Building and Environment 39 (2004) 1171 – 1178
www.elsevier.com/locate/buildenv
Diagonal air-distribution system for operating rooms:
experiment and modeling
Monika Woloszyna;∗ , Joseph Virgonea , St1ephane M1elenb
a Centre
de Thermique de Lyon:UCBL, CNRS UMR 5008, INSA de Lyon, bat. 307 20, av. A. Einstein, 69621 Villeurbanne Cedex, France
b Air Liquide, Centre de Recherche Claude Delorme, Jouy-en-Josas, France
Received 19 March 2003; received in revised form 17 March 2004; accepted 24 March 2004
Abstract
The air5ow patterns and the di6usion of contaminants in an operating room with a diagonal air-distribution system were subjected
to both experimental measurements and numerical modeling. The experiments were carried out in MINIBAT test cell equipped with
an operating table, a medical lamp and a manikin representing the surgeon. Air velocity and tracer-gas concentration were measured
automatically at more than 700 points. The numerical simulations were performed using EXP AIR software developed by Air Liquide for
analyzing air quality in operating rooms. Only isothermal conditions were investigated in this comparison with the numerical software.
The results showed that the contaminant distribution depended strongly on the presence of obstacles such as medical equipment and sta6.
? 2004 Elsevier Ltd. All rights reserved.
Keywords: Air quality; Air distribution; Contaminant; CFD; Experiment; Numerical simulation; Operating room; Tracer gas; Validation
1. Introduction
The purpose of ventilation systems in health-care facilities
is not only to maximize conditions of comfort, but also to
remove airborne contaminants. The latter task becomes vital
when such contaminants are dangerous for human health, as
is the case for certain bacteria in operating rooms. During
surgery, the patient is at risk of contamination from several sources such as his own body, the surgical team, or
medical instruments. The main way of reducing the risk of
post-operative infection is the strict application of aseptic
procedures, regardless of the ventilation system. In practice,
however, it is impossible to achieve zero contamination in
an operating room. For example, a detailed survey carried
out in 1996 showed that in France 10.5% of nosocomial infections are contracted in an operating room [1].
In order to ensure the most sterile conditions possible
during surgery, and to protect the patient from the contaminants that are present in the air, the air-distribution system in the operating room needs to be carefully designed.
CFD (computational 5uid dynamics) provides a useful way
∗ Corresponding author. Tel.: +33-4-72-43-6269; fax: +33-4-7243-8522.
E-mail address: monika.woloszyn@insa-lyon.fr (M. Woloszyn).
0360-1323/$ - see front matter ? 2004 Elsevier Ltd. All rights reserved.
doi:10.1016/j.buildenv.2004.03.013
of studying air5ows and contaminant distribution patterns
in operating-room applications [2–5]. However, experimental data obtained from model studies of buildings are still
indispensable to the design of air-distribution systems [6].
Therefore a computer program, before being used in predictive calculations, needs to be validated using experimental
results. The analysis of operating rooms is quite a speciJc
problem, due to the presence of obstacles (equipments and
sta6), and the fact that the zone of interest is small. In order
to minimize the risk of infection, a detailed analysis of the
contaminant 5ow close to the patient is more helpful than
the data regarding the overall air5ow pattern.
This study consists of a detailed analysis of the air5ow
patterns and of the contaminant distribution in an operating
room, using both experimental and numerical methods. In
this Jrst investigation only isothermal conditions are of interest, so the thermal buoyancy e6ects are not taken into account. The objective was to develop a reliable predictive numerical tool for operating-room applications. The Jrst part
of the project consisted of an experimental study of contaminant distribution. Such experiments being diKcult to perform in situ, mainly because of the sterility requirements and
the presence of complex medical apparatus, we decided to
set up a life-size experimental model of an operating room,
using an existing test cell, the MINIBAT. The numerical
1172
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
simulations in the second part of the project were performed
using EXP AIR software developed by Air Liquide [7] for
the analysis of air quality in operating rooms.
2. The experiment
2.1. The MINIBAT test cell
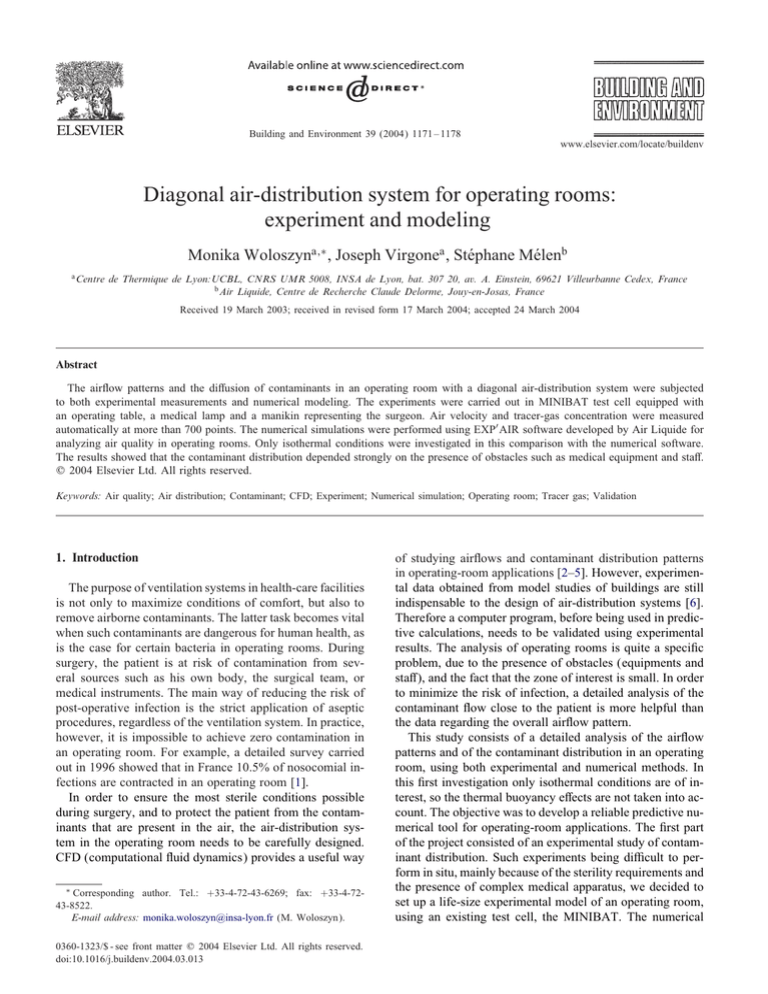
The Centre de Thermique de Lyon (CETHIL) owns a
full-size test cell, the MINIBAT, which was speciJcally designed for the detailed measurement of air5ows in Jxed conditions. This facility comprises two identical cells (Cell 1
and Cell 2) which measure each 3:10 × 3:10 × 2:50 m3 (see
Fig. 1). Cell 1 is separated by a glass wall from the climatic
chamber, whose air-treatment system can produce temperatures of between −10◦ C and +30◦ C. The thermal guard is
maintained at a uniform temperature of 20◦ C to represent
adjacent spaces.
The MINIBAT is equipped with sensors for measuring
surface and air temperatures, air velocities and tracer-gas
concentrations. Relative air humidity and operative temperature are measured near the center of each cell. Both cells
are also equipped with an automatic device that moves the
sensors over di6erent vertical planes. This device consists of
3 motors which actuate a metal arm on which is mounted an
array of 6 sensors: 2 K-type thermocouples for air temperatures, 2 omnidirectional hot-wire probes for air speeds, and
2 measuring points for gas concentrations. Tracer-gas concentrations are measured using a BrNuel and Kjaer analyzer
[8]. The precision of the results obtained in the MINIBAT
was ±0:3◦ C for air temperatures, 3% for air velocities higher
than 5 cm=s, and 4% for tracer-gas concentrations [9].
Fig. 2. Diagonal air-distribution system in the Hôtel Dieu hospital, Lyon,
France.
The air5ow can be either turbulent or laminar (i.e. unidirectional), and additional devices, such as air curtains or partitions, can also be used. Some examples of existing systems
are discussed in detail by Pfost [11], Horworth [12,13] and
Lewis [14].
The eKciency of an air-distribution system in preventing nosocomial infections depends on factors such as the
position of the air inlet and outlet, the air-inlet velocity or
air-change rate, the presence of air5ow-perturbing elements
(equipment, sta6) and the type of operation being performed.
In order to construct a realistic model of an operating
room, some measurements were taken in the Hôtel Dieu hospital in Lyon, France, whose operating room was equipped
with a diagonal-type ventilation system, with two air inlets in the ceiling, though not directly above the operating
table ([15], see also Fig. 2). The outlet was situated in the
lower part of the wall. The inlet air velocities were 3.9 and
2:15 m=s. The air velocities close to the operating table were
too low to measure (¡ 0:1 m=s). The air temperature varied
according to the surgeon and the type of operation, but the
most common values were in the range 19–20◦ C.
During the in situ visit, in addition to the air-distribution
system, and as already reported in the literature, 3 other
elements were found to a6ect the air5ow patterns.
2.2. Experimental model of an operating room
2.2.1. Key components
Air-distribution systems for operating rooms are of several di6erent types. According to [10] it would seem that
the delivery of air to the upper part of the room, with the
exhaust located on the opposite wall, is probably the system
that gives the lowest concentration of contaminant. The air
inlet can be situated either right above the patient (central
air distribution) or to one side (diagonal air distribution).
• The operating table.
• A lighting system speciJcally designed for operating
rooms, which concentrates light on a small area (up
to 100,000 lux on an area of 100 cm2 ) with a color
Thermal guard
Glass wall
Median
Air Inlet
Z
Sensors
Y
cell 1
Climatic chamber
cell 2
Door
X
Concentration
Air Velocity
Air Temperature
Vertical Displacement
Horizontal Displacement
Lateral Displacement
Fig. 1. The MINIBAT test cell.
cell 1
Air Exhaust
Pollutant
injection
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
A
B
C
A
air
inlet
table
manikin
1173
lamp
air
outlet
air
inlet
C
B
table
M
M
air
outlet
lamp
contaminant
injection
point
manikin
A
B
C
A
B
contaminant
injection
point
C
Fig. 3. The experimental set-up. (a) Horizontal view and (b) cross section at MM.
temperature above 3000 K, but with limited heat emission
in the illuminated zone. The lamps are in general placed
between the clean-air inlet and the patient.
• The medical personnel, who act as mobile obstacles
between the air inlet and the patient, and are a source
of contaminant. Their shapes and movements are impossible to represent accurately, but other parameters can be taken into account in the experimental
model.
2.2.2. Main features of the experimental model
Cell 1 of the MINIBAT was used to model operating-room
conditions.
The air exhaust was positioned in such a way as to produce diagonal air distribution. The ventilation air 5ow was
set at around 100 m3 =h so as to obtain an air velocity close
to 2:5 m=s at the air inlet, in order to represent real situation. Real velocity values were used rather than air-change
rate, because though both parameters had an impact on air5ow patterns, it was found that at higher values, air-change
rates had little in5uence on the eKciency of the ventilation
system [16].
The inside of the cell was equipped with:
• a wooden table measuring 2:00 × 0:47 × 0:14 m3 , with a
parallelepiped support 1:40×0:70×0:27 m3 , both painted
matt white;
• a manikin, i.e. a metal parallelepiped 0:20 × 0:30 ×
1:70 m3 , with its external surface painted black, representing a surgeon;
• a low-temperature lamp (PrismAlix 4003 S, obtained from
Air Liquide Healthcare), situated 1:12 m above the center
of the table.
The contaminant was represented by a stream of tracer gas
coming from the manikin’s “mouth”, at a height of 1:52 m.
The tracer-gas 5ow rate was 15 ml=min. Sulfur hexa5uoride
(SF6 ) was used because it is detectable at low concentrations
and does not react chemically with air. It is also heavier than
Fig. 4. The test cell.
air, and in this respect behaves in a similar way to the most
common air pollutants [17].
The experimental conJguration is shown in Figs. 3 and 4.
During the experiment, in order to ensure isothermal conditions, the temperatures of the thermal guard, the inlet air
and the climatic chamber were maintained at 20◦ C, and there
was no active heat source in the test cell.
The climate in the test cell (tracer-gas concentrations, air
velocities and temperatures) was measured at several points
on 4 vertical planes, as shown in Fig. 3:
• a longitudinal plane MM, between the air inlet and
outlet;
• three lateral planes:
◦ AA: between the manikin and the operating table;
◦ BB: between the operating table and the lamp;
◦ CC: between the operating table and the air outlet.
For these 4 planes the measurements were carried out on a
15 × 15 cm2 grid, except close to the manikin and the table,
where a 7:5 × 15 cm2 grid was used in order to achieve
1174
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
greater precision near the perturbing elements. The grid sizes
were chosen on the basis of previous work carried out in the
MINIBAT [9]. Finally, more than 700 measurement points
were used to characterize 3-dimensional (3D) Jelds of air
velocity and tracer-gas concentration.
2.5
air
inlet
1
1.72
1,
1,4
1,6
1.19
1,5
1,3
1,1
0.9
0.8
0.6
0.5 0.4
0.2
0.3
2
lamp
0
manikin
Z (m)
1.5
3. Numerical model
0.7
0.1
table
1
3.1. EXP AIR software
The EXP AIR is a CFD program based on a Jnite-volume
discretization of Navier Stokes equations [18] adapted to
3D simulations of indoor climate. EXP AIR is dedicated
to clean room applications; it is a reworked version of the
general CFD program ATHENA [19,20,21] developed by
Air Liquide. The simulated domain is Jnely discretized using an orthogonal mesh system, in order to reduce computational time. The coupling between velocity and pressure
is ensured by the well-known SIMPLE algorithm. The numerical results from EXP AIR have already been successfully compared with experimental measurements for natural
convection in a 2D case, and for forced convection in an
empty 3D enclosure with a low ventilation rate [21], and
the program has also some post-treatment features, such as
easy visualization of air or contaminant paths, which make
of it a valuable tool for the precise analysis and design of
air-distribution systems.
3.2. Numerical model
EXP AIR was used to model MINIBAT’s Cell 1,
equipped with diagonal ventilation, operating table, manikin
and lamp (see Section 2).
The turbulence model used here was the 2-equation standard k– model, which is well suited to the simulation of
indoor environments. The 5ows near the boundaries were
represented by using the standard logarithmic law [22].
SF6 concentrations were calculated using the conservation equation adapted to heavy gases. The model used
in EXP AIR for the description of contaminant 5ows
came from the DISPAL program, which was designed for
use in the simulation of contaminant distribution in open
spaces [23].
4. Case study: experiment and modeling
4.1. Experiment
The wall and the thermal-guard temperatures, as well as
the inlet and outlet rates, were kept steady for the duration of
the experiment (which lasted several days). In the occupancy
zone, the measured temperatures were between 20:3◦ C and
20:5◦ C. It can therefore, be considered that the cell was
isothermal.
air
outlet
0.5
0
0.5
0.75
1
1.25
1.5
1.75
2
2.25
2.5
2.75
Y (m)
Fig. 5. Iso-velocities measured in the MM plane (m/s).
2.5
60
40
air inlet
2
80
manikin
lamp
1.5
X (m)
100
contaminant
source
table
1
160
200
260
240
180
140
air outlet
0.5
120
0
0.5
220
0.95
1.4
1.85
2.3
2.75
Y (m)
Fig. 6. Iso-concentrations measured in the MM plane (mg=m3 ).
The most interesting results were those for air velocities
and tracer-gas concentrations. The iso-value plots presented
in this section were produced using EES software [24].
Fig. 5 shows the air velocities in the cell. The ventilation
jet at ceiling level can be clearly seen. In front of the manikin,
between the table and the lamp, the air velocity was very
low (¡ 10 cm=s).
The tracer-gas concentrations in the cell are shown in
Fig. 6. Two important pockets of SF6 can be seen in front of
the manikin: one close to the table, the other at 5oor level.
This illustrates the downward di6usion of SF6 , and conJrms
the existence of an almost-immobile air zone, as detected
by air-velocity measurements.
4.2. Modeling
The air5ow and the contaminant distribution in the MINIBAT were simulated using the EXP AIR software. In order
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
1175
idates (or even renders impossible) numerical simulations.
In the present case, however, a numerical convergence was
reached, and the computed values were in good agreement
with the experimental measurements (see Section 4.3 for
more details).
4.3. Experimental and numerical results: discussion
Fig. 7. SF6 concentration cartography in the MM plane simulated with
EXP AIR (mg=m3 ).
to produce a realistic description of the air5ow, a good definition of the boundary conditions was very important. The
representation of the air inlet was the focus of our interest due to its essential impact on the overall air-distribution
pattern. Several methods are to be found in the literature
for representing correctly the boundary conditions at the air
inlet [25]. The best results have been obtained using a detailed description of air-inlet geometry, representing accurately the grid [26]. However, the Jneness of mesh needed to
perform these calculations and therefore the computational
time make this approach impractical. Other methods have
been suggested, generally based on a simpliJed model of
the air inlet, without the grid, but with the same essential
characteristics (5ow, e6ective area and aspect ratio). This
model was compared with more sophisticated approaches
by International Energy Agency Annex 20, with encouraging results [26,27]. Moreover, the e6ect of the turbulent intensity was found to be less signiJcant than the description
of dynamic conditions.
In the MINIBAT, an industrial air vent, equipped with
horizontal and vertical grids, is used as the air inlet. As a
detailed description of grid geometry was not possible in
the present case, the basic approach for the representation
of boundary conditions was used. In order to assess the
parameters of the simpliJed jet (neglecting the perturbing
impact of the grid), preliminary simulations were conducted
using the commercial CFD program Fluent [28]. The inlet
boundary conditions used as input parameters in EXP AIR
simulations were determined by comparing the measured
and 5uent-simulated shapes of the air jet.
The SF6 concentrations in the medium plane were calculated by EXP AIR, as shown in Fig. 7, and the strongest concentration found at the source was 22; 118 mg=m3 , while the
average value was around 100 mg=m3 , and close to the air
inlet the program computed a value of 0:27 mg=m3 . Such a
di6erence, i.e. some 6 orders of magnitude, in general inval-
Fig. 8 shows the measured and calculated air velocities in
the median MM plane. Except for the highest velocity values for the Jrst 2 proJles (at X = 0:53 m and at X = 0:6 m
from the wall and close to the air inlet), there was very
good agreement between experimental and numerical results. Clearly, the experimental air jet from the inlet, which
follows the ceiling to the opposite wall, is accurately represented. There is a small rise in the simulated velocity proJles
at medium height between the table and the air outlet (for
X ¿ 2 m), which illustrates the recirculation of the air and
is in keeping with the experimental conJguration. Slightly
higher air-velocity values close to the 5oor for X ¿ 2:1 m,
in both the numerical and experimental proJles, show the
in5uence of the air outlet.
The di6erence between the maximum air-velocity value
for the proJles at X = 0:53 and 0:6 m is due to the way
the model represents the air inlet. As mentioned in Section
4.2, a simpliJed model, neglecting the perturbing e6ect of
the grid, was used in this study. Allowing for some imprecision in the local description of the air jet, this basic
model gives a correct representation of the overall air5ow,
keeping the computational time within reasonable limits. A
more detailed representation of the air inlet would improve
the description of the jet at the air inlet, but would also require much more computational capacity and time. Despite
the imprecision in the local representation of the air jet, the
model was satisfactory for the purpose of our study. Indeed,
the overall air5ow pattern distribution in the cell, as simulated with EXP AIR, as well as the description of the zone
of main interest between the operating table, the manikin
and the lamp was in good agreement with experimental
measurements.
The comparison between the measured and simulated contaminant concentrations in the median MM plane is shown
in Fig. 9. There is quite good overall agreement between
the measured and the simulated values, but the di6erence is
a little higher for the concentration proJles than for the air
velocities, mainly due to numerical factors. The SF6 concentrations presented in Fig. 9 are between 50 and 300 mg=m3 ,
which is much less than the maximum concentration of
22; 118 mg=m3 registered close to the source (by a factor of
100), i.e. the degree of relative precision of numerical simulation is satisfactory. Moreover, the overall distribution of
the contaminant is well represented by EXP AIR (compare
Figs. 6 and 7).
From Figs. 6, 7 and 9, it can be seen that the contaminant concentration was at its highest just below the point of
1176
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
Fig. 8. Velocity proJles in the MM plane (m/s) for di6erent positions of X (between the air inlet and outlet), as calculated with EXP AIR (—) and
measured (•).
injection, between the manikin and the table. The gas followed its natural tendency to downward di6usion, indicating
that the air movements in this zone were too weak to ensure
e6ective mixing. The result was a high concentration of the
contaminant just above the table, which in real conditions
would be undesirable.
Such “pockets” of contaminant are clearly due to the presence of obstacles which perturb air5ows. This is conJrmed
by the fact that in previous work on diagonal ventilation in
the empty MINIBAT test cell, the contaminant was found
to be quite homogenously distributed [21].
5. Conclusions
The experimental and numerical results of the present
study clearly show that the distribution of the contaminant
in an operating room, and therefore the risk to patient, de-
pends on the geometrical parameters of the room, such as the
position of the air inlet and outlet, the contaminant source,
and objects that could perturb the air5ow. For a diagonal
air-distribution system, the results presented here show that
the obstacles in the occupancy zone had a signiJcant in5uence on the distribution of the contaminant. Indeed, even
when the air velocity at the inlet was high (around 2:5 m=s),
the air in the occupancy zone was almost immobile. It can
therefore be seen that, for a Jxed source, the distribution of
the contaminant depends on the position of obstacles (equipment and sta6).
A correct representation of the contaminant distribution
in the presence of obstacles is thus an essential characteristic of a numerical program, whose purpose is to simulate
air-distribution patterns in operating rooms. The results of
the EXP AIR simulations presented here are close to the
experimental measurements, showing that EXP AIR, which
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
1177
It will be interesting, in a future work, to analyze the
thermal buoyancy e6ect. It will be necessary to consider
the in5uence of the heating sources: the surgeon power, the
patient one, the lamp.
References
Fig. 9. SF6 concentration proJles in the MM plane (mg=m3 ) for di6erent
positions of X (between the air inlet and outlet), as calculated with
EXP AIR (—) and measured (•).
includes now a dispersion model adapted to heavy gases
and an adequate representation of the air inlet, is well suited
to detailed design and analysis of diagonal air-distribution
systems for operating rooms.
With such a diagonal ventilation system, the pollutant
goes down and the patient receives the possible contaminants coming from the medical sta6. A better solution would consist in an air inlet at the bottom of the
room and an exhaust near the ceiling: in such a case,
contaminants would be extracted without falling on the
patient.
We should also point out the diKculties involved in the
experimental study of air5ow patterns in operating rooms.
Even in laboratory conditions, detailed measurements using
traditional techniques are impossible, due to low air-velocity
values. If air-distribution patterns are to be studied in the
kind of situation dealt with in the present study, where there
is a zone in which air velocity is too low to be measured
by normal type of sensors (5 cm=s for hot-wire probes), an
alternative method must be used, e.g. based on tracer-gas
measurements or CFD simulations.
[1] CTIN. Enquête Nationale de Pr1evalence des Infections Nosocomiales,
Mai-Juin 1996 Comit1e Technique national des Infections
Nosocomiales—Secr1etariat d’Etat aU la Sant1e et aU la S1ecurit1e
Sociale. Direction G1en1erale de la Sant1e. Direction des Hôpitaux.
June 1997.
[2] Depecker P, Rusaouen G, Inard C. Study and comparison of two type
of air 5ow in operating rooms using a CFD code. In: Proceedings
of Building Simulation 95, IBPSA, Madison, USA.
[3] Tinker JA, Roberts D. Indoor air quality and infection problems in
operating theatres. Proceedings of EPIC 98:285–90.
[4] Chow T-T, Ward S, Liu J-P, Chan FC-K. Air5ow in hospital
operating theatre: the Hong Kong experience. In: Proceedings of
Healthy Buildings, vol. 2, 2000. p. 419–24.
[5] Air Liquide Sant1e. L’1ere de l’a1eraulique. HMH, June 2001.
[6] Awbi HB. Ventilation of buildings. London: E& FN Spon; 1991.
313pp.
[7] Air Liquide Sant1e. Dossier technique Exp Air. ed. ALS. 2001.
[8] Bruel & Kjaer. Multipoint Sampler and Doser Type 1303 Instructions
Manual. 1991.
[9] Laporthe S. Contribution aU la qualiJcation des systUemes de ventilation
des bâtiments: int1egration d’1el1ements perturbants. ThUese de doctorat,
INSA de Lyon, 2000. 237pp.
[10] ASHRAE Application Handbook ch 7: Health Care Facilities. 1999.
[11] Pfost JF. A Re-evaluation of laminar air 5ow in hospital operating
room. Ashrae Transactions 1981;87(2):729–39.
[12] Horworth FH. Prevention of airborne infection during surgery.
Ashrae Transactions 1985;91(1b):291–304.
[13] Horworth FH. Prevention of airborne infections in operating rooms.
Hospital Engineering 1986;40(8):17–23.
[14] Lewis JR. Operating room air distribution e6ectiveness. Ashrae
Transactions 1993;99(2):1191–200.
[15] Wecxsteen H, Kastally M, Woloszyn M, Virgone J, Laporthe S.
Travaux Exp1erimentaux en vue de Valider un Code de Description
des Ecoulements d’Air Int1erieur. Rapport Jnal, Convention Insavalor
- Air liquide, no 6715, 2000.
[16] Castanet S. Contribution a1 l’1etude de la ventilation et de la qualit1e de
l’air int1erieur des locaux. ThUese de doctorat, INSA de Lyon, 1998.
289pp.
[17] Laporthe S, Virgone J, Castanet S. Comparative study of two
Tracer Gas: SF6 and N2 O. Building and Environment 2001;36(3):
313–20.
[18] Patankar SV. Numerical heat transfer and 5uid 5ow. London:
McGraw-Hill; 1980.
[19] Champinot C, Till M, Philippe L, Perrin V. Numerical modeling as
a decision making tool. Verre 1999;5(2).
[20] Shamp D, Marin O, Champinot C, Jurcik B, Joshi M, Grosman R.
Oxy-fuel furnace design optimization using coupled combustion/glass
bath numerical simulation. Conference on Glass Problems, October
1998.
[21] Melen S. Validation du code EXP AIR v4.4. Air Liquide technical
repport, 2001.
[22] Launder BE, Spalding DB. Mathematical models of turbulence.
London: Academic Press; 1972.
[23] Melen S. Notice th1eorique DISPAL v4.0—logiciel de dispersion
tridimensionnelle. Air Liquide technical repport, 1997.
[24] Klein SA, Alvarado FL. EES: Engineering Equations Solver.
Copyright 1992–2001 [http://www.fchart.com].
1178
M. Woloszyn et al. / Building and Environment 39 (2004) 1171 – 1178
[25] Teodosiu, C. Mod1elisation des systUemes techniques dans le domaine
des e1 quipements de bâtiments aU l’aide des codes de type CFD. ThUese
de doctorat, INSA de Lyon, 2001. 355pp.
[26] Emvin P, Davidson L. A numerical comparison of three inlet
approximations of the di6user in case E1 annex 20. Proceedings
of the Fifth Roomvent Conference, vol. 1. Yokohama, Japan, 1996.
p. 219–37.
[27] Heikkinen J. Modeling of supply air terminal for room air 5ow
simulation. Proceedings of the 12th AIVC Conference, vol. 3.
Ottawa-Canada, 1991. p. 213–30.
[28] Fluent Inc, 5uent user’s guide, vol. 5.0. Lebanon—NH(USA): Fluent
Inc; 1998.