Journal of Pediatric Nursing (2013) 28, e2–e9
The Texas Children’s Hospital Pediatric Advanced Warning
Score as a Predictor of Clinical Deterioration in Hospitalized
Infants and Children: A Modification of the PEWS Tool
Donnett Bell MS, RN, CNS, PNP-BC ⁎, Anh Mac MSN, RN, CPN, Yvette Ochoa BSN, RN,
Mary Gordon PhD, RN, CNS-BC, Mary Ann Gregurich PhD, MPH,
Tangula Taylor MBA, BSN, RN, NE-BC
Texas Children’s Hospital, Houston, TX
Key words:
Pediatric warning score;
Screening tool;
Pediatric clinical
deterioration;
Early warning score;
Risk assessment;
Pediatric safety
Purpose: The purpose of this study was to examine the psychometric properties of the Texas Children's
Hospital Pediatric Advanced Warning Score (PAWS) instrument as an indicator of clinical deterioration
in infants and children.
Design and methods: A retrospective chart review of 150 infants and children was performed.
Results: The overall Cronbach's alpha score was 0.75. The estimate of interrater reliability was 0.740.
Implications: The Texas Children's Hospital Pediatric Advanced Warning Score instrument was found
to be reliable and valid.
© 2013 Elsevier Inc. All rights reserved.
PEDIATRIC PATIENTS ARE admitted to acute care
settings today with higher acuities and comorbidities than in
years past. In order to safely manage more complex patients,
acute care nurses have added many new clinical skills into
their daily practices. Higher acuity children are sometimes atrisk for deterioration. Therefore, a robust system for early
recognition and timely treatment of deterioration is recommended (Haines, Perrott, & Weir, 2006). Thus, nurses
routinely assess for clinical deterioration in acute care and
successfully manage deterioration by getting help to the
bedside for emergency interventions and/or transfer the child
to a higher level of care. The goal is to identify deterioration
early to prevent a cardiac arrest from occurring in acute care.
The tool studied in acute care is the Texas Children’s
Hospital (TCH) Pediatric Advanced Warning Score
(PAWS). It is a modification of the Pediatric Early Warning
Score (PEWS) tool to assess deterioration in the pediatric
⁎ Corresponding author: Donnett Bell, MS, RN, CNS, PNP-BC.
E-mail address: dxbell@texaschildrenshospital.org
0882-5963/$ – see front matter © 2013 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.pedn.2013.04.005
patient population. This study examines the psychometric
properties of the TCH PAWS tool as an indicator of clinical
deterioration in infants and children during hospitalization.
This paper does not compare the psychometrics of the TCH
PAWS tool to the psychometrics of the PEWS tool.
Approximately 3% of children admitted to hospitals
require immediate medical assistance for the treatment of
actual or impending cardiopulmonary arrest (McCabe,
Ducan, & Heward, 2009 & Parshuram, Middaugh, &
Hutchinson, 2009). Previous studies have highlighted
clinical antecedents associated with in-hospital cardiopulmonary arrests such as clinical deterioration involving either
respiratory or mental function, systolic blood pressure
changes, hypoxia, or azotemia (Kause, Prytherch, Parr,
Flabouris, & Hillman, 2004 & Lee, Bishop, Hillman, &
Daffurn, 1995). Significant attention should be given to the
fact, that children deteriorate quickly and depending on their
age and cognitive ability some will not be able to
communicate what they are feeling, which adds a layer of
complexity to the clinical assessment (Haines et al., 2006).
Pediatric Advanced Warning Score (PAWS)
Studies by Tucker, Brewer, Baker, Demeritt, and
Vossmeyer (2009) and Monaghan (2005) describe how
early warning scoring systems allow for prompt identification of deterioration, thus facilitating earlier intervention.
The systems have rapid scoring capability because of the
objectivity and ease-of-use (approximately 15–20 seconds)
and have helped to increase confidence in nurses to
recognize children at-risk for deterioration. Additionally,
use of early warning tools promotes timely and efficient
communication between nurses and physicians (Andrews &
Waterman, 2005).
Operationally, early warning scoring systems include a
trigger (algorithm) for graded responses so that lower scores
support minimal frequency of monitoring. As scores
increase, the frequency of monitoring increases, which may
trigger activation of the Rapid Response Team (RRT) and/or
movement of the patient to higher intensity care areas
(Goldhill, McNarry, Mandersloot, & McGinley, 2005).
Rapid Response Teams have helped to decrease codes in
acute care (Akre et al., 2010).
Child Health Corporation of America Collaborative
In 2007, our hospital joined a one-year collaborative with
the Child Health Corporation of America (CHCA), which
included 19 other hospitals throughout the country. The
challenge of the collaborative was to eliminate codes in
acute care by identifying deterioration earlier and to
intervene appropriately.
Use of the Pediatric Early Warning Score (PEWS) was one
of many changes that the collaborative suggested. The PEWS
tool has 3 assessment parameters: behavior, cardiovascular,
and respiratory. Each parameter has 4 categories of scoring
(0–3 points). An additional 2 points may be added for patients
receiving every 15 minutes of nebulizer treatment or
persistent vomiting following surgery. The highest possible
cumulative score is 13. Higher scores indicate poorer
patient conditions.
The PEWS tool was found to be a reliable and valid
scoring system to identify risk for clinical deterioration.
Tucker et al. (2009) found the PEWS tool identified
children who needed a higher level of care (area under the
curve = 0.89, 95% CI = 0.84–0.94, p b .001). Also, interrater reliability was assessed with two RNs independently
scoring patients (intraclass coefficient = 0.92, p = .001).
At the time of the collaborative, our hospital was not
using an early warning-scoring tool. Thus the collaborative
team decided to investigate the PEWS tool for possible
implementation in our hospital.
The Texas Children’s Hospital Pediatric Advanced
Warning Score Tool
A multidisciplinary team of physicians, nurses, and
respiratory therapists reviewed the PEWS tool (Tucker
et al., 2009), and decided to revise it before implementation
e3
because the original study was done on a 24 bed general
medical unit. Our patient population included patients with
cardiac and surgical diagnoses, as well as patients with
medical diagnoses. The primary modifications made to the
PEWS tool were the words used to describe deterioration in
some of the categories. The team wanted to evaluate the
revised tool and its ability to capture deterioration in patients
with cardiac, surgical and medical diagnoses. Permission to
modify the PEWS tool was received from Tucker et al., 2009.
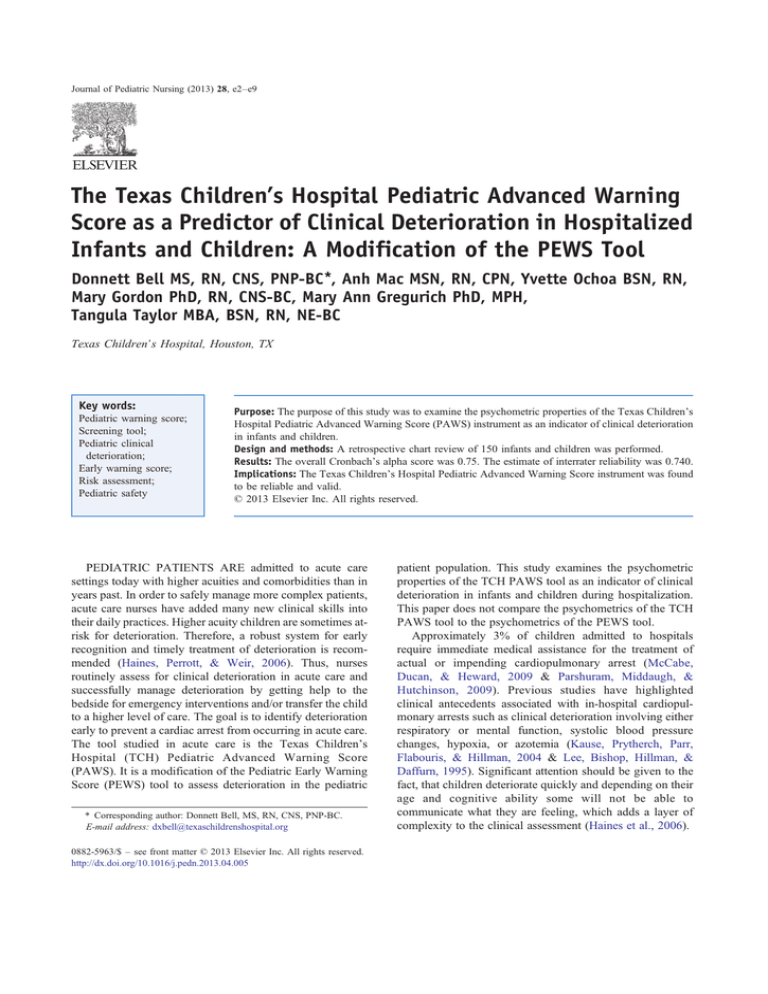
The TCH PAWS tool has 3 assessment parameters:
behavior, cardiovascular, and respiratory (Figure 1). Each
assessment parameter can be scored between 0–3 points
depending on the category of the findings. An additional
2 points may be added to the total score if respiratory
treatments are needed every hour (versus every 15 minutes
with PEWS) or if there is persistent vomiting following
surgery. The rationale for this change was to comply with the
routines for acute care policy, which specifies patients who
require nebulizer treatments every hour for more than 4 hours
require a higher level of care. The highest possible cumulative
score is 13. Higher scores indicate poorer patient conditions.
A modification was made to the respiratory parameter.
Pulse oximetry was added as the monitor for breathing
instead of the liters of oxygen per minute. No change was
made to the respiratory rate criteria. Pulse oximetry is an
accurate and reliable indicator of the level of oxygen
circulating in the blood. It is widely available and used
routinely in acute care, especially in the acute and chronic
cardiac patient populations. Pulse oximetry is most helpful
when used to trend oxygen saturation over time and also, it is
a standard of practice for monitoring the respiratory system
in our hospital. Therefore, the team changed the respiratory
parameter to include changes in oxygen saturations within
baseline limits, 5 points below baseline, or more than 5
points below baseline.
Changes were made to the scoring criteria descriptors in
the behavior parameter (Figure 1). The team removed
category 1 term “sleeping” as a descriptor of behavior,
because they felt the term did not sufficiently capture early
symptoms of deterioration in mental status. Therefore, it was
replaced with “irritable (consolable).” Category 2 was
changed to “irritable (inconsolable).” The consensus among
the team members was that irritable (consolable) behavior
usually precedes irritable (inconsolable) behavior and are
better descriptors of the observed behavior seen during
deterioration. Category 3 descriptors remained “lethargic/
confused.” The “reduced response to pain” descriptor in
category 3 was removed because it was considered a late sign
of progression toward clinical deterioration. Changes in the
Glasgow coma scale (GCS) were initially included as
descriptors in the behavior category as an additional marker
of neurological deterioration. The team felt GCS was a
standard shift assessment parameter and would be easy to
capture on the TCH PAWS tool. However, the GCS was not a
significant predictor in the behavior category and therefore, it
was removed from the final version of the PAWS tool.
e4
D. Bell et al.
Behavior
0
1
2
3
Playing/Appropriate
Irritable (consolable)
Irritable (inconsolable)
Lethargic/confused
Pink or baseline color
and
Cap. refill 1-2 seconds
Pale
or
Cap. refill 3 seconds
Pale & Cap. refill 4
seconds
or
Tachycardia of 20 above
baseline
or
Diaphoresis
Grey
or
Mottled
or
Cap. refill 5 seconds
or
Tachycardia 30 above baseline
or
Bradycardia
20 above baseline
or
O2 sats 5 pts below
baseline
or
Moderate use of accessory
muscles
Slowing of RR below baseline &
increased work of breathing
or
O2 sats > 5 points below baseline
or
Grunting
or
Severe Retractions
Green = 0-2 Score
Cardiovascular
Respiratory
RR and O2 sats within
baseline limits
and
No signs of increased work
of breathing
10 above
baseline
or
Mild using
accessory muscles
RR
RR
Score 2 extra points for patients who are on every hour respiratory treatments or with persistent vomiting
following surgery.
Review VS at time of scoring & repeat if isolated score of 3 in any category OR total score of 4
obtained.
Review O2 requirement & trend at time of scoring.
Yello w = 3 Score
Orange = 4 Score
Red =5 or
Score
Figure 1 Texas Children’s Hospital (TCH) Pediatric Advanced Warning Score (PAWS). (Adapted with permission from: Tucker et al.
(2009). Prospective Evaluation of a Pediatric Inpatient Early Warning Scoring System. Journal for Specialists in Pediatric Nursing).
Diaphoresis was added to the cardiovascular parameter in
category 2 as an early warning symptom for deterioration
(heart failure). This addition to the cardiovascular parameter
was made to accommodate deterioration in our large
population of cardiac patients. The TCH PAWS tool
considers the patients’ physiological parameters and baseline
vital signs, and recommends trending at the time of scoring.
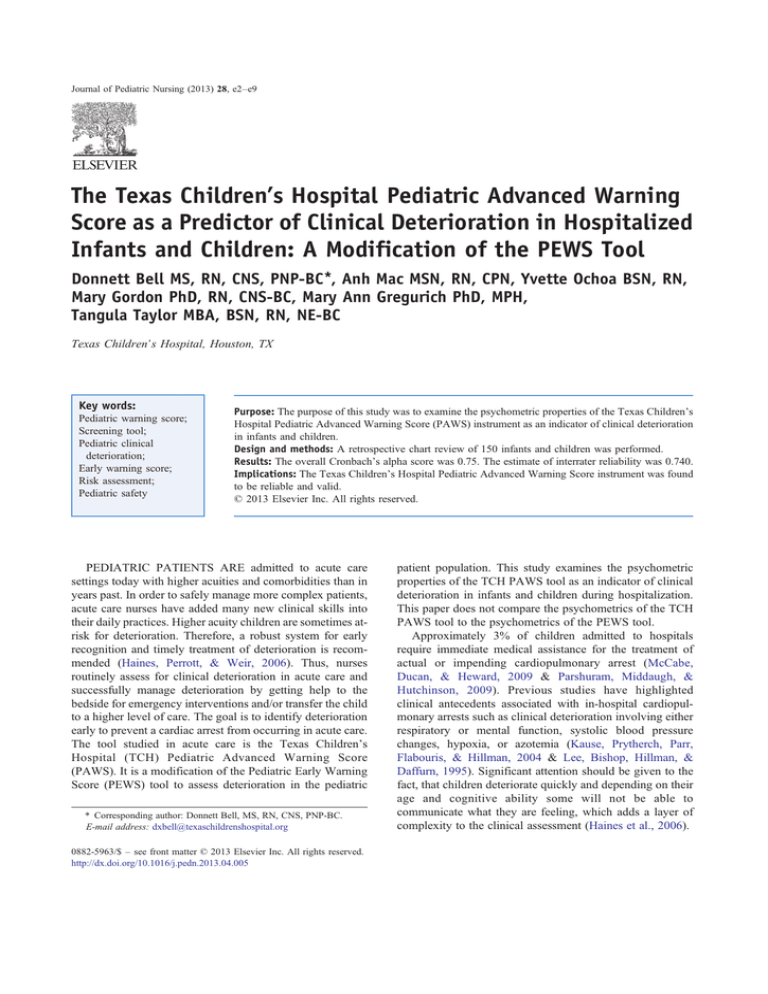
The healthcare team utilizes the algorithm (Figure 2) to
provide care by recommending more frequent assessments,
medical interventions, or initiating a call to the RRT or code
team. If a score of 3 (in any one category) or a total score of 4
or higher is reached, the algorithm suggests considering a
RRT call. The algorithm was modified to capture escalation
of concern from the intern to the senior resident at a score of
5 or higher. In addition, a code can be activated at a score of 6
or higher. The team felt waiting for a score of 7 or higher
would only delay getting help to the bedside. The word,
‘consider’, was used throughout the algorithm as the team
felt the healthcare provider should use the tool in
combination with good clinical judgment.
Prior to collecting data, PAWS education was provided to
all acute care unit nurses and physicians. The education
consisted of a one hour presentation of content and interactive
discussion of various patient scenarios. Also stressed was the
concept that a RRT or code could be initiated at any time
based on the healthcare teams' assessment, regardless of TCH
PAWS score. Individuals were trained to use the data
collection instruments, at which point they assumed respon-
sibility for training other data collectors. A statistician
incorporated all data into the database.
The hospital-wide roll out of RRT was March 2008. The
pilot study of the TCH PAWS tool was started in July 2008.
The house-wide rollout of the TCH PAWS tool was done in
August 2009.
Research Design and Methods
The purpose of this study was to examine the psychometric properties of the TCH PAWS tool as an indicator of
clinical deterioration in infants and children during hospitalization. The Baylor Institutional Review Board (IRB)
approved this study. It was anticipated that the TCH PAWS
tool could be useful as a reliable and valid indicator of early
warning signs of clinical changes that warrant a rapid clinical
response. The key psychometric properties to be examined
are reliability and validity. Reliability establishes the
consistency or repeatability of measurements made with
the instrument and validity establishes if the instrument
measures what it claims to measure. Additional aims for this
study included quantifying: (a) the rate of calls made to the
RRT, (b) the rate of communication among health care
professionals, (c) the correlation between increased TCH
PAWS with increased respiratory and heart rates, and (d) the
correlation between increased TCH PAWS with decreased
GCS scores. Interrater reliability was also established.
Pediatric Advanced Warning Score (PAWS)
e5
Figure 2 Texas Children’s Hospital (TCH) Pediatric Advanced Warning Score (PAWS) Algorithm. Impending cardiac or respiratory arrest
is an automatic code red call *9999. If there are criteria for RRT call *9999. (Adapted with permission from: Tucker et al. (2009). Prospective
Evaluation of a Pediatric Inpatient Early Warning Scoring System. Journal for Specialists in Pediatric Nursing.)
e6
D. Bell et al.
Design
The study was a non-experimental retrospective research
design.
Sample Size and Setting
The study was conducted with patients admitted to one of
three acute care units:
• General medicine/transplant unit
• Pulmonary, adolescent, and endocrine unit
• Cardiology unit
These units manage a variety of patients with the
following medical disorders such as; heart disease, cystic
fibrosis, bronchiolitis, asthma, diabetes, seizure disorders,
liver, kidney, adolescents with eating disorders, Crohns,
pancreatitis, sickle cell, and cancer patients not receiving
chemotherapy. These units also manage a variety of surgical
disorders such as; heart, liver, kidney and lung pre and post
transplant, and general surgical procedures (appendectomy,
incision and drainage, and tonsillectomies). It was determined that 286 infants and children were admitted to the
acute care settings at the hospital during the month of July
2008 and with the inclusion of cardiology patients this would
be a total of approximately 500 patients. The TCH PAWS
scores are obtained as part of routine quality care. For a
population size of 500 infants and children with similar
characteristics, a sample size of 150 patients was needed to
make estimates with a sampling error of no more than ± 5
percent, at the 95 percent confidence level. Sample size was
determined using determinations for simple random and
systematic sampling methods for health studies (Lemeshow,
Hosmer, Klar, & Lwanga, 1993).
Sampling Procedure
A retrospective chart review was performed for infants
and children admitted to one of the three acute care units
during the period of January 1, 2009 to June 1, 2009. The
institution admitted approximately 21,168 patients during
the study year. The sample size reflects 0.7 % of the patient
population. Fifty infants' and children's charts were
randomly selected from each unit for a total of 150 charts.
Patients were included in the study if their length of stay was
greater than 48 hours. A PAWS data collection tool was
designed to record data for this particular chart review.
Results
Researchers reviewed the charts of 150 infants and
children admitted in three acute care setting units from
January 1, 2009 to June 1, 2009. The mean age of the infants
and children in the review was 6.3 years (range: 0.2–
17.0 years), with almost 25% of subjects under one year of
age and 50.7% of subjects female. Table 1 presents more
detailed patient demographic information.
Reliability analysis was used to examine the psychometric
properties of the TCH PAWS tool. The analysis calculated the
reliability of the measurement scales and the relationships
between individual items in the scale. The inter-item
correlation matrix showed positive correlations among
individual items at the final measurement of the 48-hour time
period (Table 2). The weakest correlations were with the
behavioral measure category (0.414 with cardiovascular, 0.320
with respiratory). This weak correlation was also observed
clinically. For example, when there is rapid deterioration in the
respiratory and cardiovascular systems, the behavioral changes
seem slower to become evident. Internal consistency of the
TCH PAWS scores was measured using the Cronbach’s alpha
coefficient, which is a single summary statistic measuring
‘reliability’ of all items to predict the acute changes in clinical
status of infants and children during hospitalization. The
overall Cronbach’s alpha reliability coefficient for the TCH
PAWS score at the final measurement was 0.75, indicating
adequate reliability of the instrument.
In hospitalized infants and children in the acute care
setting, an increasing TCH PAWS score of ≥ 5 resulted in
calls to the rapid team response 80% of the time. There were a
total of five (5) infants and children in the acute care setting
whose first occurrence of a TCH PAWS score was ≥ 5 with
four (4) calls made to the rapid response team. The majority of
these patients were male (75.0%) with a mean age of
8.4 years. The patient with a TCH PAWS score of ≥ 5 that
did not result in a call to the rapid response team was a female
less than one year of age. When the first occurrence of a TCH
PAWS score was 3 or 4 for hospitalized infants and children
in the acute care setting, communication was established with
the patient’s physician or the health care professionals. The
chart review recorded on the TCH PAWS assessment data
collection tool resulted in 8 team communications established
Table 1
Patient Demographics.
Gender
Male
Female
Age
≤ 1 Year
1–3 Years
4–6 Years
7–12 Years
N 12 Years
Diagnosis
Respiratory
Surgery
Medical
Cardiology
N
Percentage
74
76
49.3%
50.7%
37
29
24
30
30
24.7%
19.3%
16.0%
20.0%
20.0%
42
24
63
21
28.0%
16.0%
42.0%
14.0%
Pediatric Advanced Warning Score (PAWS)
e7
Table 2 Inter-Item Correlational Matrix: Final Measure of the
48-Hour Time Period.
Behavior
score
Behavior score
Cardiovascular
score
Respiratory
score
Cardiovascular
score
Respiratory
Score
1.000
.414
.414
1.000
.320
.820
.320
.820
1.000
out of a total of 10 patients having a TCH PAWS score of 3 or
4. Therefore the communication rate among health care
professionals was 80%. Of these patients there was an equal
number of males and females (50.0%) and a mean age of
1.96 years. The mean age of patients with a TCH PAWS
score of 3 or 4 when health care professionals were not called
(20%) was 2.13 years there also were an equal number of
males and females. Of those patients when the rapid response
and communication teams were not called, the diagnoses
were evenly distributed between respiratory disorders,
medical, and cardiology and no other remarkable differences
with regard to their characteristics.
Spearman's rank correlation coefficients were computed
to evaluate the correlation between (a) increasing TCH
PAWS respiratory scores with increasing respiratory rates,
and (b) increasing TCH PAWS cardiovascular scores with
increasing heart rates in hospitalized infants and children at
each recorded measure during the 48-hour time period. All
correlations were positively correlated, ranging from 0.261
to 0.406, and were considered statistically significant.
Results of the correlation analysis are presented in Table 3.
Spearman's rank correlation coefficients were computed
between TCH PAWS cardiovascular scores and heart rates of
hospitalized infants and children at every recorded measure
during the 48-hour time period. All correlations were
positively correlated, with three statistically significant
correlations: the first measure (Time 1), Time 6, and the
last measure of the 48-hour time period (Time 8). Results of
the correlation analysis are presented in Table 4.
To determine if increasing TCH PAWS scores correlated
with decreasing GCS, Spearman’s rank correlation coeffiTable 3 PAWS 48-Hour Assessments, Spearmen’s Rank
Correlation Coefficients, and PAWS Respiratory.
Scores and respiratory rates
Assessment
Spearman’s rho
p value
Time
Time
Time
Time
Time
Time
Time
Time
0.378
0.406
0.261
0.286
0.307
0.280
0.274
0.287
b 0.001
b 0.001
0.002
0.001
b 0.001
0.001
0.001
0.001
1
2
3
4
5
6
7
8
Table 4 PAWS 48-Hour Assessments, Spearmen’s Rank
Correlation Coefficients, and PAWS Cardiovascular Scores
and Heart Rates.
Assessment
Spearman’s rho
p value
Time
Time
Time
Time
Time
Time
Time
Time
0.116
0.009
0.076
0.047
0.106
0.173
0.075
0.231
0.045
NS
NS
NS
NS
0.041
NS
0.006
1
2
3
4
5
6
7
8
cients were computed between total TCH PAWS scores and
GCS of hospitalized infants and children at every recorded
measure during the 48-hour time period. At Time 1, TCH
PAWS and GCS were negatively correlated (rho = − 0.240)
and statistically significant (p = 0.004). The result of the
correlation analysis at Time 2 was negatively correlated
(rho = − 0.066) but not statistically significant. Results of the
remaining correlation analyses (Time 3–Time 8) between the
TCH PAWS and GCS were positive and not significant.
Therefore, GCS was removed from the final TCH PAWS tool.
Interrater reliability of observers' common interpretation
of the TCH PAWS was done prospectively by computing the
intraclass correlation coefficient (ICC). To capture the
consistency of scores among nurses who evaluated the
same patient's level of deterioration, two nurse raters
assessed each patient’s level of deterioration with TCH
PAWS at the same time point. There were 58 nurses,
including float pool nurses that staff acute care units, who
participated in evaluation of the ICC. The TCH PAWS total
score strength of the relationship between both raters
simultaneously was 0.851, with a 95% confidence interval
0.75–0.91. Individual items also yielded an acceptable ICC
at 0.740, with a 95% confidence interval 0.60–0.84
(Table 5). Typically, TCH PAWS is used with a single
observer, therefore the single measure score was used as a
baseline for future interrater reliability studies. The relationship between the nurses’ scores ascertained that nurse raters
dependably gave acceptable ratings.
In 2008 (year before the study began) the rate of the RRT
calls from acute care units was 4.88 per 1000 patient days.
During the calendar year 2009, the rate of RRT calls from
acute care units was 5.85 per 1000 patient days. One outcome
goal of the collaborative was to minimize the number of codes
in acute care. The code events decreased from 0.293 per 1000
patient days in 2008–0.256 per 1000 patient days in 2009.
However, this decreased number of codes is not statistically
significant. Prior to the study, the average length of time
between codes on the pilot units was 18.1 days. The target
goal of the acute care units was to double the number of days
between codes, making the target number 36 days. The acute
units exceeded their goal by achieving 258 days between
codes during the period of 7/12/08 to 3/31/09.
e8
Table 5
D. Bell et al.
Interrater Reliability Assessment with ICC.
Intraclass correlationa
Single measures
Average measures
.740b
.851c
95% Confidence interval
F test with true value 0
Lower bound
Upper bound
Value
df1
df2
Sig
.603
.752
.835
.910
6.697
6.697
61
61
61
61
.000
.000
Two-way random effects model where both people effects and measures effects are random.
The “Average” ICC refers to the interrater reliability of two raters combined. ‘Single’ ICC refers to the reliability of one nurse.
According to McCabe, Ducan, & Heward (2009)
implementation and reinforcement of an early warning
system can take several years to achieve a reduction in
code events and improve clinical outcomes. Therefore, the
priority hospital-wide goal to decrease/eliminate code events
in acute care units continues today.
Implications for Practice
The TCH PAWS tool was found to be a valid and reliable
tool that was incorporated into clinical practice throughout
the acute care units. During the early stages of the project,
TCH PAWS was completed twice per 12-hour shift. After
benchmarking with other pediatric hospitals that utilize early
warning tools the assessment frequency was changed to
every 4 hours. Initially, there was some resistance to the
change in practice; however, it has since become a standard
of care. Hospital policy has been updated to reflect the 4hour intervals of patient scoring. Tools that helped during the
assimilation process included: leadership huddles with staff,
and frequent educational opportunities, that assisted in
demonstrating the value of TCH PAWS as it related to
ensuring safety of hospitalized infants and children.
During the pilot study, TCH PAWS was recorded on a
separate form that led to poor compliance with score
documentation. Since then, TCH PAWS documentation section
has been incorporated into the electronic medical record.
Texas Children’s Hospital Pediatric Advanced
Warning Score as a Communication Tool
Prior to transport to acute care, patients are given a TCH
PAWS score by their transferring departments (emergency
services, pediatric intensive care, progressive care, etc.). The
score is used to communicate patients’ stability. If a patient’s
score suggests that the patient may be of higher acuity and
require an increase in intensity of services, relevant information is given to the charge nurse and the patient’s status is
investigated by the Nursing Administrative Coordinator
(House Supervisor) to ensure correct patient placement. The
TCH PAWS tool is used at initial notification of deterioration
and used subsequently after each intervention to determine if a
patient’s condition has improved. The TCH PAWS tool is also
used when a RRT is initiated and is part of the Situation
Background Assessment Recommendation (SBAR) communication from bedside nurse to RRT nurse. The TCH PAWS
tool is used extensively throughout the organization and is a
vital part of the communication process.
Future Implications
The assessment of patients using TCH PAWS every
4 hours combined with consistently low scores may carry a
risk of fatigue among the nurses. Future studies are needed to
further describe this concept.
The TCH PAWS tool has been incorporated in a new
community-based facility within our healthcare system,
which opened its inpatient beds in 2011. The TCH PAWS
tool is included in criteria for transfer from the community
hospital to the main hospital in the medical center.
How Do I Apply This Information to Nursing Practice?
The TCH PAWS tool was found to be reliable and valid to
detect early clinical deterioration in children admitted to acute
care services, thus allowing for early intervention. The TCH
PAWS score can be used to trigger RRT activation. Rapid
response team intervention has been associated with decreased
code events in acute care areas. The TCH PAWS score is
included in the handoff report when a patient is transferred to
either a higher or lower level of care which facilitates
discussion of the appropriateness of the transfer. This was
noted by receiving nurses to be useful, particularly when a
patient should not be transferred to a unit due to a higher TCH
PAWS score. Implementation of TCH PAWS must be housewide and involve all disciplines to be successful as a
communication tool among health professionals.
Acknowledgments
We would like to thank the staff on 12WT, 14WT, 15WT,
Larry Jefferson, Moushumi Sur, Jennifer Hudnall, Jennifer
Sanders, Shelly Nalbone, Christine Bartlett, Rhonda Wolfe,
Cherida Bluford, Susan Iniguez, Rebecca Wolfe, Angela
Morgan, Sharon Jacobson, Marilyn Hockenberry, and
Julia Kuzin.
References
Akre, M., Finkelstein, M., Erickson, M., Liu, M., Vanderbilt, L., & Billman, G.
(2010). Sensitivity of the pediatric early warning score to identify patient
deterioration. Pediatrics, 125, 763–769.
Pediatric Advanced Warning Score (PAWS)
Andrews, T., & Waterman, H. (2005). Packaging: a grounded theory of how
to report physiological deterioration effectively. Issues and Innovations
in Nursing Practice, 52, 473–481.
Goldhill, D., McNarry, A., Mandersloot, G., & McGinley, A. (2005).
A physiologically-based early warning score for ward patients: the
association between score and outcome. Anaesthesia, 60,
547–553.
Haines, C., Perrott, M., & Weir, P. (2006). Promoting care for acutely ill
children – Development and evaluation of a Paediatric Warning Tool.
Intensive & Critical Care Nursing, 22, 73–81.
Kause, J. S. G., Prytherch, D., Parr, M., Flabouris, A., & Hillman, K. (2004).
A comparison of antecedents to cardiac arrests, death and emergency
intensive care admissions in Australia and New Zeland and the United
Kingdom. Resuscitation, 62, 275–282.
e9
Lee, A., Bishop, G., Hillman, K., & Daffurn, K. (1995). The medical
emergency team. Anesthesia and Intensive Care, 23, 183–186.
Lemeshow, S., Hosmer, D. W., Klar, J., & Lwanga, S. K. (1993). Adequacy
of sample size in health studies. New York: John Wiley & Sons.
McCabe, A., Ducan, H., & Heward, Y. (2009). Pediatric early warning
systems: where do we go from here? Paediatric Nursing, 21, 14–17.
Monaghan, A. (2005). Detecting and managing deterioration in children.
Paediatric Nursing, 17, 32–35.
Parshuram, C., Middaugh, J., & Hutchinson, K. (2009). Development and
initial validation of the Bedside Paediatric Early Warning System score.
Critical Care, 13, 1–10.
Tucker, K., Brewer, T., Baker, R., Demeritt, B., & Vossmeyer, M. (2009).
Prospective evaluation of a pediatric inpatient early warning scoring
system. Journal for Specialists in Pediatric Nursing, 14, 79–85.