... 6 2.2 Patients without capacity ................................................................................... 7 PATIENTS’ RIGHTS TO KNOW AND CHOOSE ............................8 3.1 Respecting and following patient choices ............................................................ 8 3.2 Patient‘s right to refuse treatment ....................................................................... 9 3.3 Directions for treatment refusals in an Advance Health Directive .........................10 3.4 Informed consent ..............................................................................................11 FUTILE MEDICAL TREATMENT .................................................. 12 4.1 Futile medical treatment and euthanasia – the difference....................................13 4.2 Futile medical treatment and the law generally ...................................................13 4.3 Futile medical treatment and Queensland‘s laws ................................................14 4.4 Difference between withholding and withdrawing life-sustaining treatment ...........15 MORAL QUESTIONS.................................................................... 15 5.1 What is benefit? ...............................................................................................16 5.2 How can risk of harm be minimised? ..................................................................18 5.3 What is the meaning and value of death? ...........................................................19 5.4 Can health professionals object to treating a patient on the basis of conscience? 20 5.5 Can resource allocation be used as a justification for withholding or withdrawing medical treatment? ......................................................................................................21 6.0 5.6 Euthanasia .......................................................................................................23 5.7 Assisted suicide ................................................................................................24 SPECIAL CONSIDERATIONS ...................................................... 26 6.1 People with special needs ...................................................................................26 6.1.1 The elderly .................................................................................................26 6.1.2 Children and adolescents ...........................................................................27 6.1.3 People with disabilities ...............................................................................27 6.1.4 Mental health patients ................................................................................29 6.1.5 Aboriginal and Torres Strait Islander people ................................................30 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 2 of 61 6.1.6 People from other cultures ..........................................................................32 6.2 Organ and tissue donation .....................................................................................34 Organ and Tissue Donation – Facts and Statistics* ..................................................35 7.0 ADVANCE CARE PLANNING ...................................................... 36 7.1 National Framework for Advance Care Directives ...................................................37 7.2 The decision-making pathway ...........................................................................39 Glossary ..................................................................................................................... 41 Bibliography .............................................................................................................. 49 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 3 of 61 1.0 INTRODUCTION Decision-making about end of life matters will never be straight forward. Regardless of whether a dying patient has capacity, there will be profound complexity about the decision to withhold or withdraw life-sustaining measures even if the patient has formally expressed their wishes. Queensland Health acknowledges the tension between three major themes in the ethics of withholding and withdrawing life-sustaining measures - the sanctity or preservation of life (government knows best), patient autonomy (patient knows best) and good medical practice (medical officer knows best). Recognising the complex interplay of these three critical areas, this document aims to offer workable guidance for clinicians, while assuring patients and those closest to them that all Queensland Health employees will respect their views and wishes for end-of-life care. This second part of the Implementation Guidelines for withholding and withdrawing life-sustaining measures from adult patients focuses on considerations about ethical and special matters, for example, people with decision-making disabilities. 1.1 Community expectations Arguably, because of unrealistic expectations in our society about technology and medical advancements, death can be seen as a failure of the health system, rather than a natural and inevitable event. Life cannot be prolonged indefinitely, and to assist patients and their families to accept the inevitability of death is one of the most difficult challenges for health care professionals. When discussing death and dying, the questions that arise enter the realm of ethics, including: respect for life patient autonomy dignity compassion fairness and non-discrimination duty of care quality of life moral questions about the sanctity of life. For example, high respect for the value of life does not necessarily imply a duty to always give life-sustaining treatment. Prolonging life at any cost, while strongly supported by our legal and social system, may not always be consistent with good medical practice, particularly if it pays no regard to the quality of a patient‘s life or the burdens of treatment. Therefore, the primary goal of any medical treatment should be to benefit the patient by restoring or maintaining the patient‘s health as far as possible, maximising benefit and minimising harm. 1.2 Autonomy and Obligation The following quote captures the difficult relationship between medical and ethical challenges in the health care setting. ‗[A] patient‘s unequivocal right to refuse medical treatment is well established and is ethically justified by the principle of autonomy, according to which people have a right to self-governance, to act freely in accordance with a self-chosen plan. Control over our body has been taken to be central Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 4 of 61 to the interpretation of autonomy. In the context of end-of-life care, the right to refuse treatment places a recognised limit on interventions by medical officers, who must respect refusals even 1 against their best clinical judgement and even if a patient‘s life is at risk as a result.‘ However just as respect for patient autonomy cannot be interpreted as an entitlement to every requested medical intervention, it does mean a medical officer‘s obligation to secure patient consent to the withholding or withdrawal of futile or inappropriate treatment which is not clinically indicated. 1.3 Principles for decision making and quality care at end of life Queensland Health‘s End-of-Life Care Strategy (under development) has identified twelve principles that apply to decision making and quality care at the end of life. These principles are designed to underpin the legislation and reflect good medical practice and quality care. They include: 1. Dignity, respect and compassion for the dying. 2. The right of people at the end of life to be informed of their options and to have their choices respected. 3. A non-discriminatory approach to care. 4. Relief from pain and suffering in accordance with the patient‘s best interests. 5. Support for families and carers during a patient‘s life and into bereavement. 6. Communication between the patient and those closest to them to reach an acceptable level of consensus about care options. 7. Recognition of the rights and obligations of our health professionals. 8. A collaborative approach between services to ensure patients receive coordinated and seamless quality care. 9. Access to integrative, holistic care that meets physical, emotional and spiritual needs 10. Improved public awareness and discussion of death and dying. 11. Transparency and accountability for all decision-making. 12. Continuous improvement for care at the end of life through an evidence-based approach. Health professionals should always be mindful of their obligations and the ways in which the patient‘s legal and ethical rights should influence their decision-making. Decision-making about life-sustaining measures sometimes sees an ethical collision between patients‘ rights, community expectations and the clinical obligations of the health care team. Every effort must be made to demonstrate that: 1 there is a balance between the duties and the obligations imposed by those rights and responsibilities reasonable and proportionate decisions based on ethical principles can be reached in every case. Gedge, E., Giacomini, M., & Cook, D. (2007), p. 215 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 5 of 61 2.0 BEST INTERESTS When determining a patient‘s best interests, a wide range of factors need to be considered, such as the patient‘s culture, spiritual values and personal beliefs. The test of best interests must always be carried out on a case-by-case basis, taking into consideration the full range of factors important to the patient. The test of best interests is based not only on medical considerations, but also on such things as emotions, beliefs and values that may influence treatment decisions. 2.1 The Health Care Principle and General Principles The Guardianship and Administration Act 2000 incorporates the test for best interests in the Health Care Principle2 and General Principles3 for adult patients without the capacity for decision-making. This also involves measures to ensure the appropriate use of power by substitute decision-makers, for example their statutory health attorney. These principles ensure that decisions made on behalf of an adult patient without capacity are made in their best interests. If the medical officer (or other members of the health care team) is convinced the patient‘s best interests are not being served by their Advance Health Directive or their substitute decision-maker/s insisting on inappropriate or non-standard treatment, he or she must take the matter further by seeking the opinion of a more experienced medical officer or referring the matter to the Adult Guardian. Assessing whether a treatment is in a patient‘s best interests crosses the boundary of clinical assessment to include legal and ethical considerations. While there are clinical indicators that test how well a body might be performing, there is no ethical standard for measuring someone‘s quality of life and for determining what values might be important to them. It is also highly unlikely we could confidently use the same ‗best interests‘ test between two people of similar conditions, ages and backgrounds. Therefore, it must be acknowledged that the test of best interests will always be subjective and must be carried out on a case-by-case basis, taking into consideration the full range of factors important to the patient. Almost always, best interests cannot be determined for a patient without involving those closest to them. The decision-making process for withholding and withdrawing life-sustaining measures also requires an assessment of the patient‘s best interests by reference to the standards of good medical practice. Traditionally, the test of best interests was based on medical considerations rather than such things as emotions, beliefs or values. Prolonging life at any cost was often seen as in the patient‘s best interest. However, with advancements in medicine it is now possible to sustain some essential functions far beyond the irrevocable loss of awareness. The ‗traditional‘ values or codes of practice can no longer be relied upon by medical officers for the test of best interests. Changes in medicine itself, society, the perception of professional roles and public expectations demand that all heath care professionals identify, confront and attempt to resolve ethical issues and moral conflict in health care. 4 It is essential that thorough communication and consultation occurs with the patient and those closest to them, with the patient‘s consent. 2 Sch. 1, Part 2, Guardianship and Administration Act 2000 (reproduced in Glossary) Sch. 1, Part 1, Guardianship and Administration Act 2000 (reproduced in Glossary) 4 Mitchell, K.R., Kerridge, I.H. & Lovat, T.J. (1999). Bioethics and Clinical Ethics for Health Care Professionals. Social Science Press: Sydney. p. 13. 3 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 6 of 61 2.2 Patients without capacity ‗Where treatment is able to prolong the patient‘s life but there are doubts about whether it would provide overall benefit, the health care team and those close to or representing the patient should take account of the patient‘s wishes, values and preferences in order to assess whether treatment would be in the patient‘s best interests. 5 In assessing best interests in the case of an adult without the capacity to make decisions about health matters on their own behalf, account must be taken of the following: 6 the patient‘s wishes and the views of those closest to them about what is in the patient‘s best interests (where the patient has agreed to their involvement) views of culturally appropriate people close to the patient beliefs and values that would be likely to influence the decision if the patient had capacity clinical judgements about the efficacy of the proposed medical treatment likelihood of the patient experiencing severe intractable pain or suffering level of awareness patients have of their existence and surroundings and their ability to interact with others, and demonstrate self-directed action in any capacity likelihood and extent of any degree of improvement in the patient‘s condition if treatment is provided whether the invasiveness of the treatment is justified in the circumstances likelihood of the patient experiencing increasing levels of disability and/or lack of function and dependence views of the patient‘s significant others (such as spouses, children and friends), as to what the patient would see as beneficial views of any duly appointed health care attorney or patient advocate that decisions must be made on an individual basis and that no unjustifiable discrimination occurs that all patients are entitled to the same quality of care, and that those who lack capacity should not be excluded from potentially beneficial treatment options solely by reason of their lack of capacity that decisions must not be based on whether the health care team, or the patient‘s relatives or carers, would wish to have the treatment themselves in that situation that decisions about best interests must not be motivated by a desire to bring about the patient‘s death. This list is by no means exhaustive and can include written statements made by the patient before capacity was lost. In some cases the patient might like to have their families make statements on their behalf. 5 6 British Medical Association (2007). p. 78 Based on the British Medical Association recommendations for assessing best interests Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 7 of 61 3.0 PATIENTS’ RIGHTS TO KNOW AND CHOOSE The principle of patient autonomy is critical in end-of-life decision-making. It is a general principle of law and medical practice that people have a right to consent to or refuse medical treatment. The courts have recognised that adults have the right to say in advance that they want to refuse treatment should they lose capacity in the future – even if this results in their death. ‗In contemporary ethics, the principle of autonomy asserts that humans have a right to non-interference when making decisions about themselves.‘ (Kerridge, Lowe & McPhee 2005, p. 49). In some cases, a patient may have expressed a refusal of all treatment. These wishes must be taken into consideration at the time a decision is required. For a patient without capacity, their wishes to refuse all or some forms of treatment may be ascertained in four ways: 1. Formally, through their valid Advance Health Directive. 2. Informally, through a family member or close friend. 3. Through previous discussions with a medical officer in charge of the patient‘s treatment. 4. Through previous discussions with the patient‘s General Practitioner. Within this framework, all patients have a right to be informed about their condition and their treatment options in an honest, unbiased manner. This includes the patient‘s family or substitute decision-maker where the patient lacks capacity for decision-making. Ideally, discussion with families about treatment options for a patient will have occurred before the patient loses the capacity to determine their end-of-life views and wishes. Uncertainty about prognosis or likely response to treatment should be communicated to the patient‘s family (preferably in non-technical language) as early as possible. Where possible, prognostic information should be given by a health professional who is respected as an expert or senior medical officer with experience in discussions with dying patients and their families. (For more information, see Section 4 of the Implementation Guideline) However during these discussions, the medical officer responsible for the patient‘s care is under no obligation to disclose or offer treatments that for clinical reasons can never be provided - that is, treatments that, for reasons of good medical practice will be potentially futile and of no benefit to a dying patient. Discussing options for medical treatments with a patient‘s family is an exceptionally difficult and emotion-charged time, particularly when choices are limited. Disclosing medical treatments that cannot be clinically offered to a dying patient would be considered counter-productive, confusing and distressing, not only for the patient but for the patient‘s family. 3.1 Respecting and following patient choices Respecting a patient‘s choices begins with the very first discussions held between a patient and members of the health care team. The medical officer in charge of the patient‘s care is responsible for coordinating the patient‘s end of life care, which is an important factor in meeting the standards of good medical practice. The patients‘ beliefs and values will influence their end-of-life choices and, therefore, must always be respected. Every patient experiences spiritual and/or religious feelings in a unique way. Some may directly raise these issues, whereas others may not discuss them, but may be troubled by them. They may even make medical choices based on them that may be considered unreasonable. In these situations, medical officers and the health care team will take all reasonable steps to discuss such matters with the patient to address their spiritual or religious concerns in the context of providing better care. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 8 of 61 All patients in all situations are entitled to be treated as unique individuals and afforded fair and non-discriminatory assessment of their condition. While a patient has capacity, the medical officer responsible for their care must discuss the implications of any requests or refusals of particular treatments with them. Patients are entitled to make decisions that conflict with the views of the health care team. The fact that a patient has made a decision which appears to others to be irrational or unjustified should not necessarily be taken as evidence that the individual lacks the mental capacity to make that decision, nor that they are unable to determine their own best interests. Ultimately, the decision as to what treatment to offer is a clinical one and rests with the medical officer in charge of the patient‘s care. This should involve discussing treatment options and the resource needs of other patients with other members of the health care team. While it is not acceptable to continue to indefinitely provide treatment that is not clinically indicated and which seriously disadvantages other patients who have a better chance of survival, there may be arguments for complying with requests from patients with capacity for treatment to be continued or provided for a limited time. Sometimes patients may wish to stay alive for a family event, or some other milestone. As far as reasonably possible, these wishes should be respected and efforts made to comply with these requests. There is a difference between ‗respecting‘ and ‗following‘ patient choices. Respect is a broad concept that provides for careful consideration followed by acceptance of a person‘s wishes or decisions irrespective of whether they are consistent with those of the health care team. Respecting patient choices has greater potential for flexibility, whereas following patient choices must be tempered by the views of the medical profession about what is clinically possible. While a patient‘s choices must always be respected, they may not always be capable of being followed. Respect for life must acknowledge that there comes a point in all lives where no more can reasonably or helpfully be done to benefit patients other than keeping them comfortable and free from pain. In these cases, palliative care and support will take priority over active treatments. 3.2 Patient’s right to refuse treatment In Australia there is no direct authority on the right to refuse treatment, but given the weight of common law authority in other jurisdictions, it seems reasonable to conclude that a right to refuse treatment would allow a patient to make decisions that would result in their death. There are a number of cases that could prove convincing to an Australian superior court in providing common law authority on refusing treatment. However, it is a general principle of law and medical practice that people have a right to consent to or refuse treatment. The courts have recognised that adults have the right to say in advance that they want to refuse treatment if they lose capacity in the future – even if this results in their death. Refusal of medical treatment, particularly when it is not consistent with good medical practice, is one of the most difficult decision-making areas in health care, not only because the law is so complex, but also because of the multiple variables that have led to treatment refusal. There are two ways the law looks at treatment refusal - under common law through statutes, and through the regulatory regime and Advance Health Directives. The common law position on refusal of medical treatment is based upon the principle of respect for personal autonomy.7 A person with capacity has the right to refuse any medical treatment, including palliative care, while they have capacity. A clinician could face charges for 7 Guardianship and Administration Act 2000, s. 5 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 9 of 61 assault if they were to provide treatment against the decision of a person with capacity. It could also result in a complaint to the Medical Practitioners Board. While a patient has capacity, they may choose to refuse all forms of conventional medical treatment. These wishes must be followed, while the patient has capacity. For example, a patient may refuse all active treatments and choose to return to the family home to die, comforted by family and supported by palliative care professionals. With the patient‘s consent, their decision to refuse all or certain forms of treatment should be discussed with their family/carers while the patient still has capacity. If a patient no longer has capacity, their substitute decision maker/s would have to take into account the wishes of the patient as expressed in the refusal of treatment. If the substitute decision maker/s determine that to continue or commence treatment is in the best interests of the patient, they may consent on the patient‘s behalf. A clinician would not be held liable for assault in such circumstances. However it would be the clinician‘s responsibility, knowing of the patient‘s refusal, to ensure that the substitute decision maker/s was informed of that refusal. If the medical officer believes the patient‘s decision to refuse treatment is inconsistent with good medical practice, they should seek a second opinion from a more senior medical officer or even refer the patient to another medical officer as the situation warrants. Ideally, the medical officer responsible for the patient‘s care should have already discussed the implications of refusing treatment with the patient and, with the patient‘s consent, those closest to them. In these situations, patients should be encouraged to formalise their wishes for treatment refusal, for example through an Advance Health Directive (For more information, read Section 8 of the Implementation Guideline). Careful and meticulous documentation of discussions is required in these situations. Similarly, if the medical officer believes the patient may be suffering from clinical depression or some other mental condition that has unduly influenced their decision-making and caused them to refuse treatment, they must seek the opinion of a clinician with expertise in this area, for example, a psychiatrist. It may be appropriate to negotiate with the patient an agreed plan of continuing treatment and further discussion in the near future, while acknowledging that sustained wishes for treatment refusal are ultimately paramount. Where a patient has formalised their treatment refusal through an Advance Health Directive and they lose capacity, medical officers may withhold or withdraw treatment without obtaining further consent, in accordance with the patient‘s wishes and good medical practice. (See following discussion about treatment refusals in valid and enforceable Advance Health Directives.) The decisions of patients who refuse medical treatment will ideally be based on sufficient accurate information including an awareness of the condition, the proposed treatment, any significant risks or side-effects, the probability of a successful recovery, the consequences of not having the treatment and any alternative forms of treatment. Such information should always be offered but legally, patients are not required to have accepted the offer of information in order for their refusal to be valid. 3.3 Directions for treatment refusals in an Advance Health Directive A valid Advance Health Directive that refuses a particular life-sustaining treatment has the same force as a contemporaneous decision. Many Advance Health Directives do in fact refuse medical treatments. Health care professionals must follow a valid Advanc e Health Directive and apply the refusals for treatment to the particular circumstances. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 10 of 61 However, under Queensland law, medical officers are excused from following the directions in an Advance Health Directive if they ‗reasonably consider‘ the instructions are inconsistent with good medical practice. This adds a significant layer of complexity to the decision-making about life-sustaining measures. A recent paper 8 on the legal aspects of advance refusals makes the following observation: ‗An excuse based on good medical practice seriously weakens the essence of advance directives: the ability of an adult to choose the treatment that he or she wishes to refuse, even if others may disagree. It also undermines the primacy that the common law has given to the right to selfdetermination or autonomy. The practical effect of the excuse is that an adult cannot be confident that his or her advance directive will be followed if it is not considered good medical practice for treatment to be withheld or withdrawn. The authors are of the view that the excuse should be repealed and that, in this context, the common law position reflects a more appropriate balance between the right to self-determination or autonomy, and the sanctity of life.‘ Despite this opinion, if a patient has an Advance Health Directive, treatment refusals can be potentially overturned on good medical practice grounds, whereas under common law the principle of patient autonomy remains paramount. The complexity of the law aside, if a patient regains capacity, even for a short time, their wishes for refusing life-sustaining measures must be followed. If a patient decides they do not wish to receive life-sustaining treatments, this should be carefully documented in the medical record and discussed as soon as practicably possible with their substitute decision-maker/s and, where appropriate, those closest to the patient. It also should be noted that if a patient regains capacity and decides to refuse treatment, even if this is contradictory to their Advance Health Directive, the later decision to refuse medical treatment overrides. This is because an Advance Health Directive is triggered only when a patient loses capacity. 3.4 Informed consent It is Queensland Health‘s policy that there is no requirement for informed consent or refusal when an Advance Health Directive is completed, and competent adults can write medical directions refusing future treatment with no requirement to be informed themselves about the potential consequences of their Advance Health Directive being applied. A clearly stated refusal of treatment in a valid Advance Health Directive cannot be ignored on the grounds that the person was not informed about the medical consequences when they wrote it. However it is important to note that informed consent provisions apply when decisions are made by a substitute decision-maker at the time that health or medical treatment is required, in the same way as they apply when a competent adult decides whether or not to undergo treatment. The treating health care team is obliged to give the substitute decision-maker sufficient information to make that decision in an informed manner. When treatment is indicated, the obligation is on the medical officer responsible for the patient‘s care to inform them or their substitute decision-maker, not on patients and substitute decision-makers to ensure they are informed, for their consent to be valid or their refusal to be binding. While patients are under no obligation to explain or justify their decision to refuse medical treatment to the health care team, the medical officer responsible for the patient‘s care should discuss the implications of the patient‘s decision in an open and frank manner. This is to ensure the decision is based on accurate information and not on any misunderstanding or misinterpretation of the facts. In these instances, there is a careful balance between 8 White, B. & Willmott, L., (2006), p. 16 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 11 of 61 pressuring the patient into something they do not wish and ensuring the treatment provided to the patient is consistent with good medical practice. If those closest to the patient are involved in these discussions, care must also be taken to ensure the wishes and views of the patient, rather than their family, are followed. Ultimately the medical officer in charge of the patient‘s care will decide what options are clinically appropriate to offer. It would be incumbent upon a medical officer and other members of the health care team, knowing of the patient‘s refusal, to ensure the substitute decision-maker/s informed of that treatment refusal. 4.0 FUTILE MEDICAL TREATMENT The term ‗futile treatment‘ is extremely difficult to define. It is even more difficult to develop a manual or a set of guidelines to determine whether or not treatment is futile. The issue is fraught with ethical, medical and legal challenges. There is a heavy presumption in favour of administering life-sustaining medical treatment to a patient where that treatment provides a net benefit to the patient. Modern technology and medical advancements have enabled health care to treat disease and sustain life by artificial means when organ or system failure would otherwise naturally result in death. 9 These technological and medical advances have brought with them new ethical questions. For example, is it the case that if a medical intervention is found to be technically possible in one case, it should be applied or attempted in all similar cases? Is it the case that everything that can possibly be done should be done? These are not questions which can be easily answered. Everyone, doctors most of all, know there comes a point when a patient is overcome by their disease and medicine is powerless to intervene. The difficulty lies in defining this point with the precision, accuracy and ethical cogency required to guide clinical practice and gain community acceptance. One simple definition of futile medical treatment is: treatment that gives no, or an extremely small, chance of meaningful prolongation of survival and, at best, can only briefly delay the inevitable death of the patient.10 The word ‗meaningful‘ in this context is usually interpreted in light of the values, beliefs and quality of life factors that are important to the individual patient. A meaningful recovery generally affords a level of quality of life that the patient deems acceptable, or which the average, reasonable person deems acceptable. Ultimately, judgements on whether or not a medical treatment is potentially futile are going to be at least partially subjective. Recent procedural approaches to the determination of futility accept that it is not possible to be objective on this issue, and therefore processes (some of them statutory) based on fairness and individual patient‘s best interests at the end of life should prevail. This is exemplified with the increased focus (legally, ethically and clinically) on advance care planning for patients at the end of life. 9 M. Heaney, C. Foot, W. Freeman, J. Fraser. (2007), p. 278 Murphy, B. (2008). p. 418. 10 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 12 of 61 4.1 Futile medical treatment and euthanasia – the difference Despite the complexity in defining ‗futile treatment‘, the literature on the subject makes clear between decision-making around potentially futile medical treatment and euthanasia. Withholding or withdrawing life-sustaining futile medical treatment is not done with the intention of killing the patient. It is distinguished from euthanasia and physician-assisted suicide because its primary goal is not to bring about the death of the patient. Withdrawing life-prolonging medical treatment helps the already dying patient to achieve a peaceful and dignified death, so that suffering and death is not unnecessarily prolonged as a result of medical intervention. Once the treatment focus shifts to palliative care, the primary is to relieve uncomfortable or unwanted symptoms rather than to cure the disease. The medical officer in charge of providing pain relief must do so with the primary purpose of obtaining symptomatic control of the patient‘s pain, discomfort or distress, and not to cause or hasten the patient‘s death; even though this may be one of the effects of administering such pain relief. This is known as the ‗principle of double-effect‘, and is readily distinguished from euthanasia or assisted suicide. 4.2 Futile medical treatment and the law generally There are well established common law principles that clinicians are under no moral or legal obligation to attempt medical treatment that could cause harm or would provide no benefit to a patient. The Court of Appeal recently concluded that ‗…ultimately, however, a patient cannot demand that a doctor administer a treatment which the doctor considers is adverse to the patient‘s clinical needs.‘11 Therefore, competent patients, or those holding authority to act on behalf of incompetent patients, cannot demand treatment that clinicians believe to be futile. 12 This includes all life-sustaining measures, such as cardiopulmonary resuscitation (CPR), dialysis, ventilation, and in some circumstances, even enteral or intravenous nutrition. Potentially futile medical treatment goes against a patient‘s best interests and therefore, at common law, need not be offered. Although the decision to withhold or withdraw life-prolonging medical treatment is ultimately a clinical decision, Australian courts are unclear as to what weight should be attached to family‘s views.13 While the patient‘s family can offer important insights into the patient‘s beliefs and views regarding end of life decisions, the clinician‘s duty of care is always to the patient and their best interests, not those of their family. There is plenty of case law where families have challenged the clinical assessment that providing further treatment to their loved one is deemed to be futile. 14 Courts are not bound by the views of the medical profession and will reach an independent assessment of what the patient‘s best interests require. 15 However, the courts have also said, in the context of futility, that the ‗decision as to appropriate treatment … is principally a matter for the expertise of professional medical practitioners‘. 16 If a court concludes that medical treatment is futile and therefore not in a patient‘s best interests, that treatment need not be continued. (White, B. & Willmott, L., 2005). 11 R (on the application of Burke) v General Medical Council [2006] QB 273, 301. Skene L. (2004).p. 307. 13 Ethical issues in withholding and withdrawing life-prolonging medical treatment in the ICU, Current Anaesthesia & Critical Care, 2007,18: 5, pp. 277-283. M. Heaney, C. Foot, W. Freeman, J. Fraser 14 Northridge v Central Sydney Area Health Service (2000) 50 NSWLR 549, 554 15 White, B. & Willmott, L. (2005). p. 70. 16 Isaac Messiha (by his tutor Magdy Messiha) v South East Health [2004] cited in White, B. & Willmott, L. (2005), p. 70. 12 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 13 of 61 4.3 Futile medical treatment and Queensland’s laws The situation regarding decision-making around potentially futile medical treatment is different in Queensland. Under Queensland‘s legislation, 17 a decision to withhold or withdraw lifesustaining measures requires consent, so it may be more difficult for a health provider to refuse to provide futile treatment in Queensland. 18 Specifically, Section 79 of the Guardianship and Administration Act 2000 makes it an offence for a health provider to carry out health care for an adult with impaired capacity unless the appropriate consent is obtained. The term ‗health care‘ is defined in Schedule 2 of the Guardianship and Administration Act 2000 to include the withholding or withdrawal of a lifesustaining measure if the commencement or continuation of the measures would be inconsistent with good medical practice. As a result, a health provider would be committing an offence under section 79 if they did not obtain consent to withhold or withdraw a life-sustaining measure.19 In some cases, this may come into conflict with the common law position on the provision of potentially futile medical treatment. Under Queensland‘s laws, a health provider who withholds or withdraws life-sustaining measures may still commit an offence even if a court or the Queensland Administrative Tribunal subsequently determines that the treatment was futile. 20 Since a decision under section 79 relies on consent rather than best interests (and futility), if consent to withhold the medical treatment is not obtained, the courts may determine that an offence has been committed, irrespective of the appropriateness of the treatment. This is a different situation from that under common law. At common law, a doctor will be liable for a decision to withhold or withdraw treatment only if subsequent prosecution or civil litigation shows the doctor‘s assessment of futility has been wrong. Where there is early evidence that a dispute about withholding and/or withdrawing medical treatment from a patient without capacity is likely because of the clinical judgement that providing that treatment is considered futile, the statutory regime can be used and contact made with the Office of the Adult Guardian. Guidance of the Tribunal or courts can also be sought, particularly if there is uncertainty about the patient‘s level of capacity. The statutory regime in Queensland also provides for a hierarchy of decision-makers to make decisions on behalf of an adult patient who lacks capacity. Should there be a dispute between the family21 and the health care team about withholding or withdrawing medical treatment, the Adult Guardian or the Tribunal can be approached to intervene in the case. In other words, if medical officers disagree with the demands of the family of a patient who lacks capacity, the consent mechanisms within the Powers of Attorney Act 1998 and Guardianship and Administration Act 2000 can be used to override their decisions. In many respects, however, this may make an already difficult decision-making pathway even more complex. Initiating an additional procedural hurdle to seek consent either from the Adult Guardian or the Tribunal in the case of dispute may exacerbate the patient‘s already fragile condition, damage relationships with the family of the patient, and potentially act as a catalyst for a litigious path. It is best to try to prevent such a situation occurring in the first instance through advance care planning discussions with the patient and/or their family. The available options for future medical treatment should be discussed as soon as practicable, to ensure that decision-making about withholding or withdrawing life-sustaining measures does not occur in a crisis-driven situation (see 4.2 Discussions with Families and 4.5 Resolving Disputes). 17 Powers of Attorney Act 1998 and Guardianship and Administration Act 2000 White, B. & Willmott, L. (2005). p. 72 19 Ibid., p. 71 20 Ibid. p. 72 21 Family members may or may not be legally appointed substitute decision-makers, for example, the patient may appoint a close friend as their health attorney. 18 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 14 of 61 4.4 Difference between withholding and withdrawing lifesustaining treatment While the Guardianship and Administration Act 2000 and the Powers of Attorney Act 1998 in the provisions concerning life-sustaining measures combines withholding and withdrawing medical treatment, arguably, the two operate under quite different decision-making paradigms. The clinical decision-making for both circumstances (that is, to withhold and/or withdraw) is affected by: (i) The level of clinical uncertainty; and (ii) The timeframe available for decision-making. The lines between the two decisions may converge ethically, but diverge clinically. The decision to withhold medical treatment is largely prospective: that is, whether or not to commence treatment for an event/s yet to take place. This may involve a dimension of uncertainty, because there could be unknowns about the future clinical state of the patient, for example, when and if the patient will suffer a cardiac arrest, necessitating CPR. The decision to withdraw a life-sustaining measure implies that a level of acceptance about the benefits of continuing the measures has been reached, both by the clinicians involved and the family. The decision signifies that a stage has been reached where the evidence points to the fact that the patient undeniably and irrefutably is receiving no benefit from the interventions proposing to be withdrawn. Arguably, the consent processes for withdrawing medical treatment may be less onerous than for withholding medical treatment, most likely because the patient‘s condition has stabilised to the extent that no further improvement is expected. In some cases, consent may not need to be obtained to provide life-sustaining measures (for example, under urgent health care provisions), but consent would be required to withdraw the measures. This may be the source of some confusion for families. The explanation is that decisions to withdraw medical treatment almost always occur in non-urgent clinical situations, where there is time to discuss all of the issues with the patient‘s family and obtain their consent. Decisions of this nature are often difficult and complex, and need to involve close consultation and effective communication with the health care team, the patient and those close to the patient. How well a medical officer can broach this sensitive topic with patient and family correlates to how well the patient and family understand and accept this information and trust that the health care team has the best interests of their loved one at the forefront of their treatment plan and goals. 5.0 MORAL QUESTIONS While the two terms are often used interchangeably, there is a distinction to be made between morals and ethics. For the purpose of this guideline, the following definitions are offered: Morals, such as a person‘s moral principles and convictions, are qualities that determine a person‘s character. Understanding the difference between, and notions of, right and wrong come from personal convictions - a person‘s morals. Moral principles are normative in nature; that is, they are the basis from which an imperative to act originate. Ethics relate to personal, institutional and broader social regulations and systems. To act ethically is to regulate one‘s (and/or others‘) behaviours so they are in accordance Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 15 of 61 with a moral or set of morals. Ethics is a systematic approach to morality, based on reason and moral justification. There are two significant and distinct approaches to moral philosophy - objective and subjective. Objective approaches to moral philosophy seek to determine universal principles applicable to all, whereas subjective approaches tend to hold that ethical behaviour is not universal in nature and is determined by context and consequence. Also for the purpose of these guidelines, while each patient‘s clinical treatment will be determined on a case-by-case basis, the four Governing Principles (discussed in detail in Part 1 of these guidelines) embody moral principles that are to be applied to all patients. Principle 1: All decision-making must reflect respect for life and the patient‘s right to know and choose. Principle 2: All decision-making must meet the standards of good medical practice. Principle 3: All efforts must be made to obtain the appropriate consent through a collaborative approach. Principle 4: There must be transparency in and accountability for all decisionmaking. The types of moral questions raised in this section are directed at those individuals who are responsible for making (and justifying) their decision-making processes for life-sustaining measures. Therefore health care professionals can refer to this section to test their own values about what they consider to be right and wrong. Other interested parties may find this guidance useful if they are faced with these decisions at some future time in their lives. Answers to these moral questions are, quite obviously, subjective, and as such cannot realistically be determined on a yes or no basis. However, they can provide a process for ethical deliberation for decision-making in this difficult area and will either affirm personal values or challenge them. In exploring the moral considerations inherent in making decisions about the withholding and withdrawing of life-sustaining measures, it is useful to consider the four bioethical principles: Autonomy – respect for the individaul and their ability to make decisions about their own health and future. Actions that enhance autonomy are thought of as desirable, and actions that override an individual and their autonomy are undesirable. Beneficence – actions intended to benefit the patient or others. Non-malificence – actions intended not to harm or bring harm to the patient and others. Justice – being fair or just to the wider community in terms of the consequences of an action. 5.1 What is benefit? Our health system and its health professionals have a general duty to provide treatment which benefits all patients; the bioethical principle of beneficience being one of the four cornerstones of modern health care. Benefit, in this context, means an advantage or net gain for the patient. Benefit can be physiological or it can also be other factors important to the patient, such as quality of life. A therapeutic benefit occurs when a medical treatment or procedure confers some sort of symptomatic relief for the patient or improves the patient‘s condition or prognosis in a real and meaningful way. This treatment is justified as it provides a real benefit. Health professionals also have responsibilities toward society in addition to the responsibilities they have to individual patients. Clinicians are employed by society to provide medical care Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 16 of 61 that is both appropriate and affordable. The practical expression of beneficence therefore requires judiciousness and genuine concern for the wellbeing of the total society. This must necessarily include the wise use of scarce resources and some recognition of the financial and clinical limits to clinical medicine. Thus, beneficence may be overridden by other considerations.22 The decision to prolong life by providing life-sustaining measures is usually, but not always, a benefit. When we think of benefit in health terms, concepts like progress, recovery, remission, symptom reduction and pain relief are raised in the context of the discussion. However all these concepts have degrees of benefit. For example, the benefit may be that a patient is able to maintain status quo in their condition without further deterioration. In other cases, benefit may keep the patient alive, but fail to halt the progression of a serious illness. The burden of prolonging life in the most extreme cases where there is multiple morbidity and no reasonable prospect of recovery should weigh on the side of palliative care rather than finding cures through active treatment. Arguably, in these cases, there is little or no benefit in subjecting the patient to an endless regime of tests and therapies that are potentially futile and have no chance of restoring their health. Applying life-sustaining measures to prolong life in these circumstances may be causing more harm to the patient than benefit, particularly if pain is involved. This is where the health care team must carefully weigh up and consider all factors in a patient‘s quality of life. Another key community expectation of our health system is that treatment benefits will outweigh the harms. In decision-making about withholding and withdrawing life sustaining measures, a similar test applies. It is a tenuous moral and ethical balancing act to determine what benefits a patient might receive against harm done to them. Meticulous record-keeping and open communication with a patient‘s family can assist in the decision-making process. When discussing the concept of how the patient benefits from certain forms of treatment, decisions about withholding or withdrawing a life-sustaining measure must never be made on behalf of a patient with capacity. Patients with capacity are in the best position to judge what represents an acceptable level of burden or risk for them, and their wishes must be respected even if this results in perceived harm to them. This important principle underpins the concept of patient autonomy. In circumstances where a patient does not have capacity, they are not involved in assessing whether benefit is achieved. It falls to the patient‘s family or their statutory health attorney to act on wishes expressed by the patient when they had capacity, and perhaps recorded in an Advance Health Directive. For example, if a patient is known to have the view that there is no intrinsic value in prolonging life at any cost, life-sustaining measures would, arguably, provide no benefit to that individual. The ability to apply reason in these instances hinges on the patient‘s level of awareness. For example, important factors in assessing a patient‘s awareness is demonstrated by them: 23 interacting with others awareness of their own existence and having the ability to take pleasure in the fact of that existence having the ability to achieve some purposeful or self-directed action or to achieve some important personal goal. Should treatment or health care be able to recover or maintain any of these abilities, this likely indicates some benefit to the patient. Benefits are increased if improvements are in the context of the patient‘s known wishes and values about quality of their own life. The National Health and Medical Research Council 22 23 Kerridge, Lowe & McPhee, 2005, p. 53 British Medical Association (2007). p. 11. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 17 of 61 (NHMRC) provides guidelines on post coma unresponsiveness and minimally responsive states which gives more detail about assessing awareness (as opposed to capacity). These guidelines also recommend, for example, treatment cycles after a patient‘s emergence from a coma. Assessing such things as awareness and responses to environmental stimulii does provide some assurance from a clinical perspective that a level of benefit can be determined. 5.2 How can risk of harm be minimised? The concept of non-maleficence is embodied by the phrase, ‗first, do no harm‘. Many consider that should be the main or primary consideration in health care (hence first): that is, it is more important not to harm your patient, than to do them good. Just how the idea of harm can be determined is another key moral question. There is always the presumption that medical treatment provides benefit to a patient. However, in terms of end of life care, patients may be harmed by both the withdrawal of treatment too quickly and by prolonging the treatment beyond the point where it is able to benefit the patient. It is also the case that patients with capacity, or patients whose views are known, are also harmed by treatment being provided or withheld or withdrawn against their wishes. 24 For example, where patients are known to have refused treatment, particularly through an Advance Health Directive, these instructions must be followed. While there are some legal protections in limited circumstances, medical officers who do not follow valid Advance Health Directives are increasing their risk of liability, both criminally and civilly. Equally where patients are known to have expressed views about their own quality of life, even conversationally at a time when they had capacity, these wishes must also be taken into account in the decision-making process. To treat a patient against their stated wishes is, in itself, of harm to the patient and may be even be viewed by the courts as a form of assault. 25 There may be a disparity in perspectives between harm and benefit in many medical treatments, for example, CPR, artificial nutrition and blood transfusion. Despite its exclusion as a life-sustaining measure in Queensland‘s legislation, if an adult Jehovah‘s Witness expressly forbids having a blood transfusion at the cost of prolonging their life, this wish must be followed. Likewise, patients (or their families) cannot demand treatments that are not appropriate and, in the opinion of the treating medical officer, would harm the patient or provide no benefit to them. Harm may also be caused by reluctance and prevaricating about withholding or withdrawing life sustaining measures. Failing to make difficult decisions and thereby subjecting a patient who lacks capacity to undignified invasive treatment would also qualify as harm. Quite often more time is needed to assess the best interests of the patient, particularly where there are doubts or disputes. In these instances, consideration should be given to a trial of treatment which allows time for the patient to stabilise and provides more information about the likelihood and extent of any improvement. Families may also benefit from this period as they come to terms with the condition and likely prognosis of their loved one. Failing to give patients and their families this opportunity for improvement where there is even the slightest chance it may be successful could also be harm. Reducing the risk of causing harm in end of life care should involve careful consideration of the patient‘s medical condition and likely prognosis. This information should be communicated to patients and their families as soon as possible to avoid crisis-driven decision-making. 24 25 British Medical Association (2007). p. 11. Queensland Criminal Code 1899, s. 246, also see Hunter and New England Area Health Service v A ([2009] NSWCS 761), NSW Supreme Court for recent case law regarding a decision requiring clinicians to follow Advance Health Directives to refuse medical treatment, even in acute emergencies. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 18 of 61 5.3 What is the meaning and value of death? Death is the only great certainty. The subject of powerful social and religious symbolism, it continues to be contemplated by philosophers, probed by biologists, and its reality dealt with families and clinicians on a daily basis. Our cultural and individual orientations toward death are intimately interwoven. It is well documented that the Western culture, the attitude towards death is often denial (or perhaps more accurately, suppression). Death is defined in Queensland legislation as the irreversible cessation of circulation of blood in the body of the person, or the irreversible cessation of all function of the brain of the person. 26 But a discussion about the ethical meaning of death in society goes much further than a clinical determination that death is simply the cessation of life. The meaning and value of death impacts upon decision-making in almost every sphere of society. Pondering this moral question captures (but is not limited to) such issues as: attitudes regarding care for the elderly, frail and chronically ill resource allocation in our health care budgets how we celebrate a life once it ends changing attitudes to death debated on whether there is there such a thing as a ‗duty to die‘; and what is a good death. The meaning and value of death confronts health professionals on a daily basis in hospital wards across the state. Nowhere is this more demonstrated than through those responsible for making decisions about whether to withhold or withdraw life-sustaining measures. More concerning for some researchers 27 is the absence of an agreement on the definition of dying. The lack of a clear definition means that, for the purposes of research, we can never be certain about who to include in the population or cultural groups and who to exclude. Research into end of life issues becomes, by its very nature, subjective because of this lack of conceptual clarity. In short, I view the absence of conceptual and operational congruity regarding definitions of ‗dying‘ and/or ‗terminally ill‘ as the most important issue facing end-of-life research. I cannot see the field breaking new ground or ‗reaching the next level‘ without resolving this issue. 28 Leaving the definition of ‗dying‘ aside, it can be confidently stated that death is not as predictable as it was, for example, 50 years ago. This is for many reasons, most significantly the successful combination of medical innovation and modern societies‘ preoccupation with keeping its population safe and healthy. This has caused our life expectancy to increase over the last century. For example, a girl baby born at the time of Federation lived 23 years less than a girl baby born in the new Millennium is expected to. 29 Unfortunately, in many cases, this increase in lifespan and decrease in mortality rates have not been matched by an extension of good health. The years we have gained are often spent with disability, disease, dementia and aggressive medical interventions. Before life sustaining measures such as artificial hydration, nasogastric feeding and respirators, no patient continued for long in deep coma. With the aid of modern medicine, some patients with severe loss of brain function can be kept from a rapid death. Many, however, become permanently and totally unresponsive. These patients can be seen 26 The Transplantation & Anatomy Act 1979, s. 45(1) George, L.K (2002), p. 87 28 Ibid. 29 ABS statistics, 1301.0 - Year Book Australia, 2001; ―A Century of Population Change in Australia.‖ 27 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 19 of 61 breathing, their heart beating, and may even be observed to have different facial expressions, but are in a comatose state from which they are not likely to recover. Such artificially maintained bodies present ethical dilemmas, for which the application of traditional means of determining death is neither clear nor fully satisfactory. This illustrates why decision-making about withholding and withdrawing life-sustaining measures has become so medically complex and ethically challenging. It is not just the clinical side of death that is challenging for the health care team. Awareness of death confronts us with questions that go to the very nature of existence. Often those at the end of life question the meaning and nature of life and whether there is continued existence beyond life itself. This type of questioning can manifest in an infinite variety of ways and represents coping mechanisms for human confrontation with death. In less extreme cases, life-sustaining measures can be used to prolong a well-lived life, to buy time, for example, for a patient to undergo a transplant or to experience a particular life goal or milestone. Life-sustaining measures are being used to such an extent that acute causes of death have virtually been eliminated in the developed world. Our absolute dependence on rapidly expanding medical technology means that, while a quick death might be cheated, as mentioned previously, we endure lengthy suffering from the increase in chronic and degenerative disease. The idea that our society prefers to cheat or postpone death indicates, at the extreme end, an attitude that there should be no limits to medical care because of the sanctity of life. Attitudes to the sanctity of life are directly related to the meaning and value of death. Sanctity of life is embedded in most of our social structures, most prominently in our legal and health care systems. However, the general interpretation by the courts in Australia is that while the principle of sanctity of life is very strong, it is not absolute. 30 Palliative care professionals, in particular, have increasing responsibilities in caring for growing numbers who are dying and comforting the bereaved family and friends. However, it should not be left to the sole responsibility of palliative care teams to address end of life decision-making. Irrespective of personal attitudes to the meaning and value of death, it should be that all the health care team leading up to the time of palliation will respect all patient‘s wishes and respond to the ultimate problem of death in a thoughtful and caring manner by acknowledging rituals that reflect and advance values of human worth, dignity and enduring connection. 5.4 Can health professionals object to treating a patient on the basis of conscience? Under a range of legislation, even if a patient with capacity requests it, individual health professionals are not obliged to give treatment which, in their view, contravenes good medical practice. Also, in very limited circumstances, medical officers are excused from providing care to a patient that goes against their conscience or clinical judgement. In the case where health professionals have a conflict of interest or object on the grounds of conscience, this must be declared as early as possible to ensure the patient receives appropriate hand-over to another medical officer and/or health care team. Where a medical officer disagrees with a statutory health attorney or the Adult Guardian about the patient‘s best interests, there are legislative provisions in place that set out procedures for dispute resolution. 31 If this arises, the dissenting health professional‘s views should be communicated to the health care team so if the situation arises where conscientious objection is needed on the part of a 30 31 Kerridge, I., Lowe, M. & McPhee, J. (2005). p. 263. Guardianship and Administration Act 2000, s. 145 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 20 of 61 medical officer, a back-up clinician, or team identified to accept responsibility for the patient‘s care can be put in place. In some cases, it may be necessary to get a second opinion, preferably from a clinican with specific expertise, to provide a more independent view about withholding or withdrawing a particular treatment. This particular step could consume valuable time, particularly in the case of an acute emergency. While health professionals objecting on the basis of conscience is acceptable, it should be declared at the earliest possible time so that there is no risk of harm to the patient 5.5 Can resource allocation be used as a justification for withholding or withdrawing medical treatment?32 All health professionals not only have an ethical duty to make the best use of available resources. They also an explicit responsibility to provide equity of access to the health care system. However, making the best possible use of resources inevitably means that some patients, whose lives might potentially be prolonged, may not receive all possible lifesustaining treatment. Decisions around life-sustaining measures must represent an appropriate balance between the clinical and resource needs of different patients, while having regard to the availability of medical treatments, particularly in acute settings. Increasing levels of technology not only present ethical dilemmas about assessing when treatment ceases to benefit the patient, but also raise the issue of cost when the decision is made to withhold or withdraw a particular treatment. Where funds are limited, individual facilities, medical officers and patients all compete for sometimes scarce resources. Particular difficulties could arise if, for example, patients or their families request lifeprolonging treatment to be continued for as long as technically possible, even though there is no hope of recovery. Complying with such requests could well be at the expense of other patients who have a reasonable chance of recovery if treatment is provided. Taking account of all relevant factors including obtaining consent, the decision about whether to withhold or withdraw life sustaining measures will ultimately be made by the medical officer responsible for the patient‘s care, with advice from the rest of the health care team. This is part of the difficult role health professionals face daily - balancing decisions about resources and allocating them to patients in need. Some of this decision-making also takes into account the likelihood of prolonging life leading to a significant recovery for one patient against the likelihood of merely delaying death for a short period of time or prolonging the dying process for another. Although it is highly unlikely the courts would expect all possible treatment to be given to prolong a life irrespective of costs or the impact on other patients, the onus is on the most senior medical officer of the treating team to clearly articulate the decision-making that led to the final outcome. Meticulous recordkeeping is crucial in these circumstances. The duty of care owed to all patients who lack capacity is to act in their best interests. The allocation of resources to ensure this is afforded to every patient represents decision-making at its most difficult. The demands on limited resources and the concomitant but competing best interests of other patients are factors that will feature in all decision-making about lifesustaining measures. Although the courts have given little guidance, using resource allocation as an excuse for withholding or withdrawing life-sustaining measures would most likely be challenged legally, and, arguably, serious charges could be faced under a range of different legislation. A number of legal cases have examined the provision of medical treatment on the grounds of such things as futility (most notably the Bland case33). However, the legal implications of using resource allocation in defence of a decision to withdraw a life sustaining measure is yet to be tested. 32 33 Sourced from the British Medical Association‘s Withholding and Withdrawing Life-sustaining Measures, 2007 Airedale NHS Trust v Bland [1993] AC 789 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 21 of 61 Decision-making regarding life-sustaining measures must be based on the patient‘s best interests, underpinned by good medical practice. While it is acknowledged that balancing competing interests is profoundly complex, the extent of the duty of care for the entire health care team would be judged on a case-by-case basis if the decisions were to be tested by the court. Concluding resources are too costly to keep the patient alive simply because the treatment is ‗futile‘ treads a dangerous legal path and is fraught with ambiguity and both clinical and moral complexity.34 Particular care needs to be taken to ensure that all decisions have been carefully considered, based on an individual‘s care needs, and not made on the basis of unjustifiable discrimination (both of the patient as an individual and of the patient compared to others). Decisions regarding life-sustaining measures must always be well-supported by clinical evidence, second or expert opinions, and by reference to Queensland Health documents and other relevant national guidelines. Should there be any doubts about a particular course of action expressed by any member of the health care team, or expressed by a member of the patient‘s family, these concerns should be discussed with senior clinical and managerial colleagues and referred to the Office of the Adult Guardian should the patient lack capacity. All records should be kept in the patient‘s file and later referred to the hospital area ethics committee. Resources for gravely ill or irreversibly and severely brain-damaged patients who will never recover cannot be allocated to treat other patients, and this exceptionally difficult ethical dilemma will necessarily comprise some decision-making about life-sustaining measures. For example, does a patient who suffered severe trauma at a young age and now lives in a disability long-term facility meet this criteria despite maintaining an acceptable base-line functioning? The British Medical Association 35 have also addressed some of these issues in their guidance, but do not provide definitive advice, ultimately leaving the final decisions to the medical officer in charge, supported by the health care team. ‗It is very concerning that the reality is, that cost factors probably have a disproportionate influence on decision making for this very vulnerable patient group and it is also concerning that the lack of a clear societal consensus on this most vexed area may unfairly leave medical officers open to criticism.‘ 36 The legal system, in Australia (and the UK), provides guidance only insofar as: should health care professionals not do the best for a patient with resources that are genuinely available, breaches of care standards would occur, likely resulting in negligence claims. In broad terms, however, the Civil Liability Act 2003 (Qld) provides four principles which apply in deciding whether a public authority (such as a hospital) has a duty or has breached a duty: 1. the functions required to be exercised by the authority are limited by the financial and other resources that are reasonably available to the authority for the purpose of exercising the functions; 2. the general allocation of financial or other resources by the authority is not open to challenge; 3. the functions required to be exercised by the authority are to be decided by reference to the broad range of its activities (and not merely by reference to the matter to which the proceeding relates); 4. the authority may rely on evidence of its compliance with its general procedures and any applicable standards for the exercise of its functions as evidence of the proper exercise of its functions in the matter to which the proceeding relates. 34 Kerridge, I., Lowe, M. & McPhee, J. (2005). p. 257. British Medical Association (2007). p. 79. 36 Ibid., p. 80. 35 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 22 of 61 Health professionals should never use lack of current or indeed future resources to deny treatment for any patient. To do so establishes a conflict since, in essence, the choice to treat the patient (or not) is being compared with the treatment for another (future) patient whose condition is unknown. Each patient should be assessed on a case by case basis, taking all the clinical factors into consideration. In the case where two patients share the need for the same limited resource, which is adequate for both, ‗the patient with the greater clinical need should have the first access. This is the essence of triage.‘ 37 It is important to acknowledge that medical officers are well placed to make informed decisions about patient care that can include economically smart choices, as long as patient care does not suffer. Regrettably, a common misconception held by family regarding withdrawal of medical treatment is that medical staff do so to ‗free the bed‘ for someone else. Doctors are advocates for their patients, and are bound to act in their best interests, both by law and by adhering to the standards of good medical practice. Their primary duty is always to the patient they are treating, and the care of that patient will not be compromised for the care of another potential patient. Education and counselling about the indications for withholding or withdrawal of medical treatment are probably the best way to help the family come to terms with the prospect of withdrawal of medical treatment and for continued trust in the health care team. 5.6 Euthanasia In Queensland, euthanasia is unlawful to the extent that it constitutes killing under the Queensland Criminal Code 1899.38 Euthanasia and assisted suicide both involve deliberate acts or omissions that are undertaken with the intention of ending a person‘s life and are inconsistent with the duty of care of a medical practitioner or other medical professionals. Both euthanasia and assisted suicide are criminal offences and are not endorsed by this document, nor by Queensland Health. Euthanasia itself has many definitions. The most common definition is: 'Any action or omission intended to end the life of a patient on the grounds that his or her life is not worth living.' Some look toward a ‗modern‘ definition which states that euthanasia is: 'A good death brought about by a medical officer providing drugs or an injection to bring a peaceful end to the dying process‘. Three classes of euthanasia can be identified: passive euthanasia, physician-assisted suicide and active euthanasia,although not all groups would acknowledge them as valid terms. 39 Proponents of euthanasia believe it is the compassionate choice, and supported by the same constitutional safeguards that guarantee such rights as marriage, procreation and the refusal or termination of life-saving medical treatment. Proponents feel the language of the often-cited Hippocratic Oath negates the reality of terminal disease, and believe that terminally ill people should have the right to end their pain and suffering with a quick, dignified death. Margaret Sommerville‘s article in the Australian Medical Journal in 2003 sparked controversy over a number of issues. 40 Sommerville‘s position is that the argument put forward by advocates of euthanasia that how we die is a ‗private matter‘, is flawed. Those against euthanasia believe death is never in isolation. Even if someone does not have family or friends, their death involves healthcare professionals, and therefore societal values and symbols. Therefore, where euthanasia is involved, death is no longer ‗…a private matter of 37 Kerridge, I., Lowe, M. & McPhee, J. (2005). p. 559. Queensland Criminal Code 1899, s. 284 & Chapter 28. 39 "Euthanasia Special Report," www.bbc.co.uk July 1, 1999 40 Sommerville, M. (2003)."Death talk": debating euthanasia and physician-assisted suicide in Australia. MJA 2003 178 (4): 171-174. 38 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 23 of 61 self-determination and personal beliefs because euthanasia is an act that requires two people to make it possible and a complicit society to make it acceptable.‘ 41 Opponents of euthanasia use the ‗slippery slope‘ argument and see little difference between it and murder, and challenge that any test to differentiate between voluntary and non-voluntary cases will ultimately fail. They also cite the Hippocratic Oath, arguing that medical officers have a responsibility and a sworn duty to keep their patients alive. Many opponents believe that legalising euthanasia will unfairly target the poor and disabled, groups with little access to advanced. possibly life-saving medical care. At the core of the debate between proponents and opponents of euthanasia is how to reconcile competing values - the desire of individuals to choose death with dignity when suffering, and the need to uphold an inalienable right to life of every person, as recognised by article 6(1) of the UN‘s International Covenant on Civil and Political Rights. Queensland‘s Criminal Code 1899, sections 284, 296 and 311 states: (284) Consent by a person to the causing of the person‘s own death does not affect the criminal responsibility of any person by whom such death is caused. (296) A person who does any act or makes any omission which hastens the death of another person who, when the act is done or the omission is made, is labouring under some disorder or disease arising from another cause, is deemed to have killed that other person. (311) Any person who — (a) procures another to kill himself or herself; or (b) counsels another to kill himself or herself and thereby induces the other person to do so; or (c) aids another in killing himself or herself; is guilty of a crime, and is liable to imprisonment for life. While health professionals generally understand the distinctions between euthanasia, physician-assisted suicide, and the withdrawal of life support, the public tends to confuse these terms, potentially leading to misinterpretation and often intense media scrutiny. The withdrawal of life support when it has been deemed potentially futile is widely upheld as legal by the courts through landmark cases (for example, the Bland case). The uncertain legal status of euthanasia and physician-assisted suicide is determined partly by the attitudes of the public about end of life issues such as the meaning and value of death. For example, studies in the US have shown that while 90 percent of the public would endorse withdrawal of life support in the case of terminal illness, there is much less support for active euthanasia and physician-assisted suicide.42 A study by psychologists in New Zealand also found that while physicians would provide information to patients enquiring about euthanasia, they were far less inclined to be actively involved. 43 5.7 Assisted suicide Although a distinction is often drawn between physician-assisted suicide and active voluntary euthanasia, in general the moral issues that arise are common to both. 41 Ibid. Batlle, J.C. (2003), p. 2280 43 Mitchell, K., & Owens, R.G. (2004) ―Judgments of laypersons and general practitioners on justifiability and legality of providing assistance to die to a terminally ill patient: a view from New Zealand‖. Patient Education and Counseling 54 (2004) 15–20 42 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 24 of 61 Orentlicher (2001) believes ‗…there is no morally significant difference between the act of treatment withdrawal and the act of suicide (or assisted suicide). What matters is whether the person has made a morally justified decision to hasten death‘ (p. 59). The gradual extension of legal rights in the end of life arena has led to the current debate over physician-assisted suicide. On one side of the debate, proponents of physician-assisted suicide seek to show that there is no moral difference between withholding lifesaving treatment and providing a patient the means to end life. On the other side, opponents argue that the artificial hastening of death is unlike allowing the unhindered progression of a terminal illness. However, the courts generally hold that an individual's right to self-determination, including choices about death, outweighs a normative societal interest in the sanctity of life. ‗Advocates of physician-assisted suicide argue that it has the advantage of reassuring terminally ill patients that they can continue living in the knowledge that they can end their own lives if and when they choose; and that because they die by their own hands, their action is likely to 44 represent a voluntary and informed choice.‘ Depending upon where one stands on the moral justification argument, assisted suicide is seen as different from withholding or withdrawing life-sustaining treatment in accordance with good medical practice by a qualified medical practitioner. When medical treatment is withheld or withdrawn, and it causes the death of a patient, the law generally regards the cause of death as the patient‘s underlying condition rather than the actions of others. Patient autonomy and the right to choose one‘s destiny is a core right in our society. This principle is upheld in all decisions underpinned by good medical practice. If it is accepted that it is a fundamental right of all persons to choose the manner and timing of treatment at the end of life, it must be ensured that this choice is a genuine expression of the patient‘s autonomy. ‗Autonomy is not served if the person chooses to die out of incompetence, irrationality, mistake, fraud or coercion. Accordingly, before we honour a patient‘s request for life-shortening action, whether a treatment withdrawal or an assisted suicide, we would want to confirm that the request is a valid exercise of self-determination.‘45 Nonetheless, the legal and medical debate over the ethics of physician-assisted suicide continues and the controversy comes in a variety of forms. These guidelines will not enter into, nor discuss the vast range of considerations for assisted suicide. If the academic, medical and legal community have difficulty agreeing on categorical distinctions between treatment withdrawal and assisted suicide, then this guideline can do no better than raise the broad issues, and at the same time, reiterate Queensland‘s laws in relation to this matter. Suffice to say that many of the arguments hinge on the genuineness of reasons behind making a decision to commit suicide. The decision tends to be more readily accepted where the person is gravely or terminally ill, but doubts cloud the decision where this is not the case. 44 45 Kerridge, I., Lowe, M. & McPhee, J. (2005). p. 368. Orentlicher, 2001, p. 63 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 25 of 61 6.0 SPECIAL CONSIDERATIONS 6.1 People with special needs End of life decision making, particularly resuscitation planning, is among the most difficult in medicine. When directly related to those in our community that require special consideration, it is even more complex. The six following groups are identified as requiring further guidance in discussing end of life issues: 1. The elderly 2. Children and adolescents (to be covered in separate policies and guidelines expected to be available by the end of 2010. 3. Mental health patients 4. People with disabilities 5. Aboriginal and Torres Strait Islander people 6. People from other cultures The information presented in this section is provided for context around end of life decisionmaking and is not intended to be a detailed or thorough study of each group. It highlights important issues for clinicians to consider when making decisions about life-sustaining measures for people in these special groups. 6.1.1 The elderly Despite the popular perception, neither end of life care, nor its accompanying decisions about life-sustaining measures is exclusive to the elderly. However, the proportion of elderly people in developing countries is increasing and deserving of special consideration in the context of discussions about withholding and withdrawing life-sustaining measures. Clinical and ethical issues about the elderly are expected to gain increasing prominence in the next couple of decades. In providing end of life care to the elderly, health professionals must be mindful of a number of biases that may affect the thinking of any of those involved in making the decisions. These include: a common, but unspoken ethical concern, that health resources should be rationed for the elderly so that they could be used elsewhere where they might ‗do more good‘ 46 the fact that some younger members of society undervalue many aspects of the lives of elderly people the belief that elderly people use a disproportionate share of the medical resources available. It is Queensland Health‘s policy that decisions to withhold or withdraw life-sustaining measures must be made on a case by case basis, and age or race or lifestyle must never be used to qualify these decisions. The elderly, like other demographic groups in our society, are deserving of value, care and respect. The health care team must always consider that the interests of the elderly may not necessarily be the same as the interests of their families, health professionals or health institutions. 46 Kerridge, Lowe & McPhee, 2005, p. 300 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 26 of 61 It is very likely that that an elderly patient, particularly one with dementia, will have a substitute decision-maker. While it is expected that the majority of these will do their best for their loved one, a number of commentators have raised significant ethical issues relating to elder abuse and exploitation by seemingly well-intentioned substitute decision-makers. Many of these involve financial opportunism at a time when an elderly person is most vulnerable rather than decisions and actions that cause them physical harm. Such issues can rarely be solved through single-dimension approaches, but if the health care team has evidence of or suspects that the substitute decision-maker for an elderly person who lacks capacity is not in accordance with the Health Care Principle (see Glossary), they may refer the matter to the Office of the Adult Guardian. The medical officer responsible for the patient‘s care in these instances must use his or her best judgement to ensure good medical practice and evidencebased decision-making underscore all decisions about life-sustaining measures for an elderly patient. Elderly patients should be encouraged (but never forced) to take part in advance care planning to ensure their wishes for end of life care can be respected. If they have an Advance Health Directive, care should also be taken to ensure it is reviewed regularly and updated as necessary. They may have completed an Advance Health Directive at a time when their condition was different to when they lose capacity. While protections are afforded to medical officers who do not comply with a person‘s valid Advance Health Directive, this is an exceptionally vexed area where clinical practice potentially collides with the legal framework. A medical officer may override a person‘s valid Advance Health Directive if it is uncertain, not relate to the circumstances of the patient‘s current medical condition or medical advancements cause the original directions to be inappropriate. 47 In these circumstances, the medical officer is also required to consult with the patient‘s nominated substitute decisionmaker. Providing encouragement for elderly patients to regularly review directions in their Advance Health Directive while they are capable, represents the most responsible approach, given Advance Health Directives are not time limited. 6.1.2 Children and adolescents Children and adolescents (under 18 years of age) are not covered under Queensland‘s guardianship laws48, and therefore, at this time are excluded in guidance documents associated with withholding and withdrawing life-sustaining measures. The basis for decisionmaking about life-sustaining measures for children is derived from common law, rather than the specific statutes in the guardianship laws. The common law test to be applied for children is whether they have sufficient maturity and understanding to make decisions for themselves. If not, parental or guardian consent is required. If they have impaired capacity then the Family Court or a Supreme Court can become involved in making decisions for them. Separate policies and guidelines about withholding and withdrawing life-sustaining measures from children and adolescents (including neonates) are expected to be available in 2011. 6.1.3 People with disabilities End of life care for people with disabilities poses unique challenges. It requires that clinicians, families and ethicists be aware of biases that influence decision-making, particularly in acute 47 48 S.103 Powers of Attorney Act 1998 Guardianship and Administration Act 2000 and Powers of Attorney Act 1998 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 27 of 61 settings where the aim is primarily cure and return to optimal functional level. Because a person has a disability, it should not be assumed they are unable to contribute to decisionmaking about end of life choices. Three categories of disability are referred to in the literature concerning end of life care: 49 1. A person who has lived with a disability from birth or early life, due to trauma or disease, and is now faced with a serious illness that requires life-sustaining treatment. 2. The otherwise healthy person who acquires a disability through an acute event of disease or trauma and whose condition requires that life-sustaining treatment decisions be made. 3. The person who has lived with a progressive chronic illness, such as lung or heart disease or amyotrophic lateral sclerosis, and may have gradually adjusted to disabilities imposed by the condition and now is faced with life-sustaining treatment decisions. It is widely documented that both older people and those with decision-making disabilities can encounter discrimination when they seek medical care. Just as ageism and stereotypes about older people may inappropriately limit medical care for the elderly, limits may be placed on medical care merely because of the presence of a disability. It is Queensland Health‘s policy that decisions to withhold or withdraw life-sustaining measures from every patient must be made on a case-by-case basis, and age or race or lifestyle must never be used to qualify these decisions. When people with decision-making disabilities reach the end of life, decision-making must incorporate an underlying respect for their autonomy in the broadest sense and also ensure no harm is done. It is important for clinicians to be objective as well as compassionate, and to strive to know the patient as well as possible. In this way important information from the patient, their families, friends and carers, which will include their legal substitute-decision maker (who may also be their formally appointed guardian), can be gathered to create a picture of who the person is and what their choices may be for end of life care. Respect for the values and lives of people with disabilities enhances clinicians‘ ability to assist disabled patients, their families and other members of the health care team to realise the patient‘s possibilities for continued life and peaceful death. Factors that impede clinicians‘ abilities to provide a range of clinical options for people with decision-making disabilities and their substitute decision-makers range from extreme positions of pity for the imagined plight of the disabled person to reservations about changing course to palliation because of fear of criticism from a multitude of legal and political sources. These factors can immobilise the clinicians‘ sense of agency to support and facilitate decisionmaking and to care effectively for persons with disabilities at the end of life. Clinicians should follow the usual steps for making end of life treatment decisions (see section 4.6) and carefully document the process. In the clinical context, a number of international ethicists have pointed out that using futility as the basis for clinical decision-making for disabled persons is fraught with ambiguity.50 Clinical assessments based on potential futility are inherently value laden – they are not objective 49 Robinson, E.M. et al, (2006). Complexities in Decision Making for Persons with Disabilities Nearing End of Life. Topics in Stroke Rehabilitation. 13(4): 54-67. 50 Werth, J.L. (2005). Concerns about Decisions Related to Withholding/Withdrawing Life-Sustaining Treatment and Futility for Persons With Disabilities. Journal of Disability Policy Studies. Summer 2005; 16, 1: pp 31-37. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 28 of 61 medical decisions – and at times the values of the patient and the health-care team may be in opposition, especially if the emphasis is on perceived quality of life.51 6.1.4 Mental health patients In Australia, there is a common-law right for competent patients to refuse medical treatment, including life-sustaining treatment. In Queensland, this right has received statutory recognition if a person completes an Advance Health Directive specifying they do not wish to be subjected to invasive life-sustaining, or life-prolonging medical treatment. Queensland‘s guardianship legislation begins with the presumption of capacity, therefore every person is entitled to be considered to have capacity to make decisions about health matters affecting them unless an assessment is made that they do not have capacity. It is recommended that patients with active mental illness including depression should have their decision-making capacity carefully evaluated. Capacity to make treatment decisions often fluctuates over the course of mental illness. For example, a patient‘s capacity to understand treatment options can be impeded by psychiatric symptoms or cognitive dysfunction. Similarly, individuals with schizophrenia may have acute psychotic symptoms or long-standing thought disorders that can impair their ability to make informed decisions. 52 It should be noted that, while in the grip of major depression, patients may make different decisions from what they would make otherwise. Major depression should be treated before a patient is asked to undertake advance care planning. If doubt exists about a patient's capacity, or where it is believed major depression is present, psychiatric consultation should be arranged. In the absence of an Advance Health Directive (completed before the onset of depression), severely depressed patients' decisions to refuse life-sustaining medical treatments should be treated with the utmost caution until attempts are made to treat the depression. Researchers point out that the diagnosis of major depression in the gravely ill is very difficult. 53 Low spirits are to be expected in serious illness, and many of the other features of major depression (such as weight loss and sleep disturbance) are also common in physical illnesses. Further, according to Ryan (1996), the difficulty of diagnosis is reflected in studies that reveal that non-psychiatrically trained doctors miss up to half of cases of major depression in the medically ill. However, it is the case that major depression is eminently treatable. If it can influence the seriously ill to refuse treatment, then some of those who do refuse treatment might be depressed and might change their minds if the depression were treated. For mildly depressed patients, researchers suggest that ‗it appears reasonable‘ to respect their wishes for end of life decision-making.54 In all cases where depression (minor or major) is suspected, it would be prudent for medical officers to err on the side of preserving life and treat patients suffering major or moderate depression before respecting a refusal of lifesustaining treatments. The difficulties presented by a depressed patient with fluctuating capacity who refuses lifesustaining treatments must be taken on a case by case basis, with guidance of clinicians experienced in the area of depressive illness. 51 Ibid. p. 35. Ibid. p. 579 53 Ryan, CJ. ‗Depression, decisions and the desire to die‘. MJA 1996; 165: 411 54 Hooper, S., Vaughan, K., Tennant C., & Perz J. ‗Major depression and refusal of life-sustaining medical treatment in the elderly.‘ MJA 1996; 165: 416-419 52 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 29 of 61 Life-sustaining measures are withheld or withdrawn in situations where their commencement or continuation would be potentially futile and provide no benefit to the patient. The decision to withhold life-sustaining medical treatment that is considered potentially futile will be based upon many factors besides patient preference. However, when a treatment is considered not potentially futile, patient refusal is usually central to a decision to stop. Doctors responsible for patients in these situations have a duty to ensure that the refusal is not motivated by a major depression. Given the difficulties of accurate diagnosis, should there be any doubts about the patient‘s mental status as it relates to depressive states, it is best to seek an opinion from a more experienced clinician, preferably a psychiatrist to review the patient. If an Advance Health Directive is made while a patient is in a depressive state, it is unlikely to be a valid indication of that patient's future preferences. 55 6.1.5 Aboriginal and Torres Strait Islander people On average, Aboriginal and Torres Strait Islander Australians die a great deal younger than the wider Australian community and have much higher rates of poor health outcomes. Aboriginal and Torres Strait Islander people have the lowest life expectancy of any minority in a first world country. Only 2.6 percent of the Aboriginal and Torres Strait Islander population will pass the age of 65. Unexpected deaths in this Aboriginal and Torres Strait Islander community are common. Advance care planning offers a wide range of benefits to Aboriginal and Torres Strait Islander patients with chronic illnesses and their families, not least being the reassurance that their end of life wishes will be respected. Aboriginal and Torres Strait Islander peoples are not an homogenous group. Like the many nations of Europe, Aboriginal and Torres Strait Islander peoples comprise a large number of diverse, culturally different communities. Each community has its own unique customs, cultural beliefs and associated ceremonies. Although there are degrees to which Aboriginal and Torres Strait Islander people are connected to their traditions, the concept of community and the central place of land and family obligations are common underpinning values within and across Aboriginal and Torres Strait Islander communities throughout Australia. Family extends to distant relations, with obligations and responsibilities to all members and others within the community. ‗Family‘ members may not be related according to the mainstream notion of blood relatives, but be related through traditional kinship or cultural groupings. Family and/or community support is likely to be very important to the patient. Many Aboriginal and Torres Strait Islander people express a desire to die in their own communities (Sullivan 2003). This can be more important to them than the treatment of their disease. Having to move from from isolated communities to regional or metropolitan centres for treatment or care can result in significant impact and trauma, not only for the Aboriginal and Torres Strait Islander individual, but also for their families. Flexible models of health care for those at the end of life should allow Aboriginal and Torres Strait Islander people the choice to return to their place of birth. Care which may make the Aboriginal and Torres Strait Islander peoples more comfortable may be less of a priority than the cultural and family support needed for spiritual wellbeing. A deeper understanding of Aboriginal and Torres Strait Islander peoples culture and history can be obtained through personal relationships with Aboriginal and Torres Strait Islanders and cultural awareness and cultural education programs conducted by Aboriginal and Torres Strait Islander peoples themselves. 55 Ryan, CJ. ‗Depression, decisions and the desire to die‘. MJA 1996; 165: 41 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 30 of 61 In discussions about end of life matters, information given to the Aboriginal and Torres Strait Islander people and/or their family/community should include the range of choices available to them. Knowing the choices and positives/negatives of the choices will assist the Aboriginal and Torres Strait Islander people and/or family to: make an informed decision about what is best for them – even if it means not accessing available services plan for time away from home plan for family members to accompany the patient prepare for what is likely to happen in relation to the illness. Many Aboriginal and Torres Strait Islander people tend to be depressed and sometimes angry when they encounter the mainstream health care system. This is not a response to their individual situation, more a case of the ongoing grief and trauma issues within their life as an Aboriginal and Torres Strait Islander person and the aftermath of dealing with a host of other problems. Stress, social fragmentation and financial pressure can be experienced by the family when the patient needs to be accompanied by another family member or members. The Practice Principles from the National Palliative Care Program 56 recommend the following implementation strategies when discussing end of life care with Aboriginal and Torres Strait Islander people: 1. Include Aboriginal and Torres Strait Islander organisations and/or personnel in the planning, provision and monitoring of palliative care to ensure culturally relevant requirements are addressed and preferences of the patient and/or their family are considered. 2. Communicate with the patient and their family and community in a sensitive way that values cultural difference. 3. Provide training to all personnel to enable the provision of culturally appropriate palliative care to Aboriginal and Torres Strait Islander peoples. The National Palliative Care Program also provides important resources to discuss end of life matters with Aboriginal and Torres Strait Islander people. 57 They raise the notion of ‗cultural safety‘ as an important aspect of discussing medical treatment with Aboriginal and Torres Strait Islander people. Cultural safety is practice which respects, supports and empowers the cultural identity and wellbeing of an individual, and empowers them to express identity and have their cultural needs met. Cultural safety recognises that every person brings a set of values and beliefs to all interactions with other people and all that they do. Each clinician will bring values and perspectives from their own culture to the situation. Sometimes these can be obvious; sometimes they are so subtle the clinician may not even be aware there can be an impact on the patient. The following list identifies factors to consider in reflecting on individual practice for cultural safety: differences in communication styles – culturally safe/secure communication requires an understanding of the unique styles of communication that are part of Aboriginal and Torres Strait Islander culture (the use of eye-to-eye contact, for example, may be considered a sign of disrespect by some Aboriginal and Torres Strait Islander people) differences in notions of family – for many Aboriginal and Torres Strait Islander people, extended family networks include people who may be only distantly related in non- 56 Website: Caresearch: The palliative care knowledge network, http://www.caresearch.com.au/ caresearch/ http://www.caresearch.com.au/Caresearch/Portals/0/Documents/WhatisPalliativeCare/NationalProgram/Indigenous PCproject/PracticePrinciples.pdf (p.17) 57 Website: Website: Caresearch: The palliative care knowledge network, http://www.caresearch.com.au/caresearch/http://www.caresearch.com.au/Caresearch/Portals/0/Documents/Whatis PalliativeCare/NationalProgram/IndigenousPCproject/Resource.pdf Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 31 of 61 Aboriginal and Torres Strait Islander peoples terms, yet are identified by Aboriginal and Torres Strait Islander peoples as ‗brother‘, sister‘, ‗uncle‘, ‗auntie‘, etc. Elders can hold a special place within ‗kinship‘ or ‗family‘ differences in concepts of spirituality – for many Aboriginal and Torres Strait Islander people, spirituality includes a special relationship with the land, as well as religious beliefs, notions of self and one‘s place in life. Each person will have unique spiritual requirements that are integral to the provision of medical care differences in reactions to people and the environment differences in life circumstances, family history and community differences in education and understanding of language – lower levels of education for some Aboriginal and Torres Strait Islander people may impact on their understanding of the complicated treatments and drug regimes often used to manage a terminal illness. For some more traditional Aboriginal and Torres Strait Islander people, English may be a second, third or fourth language differences in attitudes, understanding of, and approaches to, death, dying and bereavement – for some Aboriginal and Torres Strait Islander peoples, death and dying are marked by elaborate ceremonies that are extremely important and take precedence over all other activities. Death in some Aboriginal and Torres Strait Islander communities is attributed to supernatural influences which may be at odds with mainstream approaches to medicine differences in understanding of palliative care, medical terminology and the nature of illness different experiences with health organisations and bureaucracy – for example, among Aboriginal and Torres Strait Islander people (particularly older people), historical factors may have contributed to negative perceptions and distrust of the mainstream health system and a reluctance to access services differences in values and notions of ‗how things should be done‘. (Providing culturally appropriate palliative care to Aboriginal and Torres Strait Islander peoples: Resource, The National Palliative Care Program, Australian Government Department of Health and Ageing, pp. 15-16) 6.1.6 People from other cultures Culture, for the purpose of this guideline, may be defined as: ‗a complex, learned, shared system of human behaviour, rituals and symbolism‘. Despite the difference between cultures, there are usually common interests that may serve as starting points for discussion. In most cultural groups, the family has traditionally been the main source of security, assisted by adherence to their religious or spiritual beliefs. Migration from the country of birth cuts off many support systems and reduces the recognition and celebration of symbolic events. This can increase the sense of alienation and helplessness at times where difficult decisions are required. People from other cultures arrive in Australia for a variety of reasons. Mostly the decision to relocate is voluntary, but sometimes it is not. Once living in Australia, people who are displaced from their birth country tend to live in the same vicinity to retain their traditional community support. It is to this community support that people often turn to if they are faced with difficult end of life decision-making. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 32 of 61 The sometimes startling differences in approaches to death and dying for the various multicultural groups means that clinicians treating patients who identify with another culture must be mindful about how the subject can be approached with the family. Generally, many cultural groups approach religion and spirituality very seriously. There are a number of religions that cross language and cultural boundaries, so it is important when working with a person facing a life-threatening illness and their family to not assume anything, and to understand where religion fits within the spectrum. There are many for whom religion in the context of their life in Australia does not have as significant a role as it may have in their homeland. However, when faced with a life-threatening illness and the possible or subsequent death of a family member or friend, religious practices, rituals and beliefs may resume their importance. It is important for health professionals and others to acquire some knowledge about these issues to ensure a sensitive approach when working with people facing terminal illness, their family and friends. The notion of ‗cultural safety‘ is often referred to in recent literature about health care for people from other cultures. Cultural safety acknowledges that the culture of the provider can adversely impact on the recipient if there is a power imbalance. People from all cultural backgrounds may feel disempowered for many reasons, including: lack of medical knowledge lack of understanding of the illness and/or treatment/support care strategies not being involved in care planing unfamiliarity with the care environment (for example, a hospital/hospice) perceived social inequality differences in lifestyle lack of literacy/numeracy skills (for example, understanding medicine dosage) previous negative experiences with health care, and having heard negative stories from relatives about their experiences with health care. Health professionals should consider the following approaches when caring for patients from other cultures and communicating with their families: 58 conduct a family meeting. The key decision-maker may not be the same person as the primary caregiver. Be aware of family dynamics, and power relationships although people with a moderate comprehension of English may appear to understand discussions, use a professional interpreter to communicate complex medical information use written material to help disseminate information to all family members and others introduce information gradually using non-medical terminology and assess if it is being understood. invite questions when providing information to patients, family and friends. The questions may indicate some information about the speaker, as well as clarify their expectations be aware of possibly high expectations that doctors and nurses will be able to completely relieve all symptoms. ensure the family and the patient understands the range of choices available to them. This will assist them to make an informed decision about what is best for them reinforce to the family that the patient can be more in control if better informed 58 Palliative Care Australia. Andrew Taylor & Margaret Box. 1999. Multicultural Palliative Care Guidelines http://pallcare.org.au/Portals/46/Multicultural%20palliative%20care%20guidelines.pdf Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 33 of 61 offer the family the opportunity to have a priest or religious adviser in attendance, to assist with prayer and other rituals do not hesitate to ask about other relevant cultural aspects. It is respectful to show an interest in other cultures identify and respect protective behaviour allow time for and be aware of customs that show respect. This will help to establish a strong rapport with the patient, family and their friends attempt to accommodate, within reason, a large numbers of visitors for a hospitalised patient do not assume that patients will have an extended family that is able to support the dying person. Seek out culturally specific community services. Where these are not available, discuss patient and family needs with local service providers although emotional support may be declined, recognise anxious behaviour and assess if this is an appeal for help attempt to establish beliefs and fears surrounding pain-relieving medication, and show sensitivity and understanding towards patients who may resist using pain medication use published material to educate the patient and family regarding the benefits of morphine and to dispel myths recruit assistance from other community services if necessary if a referral to community services is initially declined, seek further opportunities for referral. 6.2 Organ and tissue donation Although research shows 80 percent of Australians support organ and tissue donation, only 30 percent have registered to become donors (see page following for further facts and statistics about organ and tissue donation in Australia). Fifty percent of those registered to become donors never donate because their family do not consent to organ donation. One reason for the discrepancy between supporters and actual donors is the fear that medical personal will not ‗give it their all‘ if they know someone is a registered donor. There is a popular fear that doctors will prematurely withdraw treatment if the patient is an organ donor. The idea that a potential donor will be sacrificed for multiple recipients in a utilitarian fashion is an unfortunate misconception. A ‗potential donor‘ is usually identified after all measures to preserve life and to assist the patient in making a meaningful recovery have been attempted, and unfortunately the patient fails to recover. Unless the family or patient raises the issue of donation prior to patient death, the next of kin are usually approached for consent once the formal diagnosis of death has been made. The person best qualified to liaise with next of kin is either the senior doctor caring for the patient or the donor transplant coordinator. Treating doctors of the ‗potential donor‘, the transplant team and the treating doctors of the ‗potential recipient‘ remain separate entities. It is important that they remain as such for public and patient confidence and trust in medical professionals and the delivery of medical care. It is paramount that at all times the intentions and interests of each professional body are transparent, so that confidence in our medical system remains. Organ and tissue donation is one consideration among many that may face families of patients at the end of life. Careful and sensitive communication about the potential for organ and tissue donation is conducted by donor coordinators who are experienced in and passionate about this area. Further information and contact details are available from the Queensland section of the Donate Life website (http://www.donatelife.gov.au/TheNetwork/QLD.html). Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 34 of 61 Organ and Tissue Donation – Facts and Statistics* One organ and tissue donor can save the lives of up to ten people and significantly improve the lives of dozens more. Australia has a world class reputation for successful transplant outcomes. Australia also has one of the lowest donation rates in the developed world. About 80% of Australians support organ and tissue donation. 30% of Australians don't discuss their donation wishes with their family. 40% of Australians don't realise their family makes the final decision about donation. Around 1700 people are on Australian organ transplant waiting lists at any one time. On average, people on the transplant list must wait between 6 months and 4 years. In 2009, less than half of the demand for organs was able to be met. In 2009, 247 organ donors gave 799 Australians a new chance in life. In 2009, the Australian population had 11.3 donors per million people. In 2008 the Australian population had 12 donors per million; Spain had 34, the US 24, Estonia 23, Italy 21 and the United Kingdom 15. Australia has one of the highest retrieval rates per donor (3.4 organs per donor in 2008). Australia's rate of cornea donation puts it in the top five countries for corneal donation rates. In 2008, 1096 people donated their corneas. As a result, 1696 people had their sight restored. Each year, 3000-4000 skin, heart and musculoskeletal tissues are transplanted. Australians' donor record in 2009 The following statistics on organ donation in Australia have been compiled from the Australian and New Zealand Organ Donor Registry (ANZOD). These figures will be added to on publication of ANZOD‘s annual report. For more information, visit www.anzdata.org.au. 247 donors donated to 799 recipients The average Australian donor rate was 11.3 donors per million people. By state the rate was (per million of the population): South Australia: Tasmania: Northern Territory: Victoria: Western Australia: Queensland: Australian Capital Territory: New South Wales: 20.3 9.9 8.9 11.8 8.5 10.7 14.1 10 Australians' donor record in 2008 The following statistics on organ donation in Australia have been compiled from the Australian and New Zealand Organ Donor Registry (ANZOD) 259 deceased donors gave 889 organs, 356 living donors gave 353 kidneys and 3 part livers (see table below). 43% of kidney donations were from living donors. Donors ranged from 1.3 years of age to 82.3 years, with an average age of 44.7 years. 83% of organ donors donated more than one organ each. Of the organs that were donated, 97% of kidneys, 95% of livers, 93% of hearts, 98% of lungs and 40% of pancreases were able to be transplanted. Nine livers were sent to New Zealand for transplantation. The average Australian donor rate was 12 donors per million people . [*Sourced from the national Donate Life website http://www.donatelife.gov.au/Discover/Facts-andStatistics.html (accessed 11 April 2011)] Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 35 of 61 7.0 ADVANCE CARE PLANNING ‗Advance care planning is a process of planning for future health and personal care whereby the person‘s values, beliefs and preferences are made known so they can guide decision-making at a future time when the person cannot make or communicate their decisions. Advance care planning is usually undertaken within a health or aged care setting and with the assistance of trained professionals after a person has been diagnosed with life-limiting condition. It requires respect for the person and their autonomy.‘59 People have differing values, attitudes and beliefs about living and dying. For many people, some treatments, such as being placed on extended life support, may seem too painful or undignified if there is little hope of returning to a worthwhile life. Others may be willing to endure pain and loss of dignity because they strongly believe that while there is life there is hope. Advance care planning starts with an individual thinking about the future. This involves: knowing which health problems might occur their likely outcomes, and what treatments are available in each case. It also requires understanding that health care decisions often have to be made on the basis of probabilities rather than certainties. The next step is for the individual to discuss possible health problems and treatments with those who would be involved at the time, such as medical practitioners, carers, family members and others. This is in line with a worldwide trend towards taking a holistic approach. The outcome could be an oral or written statement of intentions so that family members, at least, know about acceptable treatments. The oral or written statement may be accepted by family members and health care providers as a simple advance care plan. Under common law, it may be recognised as evidence of the person‘s intentions. Alternatively, the individual may choose to formally record their wishes in a document. In Queensland, there are two more formal and legally binding options available: appointment of an attorney for personal matters and execution of an Advance Health Directive. Both options are only available to adults who have the capacity to make decisions for themselves and are only triggered when capacity is lost. People who complete Advance Health Directives have often been diagnosed with a chronic or life-limited illness or injury. They generally know the nature and understand the course of their diagnosed condition and want to record directions about preferred care or appoint a substitute decision-maker, or both. However, a high proportion of Advance Health Directives are completed by healthy people anticipating a future time when they might be unwell or involved in an accident and unable to make decisions. Their Advance Health Directives will apply in circumstances that are as yet unknown and difficult to predict. These people usually complete their Advance Health Directives in their home, often with support from family members or close friends. They are more likely to simply appoint a person they trust to make future decisions for them rather than record detailed directions. However it remains critically important that they discuss their personal values, preferences and any advance decisions with family and others close to them. Australian and international research indicates that Advance Health Directives are neither well-known nor widely understood outside of specific advance care planning programs. There are no figures available on how many Advance Health (Care) Directives are completed around Australia or how many end up being used for decision-making. However there is evidence that advance care planning programs are increasing the uptake of formal directives in health and 59 AHMAC National Working Group, A National Framework for Advance Care Directives, Consultation Draft, September 2009, [Under development] Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 36 of 61 aged care settings for people with a known condition. Recent studies indicate advance care planning can lead to treatment decisions that respect patient preferences and reduce hospitalisation rates at the end of life, especially for nursing home residents. Research increasingly indicates the important role of communicating preferences and personal values rather than focussing exclusively on completing legal forms. It is thought that advance care planning works well most of the time for most of the people who complete them, especially those that simply appoint a substitute decision-maker. However, formalising advance care planning through completing an Advance Health Directive cannot solve all the challenges of substitute decision-making. They cannot resolve all conflicts in families, nor can they guarantee a smooth decision-making pathway for the health and aged care sectors. It is also widely acknowledged 60 that the public promise of Advance Health Directives is not always realised, and that there are challenges for those writing, interpreting, applying and abiding by Advance Health Directives. Common problems have been identified when: healthy people struggle to write medical directions in advance of any diagnosis of disease of injury decision-makers try to interpret written medical directions that are uninformed, too specific to account for new treatments or too non-specific to guide medical decisions substitute decision-makers are confused by differing legal requirements and do not understand the principles that should guide their decisions people change their stated medical treatment preferences over time but fail to update their advance care plans, especially as priorities change towards the end of life; and medical officers do not respect written directions in an advance care plan or do not understand the rights of substitute decision-makers to make decisions. Because advance care directives are not yet the norm, end of life decisions for patients without capacity are frequently made in discussions between the patient‘s medical officer and family. Communication and decision-making in these situations is a complex interplay between available treatment options, knowledge of ethical principles, and, of course, legal considerations. Queensland Health has developed guidance in the form of brochures, booklets and a public website to inform about the benefits and considerations of advance care planning. While not all the material has been released at this time, what is provided in this first phase of the End of Life Project will assist patients and their families, and also provide tools for clinicians to initiate the discussion about end-of-life decisions, such as resuscitation planning (see website for further details - health.qld.gov.au/advance-care-planning/). 7.1 National Framework for Advance Care Directives The National Framework for Advance Care Directives seeks to address the issues with concepts and mechanisms that respect the rights of people to have a say about care that will be provided when their capacity to make decisions is impaired or lost, but that also fit with norms of informed consent and clinical practice within the health and aged-care sectors. The national framework document has developed a Code for Ethical Practice for Advance Care Directives.61 The Code for Ethical Practice is intended to provide a set of principles to guide practice in health and aged care settings where Advance Health Directives are used. The following principles underpin the Best Practice Standards as they appear in the current 60 AHMAC National Working Group, A National Framework for Advance Care Directives, Consultation Draft, September 2009, [Under development] 61 Ibid. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 37 of 61 version of the national document. While the term ‗Advance Care Directive‘ is used instead of ‗Advance Health Directive‘, the same principles apply in Queensland. 1. Advance Care Directives are founded on respect for autonomy and are focused on the person. An Advance Care Directive records personal views and is intended to ensure a person‘s preferences and directions are known so they can be respected and honoured after loss of decision-making capacity. 2. Competent adults are autonomous individuals and are entitled to make their own decisions about personal and health matters. A competent adult can complete an Advance Care Directive to guide future decisionmaking and is not required to be informed, or to seek or follow medical advice, for their Advance Care Directive to be valid. 3. Autonomy can be exercised in different ways according to the person’s culture, background or history. Autonomy can be exercised by self-determined decisions, delegating decisions to others, making collaborative decisions within a family context, or a combination of these. 4. Adults are presumed competent. An adult should be presumed competent at the time of completing an Advance Care Directive unless there is good reason to question his or her competence at that time. 5. Directions in Advance Care Directives may reflect a broad concept of health. Directions are not limited to medical treatment decisions. 6. Directions in Advance Care Directives can relate to any future time. Directions can apply to any period of impaired decision-making capacity and are not limited to decisions at the end of life. 7. The person decides what constitutes quality of life for them. The person determines their own preferred outcomes of care and desired levels of personal functional ability, and decides what circumstances are intolerable or unacceptable, and what interventions are overly burdensome or intrusive. 8. The substitute decision-maker carries the same authority as that of the person when competent. The decision of a substitute decision-maker validly appointed under an Advance Care Directive expresses the wishes and directions of the person. Health care professionals advise the substitute decision-maker about appropriate, beneficial and available treatment options. 9. The substitute decision-maker must honour residual decision-making capacity. The substitute decision-maker must consider each decision as the need arises and make a substitute decision only if the person is unable or unwilling to make that particular decision. 10. The primary decision-making standard for substitute decision-makers is substituted judgement. The substitute decision-maker has an obligation to make the decision the person would have made in the current circumstances had decision-making capacity not been impaired. Substitute decision-makers should base their decision on what they know or can surmise about the person‘s life-goals, views, values and beliefs, however, and whenever expressed, taking into account information, including medical advice, that the decision-maker believes the person would have considered relevant. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 38 of 61 11. A substitute decision-maker should only base their decision on best interests when there is no evidence of the person’s preferences on which to base substituted judgement. The best interests of a person are personal in nature and not limited to medical interests or biological factors. If a person is unable to indicate what their best interests are, they are defined by their chosen substitute decision-maker or those close to them. 12. An Advance Care Directive can be relied upon if it appears valid on face value. A health care professional is entitled to assume that a properly witnessed Advance Care Directive was completed by a competent adult without undue influence or coercion and is therefore valid, unless there are reasons to question that assumption. 13. A refusal of a health-related intervention in an Advance Care Directive is binding. A person can indicate in an Advance Care Directive their advance refusal of health care, medical treatment, life-sustaining measures or hospital transfer through written directions or appointing a substitute decision-maker. If intended to apply to the situation, such refusals are binding regardless of whether they may lead to serious deterioration in health, or death, where they differ from the views of a legally recognised substitute decision-maker, family members or treating health and aged-care professionals. 14. A person, or their legally recognised substitute decision-maker, can consent to treatment offered, refuse treatment offered, but cannot demand treatment. A person cannot use an Advance Care Directive to demand particular medical interventions or treatment or to request something illegal, such as euthanasia or assisted suicide. Health care professionals are not required to offer treatment options that they consider neither medically beneficial nor clinically appropriate, nor to accede to demands for such treatment written in an Advance Care Directive but should discuss and explain all treatment options with legally recognised substitute decision-makers. 15. A valid Advance Care Directive that expresses choices or preferences relevant and specific to the situation at hand must be followed. When the terms of an Advance Care Directive do not apply directly in the circumstances, the person‘s expressed values and preferred outcomes of care should guide decisions by health and aged-care professionals and substitute decision-makers. 7.2 The decision-making pathway This decision-making pathway has been designed to guide substitute decision-makers appointed by the person through an Advance Health Directive. It should also assist health and aged-care professionals to make decisions where the person has not appointed a substitute decision-maker and no guardian has been formally appointed by the appropriate authority to make the particular decision. Such decisions should be made in consultation with family members and others assigned substitute decision-making rights by law. The following decision-making pathway is sourced from the pre-release version of the National Framework for Advance Care Directives – Consultation Draft (p. 28). Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 39 of 61 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 40 of 61 Glossary Acute emergencies (Legal provisions) 63A Guardianship and Administration Act 2000 (1) A life-sustaining measure may be withheld or withdrawn for an adult without consent if the adult‘s health provider reasonably considers— (a) the adult has impaired capacity for the health matter concerned; and (b) the commencement or continuation of the measure for the adult would be inconsistent with good medical practice; and (c) consistent with good medical practice, the decision to withhold or withdraw the measure must be taken immediately. (2) However, the measure may not be withheld or withdrawn without consent if the health provider knows the adult objects to the withholding or withdrawal. (3) The health provider must certify in the adult‘s clinical records as to the various things enabling the measure to be withheld or withdrawn because of this section. (4) For this section, artificial nutrition and hydration is not a life-sustaining measure. Advance Care Planning ―Advance care planning is a process enabling a patient to express wishes about his or her future health care in consultation with their health care providers, family members and other important people in their lives. Based on the ethical principle of patient autonomy and the legal doctrine of patient consent, advance care planning helps to ensure that the concept of consent is respected if the patient becomes incapable of participating in treatment decisions.‖62 Advance care planning for end of life can occur at any time, even for those who are young, fit and healthy. Advance care planning supports patients in communicating their wishes about end-of-life care. Advance Health Directive An Advance Health Directive acts as the patient‘s decision-maker should they lose capacity for decision-making about health matters. An Advance Health Directive also formalises an adult‘s wishes about current and future health matters and may nominate one or more people to make decisions on their behalf should they become unable to do so. Queensland‘s Advance Health Directive is given force under both the Powers of Attorney Act 1998 and the Guardianship and Administration Act 2000. The legal effect of a patient‘s Advance Health Directive is as if the patient gave the directions when they had capacity. Artificial hydration and/or nutrition Artificial nutrition and/o hydration refers specifically to techniques for providing nutrition and/or hydration because the patient is unable to swallow. It includes the use of nasogastric tube, percutaneous endoscopic gastrostomy (PEG feeding) and total parenteral nutrition. Consent - order of priority in dealing with life-sustaining measures (legal provisions) 62 Singer PA, Roberston G, Roy DJ. Bioethics for clinicians: 6. Advance care planning, CMAJ 1996;15(12):16891692. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 41 of 61 S6663 Guardianship and Administration Act 2000 (1) If an adult has impaired capacity for a health matter, the matter may only be dealt with under the first of the following subsections to apply. (2) If the adult has made an Advance Health Directive giving a direction about the matter, the matter may only be dealt with under the direction. (3) If subsection (2) does not apply and the tribunal has appointed 1 or more guardians for the matter or made an order about the matter, the matter may only be dealt with by the guardian or guardians or under the order. (4) If subsections (2) and (3) do not apply and the adult has made 1 or more enduring documents appointing 1 or more attorneys for the matter, the matter may only be dealt with by the attorney or attorneys for the matter appointed by the most recent enduring document. (5) If subsections (2) to (4) do not apply, the matter may only be dealt with by the statutory health attorney. (6) This section does not apply to a health matter relating to health care that may be carried out without consent under Division 1. S66A When consent to withholding or withdrawal of life-sustaining measure may operate (1) This section applies if a matter concerning the withholding or withdrawal of a lifesustaining measure is to be dealt with under section 66(3), (4) or (5) [above] (2) A consent to the withholding or withdrawal of a life-sustaining measure for the adult can not operate unless the adult‘s health provider reasonably considers the commencement or continuation of the measure for the adult would be inconsistent with good medical practice. General Principles (Schedule 1 – Guardianship and Administration Act 2000) 1 Presumption of capacity An adult is presumed to have capacity for a matter. 2 Same human rights (1) The right of all adults to the same basic human rights regardless of a particular adult‘s capacity must be recognised and taken into account. (2) The importance of empowering an adult to exercise the adult‘s basic human rights must also be recognised and taken into account. 3 Individual value An adult‘s right to respect for his or her human worth and dignity as an individual must be recognised and taken into account. 4 63 Valued role as member of society s. 66 Guardianship and Administration Act 2000 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 42 of 61 (1) An adult‘s right to be a valued member of society must be recognised and taken into account. (2) Accordingly, the importance of encouraging and supporting an adult to perform social roles valued in society must be taken into account. 5 Participation in community life The importance of encouraging and supporting an adult to live a life in the general community, and to take part in activities enjoyed by the general community, must be taken into account. 6 Encouragement of self-reliance The importance of encouraging and supporting an adult to achieve the adult‘s maximum physical, social, emotional and intellectual potential, and to become as self-reliant as practicable, must be taken into account. 7 Maximum participation, minimal limitations and substituted judgment (1) An adult‘s right to participate, to the greatest extent practicable, in decisions affecting the adult‘s life, including the development of policies, programs and services for people with impaired capacity for a matter, must be recognised and taken into account. (2) Also, the importance of preserving, to the greatest extent practicable, an adult‘s right to make his or her own decisions must be taken into account. (3) So, for example— (a) the adult must be given any necessary support, and access to information, to enable the adult to participate in decisions affecting the adult‘s life; and (b) to the greatest extent practicable, for exercising power for a matter for the adult, the adult‘s views and wishes are to be sought and taken into account; and (c) a person or other entity in performing a function or exercising a power under this Act must do so in the way least restrictive of the adult‘s rights. (4) Also, the principle of substituted judgment must be used so that if, from the adult‘s previous actions, it is reasonably practicable to work out what the adult‘s views and wishes would be, a person or other entity in performing a function or exercising a power under this Act must take into account what the person or other entity considers would be the adult‘s views and wishes. (5) However, a person or other entity in performing a function or exercising a power under this Act must do so in a way consistent with the adult‘s proper care and protection. (6) Views and wishes may be expressed orally, in writing or in another way, including, for example, by conduct. 8 Maintenance of existing supportive relationships The importance of maintaining an adult‘s existing supportive relationships must be taken into account. 9 Maintenance of environment and values (1) The importance of maintaining an adult‘s cultural and linguistic environment, and set of values (including any religious beliefs), must be taken into account. (2) For an adult who is a member of an Aboriginal community or a Torres Strait Islander, this means the importance of maintaining the adult‘s Aboriginal or Torres Strait Islander cultural and linguistic environment, and set of values (including Aboriginal tradition or Island custom), must be taken into account. Editor’s notes— Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 43 of 61 Aboriginal tradition means the body of traditions, observances, customs and beliefs of Aboriginal people generally or of a particular community or group of Aboriginal people, and includes any such traditions, observances, customs and beliefs relating to particular persons, areas, objects or relationships—see the Acts Interpretation Act 1954, section 36. Island custom, known in the Torres Strait as Ailan Kastom, means the body of customs, traditions, observances and beliefs of Torres Strait Islanders generally or of a particular community or group of Torres Strait Islanders, and includes any such customs, traditions, observances and beliefs relating to particular persons, areas, objects or relationships— see the Acts Interpretation Act 1954, section 36. 10 Appropriate to circumstances Power for a matter should be exercised by a guardian or administrator for an adult in a way that is appropriate to the adult‘s characteristics and needs. 11 Confidentiality An adult‘s right to confidentiality of information about the adult must be recognised and taken into account. Good Medical Practice Good medical practice is good medical practice for the medical profession in Australia having regard to (a) the recognised medical standards, practices and procedures of the medical profession in Australia; and (b) the recognised ethical standards of the medical profession in Australia. Health Care Principle (Schedule 1 Guardianship and Administration Act 2000) The health care principle is described in detail in Schedule 1, section 12 of the Guardianship and Administration Act 2000. It outlines the requirements for exercising powers for a health matter. (1) The health care principle means power for a health matter, or special health matter, for an adult should be exercised by a guardian, the adult guardian, the tribunal, or for a matter relating to prescribed special health care, another entity— (a) in the way least restrictive of the adult‘s rights; and (b) only if the exercise of power— (i) is necessary and appropriate to maintain or promote the adult‘s health or wellbeing; or (ii) is, in all the circumstances, in the adult‘s best interests. Example of exercising power in the way least restrictive of the adult‘s rights— If there is a choice between a more or less intrusive way of meeting an identified need, the less intrusive way should be adopted. (2) In deciding whether the exercise of a power is appropriate, the guardian, the adult guardian, tribunal or other entity must, to the greatest extent practicable— (a) seek the adult‘s views and wishes and take them into account; and (b) take the information given by the adult‘s health provider into account. (3) The adult‘s views and wishes may be expressed— (a) orally; or (b) in writing, for example, in an Advance Health Directive; or (c) in another way, including, for example, by conduct. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 44 of 61 (4) The health care principle does not affect any right an adult has to refuse health care. (5) In deciding whether to consent to special health care for an adult, the tribunal or other entity must, to the greatest extent practicable, seek the views of the following person and take them into account— (a) a guardian appointed by the tribunal for the adult; (b) if there is no guardian mentioned in paragraph (a), an attorney for a health matter appointed by the adult; (c) if there is no guardian or attorney mentioned in paragraph (a) or (b), the statutory health attorney for the adult. Health care64 (1) Health care, of an adult, is care or treatment of, or a service or a procedure for, the adult— (a) to diagnose, maintain, or treat the adult‘s physical or mental condition; and (b) carried out by, or under the direction or supervision of, a health provider. (2) Health care, of an adult, includes withholding or withdrawal of a life-sustaining measure for the adult if the commencement or continuation of the measure for the adult would be inconsistent with good medical practice. Health provider Means a person who provides health care, or special health care, in the practice of a profession or the ordinary course of business. Examples are medical officers, dentists, social workers, psychologists, nursing professionals. Life-sustaining measure The legislation defines a life-sustaining measure as health care intended to sustain or prolong life that maintains the operation of vital bodily functions that are temporarily or permanently incapable of independent operation. Life-sustaining measures include, but are not limited to; cardiopulmonary resuscitation, assisted ventilation and artificial nutrition and hydration. Other life-sustaining measures might include; drug therapies, antibiotics and renal and liver failure treatments (eg., haemodialysis, peritoneal dialysis, hemofiltration). Life-sustaining measures do not include unusual or extraordinary forms of treatment taking into account the available facilities and resources available to provide for the patient‘s care. Objections (s. 67 – Guardianship and Administration Act 2000) Effect of adult’s objection to health care (1) Generally, the exercise of power for a health matter or special health matter is ineffective to give consent to health care of an adult if the health provider knows, or ought reasonably to know, the adult objects to the health care. Editor’s note— Object is defined in schedule 4 (Dictionary). Note also the Powers of Attorney Act 1998, section 35(2)(a) (Advance Health Directives) provides that ‗by an Advance Health Directive [a] principal may give a direction— 64 Schedule 2, section 5, Guardianship and Administration Act 2000 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 45 of 61 (a) consenting, in the circumstances specified, to particular future health care of the principal when necessary and despite objection by the principal when the health care is provided‘. (2) However, the exercise of power for a health matter or special health matter is effective to give consent to the health care despite an objection by the adult to the health care if— (a) the adult has minimal or no understanding of 1 of the following— (i) what the health care involves; (ii) why the health care is required; and (b) the health care is likely to cause the adult— (i) no distress; or (ii) temporary distress that is outweighed by the benefit to the adult of the proposed health care. (3) Subsection (2) does not apply to the following health care— (a) removal of tissue for donation; (b) participation in special medical research or object, by an adult, to health care means— (a) the adult indicates the adult does not wish to have the health care; or (b) the adult previously indicated, in similar circumstances, the adult did not then wish to have the health care and since then the adult has not indicated otherwise. Example— An indication may be given in an enduring power of attorney or Advance Health Directive or in another way, including, for example, orally or by conduct. Palliative care65 Palliative care is specialist care for all people living with, and dying from an eventually fatal condition and for whom the primary goal is quality of life. [From World Health Organisation] Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual. Palliative care: provides relief from pain and other distressing symptoms affirms life and regards dying as a normal process intends neither to hasten nor postpone death integrates the psychological and spiritual aspects of patient care offers a support system to help patients live as actively as possible until death offers a support system to help the family cope during the patient‘s illness and in their own bereavement uses a team approach to address the needs of patients and their families, including bereavement counselling, if indicated will enhance quality of life, and may also positively influence the course of illness is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications. 65 Needs to be updated and referenced Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 46 of 61 Post-coma unresponsiveness Post-coma unresponsiveness encompasses clinical states that follow emergence from coma in which there is apparently complete lack of purposeful responsiveness, with preservation of sleep-wake cycles and cardiorespiratory function, and partial or complete preservation of hypothalamic and brain-stem autonomic (vegetative) functions. Post coma unresponsiveness is a manifestation of severe brain damage. It can be considered part of a continuous spectrum of impaired responsiveness that includes other forms of altered consciousness such as coma, death determined by loss of brain function, ‗locked-in‘ syndrome, minimally responsive state (or minimally conscious state) and dementia (Bernat 2000). These states are sometimes very difficult to diagnose. The term post-coma unresponsiveness is often used interchangeably with the more established term vegetative state however Queensland Health recommends the term postcoma unresponsiveness becomes more accepted both in diagnostics and care. Terminal condition A progressive condition that has no cure and that can be reasonably expected to cause the death of a person in the foreseeable future. The definition is inclusive of both malignant and non-malignant illness and ageing. A person has an eventually fatal condition if their death in the foreseeable future would not be a surprise. Palliative Care Australia recommends ―living with an eventually fatal (or terminal) condition.‖ Urgent health care (s. 63 Guardianship and Administration Act 2000) (1) Health care, other than special health care, of an adult may be carried out without consent if the adult‘s health provider reasonably considers— (a) the adult has impaired capacity for the health matter concerned; and (b) either— (i) the health care should be carried out urgently to meet imminent risk to the adult‘s life or health; or (ii) the health care should be carried out urgently to prevent significant pain or distress to the adult and it is not reasonably practicable to get consent from a person who may give it under this Act or the Powers of Attorney Act 1998. (2) However, the health care mentioned in subsection (1)(b)(i) may not be carried out without consent if the health provider knows the adult objects to the health care in an Advance Health Directive. (3) However, the health care mentioned in subsection (1)(b)(ii) may not be carried out without consent if the health provider knows the adult objects to the health care unless— (a) the adult has minimal or no understanding of 1 or both of the following— (i) what the health care involves; (ii) why the health care is required; and Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 47 of 61 (b) the health care is likely to cause the adult— (i) no distress; or (ii) temporary distress that is outweighed by the benefit to the adult of the health care. (4) The health provider must certify in the adult‘s clinical records as to the various things enabling the health care to be carried out because of this section. (5) In this section— health care, of an adult, does not include withholding or withdrawal of a lifesustaining measure for the adult. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 48 of 61 Bibliography ―Artificial Nutrition and Hydration in End-of-Life Care‖ - An HPNA Position Paper. Home Healthcare Nurse.22(5). May 2004. ABS statistics, 1301.0 - Year Book Australia, 2001; ―A Century of Population Change in Australia.‖ Adults can also consent to blood transfusions under s. 17 of the Transplantation and Anatomy Act 1987 AHMAC National Working Group, A National Framework for Advance Care Directives, Consultation Draft, September 2009, [Under development] Akabayashi A, Fetters MD, Elwyn TS. Family consent, communication, and advance directives for cancer disclosure: a Japanese case and discussion. J Med Ethics 1999; 25: 296-301. Andrew Taylor & Margaret Box. 1999. Multicultural Palliative Care Guidelines http://pallcare.org.au/Portals/46/Multicultural%20palliative%20care%20guidelines.pdf Ashby,MA., Mendelson,D., ‗Gardner; re BWV: Victorian Supreme Court makes landmark Australian ruling on tube feeding‘, Medical Journal of Australia, 2004; 181 (8): 442-445 Association, the Resuscitation Council (UK) and the Royal College of Nursing. October 2007 http://www.bma.org.uk/images/DecisionsRelatingResusReport_tcm41-147300.pdf Austin Health, Report on the Evaluation of the National Implementation of the Respecting Patient Choices Program, 2006. Australian Medical Council, Good Medical Practice: A Code of Conduct for Medical Officers in Australia, July 2009, p. 13-14d Administration Act 2000, sch. 2, s. 5A Australian and New Zealand Intensive Care Society, Statement on Withholding and Withdrawing Treatment, ANZICS, 2003. Australian Medical Association, AMA position statement: The Role of the Medical Practitioner in End-of-life Care, 2007. Australian Medical Association. Care of severely and terminally ill patients — 1997 [position statement]. Sydney: AMA, 1997. http://www.ama.com.au/web.nsf/doc/SHED-5FK3DB Australian Medical Council, Good Medical Practice: A Code of Conduct for Medical officers in Australia, July 2009 Ayers-Hawkins,N., Ditto,PH., Danks,DH., Smucker,WD., ‗Micromanaging death: Process preferences, values and goals in end-of-life medical decision-making‘, The Gerontologist, Vol 5, No 1, 2005 Back AL, Arnold RM. Dealing with conflict in caring for the seriously ill: ―it was just out of the question‖. JAMA 2005; 293: 1374-1381. Baile W, Lenzi R, Parker A, et al. Oncologists‘ attitudes toward and practices in giving bad news: an exploratory study. J Clin Oncol 2002; 20: 2189-2196. Baile WF, Beale EA. Giving bad news to cancer patients: matching process and content. J Clin Oncol 2001; 19: 2575-2577. Barnett MM. Effect of breaking bad news on patients‘ perceptions of doctors. J R Soc Med 2002; 95: 343-347. Batlle, J.C. (2003), p. 2280 Beauchamp T, Childress J. Principles of Biomedical Ethics. 5th ed. New York: Oxford University Press; 2001. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 49 of 61 Beauchamp,T.L., Childress,J.F., Principles of Biomedical Ethics, 5thedn, Oxford University Press, New York, 2001. Bedell S, Pelle D, Maher P, Cleary P. Do-not-resuscitate orders for critically-ill patients in the hospital: how are they used and what is their impact? JAMA 1986; 256: 233-237. Biegler P, Stewart C, Savulescu J, Skene L. Determining the validity of advance directives. Med J Aust 2000; 172: 545-548. Billings JA. Comfort measures for the terminally ill. Is dehydration painful? J Am Geriatr Soc. 1985;33:808-810. Bradley EH, Hallemeier AG, Fried TR, et al. Documentation of discussions about prognosis with terminally ill patients. Am J Med 2001; 111: 218-223. British Medical Association (2007). British Medical Association, Decisions relating to cardiopulmonary resuscitation A joint statement from the British Medical British Medical Association. Decisions relating to cardiopulmonary resuscitation. A joint statement from the British Medical Association, the Resuscitation Council (UK), and the Royal College of Nursing. London: BMA, 2002. http://www.bma.org.uk/ap.nsf/Content/cardioresus Brown RF, Butow PN, Henman M, et al. Responding to the active and passive patient: flexibility is the key. Health Expect 2002; 5: 236-245. Brown,M., ‗Participating in end-of-life decisions: the role of general practitioners‘, Australian Family Physician, Vol.31, No.1, 2002. Brown,M., ‗Who would you choose?‘ Australian Journal on Ageing, Vol.16, No.4, 1997. Brown,M., Beilby,J., Gargett,E., Participating in end-of-life decisions: the role of GPs, Hawke Instirute Working Paper Series No.7, University of South Australia, 2000. Brown,M., Grbich,C., et.al., ‗Documenting end-of-life decisions in residential aged-care facilities in South Australia‘, Australian and New Zealand Journal of Public Health, Vol.29, No.1, 2005. Bruera E. The Choi and Billings article reviewed. Oncology (Huntingt). 2002;19:522-523. Buchanan,A., Brock,D., Deciding for Others: the ethics of surrogate decision-making, Cambridge University Press, Cambridge, 1998. Burt,R.A., ‗The End of Autonomy‘, Hastings Center Special Report: Improving end-of-life care, Nov- December.2005. Callahan CM, Haag KM, Buchanan NN, Nisi R. Decision-making for percutaneous endoscopic gastrostomy among older adults in a community setting. J Am Geriatr Soc. 1999;47:11051109. Candib,L.M., Quill,T.E., Stein,H.F., ‗Truth Telling and Advance Planning at the End of Life: Problems with Autonomy in a Multicultural World‘, Families, Systems and Health, Vol.20, No.3, 2002. Cardiopulmonary Resuscitation – Guidelines for Clinical Practice and Training in Primary Care. Resuscitation Council (UK,) 2002. Cartwright,C., ‗End-of-life decision-making: practical and ethical issues for health professionals‘, Cartwright,C.M., Parker,M.H., ‗Advance care planning and end-of-life decision-making‘, AustralianFamily Physician, Vol.33, No.10, 2004. Chan A, Woodruff RK. Communicating with patients with advanced cancer. J Palliat Care 1997; 13: 29-33. Chiumello, D. et al. (2002). ‗Different modes of assisted ventilation in patients with acute respiratory failure‘. In European Respiratory Journal. Vol. 20. pp. 925-933. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 50 of 61 Chochinov HM, Hack T, Hassard T, et al. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet 2002; 360: 2026-2030. Chochinov HM, Tataryn DJ, Wilson KG, et al. Prognostic awareness and the terminally ill. Psychosomatics 2000; 41: 500-504. Choi YS, Billings JA. Changing perspectives on palliative care. Oncology (Huntingt). 2002;16:515-522. Christakis N. Death foretold: prophecy and prognosis in medical care. Chicago: University of Chicago Press, 1999. Clark,D. ‗Between Hope and Acceptance: the Medicalisation of Dying‘. British Medical Journal, Vol.324, 2002. Clayton J, Butow P, Arnold R, Tattersall M. Discussing life expectancy with terminally ill cancer patients and their carers: a qualitative study. Support Care Cancer 2005; 13: 733-742. Clayton JM, Butow PN, Arnold RM, Tattersall MHN. Discussing end-of-life issues with terminally ill cancer patients and their carers: a qualitative study. Support Care Cancer 2005; 13: 589-599. Clayton JM, Butow PN, Arnold RM, Tattersall MHN. Fostering coping and nurturing hope when discussing the future with terminally ill cancer patients and their caregivers. Cancer 2005; 103: 1965-1975. Clayton JM, Butow PN, Tattersall MHN. The needs of terminally ill cancer patients versus those of caregivers for information regarding prognosis and end-of-life issues. Cancer 2005; 103: 1957-1964. Clayton JM, Butow PN, Tattersall MHN. When and how to initiate discussion about prognosis and end-of-life issues. J Pain Symptom Manage 2005; 30: 132-144. Cogen R, Weinryb J, Pomerantz C, Fenstemacher P. Complications of jejunostomy tube feeding in nursing facility patients. Am J Gastroenterol. 1991;86:1610-1613. Consent to Medical Treatment and Palliative Care Act 1995 (SA). Coppola,K.M., Ditto,P.H., Danks,J.H., Smucker,W.D., ‗Accuracy of primary care and hospitalbased predictions of elderly outpatients‘ treatment preferences with and without advance directives‘, Archives Internal Medicine, Vol.161, Iss.3, 2001. Covinsky,K.E. et.al., ‗Communication and decision-making in seriously ill patients: findings of the SUPPORT project‘, Journal of the American Geriatrics Society, Vol.48, Iss.5, 2000. Cox A, Holbrook D, Rutter M. Psychiatric interviewing techniques VI. Experimental study: eliciting feelings. Br J Psychiatry 1981; 139: 144-152. Curtis JR, Engelberg RA, Nielsen EL, et al. Patient–physician communication about end-of-life care for patients with severe COPD. Eur Respir J 2004; 24: 200-205. Curtis JR, Wenrich MD, Carline JD, et al. Understanding physicians‘ skills at providing end-oflife care perspectives of patients, families, and health care workers. J Gen Intern Med 2001; 16: 41-49. Dahlin C, Goldsmith T. Dysphagia, dry mouth, and hiccups. In: Ferrell B, Coyle N, eds. Textbook of Palliative Nursing. New York: Oxford University Press; 2001:122-138. Daly BJ. Special challenges of withholding artificial nutrition and hydration. J Gerontol Nurs. 2000;26:25-31. Deakin CD, Nolan JP. European Resuscitation Council guidelines for resuscitation 2005. Section 3. Electrical therapies: automated external defibrillators, defibrillation, cardioversion and pacing. Resuscitation 2005;67(Suppl 1):S25–37. Decisions relating to Cardiopulmonary Resuscitation. A joint statement from the British Medical Association, Resuscitation Council (UK) and Royal College of Nursing, 2007. 21 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 51 of 61 Decisions relating to Cardiopulmonary Resuscitation: A joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. J Med Ethics 2001;27:310–316 (www.resus.org.uk). Delvecchio Good MJ, Good BJ, Schaffer C, et al. American oncology and the discourse on hope. Cult Med Psychiatry 1990; 14: 59-79. Demoratz MJ. Advance directives: getting patients to complete them before they need them. Case Manager 2005; 16: 61-63. Dexter PR, Wolinsky FD, Gramelspacher GP, et al. Effectiveness of computer-generated reminders for increasing discussions about advance directives and completion of advance directive forms. A randomized, controlled trial. Ann Intern Med 1998; 128: 102-110. Dresser,R., ‗Confronting the ―near irrelevance‖ of advance directives‘, Journal of Clinical Ethics, Vol.5, No.1, 1994. Dresser,R., Substituting Authenticity for Autonomy, The Hastings Center Report; Mar/Apr 2009. Dugan DO, Gluck EH. Discussing life-sustaining treatments: an overview and communications guide for primary care physicians. Compr Ther 2004; 30: 25-36. Dunn, H. (2001). Hard choices for loving people: CPR, artifi cial feeding, comfort care and the patient with a Dunphy K. Futilitarianism: knowing how much is enough in end-of-life health care. Palliat Med 2000; 14: 313-322. Dyer,C., ‗Bill clarifies gap in law over living wills‘, British Medical Journal, Vol.328, p.1516, 2004 Eliott JA, Olver IN. Legitimating do-not-resuscitate orders: a discursive study of cancer patients‘ speech. J Palliat Care 2003; 19: 100-106. Ellershaw JE. Dehydration and the dying patient. J Pain Sympt Manage. 1995;10:192-197. Emanuel EJ, Fairclough DL, Wolfe P, Emanuel LL. Talking with terminally ill patients and their caregivers about death, dying, and bereavement: is it stressful? Is it helpful? Arch Intern Med 2004; 164: 1999-2004. Emanuel LL, von Gunten CF, Ferris FD, editors. Communicating bad news. In: The Education for Physicians on End-of-life Care (EPEC) curriculum. Chicago: The Robert Wood Johnson Foundation, 1999. Emanuel LL, von Gunten CF, Ferris FD, eds. Medical futility. In: The Education of Physicians on End-of-life Care (EPEC) curriculum. Chicago: The Robert Wood Johnson Foundation, 1999. Emanuel LL, von Gunten CF, Ferris FD. Advance care planning. Arch Fam Med 2000; 9: 1181-1187. Emanuel,E.J., Emanuel,L.L., ‗Proxy decision-making for incompetent patients‘, Journal of American Medical Association, Vol.267, No.5, 1992. Emanuel,L., Emanuel,E., ‗Decisions at the end of life guided by communities of patients‘, Hastings Center Report, Sep-Oct.1993. Emanuel,L.L., ‗Advance directives: what have we learned so far?‘ Journal of Clinical Ethics, Vol.4, No.1, 1993. Emanuel,L.L., Danis,M., et.al., ‗Advance care planning as a process: structuring the discussions in practice‘, Journal of American Geriatrics Society, Vol.43, Iss.4, 1995. Establishing a standard crash call telephone number in hospitals. National Patient Safety Agency Alert, February 2004. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 52 of 61 Etchells E, Katz MR, Shuchman M, Wong G, Workman S, Choudhry NK, Craven J, Singer PA: Accuracy of clinical impressions and Mini-Mental State Exam scores for assessing capacity to consent to major medical treatment. Comparison with criterion-standard psychiatric ssessments. Psychosomatics 1997, 38(3):239-45. Ethical Decision-Making in Palliative Care: Cardiopulmonary Resuscitation (CPR) for People who are Terminally Ill. National Council for Hospice and Specialist Palliative Care Services. Ethics Working Party, 1997 revised Jan 2002. Euthanasia Special Report, www.bbc.co.uk July 1, 1999 Ewer MS, Kish SK, Martin CG, et al. Characteristics of cardiac arrest in cancer patients as a predictor of survival after cardiopulmonary resuscitation. Cancer 2001; 92: 1905-1912. Fagerlin A, Schneider C. Enough: the failure of the living will. Hastings Cent Rep 2004; 34: 3042. Fagerlin,A., Schneider, C., ‗Enough-the Failure of the Living Will‘, Hastings Center Report, Apr-May 2004 Fainsinger RL, Bruera E. When to treat dehydration in a terminally ill patient? Support Care Cancer. 1997;5:205-211. Fallowfield LJ, Jenkins VA, Beveridge HA. Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med 2002; 16: 297-303. Fiatarone M, O‘Neill E, Ryan N, et al. Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med. 1994; 330:1769-1775. Finucane TE, Bynum JP. Use of tube feeding to prevent aspiration pneumonia. Lancet. 1996;348:1421-1424. Finucane TE, Christmas C, Travis K. Tube feeding in patients with advanced dementia: a review of the evidence. JAMA. 1999; 282:1365-1370. Flemming K. The meaning of hope to palliative care cancer patients. Int J Palliat Nurs 1997; 3: 14-18. Freckelton, I. and K Petersen, K, (eds), Disputes and Dilemmas in Health Law (2006) 38, 38– 42. Fried TR, Bradley EH, O‘Leary J. Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc 2003; 51: 1398-1403. Friedrichsen M. Breaking bad news in the transition from curative to palliative cancer care — patient‘s view of the doctor giving the information. Support Care Cancer 2000; 8: 472-478. Friedrichsen MJ, Strang PM, Carlsson ME. Cancer patients‘ interpretations of verbal expressions when given information about ending cancer treatment. Palliat Med 2002; 16: 323-330. Gabbott D et al. Cardiopulmonary resuscitation standards for clinical practice and training in the UK. Resuscitation 2005;64:13–19 (Available for download from www.resus.org.uk). Gattellari M, Butow PN, Tattersall MH, et al. Misunderstanding in cancer patients: why shoot the messenger? Ann Oncol 1999; 10: 39-46. Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med 2001; 52: 1865-1878. Gattellari M, Voigt KJ, Butow PN, Tattersall MH. When the treatment goal is not cure: are cancer patients equipped to make informed decisions? J Clin Oncol 2002; 20: 503-513. Gedge, E., Giacomini, M., & Cook, D. (2007), Withholding and withdrawing life support in critical care settings: ethical issues concerning consent. J. Med. Ethics 33: 215-218 General Medical Council, UK - Withholding and withdrawing - guidance for doctors. http://www.gmc-uk.org/guidance/ethical_guidance/witholding_lifeprolonging_guidance.asp Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 53 of 61 Gillick MR. Rethinking the role of tube feeding in patients with advanced dementia. N Engl J Med.2000;342:206-210. Gillick,M.R., ‗Adapting advance care planning to the nursing home‘, Innovations in end-of-life care, Vol.5, No.2, 2003. Gillick,M.R., ‗Advance Care Planning‘, New England Journal of Medicine, Vol.350, No.1, 2004. Girgis A, Sanson-Fisher RW. Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol 1995; 13: 2449-2456. Glare P. Prognosis in palliative care: ten common questions. Prog Palliat Care 2004; 12: 1015. Gold Standards Framework Website, The Three Triggers, http://www.goldstandardsframework.nhs.uk/TheGSFToolkit/Identify/TheThreeTriggers.htm Golin CE, Wenger NS, Liu H, et al. A prospective study of patient– physician communication about resuscitation. J Am Geriatr Soc 2000; 48 (5 Suppl): S52-S60. Gostin LO. Deciding life and death in the courtroom. From Quinlan to Cruzan, Glucksberg, and Vacco—a brief history and analysis of constitutional protection of the ―right to die.‖ JAMA. 1997;278:1523-1528. Grbich C, Parker D, Maddocks I. Communication and information needs of care-givers of adult family members at diagnosis and during treatment of terminal cancer. Prog Palliat Care 2000; 8: 345-350. Grbich,C., Maddocks,I., et.al., ‗Palliative care in aged-care facilities for residents with noncancer disease‘, Australasian Journal on Ageing, Vol.24, No.2, 2005. Greisinger AJ, Lorimor RJ, Aday LA, et al. Terminally ill cancer patients: their most important concerns. Cancer Pract 1997; 5: 147-154. Hagerty RG, Butow PN, Ellis PM, et al. Communicating with realism and hope: incurable cancer patients‘ views on the disclosure of prognosis. J Clin Oncol 2005; 23: 1278-1288. Haidet P, Hamel MB, Davis RB, et al. Outcomes, preferences for resuscitation, and physicianpatient communication among patients with metastatic colorectal cancer. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Am J Med 1998; 105: 222-229. Hallenbeck J. Fast facts and concepts #10: Tube feed or not tube feed? J Palliat Med. 2002;5:909-910. Hamel R, DuBose ER. Views of the major faith traditions. In: Hamel R, ed. Choosing Death: Active Euthanasia, Religion, and the Public Debate. Deerfield, Ill: Trinity Press International; 1991:45-77. Heaven CM, Maguire P. Disclosure of concerns by hospice patients and their identification by nurses. Palliat Med 1997; 11: 283-290. Henman M, Butow P, Brown R, et al. Lay constructions of decision making in cancer care. Psychooncology 2002; 11: 295-306. Hickman,S.E., Hammes,B.J., et.al., ‗Hope for the Future: Achieving the original intent of advance directives‘, Hastings Center Special Report: Improving End-of-life Care: Why has it been so difficult?, Nov-Dec.2005. Hodgetts TJ et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation 2002;54:115–123. Hooper, S., Vaughan, K., Tennant C., & Perz J. ‗Major depression and refusal of lifesustaining medical treatment in the elderly.‘ MJA 1996; 165: 416-419 Hudson PL, Aranda S, Kristjanson LJ. Meeting the supportive needs of family caregivers in palliative care: challenges for health professionals. J Palliat Med 2004; 7: 19-25. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 54 of 61 Humphrey GB, Littlewood JL, Kamps WA. Physician/patient communication: a model considering the interaction of physicians‘ therapeutic strategy and patients‘ coping style. J Cancer Educ 1992; 7: 147-152. International Guidelines 2000 – A Consensus on Science. Resuscitation 2000; 46:1-448. Jacobs I et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation. Resuscitation 2004; 63:233–249. Johnson,S.H., ‗Making room for dying: End-of-life care in Nursing Homes‘, Hastings Center Special Report: Improving end-of-life care, Nov-Dec.2005. Johnston G, Abraham C. Managing awareness: negotiating and coping with a terminal prognosis. Int J Palliat Nurs 2000; 6: 485-494. Jones, R. & Holden T. 2004. p. 973. Jordens,C., Little,M., Kerridge,I., McPhee,J., ‗From advance directives to advance care planning: current legal status, ethical rationales and a new research agenda‘, Internal Medicine Journal, Vol.35, 2005. Kadakia SC, Sullivan HO, Starnes E. Percutaneous endoscopic gastrostomy or jejunostomy and the incidence of aspiration in 79 patients. Am J Surg. 1992;164:114-118. Kaplowitz SA, Campo S, Chiu WT. Cancer patients‘ desires for communication of prognosis information. Health Commun 2002; 14: 221-241. Karlawish JH, Quill T, Meier DE. A consensus-based approach to providing palliative care to patients who lack decision-making capacity: ACP-ASIM End-of-Life Care Consensus Panel. Ann Intern Med 1999;130: 835-840. Kaw M, Sekas G. Long-term follow- up of consequences of percutaneous endoscopic gastrostomy (PEG) tubes in nursing home patients. Digest Dis Sci. 1994;39:738-743. Kedziera P. Hydration, thirst, and nutrition. In: Ferrell B, Coyle N, eds. Textbook of Palliative Nursing. New York: Oxford University Press; 2001:156-163. Kerridge I, Myser C, Mitchell K, Hamblin J. Guidelines for no-CPR orders. Med J Aust 1994; 161:270-272. Kerridge,I. Lowe,M., McPhee,J., Ethics and Law for the Health Professions, 2ndedn, Federation Press, Sydney, 2005. Kirby,M., ‗Patients‘ rights – why the Australian courts have rejected Bolam‘, Journal of Medical Ethics, Vol.21, 1995. Kirk P, Kirk I, Kristjanson LJ. What do patients receiving palliative care for cancer and their families want to be told? A Canadian and Australian qualitative study. BMJ 2004; 328: 1343347. Kutner JS, Steiner JF, Corbett KK, et al. Information needs in terminal illness. Soc Sci Med 1999; 48: 1341-1352. Lamont EB, Christakis NA. Complexities in prognostication in advanced cancer: ―to help them live their lives the way they want to‖. JAMA 2003; 290: 98-104. Langmore SE, Terpenning MS, Schork A, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13:69-81. Levine,C., ‗The President‘s Council on Autonomy: Never mind!‘, Hastings Center Report, MayLey P. Towards better doctor–patient communications. In: Bennett AE, editor. Communications between doctors and patients. Oxford: Oxford University Press, 1976: 77-96. Liddell K et al. The European Clinical Trials Directive revisited: the VISEAR recommendations. Resuscitation 2006;69:9–14. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 55 of 61 life-threatening illness. Herndon, VA: A & A Publishers. Lo B, Steinbrook R. Resuscitating advance directives. Arch Intern Med 2004; 164: 1501-1506. Lofmark R, Nilstun T. Not if, but how: one way to talk with patients about forgoing life support. Postgrad Med J 2000; 76: 26-28. Luce JM. Physicians do not have a responsibility to provide futile or unreasonable care if a patient or family insists. Crit Care Med 1995; 23: 760-766. Lynn,J. Arkes, H.R. et.al., ‗Rethinking fundamental assumptions: SUPPORT‘s implications for future reform‘, Journal of the American Geriatrics Society, Vol.48, Iss.5, 2000. Mackillop WJ, Stewart WE, Ginsburg AD, Stewart SS. Cancer patients‘ perceptions of their disease and its treatment. Br J Cancer 1988; 58: 355-358. Manisty C, Waxman J. Doctors should not discuss resuscitation with terminally ill patients: FOR. BMJ 2003; 327: 614-615. Marshall,P.A., ‗The SUPPORT study Who‘s talking?‘, Hastings Center Report Special Supplement: Dying well in the hospital, Nov-Dec.1995. Martin,D.K., Emmanuel,L.L., Singer,P.A., ‗Planning for the end of life‘, The Lancet, Vol.356, pp.1672-76, Nov.2000. McCann RM, Hall WJ, Groth- Juncker A. Comfort care for terminally ill patients. The appropriate use of nutrition and hydration. JAMA. 1994;272:1263- 1266. Mitchell SL, Kiely DK, Lipsitz LA. Does artificial enteral nutrition prolong the survival of institutionalized elders with chewing and swallowing problems? J Gerontol A Biolog Sci Med Sci. 1998;53:M207-M213. Mitchell, K., & Owens, R.G. (2004) ―Judgments of laypersons and general practitioners on justifiability and legality of providing assistance to die to a terminally ill patient: a view from New Zealand‖. Patient Education and Counseling 54 (2004) 15–20 Mitchell, K.R., Kerridge, I.H. & Lovat, T.J. (1999). Bioethics and Clinical Ethics for Health Care Professionals. Social Science Press: Sydney. p. 13. Mogg,M., ‗Advance care planning: the right to decide‘, Australian Nursing Journal, Vol.13, No.8, 2006. Molloy W. Let me decide: why we all need a living will. Canada: Penguin Group, 2005. Molloy,D.W., Guyatt,G.H., et.al., ‗Systematic implementation of an advance directive program in nursing homes‘, Journal American Medical Association, Vol.283, No.11, 2000. Molloy,D.W., Let Me Decide, 2ndedn., Vancouver Health Authority, 2004. Morita T, Akechi T, Ikenaga M, et al. Communication about the ending of anticancer treatment and transition to palliative care. Ann Oncol 2004; 15: 1551-1557. Moseley,M.J., Clark,E., Morales,C., ‗Identifying opportunities to ask patients about their treatment wishes‘, Dimensions of Critical Care Nursing, Vol.12, No.6, 1993. Murray,S.A., Sheikh,A., Thomas,K., ‗Advance care planning in primary care‘, British Medical Journal, Vol.333, pp.868-869, 2006. Murray,T.H., Jennings,B., ‗The Quest to Reform End of Life Care: Rethinking Assumptions and Setting New Directions‘, Hastings Center Special Report: Improving End-of-life Care, Nov-Dec.2005. Murray,T.H., Jennings,B., Callahan,D., Kaebnick,G., ‗End of Life Care after a Decade of Reform: What Has Been Accomplished? Where Should We Go from Here?‘, Hastings Centre Report, Dec.2004–Feb.2007. Myrianthefs P., et al. Efficacy of CPR in a general, adult ICU. Resuscitation 57. 2003. 43-48 Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 56 of 61 National Council for Hospice and Specialist Palliative Care Services and the Association for Palliative Medicine. Ethical decision making in palliative care: cardiopulmonary resuscitation for people who are terminally ill. J R Coll Physicians Edinb 2002; 32: 280. Nelson LJ, Rushton CH, Cranford RE, Nelson RM, Glover JJ, Truog RD. Forgoing medically provided nutrition and hydration in pediatric patients. J Law Med Ethics. 1995;23:33-46. NHMRC‘s National Statement on Ethical Conduct in Human Research 2007 Nolan J et al. Advanced Life Support (5th edition). Resuscitation Council (UK), London 2006 (www.resus.org.uk/pages/pub_ALS.htm). Norton SA, Bowers BJ. Working toward consensus: providers‘ strategies to shift patients from curative to palliative treatment choices. Res Nurs Health 2001; 24: 258-269. Norton SA, Talerico KA. Facilitating end-of-life decision-making: strategies for communicating and assessing. J Gerontol Nurs 2000; 26(9): 6-13. NSW Health, Guideline, CPR – Decisions Relating to No Cardiopulmonary Resuscitation Orders, NSW Health. Guidelines for end-of-life care and decision-making. Sydney: NSW Health, 2005. http://www.health.nsw.gov.au/pubs/2005/endlifecare.html NSW Health. Using advance care directives: New South Wales. Sydney: NSW Health, 2004. http://www.health.nsw.gov.au/policies/gl/2005/GL2005_056.html Oliver I, Eliott J, Blake-Mortimer J. Cancer patients‘ perceptions of do not resuscitate orders. Psychooncology 2002; 11: 181-187. Originally published in the Journal of Hospice and Palliative Nursing, 5(2), 113-117. Reprinted with permission. Owens, D. A. (2007). Hydration in the terminally ill: A review of the evidence. Journal of Hospice and Palliative Nursing, 9(3), 122-123. Palliative Care Australia. A guide to palliative care service development: a population approach. Canberra: Palliative Care Australia, 2005. http://www.pallcare.org.au/Default.aspx?tabid=1221 Parker S, Clayton JM, Hancock K, et al. Communication of prognosis and issues surrounding end of life (EOL) in adults in the advanced stages of a life-limiting illness: a systematic review. Sydney: University of Sydney, NHMRC Clinical Trials Centre, 2006. http://www.ctc.usyd.edu.au/research/publications/articles_2006.htm Parker,M., Cartwright,C., ‗Mental Capacity in Medical Practice and Advance Care Planning: Clinical, Ethical and Legal Issues‘, in Mental Capacity – Australian Legal Monographs, Federation Press, NSW, 2005. Parker,M., Stewart,C., Willmott,L., Cartwright.C., ‗Two steps forward, one step back: advance care planning, Australian regulatory frameworks and the Australian Medical Association‘, Internal Medicine Journal, Vol.37, 2007. Patel R, Sinuf T, Cook D. Influencing advance directive completion rates in non-terminally ill patients: a systematic review. J Crit Care 2004; 19: 1-9. Peatfield R, Sillett R, Taylor D, McNicol M. Survival after cardiac arrest in hospital. Lancet 1977; 1: 1223-1225. Pentz RD, Lenzi R, Holmes F, et al. Discussion of the do-not-resuscitate order: a pilot study of perceptions of patients with refractory cancer. Support Care Cancer 2002; 10: 573-578. Pitorak EF. Learning to have difficult conversations leads to increased hospice referrals. Home Healthc Nurse 2003; 21: 629-632. Powers of Attorney Act 1998 (Qld) Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 57 of 61 Prendergast T. Advance care planning: Pitfalls, progress, promise. Crit Care Med 2001; 29 (2 Suppl): N34-N39. Queensland Advocacy Inc, Submission on ‘Rethinking Life-Sustaining Measures: Questions for Queensland’ (4 July 2005) 10 http://www.qai.org.au/content/online_library_documents.cfm?ID=27. Queensland Criminal Code 1899 Quill TE. Perspectives on care at the close of life. Initiating end-of-life discussions with seriously ill patients: addressing the ―elephant in the room‖. JAMA 2000; 284: 2502-2507. Quill TE. Utilization of nasogastric feeding tubes in a group of chronically ill, elderly patients in a community hospital. Arch Intern Med. 1989;149:1937-1941. Quiney NF, Gardner J, Brampton W. Resuscitation skills amongst anaesthetists. Resuscitation 1995;29:215–218. Rabeneck L, McCullough LB, Wray NP. Ethically justified, clinically comprehensive guidelines for percutaneous endoscopic gastrostomy tube placement. Lancet. 1997;349:496-498. Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: ―they don‘t know what they don‘t know‖. JAMA 2004; 291: 483-491. Rapp, R. P., Young, B., Twyman, D., Bivins, B. A., Haack, D., Tibbs, P. A., et al. (1983). The favorable effect of early parenteral feeding on survival in head-injured patients. Journal of Neurosurgery, 58, 906-912. Research on Procedures in Cardiopulmonary Resuscitation that Lie Outside Current Guidelines. Chamberlain D, Handley AJ. Resuscitation 2004; 60:13-15. Resuscitation from Cardiopulmonary Arrest: Training and Organisation. A Report of the Royal College of Physicians,1987. Resuscitation policy. Health Services Circular (HSC) 2000/028. London, Department of Health, 2000. Robinson, E.M. et al, (2006). Complexities in Decision Making for Persons with Disabilities Nearing End of Life. Topics in Stroke Rehabilitation. 13(4): 54-67. Roter DL, Larson S, Fischer GS, et al. Experts practice what they preach: a descriptive study of best and normative practices in end-of-life discussions. Arch Intern Med 2000; 160: 34773485. Rousseau P. The art of oncology: when the tumor is not the target. Death denial. J Clin Oncol 2000; 18: 3998-3999. Ryan, CJ. ‗Depression, decisions and the desire to die‘. MJA 1996; 165: 411 Sandroni C Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 2007;33(2):237–245. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 2007; 33: 237-245 Sapir R, Catane R, Kaufman B, et al. Cancer patient expectations of and communication with oncologists and oncology nurses: the experience of an integrated oncology and palliative care service. Support Care Cancer 2000; 8: 458-463. Scheider, C. (2005). Palliative care and hospice. In J. Kogut & S.L. Luthringer (Eds.), Nutritional issues in cancer care (pp. 319–329). Pittsburgh, PA: Oncology Nursing Society. Schofield P, Carey M, Love A, et al. ‗Would you like to talk about your future treatment options?‘ Discussing the transition from curative cancer treatment to palliative care. Palliat Med 2006; 20: 397-406. Schofield PE, Beeney LJ, Thompson JF, et al. Hearing the bad news of a cancer diagnosis: the Australian melanoma patient‘s perspective. Ann Oncol 2001; 12: 365-371. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 58 of 61 Schostak RZ. Jewish ethical guidelines for resuscitation and artificial nutrition and hydration of the dying elderly. J Med Ethics. 1994;20:93-100. Should Relatives Witness Resuscitation? A Report from a Project Team of the Resuscitation Council (UK) 1996. Silberfeld M, Checkland D: Faulty judgment, expert opinion, and decision-making capacity. Theor Med Bioeth 1999, 20(4):377-93. Singer, P.A. (1996). Rethinking Life & Death: The Collapse of Our Traditional Ethics. Text Publishing: Melb. Aust. Singer,P.A., Martin,D.K., Lavery,J.V., Thiel,E.C., Kelner,M., Mendelssohn,D.C., ‗Reconceptualising advance care planning from the patient‘s perspective‘, Archives Internal Medicine, Vol.158, Iss.8, 1998. Skene,L., Law and Medical Practice – Rights, Duties, Claims and Defences, Butterworths, Australia, 1998. Solomon,MZ., ‗Why are advance directives a non-issue outside of the USA?‗, Innovations in End-of-life Care, Vol.1, No.1, 1999. Sommerville, M. (2003)."Death talk": debating euthanasia and physician-assisted suicide in Australia. MJA 2003 178 (4): 171-174. Steinberg, M. et al, (1996) End of Life Decision-making: Perspectives of General Practitioners and Patients, Department of Social and Preventive Medicine, The University of Queensland. Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000; 284: 2476-2482. Steinhauser KE, Clipp EC, McNeilly M, et al. In search of a good death: observations of patients, families, and providers. Ann Intern Med 2000; 132: 825-832. Stewart C. Medical futility. In: Albrecht G, editor. Encyclopedia of disability. Thousand Oaks, Calif: SAGE Publications, 2005. Stewart, . (2005). ‗The Australian experience of advance directives and possible future directions‘ 24:Australasian Journal on Ageing S25, S28. Stewart,C., ‗Advance directives: Disputes and Dilemmas‘, in Freckleton,I., Petersen,K. (eds.), Disputes and Dilemmas in Health Law, Federation Press, Sydney, 2006. Stewart,C., ‗The Australian experience of advance directives and possible future directions‘; Australasian Journal on Ageing, Vol.24, Supplement S25-S29, Jun.2005. Stewart,C., Biegler,P., ‗A primer on the law of competence to refuse medical treatment‘, Australian Law Journal, Vol.78, No.5, 2004. Stewart,C., The Australian Medico-Legal Handbook, Churchill Livingstone Australia, 2007 Sullivan-Marx EM, Strumpf NE, Evans LK, Baumgarten M, Maislin G. Predictors of continued physical restraint use in nursing home residents following restraint reduction efforts. J Am Geriatr Soc. 1999;47:342-348. Tattersall MH, Gattellari M, Voigt K, Butow PN. When the treatment goal is not cure: are patients informed adequately? Support Care Cancer 2002; 10: 314-321. Taylor,D.M., Cameron,P.A., ‗Advance care planning in Australia: overdue for improvement‘, Internal Medicine Journal, Vol.32, pp.475-480, 2002. Teno J, Licks S, Lynn J, et al. Do advance directives provide instructions that direct care? SUPPORT investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc 1997; 45: 508-512. Teno J, Lynn J, Wenger N, et al. Advance directives for seriously ill hospitalized patients: effectiveness with the patient self-determination act and the SUPPORT intervention. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 59 of 61 SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc 1997; 45: 500-507. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA 2004; 291: 88-93. Teno JM, Stevens M, Spernak S, Lynn J. Role of written advance directives in decision making: insights from qualitative and quantitative data. J Gen Intern Med 1998; 13: 439-446. Teno,J.M., ‗Advance directives: time to move on‘, Annals of Internal Medicine, Vol.141, No.2, 2004. Teno,J.M., Hill,T.P., O‘Connor, M.A., ‗Advance Care Planning – priorities for ethical and empirical research‘, Hastings Center Report Special Supplement, Nov-Dec.1994. Teno,J.M., Lynn,J. ‗Putting advance care planning into action‘, Journal of Clinical Ethics , Vol.7, No.3, 1996. Teno,J.M., Lynn,J. et.al., ‗Do Formal Advance Directives Affect Resuscitation Decisions and the use of Resources for Seriously Ill Patients?‘ Journal of American Geriatrics Society, Vol.55, No.2, 2007. The Multi-Society Task Force on Persistent Vegetative State. (1994). Medical aspects of persistent vegetative state. New England Journal of Medicine, 330(22), 1572-1579. Thompson,T., Barbour,R., Schwartz, L., ‗Adherence to advance directives in critical care decisionmaking: vignette study‘, British Medical Journal, Vol.327, Nov.2003. Thurber,C.F., ‗Public awareness of the nature of CPR: a case for values-centred advancedirectives‘, Journal of Clinical Ethics, Vol.7, Iss.1, 1996. Tilse,C., Setterlund,D., Wilson,J., Herd,B., ‗Legal Practitioners and Older Clients: Challenges and Opportunities for Effective Practice‘, Elder Law Review, Vol.1, 2002. Tulsky JA, Chesney MA, Lo B. See one, do one, teach one? House staff experience discussing do-not-resuscitate orders. Arch Intern Med 1996; 1285-1289. Tulsky JA. Beyond advance directives: importance of communication skills at the end of life. JAMA 2005; 294: 359-365. VandeKieft GK. Breaking bad news. Am Fam Physician 2001; 64: 1975- 1978. Viola, R. A. (1997). The effects of fluid status and fluid therapy on the dying: A systematic review. Journal of Palliative Care, 13(4), 41-52. Waisel, D. & Truog, R. (1995). ‗The cardiopulmonary resuscitation – not indicated order: futility revisited‘. Ann Intern Med 122 (4): 304-8. Watson, M. et al. ‗Should hospices be exempt from following national CPR guidelines?‘ BMJ 2009;338:b986 Website: Caresearch: The palliative care knowledge network, http://www.caresearch.com.au/ caresearch/ http://www.caresearch.com.au/Caresearch/Portals/0/Documents/WhatisPalliativeCare/Nationa lProgram/IndigenousPCproject/PracticePrinciples.pdf (p.17) Weeks JC, Cook EF, O‘Day SJ, et al. Relationship between cancer patients‘ predictions of prognosis and their treatment preferences. JAMA 1998; 279: 1709-1714. Wenrich MD, Curtis JR, Shannon SE, et al. Communicating with dying patients within the spectrum of medical care from terminal diagnosis to death. Arch Intern Med 2001; 161: 868874. Werth, J.L. (2005). Concerns about Decisions Related to Withholding/Withdrawing LifeSustaining Treatment and Futility for Persons With Disabilities. Journal of Disability Policy Studies. Summer 2005; 16, 1: pp 31-37. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 60 of 61 White B, & Willmott L (2005) Rethinking Life-Sustaining Measures: Questions for Queensland - An Issues Paper reviewing the legislation governing withholding and withdrawing lifesustaining measures: QUT Printing Services Willmott, L. (2007). Advance directives to withhold life-sustaining medical treatment: eroding autonomy through statutory reform. Flinders Journal of Law Reform, 10(2). pp. 287-314. Willmott,L. White,B., Howard,M. ‗Refusing Advance Refusals: Advance directives and lifesustaining medical treatment‘, Melbourne University Law Review, Vol.30, 2006. Yun YH, Lee CG, Kim SY, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol 2004; 22: 307-314. Implementation Guideline – Withholding and Withdrawing Life-Sustaining Measures Part 2 – Ethical and Special Considerations Page 61 of 61