Standard Operating Procedure for Ambulatory Blood Pressure
advertisement

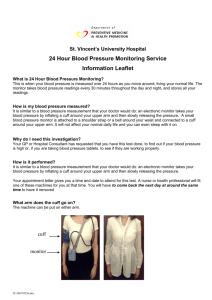
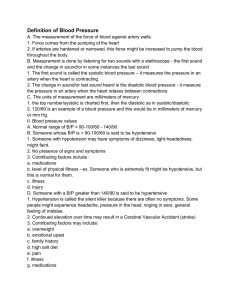
Standard Operating Procedure for Ambulatory Blood Pressure Monitoring (ABPM) This includes day & night time instructions The Clinical Indications for ABPM include Diagnosis of hypertension including the detection of: o Possible white coat hypertension o Unusual variability of blood pressure o Evaluation of nocturnal hypertension Treatment of Hypertension: o Informing equivocal treatment decisions o Evaluation of drug resistant hypertension o Determining the efficacy of drug treatment over 24 hours o Evaluation of symptomatic hypotension Diagnosis and treatment of hypertension in pregnancy ABPMs will be carried out by staff trained as competent in this procedure The ABPM must be comfortable for the patient to wear. An appropriately sized cuff containing the correct size bladder must be used. See BHS Poster: How to Measure BP with an Electronic Monitor The operator must: o be familiar with the equipment o know the calibration procedures for the device o know the normal ranges of blood pressure during the day and night o be aware of the factors influencing the diurnal pattern o Give the necessary time to instruct the patient so as to obtain as many measurements as possible (aiming for 100%) during the recording period Patients for ABPM must be capable of coping with and caring for the recorder Normal activity should be maintained during ABPM except when measurements are being made, except driving The patients arm should be still and held at heart level during measurement Recordings are usually programmed for every 30 minutes during the day (07.00 – 22.00) and 60 minutes at night (22.00 to 07.00). These times should be changed if the patient works at night You may wish patients to keep a diary of activities and symptoms during the recording period. If recording overnight, they must state when they went to bed, when they woke up and what time they took their medication, including over-the-counter medicines Initialising the Monitor Initialise according to manufacturer’s instructions Page 1 of 3 To put Monitor on Patient Ask patient to remove his/her top only. Switch monitor „on‟ and place inside pouch. Show the patient the on/off switch and explain the display screen before putting in the pouch. Place cuff on non-dominant arm unless there is a 20/10mmHg difference between arms in which case use arm with higher reading, or a clinical reason not to use a particular arm (eg lymphoedema). Line up the arrow on the cuff near the brachial artery. Explain, as you are fitting the cuff, about the position and how to adjust the cuff if it slips. Use an appropriately sized cuff (with clothing removed, measure arm circumference half way between tip of shoulder & elbow). Use a large cuff extra large or small cuff according to manufacturer‟s instructions. Pull cuff Velcro until it’s a firm fit. Wind tubing around the back of the patient’s neck and down his/her front and attach tubing to the monitor. To start the readings Do one or two readings in clinic to make sure it is working; so you can explain to the patient how it works and how it will feel. Explain about the alert mechanism before and after the reading as you are doing this. Switch monitor ‘on’ and check the time is showing. Demonstrate to patient following manufacturer’s instructions. The cuff will inflate, and then deflate. If the first reading is successful, ask the patient to put his/her shirt back on, feeding tube through the shirt opening. Attach Monitor to belt and waist, making sure tube isn’t kinked. If “Error” occurs, check the ABPM Manual Check batteries are working. An error may occur if: The patient’s blood pressure is very high or very low If the heart beat is irregular If the patient is very obese. Battery life may be compromised and the cuff may take considerably longer to inflate If the cuff or monitor is faulty Other as per manufacturer’s checklist Reason unknown Explanation & Instructions to give to patient The operator should aim to achieve 100% successful readings. This is achieved by careful explanation of the procedure to the patient and the patient being able to carry out the instructions. Patients should receive verbal and written procedure training on the ABP monitor. 1 Tell the patient they must not talk or move during the measurement 2 Tell them to stand or sit still with their arm supported during the measurement. (They can support their arm with their other arm if they are standing or rest it on a desk, table, cushion or pillow when sitting) 3 The cuff must be at heart level whenever a measurement is done Page 2 of 3 4 If the monitor has an alert mechanism, tell them the monitor beeps during the day to warn them the cuff will start inflating 5 seconds later 5 Tell them it will then deflate. If the reading is successful it will beep (or other alert) again 6 It may be unsuccessful if they are on a train, getting on/off a bus, or talking. If there is no apparent reason for the error tell them to check the cuff is in the correct position and has not slipped, check the tubing has not kinked or that the tubing has not come apart 7 Show them how to put the tubing back on the monitor if it should come apart 8 If they are wearing the monitor at night, tell them to take the monitor off their belt and put on the same side as the cuff, so that none of the tubing is around their neck. Either put under a pillow or safely on a bedside table away from water glass 9 If asked to make a diary, give the patient a diary to complete. They must document the time they went to bed and time they woke up 10 Ask them to write in the diary the names, doses and times of any medicines (including over-the-counter) they took over the 24 hour period 11 Give them an instruction sheet on care of monitor. Tell them they must not shower, or allow the monitor to get wet 12 Tell the patient to return the monitor to the clinic at the instructed time the next day Removing the monitor The following day 1 Explain to the patient how to take the monitor off and turn it off at home. 2 They should complete the diary if appropriate and return with the monitor See Manufacturers Operation Manual for Caring for the equipment Changing batteries (it is important that the batteries are replaced regularly) Washing cuffs & cleaning bladders Trouble shooting Calibration of ABPM equipment- Checking Accuracy Downloading the data from the monitor To alter the sleep pattern According to Local Agreement: Saving and Printing the ABPM Data: Accessing results, Storage and back-up of the ABPM data: Reporting of ABPM Page 3 of 3