ARVO 2015 Annual Meeting Abstracts
161 Optical properties and performance of natural and artificial
lenses
Sunday, May 03, 2015 3:15 PM–5:00 PM
Exhibit Hall Poster Session
Program #/Board # Range: 1062–1081/B0196–B0215
Organizing Section: Lens
Contributing Section(s): Biochemistry/Molecular Biology, Visual
Psychophysics/Physiological Optics
Program Number: 1062 Poster Board Number: B0196
Presentation Time: 3:15 PM–5:00 PM
Validation of the Mapcat for lens density measurements
Anirbaan Mukherjee, Richard A. Bone, Miguel A. Escanelle. Physics,
Florida International University, Miami, FL.
Purpose: To compare lens density measured by heterochromatic
flicker photometry under photopic conditions with that obtained
under scotopic conditions at absolute threshold.
Methods: The LED-based Mapcat flicker photometer, primarily
designed for measuring macular pigment optical density (MPOD),
was used to measure lens density or lens equivalent age (LEA). A 150
stimulus alternating between blue and green was viewed centrally
and subjects adjusted the blue intensity to minimize flicker in the
periphery. 25 subjects participated using their right eye only. We also
measured LEA in the same subjects by determining their absolute
thresholds when fully dark adapted. A 10 stimulus was positioned at
7.50 eccentricity from a fixation target. The stimulus was illuminated
by either a blue or green LED, similar to those used in Mapcat. It
was presented in the form of square wave pulses, 0.5 s on and 1.0 s
off. Subjects counted pulses during a 20 s period for incrementally
decreasing luminance. An inverse sigmoidal curve was fit to the
data to obtain the 50% threshold. By comparing the thresholds
with the corresponding rhodopsin absorbance, we calculated the
corresponding lens transmittances, which were converted to LEA
using a published model [Sagawa K & Takahashi Y JOSA 18, 2659
(2011)].
Results: Analysis of a plot of photopic LEA, P (yr), vs. scotopic
LEA, S (yr), yielded a regression line P = 0.942S + 0.23, (r2 = 0.66,
p < 0.0001). Although the slope was close to unity and the intercept
small, individual differences between pairs of measurements were
sometimes large.
Conclusions: Measurement of LEA under scotopic conditions
was found to be time consuming and imprecise. LEA measured by
Mapcat was fast and precise, and therefore much more practical. In
an attempt to reconcile differences between the results, where these
occurred, we examined the effect on the Mapcat results of varying
the long (L)- to medium (M)-wavelength cone ratio used in the
calculation of LEA. Using L:M ratios between reported extremes [
Sharpe et al. J. Vis. 5, 948 (2005)], we were still not able to explain
all the differences. Other factors such as eye movements causing
poor fixation in the scotopic test might be responsible. Nonetheless,
on average, the scotopic results validated the use of the Mapcat as a
valuable instrument for LEA as well as MPOD measurement.
Commercial Relationships: Anirbaan Mukherjee, None; Richard
A. Bone, None; Miguel A. Escanelle, None
Program Number: 1063 Poster Board Number: B0197
Presentation Time: 3:15 PM–5:00 PM
Characterization of Mechanical Properties of Murine Lenses for
Biomolecular Insights into Presbyopia
Luis Rodriguez, Matthew A. Reilly. University of Texas at San
Antonio, San Antonio, TX.
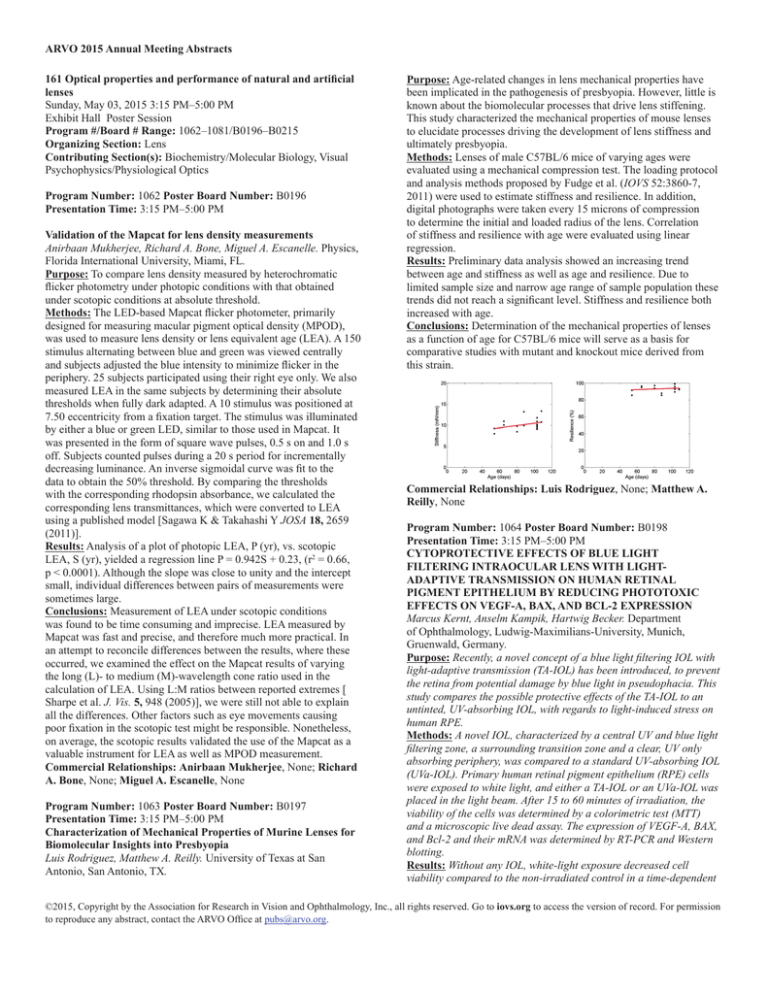
Purpose: Age-related changes in lens mechanical properties have
been implicated in the pathogenesis of presbyopia. However, little is
known about the biomolecular processes that drive lens stiffening.
This study characterized the mechanical properties of mouse lenses
to elucidate processes driving the development of lens stiffness and
ultimately presbyopia.
Methods: Lenses of male C57BL/6 mice of varying ages were
evaluated using a mechanical compression test. The loading protocol
and analysis methods proposed by Fudge et al. (IOVS 52:3860-7,
2011) were used to estimate stiffness and resilience. In addition,
digital photographs were taken every 15 microns of compression
to determine the initial and loaded radius of the lens. Correlation
of stiffness and resilience with age were evaluated using linear
regression.
Results: Preliminary data analysis showed an increasing trend
between age and stiffness as well as age and resilience. Due to
limited sample size and narrow age range of sample population these
trends did not reach a significant level. Stiffness and resilience both
increased with age.
Conclusions: Determination of the mechanical properties of lenses
as a function of age for C57BL/6 mice will serve as a basis for
comparative studies with mutant and knockout mice derived from
this strain.
Commercial Relationships: Luis Rodriguez, None; Matthew A.
Reilly, None
Program Number: 1064 Poster Board Number: B0198
Presentation Time: 3:15 PM–5:00 PM
CYTOPROTECTIVE EFFECTS OF BLUE LIGHT
FILTERING INTRAOCULAR LENS WITH LIGHTADAPTIVE TRANSMISSION ON HUMAN RETINAL
PIGMENT EPITHELIUM BY REDUCING PHOTOTOXIC
EFFECTS ON VEGF-A, BAX, AND BCL-2 EXPRESSION
Marcus Kernt, Anselm Kampik, Hartwig Becker. Department
of Ophthalmology, Ludwig-Maximilians-University, Munich,
Gruenwald, Germany.
Purpose: Recently, a novel concept of a blue light filtering IOL with
light-adaptive transmission (TA-IOL) has been introduced, to prevent
the retina from potential damage by blue light in pseudophacia. This
study compares the possible protective effects of the TA-IOL to an
untinted, UV-absorbing IOL, with regards to light-induced stress on
human RPE.
Methods: A novel IOL, characterized by a central UV and blue light
filtering zone, a surrounding transition zone and a clear, UV only
absorbing periphery, was compared to a standard UV-absorbing IOL
(UVa-IOL). Primary human retinal pigment epithelium (RPE) cells
were exposed to white light, and either a TA-IOL or an UVa-IOL was
placed in the light beam. After 15 to 60 minutes of irradiation, the
viability of the cells was determined by a colorimetric test (MTT)
and a microscopic live dead assay. The expression of VEGF-A, BAX,
and Bcl-2 and their mRNA was determined by RT-PCR and Western
blotting.
Results: Without any IOL, white-light exposure decreased cell
viability compared to the non-irradiated control in a time-dependent
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
manner. The UV- and blue-light filtering of the TA-IOL attenuated
light-induced cell damage significantly more than the UVa-IOL.
RT-PCR and Western blotting yielded a significant, time-dependent
decrease of Bcl-2 and increase of BAX and VEGF-A. This decrease
of Bcl-2 and increase of BAX and VEGF-A was significantly less with
the TA-IOL than with the UVa-IOL.
Conclusions: Both TA-IOL and UV- and UVa-IOL reduce lightinduced RPE-damage. The TA-IOL reduced damage more than the
conventional IOL. The presented concept of a TA-IOL may help to
protect the retina against light-induced damage and reduce potential
negative influences of blue light filtering IOLs on the quality of vision
under low light conditions.
Commercial Relationships: Marcus Kernt, None; Anselm
Kampik, None; Hartwig Becker, None
Program Number: 1065 Poster Board Number: B0199
Presentation Time: 3:15 PM–5:00 PM
Optics of light scattering in the human eye lens
Thomas J. Van Den Berg. 1Straylight Lab, Netherlands Inst for
Neurosci, Royal Acad, Amsterdam, Netherlands; 2Rotterdam
Ophthalmic Institute, Rotterdam, Netherlands.
Purpose: The visual phenomenon of radiation of light around a
bright light source (“ciliary corona”, glare, straylight) is known
as result of forward light scattering in the eye. The scattered light
corresponds to the peripheral part of the ocular point-spread-function.
The slitlamp image (or Scheimpflug image) of the human eye lens,
results from backward light scattering. Light scattering can be
predicted from the characteristics of scattering elements. Reversely
from scattering characteristics predictions for the scattering elements
can be derived. Optical bench study of human eye lenses will be
presented to (1) detail the light scattering characteristics, (2) the (lack
of) relationship between forward and backward scattering, and (3) the
comparison to the known in vivo psf including age effects.
Methods: Data on 15 human eye lenses, isolated from donor eyes,
from an earlier study, with LOCSIII values ranging from NO=1 to 5,
with median 2.3 are used. The angular and wavelength characteristics
are compared to light scattering theory, in particular the strong blue
dominant Rayleigh pattern, with 1/λ4 dependence, valid for small
particles (molecules), and the general Mie theory.
Results: Scatter plots testing Rayleigh behaviour for different
angles show that small particles dominate light scattering for angles
larger than 30 degrees, including backward directions. Surprisingly,
this holds for all lenses, including advanced cataractous states. At
backward directions appraoching 180 degrees, light sctattering
intensifies, indicative for the process of rough surface reflection.
At forward directions, as relevant for the psf, light scattering has
essentially different characteristics, typical for particles with sizes of
the order of wavelength. This scattering corresponds very closely to
what is known for the peripheral part of the in vivo psf according the
CIE standard functions (CIE Collection 1999;135/1:1-9).
Conclusions: Different processes govern forward and backward
scatter in the human eye lens. Correspondingly forward and backward
scatter are not strongly related, explaining why the slit image is not
an accurate predictor of forward scatter or straylight. Forward light
scatter characteristics correspond very closely to the periphery of
the in vivo psf, indicating that particles of about wavelength size are
responsible for in vivo light scattering, irrespective of cataractous
status.
Commercial Relationships: Thomas J. Van Den Berg, None
Program Number: 1066 Poster Board Number: B0200
Presentation Time: 3:15 PM–5:00 PM
Physical Model of Intraocular Scattering using a Spatial Light
Modulator
Augusto Arias Gallego2, 1, Harilaos S. Ginis1, Pablo Artal1.
1
Laboratorio de Optica, Universidad de Murcia, Murcia, Spain;
2
Institute of Vision and Optics, University of Crete, Heraklion,
Greece.
Purpose: Intraocular scattering affects the retinal image and
quality of vision. It is produced by the interaction of light with local
variations of the refractive index and its angular distribution depends
on the spatial characteristics of the scatterers. A better understanding
of the physical basis of scattering in the eye would help with possible
compensation methods. In this context, we developed a realistic
physical model to reproduce the light scattering occurring in the eye.
Methods: Theoretical analysis identified the spatial characteristics of
the required phase to reproduce intraocular scattering, represented by
the wide-angle point-spread function (PSF). Sampling of the phase
at the pupil plane should be comparable to the size of the features
that scatter light within the eye. The experimental setup used a liquid
crystal on silicon spatial light modulator (SLM) (PLUTO, Holoeye,
Germany) to generate the phase patterns. The SLM plane was
conjugated with magnification of about 0.17 with the eye’s pupil. The
induced scattering was evaluated in single pass by using the optical
integration method (Ginis et al., J Vis, 2012) and compared with
typical scatter occurring in normal eyes as given by the CIE wideangle PSFs. The physical characteristics of the SLM (8 μm pixel
size), in combination with the particular magnification and diffraction
effects limit the angular range for the generation of the PSF up to 4
degrees.
Results: The experimentally induced straylight for different phase
map was in good agreement with the theoretical predictions. Contrast
reduction in extended images associated to light scattering was
documented for demonstration purposes. The straylight parameter
(S) of the experimentally induced scatter was associated to the RMS
amplitude (h) of the phase map by the following formula: log(S) =
0.9748*log(h) + 1.826. This permits to reproduce intraocular scatter
conditions ranging from normal clear eyes to early cataract.
Conclusions: An accurate physical model of scatter was developed
using a spatial light modulator and appropriate phase distributions.
The instrument is suitable for the generation of light scattering
similar to that found in human eyes. This is not only is a useful tool
for psychophysical experiments but also documents the physical
requirements for possible compensation of light scattering in the eye.
Commercial Relationships: Augusto Arias Gallego, None;
Harilaos S. Ginis, None; Pablo Artal, None
Support: OpAL–264605 Marie Curie Initial Training Network (ITN)
Program Number: 1067 Poster Board Number: B0201
Presentation Time: 3:15 PM–5:00 PM
Quantitative analysis of Visual Acuity and Threshold Contrast
for induced scattering levels
Clemente Paz Filgueira1, 2, Elisa Colombo1, 2, Luis Issolio1, 2. 1Instituto
de Investigación en Luz, Ambiente y Visión (ILAV), Consejo
Nacional de Investigaciones Científicas y Técnicas (CONICET), San
Miguel de Tucumán, Argentina; 2Departamento de Luminotecnia, Luz
y Visión (DDLLyV), Universidad Nacional de Tucumán (UNT), San
Miguel de Tucumán, Argentina.
Purpose: To study how visual acuity and contrast threshold are
affected by different levels of scattering, considering the influence
of glare. To analyze the relationship between the straylight
parameter and contrast threshold.
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Methods: In this work we performed measurements of
corrected visual acuity (CVA), contrast threshold (Ct) based
on a computerized system for visual function measurements
(FVC100) and the straylight parameter (S) by means of CQuant.
We covered a wide range of scattering through six experiment
conditions: one free scattering condition and other 5 scattering
conditions using single diffuser filters and combination of them.
Measurements of CVA, S, Ct without glare and Ct with glare
were performed for all 6 conditions. Ct was measured for spatial
frequencies 1, 2, 4, 8 and 12 cycles per degree, mean luminance
of targets was 70cd/m2 and glare illuminance was set on 80lux.
All measurements were replicated in three subjects with CVA=1
without filters.
Results: Each Ct value is the average of three measurements. No
scattering level caused significant drops in CVA, while they did
caused the Ct to increase. We encountered that the best fitting
between S and Ct was exponential (R2 higher than 0.90 for all
spatial frequencies). We utilized the ratio between Ct with glare
and Ct without glare as an indicator of the effect of glare and
we found that the relationships between this ratio and S were
lineal with positive slopes which increased according to spatial
frequency increasing.
Conclusions: It is possible to reach normal VA under very
elevated scattering conditions (equivalents to higher level of
cataract development), in contrast with Ct which is, in fact,
sensitive to changes in scattering levels. Correlations between
Ct and S were high for all spatial frequencies, evidencing the
FVC100 ability to detect changes in scattering levels. The more
the scattering level and spatial frequency are, they cause more
influence in glare measurements
Commercial Relationships: Clemente Paz Filgueira, None;
Elisa Colombo, AR027169B1 (P); Luis Issolio, Tecnovinc S.R.L. /
AR027169B1 (P)
Support: PIP 0553 (CONICET) CIUNT 26/E519 (UNT), PICT 1807
(ANPCyT)
Program Number: 1068 Poster Board Number: B0202
Presentation Time: 3:15 PM–5:00 PM
Effects of intraocular lens opacification versus subsurface
nanoglistenings on light scatter and overall optical quality/
performance
Liliana Werner1, John Stover2, Jim Schwiegerling3, Kamal K. Das4.
1
John A. Moran Eye Center, University of Utah, Salt Lake City, UT;
2
The Scatter Works, Inc., Tucson, AZ; 3College of Optical Sciences,
University of Arizona, Tucson, AZ; 4Alcon Laboratories, Inc., Fort
Worth, TX.
Purpose: Calcification and snowflake degeneration are causes
of postoperative opacification of hydrophilic acrylic/silicone and
polymethylmethacrylate (PMMA) intraocular lenses (IOLs),
respectively, causing significant forward light scattering and
generally require IOL explantation. Light scattering of hydrophobic
acrylic lenses is due to subsurface nanoglistenings (SSNG), generally
not leading to explantation. We test the hypothesis that the effect
of calcification and snowflake degeneration on stray light and other
optical quality indicators is a different phenomenon and more
significant than that of SSNG.
Methods: 14 IOLs were explanted from living eyes due to
calcification (13 hydrophilic acrylic, 1 silicone), 4 PMMA IOLs
were explanted because of snowflake degeneration. 17 singlepiece AcrySof (Alcon) IOLs were removed from cadaver eyes
exhibiting SSNG (11 with a blue light filter – BLF – and 6 without).
The forward scattering of IOLs, including new IOL controls was
measured using a Complete Angle Scatter Instrument; stray light
values at various angles were calculated. The Modulation Transfer
Function (MTF) was obtained with an optical bench; a Badal
optometer was used to capture letter chart images through the lenses.
Results: Average stray light values (Log (s)) at a scattered angle
of 10 degrees were measured as 1.629 +/- 0.465 for PMMA IOLs
(control PMMA = 0.258), 1.791 +/- 0.370 for hydrophilic acrylic
IOLs (control hydrophilic acrylic = 1.335), and 1.539 for the
silicone lens (control 0.418). The values for the AcrySof IOLs were
1.036 +/- 0.270 for BLF lenses, and 0.975 +/- 0.264 for non BLF
lenses (controls 0.223 +/- 0.229). MTF and Badal image contrast
were drastically reduced in lenses with calcification and snowflake
degeneration, but were similar to controls (no SSNG) in AcrySof
lenses.
Conclusions: Studies from van den Berg et. al. find the impact of
stray light in human vision, with serious hindrance above 1.47 (Log
(s)). Stray light in hydrophobic IOLs due to SSNG is well below the
value of stray light hindrance of 1.47 (no lens with a value ≥ 1.47),
which would not cause noticeable visual impairments. Based on our
results stray light due to calcification and snowflake degeneration
reduced MTF and image contrast and stray light due to SSNG did
not.
Commercial Relationships: Liliana Werner, Alcon Laboratories
(F); John Stover, Alcon Laboratories (C); Jim Schwiegerling, Alcon
Laboratories (F); Kamal K. Das, Alcon Laboratories (E)
Program Number: 1069 Poster Board Number: B0203
Presentation Time: 3:15 PM–5:00 PM
Intraocular scattering shows low heritability
Antonio Benito1, Lucia Hervella1, Juan Tabernero1, Alexandros
Pennos1, Harilaos S. Ginis1, Juan Francisco Sánchez-Romera2, Juan
Ramón Ordoñana2, Marcos Ruiz-Sánchez3, Jose María Marín3, Pablo
Artal1. 1Laboratorio de Óptica, Universidad de Murcia, Murcia,
Spain; 2Murcia Twin Registry, Area of Psychobiology, Universidad
de Murcia, Murcia, Spain; 3Servicio de Oftalmología, Hospital
Universitario Arrixaca, Murcia, Spain.
Purpose: To study the relative impact of genetic factors in the
differences of intraocular scattering and straylight in a classical twins
study.
Methods: A group of 53 twins were included in the study: 24
monozygotic (MZ) (mean age: 52.4±5.5 y/o) and 29 dizygotic (DZ)
(mean age: 54.7±6.8 y/o). A complete ophthalmological exam was
performed for all subjects, excluding all those with ocular pathologies
that were known to increase intraocular scatter. Subjects with
suspected cataracts were excluded, using as exclusion criteria having
a Lens Opacities Classification System-III (LOCS-III) value for
nuclear, cortical or subcapsular cataract above grade II. Both eyes in
each subject were measured using three different and complementary
techniques to evaluate intraocular scattering. A Hartmann-Shack
wavefront sensor (AOnEye; Voptica SL, Murcia, Spain) provided
a low-angle scatter parameter (less than 0.5 degrees), similar to the
Objective Scattering Index (OSI) (Artal et al. PLoS One, 2011).
A compact optical instrument based in the principle of optical
integration (Sigma, Sinusmedii SL, Spain) allowed the estimation
of a straylight parameter (SS) for a retinal angle of 5.5 degrees.
Additional psychophysical measurements of straylight (SC) were
also performed (c-Quant, Oculus GmbH, Germany). Due to high
correlation between both eyes data from one single eye per subject
was randomly selected. Intraclass Correlation Coefficients (ICC)
were used as a descriptive statistics of twin resemblance and genetic
models were fitted to estimate heritability.
Results: On average, ICCs between siblings were similar for the
three measured scatter parameters. ICC values for OSI were 0.738 in
MZ and 0.530 in DZ twins; for SS were 0.623 in MZ twins and 0.869
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
in DZ twins, and for SCwere 0.741 in MZ and 0.664 in DZ twins.
The estimates of heritability were low (0.3) for all the measured
scattering parameters.
Conclusions: Correlations of the estimation of intraocular scatter
and straylight in the groups of identical and non-identical twins were
similar. Heritability estimates were of limited magnitude. These
results suggest that environmental and individual factors are probably
dominant to determine the level of straylight in healthy eyes of
middle-aged adults.
Commercial Relationships: Antonio Benito, None; Lucia
Hervella, None; Juan Tabernero, None; Alexandros Pennos, None;
Harilaos S. Ginis, None; Juan Francisco Sánchez-Romera, None;
Juan Ramón Ordoñana, None; Marcos Ruiz-Sánchez, None; Jose
María Marín, None; Pablo Artal, None
Support: European Research Council Advanced Grant ERC-2013AdG-339228 (SEECAT) & SEIDI, Spain (grant FIS2013-41237-R).
Program Number: 1070 Poster Board Number: B0204
Presentation Time: 3:15 PM–5:00 PM
Effect of forward light scattering on visual function in eyes with
cortical cataract
Hiroshi Sasaki1, 2, Eri Shibuya1, 3, Mai Takahashi1, 3, Ayako Okamoto1,
3
, Norihiro Mita1, 3, Natsuko Hatsusaka1, Shinsuke Shibata1,
Teppei Shibata1, Kazuyuki Sasaki1, 2, Eri Kubo1. 1Department of
Ophthalmology, Kanazawa Medical University, Kahoku, Japan;
2
Division of Vision Research for Environmental Health, Kanazawa
Medical University, Kahoku, Japan; 3Medical Technology Division,
Kanazawa Medical University, Kahoku, Japan.
Purpose: We examined correlations between forward light scattering
(FLS) and visual function in cortical cataract (COR) and transparent
(TP) eyes.
Methods: Of subjects in 2013 Monzen Eye Study and Kanazawa
Medical University Hospital cataract surgery patients from July 2013
to March 2014, 39 COR eyes of 35 subjects (66.5±6.0 yrs) were
compared with 42 TP eyes of 42 subjects (57.2±8.7 yrs) as control.
Cases with ocular disease except for refractive error were excluded.
COR was examined under maximal mydriasis by the same examiner,
graded in 4 stages (Grade 0 to 3) according to WHO classification
system, and categorized CEN+/- by opacity within/outside the central
3 mm diameter of the pupil. Opacity within this 3 mm diameter
area was measured with transillumination imaging by anterior eye
segment analysis system EAS-1000 (NIDEK). FLS was measured by
C-Quant (OCULUS®) and stray light correction level (Log(s)) was
calculated. Total higher-order aberration (HOA) in the 4 mm pupil
diameter, retinal image contrast (RIC) in the 3 mm entrance pupil,
and 25% day and evening vision contrast visual acuity (CVA) were
measured by KR-9000PW (TOPCON), PSF-1000 (TOPCON), and
CAT-2000 (NEITZ), respectively.
Results: FLS was higher in COR (1.38±0.25) than in TP (1.13±0.22)
(p<0.001). There was no significant correlation between FLS
and age in COR or TP. FLS in COR increased with grade. CEN+
(1.45±0.20) had higher FLS than CEN- (1.26±0.30) (p<0.05) with
CEN+ grade 1 (1.36±0.25), 2 (1.43±0.13), and 3 (1.51±0.24). There
was a positive correlation between area of opacity of CEN+ and
FLS (p<0.05). CEN- with COR grade 2 (1.37±0.32) had higher FLS
than TP (p<0.05). In TP eyes, FLS was significantly correlated with
decreased best corrected visual acuity (p<0.01), increased total ocular
HOA (p<0.01) and total intraocular HOA (p<0.05), but not in COR
eyes. There was no correlation between FLS and CVA in TP or COR,
however, RIC in COR showed a negative correlation with FLS in low
and intermediate frequency domains (p<0.05).
Conclusions: FLS in TP at age 40s-60s was little affected by aging.
In COR, FLS increased with severity of opacity and opacity in the
pupillary area, decreasing RIC. It was suggested that higher FLS is a
major factor in decreased visual function.
Commercial Relationships: Hiroshi Sasaki, None; Eri Shibuya,
None; Mai Takahashi, None; Ayako Okamoto, None; Norihiro
Mita, None; Natsuko Hatsusaka, None; Shinsuke Shibata, None;
Teppei Shibata, None; Kazuyuki Sasaki, None; Eri Kubo, None
Program Number: 1071 Poster Board Number: B0205
Presentation Time: 3:15 PM–5:00 PM
Experimental analysis of light scatterings in intraocular lenses
Masamoto Aose, Hiroyuki Matsushima, Kouichiro Mukai, Mayumi
Nagata, Norihito Gotoh, Tadashi Senoo. ophthalmology, Dokkyo
Medical University, Tochigi, Japan.
Purpose: Recently, phase separations of acrylic materials (glistening
and whitening (sub-surface nano glistenigs)) sometimes picked up as
complications after cataract surgeries. The glistening and whitening
increase light scattering. In this study, light scatterings of intraocular
lenses (IOLs) were evaluated using rabbit eyes.
Methods: Eyes of 8 weeks albino rabbits weighting 2 kg had
phacoemulsification in 2.4mm corneal insertion, after that, six types
of hydrophobic acrylic IOLs (SN60WF before changing of IOL
production process by Alcon (J group), SN60WF after changing of
IOL production process by Alcon (Q group), ZCB00 AMO (Z group),
AN6K Kowa (A group), NX-60 Santen (N group) and SP2 HOYA
(S group)) were implanted. After 6 months post operation, the IOLs
were extracted and cleaned to remove attachment proteins. The IOLs
were placed in our model eye maintaining a constant temperature.
The surface and inner light scatterings of the IOLs were imaged and
analyzed with an anterior segment analyzer (EAS-1000, NIDEK).
The intensity of light scattering was quantified in a selected area of
surface or inner of IOL using densitometry. To measure the increasing
rate of the light scatterings, these unused IOLs were also quantified.
Results: The surface light scattering in J group was 22.0 ± 8.5 CCT,
that in Q group was 21.5 ± 5.7 CCT, that in Z group was 10.3 ± 2.9
CCT, that in A group was 9.7 ± 3.4 CCT, that in N group was 22.7
± 4.8 CCT, and that in S group was 4.0 ± 4.4 CCT. The increasing
rate of the surface light scattering in J group was 3.8 ± 1.5, that in Q
group was 3.3 ± 0.9, that in Z group was 2.2 ± 0.6, that in A group
was 1.9 ± 0.7, that in N group was 1.7 ± 0.4, and that in S group was
1.2 ± 0.7. The increasing rate of the surface light scattering in J and Q
groups was significantly higher than that in other groups (P<.05).
Conclusions: The light scatterings of hydrophobic acrylic IOLs were
increased; however, the increasing rates of them were different.
Commercial Relationships: Masamoto Aose, None; Hiroyuki
Matsushima, None; Kouichiro Mukai, None; Mayumi Nagata,
None; Norihito Gotoh, None; Tadashi Senoo, None
Program Number: 1072 Poster Board Number: B0206
Presentation Time: 3:15 PM–5:00 PM
Higher-order aberrations of intraocular lens with intrascleral
fixation
Makoto Inoue, Naoko Matsuki, Yuji Itoh, Toshiyuki Nagamoto, Akito
Hirakata. Ophthalmology, Kyorin Eye Center, Mitaka, Japan.
Purpose: To determine the higher-order aberrations (HOAs) of
intraocular lenses (IOLs) with an intrascleral fixation technique.
Methods: A computer-aided design system was used to calculate the
length of an IOL when it was fixed in the sclera 2 mm posterior to the
limbus in a Gullstrand eye model. An acrylic single-piece (SA60AT;
Alcon) or 2 three-piece IOLs (VA-60BBR; HOYA, X-60; Santen)
was fixed at a length of 13, 14, 15, and 16 mm length. A wavefront
analyzer (LAMBDA-X) was used to measure the HOAs within the
central 3.0 or 5.2 mm optic diameter.
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Results: The length of the IOL with the intrascleral fixation was
calculated to be 13.9 to 14.9 mm in the eye model. The astigmatic
aberration of the 3-piece VA-60BBR and X-60 IOLs within the
central 5.2 mm was significantly greater with an extension of the
IOLs (both P<0.001) but not that of the single-piece SA60AT IOL.
The coma aberration of the VA-60BBR IOL within the central 5.2
mm increased significantly with an increase in the extension (P
=0.001) but not that of the SA60AT and X-60 IOLs. The astigmatic
and coma aberrations within the central 5.2 mm were significantly
greater than that within the central 3.0 mm for all IOLs. The
cylindrical power increased up to 0.034 to 0.082 D with extensions
from 13 to 16 mm.
Conclusions: When three-piece IOLs are greatly extended for
intrascleral fixation, the astigmatic and coma aberrations increase but
the range of changes is not clinically relevant to patients.
Commercial Relationships: Makoto Inoue, Alcon (R), Byer (R),
HOYA (R), Novartis (R), Santen (R), Sanwakagaku (R), Senjyu (R),
Wakamoto (R); Naoko Matsuki, None; Yuji Itoh, None; Toshiyuki
Nagamoto, Alcon (R), HOYA (R); Akito Hirakata, Alcon (R), Byer
(R), Kowa (R), Novartis (R), Santen (R), Senjyu (R)
Program Number: 1073 Poster Board Number: B0207
Presentation Time: 3:15 PM–5:00 PM
Forward Light Scatter, Stray Light and Image Quality in
Intraocular Lenses at Various Light Scattering Angles
Kamal K. Das1, Liliana Werner2, John Stover3, Jim Schwiegerling4.
1
IOL R&D, Alcon Laboratories, Inc, Fort Worth, TX; 2John A. Moran
Eye Center, University of Utah, Salt Lake City, TX; 3The Scatter
Works, Inc., Tucson, AZ; 4College of Optical Sciences, University of
Arizona, Tucson, AZ.
Purpose: Stray light due to significant forward light scattering
(FLS) may cause visual impairment. This study evaluates FLS and
compares stray light values of new and artificially aged intraocular
lenses (IOLs) at light scattering angles of 10, 15, 20, 25 and 30
degrees. Optical quality performance of the IOLs is evaluated based
on Modulation Transfer Function (MTF) and letter chart images
using a Badal optometer.
Methods: FLS of the new and artificially aged AcrySof IOLs was
measured with the Complete Angle Scattering Instrument (CASI).
The stray light values of these lenses were obtained from the
measured FLS data at light scattering angles of 10, 15, 20, 25 and 30
degrees. New AcrySof IQ SN60WF lenses with IOL powers of 15,
21, 23 and 24 Diopters (D) were used to obtain stray light values.
AcrySof SN60AT and AcrySof IQ SN60WF lenses were aged in a
laboratory for periods equivalent up to accelerated 10 years. The
same technique was used to measure FLS and compare stray light
values for the aged IOLs. The MTF and image acquisition test
systems incorporate a custom eye model with a wet cell for mounting
the IOL. Pupil sizes of 3 and 6 mm were used.
Results: The average stray light values of the SN60AT (N=2) was
0.257+/0.260 and 0.249+/0.306 for SN60WF (N=4) at a scattering
angle of 10 degrees. The stray light values decreased at higher
scattering angles of 15 to 30 degrees for both groups of lenses. The
decrease of stray light was faster for SN60WF compared to SN60AT
at all angles. The average stray light values for the SN60AT was
-0.174+/0.310 and -0.517+/0.072 for SN60WF at a scattering angle
of 30 degrees. The stray light values for the IOL powers of 15, 21, 23
and 24 D indicated a linear trend with the exception of one value for
the 24D at 10 degrees. Stray light values for 10 years aged SN60WF
was lower compared to 10 years aged SN60AT at the tested light
scattering angles. The MTF values and Badal bench did not degrade
for the laboratory aged IOLs compared to a new IOL.
Conclusions: The forward light scatter and stray light values of
all tested IOLs at various light scattering angles were well below
the stray light hindrance value of 1.47 and thus would not have a
meaningful impact on the visual function. The optical performances
of these lenses do not show any impact on the optical quality both at
smaller and larger pupils.
Commercial Relationships: Kamal K. Das, Alcon Laboratories,
Inc (E); Liliana Werner, Alcon Laboratories, Inc (C); John Stover,
Alcon Laboratories, Inc (C); Jim Schwiegerling, Alcon Laboratories,
Inc (C)
Program Number: 1074 Poster Board Number: B0208
Presentation Time: 3:15 PM–5:00 PM
A study of the long-term transparency of new Acrysof®
intraocular lenses
Kenji Kawai. Ophthalmology, Tokai Univ School of Medicine,
Isehara, Japan.
Purpose: In this study, used the Acrysof® SN60WF, which were
manufactured recently to devise a way for eliminating sub-surface
nano glistenings (SSNGs), to predict the changes in deterioration
after 20 years. We observed the appearance, measured the weight,
optic diameter and light transmittance of the lenses, and analyzed
the preservative solution of the IOLs with gas chromatography-mass
spectrometry (GC-MS)
Methods: Forty five Acrysof® SN60WF IOLs were used. Each IOL
was immersed in ultrapure water placed in a 9-mL screw-top vial at
100C for 115 days on the assumption that storage in an oven at 100C
for 23 days is equivalent to 4 years at 37C. After 115 days which is
corresponding to a period of 20 years, the appearance of the lens was
observed with a stereoscopic microscope, and then the change in
weight, optic diameter and light transmittance were measured. The
preservative solution was analyzed with GC-MS.
Results: Appearance: Glistening was observed in all of the 45 lenses.
Assumed changes to indicate deterioration such as cracks on the lens
and discoloration of the optic were observed in 11 lenses (24%).
Rate of change in lens weight: The weight of the lens decreased
significantly. After drying, the average rate of change in lens weight
was -2.45%.
Rate of change in optic diameter: The optic diameter decreased
significantly. After drying, the average rate of change in optic
diameter was -0.84%.
Rate of change in light transmittance: Deterioration was observed
in 11 lenses. At 500 nm, the light transmittance in the 10 lenses
decreased about 1% to 7%, and in one lens decreased about 36%.
Preservative solution: The peaks of phenylethyl alcohol, or a
hydrolysate[A1], were observed in 9 of 11 lenses.
Conclusions: In a 20-year severe accelerated deterioration test,
although opacification was observed in appearance of all the SA60AT
and SN60AT lenses (20 of 20 lenses, 100%) after drying, the speed of
deterioration may have been slowed because SN60WF lenses showed
fewer changes of deterioration (11 of 45 lenses, 24%) compared
to SA60AT and SN60AT, and the deterioration had little impact
on the light transmittance of the lenses. However, the weight and
optic diameter of the lenses decreased significantly. The phenylethyl
alcohol leaked into the preservative solution. These results indicate
that the lenses had deteriorated. It is assumed that the deterioration
was due to the cast molding method for manufacturing the lenses.
Commercial Relationships: Kenji Kawai, None
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Program Number: 1075 Poster Board Number: B0209
Presentation Time: 3:15 PM–5:00 PM
Combined Laser Ray Tracing and Optical Coherence
Tomography system to measure changes in lens shape and onaxis and off-axis focal length with accommodation
Bianca Maceo Heilman1, 2, Marco Ruggeri1, Alex Gonzalez1, Cornelis
J. Rowaan1, Andres Bernal3, Esdras Arrieta1, Arthur Ho4, Fabrice
Manns1, 2, Jean-Marie A. Parel1, 5. 1Ophthalmic Biophysics Center,
Bascom Palmer Eye Institute, Miami, FL; 2Biomedical Optics and
Laser Laboratory, Department of Biomedical Engineering, College
of Engineering, University of Miami, Coral Gables, FL; 3Bioniko
Consulting LLC, Sunny Isles Beach, FL; 4Brien Holden Vision
Institute, Sydney, NSW, Australia; 5Vision Cooperative Research
Centre, Brien Holden Vision Institute, University of New South
Wales, Sydney, NSW, Australia.
Purpose: To measure the changes in lens shape, focal length and
aberrations in ex vivo primate lenses on and off-axis during simulated
accommodation.
Methods: Instrumentation: A combined LRT-OCT system was
designed and built using a commercial Spectral-Domain OCT system
with 16mm depth range and 8mm axial resolution in air (Bioptigen
ENVISU R4400). The LRT uses the OCT scanning beam delivery
system to deliver input rays to the lens. The beam delivery optics are
mounted on a motorized rotation stage that pivots around the lens to
allow acquisition of off-axis spot patterns. An imaging sensor was
mounted on a two-dimensional (horizontal and vertical) motorized
positioning stage below the lens to record the spot positions along
each individual ray both on-axis and off-axis. Spot positions are used
to reconstruct the ray path and calculate lens power and aberrations.
The tissue is mounted in a manual lens stretcher (Bioniko LLC)
that we motorized to measure the lens in the unaccommodated and
accommodated states. The entire system is controlled via LabView
software to allow automated data acquisition.
Measurements: LRT-OCT experiments were performed on 2
cynomolgus monkey lenses from 1 donor (4 years, PMT= 2, 26
hrs) in the unstretched and stretched state. The LRT delivered 51
equally-spaced parallel meridional rays over a 6-mm diameter zone.
Experiments were performed at incidence angles from -20° to +20°
in 5° increments. Spot positions were recorded at 12 vertical heights
along the optical axis. The on and off-axis focal length was calculated
from the ray slopes.
Results: The system can acquire OCT images of the entire lens and
focal length measurements at each angle. The on-axis focal length is
(OD, OS): 30.2mm, 29.4mm in the unstretched state and 35.5mm,
29.6mm in the stretched state, corresponding to a power of 37.6D,
45.1D, and 44.2D, 45.4D, respectively. The off-axis focal lengths are
shown in Figure 2.
Conclusions: The system is able to measure the off-axis ray-trace of
the crystalline lens. The focal length of cynomolgus monkey lenses
was found to decrease with increasing incidence angle.
(Left) Combined LRT-OCT system. The lens stretcher and tissue cell
not shown. (Right) Lens stretcher, tissue cell and control unit.
Change in lens focal length versus incidence angle for (Left) OD and
(Right) OS in the unstretched and stretched states.
Commercial Relationships: Bianca Maceo Heilman, None; Marco
Ruggeri, None; Alex Gonzalez, None; Cornelis J. Rowaan, None;
Andres Bernal, Bioniko Consulting LLC (E); Esdras Arrieta,
None; Arthur Ho, None; Fabrice Manns, None; Jean-Marie A.
Parel, None
Support: NIH Grants R01EY021834, F31EY021444 (NRSA
Individual Predoctoral Fellowship [BM]), and Center Grant
P30EY14801; Australian Government CRC Scheme (Vision CRC);
Florida Lions Eye Bank; an unrestricted grant from Research to
Prevent Blindness; Henri and Flore Lesieur Foundation (JMP).
Program Number: 1076 Poster Board Number: B0210
Presentation Time: 3:15 PM–5:00 PM
Understanding visual complaints of two intraocular lens explant
cases
Marrie Van der Mooren1, Roger F. Steinert2, Farrell Tyson3, Robert
Rosen1, Linda Lundstrom4, Patricia A. Piers1. 1Applied Research,
AMO Groningen BV, Groningen, Netherlands; 2Gavin Herbert Eye
Institute,University of California, Irvine, CA; 3Cape Coral Eye center,
Cape Coral, FL; 4KTH Royal Institute of Technology, Stockholm,
Sweden.
Purpose: In two different cases, multifocal intraocular lenses
(MFIOLs) were explanted due to visual complications related to the
presence of micro-vacuoles in the optic body. These micro-vacuoles
cause straylight, which resulted in complaints of hazy and blurry
vision. The purpose of this study is to objectively measure and
systematically quantify the visual impact of this straylight. The study
will thereby give a better understanding of the origin of reported
visual complaints when micro-vacuoles are present.
Methods: The amount of straylight in the two explanted MFIOLs
was measured using an in-vitro setup and quantified using the
scattering parameter s. To determine the impact of straylight on
vision, photographic filters characterized in the same in-vitro setup
were used to induce straylight on five subjects. Four different
psychophysical visual tests were used: halo size, luminance detection
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
with a glare source, and contrast sensitivity (CS) with and without the
presence of glare. For all tests, the impact was modeled as a linear
interpolation of the logarithm of the test score against the logarithm
of the scattering parameter, log(s).
Results: The straylight measured by the in-vitro setup was 6 deg2/sr
for case 1 and 4 deg2/sr for case 2. Assuming a base straylight level
of 1.1 log(s), the induced increase for the two patients was 0.17 log(s)
and 0.12 log(s) respectively.
The impact for the visual tests per unit of log(s) was the following:
for halo size, 0.55 log(degrees)/log(s); for luminance detection 2.72
log(cd/m2)/log(s); for CS without glare, 0.33 log(CS)/log(s); and for
CS with glare, 0.58 log(CS)/log(s). The induced straylight for the two
explanted MFIOLs therefore corresponds to an increase of halo size
of 24% and 16%, a luminance detection threshold increase of 190%
and 112%, a contrast sensitivity decrease of 12% and 9% without a
glare source, and a contrast sensitivity decrease of 20% and 9% with
a glare source.
Conclusions: In the explanted MFIOLs we could objectively
measure straylight. This straylight corresponds psychophysically
to increases in halo size, loss of luminance sensitivity and decrease
in contrast sensitivity. Among the visual tests, measurement of
luminance detection showed the highest sensitivity.
Commercial Relationships: Marrie Van der Mooren, AMO
GRONINGEN BV (E); Roger F. Steinert, Abbott Medical Optics Inc
(C); Farrell Tyson, Abbott Medical Optics Inc. (C); Robert Rosen,
AMO Groningen BV (E); Linda Lundstrom, AMO GRONINGEN
BV (F); Patricia A. Piers, AMO GRONINGEN BV (E)
Support: Supported by Eureka grant E!7187 / INT111017
Program Number: 1077 Poster Board Number: B0211
Presentation Time: 3:15 PM–5:00 PM
Development of an improved eye model for optical path
visualization of native and artificial lens characterization under
physiological conditions
Stephan Reiss1, 2, Julia Forbrig2, Heinrich Stolz1, Anselm Juenemann2,
Rudolf Guthoff3, Stefan Sievert3, Thom Terwee4, Oliver Stachs2.
1
Inst. of Physics, University, Rostock, Germany; 2Department of
Ophthalmology, University of Rostock, Rostock, Germany; 3Institute
of Biomedical Engineering, University of Rostock, Rostock,
Germany; 4Abbott Medical Optics b.v., University of Groningen,
Roden, Netherlands.
Purpose: Apart from mathematical simulations, only the optical
path visualization of native lenses and IOLs enable a qualitative
characterization of their imaging properties. Published setup’s for
optical path visualization have taken into account all refracting
elements but not an adequate beam profile. Our approach addressed
this deficit and focused on the characterization of lens properties
concerning the focusing position, transmission properties,
misalignment and tilt.
Methods: A laser based optical setup was developed which included
a customized artificial cornea. The beam profile of a semiconductor
laser (λ = 532 nm) was used to create a laser line with a flattop intensity profile, which was generated by an inverted beam
expander (10x) and a Powell lens as a line generator (45°). During
the measurement the lenses are localized in balanced salt solution
containing fluorescein to visualize the optical path captured by a
Nikon D3S camera in combination with a 60mm lens. For setup
verification, the optical path of a dedicated artificial and native
porcine lenses (n=5) were examined regarding the focal length and
compared to literature data.
Results: The used flat-top intensity profile improves the imaging
quality of the artificial eye model significantly. The focal length
of both artificial and native lenses can be visualized. Using the
plano-convex lens a focal length of 22.3 ± 0.2 mm was determined
experimentally compared to a calculated focal length of 22.5 mm.
For porcine lenses we found a mean focal length of 24.05 ± 1.99 mm
compared to ray-tracing simulations based on the GRIN-lens model
of de Castro (focal length 23.67mm) and the experimental data of
Vilupuru (23 to 33 mm).
Conclusions: The developed instrument enables the optical path
visualization of native and artificial lenses under physiological
conditions. In combination with WinLens3D simulations and a raytracing analysis a qualitative optical path characterization is possible
to analyze the optical performance of new IOL designs.
Commercial Relationships: Stephan Reiss, None; Julia Forbrig,
None; Heinrich Stolz, None; Anselm Juenemann, None; Rudolf
Guthoff, None; Stefan Sievert, None; Thom Terwee, None; Oliver
Stachs, None
Program Number: 1078 Poster Board Number: B0212
Presentation Time: 3:15 PM–5:00 PM
Ocular straylight in the normal pseudophakic eye
Grzegorz Labuz1, 2, Nicolaas J. Reus4, Thomas J. Van Den Berg3,
Ivan Marin-Franch5. 1Rotterdam Ophthalmic Institute, Rotterdam,
Netherlands; 2Facultad de Óptica y Optometría, Universidad de
Murcia, Murcia, Spain; 3Netherlands Institute for Neuroscience,
Royal Netherlands Academy of Arts and Sciences, Amsterdam,
Netherlands; 4Department of Ophthalmology, Amphia Hospital,
Breda, Netherlands; 5Departamento de Óptica, Facultad de Física,
Universitat de València, València, Spain.
Purpose: It is well known that the ocular straylight gradually
increases with age in normal phakic eyes. A normal reference
curve has been defined for phakic eyes. However, the crystalline
lens replacement causes considerable change in straylight, which
also modifies the steepness of its increase with age. The purpose
of this study was to determine a pseudophakic norm for straylight
as a new reference. In addition, the proposed model was tested
for its predictability of the effect of lens replacement on straylight
improvement.
Methods: A retrospective cross-study data analysis was performed
to evaluate changes in intraocular scatter upon crystalline lens
exchange. The postoperative results were used to define the norm for
straylight in pseudophakia with simple linear regression. Linearity
was assessed with a loess fit. The normative limits were obtained
using quantile regression. The straylight improvement following lens
replacement was assessed based on individual pre- and postoperative
values. Orthogonal regression was used to determine the break-even
point (BEP) with age affect.
Results: The pseudophakic norm was based on 1533 eyes from 13
studies. The new reference as well as the individual postoperative
straylight values are presented in Figure 1A. The outcomes of loess fit
and quantile regression are shown in Figures 1B and 1C respectively.
The straylight improvement as a function of preoperative value is
presented in Figure 2. The BEP increase with subject age is shown
with the red line in Figure 1A.
Conclusions: We developed a norm for straylight in the
pseudophakic eye that differs from the previously published norm
for the phakic eye. The loess fit shows that the straylight-age
dependency in pseudophakia is no longer logarithmic but linear.
Moreover, the BEP values are very close to the reference line (Figure
1A). Therefore, the established reference might be considered as a
predictive feature to improve the decision-making process before
crystalline lens exchange.
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Intraocular straylight as a function of age in pseudophakic eyes.
A) The new straylight norm (solid black line) with 95% prediction
interval (dashed lines). The red line shows the BEP-age dependency.
B) The loess fit of the reference data. C) The quantile regression
limits for the 90th, 95th, and 98th percentiles.
Improvement of straylight upon lens exchange. The solid lines
corresponds to the age range 40-50 years (left) and 80-90 years
(right).
Commercial Relationships: Grzegorz Labuz, None; Nicolaas J.
Reus, None; Thomas J. Van Den Berg, The Royal Netherlands
Academy of Arts and Sciences (P); Ivan Marin-Franch, None
Support: The AGEYE project (no. 60849), the Marie Curie Initial
Training Networks program (no. FP7-PEOPLE-2013-ITN) granted
by the European Commission
Program Number: 1079 Poster Board Number: B0213
Presentation Time: 3:15 PM–5:00 PM
Clinical validation of a compact optical straylight meter in
cataract patients
Harilaos S. Ginis1, Alexandros Pennos1, Lucia Hervella1, Eloy A.
Villegas1, Onurcan Sahin2, Belen Cañizares3, Jose María Marín3,
Pablo Artal1. 1Laboratorio de Optica, Universidad de Murcia, Murcia,
Spain; 2Institute of Vision and Optics, Heraklion, Greece; 3Servicio
de Oftalmología, Hospital Virgen de la Arrixaca, Murcia, Spain.
Purpose: To validate a novel compact optical instrument for the
measurement of intraocular straylight in a clinical setting. The
instrument, based on the principle of double-pass optical integration,
was applied in a cohort of cataract patients.
Methods: The instrument (Sigma, Sinusmedii SL, Spain) projects
onto the retina an extended source composed of a central disk (visual
angle 3 degrees radius) and a concentric annulus (3-8 degrees)
that are illuminated by high-brightness green LEDs (535nm). The
central part of this source and the annulus are temporally modulated
at different frequencies. Projection of this source onto the retinal
fundus and analysis of the back-reflected signal in the Fourier
domain allows the estimation of the straylight parameter (S) for an
angle of 5.5 degrees (Ginis et al., Biomedical Optics Express 5 (9),
3036-3041). Optical straylight measurements were performed in
54 eyes of 32 cataract patients randomly recruited both prior and
after pupil dilation. Four of the patients underwent 15 consecutive
measurements to assess the variability of the measurement.
Additional psychophysical measurement of straylight (c-Quant,
Oculus, Germany), manifest refraction and cataract grading based on
the LOCSIII system were also performed. As control, measurements
of straylight were also performed in 4 eyes of 4 young subjects with
no known ophthalmic pathology.
Results: The logarithm of the straylight parameter ranged from 0.90
to 2.21 in cataract patients and 0.79 to 1.20 in healthy eyes. The
coefficient of variance for the optical measurements was 0.03. The
distribution of the straylight parameter is well correlated with cataract
grades and with the psychophysical measurements (Pearson’s r =
0.75). In subjects with small pupil diameters prior to dilation (<4mm)
straylight measurements appeared elevated. Although the difference
was not statistically significant (p=0.13), it showed that possible
backscattering from the iris in eyes with small pupil diameters may
be a source of measurement artefacts to be controlled.
Conclusions: The compact optical straylight meter (Sigma) measures
the straylight parameter both in healthy and cataract eyes with high
repeatability under standard clinical conditions. The optical values
showed a good agreement with psychophysical estimates and clinical
gradation of cataracts.
Commercial Relationships: Harilaos S. Ginis, Sinusmedii SL (I);
Alexandros Pennos, None; Lucia Hervella, None; Eloy A. Villegas,
None; Onurcan Sahin, None; Belen Cañizares, None; Jose María
Marín, None; Pablo Artal, Sinusmedii SL (I)
Support: ITN OpAL (PITN-GA-2010-264605) and European
Research Council Advanced Grant ERC-2013-AdG-339228
(SEECAT)
Program Number: 1080 Poster Board Number: B0214
Presentation Time: 3:15 PM–5:00 PM
Longitudinal chromatic aberration between in visible and nearinfrared region in eyes with intraocular lens
Masashi Nakajima2, 1, Takahiro Hiraoka3, Toshifumi Mihashi2, Yoko
Hirohara2, 1, Tetsuro Oshika3. 1Development Engineering, TOPCON
CORPORATION, Itabashi-ku, Japan; 2Infomation Processing, Tokyo
Institute of Technology, Yokohama, Japan; 3Institute of Clinical
Medicine, University of Tsukuba, Tsukuba, Japan.
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.
ARVO 2015 Annual Meeting Abstracts
Purpose: Several researchers have studied the longitudinal chromatic
aberrations (LCA) of the human eye (Marcos et al., Vis. Res., 1999,
Artal et al., JOSA A., 2002). And a few researchers objectively
measured the LCA in eyes implanted with intraocular lenses (IOL)
(Nagata et al., Jpn J Ophthalmol.1999, Pérez-Merino, Marcos et
al., IOVS, 2013). Furthermore the measurements of chromatic
dispersions of materials used for IOLs were performed in the air
(Siedlecki et al., Optom. Vis. Sci., 2007, Zhao and Mainster, Br. J.
Ophthalmol., 2007). The aim of this research is to investigate the
LCA between the center of visible wavelength and near infrared
(NIR) light in eyes implanted with IOLs. The wavelength of NIR
light is often used in objective refraction.
Methods: We performed wavefront sensing on 68 eyes of 44 normal
subjects without IOL and 14 eyes of 11 subjects implanted with IOLs.
The ages of subjects without or with IOLs were 39.0±10.0 years
(average±SD, range: from 22 to 57) and 69.6±13.3 years (range:
from 29 to 83) and spherical equivalents without or with IOLs were
-3.9±2.8 D (range: from -9.5 to 0.5) and -0.9±0.8 D (range: from
-2.6 to 0.3). Five eyes were implanted with HY-60 (HOYA, Tokyo,
JAPAN), two eyes were implanted with SN60WF, six eyes were
implanted with SN60AT, and one eye were implanted with MA50BM
(Alcon Laboratories, Fort Worth, TX). All implanted IOLs were
acrylic and SN60WF, SN60AT and HY-60 were yellow-colored type.
We used a custom-build Hartmann-Shack Wavefront Aberrometer
(HSWA) with three different light sources (561, 690, 840 nm) for
wavefront sensing (Hirohara, ARVO, 2012). We calculated spherical
equivalents (SE) of each wavelength and then calculated LCA in
diopter between 561 nm and 840 nm.
Results: LCAs(840-561) were 0.96±0.08 D in eyes without IOL and
0.94±0.14 D in eyes with IOLs (p>0.05, Student’s t-test). LCAs(840were 1.01±0.10 D in eyes with Alcon IOLs and 0.80±0.06 D in
561)
HOYA IOLs. The mean difference between Alcon and HOYA was
0.21 D and that was statistically significant (P<0.05, Student’s t-test).
Conclusions: Longitudinal chromatic aberrations were different
between IOLs from Alcon and those from HOYA even though
all IOLs were acrylic. The results suggest that some variation of
chromatic dispersion exists among IOLs and attention should be paid
to performing near infrared objective refraction to eyes implanted
with different IOLs.
Commercial Relationships: Masashi Nakajima, TOPCON (E);
Takahiro Hiraoka, None; Toshifumi Mihashi, TOPCON (F); Yoko
Hirohara, None; Tetsuro Oshika, None
Program Number: 1081 Poster Board Number: B0215
Presentation Time: 3:15 PM–5:00 PM
Large deformation indentation of porcine ocular lenses:
experiments and computational modeling
Richard Regueiro1, Louis Foucard1, Franck Vernerey2, Christopher
Bay3. 1Civil, Environmental, and Architectural Engineering,
University of Colorado Boulder, Boulder, CO; 2Mechanical
Engineering, University of Colorado Boulder, Boulder, CO;
3
Mechanical Engineering, Texas A&M University, College Station,
TX.
Purpose: Mechanical characterization and modeling of the human
lens can lead to increased understanding of trauma suffered (e.g.,
by Intra-Ocular Foreign Body (IOFB) penetration) and effects of
surgical procedures on the lens, thus possibly leading to better
surgical treatments and vision correction methods.
Methods: Fresh 2+ year-old porcine eyes obtained <1 day postmortem are dissected to extract the lens, which is then immersed
for testing in a cup full of Balanced Salt Solution (BSS) warmed
to 39.2°C (pig body temperature) to attempt to reduce the nonphysiological effects of testing in-vitro. A puncture tip (6 different
geometries) indents the lens (anteriorly and posteriorly) along its
anterior-posterior axis at a displacement rate of 0.3 mm/s to 80%
nominal strain. The capsule fails, either by puncture at the tip or
by bulging rupture along the equatorial region. Force is measured
and digital videos are taken of the indented lenses. Computational
modeling using a coupled Lagrangian-Eulerian approach simulates
the internal fiber cells as an isotropic viscous fluid (for now,
see image), and the lens capsule as a hyperelastic impermeable
membrane undergoing large deformation (no failure at the moment).
The constitutive behavior of the capsule is derived using a multi-scale
homogenization analysis of the deformation of a two-dimensional
lattice approximation of the underlying type IV collagen meshwork
structure. Axisymmetric conditions are assumed in the simulations up
to puncture.
Results: The experimentally-measured and computationallysimulated force-displacement curves for extracted lenses, and
membrane-fluid interaction of the capsule and internal substance, are
matched up to large deformation before puncture.
Conclusions: Indentation loading is meant to mimic perforation
by an IOFB. Currently, the experimental method is limited in that
it ignores relaxation and tension in the zonules attached to the
equatorial region of the lens capsule, and in turn the attachment of
the zonules to the ciliary body. The method, however, successfully
represents the puncture response of the whole lens. The coupled
Eulerian-Lagrangian computational method allows for the first
time the simulation of large indentation of the lens, accounting for
capsule-substance interaction.
Lagrangian-Eulerian multiscale computational model of membranesubstance large deformation response to indentation loading of whole
lens.
Commercial Relationships: Richard Regueiro, None; Louis
Foucard, None; Franck Vernerey, None; Christopher Bay, None
Support: U.S. Army Medical Research and Materiel Command
(USAMRMC) grant W81XWH-10-1-1036
©2015, Copyright by the Association for Research in Vision and Ophthalmology, Inc., all rights reserved. Go to iovs.org to access the version of record. For permission
to reproduce any abstract, contact the ARVO Office at pubs@arvo.org.