Serum Vitamin B12 and Folic Acid Levels in Acute Cerebral
advertisement

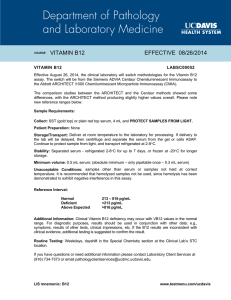
and 155-161 Folic Acid Levels in Acute Cerebral Infarction Tohoku J. Exp. Med., 2004,B12204, 155 Serum Vitamin B12 and Folic Acid Levels in Acute Cerebral Atherothrombotic Infarction ABDULKADIR KOCER, NURHAN INCE,1 E. CUNEYT CANBULAT2 and MEHMET SARGIN3 Department of Neurology, Dr. Lutfi Kirdar Kartal Education and Research Hospital, 1Department of Public Health, Istanbul Medical Faculty, University of Istanbul, 2Department of Clinical Biochemistry, PTT Education and Research Hospital, and 3Department of Family Medicine, Dr. Lutfi Kirdar Kartal Education and Research Hospital, Istanbul, Turkey KOCER, A., INCE, N., CANBULAT, E.C. and SARGIN, M. Serum Vitamin B12 and Folic Acid Levels in Acute Cerebral Atherothrombotic Infarction. Tohoku J. Exp. Med., 2004, 204 (2), 155-161 ── Hyperhomocysteinemia is an independent risk factor for atherothrombotic cerebral stroke. Vitamin B12 and folic acid are important determinants of homocysteine metabolism. We aimed to evaluate the relationship, if present, between vitamin B12 and folic acid levels and acute cerebral stroke in this study. Blood aliquots drawn within 24 hours after the stroke from hospitalized patients (n=66) with the diagnosis of acute ischemic cerebrovascular episode and also blood samples from 38 healthy controls without any vascular risk factor were analyzed. With a competitive, chemoluminescence assay, serum levels of vitamin B12 and folic acid were measured in blood samples taken within 24 hours after the stroke. The differences and correlations were tested using frequency test, student-t test and multivariate analysis. Mean serum vitamin B12 levels were significantly lower in the patients than in the control subjects, 245.40 (S.D.: 72.9) and 343.2 (S.D.: 113.0) pg/ml respectively (p=0.0001). This difference was independent from other risk factors. Likewise, mean serum folic acid levels were lower in the patients than in the control subjects, 4.62 (S.D.: 1.94) and 5.97 (S.D.: 1.19) ng/ml, respectively (p=0.003). Mean serum levels of vitamin B12 and folate at the convalescence phase were 253.05 (S.D.: 68.78) pg/ml and 4.48 (S.D.: 2.08) ng/ml, respectively; the values obtained at the acute phase were not significantly different from the values obtained at the convalescence phase. We conclude that low vitamin B12 and folic acid concentrations are associated with an increased risk of stroke, and the relationship for vitamin B12 is independent from the other known modifiable stroke risk factors. For understanding the effects of B12 and folate in stroke patients, more detailed follow-up studies with long period are needed. ──── hyperhomocysteinemia; B12; folate; atherotrombosis; stroke © 2004 Tohoku University Medical Press Received March 30, 2004; revision accepted for publication August 9, 2004. Address for reprints: Kocer Abdulkadir, M.D., Chief Assistant, Department of Neurology, Dr. Lutfi Kirdar Teaching and Research Hospital, Istanbul, Turkey. e-mail: abdulkadirkocer@yahoo.com This article was partially presented as poster (Poster Number 3 at 18 May 2004) at International Congress Of Neuromediterranee VI, 17-21 May 2004, Istanbul, Turkey. 155 156 A. Kocer et al. Hyperhomocysteinemia (HH) has been observed in arterial and venous thrombotic diseases. Even mild or moderate degrees of increments are known to increase the risk of vasooclussive diseases (Fortin and Genest 1995; Saw 1999; Robins et al. 2001; Yilmaz et al. 2001). During metabolization of homocysteine, vitamin B6, folic acid and vitamin B12 are required. Deficiencies of vitamin B6, folic acid and vitamin B12 lead to the interruption of metabolic pathways, and homocysteine rapidly escapes from tissues (Brattstrom et al. 1992; Robinson et al. 1998). The role of HH in the pathogenesis of atherothrombosis has not been fully elucidated. HH is known to lead to the production of free oxygen radicals. It also stimulates the development of smooth muscles and inhibits intracellular methylation processes (Tsai et al. 1996; Dalton et al. 1997; Engman 1998; Selhub and D’Angelo 1998). HH alters anticoagulation pathways within endothelium via inhibition of thrombomodulin formation as well (Engman 1998; Selhub and D’Angelo 1998; Saw 1999). Studies evaluating both an established threshold value for vitamins and also investigating whether HH is the only factor enhancing atherothrombotic predisposition in B6, B12 and folate deficiency will certainly lead to important outcomes regarding preventive medicine (Engman 1998; Robinson et al. 1998; Saw 1999; Robins et al. 2001; He et al. 2004). Besides methodological difficulties, homocysteine assays are relatively costly and they have not come into routine usage. In this study, we evaluated the effects of vitamin B12 and folate levels on acute cerebrovascular stroke, which is an important cause of morbidity and mortality worldwide. The present study searched for an answer to an issue: “Is deficiency of vitamin B12 or folic acid a responsible risk factor predisposing to atherothrombosis ? .” MATERIAL AND METHODS Study design and setting In this study, blood samples were drawn within 24 hours after the stroke from hospitalized patients (n=66) with the diagnosis of acute cere- brovascular episode in PTT Training and Research Hospital -related to PTT establishment serving post, telephone and telegraph services in Turkey and PTT word contains the first letters of Post, Telephone, and Telegraph words-, Istanbul, Turkey and also blood samples from 38 similarly age- and sex-matched healthy control subjects without any vascular risk factors were analyzed. After at least one month, we had blood analysis of vitamins of patients in order to compare with acute phase results. Before each analysis, the objective of the study was described and informed consent was obtained from all patients. Definition of stroke and modifiable risk factors The diagnosis of stroke was made by a neurologist according to the criteria of World Health Organization defining stroke as rapidly developing clinical symptoms lasting more than 24 hours or leading to death without any other etiology other than a vascular abnormality (Hatano 1976). The following criteria were used for the diagnosis of stroke: clinical evidence of stroke and computed tomography (CT) evidence of cerebral infarction without demonstrable source of embolism. Patients were evaluated with cranial CT (n=54) and cranial magnetic resonance imaging (MRI) (n=25) to define stroke, and were grouped as anterior and posterior system infarctions. Lacunars infarcts without large artery thrombosis, thromboembolic infarcts and hemorrhagic infarcts were not included in this study. We did not include people with a history of vitamin complex tablets intake within last three months. The modifiable risk factors were noted. Hypertension was considered to be present if at the time of diagnosis the subjects had a systolic blood pressure >160 mmHg or a diastolic pressure >95 mmHg, and if treatment for high blood pressure was administered previously. Hypercholesterolemia was considered present if subjects had serum total cholesterol >200 mg/100 ml. Hyperglycemia was considered present if subjects had a serum glucose level >115 mg/100 ml, or if treatment for diabetes was started previously. B12 and Folic Acid Levels in Acute Cerebral Infarction Laboratory analysis Routine hematological, biochemical and microbiologic analyses (blood glucose, urea, creatinine, total lipid, triglyceride, cholesterol, lipoproteins, creatinine phosphokinase, AST, ALT, bleeding, coagulation, prothrombine and partial prothrombine times) were performed. With a competitive, chemoluminescence assay using Immulite 2000 (DPC, Los Angeles, CA, USA) analyzer, serum levels of vitamin B12 and folic acid were measured in blood samples taken within 24 hours after the stroke. Statistical Analysis Intergroup differences and correlations were tested using frequency test, student t-test and multiple logistic regression. Data were expressed as mean and Standard Deviation (S.D.) in brackets. All analyses were made using the SPSS 10.0 version statistical software package, and probability value of less than 0.05 was accepted to be statistically significant. RESULTS The study group consisted of 66 patients and 38 control subjects with similar distribution of gender and age. Descriptive features of patients are shown in Table 1. Mean ages of female and 157 male patients were 67.6 (S.D.: 9.9 years, R: 50-89) and 61.5 (S.D.: 11.5 years, R: 44-85), respectively. The average stay in hospital was 11.9 (S.D.: 6.15) days. The correlations between serum levels of B12 and patients’ ages were found to be statistically significant (p=0.0001). The correlations between serum levels of folate and patients’ ages were not significant (p=0.286). The correlations between serum levels of B12, folate and controls’ ages were not found to be statistically significant (p=0.062 for B12, and p=0.70 for folate). When cohort of patients was evaluated, mean B12 values were detected to be 283.6 (S.D.: 82.1) pg/ml for females and 207.13(S.D.: 32.6) pg/ml for males; the difference was significant (p=0.0001). There was no relation between gender and mean folate levels in the patient group (males: 4.59 [S.D.: 1.47], female: 4.66 [S.D.: 2.39], p=0.902). As seen on Table 1, mean serum levels of vitamin B12 were significantly lower in the patient group than in the control group: 245.4 (S.D.: 72.9) and 343.2 ( S . D .: 113.0) pg/ml, respectively (p=0.0001). Mean serum folic acid levels of patients were lower than those of control subjects as well (4.62 s.d.: 1.94 and 5.97 S.D.: 1.19 ng/ml, respectively) and the difference was statistically significant (p=0.003). Mean serum levels of vitamin B12 (253.05 [S.D.: 68.78] pg/ml) and folate TABLE 1. Descriptive characteristics of patients and control group Case (n) Gender Male Female Mean age (years) Patients Controls 66 34 (%51.5) 32 (%48.5) 64.46 (11.10) 38 20 (%52.6) 18 (%47.4) 60.28 (12.96) p value 0.931 0.085 Serum B12 level (pg/ml) * N: 174-878 pg/ml Mean±S.D. Median 245.4 (72.9) 235 (R: 160-479) 343.2 (113.0) 329 (R: 203-635) 0.0001 Serum folate level (ng/ml) * N: 3-17 ng/ml Mean±S.D. Median 4.62 (1.94) 4.96 (R: 1.51-9.20) 5.97 (1.19) 5.54 (R: 4.0-7.51) 0.003 * Our Lab’s reference ranges. 158 A. Kocer et al. (4.48 [ S . D .: 2.08] ng/ml) at the convalescence phase were not significantly different from the acute phase values. B12 values were unrelated to the presence of vascular risk factors. As it was seen in Table 2, the multivariate analysis showed that the odd’s ratio was 1.02 for B 12 (95% CI, 1.005-1.040; p=0.013). When cases with cerebrovascular events were classified according to the localization of the damage (anterior or posterior systems), mean values of vitamin B12 were found to be lower (230.35 [S . D .: 51.59] pg/ml) in the patients whose both systems involved than in the patients with anterior or posterior circulation problems (254.88 [S.D.: 83.07] pg/ml) (p=0.68). Mean folate levels were detected to be lower in cases with anterior or posterior circulation involvement than in the ones with involvement of both anterior and posterior circulations (4.39 [S.D.: 2.09] versus 5.17 [S.D.: 1.47]); but the difference was not statistically significant. The previous stroke history was present in 20 (30.3%) and cardiac disorder was present in 21 (31.8%) of the patients. The presence of cardiac disease in cases with stroke influenced vitamin B12 levels, which were significantly decreased (p=0.002). The presence of previous stroke history in patients did not influence vitamin B12 and folate levels. DISCUSSION HH is suggested to be an independent risk factor for atherosclerotic cerebrovascular diseases aside from classical vascular risk factors such as hypertension, smoking, hyperlipidemia, hyperglycemia and hyperfibrinogenemia (Brattstrom et al. 1992; Giles et al. 1998; Robinson et al. 1998; Sacco et al. 1998). HH exerts unfavorable effects on coagulation factors and platelets. A linear correlation has been demonstrated between peripheral vascular disease and homocysteine metabolism (Selhub and D’Angelo 1998). A negative correlation exists between serum homocysteine metabolites (vitamin B12, folate) and homocysteine levels. Decreases in circulating vitamin B12 and folate levels reveal an increase in the risk of atherothrombosis (Verhof et al. 1996; Robinson et al. 1998; Giles et al. 1998; Siri et al. 1998; He et al. 2004). A correlation between cardiovascular mortality, morbidity and HH has been demonstrated in a number of cross-sectional, case-controlled cohort studies but a range for homocysteine values relevant to the risk of cardiovascular disease has not been defined yet (Verhof et al. 1996; Verhof et al. 1997; Saw 1999). An analysis of 13 different studies performed between 1969 and 1998 revealed that HH associated with vitamin B12 and folate deficiency increases the risk of stroke (Engman 1998). Although moderate reduction of total homocysteine after nondisabling cerebral infarction had no effect on vascular outcomes during the 2 years of follow-up, HH was present in acute and recovery periods of cerebrovascular accidents (Hultberg et al. 1997; Vila et al. 1998; Meicklejohn et al. 2001; Toole et al. 2004). In one of the recent studies, Meicklejhon et al. (2001) TABLE 2. Multivariate analysis of vitamin levels with modifiable risk factors. Hypertension Heart disease Diabetes Mellitus Cholesterol LDL Cholesterol Vitamin B12 Folate B coefficient S.E. Odd’s Ratio 95% CI Significant (p) −.559 .899 −.048 −.030 .046 .022 .472 1.151 1.142 .027 .023 .031 .009 .499 0.572 2.457 0.953 0.970 1.047 1.022 1.603 0.060-5.461 0.262-23.04 0.903-1.006 0.928-1.015 0.985-1.113 1.005-1.040 0.603-4.259 0.627 0.431 0.079 0.186 0.140 0.013 0.344 B12 and Folic Acid Levels in Acute Cerebral Infarction has evaluated the association of HH with episodes of stroke and reported that in the acute phase, the incidence of the risk of stroke did not differ from those of control groups, albeit the level of homocysteine increased in the subsequent phase of stroke. Hultberg et al. (1997) similarly reported the presence of HH during the recovery period. Vila et al. (1998) showed that total plasma homocysteine concentrations were higher in stroke patients compared to controls. Moderate degrees of HH were present in 20% of their cases. It has been associated with vitamin B12 decrease, whereas no correlation was found between HH and folate levels. Verhoef et al. (1996) found a correlation between lower serum B12 levels and cardiovascular diseases independent of total HH levels. On the contrary, they have established that low levels of folate are associated with HH but unrelated to cardiovascular diseases. In another study, Verhoef et al. (1997) likewise found an important relationship between low serum vitamin B12 levels and vascular diseases. In the same study, serum folate levels were assessed to be increased. Giles et al. (1995) have shown that folic acid levels below 9.2 nmol/liter predispose to an increase in the risk of cerebrovascular diseases. Yilmaz et al. (2001) evaluated serum vitamin B12 and folate levels in cases of stroke and found statistically significant correlations among cerebrovascular stroke, serum BI2 and folate levels. In our study serum levels of vitamin B12 and folate were lower in the patient group than in the control group. Like some previous studies, we found that the significance for B12 level was much more prominent when compared to folate (Table 1). Substantial decreases in vitamin B12 and folate levels in cases with acute cases of stroke were found when compared with those of the control group in our study. Multivariate analysis showed that vitamin B12 level decrease was an independent factor for acute stroke in the present study (Table 2). The results of the present study support the thesis suggesting a correlation between decrease in vitamin levels and vascular damage which might result in stroke. HH becomes more prominent in older age 159 groups and in the presence of the risk factors. Dalery et al. (1995) found that homocysteine levels in healthy women were lower than in their male counterparts. Different studies showed that HH is a more important risk factor for women in terms of ischemic stroke (Selhub et al. 2000; Verhoef 2000). Serum vitamin B12 levels manifesting a negative correlation with homocysteine were relatively higher in female patients in our study (p=0.0001). On the other hand, there was no significant relationship between gender and folate levels in patients although females had higher levels of folate. These findings were similar to the literature. Selhub et al. provided reference ranges for vitamins based on sample by sex and ethnicity (Selhub et al. 1999) and similar ranges for vitamin levels were found in the Framingham study population (Selhub et al. 2000). Although those results show that our control population had lower folate level but similar vitamin B12 levels, our vitamin level results were much lower when compared to the study conducted by Yilmaz et al. (2001); that could be explained by different age groups of study subjects. The diagnostic usefulness of folate and vitamin B12 measurements were evaluated considering plasma homocysteine in the present study. We determined vitamin B12 and folate levels because they influence homocysteine concentrations in plasma but we did not measure plasma homocysteine. This point may be a criticism of the present study. Considering only folate and vitamin B12, the sample size would not be sufficient to analyze the predictive value of these two vitamins, especially if there had been a distinct gender difference for vitamin B12. In our study the groups were well matched, so we were able to compare the differences of vitamins. Age is a confounder so that needs to be considered. B12 (but not folate) is decreased with an increasing age in the present study confirming previous papers (Robins et al. 2001; Dharmarajan et al. 2003). In the convalescent period, blood levels of vitamins showed decreased values, too. This supports that decrease in vitamin levels may be a risk 160 A. Kocer et al. factor for atherothrombotic stroke, though Yilmaz et al. (2001) found decreased levels of vitamins in both ischemic and hemorrhagic strokes and claimed that acute phase variations were also likely to effect the serum levels of those vitamins. We concluded that the assessment of serum levels of vitamin B12 and folate levels on acute cerebrovascular stroke was important for definition of risk factors. We think timely screening and replacement of vitamin B12 will help to prevent future stroke events. Although the present study may be thought as a small study with inadequate matching of cases and controls, this study is important with a good selection of groups, because the patients or cases with vitamin usage history, patients with a thromboembolic stroke, patients with pernicious anemia which also increases with age, and patients administered to hospital after 24 hours of stroke were not included. References Brattstrom, L., Lindgren, A., Israelsson, B., Malinow, M.R., Norrving, B., Upson, B. & Hamfelt, A. (1992) Hyperhomocysteinaemia in stroke: prevalence, cause, and relationships to type of stroke and stroke risk factors. Eur. J. Clin. Invest., 22, 214-221. Dalery, K., Lusier-Cacan, S., Selhub, J., Davignon, J., Latour, Y. & Genest, J. (1995) Homocysteine and coronary artery disease in French Canadian subjects: relation With vitamins B12, B6, pyridoxal phosphate, and folate. Am. J. Cardiol., 75, 1107-1111. Dalton, M.L., Gadson, P.J., Wrenn, J. & Rosenquist, T.H. (1997) Homocysteine signal cascade: Production of phospholipids, activation of protein kinase C, and the induction of c-fos and c-mybin smooth muscle cells. FASEB. J., 11, 703-711. Dharmarajan, T.S., Adiga, G.U. & Norkus, E.P. (2003) Vitamin B12 deficiency. Recognizing subtle symptoms in older adults. Geriatrics, 58, 30-34. Engman, M. (1998) Homocysteinemia: new information about an old risk factor for vascular disease. J. Insur. Med., 30, 231-236. Fortin, L.J. & Genest, J. (1995) Measurement of homocyst(e)ine in prediction of arteriosclerosis. Clin. Biochem., 28, 155-162. Giles, W.H., Kittner, S.J., Anda, R.F., Croft, J.B. & Casper, M.I. (1995) Serum folate and risk for ischemic stroke. First National Health and Nutrition Examination Survey epidemiologic follow-up study. Stroke, 26, 1166-1170. Giles, W.H., Croft, J.B., Greenlund, K.J., Ford, E.S. & Kittner, S.J. (1998) Total homocyst(e)ine concentration and the likelihood of nonfatal stroke: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Stroke, 29, 2473-2477. Hatano, S. (1976) Experience from a multicentre stroke register: a preliminary report. Bull. World Health Organ., 54, 541-553. He, K., Merchant, A., Rimm, E.B., Rosner, B.A., Stampfer, M.J., Willett, W.C. & Ascherio, A. (2004) Folate, vitamin B6, and B12 intakes in relation to risk of stroke among men. Stroke, 35, 169-174. Hultberg, B., Anderrson, A. & Lindgren, A. (1997) Marginal folate deficiency as a posssible cause of hyperhomocysteinaemia in stroke patients. Eur. J. Biochem. Clin. Biochem., 35, 25-28. Meicklejohn, D.J., Vickers, M.A., Dijkhuisen, R. & Greaves, M. (2001) Plasma homocysteine concentrations in the acute and convalescent periods of atherothrombotic stroke. Stroke, 32, 57-62. Robins, Wahlin, T.B., Wahlin, A., Winblad, B. & Backman, L. (2001) The influence of serum vitamin B12 and folate status on cognitive functioning in very old age. Biol. Psychol., 56, 247-265. Robinson, K., Arheart, K., Refsum, H., Brattstrom, L., Boers, G., Ueland, P., Rubba, P., Palma-Reis, R., Meleady, R., Daly, L., Witteman, J. & Graham, I. (1998) Low circulating folate and vitamin B6 concentrations: risk factors for stroke, peripheral vascular disease, and coronary artery disease. European COMAC Group. Circulation, 97, 437-443. Sacco, R.L., Roberts, J.K. & Jacobs, B.S. (1998) Homocysteine as a risk factor for ischemic stroke: an epidemiological story in evolution. Neuroepidemiology, 17, 167-173. Saw, S.M. (1999) Homocysteine and atherosclerotic disease: the epidemiologic evidence. Ann. Acad. Med. Singapore, 28, 565-568. Selhub, J. & D’Angelo, A. (1998) Relationship between homocysteine and thrombotic disease. Am. J. Med. Sci., 316, 129-141. Selhub, J., Jacques, P.F., Rosenberg, I.H., Rogers, G., B12 and Folic Acid Levels in Acute Cerebral Infarction Bowman, B.A., Gunter, E.W., Wright, J.D. & Johnson, C.L. (1999) Serum Total Homocysteine Concentrations in the Third National Health and Nutrition Examination Survey (1991-1994): Population Reference Ranges and Contribution of Vitamin Status to High Serum Concentrations. Ann. Intern. Med., 131, 331-339. Selhub, J., Jacques, P.F., Bostom, A.G., Wilson, P.W.F. & Rosenberg, I.H. (2000) Relationship between plasma homocysteine and vitamin status in the Framingham study population. Impact of folic acid fortification. Public Health Rev., 28, 117-145. Siri, P.W., Verhoef, P. & Kok, F.J. (1998) Vitamins B6, B12, and folate: association with plasma total homocysteine and risk of coronary atherosclerosis. J. Am. Coll. Nutr., 17, 435-441. Toole, J.F., Malinow, M.R., Chambless, L.E., Spence, J.D., Pettigrew, L.C., Howard, V.J., Sides, E.G., Wang, C.H. & Stampfer, M. (2004) Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA, 291, 565-575. Tsai, J.C., Wang, H., Parella, M.A., Yoshizumi. M., 161 Sibinga, N.E.S., Tan, L.C., Haber, E., Chang, T.H.T., Schlegel, R. & Lee, M.E. (1996) Induction of cyclin A gene expression by homocyteine in vascular smooth muscle cells. J. Clin. Invest., 146, 146-153. Verhoef, P., Stampfer, M.J. & Buring, J.E. (1996) Homocystein metabolism and risk of myocardial infarction: relation with vitamins B6, B12 and folate. Am. J. Epidemiol., 143, 845-859. Verhoef, P., Kok, F.J., Kruyssen, D.A., Schouten, E.G., Witteman, J.C., Grobbee, D.E., Ueland, P.M. & Refsum, H. (1997) Plasma total homocysteine, B vitamins, and risk of coronary atherosclerosis. Arterioscler. Thromb. Vasc. Biol., 17, 989-995. Verhoef, P. (2000) Hyperhomocysteinemia and risk of vascular disease in women. Semin. Thromb. Hemost., 26, 325-334. Vila, N., Deulofeu, R., Chamorro, A. & Piera, C. (1998) Plasma homocysteine levels in patients with ischemic cerebral infarction. Med. Clin. (Barc), 110, 605-608. Yilmaz, N., Yilmaz, M., Pence, S., Ozaslan, J., Kocoglu, H. & Yilmaz, G. (2001) Determination of serum B12 vitamin and folic acid levels in patient with stroke. Acta Medica, 44, 37-39.