I/DD Members and DSRIP: Data Initiatives Promoting Quality
advertisement
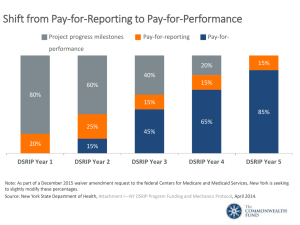
I/DD Members and DSRIP: Data Initiatives Promoting Quality Outcomes for Individuals with Disabilities Douglas G. Fish, MD Medical Director Division of Program Development and Management Office of Health Insurance Programs New York State Department of Health June 2, 2016 Saratoga, NY June 2016 Objectives • Purposes of Measurement Data • I/DD Subpopulation claims and spend data for in-patient and emergency department • Total Cost of Care for the I/DD subpopulation • Lessons from the Health And Recovery Plan (HARP) Behavioral Health Subpopulation • Potentially Avoidable Complications • Entering the World of Performance Based Outcomes & Value Based Payments Source: Intellectual/Developmental Disabilities and DSRIP. NYSDOH DSRIP Website. Published October 2015. 2 June 2016 3 DSRIP Objectives Explained Develop Integrated Delivery Systems Remove Silos • DSRIP was built on the CMS and State goals in the Triple Aim: Improving quality of care Improving health Reducing costs Enhance Primary Care and Communitybased Services Goal: Reduce avoidable hospital use – Emergency Department and Inpatient – by 25% over 5+ years of DSRIP Source: The New York State DSRIP Program. NYSDOH DSRIP Website. Integrate Behavioral Health and Primary Care • DSRIP has specific behavioral health focused projects • DSRIP’s holistic and integrated approach to healthcare transformation provides a template for integration of behavioral health initiatives into primary care plans June 2016 4 Different Purposes of Measurement Data • Data for accountability is different than data for performance improvement and care management Accountability Performance Measurement to evaluate performance, compare providers, enable consumer choice. Aggregating quantitative data for external use. Improvement Performance Measurement to learn & improve care process. Aggregating quantitative data for internal use. Care Coordination Sharing of quantitative or qualitative data in the care for individual patients. No primary focus on aggregation of data. June 2016 The Intellectual/ Developmental Disability (I/DD) Behavioral Health Sub-population • An estimated 1.5% to 2.5% of the general population has an intellectual or developmental disability • I/DD is a lifelong impairment Significant differences in functional status and abilities Co-morbidities and co-occurring conditions are common Over a lifetime, people’s health status change • Persons with I/DD who enter the Emergency Room are more than twice as likely to be admitted than the general population • An estimated 1 in 21 hospitalizations in New York State (NYS) involve persons with I/DD Source: Intellectual/Developmental Disabilities and DSRIP. NYSDOH DSRIP Website. Published October 2015. 5 6 June 2016 I/DD vs. General Population Medicaid FFS Claims and Spend Data – In-Patient Hospitalization 2014 2014 IP Claims per Unique Member (DD vs. NYS General) 2014 IP Spend per Unique Member (DD vs.NYS General) Statewide Average Statewide Average Western Western Southern Tier Southern Tier North Country North Country New York City New York City Mohawk Valley Mohawk Valley Mid-Hudson Mid-Hudson Long Island Long Island Finger Lakes Finger Lakes Central Central Capital District Capital District 0.00 0.50 1.00 General Population Claims per Unique Member Patient 1.50 Member DD Claims per Unique Patient IP Medicaid Claims * Statewide averages do not include regional duplications 2.00 2.50 $- $2,000 $4,000 $6,000 $8,000 General Population Spend per Unique Member Patient $10,000 $12,000 $14,000 $16,000 DD Spend per Unique Member Patient IP Medicaid Dollars Spent 7 June 2016 I/DD vs. General Population Medicaid FFS Claims and Spend Data – Emergency Room 2014 2014 ER Claims per Unique Member (DD vs. NYS General) 2014 ER Spend per Unique Member DD vs. NYS General) Statewide Average Statewide Average Western Western Southern Tier Southern Tier North Country North Country New York City New York City Mohawk Valley Mohawk Valley Mid-Hudson Mid-Hudson Long Island Long Island Finger Lakes Finger Lakes Central Central Capital District Capital District 0.00 0.50 1.00 1.50 2.00 2.50 General Population Claims per Unique Patient Member 3.50 4.00 Member DD Claims per Unique Patient ER Medicaid Claims * Statewide averages do not include regional duplications 3.00 4.50 $- $50 $100 $150 General Population Spend per Unique Member Patient $200 $250 $300 DD Spend per Unique Member Patient ER Medicaid Dollars Spent $350 8 June 2016 Total Cost of Care (TCC) for Medicaid I/DD Claims: Breakdown by Service Category Total Cost of Care: $7.7 Billion for 97,000 individuals analyzed within the I/DD system MSC 3% Day Services 17% Intermediate Care Facilities 17% Non-OPWDD Services 14% Residential Services 44% Employment Services 3% Respite 1% Other OPWDD 1% Other LTC Services 3% Capitated Programs 2% Nursing Homes 1% OSA 1% Other DOH 1% Pharmacy 2% Clinic 2% Other Acute Medical 1% Hospitals 2% Acute & Primary Care Services: $1.1 Billion OPWDD Specialty Services: $6.6 Billion June 2016 9 The Medicaid Population HARP Total Medicaid population HIV/AIDS Developmental Disability (I/DD) Managed Long Term Care (MLTC) General population Depression & Anxiety Trauma & Stressor Chronic Conditions (Diabetes, Asthma, etc) SUD • The total Medicaid population is divided in four subpopulations and the general population I/DD is one of those sub-populations Subpopulation arrangements are inclusive of total cost of care and outcomes are measured at the level of the whole subpopulation • There are also bundles (e.g., Depression, Chronic Conditions) • General Population They can be contracted in the general population Patients in a subpopulation can have one or more bundles • Bundles within Subpopulations However, for subpopulation contracts bundles are only used for analytical purposes They can be used to help inform analysis on what is happening within the subpopulation But they do not form the basis of any financial, contractual care arrangement June 2016 Health And Recovery Plans (HARPs) HARPs specialize in serving people with serious behavioral health conditions Eligibility is based on utilization or functional impairment Enhanced benefit package - HARPs offer all Medicaid Managed Care Plan (MMC) covered benefits plus access to additional services called Behavioral Health Home and Community Based Services (BH HCBS), if eligible Enhanced care coordination through Health Homes: A Care Manager Providers and Plans will work together to assist HARP members Performance metrics specific to higher need population and BH HCBS VBP can support the goals by making more flexible and performance-based payments that over time measure what matters to this population, like functional status improvement on domains such as housing, social stability, and employment, e.g. 10 June 2016 11 The HARP Population and the Transition to VBP Historically, the HARP population has experienced lower quality scores and associated poor outcomes • More than 20% of those discharged from general hospital psychiatric units are readmitted within 30 days. A majority of these readmissions are at different hospitals. • Approximately 42% of individuals in a New York City jail have a substance use disorder and 33% have a serious mental illness. Of those with a mental illness diagnosis, 50% have a co-occurring substance abuse disorder. • There is little coordination between inpatient care and outpatient aftercare, often resulting in these readmissions. • The unemployment rate for people with serious mental illnesses is 85%. • Only about 20% of adults with mental health disorders are seen by mental health specialists. • People who suffer from serious mental illnesses have a life expectancy that is about 25 years less than the general population, typically due to poorly managed chronic conditions. NYS is developing VBP arrangements specific to this subpopulation with financing and quality measures designed to improve outcomes, quality of care and functional status. HARP MCOs will contract with advanced networks of specialty providers for this population. Source: New York State Department of Health Medicaid Redesign Team. Behavioral Health (HARP, Depression, Bipolar Disorder).Clinical Advisory Group. NYSDOH DSRIP Website. Published 12 August 2015. June 2016 12 Evidence Informed Case Rates • Moving from DSRIP to VBP requires rate changes • Evidence Informed Case Rates (ECRs) are the Health Care Incentives and Improvement Institute (HCI3) episode definitions ECRs are patient centered, time-limited, episodes of treatment Include all covered services related to the specific condition All patient services related to a single condition E.g.: surgery, procedures, management, ancillary, lab, pharmacy services Distinguish between “typical” services from “potentially avoidable complications” Based on clinical logic: clinically vetted and developed based on evidence-informed practice guidelines or expert opinions Sum of services (based on encounter data the State receives from MCOs) June 2016 13 $250 50% 45% Total Episode Costs $200 40% 35% $150 30% 25% $100 20% 15% $50 10% 5% $- 0% Episode Name Costs Included: Total Cost % PAC Cost • Fee-for-service and MCO payments (paid encounters); • Caveat: add-on payments included in some cost data, not in others (GME/IME, HCRA, Capital). Data not yet standardized. Source: CY2014 Medicaid claims, Real Pricing, Level 5, General Population , Non-duals Please note: The slide offers preliminary data for illustration purposes. It is anticipated that elements such as volume, or cost, etc. may change slightly as the data is further developed and refined. PAC $ Percentage of Total Millions Chronic Episodes of the HARP Subpopulation (CY2014) June 2016 14 $25 50% 45% Total Episode Costs $20 40% 35% $15 30% 25% $10 20% 15% $5 10% 5% $- 0% DEPANX BIPLR ASTHMA DIAB PTSD HTN SUDS GERD Episode Name COPD ARRBLK HF LBP Total Cost % PAC Cost Costs Included: • Fee-for-service and MCO payments (paid encounters); • Caveat: add-on payments included in some cost data, not in others (GME/IME, HCRA, Capital). Data not yet standardized. Source: CY2014 Medicaid claims, Real Pricing, Level 5, General Population, Non-duals Please note: The slide offers preliminary data for illustration purposes. It is anticipated that elements such as volume, or cost, etc. may change slightly as the data is further developed and refined. OSTEOA CAD PAC $ Percentage of Total Millions Chronic Episodes of the I/DD Subpopulation (CY2014) 15 June 2016 Person Centered, Full Continuum of Care • Inclusive of all supportive care relationships across the spectrum of primary, acute, long-term support services, and OPWDD specialty services • Disease-oriented care • Clinically focused decision making • Medical model Full Continuum Patient Centered Person Centered • Non-disease oriented • Focus on the whole-person to ensure comprehensive, continuous and coordinated care Health Measures • Measures that capture population-specific outcomes for physical health • For example: • Preventive screenings • BMI Source: Kodner, Dennis. Value-Based Purchasing Health Care: Strategic Implications for Vulnerable Populations. The ArthurWebbGroup, Published June 2015. June 2016 16 Examples from HARP and MLTC Subpopulations • For other subpopulations discussions have broadened from medical and behavioral health measures to more holistic measurement of quality of life and the social determinants of health • The pilot phase will be used to further refine and validate quality measures, especially for new measures HARP Quality Measures • • • • Employment & economic stability Education Housing stability Interaction with the criminal justice system • Social connectedness • Satisfaction MLTC Quality Measures • Personal decisions about care prioritized • Continuity & stability of care relationships • Improvement in ability to self-support in community • Participation in community & social supports • Satisfaction 17 June 2016 CQL Personal Outcome Measures Under Consideration • My Self - Who I am as a result of my unique heredity, life experiences and decisions. Person-Centered Life Plans • People are connected to support networks • People have intimate relationships • People are safe • People have the best possible health • People exercise rights • People are treated fairly • People are free from abuse and neglect • People experience continuity and security • People decide when to share personal information Measures in bold overlap with group exercise My Dreams - How I want my life (self and world) to be. • People choose personal goals • People realize personal goals • People participate in the life of the community • People have friends • People are respected My World - Where I work, live, socialize, belong or connect. • People choose where and with whom they live • People choose where they work • People use their environments • People live in integrated environments • People interact with other members of the community • People perform different social roles • People choose services June 2016 18 Stakeholder Driven: I/DD VBP Advisory Group Meeting #2 Exercise • Exercise • Advisory Group divided into four groups • Brainstormed and discussed: • “What is the value proposition?” • “How do we want to be measured?” • Wrote ideas on sticky notes Ideas were grouped into thematic domains Discussed preliminary findings • Results indicative of a holistic focus on personal goal attainment, community participation, meaningful activities, rewarding relationships, quality of life, and socially desirable endeavors such as employment See the “Word Cloud” for a thematic, schematic interpretation of results! June 2016 A Thematic, Schematic Interpretation of Results The word cloud below is a visual presentation of qualitative data—words with greater prominence are words that appeared more frequently in the written submissions of the group exercise. 19 Questions? DSRIP E-mail: dsrip@health.ny.gov 20