AACR poster 5248 - Mersana Therapeutics
advertisement
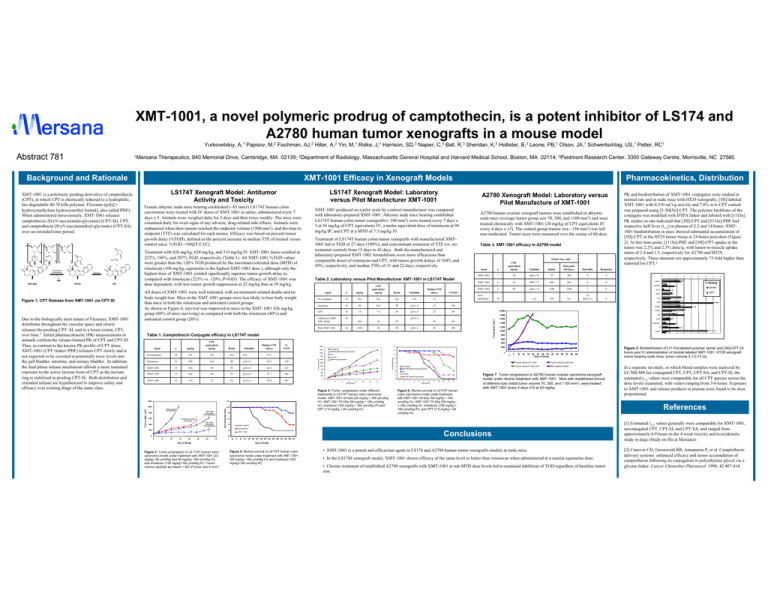
XMT-1001, a novel polymeric prodrug of camptothecin, is a potent inhibitor of LS174 and A2780 human tumor xenografts in a mouse model Yurkovetskiy, A,1 Papisov, M,2 Fischman, AJ,2 Hiller, A,2 Yin, M,1 Rolke, J,1 Harrison, SD,3 Napier, C,3 Ball, R,3 Sheridan, K,3 Hollister, B,3 Leone, PB,1 Olson, JA,1 Schwertschlag, US,1 Petter, RC1 Mersana Therapeutics, 840 Memorial Drive, Cambridge, MA 02139; 2Department of Radiology, Massachusetts General Hospital and Harvard Medical School, Boston, MA 02114; 3Piedmont Research Center, 3300 Gateway Centre, Morrisville, NC 27560 O O O O O OH O O O O LS174T Xenograft Model: Antitumor Activity and Toxicity O OH N O O H N O m O O O O HO k n N O XMT-1001 HO O O O intramolecular transacylation O N O N O O N O O PHF + OH N O N hydrolysis O N O CPT-SI O CPT Figure 1. CPT Release from XMT-1001 via CPT-SI Due to the biologically inert nature of Fleximer, XMT-1001 distributes throughout the vascular space and slowly releases the prodrug CPT–SI, and to a lesser extent, CPT, over time.1 Initial pharmacokinetic (PK) measurements in animals confirm the release-limited PK of CPT and CPT-SI. Thus, in contrast to the known PK profile of CPT alone, XMT-1001 (CPT+linker+PHF) releases CPT slowly and is not expected to be excreted at potentially toxic levels into the gall bladder, intestine, and urinary bladder. In addition, the dual-phase release mechanism affords a more sustained exposure to the active lactone form of CPT as the lactone ring is stabilized in prodrug CPT-SI. Both distribution and extended release are hypothesized to improve safety and efficacy over existing drugs of the same class. Treatment with 826 mg/kg, 628 mg/kg, and 314 mg/kg IV XMT-1001 doses resulted in 223%, 196%, and 207% TGD, respectively (Table 1). All XMT-1001 %TGD values were greater than the 120% TGD produced by the maximum tolerated dose (MTD) of irinotecan (100 mg/kg, equimolar to the highest XMT-1001 dose ), although only the highest dose of XMT-1001 yielded significantly superior tumor growth delay as compared with irinotecan (223% vs. 120%, P=0.05). The efficacy of XMT-1001 was dose dependent, with less tumor growth suppression at 22 mg/kg than at 59 mg/kg. All doses of XMT-1001 were well tolerated, with no treatment-related deaths and no body weight loss. Mice in the XMT-1001 groups were less likely to lose body weight than mice in both the irinotecan and untreated control groups. As shown in Figure 4, survival was improved in mice in the XMT-1001 826 mg/kg group (80% of mice surviving) as compared with both the irinotecan (40%) and untreated control group (20%). A2780 Xenograft Model: Laboratory versus Pilot Manufacture of XMT-1001 XMT-1001 produced on a pilot scale by contract manufacturer was compared with laboratory-prepared XMT-1001. Athymic nude mice bearing established LS174T human colon tumor xenografts (~100 mm3) were treated every 7 days x 3 at 56 mg/kg of CPT equivalents IV, a molar equivalent dose of irinotecan at 94 mg/kg IP, and CPT at a MTD of 7.5 mg/kg IV. Treatment of LS174T human colon tumor xenografts with manufactured XMT1001 led to TGD of 27 days (180%), and concomitant extension of TTE (vs. notreatment control) from 15 days to 42 days. Both the manufactured and laboratory-prepared XMT-1001 formulations were more efficacious than comparable doses of irinotecan and CPT, with tumor growth delays of 104% and 49%, respectively, and median TTEs of 31 and 22 days, respectively. Table 2. Laboratory versus Pilot Manufacturer XMT-1001 in LS174T Model Agent n mg/kg CPT equivalents mg/kg No treatment 14 NA NA A2780 human ovarian xenograft tumors were established in athymic nude mice (average tumor group size 70, 300, and 1100 mm3) and were treated chronically with XMT-1001 (20 mg/kg of CPT equivalents IV every 4 days x 15). The control group (tumor size ~150 mm3) was left non-medicated. Tumor sizes were measured over the course of 60 days. Table 3. XMT-1001 efficacy in A2780 model Tumor size, mm3 Agent n CPT equivalents mg/kg Schedule Initial End point (60 days) Mortality XMT-1001 7 20 q4d x 15 70 180 0 Agent n mg/kg CPT equivalents mg/kg Route No treatment 10 NA NA NA Irinotecan 10 100 NA Schedule NA Median TTE (days) % TGD 19.5 -- IP q7d x 3 42.9 120 XMT-1001 10 826 59 IV q7d x 3 63.0 223 XMT-1001 10 628 44 IV q7d x 3 57.7 196 10 XMT-1001 314 22 IV q7d x 3 59.8 207 irinotecan Route NA Schedule %TGD NA 15 -- 14 94 NA IP q7d x 3 31 104 CPT 14 7.5 7.5 IV q7d x 3 22 49 Laboratory XMT1001 40 kd 14 10 Control group (untreated) XMT-1001 22 mg/kg CPT-equivalents 800 600 Irinotecan Control 100 mg/kg XMT-1001 59 mg/kg CPT-equivalents 400 8 6 20 q4d x 15 300 390 0 0 6 20 q4d x 15 1100 1240 1 0 Nonmedicated 10 - n/a 150 n/a 10 (Day 21) 0 4 2 0 0 0 5 10 15 20 25 30 35 Day of Study 0 tumor 1 2 3 4 5 6 7 8 % dose/g Carrier brain CPT heart lung Pilot XMT-1001 14 spleen kidney 2,000 skin 1,800 826 56 IV 1018 56 IV q7d x 3 43 191 42 180 1,600 bone 1,400 stomach 1,200 GI 1,000 blood 800 600 400 2500 No treatment 2250 XMT1001 40kDa laboratory preparation 2000 CPT 1750 200 14 - 12 irinotecan 1500 16 XMT1001 pilot preparation 1250 1000 750 8 No treatment 6 Irinotecan XMT 1001 70 kDa pilot preparation 0 1 4 9 13 16 20 23 27 10 14 18 22 26 30 35 40 Days of Study 44 48 52 56 Tumor volume 70 mm3 Tumor volume 300 mm3 Tumor volume 1100 mm3 Not treated control 60 CPT 2 0 5 XMT 1001 40 kDa laboratory preparation 4 500 250 - 10 1 4 9 13 16 20 23 27 30 34 37 41 Day of Study Figure 6. Murine survival in LS174T human colon carcinoma model under treatment with XMT-1001 40 kDa (59 mg/kg = 160 umol/kg IV), XMT-1001 70 kDa (59 mg/kg = 160 μmol/kg IV), irinotecan (100 mg/kg = 160 umol/kg IP), and CPT (7.5 mg/kg = 60 μmol/kg IV). Figure 7. Tumor progression in A2780 human ovarian carcinoma xenograft model under chronic treatment with XMT-1001. Mice with established tumors of different size (initial tumor volume 70, 300, and 1100 mm3) were treated with XMT-1001 every 4 days x15 at 20 mg/kg. Figure 2. Biodistribution of [111In]-labeled polymer carrier and [3H]-CPT 24 hours post IV administration of double-labeled XMT-1001. HT29 xenograft tumor bearing nude mice, tumor volume 0.1-0.15 mL. In a separate rat study, in which blood samples were analyzed by LC/MS/MS for conjugated CPT, CPT, CPT-SA, and CPT-SI, the estimated t1/2 values were comparable for all CPT species across the dose levels examined, with values ranging from 3-6 hours. Exposure to XMT-1001 and release products in plasma were found to be dose proportional. References 6 200 Figure 3: Tumor progression in LS 174T human colon carcinoma model under treatment with XMT-1001 (22 mg/kg= 60 μmol/kg and 59 mg/kg= 160 umol/kg IV) and irinotecan (100 mg/kg=160 μmol/kg IP). Tumor volume reported as means + SD of tumor size in mm3. 4 XMT-1001 XMT-1001 q7d x 3 Figure 5. Tumor progression under different treatments in LS174T human colon carcinoma model: XMT-1001 40 kDa (59 mg/kg = 160 umol/kg IV), XMT-1001 70 kDa (59 mg/kg = 160 μmol/kg IV), irinotecan (100 mg/kg = 160 umol/kg IP) and CPT (7.5 mg/kg = 60 μmol/kg IV). 12 1000 Remission liver Day of Study 1200 PK and biodistribution of XMT-1001 conjugates were studied in normal rats and in nude mice with HT29 xenografts. [3H]-labeled XMT-1001 with 0.210 mCi/g activity and 7.0% w/w CPT content was prepared using [5-3H(N)]-CPT. The polymer backbone of the conjugate was modified with DTPA linker and labeled with [111In]. PK studies in rats indicated that [3H]-CPT and [111In]-PHF had respective half-lives (t1/2) in plasma of 2.2 and 14 hours. XMT1001 biodistribution in mice showed substantial accumulation of [3H]-CPT in the HT29 tumor tissue at 24 hours post-dose (Figure 2). At this time-point, [111In]-PHF and [3H]-CPT uptake in the tumor was 2.2% and 2.5% dose/g, with tumor-to-muscle uptake ratios of 2.4 and 1.5, respectively for A2780 and HT29, respectively. These amounts are approximately 75-fold higher than reported for CPT.2 muscles Median TTE (days) Table 1. Camptothecin Conjugate efficacy in LS174T model Surviving Animals OH Tumor Size, mm 3 OH Pharmacokinetics, Distribution LS174T Xenograft Model: Laboratory versus Pilot Manufacturer XMT-1001 Female athymic nude mice bearing established (~85 mm3) LS174T human colon carcinomas were treated with IV doses of XMT-1001 in saline, administered every 7 days x 3. Animals were weighed daily for 5 days and then twice weekly. The mice were examined daily for overt signs of any adverse, drug-related side effects. Animals were euthanized when their tumors reached the endpoint volume (1500 mm3), and the time to endpoint (TTE) was calculated for each mouse. Efficacy was based on percent tumor growth delay (%TGD), defined as the percent increase in median TTE of treated versus control mice: %TGD =100[(T-C)/C]. Surviving Animals XMT-1001 is a polymeric prodrug derivative of camptothecin (CPT), in which CPT is chemically tethered to a hydrophilic, bio-degradable 40-70 kDa polymer, Fleximer (poly[1hydroxymethylene hydroxymethyl formal], also called PHF). When administered intravenously, XMT-1001 releases camptothecin-20-(N-succinimido-glycinate) (CPT-SI), CPT, and camptothecin-20-(N-succinamidoyl-glycinate) (CPT-SA) over an extended time period. XMT-1001 Efficacy in Xenograft Models Tumor Size (mm3) Background and Rationale Tumor Vol (mm3) Abstract 781 1 Not treated Irinotecan XMT-1001 0 4 8 11 15 18 22 25 29 32 36 39 43 46 50 53 Conclusions [1] Estimated t1/2 values generally were comparable for XMT-1001, unconjugated CPT, CPT-SI, and CPT-SA, and ranged from approximately 4-9 hours in the 4-week toxicity and toxicokinetic study in dogs (Study on file at Mersana). Day of Study Figure 4. Murine survival in LS174T human colon carcinoma model under treatment with XMT-1001 (59 mg/kg= 160 μmol/kg IV) and irinotecan (100 mg/kg=160 umol/kg IP). • XMT-1001 is a potent and efficacious agent in LS174 and A2780 human tumor xenografts models in nude mice. • In the LS174S xenograft model, XMT-1001 shown efficacy of the same level or better than irinotecan when administered at a similar equimolar dose. • Chronic treatment of established A2780 xenografts with XMT-1001 at sub-MTD dose levels led to sustained inhibition of TGD regardless of baseline tumor size. [2] Conover CD, Greenwald RB, Annapurna P, et al. Camptothecin delivery systems: enhanced efficacy and tumor accumulation of camptothecin following its conjugation to polyethylene glycol via a glycine linker. Cancer Chemother Pharmacol. 1998; 42:407-414.