Adhesive Cementation of Indirect Composite Inlays and Onlays: A
advertisement

CONTINUING EDUCATION 2
INDIRECT COMPOSITE RESIN RESTORATIONS
Adhesive Cementation of Indirect Composite
Inlays and Onlays: A Literature Review
Camillo D’Arcangelo, DDS; Lorenzo Vanini, MD, DDS; Matteo Casinelli, DDS; Massimo Frascaria, DDS, PhD;
Francesco De Angelis, DDS, PhD; Mirco Vadini, DDS, PhD; and Maurizio D’Amario, DDS, PhD
LEARNING OBJECTIVES
Abstract: The authors conducted a literature review focused on materials and
techniques used in adhesive cementation for indirect composite resin restorations. It was based on English language sources and involved a search of online
databases in Medline, EMBASE, Cochrane Library, Web of Science, Google
Scholar, and Scopus using related topic keywords in different combinations; it
was supplemented by a traditional search of peer-reviewed journals and crossreferenced with the articles accessed. The purpose of most research on adhe-
đƫ %/1//ƫ !*0(ƫ $!/%2!ƫ
/5/0!)/ƫ".+)ƫ+0$ƫƫ
$%/0+.%(ƫ* ƫ1..!*0ġ 5ƫ
,!./,!0%2!
đƫ!4,(%*ƫ'!5ƫ %û!.!*!/ƫ
!03!!*ƫ2.%+1/ƫ $!/%2!ƫ
/5/0!)/Čƫ%*(1 %*#ƫ!0$ġ
* ġ.%*/!Čƫ/!("ġ!0$Čƫ* ƫ
/!("ġ $!/%2!
đƫ !/.%!ƫ0$!ƫ2.%+1/ƫ
sive systems has been to learn more about increased bond strength and simpli-
.!/%*ƫ!)!*0ƫ#.+1,/ƫ
fied application methods. Adherent surface treatments before cementation are
,+(5)!.%60%+*ƫ,.+!//
+. %*#ƫ0+ƫ
necessary to obtain high survival and success rates of indirect composite resin.
Each step of the clinical and laboratory procedures can have an impact on longevity and the esthetic results of
indirect restorations. Cementation seems to be the most critical step, and its long-term success relies on adherence to the clinical protocols. The authors concluded that in terms of survival rate and esthetic long-term
outcomes, indirect composite resin techniques have proven to be clinically acceptable. However, the correct
management of adhesive cementation protocols requires knowledge of adhesive principles and adherence to
the clinical protocol in order to obtain durable bonding between tooth structure and restorative materials.
T
he proliferation of resin composites and adhesive systems has met the increasing demand for esthetic restorations in both anterior and posterior teeth.1 Depending
on the respective clinical indication, resin composite
materials are suitable for both direct and indirect restorations.2 Although direct resin composites have replaced other
restorative options, there are a number of issues associated with
their use in the posterior region. These include: high polymerization shrinkage; gap formation; poor resistance to wear and tear;
color instability; and insufficient mechanical properties.3 Direct
restorations can result in contact area instability, difficulty in generating proximal contour and contact, lack of marginal integrity, and
postoperative sensitivity.4 All of these factors impact the longevity
and clinical success of restorations.5-7 Despite efforts to reduce the
566
COMPENDIUM
September 2015
issue of marginal infiltration associated with direct techniques, to
date, no method has produced acceptable results.8,9
Posterior indirect restorations are widely used in modern restorative dentistry to overcome the problems resulting from direct
techniques.2 The adhesive concepts that have been used for direct
restorative procedures are now being applied to indirect restorations and have been incorporated into daily practice.10 Indirect
composites offer an esthetic alternative to ceramics for posterior
teeth.10,11 The clinical performance of composite resin restorations is comparable to ceramic restorations, but the relatively low
cost associated with composites has resulted in increased use of
composite resin-based indirect restorations in the posterior region.12-14 Ceramic materials exhibit a very high elastic modulus, thus
they cannot absorb most of the occlusal forces. Since polymeric
Volume 36, Number 8
materials absorb a significant amount of occlusal stress, they should
be considered the material of choice.10,15
The success of adhesive restorations depends primarily upon the
luting agent and adhesive system.16 Several authors investigated the
properties of resin luting materials such as bond strength, degree of
conversion, and wear, in order to predict their clinical behavior.17-22
Among the parameters that may influence the clinical success of
indirect restorations is a proper degree of polymerization of the
resin luting agent, which should be taken into account.23 Moreover,
successful adhesion depends on proper treatment of the internal
surfaces of the restoration as well as the dentinal surface.2,16
This article discusses materials and techniques used in adhesive
cementation for indirect composite resin restorations.
The Adhesive Systems
A Historical Overview
Because the microscopic structure of two different contact surfaces
presents irregularities, an adherent is necessary. The introduction
of adhesive materials as alternatives to traditional retentive techniques has greatly revolutionized restorative dentistry.24 In the
development of dental adhesives, the ultimate goal is to achieve
strong, durable adhesion to dental hard tissues.25 In 1955, Buonocore showed how the treatment of enamel with phosphoric acid
increases the exposed enamel surface by producing micro-irregularities on it, resulting in improved adhesion potential. The modern
concept of enamel bonding can be traced to his published findings.26
In 1965, Bowen formulated the first generation of dentinal adhesive.27 The increasing interest in adhesion in dentistry led to the
development of four generations of adhesive systems, with the 4th
generation achieving good results for dentin bonding in the 1990s.28
Modern Adhesive Systems
The modern formulation of an enamel-dentin adhesive system
includes the following three components29:
Ċŋ Etchant—an organic acid with the function of demineralizing the
surface, dissolving hydroxyapatite crystals, and increasing free
surface energy.
Ċŋ Primer—an amphiphilic compound that increases the wettability of the hydrophilic substrate (dentin) to a hydrophobic agent
(bonding or resin).
Ċŋ Bonding agent—a fluid resin used to penetrate the etched and primed
substrate and, after curing, to create a real and stable adhesive bond.
In order to obtain an optimal infiltration of enamel and dentin substrates, the ideal features of an adhesive material are: low
viscosity; high superficial tension; and effective wettability. The
fundamental requisite is wettability, which depends on the intrinsic
properties of fluid and dental substrate.30
The classification of the respective adhesive systems is based on
their etching characteristics and the number of steps they require.31
Etch-and-Rinse Systems—The etch-and-rinse technique is characterized by the etching of the enamel and/or dentin with an acid
agent (orthophosphoric acid at 35% to 37%), which needs to be subsequently washed away. The etch-and-rinse adhesive systems can be
www.compendiumlive.com
further classified into three-step and two-step systems. Three-step
systems require separate etching, priming, and bonding. Two-step
adhesives are instead characterized by an application of an etching
compound and then an agent that combines a primer and a bonding.
The etching application removes the smear plugs, demineralizes the
dentin, and exposes the intertubular dentin collagen fibers, obtaining
an ideal micromechanical anchor for the adhesive.32,33
Self-Etch Systems—Self-etch refers to an adhesive system that
dissolves the smear layer and infiltrates it at the same time, without
a separate etching step.31 The self-etch adhesives have been further
classified into two-step systems and one-step systems, which simultaneously provide etching, priming, and bonding.34
Self-Adhesive Systems—In the past few years, new resin cements,
so-called “self adhesives,” have been introduced. This particular
resin cement needs only to be applied on tooth substrate, without
any etching, priming, or bonding phases.35
Tooth Preparation
After caries and/or failed restoration removal, a cavity with slightly
occlusal divergent walls (5° to 15°) and round internal angles is
prepared by using decreasing grit (from 60–70 µm to 15–20 µm grit)
cylindrical round-ended diamond burs. Preparation margins are not
bevelled but prepared via butt joint.2 After cavity preparation and
before cavity finishing, adhesive procedures are performed36 using
a rubber dam in order to achieve an immediate dentin sealing.37,38
In keeping with rubber dam placement for subsequent restoration
placement, the interproximal margin must be supragingival. To
avoid a dual marginal leakage, no direct composite is used for gingival margin rebuilding.39 If any deep subgingival margin persists after
cavity preparation—thus precluding proper rubber dam placement—
the feasibility of a surgical crown-lengthening procedure and/or an
orthodontic extrusion must be considered.40 A light-curing composite filling material is used to block out defect-related undercuts.2,41
The finishing phases are performed with diamond burs with a slight
taper and with silicone points (Table 1). The teeth are protected with
temporary eugenol-free restorations after impression making.42
TABLE 1
Tooth Preparation Phases for
Indirect Composite Resin
TOOTH PREPARATION
đƫ !.!/%*#ƫ#.%0ƫĨ".+)ƫćĀĢĈĀƫµ)ƫ0+ƫāĆĢĂĀƫµ)ƫ#.%0ĩƫ
5(%* .%(ƫ.+1* ġ!* ! ƫ %)+* ƫ1./
đƫ (%#$0(5ƫ+(1/(ƫ %2!.#!*0ƫ3((/ƫĨĆŋƫ0+ƫāĆŋĩ
đƫ +1* ƫ%*0!.*(ƫ*#(!/
đƫ 100ƫ&+%*0ƫ,.!,.0%+*ƫ).#%*/
đƫ ))! %0!ƫ !*0%*ƫ/!(%*#ƫ1/%*#ƫ $!/%2!ƫ,.+! 1.!ƫ
* ƫ.1!.ƫ )
đƫ (+'%*#ƫ+10ƫ !"!0ġ.!(0! ƫ1* !.10/
đƫ %*%/$%*#ƫ3%0$ƫ %)+* ƫ1./ƫ* ƫ/%(%+*!ƫ,+%*0/
September 2015
COMPENDIUM
567
CONTINUING EDUCATION 2 | ƫƫƫ
Dentin Treatments
Research on adhesive systems is focused mainly on increasing bond
strength and simplifying application. The application of phosphoric
acid increases the surface energy of the dentin by removing the
smear layer and promoting demineralization of surface hydroxyapatite crystals. The resin monomers, by means of the primer
agent’s amphiphilic properties, infiltrate the water-filled spaces
between collagen fibers, which results in a “hybrid layer” composed
of collagen, resin, residual hydroxyapatite, and traces of water. It
results in an ideal micromechanical anchor substrate for adhesive
systems on dentin.16,43,44
Immediate dentin sealing (IDS) is a strategy in which a dentin
bonding agent is applied to freshly cut dentin and polymerized
before making an impression.45 The recommended technique focuses on the use of the “etch-and-rinse” systems. Etching should
extend slightly over enamel to ensure the conditioning of the entire
dentin surface. The use of either two-step or three-step dentin
bonding agents is equally effective. Self-priming resins, however,
generate a more excess resin layer, which may extend over the
margin and require additional bur corrections. IDS can be immediately followed by the placement of composite in order to block
out eventual undercuts and/or build up deep cavities, reducing
restoration thickness and ensuring the light-cured polymerization
of the luting agent. Finally, enamel margins are usually reprepared
before final impression to remove excess adhesive resin and provide ideal taper.45
When the preparation exposes no dentinal areas—eg, in
TABLE 2
Suggested Treatment for the Internal
Surfaces of Indirect Restorations
COMPOSITE RESTORATION SURFACE TREATMENTS
đƫ % ƫ!0$%*#
đƫ * (/0%*#ƫ3%0$ƫ(1)%*1)ƫ+4% !
đƫ %(*!ƫ+1,(%*#
đƫ .%+$!)%(ƫ+0%*#
đƫ /!.ƫ0.!0)!*0
veneered indirect restorations—neither immediate dentin sealing nor primer agent applications are necessary, since the etching
and bonding phases ensure an optimal bond for enamel adhesion.46
Immediate dentin sealing should be followed by air blocking and
pumicing to generate ideal impressions.47 In-vitro studies have
shown increased bond strength for IDS versus delayed dentin
sealing (DDS) techniques.48-52 The IDS technique also eliminates
any concerns regarding the film thickness of the dentin sealant and
protects dentin against bacterial leakage and sensitivity during
the provisional phase of treatment.45 Moreover, it was suggested
that multiple adhesive coatings can improve the quality of resindentin bonds.53
Surface Treatments for Composite Restorations
Several techniques have been suggested for increasing bond
strength, involving treating the internal surfaces of indirect restorations (Table 2).54,55 The surface treatments aim not only to
achieve a high retentive bond strength of the restoration, but also
to avoid any microbiological leakage.56 Composite surface treatments are necessary for adhesion of indirect composite restorations.57 Acid-etching with phosphoric acid, acidulated phosphate
fluoride, or hydrofluoric (HF) acid is one of the treatments reported
in literature.58-60
The internal surfaces of indirect restorations can be abraded with aluminium oxide, using an intraoral sandblasting device.58,59,61-63 Also, silane coupling agents are used as adhesion promoters.64,65 Another method, the tribochemical coating, forms a
silica-modified surface as a result of airborne-particle abrasion
with silicon dioxide (SiO2)-coated aluminium particles. The surface becomes chemically reactive to the resin by means of silane
coupling agents.63,66,67
Many studies show that Er:YAG laser treatment enhances bond
strength between composite and resin cement.68,69 Other studies
demonstrate no influence of laser treatment on bond strength.67,70
Roughening the composite area of adhesion, sandblasting, or
both sandblasting and silanizing can provide statistically significant
additional resistance to tensile load. Acid-etching with silane treatment does not reveal significant changes in tensile bond strength.
Sandblasting treatment is the main factor responsible in improving the retentive properties of indirect composite restorations.57
wTABLE 3
Recommended Clinical Protocol, According to Review Outcomes
DENTIN SURFACE
TREATMENT
COMPOSITE SURFACE
TREATMENT
CEMENTATION
))! %0!ƫ !*0%*ƫ/!(%*#ƫ
1/%*#ƫƫ0$.!!ġ/0!,Čƫ0+0(ġƫ
!0$ƫ !*0%*ġ+* %*#ƫ#!*0ƫ
3%0$ƫƫü((! ƫ $!/%2!ƫ.!/%*ƫ
* ƫ.1!.ƫ )ƫ%/+(0%+*
+"0ġ/* (/0%*#ƫ
ĨĆĀµ)ƫ(Ăăƫ1/%*#ƫ
*ƫ%*0.+.(ƫ/* (/0ġ
%*#ƫ !2%!ƫ0ƫĂƫ.ƫ
,.!//1.!ĩƫ./%+*ƫ+"ƫ
0$!ƫ+),+/%0!ƫ%*0!.*(ƫ
/1."!/ƫ
đƫ +*/0*0(5ƫ1/%*#ƫ.1!.ƫ )ƫ%/+(0%+*ƫ3%0$ƫ0$.!!ġ/0!,Čƫ
0+0(ġ!0$Čƫ(%#$0ġ1.! ƫ!)!*0ƫ/5/0!)
568
COMPENDIUM
September 2015
đƫ .!$!0%*#ƫ0$!ƫ(%#$0ġ1.! ƫ+),+/%0!ƫ.!/%*ƫ!)!*0
đƫ !)+2%*#ƫ.!/% 1(ƫ!)!*0ƫ1/%*#ƫ!4,(+.!.Čƫ/(,!(/Čƫ
* ƫý+//ƫ!"+.!ƫ+),(!0!ƫ,+(5)!.%60%+*ƫ* ƫāĆƫ
/(,!(ƫ"0!.ƫ,+(5)!.%60%+*
Volume 36, Number 8
Cementation
Resin cements are divided into three groups according to polymerization process: chemically activated cements, light-cured cements, and dual-cured cements.16,71 Of the three, light-cured resin
cements have the clinical advantages of longer working time and
better color stability, but curing time, restoration thickness, and
overlay material significantly influence the microhardness of the
resin composites employed as luting agents.46,72
Dual-cured resin cements have the advantages of controlled
working time and adequate polymerization in areas that are inaccessible to light. Conversely, they are relatively difficult to handle.23,73,74 Photoactivation increases the degree of conversion and
surface hardness of dual-cured cements.75
Optimal luting of indirect restorations is dependent on the light
source power, irradiation time, and dual-cure luting cement or
light-curing composite chosen. Curing should be calibrated for
each material to address high degrees of conversion. Preheating
light-cured filled composites allows the materials to reach optimal
fluidity.76-78 The suggested temperature for composite preheating
is 39°C.79 The necessary working time for positioning the indirect
restorations and removing the excess cement can be extended at
the discretion of the clinician, using a light-curing composite as
luting agent, thus overcoming the relatively restricted working
time allowed by dual-cure cements.2
Total-etching of dentin substrate is recommended as the first
step for the two- and three-step adhesive systems.80 To reduce the
number of operative steps and to simplify the clinical procedures,
self-etching adhesive systems, which do not require a separate
acid-etching step, have been introduced.81 Literature reports demonstrate that multi-bottle systems with simultaneous etching and
rinsing show superior in-vitro and in-vivo activities compared to
the new all-in-one systems.44,82
The self-adhesive resins may be considered an alternative for
luting indirect composite restorations onto non-pretreated dentin
surfaces,83 even if bond strengths are lower than etch-and-rinse
systems.84,85 The etch-and-rinse technique provides more reliable
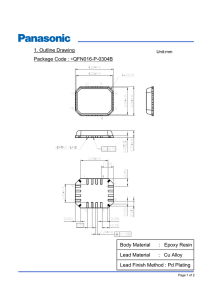
Fig 1.
Fig 2.
Fig 3.
Fig 4.
Fig 1. ƫ)* %1(.ƫü./0ƫ)+(.Čƫ3%0$ƫƫ".01.! ƫ+),+/%0!ƫ.!/0+.0%+*čƫ2%05ƫ,.!,.0%+*ċƫFig 2.ƫ))! %0!ƫ !*0%*ƫ/!(%*#ċƫFig 3.ƫ!)!*00%+*ƫ+"ƫ
*ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*ċƫFig 4.ƫ+/0+,!.0%2!ƫ2%!3ċ
www.compendiumlive.com
September 2015
COMPENDIUM
569
CONTINUING EDUCATION 2 | ƫƫƫ
bonding compared to self-etch luting agents and self-adhesive
luting agents when used to bond indirect composite restorations
to dentin.22,86-88
The constant use of rubber dam isolation is necessary for the
cementation protocol with adhesive systems. Removing residual
cement using explorers, scalpels, and floss before complete polymerization, and a 15c scalpel after polymerization, is recommended
in order to avoid compromising restoration marginal accuracy,
compared to the use of burs, discs, or strips (Table 3).2
An appropriate treatment of the fitting surface of the resin composite restoration and dentin substrate is necessary to establish
a strong and durable bond.57
It is recommended that the freshly cut dentin surfaces be sealed
with a dentin bonding agent immediately following tooth preparation, before taking impression.45 Immediate dentin sealing results in a high bond strength for total-etch and self-etch adhesives;
however, the microleakage is similar to that with conventional
cementation techniques.49
When following a protocol of cementation using an adhesive
system, constant rubber dam isolation and careful hand finishDiscussion and Conclusions
Resin-based composites give predictable results in teeth res- ing are necessary to provide predictable clinical results (Figure
toration with respect to both mechanical and
1 through Figure 4).2
esthetic properties when they are used as indiSupragingival margins facilitate impression
Resin cements are
rect restoration materials.2 Indirect composites
making, definitive restoration placement, and
make it possible to overcome some shortcomdetection of secondary caries.94 In addition,
divided into three
ings of direct techniques. Indirect restorations—
some studies have demonstrated that subgingroups according to
ie, those created outside of the mouth—result
gival restorations are associated with higher
in better proximal and occlusal contacts, better
levels of gingival bleeding, attachment loss, and
polymerization
wear and marginal leakage resistance, and engingival recession than supragingival restoraprocess: chemically
hancement of mechanical properties compared
tions.95,96 Therefore, in all cases where rubber
6,85
to direct techniques.
dam cannot be adequately placed, surgical
activated cements,
Since the dentin substrate has a high organic
crown lengthening or orthodontic extrusion
light-cured cements,
content, tubular structure variations, and the
should be taken into account. Otherwise, trapresence of outward fluid movement, bonding
ditionally cemented restorations are preferable
and dual-cured
to dentin is a less reliable technique when comto the use of adhesive procedures.
cements.
pared to enamel bonding.89,90 Bonding composite
Sandblasting of the composite surfaces has
restorations to tooth structure involves the denbeen recommended as a predictable means for
tin/adhesive-cement interface and composite
enhancing the retention between resin cements
restorations/cement interface.22
and indirect composite restorations.57,97 The apEach step of the clinical and laboratory procedures can have plication of an appropriately selected adhesive material with proper
an impact on the esthetic results and longevity of indirect resto- technique will ensure predictable results and successful long-term
rations.91 Cementation is the most critical step and involves the clinical outcomes.
application of both the adhesive system and resin luting agent.92,93
Modified United States Public Health Service criteria are the
most complete and commonly used assessment techniques in cliniFig 5.
cal trials on indirect composite restorations.37,98
XƫD’Arcangelo, et al, 2014 Ă
QƫManhart, et al, 2001 āĀĀ
ć
āĀā
As shown in Figure 5, restorations were evaluated at baseline and
ƫBarone, et al, 2008
Oƫeirskar, et al, 1999
VƫHuth, et al, 2011 ĊĊ
ƫScheibenbogen-Fuchsbrunner, et al, 1999 102
after a follow-up period for secondary caries, marginal adaptation,
marginal discoloration, color match, anatomic form, surface rough100
O
ness, endodontic complications, fracture of the restoration, fracture
90
X of the tooth, and retention of the restoration.2,6,99-102 In many of the
V
80
reported follow-up studies, indirect restorative procedures were
70
carried out by dental students,99-102 and the main reasons for failures during the observation period seemed to be secondary caries,
60
endodontic
complications, and fractures.1,2
50
The literature sources support the clinical acceptability of
40
indirect composite resin techniques regarding survival rate and
30
esthetic outcomes at up to 10 years’ follow-up.1,103 Adhesive cemen20
tation is a complex procedure that requires knowledge of adhesive
10
principles and adherence to the clinical protocol in order to obtain
durable bonding between tooth structure and restorative material.
0%
24 months
36 months
48 months
60 months
Fig 5. 1.2%2(ƫ.0!ƫ+"ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*/ƫ.!,+.0! ƫ%*ƫ
.!"!.!*!/ƫĂČƫćČƫĊĊġāĀĂċƫ$!ƫ/1.2%2(ƫ.0!ƫĨŌĩƫ%/ƫ(1(0! ƫ+*/% !.%*#ƫ
0$!ƫƫ.%0!.%ċƫ
570
COMPENDIUM
September 2015
DISCLOSURE
The authors had no disclosures to report.
Volume 36, Number 8
ABOUT THE AUTHORS
Camillo D’Arcangelo, DDS
Department of Restorative Dentistry, School of Dentistry, University G. D’Annunzio Chieti, Italy
Lorenzo Vanini, MD, DDS
Private Practice, Chiasso, Switzerland
Matteo Casinelli, DDS
Unit of Restorative Dentistry, Department of Life, Health and Environmental
Sciences, School of Dentistry, University of L’Aquila, L’Aquila, Italy
Massimo Frascaria, DDS, PhD
Unit of Restorative Dentistry, Department of Life, Health and Environmental
Sciences, School of Dentistry, University of L’Aquila, L’Aquila, Italy
Francesco De Angelis, DDS, PhD
Department of Restorative Dentistry, School of Dentistry, University G. D’Annunzio Chieti, Italy
Mirco Vadini, DDS, PhD
Department of Restorative Dentistry, School of Dentistry, University G. D’Annunzio Chieti, Italy
Maurizio D’Amario, DDS, PhD
Unit of Restorative Dentistry, Department of Life, Health and Environmental
Sciences, School of Dentistry, University of L’Aquila, L’Aquila, Italy
Queries to the author regarding this course may be submitted to
authorqueries@aegiscomm.com.
REFERENCES
1. $+. .1,ƫČƫ/% +.ƫČƫ®./0! ġ%* /(!2ƫċƫƫ,.+/,!0%2!ƫ(%*%(ƫ/01 5ƫ
+"ƫ%* %.!0ƫ* ƫ %.!0ƫ+),+/%0!ƫ* ƫ!.)%ƫ%*(5/čƫ0!*ġ5!.ƫ.!/1(0/ċƫ
Quintessence IntċƫĂĀĀćĎăĈĨĂĩčāăĊġāąąċ
2. Ě.*#!(+ƫČƫ.+3ƫČƫ!ƫ*#!(%/ƫČƫ!0ƫ(ċƫ%2!ġ5!.ƫ.!0.+/,!0%2!ƫ
(%*%(ƫ/01 5ƫ+"ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*/ƫ(10! ƫ3%0$ƫƫ(%#$0ġ1.! ƫ
+),+/%0!ƫ%*ƫ,+/0!.%+.ƫ0!!0$ċƫClin Oral InvestigċƫĂĀāąĎāĉĨĂĩčćāĆġćĂąċ
3. *$.0ƫ
Čƫ1*6!()**ƫČƫ$!*ƫČƫ%'!(ƫċƫ!$*%(ƫ,.+,!.ġ
0%!/ƫ* ƫ3!.ƫ!$2%+.ƫ+"ƫ(%#$0ġ1.! ƫ,'(!ƫ+),+/%0!ƫ.!/%*/ċƫDent
MaterċƫĂĀĀĀĎāćĨāĩčăăġąĀċ
4. !* +*`ƫ
Čƫ!0+ƫČƫ*0%#+ƫČƫ!0ƫ(ċƫ%.!0ƫ.!/%*ƫ+),+/%0!ƫ
.!/0+.0%+*/ƫ2!./1/ƫ%* %.!0ƫ+),+/%0!ƫ%*(5/čƫ+*!ġ5!.ƫ.!/1(0/ċƫJ Contemp Dent PractċƫĂĀāĀĎāāĨăĩčĂĆġăĂċ
5. !1.0/!*ƫċƫ%++),0%%(%05ƫ+"ƫ.!/%*ġ)+ %ü! ƫü((%*#ƫ)0!.%(/ċƫCrit
Rev Oral Biol MedċƫĂĀĀĀĎāāĨăĩčăăăġăĆĆċ
6. .+*!ƫČƫ!.$%ƫČƫ+//%ƫČƫ!0ƫ(ċƫ+*#%01 %*(ƫ(%*%(ƫ!2(1ġ
0%+*ƫ+"ƫ+* ! ƫ+),+/%0!ƫ%*(5/čƫƫăġ5!.ƫ/01 5ċƫQuintessence Intċƫ
ĂĀĀĉĎăĊĨāĩčćĆġĈāċ
7. %/ƫČƫ!,.%*!ƫ
Čƫ$+.0((ƫČƫ!0ƫ(ċƫ%#$ƫ%.. %*!ƫ1.%*#ƫ* ƫ
*+)(%!/ƫ+"ƫ!4,+/1.!ƫ.!%,.+%05ƫ(3ƫ%*ƫ.!/%*ġ/! ƫ)0!.%(/ċƫJ Dentċƫ
ĂĀāāĎăĊĨĉĩčĆąĊġĆĆĈċ
8. $+*!)**ƫČƫ! !.(%*ƫČƫ$)(6ƫČƫ.1* (!.ƫċƫ+0(ƫ+* %*#ƫ2/ƫ
/!(!0%2!ƫ+* %*#čƫ).#%*(ƫ ,00%+*ƫ+"ƫ(//ƫĂƫ+),+/%0!ƫ.!/0+.ġ
0%+*/ċƫOper DentċƫāĊĊĊĎĂąĨĆĩčĂćāġĂĈāċ
9. +#1!.%+ƫČƫ(!//* .ƫČƫ66++ƫČƫ!0ƫ(ċƫ%.+(!'#!ƫ%*ƫ
(//ƫƫ+),+/%0!ƫ.!/%*ƫ.!/0+.0%+*/čƫ0+0(ƫ+* %*#ƫ* ƫ+,!*ƫ/* 3%$ƫ
0!$*%-1!ċƫJ Adhes DentċƫĂĀĀĂĎąĨĂĩčāăĈġāąąċ
10.ƫ* %*%ƫċƫ* %.!0ƫ.!/%*ƫ+),+/%0!/ċƫJ Conserv DentċƫĂĀāĀĎāăĨąĩčƫ
āĉąġāĊąċ
11.ƫ.!/*%#0ƫČƫ('ƫČƫ6*ƫċƫ* +)%6! ƫ(%*%(ƫ0.%(ƫ+"ƫ%* %.!0ƫ
.!/%*ƫ+),+/%0!ƫ* ƫ!.)%ƫ2!*!!./čƫ1,ƫ0+ƫăġ5!.ƫ"+((+3ġ1,ċƫJ Adhes
DentċƫĂĀāăĎāĆĨĂĩčāĉāġāĊĀċ
12.ƫ(*'ƫ
ċƫ%!*0%ü((5ƫ/! ƫ.0%+*(!ƫ* ƫ,.+0++(ƫ"+.ƫ1/!ƫ+"ƫ)+ ġ
!.*ƫ%* %.!0ƫ.!/%*ƫ%*(5/ƫ* ƫ+*(5/ċƫJ Esthet DentċƫĂĀĀĀĎāĂĨąĩčāĊĆġĂĀĉċ
13.ƫ)((ƫċƫ0!.%(ƫ$+%!ƫ"+.ƫ.!/0+.0%2!ƫ !*0%/0.5čƫ%*(5/Čƫ+*(5/Čƫ
www.compendiumlive.com
.+3*/Čƫ* ƫ.% #!/ċƫGen DentċƫĂĀĀćĎĆąĨĆĩčăāĀġăāĂċ
14.ƫ5'!*0ƫČƫ+* !)ƫČƫ65!/%(ƫČƫ!0ƫ(ċƫû!0ƫ+"ƫ %û!.!*0ƫü*%/$%*#ƫ
0!$*%-1!/ƫ"+.ƫ.!/0+.0%2!ƫ)0!.%(/ƫ+*ƫ/1."!ƫ.+1#$*!//ƫ* ƫ0!ġ
.%(ƫ $!/%+*ċƫJ Prosthet DentċƫĂĀāĀĎāĀăĨąĩčĂĂāġĂĂĈċ
15.ƫ!%*"!( !.ƫċƫ* %.!0ƫ,+/0!.%+.ƫ+),+/%0!ƫ.!/%*/ċƫCompend Contin
Educ DentċƫĂĀĀĆĎĂćĨĈĩčąĊĆġĆĀăċ
16.ƫ*0+/ƫƫ
.Čƫ*0+/ƫ
Čƫ%6'((ƫċƫ $!/%2!ƫ!)!*00%+*ƫ+"ƫ!0$ġ
(!ƫ!.)%ƫ!/0$!0%ƫ.!/0+.0%+*/ċƫJ Can Dent AssocċƫĂĀĀĊĎĈĆĨĆĩčăĈĊġăĉąċ
17.ƫ/$(!5ƫČƫ%1$%ƫČƫ*+ƫČƫ!0ƫ(ċƫ+* ƫ/0.!*#0$ƫ2!./1/ƫ !*0%*!ƫ
/0.101.!čƫƫ)+ !((%*#ƫ,,.+$ċƫArch Oral BiolċƫāĊĊĆĎąĀĨāĂĩčāāĀĊġāāāĉċ
18.ƫ*ƫ!!.!!'ƫČƫ!. %#Y+ƫ
Čƫ).!$0/ƫČƫ*$!.(!ƫċƫ$!ƫ(%*%(ƫ
,!."+.)*!ƫ+"ƫ $!/%2!/ċƫJ DentċƫāĊĊĉĎĂćĨāĩčāġĂĀċ
19.ƫ(00ƫ
ċƫ!/%*ƫ!)!*0/čƫ%*0+ƫ0$!ƫĂā/0ƫ!*01.5ċƫCompend Contin
Educ DentċƫāĊĊĊĎĂĀĨāĂĩčāāĈăġāāĉĂċ
20.ƫ.#ƫČƫ!/.ƫČƫ+*6#ƫċƫ!$*%(ƫ,.+,!.0%!/ƫ+"ƫ
.!/%*ƫ!)!*0/ƫ3%0$ƫ %û!.!*0ƫ0%20%+*ƫ)+ !/ċƫJ Oral Rehabilċƫ
ĂĀĀĂĎĂĊĨăĩčĂĆĈġĂćĂċ
21.ƫ.!/$%ƫČƫ66+*%ƫČƫ1##!.%ƫČƫ!0ƫ(ċƫ!*0(ƫ $!/%+*ƫ.!2%!3čƫ#ġ
%*#ƫ* ƫ/0%(%05ƫ+"ƫ0$!ƫ+* ! ƫ%*0!."!ċƫDent MaterċƫĂĀĀĉĎĂąĨāĩčĊĀġāĀāċ
22.ƫĚ.*#!(+ƫČƫ!ƫ*#!(%/ƫČƫĚ).%+ƫČƫ!0ƫ(ċƫ$!ƫ%*ý1!*!ƫ
+"ƫ(10%*#ƫ/5/0!)/ƫ+*ƫ0$!ƫ)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ !*0%*ƫ0+ƫ
%* %.!0ƫ.!/%*ġ/! ƫ+),+/%0!ƫ* ƫ!.)%ƫ.!/0+.0%+*/ċƫOper Dentċƫ
ĂĀĀĊĎăąĨăĩčăĂĉġăăćċ
23.ƫĚ.*#!(+ƫČƫ!ƫ*#!(%/ƫČƫ %*%ƫČƫ!0ƫ(ċƫ*ý1!*!ƫ+"ƫ1.%*#ƫ
0%)!Čƫ+2!.(5ƫ)0!.%(ƫ* ƫ0$%'*!//ƫ+*ƫ0$.!!ƫ(%#$0ġ1.%*#ƫ+),+/ġ
%0!/ƫ1/! ƫ"+.ƫ(10%*#ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*/ċƫJ Adhes Dentċƫ
ĂĀāĂĎāąĨąĩčăĈĈġăĉąċ
24.ƫ+1(!0ƫ
ċƫƫ3+.( ƫ3%0$+10ƫ $!/%+*ĕƫJ Adhes DentċƫĂĀĀāĎăĨĂĩčāāĊċ
25.ƫ'!)1.ƫČƫ* +ƫċƫƫ.!2%!3ƫ+"ƫ+1.ƫ !2!(+,)!*0ƫ+"ƫ !*0(ƫ $!ġ
/%2!/Ģ!û!0/ƫ+"ƫ. %(ƫ,+(5)!.%60%+*ƫ%*%0%0+./ƫ* ƫ $!/%2!ƫ)+*+ġ
)!./ƫ+*ƫ $!/%+*ċƫDent Mater JċƫĂĀāĀĎĂĊĨĂĩčāĀĊġāĂāċ
26.ƫ1+*++.!ƫċƫƫ/%),(!ƫ)!0$+ ƫ+"ƫ%*.!/%*#ƫ0$!ƫ $!/%+*ƫ+"ƫ.5(ġ
%ƫü((%*#ƫ)0!.%(/ƫ0+ƫ!*)!(ƫ/1."!/ċƫJ Dent ResċƫāĊĆĆĎăąĨćĩčĉąĊġĉĆăċ
27.ƫ+3!*ƫċƫ $!/%2!ƫ+* %*#ƫ+"ƫ2.%+1/ƫ)0!.%(/ƫ0+ƫ$. ƫ0++0$ƫ0%/ġ
/1!/ċƫăċƫ+* %*#ƫ0+ƫ !*0%*ƫ%),.+2! ƫ5ƫ,.!ġ0.!0)!*0ƫ* ƫ0$!ƫ1/!ƫ+"ƫ
/1."!ġ0%2!ƫ+)+*+)!.ċƫJ Dent ResċƫāĊćĆĎąąĨĆĩčĊĀăġĊĀĆċ
28.ƫ+1(!0ƫ
ċƫ++(ġ,.++"ƫ $!/%2!/ĕƫJ Adhes DentċƫĂĀĀĂĎąĨāĩčăċ
29.ƫ*ƫ!!.!!'ƫČƫ!ƫ1*'ƫ
Čƫ00.ƫČƫ!0ƫ(ċƫ%.+0!*/%(!ƫ+* ƫ
/0.!*#0$/ƫ+"ƫ*ƫ!0$ƫĒƫ.%*/!ƫ* ƫ/!("ġ!0$ƫ $!/%2!ƫ0+ƫ!*)!(ƫ* ƫ !*ġ
0%*ƫ/ƫƫ"1*0%+*ƫ+"ƫ/1."!ƫ0.!0)!*0ċƫOper DentċƫĂĀĀăĎĂĉĨĆĩčćąĈġććĀċ
30.ƫ1//$!.ƫ
Čƫ !ƫ
+*#ƫČƫ2*ƫ!(0ƫČƫ.!* /ƫ
ċƫ$!ƫ/1."!ƫ".!!ƫ
!*!.#5ƫ+"ƫ$1)*ƫ !*0(ƫ!*)!(ċƫBiomater Med Devices Artif Organsċƫ
āĊĉąĎāĂĨāġĂĩčăĈġąĊċ
31.ƫ*ƫ!!.!!'ƫČƫ!ƫ1*'ƫ
Čƫ+/$% ƫČƫ!0ƫ(ċƫ1+*++.!ƫ)!)+.%(ƫ
(!01.!ċƫ $!/%+*ƫ0+ƫ!*)!(ƫ* ƫ !*0%*čƫ1..!*0ƫ/001/ƫ* ƫ"101.!ƫ$(ġ
(!*#!/ċƫOper DentċƫĂĀĀăĎĂĉĨăĩčĂāĆġĂăĆċ
32.ƫ/$(!5ƫČƫ.2($+ƫċƫ!*0%*!ƫ,!.)!%(%05ƫ* ƫ !*0%*!ƫ $!ġ
/%+*ċƫJ DentċƫāĊĊĈĎĂĆĨĆĩčăĆĆġăĈĂċ
33.ƫ!...%ƫČƫ#% %+ƫČƫ/+*ƫċƫ%.+)+.,$+(+#%ƫ.!(0%+*ġ
/$%,ƫ!03!!*ƫ.!/%*ƫ* ƫ !*0%*ƫ%*ƫ(//ƫƫ.!/0+.0%+*/čƫ*ƫ%*ƫ2%2+ƫ* ƫ%*ƫ
2%0.+ƫ%*2!/0%#0%+*ƫ5ƫ/**%*#ƫ!(!0.+*ƫ)%.+/+,5ċƫQuintessence Intċƫ
āĊĊąĎĂĆĨāĂĩčĉćāġĉććċ
34.ƫ.!/$%ƫČƫ!. %#Y+ƫ
Čƫ+,!/ƫČƫ!0ƫ(ċƫ+.,$+(+#%(ƫ/01 5ƫ
+"ƫ.!/%*ġ !*0%*ƫ+* %*#ƫ3%0$ƫƫ* ƫ%*ġ(!*/ƫċƫAm J Dentċƫ
ĂĀĀăĎāćĨąĩčĂćĈġĂĈąċ
35.ƫ0+*ƫČƫ+.#!/ƫČƫ+*0!/ƫČƫ!0ƫ(ċƫû!0ƫ+"ƫ,+(5.5(%ƫ% ƫ
+*ƫ0$!ƫ%*0!."!ƫ* ƫ+* ƫ/0.!*#0$ƫ+"ƫ/!("ġ $!/%2!ƫ.!/%*ƫ!)!*0/ƫ0+ƫ
!*0%*ċƫJ Adhes DentċƫĂĀāăĎāĆĨăĩčĂĂāġĂĂĈċ
36.ƫ!%*06!ƫċƫ5/0!)0%ƫ.!2%!3/čƫċƫ$!ƫ+..!(0%+*ƫ!03!!*ƫ(+ġ
.0+.5ƫ0!/0/ƫ+*ƫ).#%*(ƫ-1(%05ƫ* ƫ+* ƫ/0.!*#0$ċƫċƫ$!ƫ+..!(ġ
0%+*ƫ!03!!*ƫ).#%*(ƫ-1(%05ƫ* ƫ(%*%(ƫ+10+)!ċƫJ Adhes Dentċƫ
ĂĀĀĈĎĊĨ/1,,(ƫāĩčĈĈġāĀćċ
37.ƫ%'!(ƫČƫ+1(!0ƫ
Čƫ5*!ƫČƫ!0ƫ(ċƫ!+))!* 0%+*/ƫ"+.ƫ+* 10ġ
%*#ƫ+*0.+((! ƫ(%*%(ƫ/01 %!/ƫ+"ƫ !*0(ƫ.!/0+.0%2!ƫ)0!.%(/ċƫClin Oral
InvestigċƫĂĀĀĈĎāāĨāĩčĆġăăċ
38.ƫ!.1#%ƫČƫ!...+ƫČƫ+%)+ƫċƫ))! %0!ƫ !*0%*ƫ/!(%*#ƫ%*ƫ%* %.!0ƫ
September 2015
COMPENDIUM
571
CONTINUING EDUCATION 2 | ƫƫƫ
.!/0+.0%+*/ƫ+"ƫ !*0(ƫ".01.!/ƫ%*ƫ,! %0.%ƫ !*0%/0.5ċƫEur J Paediatr
DentċƫĂĀāăĎāąĨĂĩčāąćġāąĊċ
39.ƫ%!0/$%ƫČƫ(/1.#$ƫČƫ.!&%ƫČƫ2% /+*ƫċƫ*ƫ2%0.+ƫ!2(10%+*ƫ+"ƫ
).#%*(ƫ* ƫ%*0!.*(ƫ ,00%+*ƫ"0!.ƫ+(1/(ƫ/0.!//%*#ƫ+"ƫ%* %.!0ƫ
(//ƫƫ+),+/%0!ƫ.!/0+.0%+*/ƫ3%0$ƫ %û!.!*0ƫ.!/%*+1/ƫ/!/ċƫEur J Oral
SciċƫĂĀĀăĎāāāĨāĩčĈăġĉĀċ
40.ƫ !ƫ(ƫČƫ/0!((1%ƫċƫ$!ƫ%),+.0*!ƫ+"ƫ.!/0+.0%2!ƫ).#%*ƫ
,(!)!*0ƫ0+ƫ0$!ƫ%+(+#%ƫ3% 0$ƫ* ƫ,!.%+ +*0(ƫ$!(0$ċƫ.0ƫċƫInt J
Periodontics Restorative DentċƫāĊĊąĎāąĨāĩčĈĀġĉăċ
41.ƫ106ƫČƫ.!&%ƫČƫ( !*1.#ƫċƫ(%)%*0%+*ƫ+"ƫ,+(5)!.%60%+*ƫ
/0.!//!/ƫ0ƫ0$!ƫ).#%*/ƫ+"ƫ,+/0!.%+.ƫ+),+/%0!ƫ.!/%*ƫ.!/0+.0%+*/čƫƫ
*!3ƫ.!/0+.0%2!ƫ0!$*%-1!ċƫQuintessence IntċƫāĊĉćĎāĈĨāĂĩčĈĈĈġĈĉąċ
42.ƫ6!2! +ƫČƫ!ƫ+!/ƫČƫ).+/*+ƫČƫ$*ƫċƫāġ!.ƫ(%*%(ƫ
/01 5ƫ+"ƫ%* %.!0ƫ.!/%*ƫ+),+/%0!ƫ.!/0+.0%+*/ƫ(10! ƫ3%0$ƫƫ/!("ġ $!/%2!ƫ
.!/%*ƫ!)!*0čƫ!û!0ƫ+"ƫ!*)!(ƫ!0$%*#ċƫBraz Dent JċƫĂĀāĂĎĂăĨĂĩčĊĈġāĀăċ
43.ƫ'5/$%ƫČƫ+&%)ƫČƫ/1$.ƫċƫ$!ƫ,.+)+0%+*ƫ+"ƫ $!/%+*ƫ
5ƫ0$!ƫ%*ü(0.0%+*ƫ+"ƫ)+*+)!./ƫ%*0+ƫ0++0$ƫ/1/0.0!/ċƫJ Biomed Mater
ResċƫāĊĉĂĎāćĨăĩčĂćĆġĂĈăċ
44.ƫ!$.ƫČƫ*/)**ƫČƫ+/!*0.%00ƫČƫ* !(ƫċƫ.#%*(ƫ ,00%+*ƫ
+"ƫ0$.!!ƫ/!("ġ $!/%2!ƫ.!/%*ƫ!)!*0/ƫ2/ċƫƫ3!((ġ0.%! ƫ $!/%2!ƫ(10%*#ƫ
#!*0ċƫClin Oral InvestigċƫĂĀĀĊĎāăĨąĩčąĆĊġąćąċ
45.ƫ#*!ƫċƫ))! %0!ƫ !*0%*ƫ/!(%*#čƫƫ"1* )!*0(ƫ,.+! 1.!ƫ"+.ƫ
%* %.!0ƫ+* ! ƫ.!/0+.0%+*/ċƫJ Esthet Restor DentċƫĂĀĀĆĎāĈĨăĩčāąąġāĆĆċ
46.ƫĚ.*#!(+ƫČƫ!ƫ*#!(%/ƫČƫ %*%ƫČƫĚ).%+ƫċƫ(%*%(ƫ!2(1ġ
0%+*ƫ+*ƫ,+.!(%*ƫ()%*0!ƫ2!*!!./ƫ+* ! ƫ3%0$ƫ(%#$0ġ1.! ƫ+),+/%0!čƫ
.!/1(0/ƫ1,ƫ0+ƫĈƫ5!./ċƫClin Oral InvestigċƫĂĀāĂĎāćĨąĩčāĀĈāġāĀĈĊċ
47.ƫ#*!ƫČƫ%!(/!*ƫċƫ*0!.0%+*/ƫ!03!!*ƫ%),.!//%+*ƫ)0!.%(/ƫ* ƫ
%))! %0!ƫ !*0%*ƫ/!(%*#ċƫJ Prosthet DentċƫĂĀĀĊĎāĀĂĨĆĩčĂĊĉġăĀĆċ
48.ƫ#*!ƫČƫ%)ƫČƫ/%+*!ƫČƫ+*+2*ƫċƫ))! %0!ƫ !*0%*ƫ/!(ġ
%*#ƫ%),.+2!/ƫ+* ƫ/0.!*#0$ƫ+"ƫ%* %.!0ƫ.!/0+.0%+*/ċƫJ Prosthet Dentċƫ
ĂĀĀĆĎĊąĨćĩčĆāāġĆāĊċ
49.ƫ1.0!ƫƫ
.Čƫ !ƫ.!%0/ƫČƫ ƫ
Čƫ *ƫċƫ$!ƫ!û!0ƫ+"ƫ%))! %ġ
0!ƫ !*0%*ƫ/!(%*#ƫ+*ƫ0$!ƫ).#%*(ƫ ,00%+*ƫ* ƫ+* ƫ/0.!*#0$/ƫ+"ƫ
0+0(ġ!0$ƫ* ƫ/!("ġ!0$ƫ $!/%2!/ċƫJ Prosthet DentċƫĂĀĀĊĎāĀĂĨāĩčāġĊċ
50.ƫ !ƫ* . !ƫČƫ !ƫ+!/ƫČƫ+*0!/ƫċƫ.#%*(ƫ ,00%+*ƫ* ƫ
)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ+),+/%0!ƫ%* %.!0ƫ.!/0+.0%+*/ƫ+* ! ƫ
0+ƫ !*0%*ƫ0.!0! ƫ3%0$ƫ $!/%2!ƫ* ƫ(+3ġ2%/+/%05ƫ+),+/%0!ċƫDent
MaterċƫĂĀĀĈĎĂăĨăĩčĂĈĊġĂĉĈċ
51.ƫ!!ƫ
Čƫ.'ƫċƫ$!ƫ!û!0ƫ+"ƫ0$.!!ƫ2.%(!/ƫ+*ƫ/$!.ƫ
+* ƫ/0.!*#0$ƫ3$!*ƫ(10%*#ƫƫ.!/%*ƫ%*(5ƫ0+ƫ !*0%*ċƫOper Dentċƫ
ĂĀĀĊĎăąĨăĩčĂĉĉġĂĊĂċ
52.ƫ.+5(!/ƫČƫ2*ƫČƫ! .*ġ1//+ƫċƫû!0ƫ+"ƫ !*0%*ƫ/1."!ƫ
)+ %ü0%+*ƫ+*ƫ0$!ƫ)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ/!("ġ $!/%2!ƫ.!/%*ƫ
!)!*0/ċƫJ ProsthodontċƫĂĀāăĎĂĂĨāĩčĆĊġćĂċ
53.ƫĚ.*#!(+ƫČƫ*%*%ƫČƫ.+/,!.%ƫČƫ!0ƫ(ċƫ$!ƫ%*ý1!*!ƫ+"ƫ ġ
$!/%2!ƫ0$%'*!//ƫ+*ƫ0$!ƫ)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ0$.!!ƫ $!/%2!ƫ
/5/0!)/ċƫJ Adhes DentċƫĂĀĀĊĎāāĨĂĩčāĀĊġāāĆċ
54.ƫ.A)!.ƫČƫ+$1!.ƫČƫ.*'!*!.#!.ƫċƫ $!/%2!ƫ(10%*#ƫ+"ƫ%* %ġ
.!0ƫ.!/0+.0%+*/ċƫAm J DentċƫĂĀĀĀĎāăĨ/,!ƫ*+ĩčćĀġĈćċ
55.ƫ+.!/ƫ
Čƫ+.!/ƫČƫ!.!%.ƫ
Čƫ+*/!ƫċƫ1."!ƫ0.!0)!*0ƫ
,.+0++(/ƫ%*ƫ0$!ƫ!)!*00%+*ƫ,.+!//ƫ+"ƫ!.)%ƫ* ƫ(+.0+.5ġ
,.+!//! ƫ+),+/%0!ƫ.!/0+.0%+*/čƫƫ(%0!.01.!ƫ.!2%!3ċƫJ Esthet Restor
DentċƫĂĀĀĆĎāĈĨąĩčĂĂąġĂăĆċ
56.ƫ$)#!ƫČƫ'%.ƫČƫ!.#%6ƫČƫ"!%û!.ƫċƫû!0ƫ+"ƫ/1."!ƫ+* %ġ
0%+*%*#ƫ+*ƫ0$!ƫ.!0!*0%2!ƫ+* ƫ/0.!*#0$/ƫ+"ƫü!..!%*"+.! ƫ+),+/%0!ƫ
,+/0/ċƫJ Prosthet DentċƫĂĀĀĊĎāĀĂĨćĩčăćĉġăĈĈċ
57.ƫĚ.*#!(+ƫČƫ*%*%ƫċƫû!0ƫ+"ƫ0$.!!ƫ/1."!ƫ0.!0)!*0/ƫ+*ƫ0$!ƫ
$!/%2!ƫ,.+,!.0%!/ƫ+"ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*/ċƫJ Adhes Dentċƫ
ĂĀĀĈĎĊĨăĩčăāĊġăĂćċ
58.ƫ.+/$ƫČƫ%(+ƫČƫ%$$+ƫČƫ(10/0!%*ƫċƫû!0ƫ+"ƫ+)%*0%+*/ƫ
+"ƫ/1."!ƫ0.!0)!*0/ƫ* ƫ+* %*#ƫ#!*0/ƫ+*ƫ0$!ƫ+* ƫ/0.!*#0$ƫ+"ƫ
.!,%.! ƫ+),+/%0!/ċƫJ Prosthet DentċƫāĊĊĈĎĈĈĨĂĩčāĂĂġāĂćċ
59.ƫ1))!(ƫČƫ.'!.ƫČƫ!ƫČƫ+( "+#(!ƫċƫ1."!ƫ0.!0)!*0ƫ+"ƫ
%* %.!0ƫ.!/%*ƫ+),+/%0!ƫ/1."!/ƫ!"+.!ƫ!)!*00%+*ċƫJ Prosthet Dentċƫ
āĊĊĈĎĈĈĨćĩčĆćĉġĆĈĂċ
60.ƫ+.%ƫČƫ%*)%ƫČƫ%*!/'%ƫČƫ!0ƫ(ċƫû!0ƫ+"ƫ$5 .+ý1+.%ƫ% ƫ
572
COMPENDIUM
September 2015
!0$%*#ƫ+*ƫ/$!.ƫ+* ƫ/0.!*#0$ƫ+"ƫ*ƫ%* %.!0ƫ.!/%*ƫ+),+/%0!ƫ0+ƫ*ƫ
$!/%2!ƫ!)!*0ċƫDent Mater JċƫĂĀĀĉĎĂĈĨąĩčĆāĆġĆĂĂċ
61.ƫ2(*0%ƫČƫ!ƫ%)ƫČƫ!.%/ƫČƫ!0ƫ(ċƫû!0ƫ+"ƫ/1."!ƫ0.!0ġ
)!*0/ƫ* ƫ+* %*#ƫ#!*0/ƫ+*ƫ0$!ƫ+* ƫ/0.!*#0$ƫ+"ƫ.!,%.! ƫ+),+/ġ
%0!/ċƫJ Esthet Restor DentċƫĂĀĀĈĎāĊĨĂĩčĊĀġĊĊċ
62.ƫ1!*ġ.0*ƫČƫ+*68(!6ġ¨,!6ƫČƫ2&/ġ+ .#1!6ƫ !ƫ+*ġ
!(+ƫ
ċƫ$!ƫ!û!0ƫ+"ƫ2.%+1/ƫ/1."!ƫ0.!0)!*0/ƫ* ƫ+* %*#ƫ#!*0/ƫ
+*ƫ0$!ƫ.!,%.! ƫ/0.!*#0$ƫ+"ƫ$!0ġ0.!0! ƫ+),+/%0!/ċƫJ Prosthet Dentċƫ
ĂĀĀāĎĉćĨĆĩčąĉāġąĉĉċ
63.ƫ+1/$(%$!.ƫČƫ+ƫČƫ.#/ƫċƫû!0ƫ+"ƫ03+ƫ./%2!ƫ
/5/0!)/ƫ+*ƫ.!/%*ƫ+* %*#ƫ0+ƫ(+.0+.5ġ,.+!//! ƫ%* %.!0ƫ.!/%*ƫ+)ġ
,+/%0!ƫ.!/0+.0%+*/ċƫJ Esthet DentċƫāĊĊĊĎāāĨąĩčāĉĆġāĊćċ
64.ƫ+* ƫČƫ(¨.%+ƫČƫ/0%*#ƫċƫû!0%2!*!//ƫ+"ƫ%* %.!0ƫ+),+/ġ
%0!ƫ.!/%*ƫ/%(*%60%+*ƫ!2(10! ƫ5ƫ)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ0!/0ċƫAm
J DentċƫĂĀĀĉĎĂāĨăĩčāĆăġāĆĉċ
65.ƫ1*#ƫČƫ0%*(%**ƫ
ċƫ/,!0/ƫ+"ƫ/%(*!ƫ+1,(%*#ƫ#!*0/ƫ* ƫ/1."!ƫ
+* %0%+*%*#ƫ%*ƫ !*0%/0.5čƫ*ƫ+2!.2%!3ċƫDent MaterċƫĂĀāĂĎĂĉĨĆĩčąćĈġąĈĈċ
66.ƫ(* .+ƫČƫ!(+#%ƫČƫ($*+ƫČƫ!0ƫ(ċƫ1."!ƫ+* %0%+*%*#ƫ+"ƫƫ
+),+/%0!ƫ1/! ƫ"+.ƫ%*(5ĥ+*(5ƫ.!/0+.0%+*/čƫ!û!0ƫ+*ƫ)1ƫ0+ƫ.!/%*ƫ
!)!*0ċƫJ Adhes DentċƫĂĀĀĈĎĊĨćĩčąĊĆġąĊĉċ
67.ƫ$+ƫČƫ&%0.*#/+*ƫČƫ0%/ƫČƫ(00ƫ
ċƫû!0ƫ+"ƫ.Č.čƫ
(/!.Čƫ%.ƫ./%+*Čƫ* ƫ/%(*!ƫ,,(%0%+*ƫ+*ƫ.!,%.! ƫ/$!.ƫ+* ƫ
/0.!*#0$ƫ+"ƫ+),+/%0!/ċƫOper DentċƫĂĀāăĎăĉĨăĩčāġĊċ
68.ƫ1.*!00ƫƫ
.Čƫ$%*'%ƫČƫ 1. +ƫ !ƫċƫ!*/%(!ƫ+* ƫ/0.!*#0$ƫ
+"ƫƫ+*!ġ+00(!ƫ $!/%2!ƫ/5/0!)ƫ0+ƫ%* %.!0ƫ+),+/%0!/ƫ0.!0! ƫ3%0$ƫ
.čƫ(/!.Čƫ%.ƫ./%+*Čƫ+.ƫý1+.% .%ƫ% ċƫPhotomed Laser Surgċƫ
ĂĀĀąĎĂĂĨąĩčăĆāġăĆćċ
69.ƫ+!6%6 !$ƫČƫ*/.%ƫ
Čƫ. ƫċƫû!0ƫ+"ƫ/1."!ƫ0.!0)!*0ƫ+*ƫ
)%.+ƫ/$!.ƫ+* ƫ/0.!*#0$ƫ+"ƫ03+ƫ%* %.!0ƫ+),+/%0!/ċƫJ Conserv Dentċƫ
ĂĀāĂĎāĆĨăĩčĂĂĉġĂăĂċ
70.ƫ*!,,!(!ƫČƫ !ƫ+16ƫČƫ0%/0ƫČƫ!0ƫ(ċƫ*ý1!*!ƫ+"ƫ čƫ+.ƫ
.čƫ(/!.ƫ/1."!ƫ0.!0)!*0ƫ+*ƫ)%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ%* %.!0ƫ
.!/%*ƫ+),+/%0!/ƫ0+ƫ.!/%*ƫ!)!*0ċƫ/!./ƫ/1."!ƫ0.!0)!*0ƫ+"ƫ%* %.!0ƫ
.!/%*ƫ+),+/%0!/ċƫEur J Prosthodont Restor DentċƫĂĀāĂĎĂĀĨăĩčāăĆġāąĀċ
71.ƫ+00ƫČƫ**%#ƫċƫû!0ƫ+"ƫ %û!.!*0ƫ(10%*#ƫ)0!.%(/ƫ+*ƫ0$!ƫ).ġ
#%*(ƫ ,00%+*ƫ+"ƫ(//ƫƫ!.)%ƫ%*(5ƫ.!/0+.0%+*/ƫ%*ƫ2%0.+ċƫDent
MaterċƫĂĀĀăĎāĊĨąĩčĂćąġĂćĊċ
72.ƫ!106"!( 0ƫċƫ1(ġ1.!ƫ.!/%*ƫ!)!*0/čƫ%*ƫ2%0.+ƫ3!.ƫ* ƫ!û!0ƫ+"ƫ
-1*0%05ƫ+"ƫ.!)%*%*#ƫ +1(!ƫ+* /Čƫü((!.ƫ2+(1)!Čƫ* ƫ(%#$0ƫ1.%*#ċƫ
Acta Odontol ScandċƫāĊĊĆĎĆăĨāĩčĂĊġăąċ
73.ƫ1#$)*ƫČƫ$*ƫČƫ1!##!!.#ƫċƫ1.%*#ƫ,+0!*0%(ƫ+"ƫ 1(ġ
,+(5)!.%6(!ƫ.!/%*ƫ!)!*0/ƫ%*ƫ/%)1(0! ƫ(%*%(ƫ/%010%+*/ċƫJ Prosthet
DentċƫĂĀĀāĎĉćĨāĩčāĀāġāĀćċ
74.ƫ+")**ƫČƫ,/0$.0ƫČƫ1#+ƫČƫ(%!.ƫċƫ+),.%/+*ƫ+"ƫ
,$+0+ġ0%20%+*ƫ2!./1/ƫ$!)%(ƫ+.ƫ 1(ġ1.%*#ƫ+"ƫ.!/%*ġ/! ƫ(10%*#ƫ
!)!*0/ƫ.!#. %*#ƫý!41.(ƫ/0.!*#0$Čƫ)+ 1(1/ƫ* ƫ/1."!ƫ$. *!//ċƫJ
Oral RehabilċƫĂĀĀāĎĂĉĨāāĩčāĀĂĂġāĀĂĉċ
75.ƫ*0+/ƫ
Čƫ//+/ƫČƫ ƫ*.*`Y+ƫČƫ!0ƫ(ċƫ. !*%*#ƫ+"ƫƫ
1(ġ1.!ƫ.!/%*ƫ!)!*0ƫ1/%*#ƫƫ* ƫƫ1.%*#ƫ1*%0/ċƫJ Appl Oral
SciċƫĂĀāĀĎāĉĨĂĩčāāĀġāāĆċ
76.ƫ-12%2ƫČƫ!.100%ƫČƫ )%ƫČƫ!0ƫ(ċƫ!#.!!ƫ+"ƫ+*2!./%+*ƫ+"ƫ
0$.!!ƫ+),+/%0!ƫ)0!.%(/ƫ!),(+5! ƫ%*ƫ0$!ƫ $!/%2!ƫ!)!*00%+*ƫ+"ƫ%*ġ
%.!0ƫ.!/0+.0%+*/čƫƫ)%.+ġ)*ƫ*(5/%/ċƫJ DentċƫĂĀĀĊĎăĈĨĉĩčćāĀġćāĆċ
77.ƫ !ƫ!*!6!/ƫ
Čƫ..%/ƫČƫ%**%*%ƫċƫ*ý1!*!ƫ+"ƫ(%#$0ġ0%20! ƫ
* ƫ10+ġƫ* ƫ 1(ġ,+(5)!.%6%*#ƫ $!/%2!ƫ/5/0!)/ƫ+*ƫ+* ƫ/0.!*#0$ƫ
+"ƫ%* %.!0ƫ+),+/%0!ƫ.!/%*ƫ0+ƫ !*0%*ċƫJ Prosthet DentċƫĂĀĀćĎĊćĨĂĩčāāĆġāĂāċ
78.ƫĚ).%+ƫČƫ%+*%ƫČƫ,+#.!+ƫČƫ!0ƫ(ċƫû!0ƫ+"ƫ.!,!0! ƫ
,.!$!0%*#ƫ5(!/ƫ+*ƫý!41.(ƫ/0.!*#0$ƫ+"ƫ.!/%*ƫ+),+/%0!/ċƫOper Dentċƫ
ĂĀāăĎăĉĨāĩčăăġăĉċ
79.ƫĚ).%+ƫČƫ!ƫ*#!(%/ƫČƫ %*%ƫČƫ!0ƫ(ċƫ*ý1!*!ƫ+"ƫƫ.!,!0! ƫ
,.!$!0%*#ƫ,.+! 1.!ƫ+*ƫ)!$*%(ƫ,.+,!.0%!/ƫ+"ƫ0$.!!ƫ.!/%*ƫ+)ġ
,+/%0!/ċƫOper DentċƫĂĀāĆĎąĀĨĂĩčāĉāġāĉĊċ
80.ƫ!. %#Y+ƫ
ċƫ!3ƫ !2!(+,)!*0/ƫ%*ƫ !*0(ƫ $!/%+*ċƫDent Clin North
AmċƫĂĀĀĈĎĆāĨĂĩčăăăġăĆĈČƫ2%%%ċ
81.ƫ*ƫČƫ')+0+ƫČƫ1'1/$%)ƫČƫ'%&%ƫċƫ2(10%+*ƫ+"ƫ,$5/%(ƫ
,.+,!.0%!/ƫ* ƫ/1."!ƫ !#. 0%+*ƫ+"ƫ/!("ġ $!/%2!ƫ.!/%*ƫ!)!*0/ċƫ
Volume 36, Number 8
Dent MaterċƫĂĀĀĈĎĂćĨćĩčĊĀćġĊāąċ
82.ƫ(1*'ƫČƫ/(*/'5ƫċƫû!0%2!*!//ƫ+"ƫ((ġ%*ġ+*!ƫ $!/%2!ƫ/5/0!)/ƫ
0!/0! ƫ5ƫ0$!.)+5(%*#ƫ"+((+3%*#ƫ/$+.0ƫ* ƫ(+*#ġ0!.)ƫ30!.ƫ/0+.#!ċƫ
J Adhes DentċƫĂĀĀĈĎĊĨĂƫ/1,,(ĩčĂăāġĂąĀċ
83.ƫ!ƫ1*'ƫ
Čƫ.#/ƫČƫ*ƫ* 150ƫČƫ!0ƫ(ċƫ+* %*#ƫ+"ƫ*ƫ10+ġ $!ġ
/%2!ƫ(10%*#ƫ)0!.%(ƫ0+ƫ!*)!(ƫ* ƫ !*0%*ċƫDent MaterċƫĂĀĀąĎĂĀĨāĀĩčĊćăġĊĈāċ
84.ƫ +2%ƫČƫ+*0%!((%ƫČƫ+.%ƫČƫ!0ƫ(ċƫ!("ġ $!/%2!ƫ.!/%*ƫ!ġ
)!*0/čƫƫ(%0!.01.!ƫ.!2%!3ċƫJ Adhes DentċƫĂĀĀĉĎāĀĨąĩčĂĆāġĂĆĉċ
85.ƫØ.')!*ƫČƫ1.'*ƫČƫ%)%((%ƫČƫ­'/Ø6ƫċƫ!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ
%* %.!0ƫ+),+/%0!/ƫ(10! ƫ3%0$ƫ0$.!!ƫ*!3ƫ/!("ġ $!/%2!ƫ.!/%*ƫ!)!*0/ƫ
0+ƫ !*0%*ċƫJ Appl Oral SciċƫĂĀāāĎāĊĨąĩčăćăġăćĊċ
86.ƫ1!*0!/ƫČƫ!((+/ƫČƫ+*68(!6ġ¨,!6ƫċƫ+* ƫ/0.!*#0$ƫ+"ƫ/!("ġ
$!/%2!ƫ.!/%*ƫ!)!*0/ƫ0+ƫ %û!.!*0ƫ0.!0! ƫ%* %.!0ƫ+),+/%0!/ċƫClin
Oral InvestigċƫĂĀāăĎāĈĨăĩčĈāĈġĈĂąċ
87.ƫ%.8( !6ƫČƫ!((+/ƫČƫ..% +ƫČƫ+ .#1!6ƫ
ċƫ.(5ƫ$. *!//ƫ
+"ƫ/!("ġ $!/%2!ƫ.!/%*ƫ!)!*0/ƫ1.! ƫ1* !.ƫ%* %.!0ƫ.!/%*ƫ+),+/%0!ƫ
.!/0+.0%+*/ċƫJ Esthet Restor DentċƫĂĀāāĎĂăĨĂĩčāāćġāĂąċ
88.ƫ%+00%ƫČƫ/6ƫČƫ!*ƫČƫ!0ƫ(ċƫ%.+0!*/%(!ƫ+* ƫ/0.!*#0$ƫ+"ƫ
*!3ƫ/!("ġ $!/%2!ƫ(10%*#ƫ#!*0/ƫ* ƫ+*2!*0%+*(ƫ)1(0%/0!,ƫ/5/0!)/ċƫJ
Prosthet DentċƫĂĀĀĊĎāĀĂĨĆĩčăĀćġăāĂċ
89.ƫ/$(!5ƫČƫ*+ƫČƫ%1$%ƫČƫ!0ƫ(ċƫ $!/%+*ƫ0!/0%*#ƫ+"ƫ !*0%*ƫ
+* %*#ƫ#!*0/čƫƫ.!2%!3ċƫDent MaterċƫāĊĊĆĎāāĨĂĩčāāĈġāĂĆċ
90.ƫ.*'!*!.#!.ƫČƫ.A)!.ƫČƫ!0/$!(0ƫċƫ!$*%-1!ƫ/!*/%0%2%05ƫ+"ƫ
!*0%*ƫ+* %*#čƫ!û!0ƫ+"ƫ,,(%0%+*ƫ)%/0'!/ƫ+*ƫ+* ƫ/0.!*#0$ƫ* ƫ
).#%*(ƫ ,00%+*ċƫOper DentċƫĂĀĀĀĎĂĆĨąĩčăĂąġăăĀċ
91.ƫ0!3.0ƫČƫ
%*ƫČƫ+ #!/ƫ
ċƫ$!.ƫ+* ƫ/0.!*#0$ƫ+"ƫ.!/%*ƫ!)!*0/ƫ
0+ƫ+0$ƫ!.)%ƫ* ƫ !*0%*ċƫJ Prosthet DentċƫĂĀĀĂĎĉĉĨăĩčĂĈĈġĂĉąċ
92.ƫ3%"0ƫ
ƫ
.Čƫ!. %#Y+ƫ
Čƫ+)!ƫČƫ!0ƫ(ċƫû!0/ƫ+"ƫ.!/0+.0%2!ƫ
* ƫ $!/%2!ƫ1.%*#ƫ)!0$+ /ƫ+*ƫ !*0%*ƫ+* ƫ/0.!*#0$/ċƫAm J Dentċƫ
ĂĀĀāĎāąĨăĩčāăĈġāąĀċ
93.ƫ'ƫČƫ%ƫČƫ$!1*#ƫČƫ!0ƫ(ċƫ%.+ġ0!*/%(!ƫ+* ƫ0!/0%*#ƫ+"ƫ
Introducing...
.!/%*ƫ!)!*0/ƫ0+ƫ !*0%*ƫ* ƫ*ƫ%* %.!0ƫ.!/%*ƫ+),+/%0!ċƫDent Materċƫ
ĂĀĀĂĎāĉĨĉĩčćĀĊġćĂāċ
94.ƫ ƫ.16ƫČƫ.0+/ƫ
Čƫ%(2!%.ƫČƫ!0ƫ(ċƫ +*0+,(/05ƫ//+%0! ƫ
3%0$ƫ(%*%(ƫ.+3*ƫ(!*#0$!*%*#ƫ%*ƫ)*#!)!*0ƫ+"ƫ!40!*/%2!ƫ.+3*ƫ
!/0.10%+*ċƫJ Conserv DentċƫĂĀāĂĎāĆĨāĩčĆćġćĀċ
95.ƫ !.ƫ
Čƫ+6%!.ƫČƫ((ƫƫ
.Čƫ)/!5ƫċƫû!0ƫ+"ƫ.+3*ƫ
).#%*/ƫ+*ƫ,!.%+ +*0(ƫ+* %0%+*/ƫ%*ƫ.!#1(.(5ƫ00!* %*#ƫ,0%!*0/ċƫJ
Prosthet DentċƫāĊĊāĎćĆĨāĩčĈĆġĈĊċ
96.ƫ$A06(!ƫČƫ* ƫČƫ*!.1 ƫČƫ!0ƫ(ċƫ$!ƫ%*ý1!*!ƫ+"ƫ).#%*/ƫ+"ƫ
.!/0+.0%+*/ƫ+"ƫ0$!ƫ,!.%+ +*0(ƫ0%//1!/ƫ+2!.ƫĂćƫ5!./ċƫJ Clin PeriodontolċƫĂĀĀāĎĂĉĨāĩčĆĈġćąċ
97.ƫ%(//+*ƫČƫ(! %*ƫČƫ.(//+*ƫČƫ!0ƫ(ċƫ0+./ƫû!0%*#ƫ0$!ƫ
/$!.ƫ+* ƫ/0.!*#0$ƫ+"ƫ+* ! ƫ+),+/%0!ƫ%*(5/ċƫInt J Prosthodontċƫ
ĂĀĀĀĎāăĨāĩčĆĂġĆĉċ
98.ƫ5*!ƫČƫ$)(6ƫċƫ!,.%*0%*#ƫ0$!ƫ(//%ƫ.0%(!ƫ+*ƫƫ
!2(10%+*ƫ)!0$+ /ƫ"+.ƫ)!/1.%*#ƫ0$!ƫ(%*%(ƫ.!/!.$ƫ,!."+.)*!ƫ+"ƫ
.!/0+.0%2!ƫ)0!.%(/ċƫClin Oral InvestigċƫĂĀĀĆĎĊĨąĩčĂĀĊġĂāąċ
99.ƫ10$ƫČƫ$!*ƫČƫ!$(ƫČƫ!0ƫ(ċƫ(%*%(ƫ/01 5ƫ+"ƫ%* %.!0ƫ+),+/ġ
%0!ƫ.!/%*ƫ%*(5/ƫ%*ƫ,+/0!.%+.ƫ/0.!//ġ!.%*#ƫ2%0%!/ƫ,(! ƫ5ƫ !*0(ƫ
/01 !*0/čƫ.!/1(0/ƫ"0!.ƫąƫ5!./ċƫJ DentċƫĂĀāāĎăĊĨĈĩčąĈĉġąĉĉċ
100ċƫ*$.0ƫ
Čƫ$!*ƫČƫ!1!.!.ƫČƫ!0ƫ(ċƫ$.!!ġ5!.ƫ(%*%(ƫ!2(1ġ
0%+*ƫ+"ƫ+),+/%0!ƫ* ƫ!.)%ƫ%*(5/ċƫAm J DentċƫĂĀĀāĎāąĨĂĩčĊĆġĊĊċ
101ċƫ!%./'.ƫ
Čƫ!*1#ƫČƫ$+.!/!*ƫČƫ!0ƫ(ċƫ(%*%(ƫ,!."+.)*!ƫ+"ƫ
%* %.!0ƫ+),+/%0!ƫ.!/%*ƫ%*(5/ĥ+*(5/ƫ%*ƫƫ !*0(ƫ/$++(čƫ+/!.20%+*/ƫ
1,ƫ0+ƫăąƫ)+*0$/ċƫActa Odontol ScandċƫāĊĊĊĎĆĈĨąĩčĂāćġĂĂĀċ
102ċƫ$!%!*+#!*ġ1$/.1**!.ƫČƫ*$.0ƫ
Čƫ.!)!./ƫČƫ!0ƫ(ċƫ3+ġ
5!.ƫ(%*%(ƫ!2(10%+*ƫ+"ƫ %.!0ƫ* ƫ%* %.!0ƫ+),+/%0!ƫ.!/0+.0%+*/ƫ%*ƫ
,+/0!.%+.ƫ0!!0$ċƫJ Prosthet DentċƫāĊĊĊĎĉĂĨąĩčăĊāġăĊĈċ
103ċƫ!0%*ƫČƫ*(1ƫČƫ+*+#(1ƫċƫƫü2!ġ5!.ƫ(%*%(ƫ!2(10%+*ƫ+"ƫ
%.!0ƫ**+ü((! ƫ* ƫ%* %.!0ƫ+),+/%0!ƫ.!/%*ƫ.!/0+.0%+*/ƫ%*ƫ,+/0!.%+.ƫ
0!!0$ċƫOper DentċƫĂĀāăĎăĉĨĂĩčāġāāċ
“Digital Technology
Integration for Efficient
Clinical Workflow”
RELEASE DATE: 7.29.2015
eBooks from AEGIS Communications put the dental
information you’re looking for right at your fingertips,
right when you need it. These high-quality, customized
“Knowledge is Power:
Targeting and Tracking
Your Marketing Strategy ”
educational tools focus on the latest concepts and
techniques, providing timely solutions for your
practice. Accessible 24/7, AEGIS eBooks can be
easily downloaded to your laptop or mobile device
RELEASE DATE: 7.28.2015
for future reference and sharing. Try one today!
ALSO AVAILABLE FOR DOWNLOAD:
“Going Digital”
COMING SOON:
Start Your Library Today
www.compendiumlive.com
insidedentistry.net/ebooks
“Is Your Practice Ready for the New EPA Rules”
September Future:
2015 COMPENDIUM
573
“A Drill-Free
How Lasers Deliver for Your Patients and Your Practice”
CONTINUING EDUCATION 2
QUIZ
Adhesive Cementation of Indirect Composite Inlays and Onlays: A Literature Review
Camillo D’Arcangelo, DDS; Lorenzo Vanini, MD, DDS; Matteo Casinelli, DDS; Massimo Frascaria, DDS, PhD;
Francesco De Angelis, DDS, PhD; Mirco Vadini, DDS, PhD; and Maurizio D’Amario, DDS, PhD
This article provides 2 hours of CE credit from AEGIS Publications, LLC. Record your answers on the enclosed Answer Form or submit them on a separate
sheet of paper. You may also phone your answers in to 877-423-4471 or fax them to 215-504-1502 or log on to compendiumce.com/go/1516. Be sure to
include your name, address, telephone number, and last 4 digits of your Social Security number.
Please complete Answer Form on page 576, including your name and payment information.
You can also take this course online at compendiumce.com/go/1516.
1.
ƫ
ƫ
ƫ
ƫ
2.
ƫ
ƫ
ƫ
ƫ
Issues associated with the use of direct resin composites in the
posterior region include:
ċƫ ƫ$%#$ƫ,+(5)!.%60%+*ƫ/$.%*'#!ċ
ċƫ ƫ#,ƫ"+.)0%+*ċƫ
ċƫ ƫ+(+.ƫ%*/0%(%05ċ
ċƫ ƫ((ƫ+"ƫ0$!ƫ+2!
6.
While the clinical performance of composite resin restorations is
comparable to ceramic restorations, increased use of composite
resin-based indirect restorations in the posterior region is a
result of:
ċƫ ƫ+),+/%0!/Ěƫ!4!((!*0ƫ.!/%/0*!ƫ0+ƫ3!.ƫ* ƫ0!.ċ
ċƫ ƫ+),+/%0!/Ěƫ/1,!.ƫ).#%*(ƫ%*0!#.%05ċ
ċƫ ƫ0$!ƫ.!(0%2!(5ƫ(+3ƫ+/0ƫ//+%0! ƫ3%0$ƫ+),+/%0!/ċ
ċƫ ƫƫ('ƫ+"ƫ,+/0+,!.0%2!ƫ/!*/%0%2%05ƫ//+%0! ƫ3%0$ƫ+),+/%0!/ċ
7.
ƫ
ƫ
ƫ
ƫ
ƫ
ƫ
ƫ
ƫ
8.
3.
ƫ
ƫ
ƫ
ƫ
4.
ƫ
ƫ
ƫ
ƫ
5.
ƫ
ƫ
ƫ
ƫ
An adherent is necessary because the microscopic structure of
two different contact surfaces presents:
ċƫ ƫ%..!#1(.%0%!/ċ
ċƫ ƫ.+1* ƫ%*0!.*(ƫ*#(!/ċ
ċƫ ƫƫ(!*Čƫ/)++0$ƫ/1."!ċ
ċƫ ƫƫ100ƫ&+%*0ċ
ƫ
ƫ
ƫ
ƫ
After cavity preparation and before cavity finishing, adhesive
procedures are performed using a rubber dam in order to:
ċƫ ƫ !.!/!ƫ#.%0ċ
ċƫ ƫ$%!2!ƫ*ƫ%))! %0!ƫ !*0%*ƫ/!(%*#ċ
ċƫ ƫ!4,+/!ƫ%*0!.011(.ƫ !*0%*ƫ+((#!*ƫü!./ċ
ċƫ ƫ %//+(2!ƫ0$!ƫ$5.% ƫ(5!.ċ
The application of phosphoric acid increases the surface
energy of dentin by removing the what and promoting
demineralization of surface hydroxyapatite crystals?
ċƫ ƫ+((#!*ƫü!./
ċƫ ƫ0.%+$!)%(ƫ+0%*#
ċƫ ƫ$5.% ƫ(5!.
ċƫ ƫ/)!.ƫ(5!.
Immediate dentin sealing (IDS) is a strategy in which a dentin
bonding agent is applied to freshly cut dentin and
polymerized before:
ċƫ ƫ.%!/ƫ.!)+2(ċ
ċƫ ƫ)'%*#ƫ*ƫ%),.!//%+*ċ
ċƫ ƫ).#%*ƫ,.!,.0%+*ċ
ċƫ ƫ(/!.ƫ0.!0)!*0ċ
What is an organic acid that demineralizes the surface, dissolves
hydroxyapatite crystals, and increases free surface energy?
ċƫ ƫ,.%)!.
ċƫ ƫ+* %*#ƫ#!*0
ċƫ ƫ!0$*0
ċƫ ƫ(%#$0ġ1.! ƫ+),+/%0!ƫü((%*#ƫ)0!.%(
9.
What refers to an adhesive system that dissolves the smear layer and
infiltrates it at the same time, without a separate etching step?
ċƫ ƫ/!("ġ!0$
ċƫ ƫ/!("ġ $!/%2!
ċƫ ƫ!0$ġ* ġ.%*/!
ċƫ ƫ/!(!0%2!ġ!0$
10. Light-cured filled composites can reach optimal fluidity by
doing what to them?
ƫ
ċƫ ƫ!0$%*#ƫ* ƫ.%*/%*#ƫ0$!)
ƫ
ċƫ ƫ%/+(0%*#ƫ0$!)
ƫ
ċƫ ƫ,.!$!0%*#ƫ0$!)
ƫ
ċƫ ƫ%.ƫ(+'%*#ƫ0$!)
ƫ
ƫ
ƫ
ƫ
What is the main factor responsible in improving the retentive
properties of indirect composite restorations?
ċƫ ƫ/* (/0%*#ƫ0.!0)!*0
ċƫ ƫ% ġ!0$%*#
ċƫ ƫ/%(*%60%+*
ċƫ ƫ,1)%%*#
Course is valid from 9/1/2015 to 9/30/2018. Participants
must attain a score of 70% on each quiz to receive credit. Participants receiving a failing grade on any exam will be notified
and permitted to take one re-examination. Participants will
receive an annual report documenting their accumulated
credits, and are urged to contact their own state registry
boards for special CE requirements.
574
COMPENDIUM
September 2015
AEGIS Publications, LLC, is an ADA CERP Recognized
Provider. ADA CERP is a service of the American Dental
Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does
not approve or endorse individual courses or instructors, nor
does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be
directed to the provider or to ADA CERP at www.ada.org/cerp.
Program Approval for
Continuing Education
Approved PACE Program Provider
FAGD/MAGD Credit
Approval does not imply acceptance
by a state or provincial board of
dentistry or AGD endorsement
1/1/2013 to 12/31/2016
Provider ID# 209722
Volume 36, Number 8