Increased Creatine Kinase MB in the Absence
advertisement

CLIN.
CHEM.
32/11,
2044-2051
(Washington
(1986)
University
Case
Conference)
Increased Creatine Kinase MB in the Absence of Acute Myocardial Infarction
Editors: Kwok-Ming Chan and Jack H. Ladenson
Presentor: Glenn F. Pierce
Discussants:
Glenn F. Pierce and Allan S. Jafte’
Measurement
of creatine
zymes plays a vital role in
infarction.
An increase
in
as objective
and definitive
However,
any test, even
value,
may
occasionally
kinase
(CK; EC 2.7.3.2)
isoenthe diagnosis
of acute myocardial
CK-MB has been used frequently
evidence
of myocardial
infarction.
one with such a high predictive
exhibit
resu!ts
unrelated
spontaneously
within
10 ruin,
sarily associated
with activity.
He was admitted
to the coronary-care
of a physical
cardiogram
to myocar-
dial infarction,
which can lead to incorrect
diagnosis
and (or)
cost!y and prolonged
evaluations.
Furthermore,
false-negative results may also occur, although
for CK determinations
these are most often related to errors in the time of sampling
rather than a lack of analytical
sensitivity.
Increases
of CK-MB
may be measured
in several
circumstances
in which
patients
have
not sustained
an acute
myocardial
infarction-the
result of either (a) real increases
of CK-MB
for reasons
other than myocardial
infarction
or
(b) interfering
substances
being
measured
as CK-MB
by
some
analytical
following
cases
serum
CK-MB
procedures
are examples
(false-positive
of situations
increases
in the
infarction.
We discuss
myocardial
absence
these
measurements
increases).
under
The
which
of apparent
acute
owing
to the presence
of interfering
experienced
two
without
associated
Increased
Muscle
Case
recent
CK-MB
1. Patient
onset
in Serum
A, a 41-year-old
of chest
tightness.
His
man,
past
medical
Case
9-m fall
to Skeletal
presented
history
with
to
acute
further
after Trauma
a
was
additional
clinical
do well
myocardial
patient
was
CK-MB
evidence
intermittent
increase
in
infarction.
discharged
complication.
2. Patient
E was a 20-year-old
off a roof. Initial
and radiological
man
examination
without
who
any
survived
revealed
a
multiple
fractures,
studies
indicated
contusions
to
pancreas,
kidney,
lung, and heart. Results
of cardiac examination
and electrocardiogram
were normal.
Both total CK
Neuromuscular
Increased
Vol. 32, No. 11, 1986
the
subsequently
Clinical Chemistry Case Conference
of the Division
of Laboratory
Medicine,
Departments
of Pathology
and Medicine,
Washington
University
School of Medicine, St. Louis, MO 63110. Correspondence should be addressed
to the conference
editors at this address.
‘Cardiovascular
Division,
Department
of Medicine, Washington
University
School of Medicine, St. Louis, MO 63110.
CHEMISTRY,
in
pattern
of the resulting
rapid increase
resembled
the pattern
in patients
and CK-MB
determinations
resembling
that in acute
The patient
subsequently
CLINICAL
distinct
increases
or electrocardiographic
despite
unremarkable
except
for six episodes
of numbness
in his
right arm during
the preceding
10 months,
associated
with
no diaphoresis
or radiation
of the numbness.
Each episode
2044
results
CK-MB,
the intramuscular
injection
he received
before
the
catheterization
was suspected
to be the cause of the increase.
When
CK-MB
and total
CK began
to decline,
another
intramuscular
injection
was administered
to test
with
of the Cases
where
of re-infarction
or extension
of the myocardium.
The first
occurred
after
a cardiac
catheterization
(which
showed
moderate
single-vessel
disease),
but because
the patient
The
Presentation
unit,
not neces-
examination
were unremarkable.
His electrorevealed
nonspecific
ST-segment
and
T-wave
No electrocardiographic
changes
evolved,
this hypothesis.
The
of CK-MB
temporally
substances.
was
abnormalities.
and results
of a radionuclide
ventriculogram
appeared
normal. Results
of laboratory
tests were within
normal
limits
on admission,
except
for total
CK activity
of 498 U/L
(normal
0-185
U/L). CK-MB
at admission
(measured
by an
ion-exchange
method)
was 12 U/L (5% of total). During
the
next five days CK-MB
activity
in the serum
decreased
to 4
UIL and total
CK to 120 U/L (Table
1). The patient
continued
cases,
not to negate
in the diagnosis
of
the usefulness
of CK-MB
myocardial
infarction
but to emphasize
the need for careful
clinical
and laboratory
interpretation
of results.
In addition,
we also review various
current
methods
of CK-MB
measurement and conditions
that can result in apparently
increased
CK-MB
and
resolved
Case
elective
had been
20 years.
Serum
3. Patient
treatment
showed
a temporal
myocardial
infarction
had an uncomplicated
CK-MB
in Patients
rise and fall
(Table
1).
recovery.
with
Diseases
C, a 67-year-old
man,
of diabetic
retinopathy.
well controlled
Triple-vessel
with insulin
coronary-bypass
was
admitted
Diabetes
during
the
surgery
for
mellitus
preceding
has been
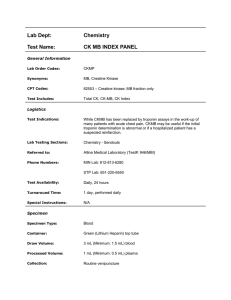
Table
Hospital day
Case
1. Creatine
Kinase
(U/L) Measurements
CK-MB
Time of
sampling
CK
Ion-exchange
Electrophoresls
Comments
1
01:00
06:00
416
295
12
6
2
5
09:00
06:00
191
131
4
3
6
7
06:00
17:00
120
450
4
10
IM injection
+
catheterization;
evidence of
cardiac
no
reinfarction
8
9
10
11
12
07:00
16:00
06:00
06:00
06:00
06:00
06:00
16
20
13
13
13
10
23
646
763
593
593
510
325
927
IM injection
14 h
earlier
13
16:00
06:00
1276
1045
28
25
No evidence
reinfarction
Discharge
14
Case
2
2
3
Case
1240
12736
7775
<15
>15
<15
(<5)
(>5)
(<5)
4263
3022
2972
3460
>15
>15
<15
<15
(<5)
(<5)
(<5)
(<5)
3
8
23:00
18:00
18:00
18:00
Results by agarose gel electrophoresis
four years
earlier
CK-BB
CK-BB
CK-BB
present
absent
absent
5
1
2
done
of
for intractable
angina.
The
in
U/L (and % of total CK).
patient
had
been
free of chest
pain since surgery
and had been
taking
procainamide
for four years for treatment
of postoperative
ventricular
ectopy.
Results
of physical
examination
on admission
were unremarkable.
His electrocardiogram
revealed
second-degree
AV block, with a rate of 40 beats/mm.
The patient
was
asymptomatic,
and blood-pressure
was within
normal
limits.
At the time of admission,
total
CK activity
in serum
was
578 U/L; CK-MB
was >15 UIL by agarose
gel electrophoresis (i.e., >5% of the total
CK).
The patient
was admitted
to the telemetry
unit and had a
pacemaker
inserted.
Over
the next two weeks he remained
asyrnptomatic,
with no electrocardiographic
changes,
chest
pam,
or hemodynamic
instability.
Values
for total
CK
varied from 249 to 595 U/L, and the proportion
that was CKMB as quantified
by the ion-exchange
method
ranged
from
12 to 23 UIL (normal
<12 UIL). Results
for isoenzymes
of
lactate dehydrogenase
(LDH; EC 1.1.1.27)
remained
within
normal
limits.
On further questioning,
the patient
reported
that for more
than six months
he had had difficulty
in arising
from
a
sitting
position
and in climbing
stairs.
Physical
examination demonstrated
a significant
degree
of proximal
muscle
weakness
and atrophy
in the lower
extremities.
Serum
aldolase
(EC 4.1.2.13)
activity
was 10.7 UIL (normal
1.5-8.1
UIL),
anti-nuclear
antibody
titer
was
1:2560,
with
a 3+
homogeneous
and rim pattern
of immunofluorescence,
and
anti-DNA
antibodies
were 3.3% (percent
of radiolabeled
DNA
bound;
resulted
from
norma!
the
0-4%).
diabetes
myopathy
may
also compatible
myositis.
Procainamide
but
This
was
have
with
procamnamide-induced
lupus
was
discontinued
and the patient’s
CK-MB
concentration
gradually decreased
to within
the normal
reference
interval.
Case 4. Patient
D, a 53-year-old
woman,
had been admitted to another
hospital
for complaints
of chest tightness,
fevers,
chills, and weakness.
Her past history
was significant for rheumatoid
arthritis
for 15 years and polymyositis
for 10 years.
The polymyositis
had, in the past,
been
responsive
to glucocorticoids.
She reported
having
been in
remission
for the last several
years, and she was taking
no
medication.
Examination
at the time of admission
demonstrated normal cardiac
function,
coarse rhonchi
at both lung
bases, joint deformities,
and proximal
muscle
weakness.
Her
electrocardiogram
showed
no abnormal
features.
At admission,
her value
for total
CK was 2680 UIL; CKMB (as measured
by an ion-exchange
method)
was 460 UIL.
The patient
became
increasingly
weaker,
and clinically
she was
thought
to be in congestive
heart
failure
from
myocardial
infarction;
for that reason
she was transferred
to
Barnes
Hospital
for further
evaluation.
Examination
after
transfer
showed
no change
from previous
findings,
and her
electrocardiographic
pattern
was still normal.
Total CK was
3108 U/L; CK-MB was >15 UIL as measured
by agarose
gel
electrophoresis
increased,
(<5%
but
activity
was
The patient
sone
for
the
23.1
was
relapsing
of total
isoenzyme
CK).
LDH
pattern
activity
was
was
normal.
slightly
Aldolase
U/L.
treated
with
polymyositis,
CLINICAL
CHEMISTRY,
methotrexate
and
showed
and prednia dramatic
Vol. 32, No. 11,
1986
2045
improvement
in strength
within
one week. At the time of
discharge,
her value for total CK was 1788 U/L, and CK-MB
remained
>15 U/L by agarose
gel electrophoresis
(<5% of
total).
Increased
Serum
CK-MB
in a Hypothyroid
Patient
5. Patient
E was a 54-year-old
woman
who was
admitted
for evaluation
of her insulin-dependent
diabetes
mellitus.
She had no past history
of symptomatic
heart
disease.
On admission,
she was noted
to have
signs
of
hypothyroidism,
including
coarse,
dry skin and prolonged
relaxation
times for deep-tendon
reflexes.
Chest roentgenogram
revealed
a globular
heart, echocardiogram
a pericardial
effusion,
and the electrocardiogram
a
low QRS voltage.
Laboratory
analysis
gave the following
results: total thyroxin
concentration
<25 p.gfL (normal
50110 j.tgfL), triiodothyronine
uptake
26.5% (normal
35-45%),
thyroxin
index <6.6 (normal
17.5-49.5),
and thyrotropin
concentration
33.9 milli-int.
units/L
(normal
0.45-6.2).
Total CK activity
was markedly
above normal
at the time of
admission
(4263 U/L) and CK-MB
as determined
by electrophoresis
was >15 U/L on two occasions
(Table
1). The
proportion
of CK that was CK-MB remained
<5% throughout her hospitalization,
and LDH isoenzyme
activities
were
within
The
normal
patient
recovered
limits.
began
thyroxin
replacement
therapy
and
uneventfully.
Discussion
Creatine
Kinase
Isoenzymes
Creatine
kinase
exists in three mu!timo!ecular
forms or
isoenzymes:
MM, MB, and BB. The active
form of each
isoenzyme
consists
of dimers
of M and B subunits
(1), each
subunit
having
a molecular
mass
of 42 000 Da. Depending
on the sampling
site (2,3), 8 to 20% of the total CK activity
in myocardial
tissue is from CK-MB.
This variability
in the
CK-MB
content
of various
parts of the myocardium
may
partly explain
the variability
in the CK-MB values observed
among
patients
whose
acute
myocardial
infarctions
are
thought
to be of similar sizes (3). In one recent report it was
suggested
that CK-MB is present only in diseased
myocardium, whereas
healthy
myocardium
resembles
skeletal
muscle, containing
essentially
only CK-MM
(4); this suggestion
has not yet been confirmed.
The current
belief is that CKMB is also present
in skeletal
muscle
but normally
at only
1% of the amount
of CK-MM
(2). However,
after
muscle
danage
or regeneration,
the fraction
of CK-MB can increase
transiently
to 7 to 12% of total CK in marathon
runners
(5,
6), or to 10-50%
in chronic
muscle
injury such as is seen in
Duchenne
muscular
dystrophy
(7). The magnitude
and
frequency
of increases
of serum CK-MB
in various
skeletal
muscle
disorders
have been reviewed
extensively
(8). Placenta and some tumor tissues
(10) may also contain
a small
amount
(<5% of total CK) of CK-MB,
but these rarely are
the source of an increased
CK-MB
in serum.
CK-BB
is found primarily
in brain (where
it makes
up
100% of total CK activity)
(2), prostate
(59-95%
of total CK)
(2, 11), placenta
(46-80%
of total CK) (2,9), gastrointestinal
tract (85-96%
of total CK) (2), and, infrequently,
in any of a
wide variety
of tumors
(2-100%
of total CK) (10). CK-BB,
given its short biological
half-life,
is rarely present
in the
serum
unless
there is ongoing
damage
to one of these tissues
(12-14).
Developmentally,
CK-BB
is the principal
isoenzyme
of fetal skeletal
muscle
during
the first and second
2046
CLINICAL
CHEMISTRY,
Vol. 32, No. 11, 1986
of gestation,
CK-MM.
Thus,
detectable
in this
skeletal-muscle
CK
but it is gradually
replaced
by CKafter
the sixth month, CK-BB is rarel
tissue
(15-17).
At term,
the infant’
consists
primarily
of CK-MM.
and
Diagnosis
Case
also
month
of Acute
The diagnosis
ally
has
been
Myocardial
of an acute
based
upon
Infarction
myocardial
the
triad
infarction
traditio
of characteristic
che
pain,
specific
electrocardiographic
abnormalities
(ST-se
ment changes
and Q waves),
and increased
concentrations
o
U) and CK enzymes
with specific isoenzyme
patterns
(18
20). However,
because
the differential
diagnostic
value o
chest pain is limited
and the electrocardiographic
chang
may have varying
degrees
of sensitivity
(44-83%)
(21-25
and specificity
(26-31),
measurement
of serum enzymes
as
reflection
of cell death still plays a vital role in the diagnosi
of acute myocardial
infarction.
Although
various
enzyme
[CK-MB,
LDH isoenzyme
1, aspartate
aminotransfer
(EC 2.6.1.1)1
or proteins
(e.g., myoglobin,
myosin
ligh
chains,
actin, troponin,
and tropomyosin)
are released
b
ischemic
and necrotic
myocardial
cells (32-40),
measur
ment of the majority
of them remains
of limited
diagnosti
usefulness
because
they are so poorly specific
or sensitive
At present,
measurement
of serum CK-MB
and LDH isoen
zymes are the principal
biochemical
approaches
for assess
ing myocardial
infarction,
as in the cases presented
here.
general,
LDH isoenzymes
are only measured
when infarction is thought
to have occurred
more than 24 h before the
diagnostic
samples
were collected.
Because
concentrations
of CK-MB
and LDH isoenzymes
peak in the serum
at different
intervals
after
an acute
myocardial
infarction,
proper sampling
times are essential
in ensuring
optimal
utility
of these enzyme
values.
In the
absence
of myocardial
re-perfusion,
CK-MB peaks
an average of 18 h after the onset of acute myocardial
infarction;
the
ratio of LDH isoenzyme
1 to LDH isoen.zyme
2 is greatest
about 72 h after onset (20). Thus, measurement
of CK-MB
allows
an acute
myocardial
infarct
to be detected
earliem
than
does measurement
of LDH
isoenzymes.
However,
because
CK-MB
values decline
more rapidly
(within
two tc
four days of infarction)
while LDH 1 may remain
increased
for seven to 14 days, measurement
of LDH 1 or of the ratio ol
LDH 1 to 2 is helpful
in patients
whose blood is sampled
more than 24 h after
a possible
infarct.
Serial
measurements of total CK and of CK-MB
every 12 h for 48 h is the
most sensitive
and
specific
way
to evaluate
the patient
suspected
of having
had an acute
myocardial
infarction.
Sustained
increases
of CK-MB
without
the characteristic
temporal
pattern
are unlikely
to be due to acute myocardia]
infarction.
Rather,
sustained
increases
of total
CK
and
CK-
MB may imply ongoing
muscle
damage
such as might be
seen
in myocarditis,
hypothyroidism
(case 5), or chronic
myopathic
diseases
(case 4), most of which are unlikely
to be
confused
with acute myocardial
infarction.
Because
most
patients
with
acute
myocardial
infarction
have
CK-ME
greater
than
5% of total CK activity,
it has been suggested
that the specificity
of the serum
CK-MB
assay can furthei
be enhanced
by monitoring
the percentage
of CK that is ME
(20).
Unfortunately,
the wide
variation
in the CK-ME
content
from one group of muscle
to another
or even within
the same muscle
group among patients,
and the higher
CK.
MB content
in those who exercise
(5, 6), limit the potential
utility
of any percentage
criteria.
Moreover,
percentagE
criteria
could be very difficult
to utilize
when
diagnosing
acute myocardial
infarction
in the presence
of concomitant
skeletal
muscle
injury.
The greater
the extent
of muscle
injury, the easier
it is to miss changes
in CK-MB
due to
cardiac
injury
because
the cardiac
CK-MB
is diluted
by
large quantities
of CK-MM,
thereby
decreasing
the percentage of CK-MB.
Additional
information
on the clinical
use of
CK and LDH isoenzymes
in the diagnosis
of myocardial
infarction,
the relationship
between
the onset of symptoms
of infarction
and appearance
and disappearance
of enzyme,
and comparison
of the diagnostic
sensitivity
and specificity
of CK-MB
and LDH 1 or ratio of LDH 1 to LDH 2 can be
found in several
reviews
(20, 32, 33,37,
38, 41).
Increases
Myocardial
in CK-MB
Infarction
Not Associated
with Acute
Although
an increase
in serum
CK is a specific diagnostic
‘indicator
for acute myocardial
infarction,
the CK-MB
can
also become
increased,
either
acutely
or chronically,
in
conditions
other
than
acute
myocardial
infarction.
The
increase
in serum
CK-MB
values
could be the result of the
combination
of either
(a) an increased
release
of nonmyocardial
CK into the circulation,
(b) increase
due to
cardiac
injury
other than infarction,
or (c) decreased
clearance of CK-MB
from the blood.
Increase
in serum CK-MB
due to increased
release of nonmyocardial
CK. The most common
cause of increased
release of non-myocardial
CK into the circulation
is injury to
muscle
such as occurs with major trauma
(including
burns,
electrical
injuries,
crush
injuries,
and noncardiothoracic
surgery),
grand
mal seizures,
acute
alcoholic
myopathy,
hyperthennia
and hypothermia,
cardiopulmonary
resuscitation, defibrillation,
and intramuscular
injections
(42-47)
(Table 2). Two types of increases
can occur,
one due to the
release
of a small amount
of CK-MB
from
muscle
and one
due to skeletal
muscle
regeneration,
which may result
in
increased
B subunits
of CK in the muscle
itself. Reportedly,
a substantial
percentage
(30%) of burn patients
(45) and a
small
percentage
of patients
with severe
trauma
to their
skeletal
muscle
can have >10% CK-MB
in their serum
(19,
48). However,
in most cases the serum
CK-MB
does not
increase
and the percentage
of CK-MB
to total CK activity
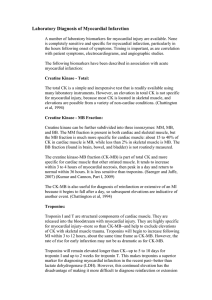
Table 2. Causes
of CK-MB Increases Not Associated
with Acute Myocardlal Infarction
Release
of nonmyocardial
CK
Trauma to muscle
crush
injury
bums
electrical
injuries
noncardiothoracic
surgery
extreme exercise
Grand mal seizures
Various inflammatory
and noninflammatory
chronic renal failure
hypothyroidism
chronic alcoholism
Hyperthermia
and hypothermia
Cardiopulmonary
myopathies
63).
resuscitation
Defibrillation
Intramuscular injections
Cardiac injury other than acute myocardia!
Cardiac contusions from trauma
Cardiothoracic surgery
Myocarditis
Decreased
clearance
of serum
Hypo- and hyperthyroidism
CK-MB
remains
low, as illustrated
in case 1. Interestingly,
in this
case, intramuscular
injection
resulted
in a four- to five-fold
increase
in total
CK and a two-fold
increase
in CK-MB
(Table
1). Although
such
increases
in serum
CK-MB
may
rarely
be sustained,
the same temporal
pattern
can often be
seen in patients
with concomitant
myocardial
infarction,
or
in cases in which
damage
to myocardial
tissues
was also
involved
(47, 49). Thus often it is difficult
to correlate
CKMB (in absolute
values or percentage)
with cardiac injury in
trauma
victims
(50). This is illustrated
in case 2, where
trauma
from a fall from a roof led to skeletal-muscle
damage
and cardiac
contusion.
After
muscle
injury, profound
exercise,
or in a variety
of
acute or chronic
inflammatory
and noninflammatory
myopathic
states
such as occurred
in cases
3 and 4, repair
processes
cause regeneration
of muscle
fibers more similar
to that of neonatal
life. This can result in the increase
in the
proportion
of both CK-MB
and CK-BB.
For example,
the
proportion
of CK-MB in muscle can become
as great
as 8.9%
after long-distance
running
(5, 6, 48). In these situations
serum
CK-MB
can become
increased
as a result
of an
increased
proportion
of CK-MB
within
skeletal
muscle
combined
with its increased
release
into the circulation
(8,
42-44,51-56).
Except
in rare cases (51) the increase
of CKMB is usually
sustained
instead
of being as temporary
as in
myocardial
infarction.
Thus
if the temporal
pattern
or
clinical
course of the patient
with increased
CK-MB
is not
compatible
with an acute infarction,
reinfarction,
or extension, more-chronic
causes
of increased
CK-MB
activity
should be considered.
Chronic
renal
failure,
and occasionally
hypothyroidism,
can also cause an increased
value for serum CK-MB
as a
result
of myopathies
associated
with these diseases
(43, 53,
54). Likewise,
the increase
in CK-MB
is persistent
and the
proportion
of CK-MB
generally
remains
low, as is illustrated here by case 5.
There are other rare causes
of increased
serum
CK-MB.
Placenta
contains
increased
CK-MB
and has been reported
to be the source of increased
serum
CK-MB
values
on rare
occasions
(9). One case report of increased
serum
CK-MB
(42-66%)
due to ectopic CK-MB
production
was reported
in
a patient
with colon carcinoma
(57). Recently,
Ng et al. (58)
reported
an unusual
case of increased
serum CK-MB
activity in a patient
with theophylline
intoxication.
Increased
serum CK-MB
due to cardiac
injury other than
acute myocardial
infarction.
CK-MB
can be released
in any
type of myocardial
injury,
not just myocardial
infarction:
in
cases of cardiac
contusions
resulting
from trauma
(case 2),
as well as after cardiothoracic
surgery
(48,59-61)
(Table 2)
and in myocarditis
due to viral, autoimmune,
or metastatic
involvement
of myocardium
(20). Pericarditis
in the absence
of myocarditis
has not been shown
to increase
serum
CKMB. Coronary
arteriography,
uncomplicated
angioplasty,
and hemodyn.amic
monitoring
seldom
cause an increase
in
CK-MB
that exceeds
the normal
reference
interval
(50, 62,
infarction
Increase
in serum
CK-MB
due to decreased
clearance
of
enzyme.
Changes
in clearance
of serum
enzymes
by the
reticuloendothelial
system
can be induced
by hypothyroidism and hyperthyroidism
(Table
2). Thus,
in addition
to
causing
myopathy,
hypothyroidism
can also lead to delayed
clearance
of CK-MB from serum-and
both of these can lead
to an increased
concentration
of CK-MB.
However,
the
increased
CK-MB
concentration
will persist until the hypemetabolic
state
is resolved,
so it is relatively
simple
to
CLINICAL CHEMISTRY,
Vol. 32, No. 11, 1986
2047
distinguish
between
the increase
and decrease
levels expected
in patients
with acute myocardial
and those associated
with hypothyroidism.
increases
in CK-MB
Interferences
in enzyme
infarction
due to Methodological
CK-MB can be detected
by a variety
of analytical
methods
that are based on charge
differences
in the CK isoenzymes
or on immunological
reactivity.
Attempts
to rely on differences in the kinetic
properties
of the isoenzymes
have not
proven effective
(64). The reported
sensitivity
and specificity
of the various
methods
for diagnosing
acute
myocardial
infarction
vary
widely-such
variation
could in part be
related
to the patient
populations
studied
and the time of
sampling
CK-MB
rather
than to differences
in analytical
procedures
(20, 65, 66).
Methods
based on differences
in charge.
At present,
electrophoretic
separation
of CK-isoenzymes
on agarose
gel
followed
by their identification
by catalytic
activity
remains
the most commonly
utilized
procedure
(Table
3) (67). The
amount
of CK-MB
present
is either
estimated
by visual
comparison
with a standard
of known
CK-MB
activity
or
quantified
by densitometric
scanning
(68, 69). Although
electrophoresis
is a specific
method
for detecting
CK-MB,
it
is only semiquantitative
and is time consuming,
technically
tedious,
and has too-limited
analytical
sensitivity
(detection
limit, 5 U/L). A percentage
criterion
is implicit
with this
technique.
In general,
samples
with a total activity
concen
tration
of >300
U/L are diluted
to 300 U/L before bein
applied
to the gel. Thus the proportion
of CK-MB
m
exceed 2% for it to be detected.
“Atypical
CK” variants
sue
as macro CK-1 and macro
CK-2 circulating
in plasma
readily
detected
by electrophoresis.
Detailed
discussions
o
these various
atypical
forms of CK isoenzynles
can be foun
in a recent review (66). Usually,
macro CK-1 represents
th
macromolecular
complex
produced
when CK-BB is linked
imniunoglobulins,
but in a few cases CK-MM-immunoglo
ulin (IgA) complexes
have also been reported.
Macro CKappears
to be an oligomeric
form of mitochondrial
CK tha
migrates
cathodally
from or very close to CK-MM.
Bot
macroCKs
may be found in asymptomatic
normal
individ
uals, but macro CK-1 has been observed
more frequently
i
elderly
women,
and it has no correlation
with
distin
diseases.
In contrast,
macro CK-2 is often seen in the plasm
of severely
ill patients,
frequently
those
suffering
fro
malignant
diseases
or hepatic
cirrhosis
(65, 70, 71). Th
amount
of macro CK-2 present
in the serum
does not seem
to correlate
with the stage
of malignancy
(71) but may
parallel
the course
of nonmalignant
diseases
(70). These
atypical
CK bands
generally
migrate
between
CK-MM
and
CK-MB
and therefore
should
rarely
pose any analytical
problem for those experienced
with the electrophoretic
technique (72). However,
their presence
may interfere
with CKMB measurement
by non-electrophoretic
methods.
Table 3. Assays of CK-MB
S.nsltlvfty
Specificity
Interference
Frequency
Nature olauay
Adenylate
of use’
Activity-concentration
CK-MM
CK-BB
Macro CK-1
Macro CK-2
klnase
no
no
no
no
no
Comments
assays
Separation by charge
Electrophoresis
81%
98
99
Fluorescent
compounds
(drugs or bilirubin)
may complex with
albumin and migrate
close to CK-MB.
Assay only
semiquantitative.
9%
Ion exchange
Immunoinhibition
7%
99
95
85
96
-
90
90
-
85
80
±
yes
yes
yes
no
CK-MM, CK-BB, and
macro CKs may
interfere variably.
Measures
all but Msubunit activity. Assay
subject to multiple
yes
yes
yes
yes
±
±
no
no
no
Immunopptn.
step
designed to improve
the specificity of the
immunoinhibition
assay. High concns.
of CK-MM and CK-BB
still interfere,
no
±
±
±
no
no
no
no
no
no
BB and macro CK
interference
depends
on specificity of
antibody.
Presence of anti-goat or
anti-mouse
IgG
antibodies in samples
of certain patients will
cause positive
interferences.
Immunoinhibition
immunopptn.
&
Mass-concentration
assays
Radioimmunoassay
(one antibody)
‘Sandwich’
enzyme
immunoassay
(two antibodies)
>90
-
>95
interference.
‘Derived
2048
from references 20, 41, 63-66.
CLINICAL
CHEMISTRY,
Vol. 32, No. 11, 1986
In addition,
certain
fluorescent compounds such as bilirubin or drugs can bind to albumin
and interfere
with the
electrophoresis
procedure
because
they migrate
near the
CK-MB band (73-75).
Increased
binding
of fluorescent
compounds
has been reported
in patients
with chronic
renal
failure
(76). That
these
fluorescent
bands
are artifacts
related
to fluorescent
compound/albumin
complexes
can be
confirmed
by their
persistence
when
the agarose
gel is
examined
under ultraviolet
light in the absence
of specific
substrate
for CK (74).
Ion-exchange
separation
of CK
isoenzymes
on either
columns
(77, 78) or glass beads (79) followed
by catalytic
CK
measurement
is another
common
method
of quantifying
CK-MB activity.
The bead method
can detect CK-MB activity of <5 U/L, is rapid, is generally
not affected
by macro
CKs, and there is little carryover
of CK-MM
into the CKMB fraction
(79). However,
it measures
all B subunit
activity-i.e.,
both MB and BB. In a more general
hospital
population,
an incidence
of increased
CK-BB
of up to 3.2%
has been reported
(80) and could result in falsely
increased
CK-MB as measured
by this method.
The original
automated ion-exchange
chromatographic
method
used in the Du
Pont aca suffers
numerous
problems,
ranging
from positive
interference
with
CK-BB
or CK-MM
in some patients,
owing to incomplete
retention
of these isoenzymes
on the
column
(81, 82), sensitivity
to ionic strength
of the eluting
buffer and the serum
matrix
(81), and falsely increased
CKMB values
for heparinized
plasma
samples
(83).
Subsequently,
this method
has been modified
to decrease
positive
interference
by CK-MM
by adding anti-CK-MM
antibodies,
which inhibit
the M subunit
catalytic
activity
(84). The new
method,
however,
reportedly
is still adversely
affected
by
atypical
CK enzymes
(85).
Like the measurement
of total CK, the measurement
of
CK-MB activity
can be influenced
by the presence
of adenylate kinase
(EC 2.7.4.3),
which can be released
from erythrocytes during
hemolysis
or from damaged
tissue
such as
muscle,
liver, or platelets;
and can act on ADP, the substrate
in the creatine
kinase
assay,
to generate
additional
amounts
of ATP, thereby
increasing
the apparent
creatine
kinase
activity
(86, 87). False-positive
reaction
due to the presence
of adenylate
kinase
can be assessed
by including
an individual sample
blank
in which
creatine
phosphate
is omitted
from the reagent
(88). However,
a better
approach
is to
include
inhibitors
of adenylate
kinase
in the reagent,
such
as adenosine
monophosphate
or diadenosine
pentaphosphate
(86, 87, 89).
Methods
based on differences
in immunological
reactivity.
Other
methods
of measuring
CK-MB
activity
are based on
the immunological
reactivity
of the CK-M and CK-B subunits with various
antibodies.
One of the earliest
approaches involved
addition
of anti-M antibodies
to serum to inhibit
the M-subunit,
followed
by quantification
of residual
Bsubunit
activity
(90-93).
The assay
measured
all but Msubunit
activity.
Thus, besides the B-subunit
of CK-MB,
the
assay
also measured
macro
CKs,
CK-BB,
and adenylate
kinase,
depending
on the reagent
composition.
Besides
suffering
from lack of specificity
and poor analytical
precision, the immunoinhibition
assay is also less sensitive
than
electrophoretic
and ion-exchange
methods
(Table 3) (20,41,
66,94).
Yet, because
of simplicity,
this assay is suggested
to
be useful
in screening,
because
it permits
a rapid turnaround.
All positive
results
should
be confirmed
by morespecific assays.
Attempts
to improve
the specificity
of immunoinhibition
assays
have resulted
in the addition
of an immunoprecipitation
step to remove
all M-subunit-containing
enzymes
in
a second
reaction
tube, by using specific
anti-M
antibodies
(95, 96). The remaining
CK-BB
and nonspecific
activity
is
measured.
The CK-MB
value
is calculated
by subtracting
the residual
CK activity
after immunoprecipitation
from
that obtained
from
the immunoinhibition
assay.
Initial
studies
with this assay
were favorable;
however,
interference by high concentrations
of CK-BB
or CK-MM
is still a
concern.
Other methods
of quantifying
CK-MB based on its immunological
reactivity
include
radioimmunoassay
or immunoenzymometric
assays.
The two-site
assay
is a common
approach
in which
specific
anti-B or anti-M antibodies
that
are attached
to a solid phase are used to extract
the CK-BB
and CK-MB
isoenzymes
or the CK-MM
and CK-MB
isoenzymes (85,97-101).
In immunoenzymometric
assays,
this is
followed
by the addition
of an anti-M
or anti-B
antibody
coupled
to either
horseradish
peroxidase
(EC 1.1.1.1.7)
or
alkaline
phosphatase
(EC 3.1.3.1),
which
can be measured
enzymatically
in the presence
of an appropriate
substrate.
The antibodies
utilized
in these
mass
assays
are either
monoclonal
or polyclonal.
The two-site
immunoassays
appear to be specific,
but sera of some patients
reportedly
cause false positive
interference
with at least
one of the
commercial
assays (102). Recently,
one of us has reported
an
unique
immuno-extraction
approach
involving
a monoclonal antibody
that reacts only with CK-MB
but not CK-BB,
CK-MM,
or mitochondrial
CK (102). The CK-MB extracted
by this antibody
on solid-phase
was then quantified
by its
enzymatic
activity.
Summary
Although
measurement
of CK-MB
is a very sensitive,
and cost-effective
test for use in diagnosis
or exclusion of acute myocardial
infarction,
it should not be used as
the sole diagnostic
indicator,
and all positive
values
must be
critically
analyzed
to exclude
other
causes
of increased
values
in serum.
This is particularly
important
when the
population
being tested
consists
of patients
with multiple
medical
problems,
with low to medium
probability
of myocardial
infarction,
and without
clinical
or other biochemical
(i.e., LDH 1) evidence
of acute myocardial
infarction.
When
the
temporal
pattern
and absolute
CK-MB
values
are considered
together
with the patient’s
clinical
status,
the diagnostic specificity
is dramatically
increased.
In addition,
one
must be familiar
with the limitations
of individual
assay
systems
in order to exclude
method-related
artifactual
values.
specific,
References
1. Lang H. Creatine kinase
ical application
[Review].
Verlag,
isoenzymes-pathophysiology
Berlin-Heidelberg-New
and clinYork:
Springer
1981.
2. Tsung
SH. Creatine kinase isoenzyme
patterns
in human
tissue
at surgery. Clin Chem 1976;22:173-5.
3. Marmor
A, Margolis
T, Alpan G, et al. Regional
distribution
of
the MB isoenzyme
of creatine
kinase in the human
heart. Arch
Pathol Lab Med 1980;104:425-7.
4. Ingwall
JS, Kramer
MF, Fifer MA, et al. The creatine
kinase
system in normal and diseased
human myocardiuni.
N EngI J Med
1985;313:1050-4.
5. Apple FS, Rogers MA, Sherman
WM, et al. Profile of creatine
kinase isoenzymes
in skeletal muscles of marathon
runners.
Clin
Chem 1984;30:413-6.
obtained
CLINICAL
CHEMISTRY,
Vol. 32, No. 11, 1986
2049
6. Siegel
creatine
AJ, Silverman
LM,
MB isoenzyme
kinase
Evans WJ. Elevated
levels in marathon
skeletal
muscle
J Am
runners.
Med Assoc 1983;250:2835-7.
7. Somer H, Dubowitz
V, Donner
M. Creatine
kinase isoenzymes
in
neuromuscular
diseases.
J Neurol Sci 1976;29:129-36.
8. Lott JA, Landesman
PW. The enzymology
of skeletal muscle
disorders
[Review]. Crit Rev Clin Lab Sci 1984;20:153-90.
9. Laboda HM, Britton
VJ. Creatine kinase isoenzyme
activity in
human
placenta
and in serum of women in labor. Clin Chem
1977;23:1329-32.
10. Tsung SH. Creatine kinase
activity
and isoenzyme
pattern in
various normal tissues and neoplasms. Clin Chem 1983;29:2040-3.
11. Kimler SC, Sandhu
RS. Circulating
CK-MB and CK-BB isoenzymes after prostate
resection. Clin Chem 1980;26:55-9.
12. Aleyassine
H, MacIsaac
SG. The diagnostic
significance
of
creatine kinase-BB
isoenzyme
in adenocarcinoma
of prostate.
Clin
Biochem
33. Galen RS, Reiffel JA, Gambino R. Diagnosis
of acute myocardial infarction.
Relative efficiency of serum enzyme
and isoenzyme
measurements
[Review].
J Am Med Assoc 1975;232:145-7.
34. Cairns
JA, Missirlis
E, Walker
WHC. Usefulness
of serial
determinations
of myoglobin
and creatine
kinase
in serum compared for assessment
of acute myocardial
infarction.
Clin Chem
1983;29:469-73.
35. Grenadier
E, Keidar 5, Kahana
L, et al. The roles of serum
myoglobin, total CPK and CK-MB isoenzyme in the acute phase of
myocardial
infarction.
Am Heart J 1983;105:408-16.
36. Fisher ML, Carliner NH, Becker LC, et al. Serum creatine
kinase
in the
diagnosis
of acute
myocardial
13. Goodman
ZD, Hamilton
SR. Transient
creatine
kinase
isoenzyme
BB activity after
increase
in
prostatectomy
serum
in a
DE, Savory
J, Wills MR. Serum lactate
isoenzymes
in the diagnosis
of myocardial
infarction
Clin Lab Sci 1982;12:408-1O.
patient with massive
benign prostatic
hyperplasia.
Clin Chem
1980;26:511-2.
14. Tsung SH. Circulating
CK-MB and CK-BB isoenzymes
after
gastrointestinal
surgery. J Clin Pathol 1982;35:200-3.
15. Goto I, Nagamine
M, Katsuki
S. Creatine
phosphokinase
isozyrnes in muscles. Arch Neurol
1969;20:422-9.
16. Tzvetanova
E. Creatine kinase isoenzymes
in muscle tissue of
patients with neuromuscular
diseases
and human fetuses. Enzyme
39. Kaplan
1971;12:279-88.
42. Eckfeldt
JH, Weir EK, Chesler
isoenzyme
MB in acute
and chronic
1981;105:1032-3.
CD,
Emery
AEH.
Changes
in creatine
kinase
and its
J Neurol
iaoenzymes
in human fetal muscle during development.
Sci 1975;24:483-92.
18. Hackahaw
BT. Myocardial
infarctions
and serum enzymes
[Editorial]. Clin Chem 1984;30:1285.
19. Wagner GS, Roe CR, Limbird LE, et al. The importance
of
identification
of the myocardial-specific
isoenzyme
of creatine
phosphokinase
(MB form) in the diagnosis of acute myocardial
infarction. Circulation
1973;47:263-9.
20. Lott JA, Stang JM. Serum enzymes
and isoenzymes
in the
diagnosis
and differential
diagnosis
of myocardial
ischemia and
necrosis
21.
[Review].
McQueen
accuracy
Clin
Chem
MJ, Holder
of serial
1980;26:1241-50.
D, El-Maraghi
electrocardiograms
NRH.
in the
Assessment
diagnosis
of the
of myocardial
infarction.
Am Heart J 1983;105:258-61.
22. Belier
5, Schor S, Kariv
I, et al. Evaluation
of electrocardiogram in emergency
room as a decision-making
tool.
Chest
1977;71:486-91.
23. McGuinness
JB, Begg TB, Semple T. First electrocardiogram
in
recent myocardial
infarction.
Br Med J 1976;2:449-51.
24. Rude RE, Poole WK, Muller JE, et al. Electrocardiographic
and
clinical criteria
for recognition
of acute myocardial
infarction
based
on analysis of 3,697 patients. Am J Cardiol 1983;52:936-42.
25. Fischl SJ, Herman
MV, Gorlin B. The intermediate
coronary
syndrome:
clinical,
angiographic
and therapeutic
aspects. N Engl J
Med
1978;288:1193-8.
26. Snvastava
SC, Robson AO. Electrocardiographic
abnormalities
associated
with subarachnoid
hemorrhage.
Lancet
1964ii:431-3.
27. Nora JR, Pilz CG. Pseudoinfarction
pattern associated
with
electrolyte disturbance.
Arch Intern
Med 1959;104:300-1O.
28. Fulton MC, Marriott
HJL. Acute pancreatitis
simulating
myocardial
infarction
in the electrocardiogram.
Ann Intern Med
1963;59:730-2.
29. Burch GE, DePasquale
of pulmonary
heart disease.
30.
NP. The electrocardiographic
Am J Cardiol
1963;11:622-38.
D, Susilavorn
B, Chou
manifestation
of pulmonary
Romhilt
graphic
TC. Unusual
embolism.
diagnosis
electrocardioAm Heart
J
40. Katus
light chains. Am J Cardiol
41. Lott JA. Electrophoretic
myocardial
ary):23-31.
infarction
markers
1984;54:964-70.
CK and LD isoenzyrne
[Review].
Lab
Management
for
assays
in
1983;(Febru-
E. Serum creatine
alcoholism.
Am
44. Ma KW, Brown DC, Steele BW, et al. Serum
MB isoenzyme
activity
in long-term
hemodialysis
Intern
Med 1981;141:164-6.
kinase
Heart
J
creatine
patients.
kinase
Arch
45. Shahangian
5, Ash KO, Wahlstrom
NO Jr, et al. Creatine
kinase
and lactate dehydrogenase
isoenzymes
in serum of patients
suffering
burns, blunt trauma,
or myocardial
infarction.
Clin Chem
1984;30:1332-8.
46. Reiffel JA, McCarthy
DM, Leahey
EB Jr. Does DC cardioversion affect isoenzyme
recognition
of myocardial
infarction?
Am
Heart J 1979;97:810-1.
47. Pauletto
P, Scannapieco
G, Compostella
L, et al. Myocardial
DC countershock:
myoglobin
and CK-MB
radioimmunoassay
evaluation.
Acts Cardiol 1984;34:115-20.
48. Jaffe AS, Garfinkel BT, Bitter CS, et al. Plasma MB creatine
kinase
after
vigorous
exercise
in professional
athletes.
Am J
Cardiol 1984;53:856-8.
damage
after
49. Kettunen
cardiography,
Chim
Acts
50. Potkin
nomnvasive
Circulation
P. CK isoenzymes
cardiac
and transaminases
surgery
and non-cardiac
after
coronary
thoracotomy.
Clin
1983;127:97-103.
RT, Werner JA, Trobaugh
GB, et al. Evaluation
of
tests of cardiac damage in suspected
cardiac contusion.
1982;66:627-31.
51. Keshgegian
AA (ed.). Serum
chronic
muscle
disease
[Lankenau
Chem 1984;30:575-8.
creatine
Hospital
kinase
Case
MB isoenzyme
in
Conference].
Clin
52. Tsung
SH, Huang
isoenzyme
MB activity
with dermatomyositis.
TY, Han D, et al. Total creatine kinase and
in serum and skeletal
muscle
of a patient
Clin Chem 1980;26:1912-3.
53. Larca U, Coppola
in dermatomyositis:
1981;94:341-3.
JT, Honig S. Creatine kinase MB isoenzyme
a non-cardiac
source.
Ann Intern
Med
54.
No. 11, 1986
Med
43. Siegel AJ, Dawson
DM. Peripheral
source
of MB band
of
creatine
kinase
in alcoholic
rhabdomyolysis.
Nonspecificity
of MB
isoenzyme for myocardial
injury in undiluted
serum samples.
JAm
Med Assoc 1980;244:580-2.
sive muscular
Vol.32,
and
Intern
HA, Yasuda
T, Gold HK, et al. Diagnosis
of acute
infarction
by detection
of circulating
cardiac myosin
myocardial
31. Haiat R, Chiche P. Transient
abnormal
Q waves in the course
of ischemic heart disease.
Chest 1974;65:140-4.
32. Roberts
R. The two out of three criteria
for the diagnosis
of
infarction.
Is it pass#{233}?
[Review]. Chest 1984;86:511-3.
CLINICAL CHEMISTRY,
infarction
dehydrogenase
[Review]. Ann
LA, Stein
EA. In search
of biochemical
MI. Diagnostic
Med 1985;(February):25-33.
acute
1970;80:237-41.
2050
Optimal
1980;140:329-34.
38. Bruns
1980;13:109-12.
17. Foxall
infarction.
sampling frequency. J Am Med Assoc 1983;249:393-4.
37. Irvin RG, Cobb FR, Roe CR. Acute myocardial
MB creatine
phosphokinase
[Review].
Arch
Tzvet.anova
E. Serum
dystrophy.
55. Asseo PP, Panidis
analysis
56.
in thyroid
Goldman
creatine
Enzyme
DK. Creatine
disorders
J, Mats
kinase
[Letter].
R, Mortimer
isoenzymes
in
progres-
1978;23:238-45.
kinase
Clin
activity
and isoenzyme
Chem 1984;30:1107-8.
R, et al. High
elevations
of
creatine
phosphokinase
in hypothyroidism.
An isoenzyme
J Am Med Assoc 1977;238:325-6.
57. Annesley
TM, McKenna BJ. Ectopic
duction
in metastatic
cancer.
analysis.
activity
with
creatine
Am J Clin
Pathol
kinase
MB pro-
1983;79:255-9.
82.
kinase
isoenzyme
Chem
1985;31:1741-2.
83. Lang
for CK-MB
59.
Raabe
DS Jr, Morise
A, Sbarbaro
JA, et al. Diagnostic
criteria
84.
for acute myocardial
infarction
in patients undergoing
coronary
artery bypass surgery. Circulation
1980;62:869-78.
60. Devine JE, Spats LA. Creatine
kinase (CK) isoenzyme
activities in cardiac surgery. Clin Biochem
1982;291-4.
61. Gambino
SR, Schneller
J. Creatine
kinase
MB isoenzymes
in
serum of patients who undergo cardiac surgery [Letter].
Clin Chem
1984;30:1114-5.
62. Rosenbium
AM, Ludbrook
PA, Jaffe AS. Significance
of elevated MB creatine
kinase
in patients
after cardiac
catheterization.
Catheterization
Cardiovasc
Diagnosis
1984;1O:547-52.
63. Jaffe AS, Paucity
of subtle myocardial
injury after angioplasty
delineated
with MB-CK. Ibid., in press.
64. Vacca G. Creatine kinase MB isoenzyme:
a comparison
of the
electrophoretic
method
with the selective activating
method and
the immunological
method.
Clin Chim Acts 1977;75:175-6.
65. Lang H, WUrzburg
U. Creatine
kinase,
forms [Review].
Clin Chem 1982;28:1439-47.
66.
Lott
JA.
Serum
enzyme
an
determinations
of many
enzyme
in the
diagnosis
of
acute
myocardial
infarction:
an update.
Human
Pathol
1984;15:706-16.
67. Boone DJ, Duncan
PH, MacNeil
ML, et al. Results of a
nationwide
survey
of analysis
for creatine
kinase
and creatine
kinase
isoenzymes.
Clin
Chem
from
the sample
matrix.
PM, Boehm M, Hajdusich
P, et al. Immunoinhibition
and
column
chromatography
compared
for assay
of creatine
isoenzyme
MB in serum.
Clin Chem
1982;28:166.-9.
58. Ng RH, Roe C, Funt
D, et al. Increased
activity of creatine
in a theophylline
intoxicated
patient.
Clin
ace: interferences
1984;30:238-42.
Bayer
automated
kinase
MB
the DuPont
Clin Chem
GE,
Mueller
Leroux
ML,
kinase
1985;31:1572-3.
creatine
85. Koch
evaluation
MB. Clin
RG.
of heparinized
plasma on results
Clin Chem 1981;27:1951-2.
PRE. Old and new ace methods
for
MB compared
[Letter].
Clin Chem
Effect
with the aca [Letter].
Desjardins
isoenzyme
TR, Mehta
UJ, Nipper
of kits for measurements
Chem 1986;32:186-91.
HC. Clinical
and
of creatine
kinase
analytical
isoenzyme
86. Szasz G, Gerhardt
W, Gruber
W, et al. Creatine
kinase
in
serum:
2. Interference
of adenylate
kinase
with the assay.
Clin
Chem 1976;22:1806-1
1.
87. Szasz G, Gerhardt
W, Gruber
W. Creatine
kinase
in serum:
3.
Further
study
1977;23:1888-92.
88. Hess JW,
trophotometric
1968;50:89-97.
of adenylate
Murdock
method
kinase
inhibitors.
Clin
Chem
KJ, Natho GJW. Creatine
kinase-a
specwith improved
sensitivity.
Am J Clin Pathol
and
89. Nealon DA. Relative
inhibition
of human adenylate
kinase
creatine
kinase
isoenzymes
by adenosine
5’-monophosphate
diadenosine
pentaphosphate
[Letter].
Clin Chem 1985;31:333-4.
and
90. Gerhardt
W, Waldenstrom
J. Creatine kinase B-subunit activity in serum after immunoinhibition
of M-subunit
activity.
Clin
Chem 1979;25: 1274-80.
91.
Morn
LG.
imniunoinhibition
Creatine
kinase
isoenzyme-antibody
reactions
in
and immunonephelometry.
Clin Chem 1979;25-
1415-9.
1984;30:33-7.
isoen-
92. Obzansky
D, Lott JA. Clinical
evaluation
of an iminunoinhibi-
zyme
MB
Invest
1979;39:607-12.
69. Hamilton
SR, Wimsatt
T, Torrieri
R, et al. Serum creatine
kinase
isoenzyme
MB activity:
evaluation
of a kit employing
tion procedure
for creatine
kinase-MB.
Clin
TJ, Foreback
CC. Automated
Chem 1980;26:150-2.
creatine
kinase-MB
agarose-gel
electrophoresis
with overlay paper fluorescence
scanning. Clin Chim Acts 1979;91:285-94.
70. Stein W, Bohner
J, Renn W, Maulbetsch
R. Macro creatine
kinase type 2: results of a prospective
study in hospitalized
patients.
Clin Chem 1985;31:1959-64.
71. Rogalsky VY, Koven IH, Miller DR, et al. Electrophoretic
94. Seckinger
DL, Vazquez
DA, Rosenthal
isoenzyme
methodology
and the diagnosis
infarction.
Am J Clin Pathol
1983;80:164-9.
68. Grande
P, Christiansen
C, Naestoft J. Creatine kinase
assay
by electrophoresis.
Scand
J Clin Lab
characteristics
of macro creatine
kinase type 2 in serum. Clin Chem
1986;32:13-5.
72. Medeiros
LI, Greco FA, Walsh D, Gerson
B. Macro creatine
kinase type 1 with electrophoretic
mobility
identical
to that of the
MB isoenzyme.
Clin Chem 1985;31:1393-6.
73. Aleyassine H, Tonks DB. Albumin-bound
tial source of error in fluorometric
assay
isoenzyme
[Letter].
Clin
Chem
fluorescence:
a potenof creatine
kinase
BB
1978;24:1849-50.
Chem 1979;25:1518-9.
76. Jaffe AS, Hitter
C, Melt.zer
V, et al. Unmasking
artifactual
increases
in creatine
kinase
isoenzymes
in patients
with renal
failure. J Lab Clin Med 1984;104:193-202.
77. Shell WE, Kligerman
M, Rorke MP, et al. Sensitivity
and
specificity
of MB creatine
kinase activity determined
with column
chromatography.
Am J Cardiol 1979;64:67-75.
78. Bondar RJL, Shevchik
DG, Hsu M-Y, et al. Improved
tion of creatine kinase isoenzymes
by use of DEAE-Sepharose
6B. Clin Chem 1980;26:618-24.
separaCL-
79. Henry PD, Roberts R, Sobel BE. Rapid separation
of plasma
creatine
kinase isoenzymes
by batch adsorption on glass beads. Clin
1975;21:844-9.
80. Apple FS, Greenspan
kinase BB in hospitalized
402.
81.
Stein
W,
Bohner
NS, Dietzler
patients.
Ann
J.
Determination
DN. Elevation
of creatine
Clin Lab Sci 1982;12:398of creatine
kinase
MB
a clinical
evaluation.
Clin Chem
1980;26:568-72.
PK,
et a!. Cardiac
of acute
myocardial
Wu AHB, Bowers
GN Jr. Evaluation
and comparison
of immunoinhibition
and immunoprecipitation
methods for differentiating MB from BB and macro forms of creatine kinase isoenzymes
in
patients and healthy individuals.
Clin Chem 1982;28:2017-21.
96. Wicks R, Usategui-Gomez
M, Miller M, et al. Immunochemical
95.
determination
of CK-MB
isoenzyme
in
enzymic approach.
Clin Chem 1982;28:54-8.
97. Sheehan
M, Haythorn
assay
for creatine
kinase
1985;31:160-1.
human
serum.
II.
An
P. Evaluation
of an imrnunoenzymetric
isoenzyme
MB (CK-MB).
Clin Chem
DW, Taylor E, Frye R, et al, Inimunoenzymetric
assay for
kinase
MB with subunit-specific
monoclonal
antibodies
compared
with an immunochemical
method
and electrophoresis.
Clin Chem 1985;31:465-9.
98.
74. Kincaid
HL. More on the detection
of serum CK-BB activity
and nonspecific fluorescence
[Letter]. Clin Chem 1979;25:337-8.
75. Gerson
B, Peterson
K. Creatine kinase
isoenzyme
BB and a
fluorescent
artifact
in hemodialysis
patients’
sera [Letter].
Clin
Chem
93. Delahunty
estimation by immuno-inhibition:
Chan
creatine
99. Wu AHB, Cornet TO, Bretaudiere
J-P, et a!. Comparison
of
enzyme
immunoassay
and immunoprecipitation
for creatine
kinase
MB in diagnosis
of acute
myocardial
infarction.
Clin
Chem
1985;31:470-4.
100. McBride JH, Rodgerson
DO, Diamond U. Creatine kinase
isoenzyme
MB as measured
by anion-exchange
chromatography,
immunoradiometric
assay, and immunoenzymetric
assay.
Clin
Chem 1985;31:1099-100.
101. Fenton
JJ, Bi-unstetter
5, Gordon
WC, et al. Diagnostic
efficacy
of a new enzyme
immunoassay
for creatine
kinase
MB
isoenzyme.
Clin Chem 1984;30:1399-401.
Pershadsingh
HA, Laurino
JP, Maynard
Y, et al. False
in serum
creatine kinase-MB
isoenzyme
detected
in two
patients
by the Behring
CK-MB quantitative
immunometric
assay
[Technical
Briefl. Clin Chem 1986;32:1410.
102.
increases
103. Vaidya
HC, Maynard
Y, Dietzler DN, et a!. Direct measurement of creatine
kinase-MB
activity
in serum after extraction
with
a monoclonal
antibody
specific
to the MB isoenzyme.
Clin Chem
1986;32:657-63.
CLINICAL
CHEMISTRY,
Vol. 32, No. 11, 1986
2051