Wait Times - Health Association Nova Scotia
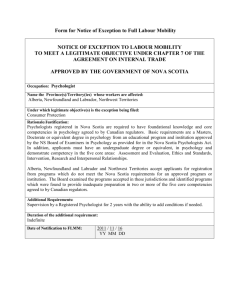
advertisement
Wait Times Research Paper Prepared By: Lauren Scott Nova Scotia Association of Health Organizations October 2005 Wait Times Research Paper Introduction A recent Supreme Court decision ruled that Quebec’s ban on private health care insurance for medically necessary services is illegal. This issue was not really about private versus public health care. The real underlying issue was about wait lists or more accurately wait times. The Canadian health care system never seems to resolve the issue of public versus private health care but when one looks at the issue at a deeper level, one of the issues at the heart of the debate is wait times. The call for a larger role for private health care is mostly about the “right” to access service more quickly if you have the ability to pay. This research paper intends to consider the issue of wait lists and wait times in more detail. Definitions The following are definitions used by the Nova Scotia Department of Health in their launch of the Nova Scotia Wait Times Web Site (2005): Wait List Î wait lists are maintained by facilities and/or individual doctors to keep track of people waiting to be scheduled for consults, tests or procedures, or treatments. Wait Time Î wait time is the time between when a patient and the doctor/nurse practitioner determine a service is needed and when the service is actually carried out. Interestingly, defining wait time is one of the issues. For example, one survey found that 58 per cent of organizations felt that when an MRI was booked was the starting point for determining wait time (Sanmartin et. al., 2000). This is not in sync with the above definition. In fact, when Nova Scotia’s information is examined more closely not all wait times are measured as they have defined. In Nova Scotia, cardiovascular surgery wait time is measured by “the number of calendar days from the day the decision is made that surgery is necessary to the day they receive the service”. This measurement is consistent with the above definition. Whereas, referrals to specialists is measured by “the number of www.nsaho.ns.ca Page 1 October 2005 calendar days from the day the referral arrives in the cancer centre to the day the specialist appointment takes place.” If there were standardized definitions it would make it easier to compare data across jurisdictions. In addition, there are complications based on the fact that there is more than one method to measure wait times (Sanmartin et. al., 2000). Measurement Methods Cross-sectional Î This method answers the question, “how long have patients currently on the list been waiting”. Retrospective Method Î This method would be used to determine how long people who had already received service, during a selected time period, had waited. For example, how long did people who received the service in January of 2005 wait. Prospective Method Î This method follows people from the time they are placed on the list until they receive service. For example, all people put on the list in November 2005 would be monitored until their receive service. All three methods are useful depending on what information is being gathered and in fact, all three methods might be used to gain a more complete picture. However, comparability is compromised if different measurement methods are being used (Sanmartin et. al, 2005). It appears that Nova Scotia is mostly using the retrospective method to determine the wait times being reported on the new web site (NS Web Site, 2005). Statistics Wait times can be reported statistically as mean, median or interval measures (Sanmartin et. al., 2000). The mean being the average and the median meaning that half of the people waited shorter than the median number and half of the people waited longer (NS Web Site, 2005). Interval measures are also used; an example would be the “proportion of patients who have waited for more than 60 days” (Sanmartin et. al., 2000). Using mean wait times as a reporting mechanism can be misleading; it is strongly influenced by small numbers of large waits (Sanmartin et. al., 2000). It is the mean or the average wait time that Nova Scotia seems to be using most frequently (NS Web Site, 2005). Why Wait List? Wait lists are always portrayed as a negative thing. First and foremost, it is important to remember that wait lists in and of themselves are not necessarily a www.nsaho.ns.ca Page 2 October 2005 problem. “There is a significant difference between being on a long list and being on a list for a long time” (Lewis et. al., 2000). The intent behind wait lists is to ensure that those with the greatest need for the service receive it first (Lewis et. al., 2000). “In theory universal coverage on equal terms and conditions also allows all patients to be assessed, with wait list priorities assigned according to need. This approach of managed delay can be contrasted with the potential for arbitrary delay, and denial, based on insurance coverage and/or income….(Naylor et. al., 1995). If everyone were to receive service immediately, excess capacity would need to exist within the system. This is not an efficient use of resources (Naylor et. al., 1995). Not to mention, if individuals were to receive service immediately there is no time for “sober second thought.” Waiting can also provide benefits in that many patients choose not to go through with the procedure, seek a second opinion, adapt to the condition, or gain benefit from trial management (Lewis et. al., 2000). While it is possible to identify benefits to some period of waiting, excessive waits clearly raise the possibility of suffering and irreparable damage to a person’s health. Root Causes of Excessive Waits The most commonly sited reasons for long waits are (Sanmartin et. al., 2000): • • Inadequate resources (funding, human resources, OR time etc.); and Poor management of existing resources. Most of the focus is on the first one, particularly funding. Solutions Additional Resources Just as the focus of the problem is on inadequate resourcing, the solutions are also most frequently targeted there. In fact, research has demonstrated that if asked “what is the best solution to reduce wait times” most respondents believe more funding (Sanmartin et. al., 2000). There is evidence that these types of solutions can make positive change. British Columbia’s cardiac wait lists were reduced by one-third in 10 months through more funding and better recruitment of staff. More importantly, wait times were reduced from 18 weeks to 14.9 weeks (Jones, 2004). www.nsaho.ns.ca Page 3 October 2005 However, there is strong evidence that this type of targeted increase in funding does not have a lasting impact on wait times or can result in undesired outcomes. For example, in the UK funding was made available to provide service to those who had waited beyond a predetermined threshold (all those who had waited 12 months or more for example). This reduced the wait list over all but had the unintended result that wait times were increased for higher-priority patients. In some cases, wait lists became even longer when funding was targeted for their reduction. Sanmartin et. al. (2000) refer to this as a “feedback” phenomenon, meaning that family physicians tend to refer patients for those services that have a decreasing wait time. It must also be recognized that when resources are put into the system to reduce specific wait times, those resources have to come from elsewhere. This applies to more than just funding. For example, if more operating room time is allocated to reduce the wait time for a specific procedure this may mean that other procedures are backing up (Lewis et. al., 2000). Private Health Care One of the most common solutions presented to reduce wait times is to allow for an expanded role for private health care. The idea being that those who can afford to pay for service in the private sector will do so, receive faster care and in doing so decrease the number of people waiting in the public sector (Sanmartin et. al., 2000). There are problems with this theory, however. A shortage of health care professionals already exists. With the expansion of the private sector it is difficult to imagine how this would not drain the public sector of workers thereby increasing wait times further. It is possible that more people could be trained but this is a lengthy process that takes time before results are achieved. It is also very expensive and is mostly done at public expense. It is unclear how the public would feel about training health care professionals with public funds only to have them go and work in the private sector (Flood and Sullivan, 2005; Sanmartin et. al., 2000). The more important response to this theory is that there is no clear evidence that this is what actually occurs. In fact, the evidence appears to be the contrary in many cases – wait times appear longer in countries with two-tier health care (Flood and Sullivan, 2005). In the UK, private health care is focused on hips, hernias, haemorrhoids, cataracts and gynaecological problems. Despite these services being provided in the private sector these same services have some of the longest wait times in the public sector. In addition, “regions with the longest wait lists also have the highest rates of private surgery” (Sanmartin et. al., 2000). www.nsaho.ns.ca Page 4 October 2005 Health Care Guarantee A health care guarantee is when there is a predetermined time for each procedure that is deemed acceptable to wait. These predetermined thresholds should be scientifically determined. When patients reach that predetermined threshold of waiting “too long” then the government pays for them to receive the procedure in another jurisdiction. The Standing Senate Committee on Social Affairs, Science and Technology (2002) supports the implementation of a health care guarantee in Canada. One of the issues with a health care guarantee is that it is really a method of targeted reduction discussed under the section additional resources and hence, has the same difficulties. If the focus is on ensuring individuals do not have to wait past a predetermined time rather than on priority it increases the wait for individuals of high priority. Better Management Wait lists are generally managed by individual physicians and/or facilities (Sanmartin et. al., 2000), which is also how Nova Scotia has chosen to define it. It is this very fact that causes part of the problem. As Steven Lewis said (2000), “the probability that tens of thousands of individual, uncoordinated decisions taken in a large, complex and diverse system will combine to yield fairness for all is vanishingly low.” Nova Scotia is making progress with the establishment of a wait times’ web site for some services. This does enable patients to see that waits may be shorter elsewhere and discuss with their physician seeking the service there. However, this not pooling lists together. Nova Scotia is the first Atlantic province to make this information available to the public. Auditing of wait lists is rarely done in Canada. However, it has the potential to have a significant impact on wait times in this country. Research has consistently shown that there are many patients on wait lists inappropriately. Inappropriate placements range from 15 to 70 per cent, with research indicating numbers most commonly between 20 to 40 per cent (Sanmartin et. al., 2000). These inappropriate individuals include: • Procedure has already been done; • Procedure is no longer required; • Patient is unaware that they are on the wait list and request to be removed when notified; • Patient has died; • Procedure is not appropriate for the patient; • Alternate procedure is preferable; and • Change in patient’s clinical condition. www.nsaho.ns.ca Page 5 October 2005 There is also a significant issue of missed appointments that needs to be addressed. A study done in the UK found that if people notified the care provider of when they were going to miss an outpatient appointment wait times could have been reduced from 6 months to one week (Rachlis, 2000). In Nova Scotia, it was found that 113 people could have received service faster as in July 2005 ten per cent of the 1, 136 patients scheduled for an ultrasound at the QEII did not show up. Also in July, 2005 twenty per cent of people scheduled to receive an upper GI and Barium Enema at a hospital in the province did not show up (Nova Scotia Web Site, 2005). Information and Information Systems First, there needs to be tools in place that allow patients to be prioritized first within individual lists and then again when placed on pooled lists (Lewis et. al., 2000). Then there needs to be reliable data on which to do analysis. Research has shown that Canada focuses its spending on direct health care and has been reluctant to invest in those supportive components of health care such as information systems, although, arguably this is shifting. Lewis et. al. (2000) states that Canada is held, “hostage to its own failure to invest in the fundamental infrastructure for intelligence gathering.” In order for Canada to be able to effectively reduce wait times and see results over the long term the situation must first be understood. Series of Solutions Lewis et. al. (2000) identify a series of actions that they believe will result in an increased understanding of wait times and the reduction of those wait times: • • • • Standardized concepts and terms Î as previously discussed, it is important that all jurisdictions are defining and measuring wait times in the same way. Audit, evaluation and quality control Î wait lists need to audited to ensure that those who are on the list are appropriate. Systematic, not isolated solutions Î as previously discussed, targeted solutions can have the unintended effect of increasing the wait times of those with higher priority who do not meet the threshold of having waited too long. Public ownership of lists Î Lewis et. al (2000) argue that the public needs an opportunity to weigh in on this debate and declare their values and preferences. For example, there are ongoing debates about whether factors such as employment status and age should effect where you are placed on a waiting list. Public ownership of lists is also about giving the www.nsaho.ns.ca Page 6 October 2005 public an opportunity to choose to seek services from physicians or facilities with shorter wait times. • It is also important to understand patients’ acceptance of wait times. One study found that the strongest predictor of patients’ response to wait times was how long they perceived the wait was going to be. The same study found that when asked how long was acceptable to wait, their general wait time was shorter than they were willing to wait themselves (wait time for an ultrasound should be no longer than three months but when asked how long they are willing to wait might say four months) (Dunn et. al., 1997). Fairness among providers Î when the public is given the opportunity to redirect their service to the shortest wait lists then conflict between providers may arise. If operating in a fee for service environment, providers “losing” patients to another provider represents a loss of income; thereby making providers less willing to allow patients to move around. It need to be understood why some providers have shorter wait times than others. It is not sufficient to shift patients between lists without understanding the reasons for variability. There are any number of reasons for variability that are acceptable but it must be understood – does a provider have short wait times because they are efficient? does a provider have long wait times because they are not following best practice or do they have long wait times because they are perceived as “best in the business” and everyone wants to see receive service from them (Lewis et. al., 2000). Conclusion Clearly, reducing wait times is a far from straight forward issue. However, it is reassuring to realize that there are a number of avenues to consider in determining how to bring wait times under control. It is also important to realize that not all solutions are extreme. It is not necessary to create a larger role for the private sector immediately. The system has yet to consider the impact of wait list auditing and controlling for missed appointments, for example. This is an issue to which there are solutions. The action that needs to be taken is to determine which solutions are likely to have the best chance for success and which ones are most palatable to the Canadian public. www.nsaho.ns.ca Page 7 October 2005 References Bloom, B., and M. Fendrick. (February 1987). Waiting for Care: Queuing and Resource Allocation. Medical Care Journal. Vol. 25, No. 2. Dunn, E., Black, C., Alonso, J., Norregaard, J., and G. Anderson. (1997). Patients’ Acceptance of Waiting for Cataract Surgery: What Makes a Wait Too Long. Soc. Sci. Med. Journal. Vol. 44. No. 11. Esmail, N., and M. Walker. (2005). Waiting Your Turn: Hospital Waiting Lists in Canada, 15th edition. Fraser Institute. Flood, C., and T. Sullivan. (July 2005). Supreme Disagreement: The Highest Court Affirms an Empty Right. Canadian Medical Association Journal. Vol. 173. Iss. 2. Galloway, G. (October 14, 2005). MDs Upset Over Broken Waiting-Times Pledge. Globe and Mail. Hadorn, D. (August 2005). The Chaoulli Challenge: Getting a Grip on Waiting Lists. The Canadian Medical Association Journal. Vol. 173, Iss. 3. Hartt, S., and P. Monahan. (May 2002). The Charter and Health Care: Guaranteeing Timely Access to Health Care for Canadians. C.D. Howe Institute. The Health Papers. Jones, D. (September 2004). BC Cuts Cardiac Wait-List by One-Third. Canadian Medical Association Journal. Vol. 171, Iss.6. Lewis, S., Barer, M., Sanmartin, C., Sheps, S., Shortt, S., and P. MacDonald. (May 2000). Ending Waiting-List Mismanagement: Principles and Practice. Canadian Medical Association Journal. Vol. 162, Iss. 9. Naylor, C.D., Sykora, K., Jaglal, S., Jefferson, S., and the Steering Committee of the Adult Cardiac Care Network of Ontario. (December 1995). Waiting for Coronary Artery Bypass Survey: Population-Based Study of 8517 Consecutive Patients in Ontario, Canada. The Lancet. Vol. 346, No. 8990. Nova Scotia Department of Health. (October 2005). Wait times Web Site Launch Package. Rachlis, M. Modernizing Medicare for the Twenty-First Century. BC Health Innovation Forum. www.nsaho.ns.ca Page 8 October 2005 Romanow, R. and the Commission on the Future of Health Care in Canada. (November 2002). Building on Values: The Future of Health Care in Canada. Sanmartin, C., Shortt, S., Barer, M., Sheps, S., Lewis, S., and P. MacDonald. (May 2000). Waiting for Medical Services in Canada: Lots of Heat but Little Light. Canadian Medical Association Journal. Vol. 162, Iss. 9. Sibbald, B. (September 2005). CMA Okays Private Health Care for Waiting kljPatients. Canadian Medical Association Journal. Vol. 173, Iss. 6. Smith, A. (October 8, 2005). Waiting Lists Go Online. Chronicle Herald. Standing Senate Committee on Social Affairs, Science and Technology. (April 2002). The Health of Canadians. The Taming of the Queue II: Wait Time Measurement, Monitoring and Management. Colloquium Report. March 31-April 1, 2005 Ottawa, Ontario. www.nsaho.ns.ca Page 9 October 2005