Evidence for Clonal Dissemination of the
Serotype K1 Klebsiella pneumoniae Strain
Causing Invasive Liver Abscesses in Korea
Updated information and services can be found at:
http://jcm.asm.org/content/46/12/4061
These include:
REFERENCES
CONTENT ALERTS
This article cites 19 articles, 10 of which can be accessed free
at: http://jcm.asm.org/content/46/12/4061#ref-list-1
Receive: RSS Feeds, eTOCs, free email alerts (when new
articles cite this article), more»
Information about commercial reprint orders: http://journals.asm.org/site/misc/reprints.xhtml
To subscribe to to another ASM Journal go to: http://journals.asm.org/site/subscriptions/
Downloaded from http://jcm.asm.org/ on February 27, 2014 by PENN STATE UNIV
Doo Ryeon Chung, Ha Rim Lee, Seung Soon Lee, Shin Woo
Kim, Hyun-Ha Chang, Sook-In Jung, Myoung-don Oh, Kwan
Soo Ko, Cheol-In Kang, Kyong Ran Peck and Jae-Hoon
Song
J. Clin. Microbiol. 2008, 46(12):4061. DOI:
10.1128/JCM.01577-08.
Published Ahead of Print 29 October 2008.
JOURNAL OF CLINICAL MICROBIOLOGY, Dec. 2008, p. 4061–4063
0095-1137/08/$08.00⫹0 doi:10.1128/JCM.01577-08
Copyright © 2008, American Society for Microbiology. All Rights Reserved.
Vol. 46, No. 12
Evidence for Clonal Dissemination of the Serotype K1 Klebsiella pneumoniae
Strain Causing Invasive Liver Abscesses in Korea䌤
Doo Ryeon Chung,1* Ha Rim Lee,1 Seung Soon Lee,2 Shin Woo Kim,3 Hyun-Ha Chang,3
Sook-In Jung,4 Myoung-don Oh,5 Kwan Soo Ko,6 Cheol-In Kang,1
Kyong Ran Peck,1 and Jae-Hoon Song1
Received 14 August 2008/Returned for modification 29 September 2008/Accepted 16 October 2008
Seventy-three liver abscess isolates of serotype K1 Klebsiella pneumoniae from a nationwide collection in
Korea were genotypically characterized using pulsed-field gel electrophoresis and multilocus sequence typing.
We found that serotype K1 K. pneumoniae strains that caused liver abscesses in Korea were genotypically
related and that most were sequence type 23.
Serotype K1 K. pneumoniae isolates that were collected from
community-acquired liver abscesses during a nationwide prospective study by the Korean Study Group for Liver Abscess (4) were
included. The residences of the patients were widely distributed
throughout the entire country of South Korea. Community-acquired infection was defined as an infection diagnosed within 48 h
of admission to the hospital. The K antigen serotype was determined using both slide agglutination testing with antisera (Denka
Seiken, Tokyo, Japan) and magA PCR, as previously described
(4). Seventy-three liver abscess isolates were randomly selected
and were genotyped. Five ATCC reference strains of serotype
K1 (ATCC 8044, ATCC 8045, ATCC 8047, ATCC 35593,
and ATCC 13886) were also typed for comparison. For pulsedfield gel electrophoresis (PFGE), agarose-embedded bacterial
genomic DNA was digested with 20 U of XbaI. The restriction
fragments were separated by electrophoresis in 0.5⫻ Tris-borateEDTA buffer. Electrophoresis was conducted using a CHEF
Mapper XA (Bio-Rad Laboratories, Hercules, CA). The PFGE
patterns were analyzed by using BioNumerics software, version
4.01 (Applied Maths, Belgium). Clustering of patterns was done
by the unweighted-pair group method with arithmetic averaging
and the Dice coefficient. The Dice similarity coefficient was used
with optimization and position tolerance settings of 1.0%. A
PFGE-based clonal group (CG) was defined as a group of isolates
with ⱖ70% similarity on a dendrogram.
In order to better characterize the evolutionary genetic relationships among the isolates, multilocus sequence typing
(MLST) was performed on the isolates of serotype K1 K.
pneumoniae by determining the nucleotide sequences of seven
housekeeping genes (gapA, infB, mdh, pgi, phoE, rpoB, and
tonB), as described previously (7). ATCC reference strains of
serotype K1 were compared with our strains. The internal
fragments of those genes were amplified by PCR, and the
nucleotide sequences were determined for both strands. Sequence types (STs) were assigned by reference to the K. pneumoniae MLST website (http://pubmlst.org/kpneumoniae/) developed by Keith Jolley and sited at the University of Oxford
(11). For phylogenetic analysis of the strains, the eBURST
Klebsiella pneumoniae has become a major etiologic agent of
liver abscess in recent decades, and such an epidemiologic
change has been most prominent in Asian countries, including
Taiwan and Korea (4, 13, 18). Meta-analysis of the etiology of
pyogenic liver abscesses in Korea has clearly documented that
the etiology of pyogenic liver abscesses has continuously
changed in this country during the last half-century (4). A
recent nationwide Korean study showed that K. pneumoniae
accounted for 78.2% of community-acquired liver abscesses in
Korea (4). The K. pneumoniae liver abscess has distinctive
clinical characteristics, such as a strong association with diabetes mellitus (10, 12) and a high tendency for other metastatic
infectious foci (2, 4, 9). Previous studies have shown that K1 is
the predominant serotype among K. pneumoniae isolates that
cause liver abscesses in Taiwan and Korea, accounting for
around 60% of cases (4, 9). However, the K1 serotype had
been uncommon among the clinical isolates before the 1990s
(1, 5, 6). Furthermore, infection by this serotype has been more
widespread in the Asian countries even though there have
been reports addressing a recent increasing role of K. pneumoniae in liver abscess in the United States (8, 15, 16). To date,
there is no explanation for the epidemiological changes and
global differences observed.
In order to elucidate the reasons for the emergence of serotype K1 K. pneumoniae as a major causative organism for
liver abscesses in some Asian countries, molecular characterization of the isolates is essential. In this study, we determined
the genotypes of serotype K1 K. pneumoniae liver abscess isolates collected through a prospective nationwide study in Korea and investigated the possibility of regional spread of these
invasive strains in Korea.
* Corresponding author. Mailing address: Division of Infectious Diseases, Department of Internal Medicine, Samsung Medical Center,
Sungkyunkwan University School of Medicine, 50 Ilwon-dong, Gangnamgu, Seoul 135-710, Korea. Phone: 82-2-3410-0323. Fax: 82-2-3410-0041.
E-mail: drchung@skku.edu.
䌤
Published ahead of print on 29 October 2008.
4061
Downloaded from http://jcm.asm.org/ on February 27, 2014 by PENN STATE UNIV
Division of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul,1
Hallym University Sacred Heart Hospital, Anyang-si,2 Kyungpook National University Hospital, Daegu,3
Chonnam University Hospital, Gwangju,4 Seoul National University Hospital, Seoul,5 and
Department of Molecular Cell Biology, Sungkyunkwan University School of
Medicine, Suwon,6 Korea
4062
NOTES
J. CLIN. MICROBIOL.
algorithm, available at http://eburst.mlst.net/, was used. STs
were clustered into groups, employing the group definition
where all members assigned to the same group share identical
alleles at ⱖ5 of the 7 loci.
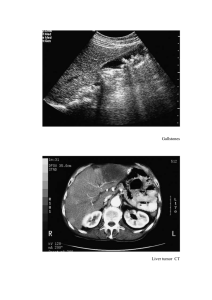
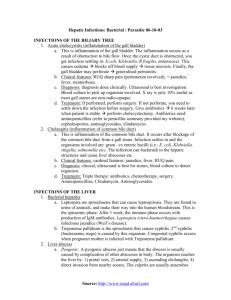
The PFGE patterns of the 73 K. pneumoniae isolates of the
K1 serotype were analyzed (Fig. 1). Sixty-nine (94.5%) out of
73 isolates were clustered into a major group with ⬎70%
similarity and were designated CG1. Within this group, eight
subgroups were further clustered with ⬎80% similarity. All five
ATCC strains of the K1 serotype showed closely related PFGE
patterns within each other; however, their PFGE patterns were
different from those of our isolates.
Strikingly, MLST showed that 71 (97.3%) out of 73 isolates
had the same ST, ST23 (Fig. 1). The other two isolates were
assigned to ST163 and ST217 and were single-locus variants of
ST23. All five ATCC strains were classified as ST82. By the
group definition in eBURST, all of the liver abscess isolates
found in our study were grouped as a single clonal complex
that contrasted with the ATCC strains of ST82. Bootstrap
resampling of the eBURST analysis yielded a value of 91% for
prediction of ST23 as the primary founder of this clonal complex.
The results of this study provide evidence that the K1 serotype K. pneumoniae strains, responsible for the increasing prevalence of invasive liver abscesses in Korea, are genetically
homogeneous. Our findings showed that most isolates of serotype K1 K. pneumoniae from liver abscess cases in Korea
showed very similar PFGE patterns; most isolates belonged to
Downloaded from http://jcm.asm.org/ on February 27, 2014 by PENN STATE UNIV
FIG. 1. Dendrogram of PFGE profiles and MLST STs of the K1 serotype K. pneumoniae liver abscess isolates.
VOL. 46, 2008
We thank all the members of the Korean Study Group for Liver
Abscess. The Korean Study Group for Liver Abscess is represented by
Doo Ryeon Chung (Samsung Medical Center, Sungkyunkwan University
School of Medicine, Seoul, Korea), Seung Soon Lee and Choong Kee
Park (Hallym University Sacred Heart Hospital, Anyang-si), Joong Sik
Eom and Jae Seok Kim (Kangdong Sacred Heart Hospital, Seoul),
Heung Jeong Woo (Hangang Sacred Heart Hospital, Seoul), Myung Seok
Lee (Kangnam Sacred Heart Hospital, Seoul), Hong Bin Kim (Seoul
National University Bundang Hospital, Seongnam-si), Myoung-don Oh
(Seoul National University Hospital, Seoul), Hee Jung Choi (Ewha Womans University MokDong Hospital, Seoul), Jae-Hoon Song (Samsung
Medical Center, Seoul), Jin Hong Yoo (Catholic University Medical College, Holy Family Hospital, Bucheon-si), Seong Heon Wie (Catholic
University Medical College, St. Vincent’s Hospital, Suwon), Young Hwa
Choi and Wee Gyo Lee (Ajou University Hospital, Suwon), Jin Soo Lee
and Moon Hyun Chung (Inha University Hospital, Incheon), Yeon Sook
Kim (Chungnam National University Hospital, Daejeon), Sang Won Park
4063
(Dankook University Hospital, Cheonan-si), Hee Bok Chae (Chungbuk
National University Hospital, Cheongju-si), Hyun Ha Chang and Shin
Woo Kim (Kyungpook National University Hospital, Daegu), Hyuk Lee
(Dong-A University Medical Center, Busan), Mi Sook Lee (Ulsan University Hospital, Ulsan), Sook In Jung (Chonnam National University
Hospital, Gwangju), Byung-Cheol Song (Cheju National University Hospital, Jeju-si), and Dong Joon Kim (Chunchon Sacred Heart Hospital,
Chuncheon-si).
REFERENCES
1. Blanchette, E. A., and S. J. Rubin. 1980. Seroepidemiology of clinical isolates
of Klebsiella in Connecticut. J. Clin. Microbiol. 11:474–478.
2. Cheng, D. L., Y. C. Liu, M. Y. Yen, C. Y. Liu, and R. S. Wang. 1991. Septic
metastatic lesions of pyogenic liver abscess. Their association with Klebsiella
pneumoniae bacteremia in diabetic patients. Arch. Intern. Med. 151:1557–
1559.
3. Cheng, H. P., F. Y. Chang, C. P. Fung, and L. K. Siu. 2002. Klebsiella
pneumoniae liver abscess in Taiwan is not caused by a clonal spread strain.
J. Microbiol. Immunol. Infect. 35:85–88.
4. Chung, D. R., S. S. Lee, H. R. Lee, H. B. Kim, H. J. Choi, J. S. Eom, J. S.
Kim, Y. H. Choi, J. S. Lee, M. H. Chung, Y. S. Kim, H. Lee, M. S. Lee, and
C. K. Park. 2007. Emerging invasive liver abscess caused by K1 serotype
Klebsiella pneumoniae in Korea. J. Infect. 54:578–583.
5. Cryz, S. J., Jr. 1990. Klebsiella polysaccharide vaccines. Adv. Biotechnol.
Processes 13:87–103.
6. Cryz, S. J., Jr., P. M. Mortimer, V. Mansfield, and R. Germanier. 1986.
Seroepidemiology of Klebsiella bacteremic isolates and implications for vaccine development. J. Clin. Microbiol. 23:687–690.
7. Diancourt, L., V. Passet, J. Verhoef, P. A. Grimont, and S. Brisse. 2005.
Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates.
J. Clin. Microbiol. 43:4178–4182.
8. Fang, F. C., N. Sandler, and S. J. Libby. 2005. Liver abscess caused by
magA⫹ Klebsiella pneumoniae in North America. J. Clin. Microbiol. 43:991–
992.
9. Fung, C. P., F. Y. Chang, S. C. Lee, B. S. Hu, B. I. Kuo, C. Y. Liu, M. Ho, and
L. K. Siu. 2002. A global emerging disease of Klebsiella pneumoniae liver
abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut 50:420–424.
10. Han, S. H. 1995. Review of hepatic abscess from Klebsiella pneumoniae. An
association with diabetes mellitus and septic endophthalmitis. West. J. Med.
162:220–224.
11. Jolley, K. A., M. S. Chan, and M. C. Maiden. 2004. mlstdbNet—distributed
multilocus sequence typing (MLST) databases. BMC Bioinformatics 5:86.
12. Kim, J. K., D. R. Chung, S. H. Wie, J. H. Yoo, S. W. Park, et al. 29 July 2008,
posting date. Risk factor analysis of invasive liver abscess caused by the K1
serotype Klebsiella pneumoniae. Eur. J. Clin. Microbiol. Infect. Dis. doi:
10.1007/s10096-008-0595-2.
13. Ko, W. C., D. L. Paterson, A. J. Sagnimeni, D. S. Hansen, A. von Gottberg,
S. Mohapatra, J. M. Casellas, H. Goossens, L. Mulazimoglu, G. Trenholme,
K. P. Klugman, J. G. McCormack, and V. L. Yu. 2002. Community-acquired
Klebsiella pneumoniae bacteremia: global differences in clinical patterns.
Emerg. Infect. Dis. 8:160–166.
14. Lau, Y. J., B. S. Hu, W. L. Wu, Y. H. Lin, H. Y. Chang, and Z. Y. Shi. 2000.
Identification of a major cluster of Klebsiella pneumoniae isolates from patients with liver abscess in Taiwan. J. Clin. Microbiol. 38:412–414.
15. Lederman, E. R., and N. F. Crum. 2005. Pyogenic liver abscess with a focus
on Klebsiella pneumoniae as a primary pathogen: an emerging disease with
unique clinical characteristics. Am. J. Gastroenterol. 100:322–331.
16. Rahimian, J., T. Wilson, V. Oram, and R. S. Holzman. 2004. Pyogenic liver
abscess: recent trends in etiology and mortality. Clin. Infect. Dis. 39:1654–
1659.
17. Turton, J. F., H. Englender, S. N. Gabriel, S. E. Turton, M. E. Kaufmann,
and T. L. Pitt. 2007. Genetically similar isolates of Klebsiella pneumoniae
serotype K1 causing liver abscesses in three continents. J. Med. Microbiol.
56:593–597.
18. Wang, J. H., Y. C. Liu, S. S. Lee, M. Y. Yen, Y. S. Chen, S. R. Wann, and
H. H. Lin. 1998. Primary liver abscess due to Klebsiella pneumoniae in
Taiwan. Clin. Infect. Dis. 26:1434–1438.
19. Yeh, K. M., A. Kurup, L. K. Siu, Y. L. Koh, C. P. Fung, J. C. Lin, T. L. Chen,
F. Y. Chang, and T. H. Koh. 2007. Capsular serotype K1 or K2, rather than
magA and rmpA, is a major virulence determinant for Klebsiella pneumoniae
liver abscess in Singapore and Taiwan. J. Clin. Microbiol. 45:466–471.
Downloaded from http://jcm.asm.org/ on February 27, 2014 by PENN STATE UNIV
the same ST, ST23. This is the first report demonstrating that
the recent increasing prevalence of serotype K1 K. pneumoniae
liver abscesses is attributable to the nationwide dissemination
of the ST23 strain throughout the entire country. The K. pneumoniae strains of ST23 were originally registered in the database by a European investigator from three blood isolates from
Belgium, The Netherlands, and Spain (7). Furthermore, a recent report from England suggested the possibility that this
genotype (ST23) is geographically widespread, based on the
results of PFGE and MLST evaluations of 16 K. pneumoniae
isolates from the United Kingdom, Hong Kong, Israel, Taiwan,
and Australia (17). Although previous studies using PFGE
pattern analysis in Taiwan showed controversial results regarding the clonality of the K. pneumoniae liver abscess isolates (3,
14, 19), some isolates showed similar PFGE patterns with the
Korean isolates in our study (CG1) (14). Many factors, including different definitions of clonality, limit the interpretation
and comparison of the PFGE patterns from different laboratories in many countries. In this view, comparison with the
MLST data from other regions will be valuable for further
understanding of the worldwide epidemiology of K1 K. pneumoniae infection.
These findings suggest the possibility of global dissemination
of the virulent K1 serotype K. pneumoniae strains of ST23 and
its association with invasive diseases, including liver abscesses.
Although the spread of virulent strains has contributed to the
increasing prevalence of K. pneumoniae liver abscesses in Korea, host factors, such as ethnicity, dietary practices, and the
local food chain, must also be considered a contributing factor.
Further research is necessary to understand the distinct global
epidemiology of invasive disease caused by K. pneumoniae.
In conclusion, serotype K1 K. pneumoniae isolates causing
liver abscesses in Korea are genotypically closely related, and
most isolates identified were ST23 or its single-locus variants.
These findings suggest that nationwide clonal dissemination of
these virulent strains of ST23 may be associated with an increasing prevalence of invasive liver abscesses caused by the
K1 type K. pneumoniae in Korea.
NOTES