Corporate Compliance and Ethics Office Oversight of FWA Activities
advertisement

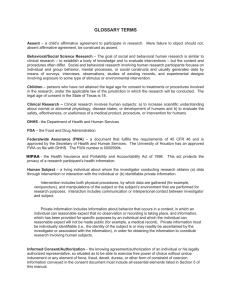
Corporate Compliance and Ethics Office Oversight of FWA Activities [Name] maintains a comprehensive compliance plan to detect, correct and prevent fraud, waste and abuse (“FWA”). FWA is integral to [Name’s] compliance program and applies to all [Name] business including commercial plans, Medicare Advantage plans, Medicare Prescription Drug plans, and Medicaid managed care plans. The [Name] commitment to detection, correction and prevention of FWA includes: Designation of a Special Investigation Unit (“SIU”) staffed by a Medical Director, and experienced nurses and investigators; Investment in state of the art analytical software; Partnership with and oversight of the pharmacy benefit manager’s (“PBM”) SIU and its FWA activities; Routine audits based on risk assessments; Designation of a Compliance Program Integrity Officer The Compliance Program Integrity Officer (“PIO”) is responsible for providing guidance to and oversight of CHC fraud, waste and abuse activities. The PIO reports to the Chief Compliance Officer and works closely with the [Name] Medicare, Medicaid and Commercial Compliance Officers to support FWA requirements. The PIO collaborates with the Customer Service Organization (“CSO”) recovery department, the SIU and the PBM to provide guidance and oversight for FWA reporting, monitoring, investigations, analysis of system vulnerabilities, and corrective actions. The Compliance Program oversight of FWA activities includes but is not limited to the following: 1. Verifying written fraud, waste and abuse policies and procedures are developed and maintained, including but not limited to: a. identification of FWA in the provider network b. voluntary self-reporting of potential fraud to the appropriate government authorities c. responding timely to data requests from government authorities or their designees d. conducting timely and reasonable investigations into potential FWA e. coordinating and cooperating with MEDICs, CMS, Medicaid Fraud Control Units (MFCU), State Attorneys General, State OIG, and law enforcement audits and requests for information f. receipt and management of FDR reporting of potential FWA 2. Verifying monitoring, including but not limited to: a. identification of overpayments and underpayments at any level and properly reporting and repaying where applicable Approval Pending Confidential, Proprietary and FOIA Exempt Corporate Compliance and Ethics Compliance Oversight of FWA Activities b. identification of claims submitted or prescribed by an excluded or deceased provider, and reporting and repaying any overpayments c. review of OIG, SAM/GSA and state exclusion lists: i. Prior to hire, appointment, election or contracting for all new employees, including officers and directors, board members, providers, FDRs (including broker/agents) and FDR employees assigned to [Name] business ii. Monthly for all employees, including officers and directors, board members, providers, and FDRs (including broker/agents) and FDR employees assigned to [Name] business 3. Developing and facilitating delivery of FWA training/education to all employees, board members, officers, FDRs (including brokers/agents) and FDRs’ employees assigned to [Name] business. 4. Periodic review and distribution of FWA reporting methods 5. Development, annual review, and adoption of a comprehensive Anti-Fraud Plan 6. Providing, or ensuring the provision of, monitoring reports to the Medicare Compliance Officer, Medicaid Compliance Officer, Commercial Compliance Officer, Chief Compliance Officer, and the corresponding compliance committees that includes but are not limited to: a. investigation outcomes b. drug utilization reports that identify possible therapeutic abuse or illegal activity by an enrollee c. reports on prescribing patterns by physicians to identify possible provider/prescriber or pharmacy fraud d. geographic zip code reports to identify possible doctor shopping or script mills e. reports on specific high risk Medicare counties f. reports on claims system recognition and edits g. reports on providers with a history of complaints h. member fraud i. medical/provider fraud j. OIG/SAM_GSA/state exclusions FWA Oversight Structure Health Plan FWA committees, including commercial, Medicaid and Medicare program requirements Page 2 of 4 Corporate Compliance and Ethics Compliance Oversight of FWA Activities o SIU/Recovery to provide Health Plan specific reports of FWA activity (dashboards) including PBM data, and provider exclusion/debarment actions o Agent Oversight to provide Health Plan specific reports of FWA activity o PIO is an ex officio member of the Health Plan FWA Committees o Chaired by Health Plan compliance personnel o Reports/meeting minutes distributed to the PIO Commercial Compliance Committee o Commercial product summary reports of FWA activity (dashboards) including PBM data, provider exclusion/debarment actions, and recommendations to the PBM for pharmacy audits and/or termination from the [Name] network. o Agent Oversight to provide specific summary reports of FWA activity o Vendor Oversight to provide summary FDR exclusion report o PIO is a member of Commercial Compliance Committee o Chaired by Commercial Compliance Officer Medicare Compliance Committee o Medicare FWA Sub-Committee to provide Medicare specific reports of FWA activity (dashboards) including PBM data, MEDIC referrals, provider exclusion/debarment actions, and recommendations to the PBM for pharmacy audits and/or termination from the network. o Agent Oversight (as applicable) to provide Medicare specific and summary reports of FWA activity o Vendor Oversight to provide FDR exclusion report (as applicable) o PIO is a member of Medicare Compliance Committee, and the FWA SubCommittee . o Chaired by Medicare Compliance Officer Medicaid Compliance Committee o SIU/Recovery to provide Health Plan specific and/or summary reports of FWA activity (dashboards) including PBM data, and provider exclusion/debarment actions o PIO is a member of the Medicaid Compliance Committee o Chaired by Medicaid Compliance Officer Chief Compliance Officer o PIO to provide summary reports from Health Plan FWA committees, Medicare Compliance Committee, Medicaid Compliance Committee and ad hoc reports as requested o Submits reports on FWA oversight to the Audit Committee of the Board of Directors Page 3 of 4 Corporate Compliance and Ethics Compliance Oversight of FWA Activities Page 4 of 4