toxicological sciences 132(2), 443–457 2013
doi:10.1093/toxsci/kft016
Advance Access publication January 28, 2013
Identification of Transcription Factors and Coactivators Affected by
Dibutylphthalate Interactions in Fetal Rat Testes
Simon M. Plummer,*,1,2 Dhritiman Dan,* Joanne Quinney,* Nina Hallmark,† Richard D. Phillips,† Michael Millar,‡
Sheila MacPherson,‡ and Clifford R. Elcombe*
*CXR Biosciences Ltd, Dundee DD1 5JJ, UK; †ExxonMobil Biomedical Sciences, Inc., Annandale, New Jersey 08801; and ‡MRC Human Reproductive
Sciences Unit, Edinburgh EH16 4TJ, UK.
1
Received November 27, 2012; accepted January 14, 2013
Previous analysis of in utero dibutylphthalate (DBP)-exposed
fetal rat testes indicated that DBP’s antiandrogenic effects were
mediated, in part, by indirect inhibition of steroidogenic factor 1
(SF1), suggesting that peroxisome proliferator–activated receptor
alpha (PPARα) might be involved through coactivator (CREBbinding protein [CBP]) sequestration. To test this hypothesis, we
have performed chromatin immunoprecipitation (ChIP) microarray analysis to assess the DNA binding of PPARα, SF1, CBP, and
RNA polymerase II in DBP–induced testicular maldevelopment
target genes. Pathway analysis of expression array data in fetal
rat testes examined at gestational day (GD) 15, 17, or 19 indicated that lipid metabolism genes regulated by SF1 and PPARα,
respectively, were overrepresented, and the time dependency of
changes to PPARα-regulated lipid metabolism genes correlated
with DBP-mediated repression of SF1-regulated steroidogenesis genes. ChIP microarrays were used to investigate whether
DBP-mediated repression of SF1-regulated genes was associated
with changes in SF1 binding to genes involved in DBP-induced
testicular maldevelopment. DBP treatment caused reductions in
SF1 binding in CYP11a, StAR, and CYP17a. Follicle-stimulating
hormone receptor (FSHR), regulated by SF1 but unaffected by
DBP-treatment, also contained SF1-binding peaks, but DBP did
not change this compared with control. GD15 and GD19 fetal testes contained PPARα protein–binding peaks in CYP11a, StAR,
and CYP17a regulatory regions. In contrast to its repressive effect
on SF1, DBP treatment caused increases in these peaks compared
with control. PPARα-binding peaks in the FSHR promoter were
not detected in GD15 samples. Hence, the repressive effect of DBP
on SF1-regulated steroidogenic genes correlates with inhibition
of SF1-DNA binding and increased PPARα-DNA binding. The
data indicate that PPARα may act as an indirect transrepressor
of SF1 on steroidogenic genes in fetal rat testes in response to DBP
treatment.
Key Words: transcription; steroidogenesis; dibutylphthalate;
testes; dysgenesis.
In utero exposure of male rats to dibutylphthalate (DBP) has
been shown to induce reproductive tract abnormalities, due,
in part, to decreased testosterone synthesis as a result of gene
expression changes in pathways that regulate the synthesis of
this hormone (Gray et al., 2000; Liu et al., 2005; Parks et al.,
2000). Many of the effects of DBP relevant to inhibition of steroid biosynthesis are thought to occur in the Leydig cells (Liu
et al., 2005; Plummer et al., 2007). There is also evidence that
in utero DBP treatment can perturb Sertoli cell and gonocyte
development (Johnson et al., 2007; Mahood et al., 2005). The
possibility that DBP might affect human reproductive development has focused attention on the necessity to understand
mechanisms of DBP-induced testicular maldevelopment in the
rat and human in the hope that greater understanding of these
mechanisms will lead to better tools for risk assessment of this
chemical.
Our previous transcription profiling studies have suggested
that this mechanism partly involves indirect inhibition of steroidogenic factor 1 (SF1) action, a transcription factor essential for
steroidogenesis gene expression in rat testes (Plummer et al.,
2007). To better understand the molecular processes involved
in DBP-induced testicular maldevelopment at the level of transcription factor and coactivator binding to DNA, chromatin
immunoprecipitation (ChIP on chip) microarray analysis was
performed to identify the effects of DBP on the binding of these
proteins to target gene promoters.
Our expression microarray data suggested that one
explanation for the effects of DBP on genes relevant to DBPinduced testicular maldevelopment is indirect inhibition of
SF1 action through peroxisome proliferator–activated receptor
alpha (PPARα)-mediated coactivator sequestration (Plummer
et al., 2007). PPARα and SF1 share a common coactivator,
CREB-binding protein (CBP), which is present in limiting
concentrations (McCampbell et al., 2000). Binding of CBP to
© The Author 2013. Published by Oxford University Press on behalf of the Society of Toxicology.
All rights reserved. For permissions, please email: journals.permissions@oup.com.
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
To whom correspondence should be addressed. Fax: +44(0)1382 322909. E-mail: simonplummer@micromatrices.com.
2
Present address: MicroMatrices Associates Ltd, Dundee University Incubator, Dundee DD1 5JJ, UK.
444
PLUMMER ET AL.
PPARα could therefore starve SF1 of a cofactor essential for its
transactivation functions.
The study was designed to test a hypothesis derived from our
previous investigation (Plummer et al., 2007) that high doses of
DBP affect transcription factor (SF1 and PPARα) and coactivator (CBP) binding to genes involved in DITMD by ChIP-onchip microarray analysis. We also measured RNA polymerase
II (RNA polII) binding to the coding regions of DBP-induced
testicular maldevelopment target genes in order to assess how
their rate of transcription is affected by DBP treatment. The
main aim of this study was to investigate the idea that PPARα
is involved in the indirect inhibitory effects of DBP on SF1regulated steroidogenic genes in fetal rat testes.
Animals and treatments. Time-mated female Wistar rats (Harlan) aged
10–12 weeks were treated once daily from gestational day (GD) 12 with vehicle (control—corn oil) or DBP at 500 mg/kg (CAS no. 84-74-2, Sigma-Aldrich
Co. Ltd, Dorset) in 1 ml/kg corn oil, by oral gavage, until the day prior to
sample (Plummer et al., 2007). The time (day) of mating was determined by
the presence of a vaginal plug, and this day was designated GD1. The DBP
administered was 99% pure according to the supplier. The housing, handling,
and treatment of the animals were carried out according to U.K. Home Office
guidelines. At the end of the study, either GD15 or GD19, dams were killed 2 h
after the last dose of DBP by exposure to an increasing concentration of CO2.
Litters were removed and fetuses placed in ice-cold PBS prior to microdissection. Fetal testes were carefully retrieved using a dissection microscope (Leica
CLS ×100) and either snap frozen in liquid nitrogen or fixed in Bouin’s as
previously described (Plummer et al., 2007).
Immunohistochemical staining. In order to confirm that the transcription factors of interest were present in the fetal testis tissue at both ages of
interest, immunohistochemistry was conducted for PPARα on GD15 fetal testis tissue samples. GD15 fetal testes from vehicle-exposed litters were fixed
in Bouin’s for 2 h, transferred to 70% ethanol, and stored at 4°C. The fixed
tissue was processed and embedded into paraffin blocks. Sections of 10μM
were dewaxed and rehydrated before being blocked in methanol containing 3%
H2O2, for 30 min at room temperature. After rehydration, sections were washed
in deionized water for 5 min followed by Tris-buffered saline (TBS) for 5 min
before being blocked in 20% normal donkey serum (NDS)/TBS/5% bovine
serum albumin (BSA), 30 min at room temperature. Samples were incubated
overnight at 4°C with PPARα antibody (Abcam; ab24509) diluted to 1:500
in NDS/TBS/BSA. Samples were washed 2 × 5 min in TBS before incubation
with donkey anti-rabbit peroxidase diluted to 1:750 in NDS/TBS/BSA, 30 min
at room temperature. Unbound antibody was washed (2 × 5 min) in TBS prior
to addition of tyramide-fluorescein isothiocyanate (FITC) diluted to 1:50 for
10 min. Sections were washed 2 × 5 min in TBS before being subjected to pressure cooking for 5 min on full heat. Tap water was used to cool the slides at
the end of cooking. Sections were blocked in 20% NDS/TBS/5% BSA for
30 min at room temperature prior to overnight incubation at 4°C with 3βHSD
(sc-30820, Santa Cruz Biotechnology, Inc.) diluted to 1:200 in NDS/TBS/
BSA. Sections were washed 2 × 5 min in TBS before incubation with donkey
anti-goat ALEXA 555 diluted to 1:200 in NDS/TBS/BSA for 60 min at room
temperature. Sections were counterstained with 4′,6-diamidino-2-phenylindole
(DAPI), washed once in PBS before coverslipping using permafluor. Slides
were imaged using a Zeiss LSM 710 confocal microscope.
Expression microarray data analysis. Expression microarray data derived
from a previously published study (Plummer et al., 2007) were reanalyzed
using Rosetta Resolver 6 software to define a list of significantly altered genes
(the “Signature List”). Resolver software calculates a p value based on an
ChIP, purification, and quality control. ChIP was performed as the first
step in a process designed to test whether DNA sequences in the promoter
regions of DITMD “target” genes were differentially bound by the transcription factors (SF1 and PPARα) and coactivators/transcription machinery proteins (CBP and RNA polII) in response to the treatment. These antibodies have
been previously validated for ChIP (Ferraz-de-Souza et al., 2011, Saramaki
et al., 2009; Active Motif instructions for product no. 39097). Briefly, eight
testes from each litter were pooled and used to prepare samples for chromatin
fragmentation for each treatment (control and DBP treated) and each time point
(GD-15 and GD-19) in quadruplicate (four biological replicates). Frozen testis
samples were fixed or crosslinked with formaldehyde solution according to the
Active Motif Chip-IT Express kit (Cat no. 053009) method. Glycine stop fixation solution was used to stop the fixation reactions. The fixed testes were lysed
and their chromatin fragmented using a Bioruptor (Diagenode).
The quality of the chromatin fragmentation procedure was checked using
1% agarose gel electrophoresis. The fragmented DNA size was shown to be
between 100 and 500 bp when assessed against DNA molecular weight markers
in the gel (data not shown).
Four different antibodies were used for ChIP. The antibodies used for
the ChIP reactions were raised against the following proteins: RNA polII
(Active Motif-39097), SF1 (Upstate Millipore 07-618), CBP (Santa Cruz
Biotechnology Ltd no. SC-369), and PPARα (Sigma PO869-100UG).
Eight testes from four different litters from vehicle- and DBP-treated dams
were sampled at GD15 and GD19, corresponding to four biological replicates
per time point or treatment, and analyzed using ChIP microarrays. Fragmented
DNA samples were divided into four 90 µl aliquots of immunoprecipitated (IP)
DNA samples and four 20 µl aliquots of input DNA samples. IP DNA samples
were immunoprecipitated with the antibodies using the Active Motif ChIP-IT
Express kit (Cat no. 053009) according to the kit method. Input samples were
stored at −70°C prior to DNA purification. The IP DNA samples were reverse
crosslinked and treated with proteinase K. The genomic (input) DNA was also
treated with proteinase K, and both IP and input samples were purified using
a DNeasy blood and tissue cleanup kit (Qiagen). The samples were eluted in a
volume of 20 µl, and 5 µl of this sample was amplified using the Sigma WGA4
kit (described subsequently).
Whole-genome amplification of the IP and input DNA. Chromatin IP
and input DNA samples were amplified before labeling and microarray hybridization. A whole-genome amplification kit (WGA4, Sigma) was used to amplify
the IP and input DNA to produce a quantity of DNA suitable for labeling and
hybridization on the microarrays, according to the kit method.
Quality control of the DNA enrichment process using SYBR green
dye. The quality of the DNA enrichment process was checked by performing real-time PCR (QPCR) reactions in the presence of SYBR green dye. PCR
primers designed against “target” gene promoters known to be bound by the
transcription factor or coactivators under the study were used in these reactions (Table 1). Target gene enrichment in the amplified IP DNA samples was
assessed by comparing SYBR green amplification profiles of IP versus input
DNA samples using ABI Sequence Detection System 7000 software.
ChIP microarray design. Agilent custom Rat ChIP-on-chip microarray
slides 8 × 15k (G4499A, AMADID-023386) designed using Agilent eArray
software were used for the study. Briefly, the UCSC Genome browser was used
to retrieve transcription start (TS) sites for DITMD “hypothesis” genes. Excel
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Materials and Methods
error-weighted mean of the data for the different replicates. The Rosetta error
model (Weng et al., 2006) calculates both the propagated (technical) and scattered (biological) error and combines these two errors to make a more reliable
error estimation. The p value allows an estimation of the confidence that a given
feature/gene is not significantly different (the null hypothesis) relative to the
reference. A p value < 0.01 was considered significant. Rosetta Resolver trends
analysis was used to identify genes displaying similar patterns of alteration
across time.
Ingenuity Pathways Analysis (IPA) Network analysis and Functional Pathways
representation analysis were used to examine bias in lists of genes significantly
altered by the treatment toward particular biological functions or pathways.
445
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
Table 1 Primers for QPCR Using SYBR Green Dye for the QC of IP Enrichment Assessment
Antibody
Primers
Primer sequence
RNAPII
RNAPII forward primer
RNAPII reverse primer
CYP17 forward primer
CYP17 reverse primer
PPARUCP2 forward
PPARUCP2 reverse
AGA TGA AAC CGT TGT CCA AAC
AGG TTA CGG CAG TTT GTC TCT
GGC TGG GCT CCA GGA GAA TCT TTC TTC CAC
CGG CAG GCA AGA TAG ACA GCA GTG GAG TAG
cttggcaggaattgcttccctggcc
tccagcttcaggctcctcctcacc
SF1/CBP
PPARα (UCP2)
DNA labeling and ChIP microarray analysis. ChIP microarray analysis
involved two color labeling of DNA (Cy5-labeled IP DNA and Cy3-labeled
input DNA) derived from immunoprecipitations with four different antibodies
of four control (corn oil) and four DBP-treated litters, each at two time points
(4 × 2 × 4 × 2 = 64 arrays).
Amplified IP and input DNA of 1.3 µg (13 µl) were fluorescently labeled
using a Genomic DNA Labeling kit plus (Agilent no. 5188-5309). The amplified IP DNA samples were labeled using Cy5-labeled nucleotides (red channel) and the input (genomic) DNA samples were labeled with Cy3-labeled
nucleotides (green channel). The labeled DNA samples were purified using
“Microcon filters.” Agilent 8 × 15 K Rat custom Chip-on chip arrays (Amadid
no. 023386) were hybridized, washed, and scanned using an “Agilent
Microarray Scanner.” All methods used followed the “Agilent Chip-on-chip
protocol 10th May 2008 part no. G4481-90010.”
ChIP microarray data processing and bioinformatics. Images from the
scanner were processed using Agilent Feature Extraction Software v 9.5 to generate raw data (.txt files). These Cy5/Cy3 ratio data were used for subsequent
statistical analysis. Peaks (DNA-protein binding events) constituting collections of a minimum of two probes with significantly raised Cy5/Cy3 ratios
were screened for and detected using the Whitehead per-array neighborhood
peak detection algorithm by Agilent ChIP analytics software. The algorithm
scores’ peaks by performing a random sampling of the data and determining
the likelihood/probability that a putative peak found in the data could have
been identified by chance. A binding event was considered significant if the
mean p values of the peak probe and its two neighbors pxbar were less than
0.05 (pxbar < 0.05). Pxbar is calculated from the mean of the ChIP analytics
error model–derived p value of the central probe and its two neighbors. Peaks
were reviewed or visualized according to their location in the promoters of
target genes in order to assess to which region(s) of the DBP-induced testicular
maldevelopment promoter(s) the gene regulatory protein was bound. In order
to assess the effects of DBP on DNA-protein binding, we used ChIP analytics software to generate a mean of the data from each of the four replicates
for each of the two treatments (control and DBP). Student’s t-test was used
to assess whether there were significant (p < 0.05) differences between peakprobe Cy5/Cy3 ratios between control and DBP-treated samples. Probes on
the ChIP array that were contained in peaks were also tested for homology
with the SF1 and PPARα “consensus” binding sequences, AAGGTCA and
AGGTCANNAGGTCA, respectively, using the EMBOSS alignment tool from
the European Bioinformatics Lab (EBL) website. The microarray data for this
study are held publically in the NCBI Geo database (http://www.ncbi.nlm.nih.
gov/geo) under accession number GSE39225.
Expression microarray data processing and bioinformatics. A Lowess
curve was fitted to the log-intensity versus log-ratio plot, and 20.0% of the
data were used to calculate the Lowess fit at each point. This curve was used to
adjust the control value for each measurement. If the control channel was lower
than 10, then 10 was used instead.
For GD15 and GD19 microarray data, a one-sample t-test was performed
using multiple test correction: Benjamini and Hochberg (BH) false discovery
rate on genes from a list with fold change values greater than 1.2–1.5 or −1.2
to −1.5, with p < 0.05. The resulting gene list was analyzed using IPA to examine overrepresented functional pathways. NB: for BH multiple test correction,
a p value < 0.1 is considered significant. This analysis was performed using
GeneSpring GX 7.3.1.
RESULTS
Expression Array Analysis
Previously derived expression microarray data (Plummer
et al., 2007) were reanalyzed using Rosetta Resolver and
GeneSpring software and IPA software. Our previous analysis of
the data using Rosetta luminator software (Plummer et al., 2007)
had indicated that steroidogenic genes CYP11a and CYP17a
were not significantly regulated at GD15; however, the Resolver
reanalysis showed that these genes were significantly (p < 0.01)
downregulated (~1.5-fold) at GD15 (Supplementary table 1).
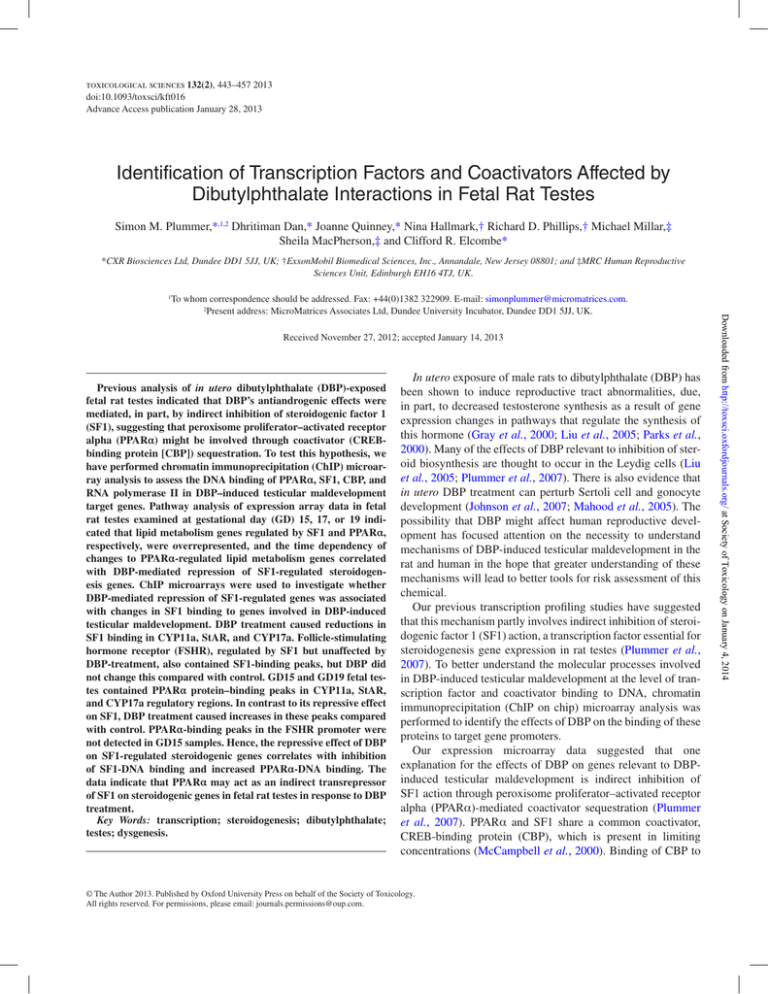
The IPA of GeneSpring multiple test–corrected differentially
expressed gene lists showed that the functional pathway of lipid
metabolism was the top-ranked overrepresented one at GD15
and GD19 (Fig. 1; Supplementary data).
Examination of the genes in the lipid metabolism functional
pathway showed that the majority were induced at GD15 and
repressed at GD19 (Supplementary table 1). Closer review of
the lipid metabolism genes repressed at GD19 highlighted that
many, including genes involved in steroidogenesis, were regulated by SF1. However, at GD15, several of the lipid metabolism genes were involved in mitochondrial β oxidation and
lipid transport pathways and regulated by PPARα.
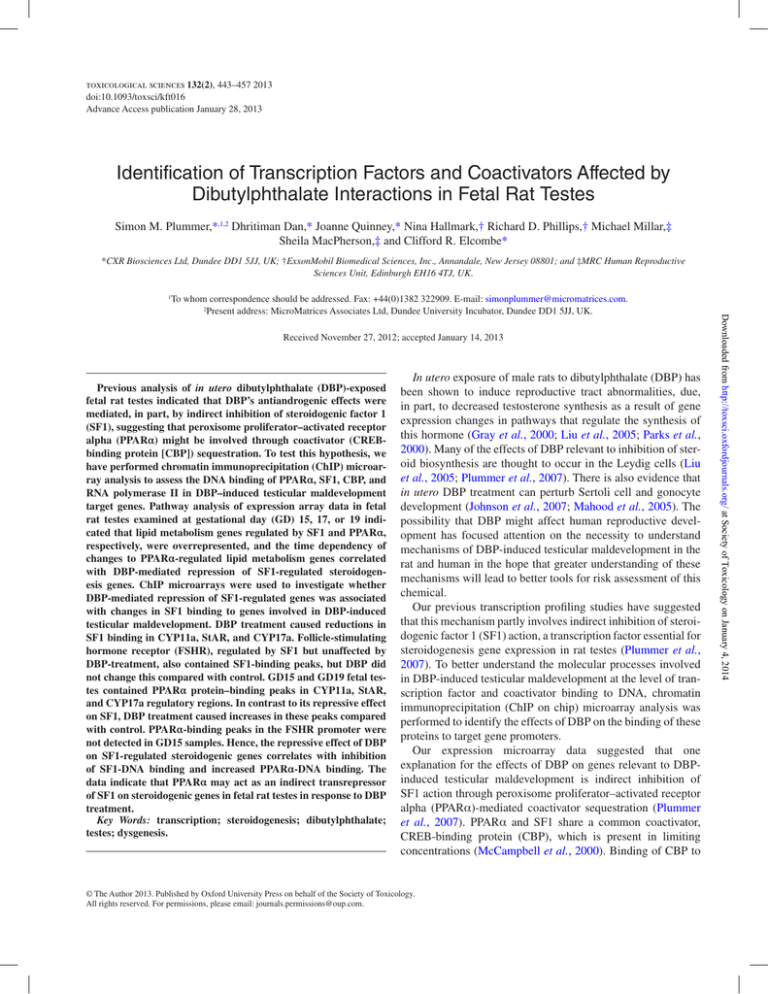
Trends analysis of steroidogenic and lipid metabolism genes
across time showed that the dynamics of changes to genes in
these pathways was strikingly similar indicating the possibility
that they may be coregulated (Fig. 2).
ChIP microarray analysis (GD15 and GD19)
SF1. To investigate a possible relationship between the
antiandrogenic effects of DBP and the binding of SF1 to
steroidogenic gene promoters, binding events (peaks) of SF1
protein to SF1-regulated gene promoters in GD 19 fetal testes were assessed using a custom ChIP microarray designed
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
software was used to generate list of chromosome coordinates 5.5 kb upstream
(promoters) and 2 kb downstream (coding regions) of the TS site. Agilent eArray software was used to perform a probe search within the chromosome coordinates and to generate a probe list from the Agilent database at 100 bp spacing.
The UCSC genome browser was used to confirm binding of probes in the promoter regions of target genes.
446
PLUMMER ET AL.
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 1. IPA representation analysis histogram showing the top 10 functional pathways overrepresented in the signature lists (a) GD15 and (b) GD19.
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
against genes altered by DBP in the lipid metabolism/steroidogenesis pathways (Methods section). Peaks for SF1
binding were found in three genes in the steroidogenic cascade as follows: cytochrome P450, family 11, and subfamily A (CYP11a), pxbar < 0.01, in the promoter and first intron
(Figs. 3a and 3b), respectively; steroidogenic acute regulator
(StAR), pxbar < 0.05 (Fig. 4), cytochrome P450, family 17, and
subfamily A (CYP17a) (Table 2). Probes on the ChIP array that
were contained in the peaks were tested for homology with
the SF1 “consensus” binding sequence (AAGGTCA) (Chou
et al., 1996) using the EMBOSS alignment tool (Table 2). Peak
probes in CYP11a, StAR, and CYP17a contained sequences
that “matched” the SF1 consensus sequence with 70–85%
homology consistent with the idea that they are SF1-binding
sites (Table 2). DBP-treatment caused a significant (p < 0.05)
reduction in peak probe intensity ratios (Cy5/Cy3 ratios) for
SF1 binding compared with control for CYP11a, StAR, and
CYP17a (Figs. 3a, 3b, and 4 and Table 2).
Follicle-stimulating hormone receptor (FSHR) previously
shown to be regulated by SF1 (Heckert, 2001) was found to
contain SF1-binding peaks. However, its expression was unaffected by DBP treatment in our expression microarray data.
Consistent with its lack of effect on FSHR expression, DBP
also did not cause any significant changes to the height of the SF1binding peaks in the promoter of this gene (Fig. 5 and Table 2).
No SF1 peaks were detected in the promoters of the inhibin
alpha (INHA), insulin like 3 (INSL3), scavenger receptor, class
B, member 1 (SCARB1), and hydroxymethylglutaryl coenzyme
a synthetase/reductase (HMGCS/R) genes at GD19 (data not
shown). We checked the effects of DBP treatment on probes that
correspond to a previously published SF1 regulatory binding site
in the INHA, INSL3, SCARB1, and HMGCS genes (Ito et al.,
2000; Lopez et al., 1999; Mascaro et al., 2000; Zimmermann
et al., 1998). Analysis of INHA showed that DBP caused
a reduction in the log-ratio value of a probe in the main SF1
regulatory binding site (−83 bp for TS site), which approached
significance (p < 0.06) (Table 2). Although no peak was detected
(NB: requires two or more probes to be significantly [pxbar <
0.05] above background), this indicates that DBP likely inhibits
SF1 binding at this key site in the INHA gene. We also checked
probe coverage for literature-reported SF1 regulatory binding
sites in the INSL3, SCARB1, and HMGCS promoters. The SF1
regulatory binding sites for these genes were found not to be
covered by our ChIP microarray probes; hence, no conclusion
could be drawn from these data on the potential impact of DBP
exposure on SF1 binding for these genes.
In GD15 fetal testes, there were no SF1 protein–binding
peaks in StAR (data not shown), suggesting that SF1 activation of this gene is not optimal at this time point. This is consistent with a minimal repressive effect of DBP on expression
of this gene at this time point compared with later time points
(Supplementary table 1).
PPARα. We initially tested the PPARα antibody for its
ability to immunoprecipitate PPARα/DNA chromatin complexes in the context of our ChIP-on-chip array using rat hepatocytes exposed to Wyeth 14,643 (Wy) as a positive control. In
this validation experiment, we examined the binding of PPARα
to the promoter region of the canonical PPARα-regulated gene
acyl CoA oxidase 1 (ACOX1). We found that treatment of rat
hepatocytes with a concentration of Wy (10µM), previously
reported to induce fatty acid coenzyme oxidase in rat hepatocytes (Tamasi et al., 2008), induced ACOX1 mRNA expression (13-fold) and caused a significant PPARα-binding peak
in the ACOX1 promoter to a site ~600 bp from the ACOX1 TS
site (Supplementary fig. 1) previously identified by Tugwood
et al. (1992). Hence, the corroboration of a previously identified PPARα-binding site in rat hepatocytes with the PPARα
antibody (Sigma PO869) indicates that this antibody can detect
PPARα protein/DNA binding in the context of our ChIP-onchip array assay and is thus fit to use for this purpose.
Fetal testes contained significant (pxbar < 0.01) PPARα protein–binding peaks in Acsl1 at GD15 (Fig. 6a), CYP11a at GD15
(not shown) and GD19 (Fig. 6b), and StAR at GD15 (Table 2).
Homology matching in the PPARα peak probes showed they
contained sequences ~70% homologous to the PPARα “consensus” binding sequence (AGGTCANNAGGTCA) (IJpenberg
et al., 1997; Table 2). A search for PPARα consensus binding
sites in the Acsl1 gene identified a cluster of PPARα consensus
binding sites in the boundary between the first exon and first
intron, i.e., in the same region where the Acsl1 DBP-induced
PPARα peak was detected (Fig. 7).
In contrast to its effect on SF1, DBP treatment caused significant (p < 0.05) increases in the height (Cy5/Cy3 ratio) of
these peaks compared with control (Table 2). We also detected
PPARα-binding peaks for CYP17a, INHA, SCARB1, and
HMGCS (data not shown). As there was no detection of SF1
regulatory binding peaks for SCARB1 and HMGCS in control
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 2. Resolver trends cluster of genes involved in steroidogenesis and
lipid metabolism regulated by SF1 (green) and PPARα (red), respectively.
Results are log intensity ratios for the genes at GD15, GD17, and GD19.
447
448
PLUMMER ET AL.
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 3. SF1 binding to the (a) CYP11a promoter and (b) first intron in control (green lines) and in utero DBP-exposed (red lines) GD19 fetal rat testes.
The top panel of (a) shows visualization of probe Cy5/Cy3 intensity ratios for each of four replicates of control and DBP-treated samples in the region of the
CYP11a promoter. The bottom panel of (a) shows mean data from the four replicates for each treatment. SF1 protein–binding peaks, detected using the Whitehead
algorithm (Methods section), are highlighted in orange. The x-axis represents the genomic position of probes in the CYP11a promoter or gene body. The y-axis
is the Cy5/Cy3 fluorescence log intensity ratio (binding signal). The green and red lines represent log ratios of probes in the control and DBP-treated samples,
respectively. Probes in the peaks were searched for homology to a consensus binding sequence for SF1. A probe in the promoter peak contained a “consensus”
SF1-binding sequence matched at ~70% homology (red), which supports the contention that SF1 binds to this DNA region.
449
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
Table 2 Intensity Ratio (Cy5/Cy3) Data for Probes Contained in Binding Peaks for SF1 and PPARα in SF1-Transactivated Gene Promoters
Printed on the Agilent ChIP-on-Chip Microarray
Control
ChIP Ab/Gene name
GD-19
SF1
StAR
CYP11a1
CYP17a1
INHA
FSHR
RNA polII
StAR
CYP11a1
GD-15
PPARα
Acsl1
StAR
CYP11a1
CYP17a1
Probe name
Consensus sequence similarity
A_45_P10764037
A_45_P25439518
A_45_P10764063
A_45_P25439542
A_45_P06692896
A_45_P06692897
A_45_P01178980
A_45_P07412993
A_45_P05049360
A_45_P19907416
86%
71%
71%
71%
71%
86%
86%
71%
86%
86%
A_45_P25439528
A_45_P10764052
A_45_P06692928
A_45_P10656093
A_45_P10764056
A_45_P06692901
A_45_P01178983
A_45_P16144883
A_45_P01178990
Location
DBP Treated
t-Test
Cy5/Cy3 ratio mean
SD
Cy5/Cy3 ratio mean
SD
p value
−3317
−3393
−43
−56
−5036
−4436
−1046
−128
−2743
−2768
2.6
2.3
2.6
2.2
1.9
2.5
1.9
1.5
1.6
1.7
0.20
0.60
0.60
0.50
0.70
1.60
0.82
0.13
0.40
0.35
1.0
0.8
0.8
1.1
0.6
0.7
0.7
1.3
1.7
1.8
0.76
0.13
0.22
0.31
0.03
0.02
0.02
0.11
0.55
0.36
0.01
0.01
0.01
0.01
0.02
0.05
0.03
0.07
0.40
0.40
N/A
N/A
N/A
−1642
−1590
(+) 1912
2.1
2.4
1.7
0.56
0.58
0.63
1.0
1.5
1.0
0.27
0.619
0.054
0.01
0.03
0.06
71%
62%
69%
79%
79%
79%
−955
−1186
−3934
−669
−67
−107
0.3
0.7
1.0
0.6
0.8
0.8
0.04
0.32
0.30
0.11
0.26
0.19
1.3
1.6
1.4
1.2
1.6
1.4
0.63
0.52
0.12
0.53
0.46
0.32
0.03
0.02
0.03
0.04
0.02
0.01
Note. The table shows fluorescence intensity signals for probes contained in SF1, PPARα, or RNA polII–protein binding peaks in DITMD “target” genes. The
data for each probe are represented as ratios between the Cy5 and Cy3 mean signals (Cy5/Cy3). The Cy5 and Cy3 signals represent the intensity of hybridization of IP and input DNA for each treatment sample on a probe on the array. Peaks were identified in Agilent DNA analytics software using the Whitehead peak
detection algorithm (Methods section). The sequence of each probe contained in SF1 and PPARα peaks was matched with a “consensus” DNA-binding sequence
of these two transcription factors (Chou et al., 1996; IJpenberg et al., 1997; Neve et al., 2000), respectively, to generate a % homology value. The distance of the
probe upstream from the TS site is shown in column 4 (location). Results are means ± SD of four biological replicate data points per treatment. A Student’s t-test
was used to calculate a p value for each probe. P values < 0.05, representing lower than 5% probability that a difference between the two treatments occurred by
chance, were considered significant.
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 4. Binding of SF1 to the StAR promoter in control (green line) and in utero DBP-exposed (red line) GD19 fetal rat testes. Orange boxes show significant peaks detected using the Whitehead peak detection algorithm. The x-axis represents the genomic position of probes (crosses). The y-axis shows the Cy5/
Cy3 fluorescence log intensity ratio. DBP treatment inhibits binding of SF1 to the StAR promoter. Results are the mean of data for the four replicate treatments.
450
PLUMMER ET AL.
samples, it was not possible to assess whether this transcription
factor was affected by DBP treatment. We did not detect any
differences in PPARα binding in the promoter region of FSHR
(Fig. 8) consistent with a lack of effect of DBP on this SF1regulated gene. Hence, increased binding of PPARα to SF1regulated gene promoters in steroidogenesis genes repressed
by DBP treatment (CYP11a, StAR, CYP17a, and INHA) correlates with inhibition of binding of SF1 in these regions.
CBP. No CBP-binding peaks were detected by probes contained in the SF1-binding peaks for CYP11a, StAR, or CYP17a
in either control or DBP-treated samples. By contrast, peak
detection analysis of the CYP11a and Acsl1 genes showed CBP
peaks in the same location as that for PPARα binding at GD19
and GD15 (not shown), respectively (Fig. 9 and Supplementary
table 2).
RNA polII. RNA polII is an essential part of the eukaryotic transcriptional machinery, and transcriptional rate of genes
is correlated to the number of RNA polII molecules associated with gene coding regions in DNA. Hence, we assessed
RNA polII binding in the coding regions of DITMD “target”
genes in order to assess whether the treatment affected their
transcriptional rate.
We detected increased RNA polII binding downstream of
the TS site in the CYP11a gene in control GD19 fetal testes. This binding was inhibited by DBP treatment (Table 2).
Increased RNA polII binding was also detected in StAR; however, this occurred upstream of the TS site (Table 2). We did
not detect RNA polII binding up- or downstream of the TS
site for CYP17a at GD19. As it seems likely that CYP17a
is actively transcribed by RNA polII at this time because
CYP17a expression is required for fetal testis steroidogenesis,
we conclude that this is not reflected by our analysis of RNA
polII-DNA binding at this time (data not shown). The reason
for the discrepancy is not clear but may reflect heterogeneity
in the kinetics of steroidogenesis gene transactivation in the
testes over this period.
No RNA polII peaks were detected for INHA, SCARB1, and
INSL3. There were RNA polII peaks for HMGCS downstream
of the TS site that had higher mean log-ratio values in control
compared with DBP-treated samples. However, this difference
was not reflected by significant differences in the log ratios of
probes in these peaks (data not shown).
PPARα immunostaining. PPARα was expressed in the
interstitial region of the GD15 testis, with little or no detectable
expression in seminiferous cords (Fig. 10a). We also detected
PPARα expression in the interstitial region at GD19 (data not
shown). The expression of PPARα was dispersed throughout
the interstitial region, but some areas displayed higher levels
of expression than others. There was some colocalization of
PPARα staining and 3βHSD staining (Leydig cell marker;
Fisher et al., 2003) in cells in the interstitial region. A small
number of Leydig cells showed only 3βHSD staining; however, the majority of interstitial cells stained weakly for 3βHSD
(Fig. 10b).
Higher magnification images showed that PPARα protein
in interstitial regions of the testes was partially colocalized as
shown by dual staining for 3βHSD and PPARα (Fig. 10b). As
there were a large number of interstitial cells that showed only
PPARα staining, this indicates that PPARα expression was not
confined to differentiated fetal Leydig cells.
Discussion
Expression microarray pathway analysis and ChIP microarray analysis were employed to investigate the potential effects
of DBP on binding of selected transcription factors to genes
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 5. The binding of SF1 transcription factor on the FSHR promoter in control (green line) and in utero DBP-exposed (red line) GD19 fetal rat testes.
Results represent the mean of four biological replicates per treatment. The orange boxes show significant peaks detected using the Whitehead peak detection
algorithm. The x-axis represents the genomic position of probes (crosses). The y-axis shows the Cy5/Cy3 fluorescence log intensity ratio. The binding of SF1 to
the FSHR promoter was not significantly altered by DBP treatment. Results are the mean of data for the four replicates treatments.
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
451
postulated to be involved in the mechanism(s) of DBP-induced
testicular maldevelopment. This analysis facilitated examination of DNA binding to genes that we had previously found
to be altered in fetal rat testis tissue (Plummer et al., 2007).
Inhibition by DBP of transcription factor SF1-regulated gene
expression correlated with inhibition of SF1-DNA binding to
the promoters of these genes, suggesting that the effects of DBP
could be mediated by SF1 transrepression. These data suggest
that the effects of DBP on steroidogenesis gene expression are
partly mediated by inhibition of SF1 DNA binding in the promoter regions of CYP11a, StAR, CYP17a, and INHA. This
correlates with existing data that showed that DBP inhibited
SF1 binding to DNA regions from the CYP11a, StAR, and
CYP17a promoters (Kuhl et al., 2007). These investigators
postulated that because “inactive” phthalate compounds (e.g.,
diethylphthalate) also caused reductions in SF1 binding to
these genes, this transcription factor could not be solely responsible for the repressive effects of “active” phthalates, e.g., DBP,
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 6. PPARα binding to (a) Acsl1 (first intron) and (b) CYP11a (promoter) in control (green line) and in utero DBP exposed (red line) in GD15 and GD19
fetal rat testes, respectively. The orange boxes show significant peaks detected using the Whitehead peak detection algorithm. The x-axis represents the genomic
position of probes. The y-axis shows the Cy5/Cy3 fluorescence log intensity ratio (binding signal). The green and red lines represent log ratios of probes in the
control and DBP-treated samples, respectively. PPARα binding is increased by DBP treatment relative to control. Results are the mean of data for four replicates
per treatment.
452
PLUMMER ET AL.
Fig. 7. Homology mapping of PPARα “consensus” binding sites in a region of the Acsl1 gene 5.5 kb upstream of the TS site to 2 kb downstream of the
TS site. The red circle shows a cluster of PPARα consensus binding sites in the same region where a DBP-induced PPARα-binding peak was detected (Fig. 6a).
on steroidogenesis genes. However, the present data support
the contention that SF1 is a “target” for DBP-mediated repression of certain steroidogenesis genes. These data have shown
that DBP inhibits SF1 binding in the promoters and introns of
SF1-transactivated genes that are downregulated by DBP at the
mRNA level (CYP11a, StAR, and CYP17a). Previous studies
have shown that nuclear hormone receptor (NHR)-regulated
genes show binding of these transcription factors to intronic
regions (Dong et al., 2009), and intronic regulatory sites appear
to be common for several NHRs.
The binding of SF1 to the SF1-transactivated gene promoter of FSHR, which was unaffected by DBP at the mRNA
level (Plummer et al., 2007), was not inhibited by DBP in
this study. Hence, the effect of DBP on SF1-regulated steroidogenesis genes in fetal testes correlates with inhibition of
SF1 binding to their promoters. This supports the hypothesis
that the effects of DBP on SF1 are indirect as not all SF1
regulated genes are affected by DBP exposure. These data
also support the contention that the repressive effects of DBP
on SF1-regulated steroidogenic genes are mediated, in part,
via inhibition of SF1-DNA binding to steroidogenic promoters. This contention is contradictory to the recent work of
Kuhl et al. (2007) who postulated that c/ebp rather than SF1
is a target for the antiandrogenic effects of DBP (Kuhl et al.,
2007). These investigators also suggested that SF1 does not
play an important role in steroidogenesis in the rat, a suggestion that is incompatible with data indicating that SF1 is
required for the expression of StAR (Sandhoff et al., 1998), a
protein that is rate limiting for steroidogenesis in rats (Manna
and Stocco, 2005).
Data from investigations of SF1 conditional knockout mice
indicate that SF1 is required for fetal testis steroidogenesis
and StAR expression in mice (Jeyasuria et al., 2004). In this
regard, it is interesting that fetal mice are refractory to the
antiandrogenic effects of certain phthalates (Gaido et al.,
2007). Because the effects of DBP appear indirect (Plummer
et al., 2007), it seems possible that mice, unlike rats, lack a
“target” that mediates the antiandrogenic effects of DBP in
fetal testes. It is not known whether fetal mice or humans
express PPARα in testes although adult human testes do
express PPARα (Schultz et al., 1999). In this regard, it is
interesting that diethylhexylphthalate (DEHP) has recently
been shown to inhibit steroidogenesis in adult human testis
explants (Desdoits-Lethimonier et al., 2012).
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 8. Lack of binding peaks of PPARα on the FSHR promoter in control (green line) and in utero DBP-exposed (red line) GD15 fetal rat testes. Results
represent the mean of four biological replicates per treatment. The x-axis represents the genomic position of probes (crosses). The y-axis shows the Cy5/Cy3
fluorescence log intensity ratio. The binding of PPARα to the FSHR promoter was not significantly altered by DBP treatment. Results are the mean of data for
the four replicate treatments.
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
453
The profile of DBP-mediated changes to SF1-regulated steroidogenic genes across time was similar to the profiles of change
taking place in PPARα-regulated lipid metabolism genes. The
inhibitory effects of DBP on the binding of SF1 to the SF1regulated steroidogenesis genes correlated with changes in the
binding of PPARα, a nuclear receptor known to be activated by
DBP (Hurst and Waxman, 2003). There are in vitro data suggesting that PPARα is involved in the antiandrogenic effects
of phthalates on Leydig cells (Gazouli et al., 2002), and it has
been suggested that PPARα could also be involved in the in
vivo effects of these compounds on steroidogenesis in testes
(Corton and Lapinskas, 2005). In this study, SF1-transactivated
steroidogenesis genes inhibited by DBP treatment showed
DBP-mediated increases in PPARα binding. There were also
coincident DBP-mediated increases in CBP binding to some of
the PPARα-DNA-binding sites.
The effects of DBP on PPARα in fetal testes and the effects
of DBP on SF1 gene expression and SF1 binding in DITMD
promoters are related in that increased PPARα binding correlated with inhibition of SF1 binding. DBP-mediated increases
in PPARα binding also correlated with DBP-mediated SF1regulated steroidogenic gene repression. We did not detect the
binding of PPARα in the promoter of FSHR. These results are
consistent with a lack of DBP-treatment-mediated repression
of FSHR at the mRNA level (Plummer et al., 2007) and support
the contention that PPARα binding could be involved in SF1transregulated gene repression in certain DBP-induced testicular maldevelopment “target” genes.
DBP-mediated increases in binding of PPARα to steroidogenic genes occur at binding sites different from those of
SF1, indicating that PPARα may be an indirect repressor of
SF1 binding. This suggests that PPARα is an indirect transrepressor of these SF1-regulated genes. It is possible that PPARα
could act via sequestration of the shared coactivator CBP. CBPbinding peaks were detected in CYP11a and Acsl1 coincident
to PPARα-binding sites consistent with the fact that CBP forms
part of a transcriptional complex with PPARα and is required
for PPARα transactivation (Misra et al., 2002). This indicates
that CBP is associated with PPARα and that sequestration of
this coactivator could partly explain the repressive effects of
DBP on SF1. Another possible explanation for the PPARα
effects could be the involvement of a direct SF1 transrepressor. Possible candidates for this are DAX (Yu et al., 1996) and
COUP-TF2 (Martin and Tremblay, 2010), a direct repressor of
SF1 (Yu et al., 1996). COUP-TF2 also transrepresses PPARα
by directly binding to a PPRE in the malic enzyme and fatty
acyl-CoA dehydrogenase promoters (Baes et al., 1995, Miyata
et al., 1993). The COUP-TF2 promoter contains an HRE
which, in the presence of COUP-TF2, inhibits its own transactivation (Soosaar et al., 1996). As COUP-TF2 transrepresses
PPARα by binding to a PPRE, it is plausible that the converse
would also be true as both transcription factors bind to PPRE/
HRE sites. Hence, it is possible that PPARα could increase the
expression of COUP-TF2 through inhibition of this negative
feedback loop. It has recently been shown that in utero DBP
(500 mg/kg) treatment increases the expression of COUP-TF2
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 9. CBP binding to the CYP11a promoter in control (green line) and in utero DBP-exposed (red line) GD19 fetal rat testes. The orange box shows a
significant peak (pxbar < 0.05) detected using the Whitehead peak detection algorithm. The x-axis represents the genomic position of probes (crosses). The y-axis
shows the Cy5/Cy3 fluorescence log intensity ratio (binding signal). DBP treatment increased the binding of CBP in the CYP11a promoter in a region identical to
that bound by PPARα. Results are the mean of data for the four replicate treatments.
454
PLUMMER ET AL.
in Leydig cells in fetal rat testes at GD18.5 and that this effect
correlates with decreased testosterone levels (Van den Driesche
et al., 2012). Hence, the chronology of effects of DBP on
PPARα-DNA binding to target genes and COUP-TF2 expression is consistent with this hypothesis that may explain the
puzzle of how DBP mediates is indirect inhibitory effects on
SF1-regulated steroidogenesis genes in Leydig cells (Johnson
et al., 2012).
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Fig. 10. (a) GD15 testis cross section showing the morphology of the
seminiferous cords and interstitial region. The blue dye is DAPI staining showing all cell nuclei. Leydig cell marker 3βHSD was labeled with an ALEXA
555 dye that fluoresces red. PPARα-expressing cells have been labeled with
FITC dye that fluoresces green. (b) Combined image of staining in GD15 testis
showing images for the three fluorescent labels overlaid to show colocalization
of antibodies to cells in the interstitial region (blue = DAPI; green = PPARα;
red = 3βHSD).
SF1-binding peaks were not detected in the SCARB1 and
HMGCS promoters. There are data suggesting that SF1 transactivates these genes in testes (Val et al., 2003). Lack of SF1
peak detection in the promoters of these genes in this study
could be due to insufficient density of probes on the ChIP
microarray that contain binding sites for these proteins.
DBP is metabolized in rodents to MBP which is thought to
be the “active” metabolite of DBP with regard to its effects on
testicular development (Corton and Lapinskas, 2005; Williams
and Blanchfield, 1975). Other phthalates such as DEHP and its
active metabolite monoethylhexylphthalate (MEHP) have also
been found to cause testicular maldevelopment in rats (Albro
and Lavenhar, 1989; Gray et al., 2000). However, some phthalates, e.g., diethylphthalate (DEP), are inactive in this regard
(Gray et al., 2000). MBP, MEHP, and monoethylphthalate
(MEP) have been found to gain access to the fetal testes during
a critical “window,” GDs 16–19 (Carruthers and Foster, 2005;
Clewell et al., 2008, 2009). Hence, it has been suggested that the
ability of these compounds to cause testicular maldevelopment
is determined mainly via differences in their potency to inhibit
testosterone production rather than differences in their ability
to gain access to the fetal testes. MBP and MEHP are both agonists for PPARα (Hurst and Waxman, 2003). However, MEP,
unlike MEHP and MBP, does not activate PPARα (Bility et al.,
2004; Corton and Lapinskas, 2005). Hence, the PPARα agonist activity of these phthalate metabolites correlates with their
abilities to induce TMD in rats. It is not known whether nonphthalate PPARα agonist compounds induce testicular maldevelopment in rats. Recently, Hannas et al. (2012) found in utero
treatment with the PPARα agonist Wy did not cause testicular
maldevelopment or inhibit fetal testis testosterone synthesis or
gene expression and suggested that this indicated that PPARα
could not be involved in the antiandrogenic effects of phthalates
(Hannas et al., 2012). However, as Wy undergoes extensive first
pass metabolism in rats (NTP Technical report on the toxicity
studies of Wy; National Toxicology Program, 2007) and also
may not cross the placenta to gain access to the fetal testes, it
is possible that the lack of effects of Wy in this model may be
due to lack of fetal testis bioavailability. The inhibitory effect of
fenofibrate, a potent PPARα agonist, on StAR gene expression
in mouse ovary was reported to be directly mediated via PPARα
in studies involving PPARα knockout mice (Toda et al., 2003).
Hence, there is evidence that nonphthalate PPARα agonist compounds can also repress SF1-transactivated genes in a PPARαdependent manner in vivo. DBP does not cause antiandrogenic
effects in mice (Gaido et al., 2007), so it is not possible to assess
whether there is concurrence in PPARα-mediated repression of
SF1-regulated steroidogenic genes and inhibition of testosterone synthesis in wild-type and PPARα knockout mouse strains.
It will be necessary to assess the expression of PPARα in fetal
mouse testes to determine whether the lack of induction of testicular maldevelopment by DBP in mice could be caused by the
lack of expression of PPARα in mouse fetal Leydig cells. Lack
of expression of PPARα in mouse fetal testes could explain why
455
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
mediating antiandrogenic effects of DBP at this time in development. The results showed that the majority of interstitial
cells, staining weakly for 3βHSD, also contained PPARα
staining, indicating that these cells could be differentiating
Leydig cells. Studies of fetal testes using electron microscopy
have shown that at GD17 the interstitial tissue contains a significant number of differentiating fetal Leydig cells (Kerr and
Knell, 1988). Hence, it seems likely that the ability of PPARα
to interfere with SF1 binding/transactivation caused by exposure to DBP could precede functional maturity of Leydig
cells, affecting their ability to produce testosterone. PPARα
expression was not observed in tubular regions including
Sertoli cells. This is consistent with the lack of effect of DBP
on FSHR that is expressed primarily in Sertoli cells (Salhanick
and Wiebe, 1980).
To conclude, expression microarray pathways clustering
analysis and ChIP-on-chip microarray analysis of SF1 and
PPARα binding in in utero DBP-exposed fetal rat testes have
shown inhibition of testosterone synthesis gene expression
correlates with inhibition of binding of SF1 to “target” gene
promoters. This effect also correlated with increased binding
of PPARα, a receptor known to be activated by DBP, to the
promoters of these genes. The SF1-regulated gene FSHR, unaffected by DBP at the RNA level, showed no DBP-mediated
alteration to SF1 or PPARα binding. Hence, the effects of DBP
on SF1 binding and expression of steroidogenic genes correlate
with increased binding of PPARα, which is consistent with its
postulated role as an indirect transrepressor of steroidogenic
(SF1-regulated) genes in this model.
Supplementary Data
Supplementary data are available online at http://toxsci.
oxfordjournals.org/.
Funding
ExxonMobil BioMedical Sciences Inc.
Acknowledgments
Technical assistance of Corinne Haines, Barbara Elcombe,
and Beverly Craig is gratefully acknowledged. We also thank
Richard Sharpe for comments on this manuscript and Clemens
Wrzodek for assistance with PPARα-binding site mapping
analysis.
References
Fig. 11. Hypothesis schematic: PPARα acts as an indirect transrepressor of steroidogenic genes in fetal rat testes via CBP coactivator sequestration
and indirect transrepression of SF1-DNA binding in the promoter regions of
steroidogenic “target” genes.
Albro, P. W., and Lavenhar, S. R. (1989). Metabolism of di(2-ethylhexyl)phthalate. Drug Metab. Rev. 21, 13–34.
Baes, M., Castelein, H., Desmet, L., and Declercq, P. E. (1995). Antagonism
of COUP-TF and PPAR alpha/RXR alpha on the activation of the malic
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
fetal mouse testes are resistant to the antiandrogenic effects of
in utero DBP treatment.
Recent studies have shown that human fetal testis explants
(Heger et al., 2012; Mitchell et al., 2012) are also refractory
to the antiandrogenic effects of DBP and a similar explanation could also account for this observation. A recent study by
Desdoits-Lethimonier et al. (2012) has found that DEHP and
its metabolite MEHP inhibit testosterone production in adult
human testes. In this regard, it is intriguing that PPARα has
been shown to be expressed in Leydig cells of adult human testes (Schultz et al., 1999). As the chromosomal context of steroidogenic genes in human testes undoubtedly is different from
that of the rat, it will be interesting to assess whether PPARα
binds to the regulatory regions of these genes in human testes.
To our knowledge, this study is the first one to apply ChIP
microarray analysis (ChIP on chip) in fetal testes. This has
facilitated coordinated analysis of transcription factor binding to a battery of genes involved in DBP-induced testicular
maldevelopment. The binding of SF1 to several testicular maldevelopment genes involved in steroidogenesis and testis development was found to be inhibited by DBP treatment, and this
correlates with increased binding of PPARα and CBP at sites
peripheral to SF1-binding sites. Hence, these data support the
conclusion that PPARα could inhibit SF1 by indirectly disrupting the binding and activity of this transcription factor in fetal
rat testes. A schematic summarizing this hypothesis is shown
in Figure 11. We have shown for the first time that PPARα
binds to the promoters of certain steroidogenic genes and that
increased PPARα binding correlates with DBP-mediated inhibition of SF1 binding and steroidogenic gene expression.
Our immunostaining studies have confirmed that PPARα
is expressed in the fetal rat testes at GD15; hence, the ontogeny of its expression is consistent with a postulated role in
456
PLUMMER ET AL.
enzyme gene promoter: Modulation by 9-cis RA. Biochem. Biophys. Res.
Commun. 215, 338–345.
Bility, M. T., Thompson, J. T., McKee, R. H., David, R. M., Butala, J. H.,
Vanden Heuvel, J. P., and Peters, J. M. (2004). Activation of mouse and
human peroxisome proliferator-activated receptors (PPARs) by phthalate
monoesters. Toxicol. Sci. 82, 170–182.
Carruthers, C. M., and Foster, P. M. (2005). Critical window of male reproductive tract development in rats following gestational exposure to di-n-butyl
phthalate. Birth Defects Res. B Dev. Reprod. Toxicol. 74, 277–285.
Chou, S. J., Lai, K. N., and Chung, B. C. (1996). Characterization of the
upstream sequence of the human CYP11A1 gene for cell type-specific
expression. J. Biol. Chem. 271, 22125–22129.
Clewell, R. A., Campbell, J. L., Ross, S. M., Gaido, K. W., Clewell, H. J., 3rd,
and Andersen, M. E. (2009). Assessing the relevance of in vitro measures of
phthalate inhibition of steroidogenesis for in vivo response. Toxicol. In Vitro
24, 327–334.
Corton, J. C., and Lapinskas, P. J. (2005). Peroxisome proliferator-activated
receptors: Mediators of phthalate ester-induced effects in the male reproductive tract? Toxicol. Sci. 83, 4–17.
Desdoits-Lethimonier, C., Albert, O., Le Bizec, B., Perdu, E., Zalko, D.,
Courant, F., Lesne, L., Guille, F., Dejucq-Rainsford, N., and Jegou, B.
(2012). Human testis steroidogenesis is inhibited by phthalates. Hum.
Reprod. 27, 1451–1459.
Dong, H., Yauk, C. L., Rowan-Carroll, A., You, S. H., Zoeller, R. T., Lambert,
I., and Wade, M. G. (2009). Identification of thyroid hormone receptor binding sites and target genes using ChIP-on-chip in developing mouse cerebellum. PLoS ONE 4, e4610.
Ferraz-de-Souza, B., Lin, L., Shah, S., Jina, N., Mike Hubank, M., Dattani, M.
T., and Achermann, J. C. (2011). ChIP-on-chip analysis reveals angiopoietin 2 (Ang2, ANGPT2) as a novel target of steroidogenic factor-1 (SF-1,
NR5A1) in the human adrenal gland. FASEB J. 25(4), 1166–1175.
Fisher, J. S., MacPherson, S., Marchetti, N., and Sharpe, R. M. (2003). Human
‘testicular dysgenesis syndrome’: A possible model using in-utero exposure
of the rat to dibutyl phthalate. Hum. Reprod. 18(6), 1–13.
Gaido, K. W., Hensley, J. B., Liu, D., Wallace, D. G., Borghoff, S., Johnson, K.
J., Hall, S. J., and Boekelheide, K. (2007). Fetal mouse phthalate exposure
shows that Gonocyte multinucleation is not associated with decreased testicular testosterone. Toxicol. Sci. 97, 491–503.
Gazouli, M., Yao, Z. X., Boujrad, N., Corton, J. C., Culty, M., and Papadopoulos,
V. (2002). Effect of peroxisome proliferators on Leydig cell peripheral-type
benzodiazepine receptor gene expression, hormone-stimulated cholesterol
transport, and steroidogenesis: Role of the peroxisome proliferator-activator
receptor alpha. Endocrinology 143, 2571–2583.
Gray, L. E., Jr, Ostby, J., Furr, J., Price, M., Veeramachaneni, D. N., and Parks,
L. (2000). Perinatal exposure to the phthalates DEHP, BBP, and DINP,
but not DEP, DMP, or DOTP, alters sexual differentiation of the male rat.
Toxicol. Sci. 58, 350–365.
Hannas, B. R., Lambright, C. S., Furr, J., Evans, N., Foster, P. M., Gray, E. L.,
and Wilson, V. S. (2012). Genomic biomarkers of phthalate-induced male
reproductive developmental toxicity: A targeted RT-PCR array approach for
defining relative potency. Toxicol. Sci. 125, 544–557.
Heckert, L. L. (2001). Activation of the rat follicle-stimulating hormone receptor promoter by steroidogenic factor 1 is blocked by protein kinase a and
requires upstream stimulatory factor binding to a proximal E box element.
Mol. Endocrinol. 15, 704–715.
Heger, N. E., Hall, S. J., Sandrof, M. A., McDonnell, E. V., Hensley, J. B.,
McDowell, E. N., Martin, K. A., Gaido, K. W., Johnson, K. J., and Boekelheide,
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
Clewell, R. A., Kremer, J. J., Williams, C. C., Campbell, J. L., Jr, Andersen, M.
E., and Borghoff, S. J. (2008). Tissue exposures to free and glucuronidated
monobutylyphthalate in the pregnant and fetal rat following exposure to di-nbutylphthalate: Evaluation with a PBPK model. Toxicol. Sci. 103, 241–259.
K. (2012). Human fetal testis xenografts are resistant to phthalate-induced
endocrine disruption. Environ. Health Perspect. 120, 1137–1143.
Hurst, C. H., and Waxman, D. J. (2003). Activation of PPARalpha and
PPARgamma by environmental phthalate monoesters. Toxicol. Sci. 74,
297–308.
IJpenberg, A., Jeannin, E., Wahli, W., and Desvergne, B. (1997). Polarity and
specific sequence requirements of peroxisome proliferator-activated receptor (PPAR)/retinoid X receptor heterodimer binding to DNA. A functional
analysis of the malic enzyme gene PPAR response element. J. Biol. Chem.
272, 20108–20117.
Ito, M., Park, Y., Weck, J., Mayo, K. E., and Jameson, J. L. (2000). Synergistic
activation of the inhibin alpha-promoter by steroidogenic factor-1 and cyclic
adenosine 3’,5’-monophosphate. Mol. Endocrinol. 14, 66–81.
Jeyasuria, P., Ikeda, Y., Jamin, S. P., Zhao, L., De Rooij, D. G., Themmen,
A. P., Behringer, R. R., and Parker, K. L. (2004). Cell-specific knockout of
steroidogenic factor 1 reveals its essential roles in gonadal function. Mol.
Endocrinol. 18(7), 1610–1619.
Johnson, K. J., Hensley, J. B., Kelso, M. D., Wallace, D. G., and Gaido, K.
W. (2007). Mapping gene expression changes in the fetal rat testis following acute dibutyl phthalate exposure defines a complex temporal cascade of
responding cell types. Biol. Reprod. 77, 978–989.
Johnson, K. J., Heger, N. E., and Boekelheide, K. (2012). Of mice and men
(and rats): Phthalate-induced fetal testis endocrine disruption is speciesdependent. Toxicol. Sci. 129, 235–248.
Kerr, J. B., and Knell, C. M. (1988). The fate of fetal Leydig cells during
the development of the fetal and postnatal rat testis. Development 103,
535–544.
Kuhl, A. J., Ross, S. M., and Gaido, K. W. (2007). CCAAT/enhancer binding
protein beta, but not steroidogenic factor-1, modulates the phthalate-induced
dysregulation of rat fetal testicular steroidogenesis. Endocrinology 148,
5851–5864.
Liu, K., Lehmann, K. P., Sar, M., Young, S. S., and Gaido, K. W. (2005). Gene
expression profiling following in utero exposure to phthalate esters reveals
new gene targets in the etiology of testicular dysgenesis. Biol. Reprod. 73,
180–192.
Lopez, D., Sandhoff, T. W., and McLean, M. P. (1999). Steroidogenic factor-1
mediates cyclic 3’,5’-adenosine monophosphate regulation of the high density lipoprotein receptor. Endocrinology 140, 3034–3044.
Mahood, I. K., Hallmark, N., McKinnell, C., Walker, M., Fisher, J. S., and
Sharpe, R. M. (2005). Abnormal Leydig cell aggregation in the fetal testis
of rats exposed to di (n-butyl) phthalate and its possible role in testicular
dysgenesis. Endocrinology 146, 613–623.
Manna, P. R., and Stocco, D. M. (2005). Regulation of the steroidogenic acute
regulatory protein expression: Functional and physiological consequences.
Curr. Drug Targets Immune Endocr. Metabol. Disord. 5, 93–108.
Martin, L. J., and Tremblay, J. J. (2010). Nuclear receptors in Leydig cell gene
expression and function. Biol. Reprod. 83, 3–14.
Mascaro, C., Nadal, A., Hegardt, F. G., Marrero, P. F., and Haro, D. (2000).
Contribution of steroidogenic factor 1 to the regulation of cholesterol synthesis. Biochem. J. 350(Pt 3), 785–790.
McCampbell, A., Taylor, J. P., Taye, A. A., Robitschek, J., Li, M., Walcott, J.,
Merry, D., Chai, Y., Paulson, H., Sobue, G., et al. (2000). CREB-binding
protein sequestration by expanded polyglutamine. Hum. Mol. Genet. 9,
2197–2202.
Misra, P., Qi, C., Yu, S., Shah, S. H., Cao, W. Q., Rao, M. S., Thimmapaya, B.,
Zhu, Y., and Reddy, J. K. (2002). Interaction of PIMT with transcriptional
coactivators CBP, p300, and PBP differential role in transcriptional regulation. J. Biol. Chem. 277, 20011–20019.
Mitchell, R. T., Childs, A. J., Anderson, R. A., van den Driesche, S., Saunders,
P. T., McKinnell, C., Wallace, W. H., Kelnar, C. J., and Sharpe, R. M. (2012).
Do phthalates affect steroidogenesis by the human fetal testis? Exposure of
TRANSCRIPTION FACTORS AND DIBUTYLPHTHALATE
Soosaar, A., Neuman, K., Nornes, H. O., and Neuman, T. (1996). Cell type specific regulation of COUP-TF II promoter activity. FEBS Lett. 391, 95–100.
Tamasi, V., Miller, K. K. M., Ripp, S. L., Vila, E., Geoghagen, T. E., and
Prough, R. A. (2008) Modulation of receptor phosphorylation contributes
to Activation of Peroxisome Proliferator activated receptor alpha by dehydroepiandrosterone and other peroxisome proliferators. Mol. Pharmacol. 73,
968–976.
Toda, K., Okada, T., Miyaura, C., and Saibara, T. (2003). Fenofibrate, a ligand
for PPARalpha, inhibits aromatase cytochrome P450 expression in the ovary
of mouse. J. Lipid Res. 44, 265–270.
Tugwood, J. D., Issemann, I., Anderson, R. G., Bundell, K. R., McPheat, W. L.,
and Green, S. (1992). The mouse peroxisome proliferator activated receptor
recognizes a response element in the 5’ flanking sequence of the rat acyl
CoA oxidase gene. EMBO J. 11, 433–439.
Val, P., Lefrançois-Martinez, A. M., Veyssière, G., and Martinez, A. (2003).
SF-1 a key player in the development and differentiation of steroidogenic
tissues. Nucl. Recept. 1, 8.
van den Driesche, S., Walker, M., McKinnell, C., Scott, H. M., Eddie, S. L.,
Mitchell, R. T., Seckl, J. R., Drake, A. J., Smith, L. B., Anderson, R. A.,
et al. (2012). Proposed role for COUP-TFII in regulating fetal Leydig cell
steroidogenesis, perturbation of which leads to masculinization disorders in
rodents. PLoS ONE 7, e37064.
Weng, L., Dai, H., Zhan, Y., He, Y., Stepaniants, S. B., and Bassett, D.E.
(2006). Rosetta error model for gene expression analysis. Bioinformatics 22,
1111–1121.
Williams, D. T., and Blanchfield, B. J. (1975). The retention, distribution,
excretion, and metabolism of dibutyl phthalate-7-14 C in the rat. J. Agric.
Food Chem. 23, 854–858.
Yu, R. N., Ito, M., and Jameson, J. L. (1996). The murine Dax-1 promoter
is stimulated by SF-1 (steroidogenic factor-1) and inhibited by COUP-TF
(Chicken Ovalbumin Upstream Promoter-Transcription Factor) via a
composite nuclear receptor-regulatory element. Mol. Endocrinol. 12(7),
1010–1022.
Zimmermann, S., Schwärzler, A., Buth, S., Engel, W., and Adham, I. M. (1998).
Transcription of the Leydig insulin-like gene is mediated by steroidogenic
factor-1. Mol. Endocrinol. 12, 706–713.
Downloaded from http://toxsci.oxfordjournals.org/ at Society of Toxicology on January 4, 2014
human fetal testis xenografts to di-n-butyl phthalate. J. Clin. Endocrinol.
Metab. 97, E341–E348.
Miyata, K. S., Zhang, B., Marcus, S. L., Capone, J. P., and Rachubinski, R. A.
(1993). Chicken ovalbumin upstream promoter transcription factor (COUP-TF)
binds to a peroxisome proliferator-responsive element and antagonizes peroxisome proliferator-mediated signaling. J. Biol. Chem. 268, 19169–19172.
National Toxicology Program. (2007). NTP Technical Report on the Toxicity
Studies of Wy-14,643 Administered in Feed to Sprague-Dawley Rats, B6C3F
Mice and Syrian Hamsters. National Toxicology Program Toxicity Report
Series Number 62. NTP, Research Triangle Park, NC.
Neve, B. P., Fruchart, J. C., and Staels, B. (2000). Role of the peroxisome proliferator-activated receptors (PPAR) in atherosclerosis. Biochem. Pharmacol.
60, 1245–1250.
Parks, L. G., Ostby, J. S., Lambright, C. R., Abbott, B. D., Klinefelter, G. R.,
Barlow, N. J., and Gray, L. E., Jr. (2000). The plasticizer diethylhexyl phthalate induces malformations by decreasing fetal testosterone synthesis during
sexual differentiation in the male rat. Toxicol. Sci. 58, 339–349.
Plummer, S., Sharpe, R. M., Hallmark, N., Mahood, I. K., and Elcombe, C.
(2007). Time-dependent and compartment-specific effects of in utero exposure to Di(n-butyl) phthalate on gene/protein expression in the fetal rat testis as revealed by transcription profiling and laser capture microdissection.
Toxicol. Sci. 97, 520–532.
Salhanick, A. I., and Wiebe, J. P. (1980). FSH receptors in isolated Sertoli cells:
Changes in concentration of binding sites at the onset of sexual maturation.
Life Sci. 26, 2281–2288.
Sandhoff, T. W., Hales, D. B., Hales, K. H., and McLean, M. P. (1998).
Transcriptional regulation of the rat steroidogenic acute regulatory protein
gene by steroidogenic factor 1. Endocrinology 139, 4820–4831.
Saramaki, A., Diermeier, S., Kellner, R., Laitinen, H., Vaïsänen, S., and
Carlberg, C. (2009). Cyclical chromatin looping and transcription factor
association on the regulatory regions of the p21 (CDKN1A) gene in response
to 1alpha,25-dihydroxyvitamin D3. J. Biol. Chem. 284, 8073–8082.
Schultz, R., Yan, W., Toppari, J., Volkl, A., Gustaffson, J., and Pelto-Huikko,
M. (1999). Expression of peroxisome proliferator-activated receptor a messenger ribonucleic acid and protein in human and rat testis. Endocrinology
140(7), 2968–2975.
457