Medical Engineering & Physics 26 (2004) 569–579
www.elsevier.com/locate/medengphy
The effect of duty cycle and frequency on muscle torque production
using kilohertz frequency range alternating current
Alex R. Ward a,, Valma J. Robertson b, Harry Ioannou a
a
Department of Human Physiology and Anatomy, School of Human Biosciences, La Trobe University, Bundoora, Melbourne, Vic. 3086, Australia
b
School of Physiotherapy, La Trobe University, Vic. 3086, Australia
Received 24 February 2003; received in revised form 11 March 2004; accepted 20 April 2004
Abstract
We investigated the frequency and duty cycle dependence of maximal electrically induced torque (MEIT) of the wrist extensors.
Fifty hertz burst modulated sinusoidal alternating current (AC) in the frequency range 0.5–20 kHz was used, with duty cycles
ranging from a minimum (one cycle) to maximum (continuous AC).
MEITs were similar at low frequencies but decreased markedly above 2.5 kHz. MEITs also decreased markedly above a 20%
duty cycle. Subjective reports of discomfort were fewest at 4 kHz and at duty cycles in the range 20–25%.
Our conclusion is that for maximum torque production, a frequency of 1 kHz and a duty cycle of 20% are indicated. When
comfort is a major consideration, a frequency of 2.5 kHz provides an acceptable trade-off between MEIT and comfort.
The findings also suggest that low duty cycle, burst modulated AC stimulation may be more effective than stimulation using
conventional low-frequency pulsed current.
# 2004 IPEM. Published by Elsevier Ltd. All rights reserved.
Keywords: Electrical stimulation; Alternating current; Frequency; Duty cycle; Torque
1. Introduction
Electrical stimulation is widely used in rehabilitation
for pain control, muscle re-education, prevention of
atrophy, and restoration of function (functional electrical stimulation or FES) [1,2]. Its potential application
in athletic performance through muscle strengthening
has also been explored using healthy subjects and athletes [3,4]. Both low-frequency rectangular pulsed current and sinusoidal alternating current (AC) in the low
kilohertz frequency range are used. When kilohertz frequency AC is used, it is modulated at a low frequency
[5], typically 50 Hz. For muscle strengthening, burst
modulated kilohertz frequency AC has been claimed to
be more effective than low-frequency rectangular
pulsed current [1–4], however, there have been insufAbbreviations: AC, alternating current; MEIT, maximal
electrically induced torque
Corresponding author. Tel.: +61-3-9479-5787; fax: +61-3-94795784.
E-mail address: a.ward@latrobe.edu.au (A.R. Ward).
ficient comparative studies and the findings are either
inconclusive or contradictory [5,6].
The most commonly used sinusoidal AC frequencies
are 2.5 and 4 kHz, though there is only limited empirical evidence to justify the choice [1–3]. A frequency of
2.5 kHz is advocated for the production of maximal
electrically induced torque (MEIT) [5,6]. A frequency
of 4 kHz is claimed to be more comfortable and therefore a more appropriate choice if maximal torque is
not the objective [1–3,7,8]. These claims are consistent
with early qualitative observations of the effects of kilohertz frequency AC [9]. d’Arsonval [10] reported that
when a constant voltage AC stimulus is applied transcutaneously, neuromuscular excitation becomes stronger up to 1.25–1.5 kHz, is constant between 1.5 and 2.5
kHz and decreases to 5 kHz (the highest frequency his
apparatus could produce). He also noted that current
with a frequency of 1.5 kHz is more painful than 5
kHz but much more comfortable than low-frequency
AC stimulation (75 and 20 Hz were the comparisons).
1350-4533/$ - see front matter # 2004 IPEM. Published by Elsevier Ltd. All rights reserved.
doi:10.1016/j.medengphy.2004.04.007
570
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
Stimulation using 2.5 kHz AC gained popularity in
the late 1970s, largely as a result of the activities of a
Russian scientist, Kots, who claimed force gains of up
to 40% in elite athletes as a result of what was then
regarded as a new form of electrical stimulation
[6,11,12]. He did not provide details of his published
work, nor did he give references and what became
known as ‘Russian current’ found popularity despite
the lack of research in the English-language literature
[5,6]. The AC frequency advocated by Kots was either
1 or 2.5 kHz, depending on whether stimulation was
via the nerve trunk (1 kHz) or over the muscle
(2.5 kHz) [6,12]. The recommended burst frequency
was 50 Hz and the duty cycle (burst ‘on’ to ‘on þ off’
time), 50%. The features of the stimulus waveform are
illustrated in Fig. 1(a). A frequency of 2.5 kHz is usual
for commercially produced Russian current stimulators, and 1 kHz appears to have been overlooked.
A recent study [13] which measured MEIT of the
wrist extensors used AC frequencies in the range
1–15 kHz and found that greatest MEIT was elicited at
1 kHz. This study also used a 50 Hz burst frequency, a
duty cycle of 50% and an electrode placement typical
of those used clinically. Whether frequencies lower
than 1 kHz might elicit greater MEIT was not examined, but Kots and co-workers [6,12] reported that the
MEIT measured at 0.5 kHz was appreciably less than
at 1 or 2.5 kHz. This suggests that 1 kHz is optimal for
torque production but further experimental evidence is
required.
Few studies have examined the effect of duty cycle
on torque production. Kots [6,12] stated that he adopted a 50% duty cycle as it produced a similar MEIT to
a continuous sinewave stimulus of the same peak intensity, but resulted in half the average current, so the risk
of tissue damage was reduced. This rationale appears
valid: AC with a 50% duty cycle delivers one-quarter
the power of a continuous stimulus of the same peak
intensity. Kots apparently did not consider whether
lower duty cycles might have a greater advantage.
One study which did examine the effect of duty cycle
was reported by Bankov [14]. Bankov used 5 kHz
sinusoidal AC, modulated at 60 Hz with duty cycles of
6%, 12% and 30%. The modulation envelope was sinusoidal in shape. Biceps brachii were stimulated at an
intensity which produced sufficient force to keep the
v
elbow joint at 90 flexion with the upper arm vertical.
Subjects were asked to comment on the relative discomfort of the stimulus and consistently reported an
increase in discomfort with increasing duty cycle.
Another study which included duty cycle as a variable was that of Moreno-Aranda and Seireg [15], they
investigated the effects of kilohertz frequency, burst frequency and duty cycle on finger flexor torque production and discomfort. Stimulus voltages were kept
constant and the AC frequency, initially at 500 Hz, was
increased in steps to 10 kHz. The duty cycle was varied
in the range 10–100% and burst frequency in the range
25–400 Hz at each AC frequency. The authors found
that the optimal parameters for torque production
were an AC frequency of 4 kHz, a burst frequency of
100 Hz, and a duty cycle of 20%. The authors also
found that discomfort decreased with increasing frequency over the range examined and concluded that
for the best compromise between torque production
Fig. 1. Burst modulated sinusoidal current with a burst frequency of 50 Hz and (a) a 50% duty cycle and (b) a 10% duty cycle. The period is 20
ms, so the burst frequency in each case is 50 Hz.
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
and comfort, the optimum frequency was 10 kHz with
other parameters remaining the same.
The studies by Bankov [14] and Moreno-Aranda and
Seireg [15] each had important limitations. Bankov [14]
chose a fixed, low level of torque production as the
parameter to be kept constant. The choice has obvious
relevance for clinical situations where muscle contractions are required, but maximum torque production is
not a central objective. Moreno-Aranda and Seireg [15]
chose a constant stimulus voltage across conditions
and examined how both torque production and discomfort varied with duty cycle and frequency. Their
focus was on efficiency, i.e. how to best evoke a reasonable amount of torque with minimal discomfort at a
particular stimulation intensity.
The existing literature indicates that no optimal duty
cycle for medium frequency AC stimulation has been
established. ‘Optimal’ may well depend on the chosen
experimental constraints. Bankov [14] kept muscle torque at a constant level. Moreno-Aranda and Seireg [15]
kept stimulus intensity constant. Both authors concluded that an optimal duty cycle was less than the
50% commonly used and was probably 20% or less. An
important question is whether the same duty cycle
range is optimal in terms of maximum torque
production.
The aim of the present study was to examine the
effect of duty cycle on maximum electrically induced
torque (MEIT) in normal, healthy subjects. A secondary aim was to examine the effect of AC frequency and
whether the variation in MEIT with duty cycle was frequency dependent. Discomfort was qualitatively assessed to establish whether MEIT is limited by the
discomfort associated with electrical stimulation.
2. Method
Sixteen subjects, eight males and eight females, participated in the study. Subjects were recruited from staff
and students of the School of Physiotherapy, La Trobe
University. Subjects’ ages ranged from 19 to 52 years
with a mean of 26.0 years (standard deviation 10.4
years). Prior to data collection, ethics approval was
571
obtained from the Human Research Ethics Committee
of the Faculty of Health Sciences, La Trobe University.
Inclusion criteria required that all subjects had previously used and experienced electrical stimulation.
This meant that subjects would be familiar with electrical stimulation and more consistent when manually
adjusting the stimulus intensity. Other inclusion criteria
required that the subject had no pathology affecting the
left forearm, no pacemaker and no damage to the skin
overlying the wrist extensor muscles. Subjects were
required for two sessions of electrical stimulation and
were asked to experience all 41 conditions (combinations of six frequencies and eight duty cycles, see
Table 1), applied in a different, randomised order at
each session. Randomisation was important as an
order effect (principally due to fatigue) was expected.
Subjects were asked to inform the experimenter if any
test conditions felt noticeably more uncomfortable than
others.
After the procedure was explained to each subject,
and informed consent obtained, the skin of the posterior surface of the left forearm was cleaned using an
alcohol swab and conductive rubber electrodes, measuring 44 40 mm, were attached using conductive,
adhesive skin mounts (American Imex type 00200). The
electrodes were positioned so as to efficiently stimulate
the wrist extensors: on a line from the head of the
radius to the distal radioulnar joint with the proximal
electrode 1 cm distal to the head of the radius and the
distal electrode 5 cm distal to the proximal electrode
along this line. The electrode leads were attached,
ensuring that the cathode was the distal electrode, i.e.
the distal electrode was the negative terminal for the
initial half-cycle of the sinewave burst.
The stimulator was a purpose-built device designed
to produce a burst of sinewaves with user selection of
the burst frequency and number of sinewaves per burst.
A zero-crossing detector was used to ensure that only
complete sinewaves were gated. The burst frequency
was set at 50 Hz. The number of sinewaves per burst
was varied from a single sinewave (minimum duty
cycle) to continuous output (100% duty cycle) in discrete steps. Test frequencies of 0.5, 1, 2.5, 4, 10 and 20
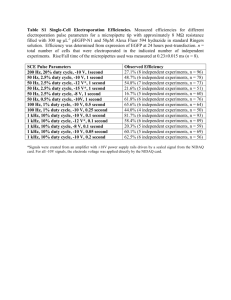
Table 1
The combinations of frequency and duty cycle used in this study. Whole numbers of sinewave cycles were used (numbers shown in parentheses).
Duty cycles above 50% were not used at 10 and 20 kHz because of the risk of burns and blistering
Frequency
(kHz)
0.5
1
2.5
4
10
20
Duty cycle (%)
0.25 (1)
0.5 (1)
0.5 (2)
1.25 (1)
1 (2)
1.25 (5)
2 (1)
2.5 (2)
2.5 (5)
2.5 (10)
5 (1)
4 (2)
6.25 (5)
5 (10)
5 (20)
10 (1)
10 (2)
10 (5)
12.5 (10)
10 (20)
12.5 (50)
20 (2)
25 (5)
20 (10)
25 (20)
25 (50)
25 (100)
50 (5)
50 (10)
40 (20)
50 (40)
50 (100)
50 (200)
70
75
60
75
(7)
(15)
(30)
(60)
100 (cont)
100 (cont)
100 (cont)
100 (cont)
572
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
kHz were used. At 10 and 20 kHz, duty cycles greater
than 50% were not tested as preliminary experimentation, using one of the investigators as a subject, indicated a risk of burns and blistering due to the high
average currents involved. Table 1 lists the test combinations of frequency and duty cycle.
The subject’s forearm was secured in a device built
expressly for measuring wrist extensor torque,
described previously [13]. The wrist axis was aligned
with the rotational axis of the apparatus and the forearm and hand were secured with velcro straps. A force
gauge (Mecmesin Inc. model MFG500: range 0–500 N,
with a resolution of 0.2 N) connected to the pivoting
arm of the apparatus measured wrist extensor torque,
calculated as force distance from the axis of rotation
(53 mm). Since the extremely high stiffness of the force
gauge prevented rotation about the axis these measurements were essentially of isometric torque.
Prior to data collection, each subject was asked to
experiment with the stimulus intensity for familiarisation and to increase the intensity to a level which they
regarded as the maximum tolerable. After two repeats,
data collection began, following a randomised order of
conditions produced for the particular subject. For
each condition, the subject was asked to adjust the
stimulus intensity to the ‘maximum tolerable’ level,
indicating to the investigator when they had done so,
so that 3-s measurements of torque, stimulus voltage,
and current could be made. This was followed by a 3-s
rest interval. The measurements were repeated twice so
that three measurements were obtained for each test
condition.
3. Results
3.1. The effect of frequency on MEIT
To examine the effect of frequency on MEIT, the
data were averaged across subjects at each particular
frequency and duty cycle. Plots of average MEIT versus frequency at different duty cycles are shown in
Fig. 2. Exact matching of duty cycles across frequencies was not possible because of the requirement
that whole numbers of sinewaves be used. Errors,
expressed as standard deviations, are not shown in
Figs. 2, 3 and 6, because if ‘error’ is defined as the
standard deviation for measurements across all subjects, it would be very large (approaching 100%). The
true error is much smaller than a standard deviation
would indicate. This is because the intra-subject variance in MEIT is large. The effect of intra-subject variation as a potentially confounding variable was
eliminated in our study by the experimental design:
measurements were made at all frequencies and duty
cycles with each subject. Fatigue also adds to the vari-
ation in measured MEIT values: torque measurements
were lower if they occur later in a measurement session. The effect of fatigue as a potentially confounding
variable was minimized by randomising the order of
presentation of each frequency/duty cycle combination
across subjects.
The dashed line in Fig. 2(a) indicates that at 0.5
kHz, the lowest duty cycle possible (one sinewave) is
10%. Dashed lines in graphs (e) and (f) indicate that at
duty cycles of 60/70/75% and 100%, the average current output, as indicated previously, was possibly too
high to be safe and was therefore not tested.
Fig. 2 shows that for all duty cycle ranges, maximum
torque was produced at low frequencies (0.5, 1 and 2.5
kHz) and for all but one of the six frequencies,
maximum torque was elicited at 1 kHz. Between 2.5
and 20 kHz, there was a rapid decrease in torque with
increasing frequency.
Establishing 1 kHz as the optimum frequency
required a statistical comparison of torques produced
at 0.5, 1 and 2.5 kHz. We compared the data using a
non-parametric, binomial sign test (which is robust and
makes no assumptions about sample size or normality
of distributions). Comparison of data obtained at frequencies of 1 and 0.5 kHz yielded a p-value of 0.03.
The results thus indicated that although the torques
differed by only about 3%, which is small in clinical
terms, the difference was statistically significant. The
difference between the means at 1 and 2.5 kHz was
almost 7% but did not reach statistical significance. A
p-value of 0.06 was obtained, suggesting a problem of
statistical power rather than there being no real
difference.
The evidence thus indicates that 1–2.5 kHz is an
optimum frequency range for electrically induced torque production. A frequency of 0.5 kHz elicits significantly less torque than 1 kHz. Above 2.5 kHz, a rapid
decrease in MEIT occurs with increasing frequency.
3.2. The effect of duty cycle on MEIT
To investigate the effect of duty cycle on MEIT,
graphs of torque vs. duty cycle were plotted at each
frequency (Fig. 3).
Fig. 3 shows that, at least in the range 20–100% duty
cycle, there is a clear downward trend in MEIT with
increasing duty cycle for all frequencies. Fig. 3(c), a frequency of 2.5 kHz, seems to show that maximum torque production occurs at 10% duty cycle. However,
this is not reflected in the duty cycle vs. torque graphs
for 0.5 kHz (Fig. 3(a)) and 1 kHz (Fig. 3(b)). Fig. 3(d)
shows that at 4 kHz, maximum torque production
appears to occur at the 12.5% duty cycle. Results for
frequencies of 10 and 20 kHz (Fig. 3(e) and (f), respectively) at low duty cycles are equally inconclusive.
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
573
Fig. 2. Plots of average torque vs. frequency for all duty cycles. The dashed line in (a) indicates that at 0.5 kHz, testing was not possible as one
sinewave at 0.5 kHz is a 10% duty cycle. Dashed lines in graphs (e) and (f) indicate that at the higher duty cycles, the average current output was
possibly too high to be safe.
To further examine the variation in MEIT at low
duty cycles, lines of best fit were calculated at each frequency using the 20–100% data. These are the lines
drawn in Fig. 3. Next, a predicted MEIT was calculated using the line of best fit for each measured duty
cycle less than 20%. Calculated values in the range less
than 20% were compared with measured values using a
non-parametric, binomial sign test. The difference was
found to be significant (p ¼ 0:008), indicating that the
graphs depart from linearity at low duty cycles. This
means that the graphs either curve, plateau or decrease
below 20% duty cycle. To establish which of these
applies, a linear regression was performed using data
for all frequencies and duty cycles of 10% or less, stan-
dardising to compensate for absolute changes with frequency. The gradient obtained (m ¼ 0:43 0:38,
r ¼ 0:28) demonstrates a weak, barely significant
downward trend in MEIT between 10% and 0% duty
cycle. This indicates either a plateau in MEIT or a
slight downward trend over the lowest duty cycles.
3.3. Discomfort
Subjects were asked to comment if any conditions
felt more uncomfortable than others. The reason for
asking this question was a previous empirical observation we have made when using burst modulated
kilohertz frequency AC stimulation. MEIT does not
seem to be determined solely by pain evoked directly
574
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
Fig. 3. Plots of average torque vs. duty cycle at all frequencies. Lines of best fit for data in the duty cycle range 20–100% are shown. r2 values
greater than 0.96 were obtained at all duty cycles. Dashed lines in graphs (e) and (f) indicate that at the higher duty cycles, the average current
output was possibly too high to be safe.
by the stimulation, but partly by the perception of the
forcefulness of the resulting contraction. That is, the
limit is often set by a subject’s feeling that if the contraction were any stronger, muscle or tendon damage
might occur. Hence, some variation in perceived discomfort was anticipated, even though the stimulation
was to the ‘maximum tolerable’ level.
The frequency of reports of discomfort is shown in
Table 2, together with the number of different conditions within each duty cycle range (values in parentheses). In order to compensate for particular frequencies
having a greater number of conditions than others,
data were standardised by dividing by the number of
conditions that were used within a particular duty cycle
range. Standardised numbers were then summed across
duty cycles to obtain an index of discomfort for each
tested frequency. The 0.5 kHz total was multiplied by
6/5 to compensate for there being no conditions in the
‘less than 10%’ category. Similarly, 10 and 20 kHz
totals were multiplied by 6/4 as they were only represented in four of the six duty cycle groups. A graph of
these standardised totals vs. frequency is shown in
Fig. 4.
Fig. 4 indicates that 0.5 kHz is the most uncomfortable frequency, accounting for 35% of all comments.
There is a gradual decrease with increasing frequency
to 4 kHz. From 4 to 20 kHz, there is an increase in
negative comments.
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
575
Table 2
Number of reports of discomfort categorized by frequency and duty cycle. Values in parentheses are the number of different conditions within the
duty cycle range
Frequency (kHz)
0.5
1
2.5
4
10
20
Duty cycle
<10%
10/12.5%
20/25%
40/50%
60/70/75%
100%
(0)
2 (1)
5 (2)
5 (3)
18 (4)
27 (5)
9 (1)
1 (1)
2 (1)
1 (1)
5 (1)
3 (1)
4 (1)
2 (1)
1 (1)
0 (1)
1 (1)
4 (1)
5 (1)
2 (1)
2 (1)
2 (1)
1 (1)
3 (1)
9 (1)
5 (1)
1 (1)
3 (1)
(0)
(0)
11 (1)
7 (1)
7 (1)
5 (1)
(0)
(0)
To examine the variation in discomfort with duty
cycle, standardised data were summed across frequencies. The <10% total was multiplied by 6/5 to
compensate for there being no conditions in the 0.5
kHz category. Similarly, 60/70/75% and 100% totals
were multiplied by 6/4 as they were only represented in
four of the six frequencies. A graph of standardised
number of comments vs. duty cycle was plotted (Fig. 5,
lightly shaded columns). Also shown are totals of only
those frequencies which had duty cycles in each category (1, 2.5 and 4 kHz, dark shading).
The totals across all frequencies have fewer reports
of discomfort in the <10% than in the 10/12.5% category. This is evidently because there is no contribution
to the <10% category at 0.5 kHz and this is the frequency associated with a disproportionally large number of reports of discomfort (Fig. 4). When only those
frequencies which have representation in all duty cycle
categories are used (dark shaded columns in Fig. 5),
the variation is more systematic. Whether the totals for
all frequencies are used or the totals for the more
restricted range, a minimum in reports of discomfort
occurs in the 20/25% duty cycle category. Greatest discomfort is associated with duty cycles of more than
50%.
Fig. 4. Number of reports of discomfort at each frequency. Values
are standardised to take account of varying numbers of conditions
tested at each frequency (see text).
Fig. 5. Standardised number of reports of discomfort vs. duty cycle
summed over all frequencies (lightly shaded columns) and only summed over frequencies of 1, 2.5 and 4 kHz (dark columns).
3.4. Stimulation efficiency
Stimulation efficiency is reflected by the stimulus
voltage needed to generate a given amount of torque.
In order to investigate stimulation efficiency, mean
stimulus intensity values were divided by their corresponding MEIT values to give a voltage/torque ratio
(V/N m). The results for each test frequency are shown
in Fig. 6.
Stimulus efficiency is greatest when the stimulus voltage used is lowest for a given torque value. This is
found in Fig. 6 at the minimum of the V/N m curves.
Fig. 6(a) shows that at 0.5 kHz, there is little variation
in the range 10–75% duty cycle. Only the 100% figure is
appreciably higher. A minimum possibly exists at 50%.
At 1 kHz (Fig. 6(b)), some variation can be seen, with
a minimum around a 30–40% duty cycle. The graphs
576
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
Fig. 6. Voltage/torque ratio vs. duty cycle at each frequency. Dashed lines in graphs (e) and (f) indicate that at the higher duty cycles, the average current output was possibly too high to be safe.
for 2.5, 4 and 10 kHz appear to have minima at progressively lower duty cycles.
Another feature, most apparent at 20 kHz, is the
steepness of the initial drop in voltage/torque ratio. At
20 kHz, the voltage/torque ratio decreases to almost
half as the duty cycle increases from 0.25% to 2.5%.
This effect decreases with decreasing frequency, partly
because one sinewave at a lower frequency has a higher
duty cycle than a higher frequency sinewave so small
duty cycles do not exist at lower frequencies. Nonetheless, when common duty cycles are compared, the rate
of decrease measured at 20 kHz is higher than that
observed at lower frequencies. The 10 kHz rate is
lower, but still higher than that observed at 4 kHz.
4. Discussion
4.1. Frequency effects
The present study found that the greatest torque was
produced at a frequency of 1 kHz (Fig. 3). A previous
study by Ward and Robertson [13] compared frequencies in the range 1–10 kHz and also found that the
greatest torque was elicited at 1 kHz. Lower frequencies were not tested in the earlier study so it was
not established whether 1 kHz or some lower frequency
was optimal. The present study, which found significantly higher MEIT at 1 kHz than 0.5 kHz, confirms
and extends the earlier findings.
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
The present study also found that the difference in
MEIT between 1 and 2.5 kHz did not achieve statistical significance, but the calculated p-value of 0.06 suggests, as noted previously, a problem of statistical
power rather than that there was no real difference. A
reanalysis of the data reported by Ward and Robertson
[13] shows that significantly greater MEIT was induced
at 1 kHz than 2 kHz (binomial sign test, p ¼ 0:006),
thus supporting the notion that a frequency of 1 kHz is
optimal.
Whatever the optimum frequency, the lower frequencies (0.5, 1, and 2.5 kHz) produced considerably
more torque than the higher frequencies (4, 10, and 20
kHz) and there was a general downward trend of torque produced with increasing frequency from 2.5 kHz.
The variation in MEIT between 0.5 and 1 kHz averaged only 3% and that between 2.5 and 1 kHz, 7%.
This suggests that despite the statistical significance of
the differences, the clinical significance is more questionable.
The decrease in discomfort between 0.5 and 1 kHz is
continued to 4 kHz (Fig. 4). This suggests that if one
had to choose between 0.5, 1, and 2.5, 0.5 kHz would
be rejected because of greater discomfort and lesser
MEIT. A frequency of 1 kHz would be preferred if
MEIT was the sole criterion. With relative comfort as
an additional criterion, 2.5 kHz would be the preferred
option. The findings suggest that the traditional
Russian current frequency of 2.5 kHz is not optimal
from the point of view of MEIT, but is close to optimal, and more comfortable than 1 kHz. Thus, 2.5 kHz
might be chosen as a trade-off between MEIT and discomfort. Torque production is not much less than at
1 kHz and comfort is greater.
Minimum discomfort occurs with a frequency of 4
kHz. This supports the notion that so-called ‘interferential currents’, which are commonly used clinically at
this frequency [1,2], can provide a very comfortable
form of electrical stimulation. Comfort evidently has
the penalty of lesser muscle force production. Whether
greater comfort translates into clinical effectiveness
remains open to question.
The variation in MEIT with frequency can be attributed, at least in part, to the different strength–duration
behaviour of nerve fibres with different diameters. As
Li and Bak [16] observed, the strength–duration graph
for smaller diameter fibres is shifted to the right
(to longer pulse durations). This is illustrated qualitatively in Fig. 7.
An AC frequency of 1 kHz, for example, has sinewaves with a positive phase which is one-half of a millisecond duration (500 ls). An AC frequency of 10 kHz
has sinewaves with a positive phase which is one-tenth
of the 1 kHz value; that is, a pulse width of 50 ls.
Fig. 7 indicates that with long duration pulses, thresholds for large and small diameter fibres are closer
577
Fig. 7. Strength–duration curves for different nerve fibre types. A-b,
A-beta or class II fibres, A-d, A-delta or class III fibres, C, C or class
IV fibres. Adapted from Li and Bak [16].
together. This means that with supra-threshold stimulation, fibres with a wider range of diameters will be
stimulated. With short duration pulses, there would be
less stimulation of smaller diameter fibres. The motoneurons innervating skeletal muscle have a range of
fibre diameters, so it would be expected that a larger
population of muscle fibres would be recruited with
long duration pulses. This, then, would explain the
increase in MEIT with decreasing frequency. The penalty of stimulating fibres with a wider range of diameters is a predicted excitation of more A-d (pain
signalling) fibres. This would account for the progressive increase in discomfort below 4 kHz.
4.2. Duty cycle effects
With increasing duty cycle, torque decreased (Fig. 2).
This was clearly evident at all frequencies for duty
cycles of 20% and above. Below 20% duty cycle, torque
appeared to reach a maximum somewhere between
10% and 20%. An optimum within this range was not
able to be determined due to the amount of scatter in
the results. Analysis of the data showed a positive
trend (increasing MEIT with increasing duty cycle) up
to 10%. Moreno-Aranda and Seireg [15] suggest that a
20% duty cycle is optimal for maximum torque production. Bankov [14] suggests that 12% is optimal. The
present findings are in agreement with those earlier studies, despite the different methods used. Although no
optimal value has been determined, the results indicate
that it is somewhere in the range 10–20% and that the
difference over this range is not large. Importantly, the
50% duty cycle adopted by Kots [6,12] is not appropriate if maximal torque production is the objective. A
578
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
duty cycle in the range 10–20% would be more effective.
This study also found that duty cycle affected perceived discomfort. The most frequently reported as
uncomfortable was the 100% duty cycle (Fig. 5). A
50% duty cycle was more comfortable but least discomfort was reported with a 20–25% duty cycle. The
minimum in the discomfort graph at 20–25% duty
cycle, together with the finding of greatest MEIT using
a 10–20% duty cycle, suggests that a 20% duty cycle is
the optimum for eliciting MEIT with minimum discomfort.
A possible explanation for the findings is that with
long duration bursts of AC, nerve fibre firing rates will
be multiples of the 50 Hz burst frequency [17,18].
Maximum firing rates approaching 1 kHz have been
observed in isolated a-motoneurons stimulated suprathreshold using continuous (unmodulated) stimuli with
frequencies in the range 1–10 kHz [19]. It follows that
with bursts of current using a 50% duty cycle, the
maximum firing rate would be less than 500 Hz and at
a 20% duty cycle, less than 200 Hz. While a nerve fibre
firing rate of somewhat less than 200 Hz might elicit
greater MEIT than 50 Hz, firing rates approaching 500
or 1 kHz would result in rapid fibre dropout due to
neurotransmitter depletion, propagation failure [20,21]
and/or nerve block [17–19]. Similarly, fibre firing rates
could provide an explanation for minimum discomfort
with a 20% duty cycle. Gating of pain fibre activity is
believed to be optimal when sensory fibres are stimulated at rates of 100 Hz or so [1–3,22]. Firing rates in
excess of 200 Hz would thus be less efficient than lower
firing rates for the modulation of pain sensation.
AC depended strongly on the burst duration, i.e. the
number of cycles in the burst, and also on the AC frequency. The AC frequency is important because the
nerve fibre membrane acts as a rectifier [25] so an AC
stimulus is able to push the nerve fibre closer to threshold with each successive pulse in a burst. Membrane
threshold is reached when successive pulses result in
sufficient depolarization to produce an action potential.
The Gildemeister effect, as it became known, was
demonstrated quantitatively by Schwarz and Volkmer
[26] who measured the change in membrane potential
of isolated nerve fibres as a result of successive pulses
in a burst of kHz frequency AC. The Gildemeister
effect requires that the pulses occur sufficiently rapidly
that the membrane does not have time to recover
between them. Depolarization due to summation is
thus expected to occur more readily at higher kilohertz
frequencies. The large drop in voltage/torque ratio at
20 kHz which occurs over low duty cycles (<10% in
Fig. 6(f)) is consistent with the notion of summation of
successive pulses. The lesser drop in voltage/torque
ratios at lower frequencies is explicable in terms of a
greater time between AC pulses, allowing the membrane to recover between them.
The progressive rise in the voltage/torque ratios with
higher duty cycles (above 20%) in Fig. 6 is explicable
by nerve fibre firing rates which are several multiples of
the burst frequency. As noted previously, this would
result in fibre dropout due to neurotransmitter
depletion, propagation failure [20,21] and/or nerve
block [18,19]. It would have the consequence of
reduced MEIT for a given stimulus intensity and hence
a higher voltage/torque ratio.
4.3. Stimulation efficiency
Stimulation efficiency, assessed in terms of the voltage/torque ratio, varied markedly with duty cycle.
Fig. 6 shows that at all but the lowest of the tested frequencies (0.5 kHz), a duty cycle of approximately 20%
produced the best stimulation efficiency (lowest voltage/torque ratio). Results at the extremes of the frequency range were equivocal, but in the range 1–10
kHz, a 20% duty cycle was optimal from the perspective of maximum torque production with minimum
stimulus intensity.
An interesting observation is the drop in voltage/torque ratio in the range 0–20%. The ratio is small at the
lowest frequencies (0.5 and 1 kHz) but becomes more
marked at higher frequencies (Fig. 6). The increasing
rate and amount of drop at higher frequencies are
likely due to summation of subthreshold depolarizations. Summation was first proposed by Gildemeister
[23,24] as an explanation for his observations that the
subjective sensation, and whether there was any sensation, associated with bursts of kilohertz frequency
5. Conclusion
The 50% duty cycle which is commonly used clinically is less than optimal from the point of view of
maximum muscle force production. The greatest MEIT
is elicited, not at 50%, but with a duty cycle of 20% or
less. A possible explanation is that at higher duty
cycles, nerve fibre firing rates are too high to maximize
and sustain an electrically induced contraction. A duty
cycle of 20% appears to be optimal when MEIT, comfort and stimulation efficiency are taken into account.
For maximum torque production, a frequency of 1
kHz is indicated. When comfort is also a consideration,
a frequency of 2.5 kHz provides a trade-off between
MEIT and comfort and this is the frequency traditionally used for Russian current stimulation. Least discomfort occurs at 4 kHz, the frequency traditionally
used for interferential current stimulation, but less
MEIT is produced.
Whether a 1 or 2.5 kHz stimulus with a duty cycle of
10–20% is more efficient than a low-frequency pulsed
A.R. Ward et al. / Medical Engineering & Physics 26 (2004) 569–579
current stimulus remains open to question. The present
findings strongly suggest that low duty cycle, burst
modulated, AC stimulation produces at least the same
amount of torque as low-frequency pulsed current but
with less discomfort.
References
[1] Low J, Reed A. Electrotherapy explained, 3rd ed. Oxford:
Butterworth-Heinemann; 2000.
[2] Nelson RM, Hayes KW, Currier DP. Clinical electrotherapy,
3rd ed. Stamford, CT: Appleton & Lange; 1999.
[3] Selkowitz DM. Electrical currents. In: Cameron MH, editor.
Physical agents in rehabilitation from research to practice. Philadelphia: WB Saunders; 1999, p. 345–427.
[4] Lloyd T, De Domeneco G, Strauss GR. A review of the use of
electro-motor stimulation in human muscle. Aust J Physiother
1986;32:18–30.
[5] Selkowitz DM. High frequency electrical stimulation in muscle
strengthening. Am J Sports Med 1989;17:103–11.
[6] Ward AR, Shkuratova N. Russian currents: the early experimental evidence. Phys Ther 2002;82:1019–30.
[7] De Domenico G. Basic guidelines for interferential therapy.
Ryde: Theramed Books; 1981.
[8] Savage B. Interferential therapy. London: Faber & Faber; 1984.
[9] d’Arsonval A. Action de l’électricité sur les êtres vivants. Exposé
des titres et traveaux scientifiques du Dr A. d’Arsonval. Paris:
Imprimerie de la cour d’appel; 1894, p. 37–77.
[10] d’Arsonval A. Action physiologique des courants alternatifs.
Comptes Rendus Société de Biologie, May 2, 1891:283–7.
[11] Babkin D, Timtsenko N, (Trans.). Electrostimulation: notes from
Dr Y.M. Kots’ (USSR) lectures and laboratory periods presented
at the Canadian–Soviet Exchange Symposium on Electrostimulation of Skeletal Muscles, Concordia University, Montreal,
Quebec, Canada, December 6–15, 1977 [Available from Dr Ward].
[12] Andrianova GG, Kots YM, Marmyanov VA, Xvilon VA. Primenenie elektrostimuliatsii dlia trenirovki mishechnoj sili.
Novosti Meditsinskogo Priborostroeniia 1971;3:40–7.
579
[13] Ward AR, Robertson VJ. The variation in torque production
with frequency using medium frequency alternating current.
Arch Phys Med Rehabil 1998;79:1399–404.
[14] Bankov S. Medium frequency modulated impulse current for
electric stimulation of non-denervated muscles. Acta Medica
Bulgarica 1980;7:12–7.
[15] Moreno-Aranda J, Seireg A. Investigation of over-the-skin electrical stimulation parameters for different normal muscles and
subjects. J Biomech 1981;14:587–93.
[16] Li CL, Bak A. Excitability characteristics of the A- and C-fibres
in a peripheral nerve. Exp Neurol 1976;50:67–79.
[17] Ward AR, Robertson VJ. The variation in fatigue rate with frequency using medium frequency alternating current. Med Eng
Phys 2001;22:637–46.
[18] Ward AR, Robertson VJ. Variation in motor threshold with frequency using kHz frequency alternating current. Musc Nerve
2001;24:1303–11.
[19] Bowman BR, McNeal DR. Response of single alpha motoneurons to high frequency pulse trains. Appl Neurophysiol
1986;49:121–38.
[20] Jones DA. High- and low-frequency fatigue revisited. Acta Physiol Scand 1996;156:265–70.
[21] Jones DA. Muscle fatigue due to changes beyond the neuromuscular junction. In: Porter R, Whelan J, editors. Human muscle fatigue: physiological mechanisms. London: Pitman Medical;
1981, p. 178–96.
[22] Johnson M, Ashton CH, Bousfield DR, Thompson JW. Analgesic effects of different frequencies of transcutaneous electrical
nerve stimulation on cold induced pain in normal subjects. Pain
1989;39:231–6.
[23] Gildemeister M. Untersuchungen über die Wirkung der Mittelfrequenzströme auf den Menschen. Pflügers Arch 1944;247:
366–404.
[24] Gildemeister M. Zur theorie des elektrischen Reizes. V. Polarisation durch Wechselströme. Berichte uber die Verhandlungen
der Sachsischen Akademie der Wissenschaften zu Leipzig. Mathematisch–Physische Klasse 1930;81:303–13.
[25] Sabah NH. Rectification in biological membranes. IEEE Eng
Med Biol 2000;1:106–13.
[26] Schwarz F, Volkmer H. Über die Summation lokaler Potentiale
bei Reizung motorischer Nervenfasern mit elektrischen Wechselimpulsen. Acta Biol Med German 1965;15:283–301.