as a PDF
advertisement

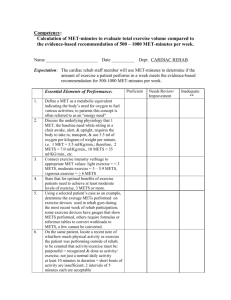
Diabetes Care In Press, published online January 26, 2007 Impact of Insulin Resistance on Risk of Type 2 Diabetes and Cardiovascular Disease in People with Metabolic Syndrome Received for publication 7 December 2006 and accepted in revised form 18 January 2007. Short title: Insulin Resistance and Metabolic Syndrome James B. Meigs, MD, MPH Martin K. Rutter, MD Lisa M. Sullivan, PhD Caroline S Fox, MD, MPH Ralph B. D’Agostino Sr, PhD Peter W. F. Wilson, MD From Harvard Medical School and the General Medicine Division, Department of Medicine, Massachusetts General Hospital, Boston, MA (JBM); The Manchester Diabetes Centre, Manchester Royal Infirmary and The Division of Cardiovascular and Endocrine Sciences, University of Manchester, UK (MKR); Department of Biostatistics, Boston University School of Public Health, Boston, MA (LMS); Department of Mathematics, Statistics, and Consulting Unit, Boston University, Boston, MA (RDA); the National Heart, Lung, and Blood Institute’s Framingham (Mass) Heart Study (CSF), and Emory University School of Medicine, Atlanta, GA (PWFW). Address for Correspondence: James B Meigs MD MPH, General Medicine Division, Massachusetts General Hospital, 50 Staniford Street, 9th Floor, Boston, MA 02114, USA. Email: jmeigs@partners.org. Copyright American Diabetes Association, Inc., 2007 Abstract OBJECTIVE - Metabolic syndrome (MetS) increases risk for type 2 DM and CVD and may be associated with insulin resistance (IR). RESEARCH DESIGN AND METHODS - We tested the hypothesis that MetS confers risk with or without concomitant IR among 2803 Framingham Offspring Study subjects followed up to 11 years for new DM (135 cases) or CVD (240). We classified subjects by presence of MetS (using ATP3, IDF, or EGIR criteria) and IR (HOMA-IR ≥75%ile) and used separate risk factor-adjusted proportional hazards models to estimate relative risks (RR) for DM or CVD using as referents those without IR, MetS, or without both. RESULTS – Fifty-six percent with ATP3, 52% with IDF, and 100% with EGIR MetS had IR. IR increased risk for DM (RR 2.6, 95% CI 1.7-4.0) and CVD (1.8, 1.4-2.3), as did MetS (DM: ATP3, 3.5, 2.2-5.6; IDF, 4.6, 2.7-7.7; EGIR, 3.3, 2.1-5.1; CVD: ATP3, 1.8, 1.4-2.3; IDF, 1.7, 1.3-2.3; EGIR, 2.1, 1.62.7). Relative to those without either Mets or IR, MetS and IR increased risk for DM (ATP3, 6.0, 3.310.8; IDF 6.9, 3.7-13.0) and CVD (ATP3, 2.3, 1.7-3.1; IDF 2.2, 1.6-3.0). Any MetS without IR increased risk for DM ~3-fold (p<0.001); IDF MetS without IR (RR 1.6, p=0.01) but not ATP3 MetS without IR (RR 1.3, p=0.2) increased risk for CVD. CONCLUSIONS - MetS increased risk for DM regardless of IR. ATP3 MetS may need IR to increase risk for CVD. The simultaneous presence of MetS and IR identify an especially high risk individual. Background People with the cluster of risk factors including obesity, impaired fasting glucose, hypertension, low HDL cholesterol and elevated triglycerides are thought to have a ‘metabolic syndrome’ (MetS) reflecting underlying insulin resistance (IR). Both MetS and IR are factors in the development of type 2 diabetes and cardiovascular disease (CVD)1. Several competing definitions of MetS are in use, and each is linked differently to the presence of IR. These definitions include that of the National Cholesterol Education Program’s Third Adult Treatment Panel (ATP3),2; the International Diabetes Federation (IDF) 3, and the European Group for the Study of Insulin Resistance (EGIR)4. The EGIR definition requires the presence of IR plus any two other metabolic traits; ATP3 and IDF require at least three metabolic traits but do not require the presence of IR. In studies of ATP3 MetS as many as half of subjects do not have IR 5-7 There are few population-based data comparing how well the ATP3 or IDF MetS definitions identify subjects with IR 8 or comparing how well ATP3, IDF, or EGIR MetS predict subsequent risk for incident diabetes 9, 10 or CVD 11-13. In addition, while it has been implied that the presence of MetS is a surrogate for the presence of IR, there are few data on DM or CVD risk associated with MetS in the absence of IR, or in the presence of both MetS and IR. With this background in mind we performed an analysis in the Framingham Offspring Study (FOS) using three MetS definitions in a test of the hypothesis that MetS confers risk for subsequent development of diabetes or CVD with or without concomitant IR. Research Design and Methods Study Subjects The FOS is a community-based prospective observational study of CVD and its risk factors 14. During the fifth exam cycle (the baseline exam, 1991-1995), 3799 participants fasted overnight and had a standardized medical examination, including a 2-hour oral glucose tolerance test (OGTT). From 3,799 participants, we excluded those with prevalent diabetes (n=429), prevalent CVD (n=269), or missing information on covariates (n=298), which left 2,803 subjects for analysis. Subjects were followed from baseline over a mean of 6.8 years for new cases of diabetes and a mean of 11.6 years for first CVD events. The Institutional Review Board of Boston University approved the study protocol, and all subjects gave written informed consent at each examination. Clinical Definitions and Laboratory Methods We defined MetS according to updated 2005 NCEP ATP3 criteria 2, IDF criteria 3, and EGIR criteria 4. Key features and differences among these three MetS definitions are as follows. ATP3 MetS requires the presence of any three of the following five traits: a large waist circumference, impaired fasting glucose (IFG), low HDL cholesterol, high triglycerides, or hypertension; IDF requires a large waist circumference plus any two of the preceding metabolic traits, and EGIR requires IR plus any two of the preceding traits, with the exception that lipid traits are not counted separately (low HDL-C or high triglycerides count as one trait). The other major differences are that a larger waist defines ‘large waist circumference’ for ATP3 (≥102 cm in men or ≥88 cm in women) than for IDF or EGIR (≥94 cm in white men or ≥80 cm in white women), and by current criteria IFG is defined by a fasting plasma glucose (FPG) of 5.6-6.9 mmol/l in the ATP3 and IDF definitions and a FPG of 6.16.9 mmol/l in the EGIR definition. We measured IR with the homeostasis model using the following validated formula: HOMA-IR = (fasting glucose (mmol/l) x fasting insulin (µU/mL)) / 22.5 15, 16 . Values of HOMA-IR in each quarter were: Q1, 2.21-5.07; Q2, 5.08-6.18; Q3, 6.19-7.84; and Q4, 7.85-30.80 units. We defined IR as a HOMAIR value greater than the 75th percentile (7.84) among non-diabetic subjects 4. We measured height, weight, and waist circumference with the subject standing in light clothes. Waist circumference was measured at the level of the umbilicus. Pair-wise inter-technician (three technicians) intra-class correlations performed periodically for waist circumference quality control ranged from 0.96 to 0.99. Blood pressure values were taken as the mean of two measurements after the subject had been seated for at least five minutes. Those who reported smoking cigarettes regularly during the year prior to the exam were considered current smokers. We based a positive parental history of diabetes on selfreport of diabetes in one or both parents 17. We defined impaired glucose tolerance (IGT) as a 2hour OGTT glucose level of 7.8–11.0 mmol/l. Laboratory methods for glucose, insulin, and lipid assays have been published previously 18 Diabetes and CVD Assessment We defined diabetes at the baseline exam as a FPG ≥ 7.0 mmol/l, a 2-hour OGTT glucose of ≥ 11.1 mmol/l, or use of hypoglycemic drug therapy. We defined diabetes at follow-up as development of a FPG ≥ 7.0 mmol/l or new use of hypoglycemic drug therapy during the study interval. Over 99% of diabetes among Framingham Offspring is type 2 diabetes 18. We defined baseline and follow-up CVD by standard Framingham Heart Study criteria as any of the following: new onset angina, fatal and non-fatal myocardial infarction or stroke, transient ischemic attack, heart failure, or intermittent claudication 19. Statistical Analysis We used chi-square tests or ANOVA to test differences in baseline characteristics by MetS and IR categories. We used the kappa (ê ) statistic to assess the level of agreement between MetS definitions, where poor agreement is considered a ê < 0.20, fair, ê = 0.21 to 0.40; moderate, ê = 0.41 to 0.60; substantial, ê = 0.61 to 0.80; and very good agreement, ê > 0.80 20. Subjects were followed from baseline through the seventh (19982001) exam for diabetes and through December, 2004 for CVD events. Risk for diabetes or CVD was examined in separate analyses. We calculated incidence rates for diabetes or CVD as the number of diabetes or CVD events divided by personyears of follow-up in each category. For diabetes incidence, we used the exam visit date that a new case of diabetes was identified as the date of diagnosis. For CVD events, we used the actual date of the event as the date of diagnosis, and for subjects without events, the date of their last follow-up exam as the censoring date. We used hazard ratios from proportional hazards regression models (accounting for interval censoring for diabetes events) to estimate relative risks (RR) and 95% confidence intervals (CIs) for incident diabetes or CVD conditioned on baseline MetS or IR categories. Models were adjusted for age and sex, and used those with without MetS or IR as the referent groups. Multivariable models were adjusted for major disease risk factors beyond those comprising metabolic syndrome. Models predicting incident diabetes included covariates for age, sex, parental history of diabetes, body mass index (BMI, as kg weight per meter height squared) and IGT. Multivariable models predicting incident CVD included covariates for age, sex, LDL cholesterol level, and smoking. First-order sex-by-MetS interaction terms were not significant (in part because there were too few events in some subgroups to calculate stable sexspecific risk estimates) so we did not conduct sexspecific analyses. For instance, even in the sexcombined analysis, in the smallest groups (no MetS but with IR) we had only 30–40% power to detect a difference in the observed proportions at alpha=0.05. We used areas under the receiver operating characteristic curve (aROC) to compare the ability of MetS and/or IR to discriminate future diabetes or CVD risk. The aROC is interpreted as the probability that the modeled phenotype(s) correctly discriminate subjects developing endpoints from those without endpoints, where 0.5 is chance discrimination and 1.0 is perfect discrimination. We estimated the population attributable risk percent for diabetes or CVD associated with exposure categories (for instance, the ATP3 MetS and IR) as PAR% = (proportion of cases in the exposure category x ((relative risk exposure category – 1) / relative risk 21 exposure category)) x 100 . We performed all analyses using SAS (SAS Institute, Cary, NC) and considered a two-sided value of p< 0.05 to be statistically significant. Results The mean age of the study population overall was 54 (range 26-82) years, and 55% were women. Baseline characteristics of study subjects are shown in Table 1. Diabetes and CVD risk factor levels were generally more adverse among people with IR compared to those without IR, and most adverse among those with MetS and IR. Among 2803 people the prevalence of ATP3 MetS was 27.8%, of IDF MetS 34.2%, and of EGIR MetS 19.1%. By definition, the prevalence of IR was 25%. Among those with ATP3 MetS the prevalence of IR was 56.4%, among those with IDF MetS, 52%, and, by definition, 100% among those with EGIR MetS. The prevalence of IR in those without ATP3 MetS was 12.8% and among those without IDF MetS, 11.0%. There was substantial agreement in MetS classification by ATP3 vs. IDF criteria (ê statistic 0.77 overall; women, 0.81; men, 0.71) and moderate agreement between IDF and EGIR or ATP3 criteria (IDF vs. EGIR: ê statistic 0.50; EGIR vs. ATP3: ê statistic 0.53). Incidence rates for diabetes stratified by the presence or absence of MetS and IR were generally similar for all three MetS definitions (Figure). The diabetes incidence rates were dramatically higher for those with both MetS and IR compared with the other categories. Similar relationships were apparent for the incidence of CVD,. Regression models confirmed that all three MetS definitions conferred generally similar risk for incident diabetes (Table 2). Of the three, IDF MetS was associated with a perhaps slightly higher age-sex-risk factor adjusted relative risk for diabetes (4.6) than was ATP3 MetS (3.5) or EGIR MetS (3.3), and all had a somewhat higher relative risk for diabetes than did IR (2.6). In fully adjusted models IR without MetS (by any definition) was not associated with a significantly increased risk for diabetes, but this was the most uncommon subgroup contributing the fewest events (Figure). MetS without IR was associated with a significant ~3-fold increased risk. ATP3 or IDF MetS and IR were associated with a 6-7-fold increased risk for diabetes, consistent with an additive (on the log scale) effect of MetS and IR on diabetes risk. In all models, first-order interaction terms for MetS-by-IR were not significant (all p > 0.6), confirming that MetS did not confer greater diabetes risk in the presence of IR than in the absence of IR. As we have previously shown that the number of MetS-related traits is positively associated with risk for diabetes 1 it was perhaps not surprising that EGIR MetS (which although requires IR is a sum of as few as 3 to as many as 5 traits) conferred a lower relative risk (3.3) than ATP3 or IDF MetS and IR (which at minimum represent a sum of as few as 4 and as many as 6 traits). To demonstrate this point we conducted a subsidiary analysis of ATP3 or IDF MetS and IR, but with MetS defined as any two or more component traits. In this analysis relative risks were very similar as for EGIR MetS. For instance, the risk for diabetes relative to all subjects without ATP3 MetS (2 or more traits) and without IR was 3.03 (95% CI 1.93- 4.74). In fully adjusted models all three MetS definitions, IR, and their joint combinations were associated with similar discriminatory capacity for diabetes (adjusted aROCs 0.83-0.85), and MetS with IR accounted for 42-66% of diabetes risk in the population (Table 2). Also shown in Table 2 are relative risks for CVD. As reported previously 1 adjusted relative risks for CVD associated with MetS were substantially lower than for diabetes (Table 2), ranging from 1.7–2.1. IR conferred similar (1.8) risk for CVD as did MetS by any definition. In fully adjusted models IR without MetS did not confer significantly increased risk for CVD, and only IDF MetS without IR significantly increased risk for CVD. As for diabetes, relative risk sizes were consistent with an additive effect of MetS and IR on risk of CVD, and first-order interaction terms for MetS-by-IR were not significant (all p >0.3). In fully adjusted models, all MetS definitions were associated with similar discriminatory capacity for CVD (adjusted aROCs 0.73 – 0.74) and MetS and IR accounted for 14% 23% of CVD risk in the population. Additional Subsidiary Analyses FPG is a component of the MetS definitions, and it is also a component of HOMAIR. This could potentially lead to overfitting FPG in statistical models that included both MetS and HOMA-IR. We therefore we used hyperinsulinemia (≥upper quartile of fasting serum insulin in subjects without diabetes) as an alternative measure of IR. The results of this analysis were virtually identical to those using to HOMA-IR (not shown). The increased CVD risk associated with MetS might be explained, at least in part, by incident diabetes and therefore we performed an analysis that excluded those who developed diabetes from the analysis of CVD events. This analysis yielded a modest attenuation (~10-15% lower) of the relative risks associated with MetS and IR for incident diabetes and CVD but the results of the analysis, including significance levels, were essentially unchanged (not shown). The increased diabetes risk associated with MetS could be largely explained by the IFG component of the definition. To explore this further we excluded subjects with IFG from the analysis and we used hyperinsulinemia as a measure of IR (rather than HOMA-IR) to remove fasting glucose as an exposure variable. In this analysis ATP III and IDF MetS remained significant predictors of incident diabetes in ageand sex-adjusted analyses (ATP III MetS (no IFG): RR=2.2, p=0.02; IDF MetS (no IFG): RR=3.2, p=0.0003) but neither remained significant predictors in multivariable-adjusted analyses (ATP III MetS (no IFG): RR=1.1, p=0.9; IDF MetS (no IFG): RR=1.9, p=0.06). Compared to the referent group, hyperinsulinemic subjects with ATP III (no IFG) or IDF MetS (no IFG) were at increased risk for incident diabetes in age- and sex-adjusted analyses (ATP III MetS (no IFG) + hyperinsulinemia: RR=4.2, p=0.0003; IDF MetS (no IFG) + hyperinsulinemia: RR=6.0, p<0.0001) but only IDF MetS (no IFG)/hyperinsulinemic subjects remained at increased risk in multivariable-adjusted models (ATP III MetS (no IFG) + hyperinsulinemia: RR=1.7, p=0.3; IDF MetS (no IFG) + hyperinsulinemia: RR=3.1, p<0.01). This analysis suggests that the covariates in the multivariate models, parental history of diabetes and IGT, largely accounted for the association of non-glucose MetS traits with risk of diabetes. Conclusions This study provides several insights: a) the level of agreement among ATP3, IDF and EGIR MetS definitions is moderate or better, but only half of individuals with ATP3 or IDF MetS are insulin resistant defined by the conventional top quartile of the HOMA-IR distribution; b) individuals with ATP3 or IDF MetS but without IR are at increased risk for diabetes, and those with IDF MetS but without IR are at increased risk for CVD, however, the joint presence of IR and MetS indicates substantially increased risk for diabetes or CVD; and c) all three MetS definitions, IR, and their joint combinations are associated with similar discriminatory capacity and PAR% for incident diabetes or CVD. The data support the general concept of risk factor clustering as a diabetes and CVD risk factor, and suggest that adding measurement of IR helps to identify increased risk in individuals with MetS, but on a population level, diagnosis of risk factor clustering with or without IR leads to equivalent ability to sort groups into higher and lower-risk categories. Our data confirm those of other population studies showing a higher prevalence of IDF MetS compared with ATP3 MetS 22-26 , largely due to lower thresholds for elevated waist circumference in IDF Mets vs. ATP3 MetS. Few studies have examined the prevalence of EGIR MetS 27. Its relatively low prevalence in Framingham is accounted for by the requirement for IR and higher thresholds defining elevated glucose, triglycerides and blood pressure. A relatively high level of agreement between ATP3 and IDF MetS definitions is not surprising since both definitions share common risk factors defined by generally similar thresholds. Our data also confirm other studies showing that only about half of people with MetS have evidence of IR. 8.5, 6 In a prior analysis from Framingham we showed that even among obese subjects with ATP3 MetS the prevalence of IR was only 68% 7. This present study extends these data, and we show that the widely-promoted ATP3 and IDF MetS definitions are not, as commonly stated, 2, 3 synonymous with IR. Only the EGIR definition, which requires the presence of IR, represents a true ‘insulin resistance syndrome’. Several groups have promoted different definitions of American, white, black, and Chinese samples suggest that ATP3 and IDF MetS confer roughly equivalent risk for diabetes, 9, 10 an observation that we confirm in a large, unselected community clustering might have value on the individual based white sample. We extend this observation to clinical level in people with MetS but is probably show that MetS alone, but perhaps not the unnecessary to further discriminate high risk uncommon IR alone, increases risk for diabetes, groups on the population level. and that MetS and IR have additive effects of this study include a derived large, from fact at independent physiologic domains increasing diabetes risk. Data from Pima Indians also shows thStrengths prospectively evaluated, community-based sample be a significant diabetes risk factor. However the assessed for standardized exposures and outcomes. IR effect was in the direction of increased risk, Limitations include that we did not have adequate and the additive pattern of risk in the group with sample size to subdivide the sample by sex. We MetS and IR suggests that low power in the group did not directly measure IR; use of proxy with MetS but without IR accounted in part for the measures will misclassify some people and statistically non-significant association with diminish the true magnitude of associations of IR diabetes. In addition, a non-significant effect in with outcomes. Finally, the Framingham this group might be explained by imprecision in population is white, so findings may have limited the true estimation of IR inherent in use of proxy generalizability. measures, or the possibility that metabolic In summary, prospective analysis correlates of IR confer much of its diabetogenic demonstrates that ATP3 and IDF MetS are not effect. 9 However, that MetS is a risk factor for synonymous with an insulin resistant phenotype. diabetes even in the absence of IR, and the clearly The presence of IR substantially increases additive effects of MetS and IR on diabetes risk individual diabetes or CVD risk in people with suggest that both are independent determinants of MetS, but population risk prediction using MetS is diabetes, and may operate by at least partially similar with or without concurrent IR. A clinical distinct pathways. trial may be needed to test whether clinical use of The foregoing discussion concerning risk IR adds value to care aimed at reducing individual for diabetes also applies to risk for CVD. In metabolic risk. No one MetS definition offers a addition, the present study underscores that, by clear advantage for diabetes or CVD risk any definition, and regardless of the presence or detection. As such consensus on a definition for absence of IR, MetS is a far more powerful risk risk factor clustering would be helpful, as factor for diabetes than for CVD. 1 Several studies regardless how defined, risk factor clustering have examined the risk for CVD associated with identifies individuals and groups at marked MetS by various definitions, and they have found increased risk for future diabetes and modest risk that all definitions of MetS are generally for future CVD. associated with a two-fold increased relative risk for new CVD.10-13, 26 One can conclude that none of the competing MetS definitions provides a Acknowledgements and Disclosures distinct advantage over the others as a CVD risk Supported by the NHLBI’s Framingham Heart prediction tool. We previously published an Study (Contract No. N01-HC-25195), a grant from analysis of Framingham data demonstrating that GlaxoSmithKline, and by an American Diabetes ATP3 MetS and IR were independently associated Association Career Development Award to Dr. with incident CVD over seven years of follow-up 29 Meigs. Dr. Meigs currently has research grants . The present study advances that analysis by from GlaxoSmithKline, Wyeth and sanofi-aventis, extending surveillance up to 11 years, and serves on safety or advisory boards for dichotomizing MetS and IR into clinically GlaxoSmithKline, Merck, and Lilly. Dr. Wilson is identifiable groups, and demonstrating a clear supported by grants from GlaxoSmithKline and additive effect of MetS and IR on both diabetes Wyeth. The funding agencies had no influence and CVD risk. Elsewhere we have advocated the over the decision to publish the findings. The measurement of IR as part of MetS, to render it a authors thank Peter Shrader MS for assistance true insulin resistance syndrome, as in the EGIR 30 with the statistical analyses. definition . The present study suggests that measurement of IR as a component of risk factor References 1. Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066-3072. 2. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr., Spertus JA, Costa F. Diagnosis and Management of the Metabolic Syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112: 2735-52. 3. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469-480. 4. Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet Med. 1999;16:442-443. 5. Liao Y, Kwon S, Shaughnessy S, Wallace P, Hutto A, Jenkins AJ, Klein RL, Garvey WT. Critical evaluation of adult treatment panel III criteria in identifying insulin resistance with dyslipidemia. Diabetes Care. 2004;27:978-983. 6. Cheal KL, Abbasi F, Lamendola C, McLaughlin T, Reaven GM, Ford ES. Relationship to Insulin Resistance of the Adult Treatment Panel III Diagnostic Criteria for Identification of the Metabolic Syndrome. Diabetes. 2004;53:1195-1200. 7. Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan L, D'Agostino RB. Body Mass Index, Metabolic Syndrome and Risk of Type 2 Diabetes or Cardiovascular Disease. J Clin Endocrinol Metab. 2006;91: 2906-12. 8. Rathmann W, Haastert B, Icks A, Giani G, Holle R, Koenig W, Lowel H, Meisinger C. Prevalence of the metabolic syndrome in the elderly population according to IDF, WHO, and NCEP definitions and associations with C-reactive protein: the KORA Survey 2000. Diabetes Care. 2006;29:461-6 9. Hanley AJ, Karter AJ, Williams K, Festa A, D'Agostino RB, Jr., Wagenknecht LE, Haffner SM. Prediction of type 2 diabetes mellitus with alternative definitions of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Circulation. 2005;112:3713-3721. 10. Wang JJ, Li HB, Kinnunen L, Hu G, Jarvinen TM, Miettinen ME, Yuan S, Tuomilehto J. How well does the metabolic syndrome defined by five definitions predict incident diabetes and incident coronary heart disease in a Chinese population? Atherosclerosis. 2006;[Epub ahead of print]. 11. Dekker JM, Girman C, Rhodes T, Nijpels G, Stehouwer CD, Bouter LM, Heine RJ. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation. 2005;112(5):666-673. 12. Katzmarzyk PT, Janssen I, Ross R, Church TS, Blair SN. The importance of waist circumference in the definition of metabolic syndrome: prospective analyses of mortality in men. Diabetes Care. 2006;29:404-409. 13. Lawlor DA, Smith GD, Ebrahim S. Does the new International Diabetes Federation definition of the metabolic syndrome predict CHD any more strongly than older definitions? Findings from the British Women's Heart and Health Study. Diabetologia. 2006;49:41-48. 14. Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281-290. 15. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-419. 16. Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23:57-63. Murabito JM, Nam BH, D'Agostino RB, Sr., Lloyd-Jones DM, O'Donnell CJ, Wilson PW. Accuracy of offspring reports of parental cardiovascular disease history: the Framingham Offspring Study. Ann Intern Med. 2004;140:434-440. Meigs JB, Mittleman MA, Nathan DM, Tofler GH, Singer DE, Murphy-Sheehy PM, Lipinska I, D'Agostino RB, Wilson PW. Hyperinsulinemia, hyperglycemia, and impaired hemostasis: the Framingham Offspring Study. JAMA. 2000;283:221-228. Cupples LA, D'Agostino RB. Section 34: Some risk factors related to the annual incidence of cardiovascular disease and death using pooled repeated biennial measurements: Framingham Heart Study, 30-year followup. Washington D.C: U.S. Department of Commerce; 1988. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15-19. Adams RJ, Appleton S, Wilson DH, Taylor AW, Dal Grande E, Chittleborough C, Gill T, Ruffin R. Population comparison of two clinical approaches to the metabolic syndrome: implications of the new International Diabetes Federation consensus definition. Diabetes Care. 2005;28:27772779. Athyros VG, Ganotakis ES, Elisaf M, Mikhailidis DP. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr Med Res Opin. 2005;21:1157-1159. Ford ES. Prevalence of the metabolic syndrome defined by the international diabetes Federation among adults in the u.s. Diabetes Care. 2005;28:2745-2749. Lorenzo C, Serrano-Rios M, Martinez-Larrad MT, Gonzalez-Sanchez JL, Seclen S, Villena A, Gonzalez-Villalpando C, Williams K, Haffner SM. Geographic variations of the International Diabetes Federation and the National Cholesterol Education Program-Adult Treatment Panel III definitions of the metabolic syndrome in nondiabetic subjects. Diabetes Care. 2006;29:685-691. Saely CH, Koch L, Schmid F, Marte T, Aczel S, Langer P, Hoefle G, Drexel H. Adult Treatment Panel III 2001 but not International Diabetes Federation 2005 criteria of the metabolic syndrome predict clinical cardiovascular events in subjects who underwent coronary angiography. Diabetes Care. 2006;29:901-907. Balkau B, Charles MA, Drivsholm T, Borch-Johnsen K, Wareham N, Yudkin JS, Morris R, Zavaroni I, van Dam R, Feskins E, Gabriel R, Diet M, Nilsson P, Hedblad B. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabetes Metab. 2002;28:364-376. Hanson RL, Imperatore G, Bennett PH, Knowler WC. Components of the "Metabolic Syndrome" and incidence of type 2 diabetes. Diabetes. 2002;51:3120-3127. Rutter MK, Meigs JB, Sullivan LM, D'Agostino RB, Sr., Wilson PW. Insulin resistance, the metabolic syndrome, and incident cardiovascular events in the Framingham Offspring Study. Diabetes. 2005;54:3252-3257. Meigs JB. Definitions and mechanisms of the metabolic syndrome. Curr Opin Endocrinol Diabetes. 2006;13:103-110. Table 1: Baseline Characteristics According to ATP3 Metabolic Syndrome and Insulin Resistance Category No ATP3 MetS ATP3 MetS No IR IR No IR IR p-value N 1764 259Ź 340 440 Age (years) 52.3 53.1 56.6 56.2 <.0001 Sex (% female) 60.7 40.5 54.1 40.9 <.0001 Waist circumference (cm) 86 96 98.3 105.5 <.0001 Systolic Blood Pressure (mm Hg) 119 124 135 137 <.0001 Diastolic Blood Pressure (mm Hg) 72 76 79 80 <.0001 HDL cholesterol (mmol/l) 1.45 1.24 1.12 1.04 <.0001 Triglycerides (mmol/l) 1.08 1.39 2.02 2.13 <.0001 Fasting Glucose (mmol/l) 5.1 5.4 5.4 5.7 <.0001 2-hr OGTT glucose (mmol/l) 5.4 6.1 6.3 6.9 <.0001 BMI (kg/m2) 25.3 28.5 29 31.8 <.0001 Parental History of DM (%) 15.2 22.8 16.8 21.8 0.0006 LDL cholesterol (mmol/l) 3.2 3.4 3.6 3.4 <.0001 Smoking (%) 18.9 14.7 22.1 16.6 0.08 Data are mean values for continuous variables, proportions (%) for categorical variables and p-values from 3 d.f. ANOVA for overall comparisons Table 2. Relative Risks for Incident Type 2 Diabetes or CVD by ATP3, IDF or EGIR Metabolic Syndrome and/or Insulin Resistance Category Multivariable-Adjusted† Age-Sex-Adjusted ATP3 IDF EGIR ATP3 IDF EGIR 10.5 (6.5-16.9) d 0.78 76 8.1 (5.6-11.7) d 0.78 57 3.5 (2.2-5.6) d 0.84 55 2.6 (1.7-4.0) d 0.83 42 4.6 (2.7-7.7) d 0.85 66 3.3 (2.1-5.1) d 0.84 45 1.0 2.0 (0.9-4.3) 3.0 (1.6-5.7) c 6.0 (3.3-10.8) d 0.85 50 1.0 1.5 (0.5-4.1) 3.6 (1.9-6.8) d 6.9 (3.7-13.0) d 0.85 55 1.0 0.9 (0.4-2.4) § 3.2 (2.0-5.1) d 0.84 44 1.8 (1.4-2.3) d 0.73 21 1.8 (1.4-2.3) d 0.73 18 1.7 (1.3-2.3) d 0.74 23 2.1 (1.6-2.7) d 0.73 19 1.0 1.2 (0.7-1.9) 1.3 (0.9-1.9) 2.3 (1.7-3.1) d 0.73 18 1.0 1.6 (1.0-2.7) 1.6 (1.1-2.2) a 2.2 (1.6-3.0) d 0.73 17 1.0 0.7 (0.4-1.5) § 2.0 (1.6-2.7) d 0.74 19 aROC PAR% Insulin Resistance* aROC PAR% Type 2 Diabetes 8.6 (5.7-12.9) d 0.78 67 6.5 (4.4-9.4) d 0.76 58 No MetS/No IR No MetS/IR* MetS/No IR* MetS/IR* aROC (MetS/IR) PAR% (MetS/IR) 1.0 3.4 (1.6-7.1) b 5.4 (2.9-9.9) d 16.7 (10.2-27.4) d 0.82 56 1.0 2.4 (0.9-6.7) 5.9 (3.2-11.0) d 19.0 (11.0-32.8) d 0.82 61 1.0 1.4 (0.6-3.6) § 8.4 (5.7-12.3) d 0.78 57 MetS* aROC PAR% Insulin Resistance* aROC PAR% 1.8 (1.4-2.4) d 0.71 21 1.8 (1.4-2.3) d 0.70 18 1.8 (1.4-2.3) d 0.71 24 2.0 (1.6-2.7) d 0.71 19 No MetS/No IR No MetS/IR* MetS/No IR* MetS/IR* aROC (MetS/IR) PAR% (MetS/IR) 1.0 1.2 (0.8-1.9) 1.4 (1.0-2.1) 2.3 (1.7-3.1) d 0.71 18 1.0 1.7 (1.1-2.8) a 1.7 (1.2-2.4) b 2.2 (1.6-3.0) d 0.71 17 1.0 0.8 (0.4-1.6) § 2.0 (1.5-2.7) d 0.71 19 MetS* CVD P values are a, p<0.05; b, p<0.01; c, p<0.001, d, p<0.0001 * Referent is no MetS, no IR, or no MetS/No IR; aROC = area under the receiver operating characteristic curve; PAR% = population attributable risk † Multivariable-adjusted = for DM: parental history of diabetes, BMI, and 2hr OGTT glucose; for CVD: LDL cholesterol and smoking § All with EGIR MetS are insulin resistant; there is no EGIR MetS/No IR category 3.5 DM ATP3 IDF EGIR CVD Percent per Year 3.0 2.5 2.0 1.5 1.0 * * 0.5 0.0 No MetSNo IR ATP3 IDF EGIR 21 16 43 No MetSIR MetSNo IR 11 5 5 22 27 * MetSIR 81 87 87 No MetSNo IR No MetSIR MetSNo IR 107 91 143 22 21 9 36 52 * MetSIR 75 76 88 Figure. Annualized incidence rates of type 2 diabetes (DM, left-hand panel) or cardiovascular disease (CVD, right-hand panel) by ATP3, IDF, or EGIR metabolic syndrome (MetS) with or without insulin resistance (IR). Number of DM or CVD events are given below each category. * By defintion all subjects with EGIR metabolic syndrome had insulin resistance.