Clinical update no. 288 20 September 2012
advertisement
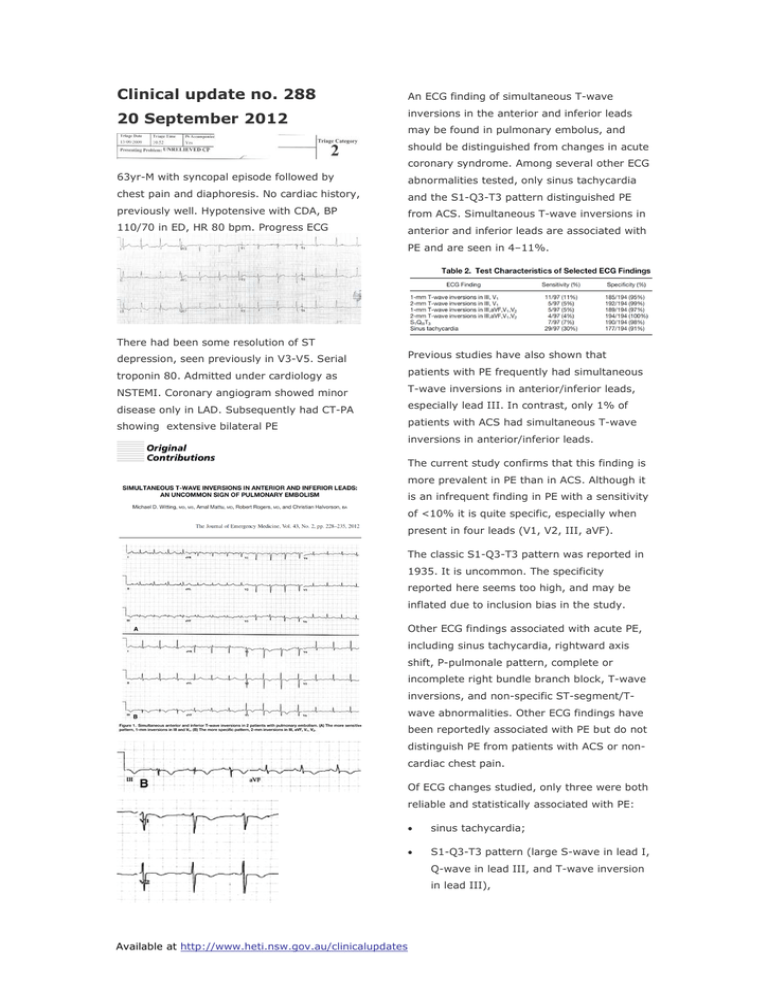
Clinical update no. 288 20 September 2012 An ECG finding of simultaneous T-wave inversions in the anterior and inferior leads may be found in pulmonary embolus, and should be distinguished from changes in acute coronary syndrome. Among several other ECG 63yr-M with syncopal episode followed by abnormalities tested, only sinus tachycardia chest pain and diaphoresis. No cardiac history, and the S1-Q3-T3 pattern distinguished PE previously well. Hypotensive with CDA, BP from ACS. Simultaneous T-wave inversions in 110/70 in ED, HR 80 bpm. Progress ECG anterior and inferior leads are associated with PE and are seen in 4–11%. There had been some resolution of ST depression, seen previously in V3-V5. Serial Previous studies have also shown that troponin 80. Admitted under cardiology as patients with PE frequently had simultaneous NSTEMI. Coronary angiogram showed minor disease only in LAD. Subsequently had CT-PA showing extensive bilateral PE T-wave inversions in anterior/inferior leads, especially lead III. In contrast, only 1% of patients with ACS had simultaneous T-wave inversions in anterior/inferior leads. The current study confirms that this finding is more prevalent in PE than in ACS. Although it is an infrequent finding in PE with a sensitivity of <10% it is quite specific, especially when present in four leads (V1, V2, III, aVF). The classic S1-Q3-T3 pattern was reported in 1935. It is uncommon. The specificity reported here seems too high, and may be inflated due to inclusion bias in the study. Other ECG findings associated with acute PE, including sinus tachycardia, rightward axis shift, P-pulmonale pattern, complete or incomplete right bundle branch block, T-wave inversions, and non-specific ST-segment/Twave abnormalities. Other ECG findings have been reportedly associated with PE but do not distinguish PE from patients with ACS or noncardiac chest pain. Of ECG changes studied, only three were both reliable and statistically associated with PE: • sinus tachycardia; • S1-Q3-T3 pattern (large S-wave in lead I, Q-wave in lead III, and T-wave inversion in lead III), Available at http://www.heti.nsw.gov.au/clinicalupdates • The described TIII-V1 pattern. To produce ECG changes, a PE must be large, The following patient did not have PE – S1Q3T3 is not specific. and is presumed to produce ECG changes by causing acute pulmonary hypertension, giving a change in cardiac position due to right heart dilatation, right ventricular ischemia, intraventricular conduction disturbances due to ischaemia, and increased sympathetic stimulation. Other factors producing negative T waves include hypoxemia and the release of chemical mediators within the right ventricle. V1 faces the anterior region of the right ventricle and Following ECG after collapse 3 days post hip replacement shows new right axis deviation, new RBBB with R wave in V1, and acute right heart strain. Normal pre-op ECG also shown lead III faces the inferior region of the right ventricle, giving the observed pattern. Changes with PE are acute, though chronic pulmonary hypertension can produce similar findings. A new ECG findings of pulmonary hypertension suggest acute PE. T-wave inversions may lead to a workup for ACS which if negative may lead to discharge without consideration of PE. Conversely, many findings traditionally described for PE are simply not worth remembering because they are unreliably measured and are no more prevalent in patients with PE than in other populations. Cases: the following in an unstable patient with clinically suspected PE. New onset right axis changes are from acute PE, Na channel blocking drug toxicity (e.g. TCAs), hyperkalaemia, or artefact from lead misplacement. ECG findings with right ventricular hypertrophy are: tall R wave > 6 mm in V1, right axis deviation, and right atrial changes (P wave >2.5mm in II and > 1.5 mm in V1) Available at http://www.heti.nsw.gov.au/clinicalupdates






