NIPI Reference Book (Bihar) - ACCESS Health International
advertisement

November/2011
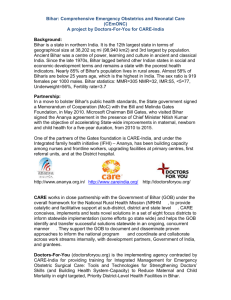
ACCESS HEALTH
INTERNATIONAL
NIPI REFERENCE BOOK
(BIHAR)
Bihar | Ikram Khan, Priya Anant and Prabal Singh
NIPI Reference Book-Bihar
Purpose of this Book
This book is a compilation of data from various sources relevant to our work on the
Norway India Partnership Initiative (NIPI) Funded project “Government contracting for
improved health services” in Bihar. We have used data from various sources and
structured it to serve as a quick reference guide. We have acknowledged the source in
most places, but apologise for omissions if any. This resource book would be updated
with data once a year and would be available online, meant for others interested in
infant health in Bihar.
Thanks,
Priya Anant, Associate Director
ACCESS Health International
2
NIPI Reference Book-Bihar
Contents
Chapter-1 ................................................................................................................................................ 7
1.
Healthcare in Bihar.......................................................................................................................... 8
1.1
Introduction ............................................................................................................................ 8
1.2 Health Systems and Structure....................................................................................................... 9
1.3
Health Infrastructure ............................................................................................................ 13
1.4
Human Resources ................................................................................................................. 14
1.5
State Health Budget Trend.................................................................................................... 15
1.6 Important Issues concerning Health in Bihar.............................................................................. 18
1.7 Initiatives ..................................................................................................................................... 21
1.8 Recent Reforms in Health ........................................................................................................... 25
Chapter-2 .............................................................................................................................................. 27
2. Maternal & Child Healthcare Status in Bihar .................................................................................... 28
2.1 Maternal and Child Health Indicators of Bihar ........................................................................... 28
2.2 Key Achievements in MCH in Bihar ............................................................................................. 31
2.3
State Schemes to Improve Maternal and Child Health......................................................... 33
Chapter-3 .............................................................................................................................................. 38
3. Public Private Partnership (PPP) ....................................................................................................... 39
3.1 Key stakeholders in Healthcare’s PPP ......................................................................................... 39
3.1.1 Department for International Development (DFID) ............................................................ 39
3.1.2 Norway- India Partnership Initiative (NIPI) .......................................................................... 40
3.2 PPP Initiatives by Health Department, GoB ................................................................................ 41
3.3
PPP in Rest of India and World on MCH ............................................................................... 45
3.3.1
Chiranjeevi Yojana (CY) ................................................................................................. 45
3.3.1
Janani ............................................................................................................................ 47
3.3.2
Child Helpline International .......................................................................................... 48
3.3.3
RapidSMS Malawi ......................................................................................................... 49
3.3.4
Vietnam’s Nutritious Food Program ............................................................................. 50
3.3.5
Karra Society for Rural Action ....................................................................................... 51
3.3.6
Wired Mothers .............................................................................................................. 51
Chapter-4 .............................................................................................................................................. 53
4.
District Profile ............................................................................................................................... 54
4.1
4.1.1
Nalanda ................................................................................................................................. 54
Introduction ...................................................................................................................... 54
3
NIPI Reference Book-Bihar
4.1.2 District Health System .......................................................................................................... 58
4.1.3 Health Infrastructure ........................................................................................................... 60
4.1.4 Nalanda Facility Survey Findings .......................................................................................... 62
4.2 Jehanabad ................................................................................................................................... 67
4.2.1 Introduction ......................................................................................................................... 67
4.2.2 Health System ...................................................................................................................... 70
4.2.3 Health Infrastructure ........................................................................................................... 72
4.2.4 Jehanabad Facility Survey Findings ...................................................................................... 76
4.3 Sheikhpura .................................................................................................................................. 81
4.3.1 Introduction ......................................................................................................................... 81
4.3.2 District health System .......................................................................................................... 85
4.3.3 Health Infrastructure ........................................................................................................... 85
4.3.4 Sheikhpura Facility Survey Findings ..................................................................................... 87
Chapter-5 .............................................................................................................................................. 92
5.
Maternal and Child Health in NIPI’s focus districts....................................................................... 93
5.1
Maternal Health .................................................................................................................... 93
5.1.1 Delivery Care ........................................................................................................................ 93
5.1.2.
Institutional delivery ..................................................................................................... 96
5.1.3 Postnatal Care .................................................................................................................... 100
5.2 Newborn Care ........................................................................................................................... 102
5.2.1
Breastfeeding and Supplementation .......................................................................... 103
5.2.2 Child Morbidity and Treatment ......................................................................................... 108
5.2.3 Summary Observation........................................................................................................ 110
5.3 Child Immunization .................................................................................................................... 111
5.3.1 Vaccination coverage ......................................................................................................... 112
Chapter-6 ............................................................................................................................................ 116
6.
Resource Persons ........................................................................................................................ 117
6.1 List of Resource Person at State Level ...................................................................................... 117
6.2
List of Resource person at District Level ............................................................................. 118
6.3 NGOs in Bihar ............................................................................................................................ 121
Works Cited ......................................................................................................................................... 126
Appendix-I ........................................................................................................................................... 129
4
NIPI Reference Book-Bihar
List of Tables
Table 1: Demographic, Socio-economic and Health profile of Bihar State as compared to India......... 8
Table 2: Health Provider consulted by Patients for Treatment (%) ........................................................ 9
Table 3: Infant Mortality Rate (SRS-09) .................................................................................................. 9
Table 4: Health Infrastructure of Bihar ................................................................................................. 13
Table 5 : Health Institution ................................................................................................................... 14
Table 6 Public Health Personnel ........................................................................................................... 15
Table 7 Availability of nursing education programmes in India and Bihar .......................................... 15
Table 8 Analysis of Health Budget of Bihar (Rupees in Crore) ........................................................... 16
Table 9 Allocation by GoI under NRHM to Bihar State (INR in Crore) .............................................. 16
Table 10 Public Health Subsidies in Bihar ........................................................................................... 17
Table 11 Cost drivers of Department of H& FW and NRHM at State Level (Rs in Crore) ................. 17
Table 12 New Super Specialty Units in Medical Colleges ................................................................... 21
Table 13 Trends in Infant Mortality Rate in Bihar and India ................................................................. 28
Table 14: Infant mortality rate by sex and residence, 2009 (SRS-09) ................................................... 28
Table 15 RCH II Goals (Bihar State Report) ........................................................................................ 29
Table 16 RCH II Outcomes (Bihar State Report) ................................................................................. 29
Table 17 Maternal and Child health Profile of NIPI focused districts and Bihar State ........................ 29
Table 18: Trends in Child Mortality Rate in Bihar and India ................................................................. 30
Table 19 Distribution of Women Receiving Pre-Natal Care by Source of Care .................................. 30
Table 20 Stakeholder roles in a Healthcare PPP ................................................................................... 39
Table 21: Nalanda – At A Glance (Nalanda DHP, 2010) ........................................................................ 54
Table 22: Comparative Population data (2001 Census) (Nalanda_DHP, 2010) .................................... 55
Table 23: Health Indicator..................................................................................................................... 58
Table 24: Institutional Delivery in Nalanda district (PHC wise) (Nalanda_DHP, 2010) ......................... 58
Table 25 MCH Indicators in Nalanda district ....................................................................................... 59
Table 26: Public Health Care Delivery System: Organisational Structure and Infrastructure .............. 61
Table 27: Health Infrastructure............................................................................................................. 62
Table 28: Statistical Profile (based on 2001 census) (Jehanabad_DHP, 2009) ..................................... 68
Table 29: Other Important data :- (Jehanabad_DHP, 2009) ................................................................. 68
Table 30: Health Indicators ................................................................................................................... 70
Table 31 MCH Indicators in Jehanabad district.................................................................................... 71
Table 32: Health Infrastructure............................................................................................................. 74
Table 33: Final Budget of Jehanabad .................................................................................................... 75
Table 34 MCH Indicators in Sheikhpura district .................................................................................. 83
Table 35: Health Infrastructure............................................................................................................. 85
Table 36: Human Resource ................................................................................................................... 86
Table 37: Place of delivery v/s number of living children, NIPI-08 ....................................................... 94
Table 38: Place of delivery v/s economic status of respondents’ household, NIPI-08 ......................... 95
Table 39: Average transportation expenses (in Rupees), NIPI-08 ........................................................ 96
Table 40: Nature of Institutional delivery, NIPI-08 ............................................................................... 96
Table 41: Cost incurred in institutional delivery1, NIPI-08 ................................................................... 97
5
NIPI Reference Book-Bihar
Table 42: Problem experienced during delivery by women of different age groups, NIPI-08 ............. 98
Table 43: Reason for home delivery, NIPI-08 ....................................................................................... 98
Table 44: Reasons behind choosing a specific person to conduct the delivery, NIPI-08 ...................... 99
Table 45: Cost incurred in home delivery, NIPI-08 ............................................................................. 100
Table 46: Timings of First Post Natal Care, NIPI-08 ............................................................................ 101
Table 47: Timing of first neonatal check-up by Districts, NIPI-08 ....................................................... 103
Table 48: Breastfeeding practices, NIPI-08 ......................................................................................... 104
Table 49: Initiation of breastfeed and gender of child, NIPI-08 ......................................................... 105
Table 50: Feeding of prelacteal liquids, NIPI-08 ................................................................................. 106
Table 51: Period of exclusive breastfeeding by background variables, NIPI-08 ................................. 107
Table 52: Prevalence of illness in children under study, NIPI-08 ........................................................ 109
Table 53: BCG and Polio 0‟ coverage by background variables, NIPI-08 ............................................ 112
Table 54: Child Immunisation Coverage in NIPI Districts, Bihar ......................................................... 113
Table 55: Immunization coverage – all basic vaccines........................................................................ 114
Table 56: Problems faced by mother/community in vaccinating the child, NIPI-08 .......................... 115
List of Figure
Figure 1: District Health Society-Organogram ...................................................................................... 11
Figure 2 Health Expenditure distribution 2007-08 ............................................................................... 18
Figure 3: District Health Administrative Setup (Nalanda_DHP, 2010) .................................................. 57
Figure 4 Nalanda District ...................................................................................................................... 59
Figure 5 Jehanabad District .................................................................................................................. 71
Figure 6: Health Facility in Jehanabad .................................................................................................. 73
Figure 7 Sheikhpura District ................................................................................................................. 83
6
NIPI Reference Book-Bihar
Chapter-1
Healthcare in Bihar
7
NIPI Reference Book-Bihar
1. Healthcare in Bihar
1.1 Introduction
Bihar with a population of 104 million is the second most populous state in India, next only
to Uttar Pradesh. Despite efforts in the last few decades to stabilize population growth, the
state’s population continues to grow at a much faster rate (25.07 percent) than the national
population (17.6 percent) in terms of decennial growth. The state is densely populated with
880 persons per square kilometer as against the country average of 324. The sex ratio of the
state at 916 females per 1000 males is also less favorable than the national average of 940
females per 1000 males. The state has 38 districts divided into 9 administrative divisions. In
addition, the state has 101 sub-divisions, 534 community development blocks, 9 urban
agglomerations, 130 towns and 37,741 villages. All key health indicators in Bihar are worse
than the national average. Increasing fertility, lack of improvement in antenatal care and
worsening of under-nourishment amongst children are key areas of concern. In other areas
there is improvement, albeit very minimal.
Table 1: Demographic, Socio-economic and Health profile of Bihar State as compared to India
S. No.
1
2
3
4
5
6
7
8
9
10
11
12
Item
Total population (Census 2011) (in millions)
Decadal Growth (Census 2011) (%)
Crude Birth Rate (SRS 2008)
Crude Death Rate (SRS 2008)
Total Fertility Rate (SRS 2007)
Infant Mortality Rate (SRS, 2009 & AHS 201011*)
Maternal Mortality Ratio (SRS 2007 - 2009)
Sex Ratio (Census 2011)
Population below Poverty line (%)
Schedule Caste population (in millions)
Schedule Tribe population (in millions)
Female Literacy Rate (Census 2011) (%)
Bihar
103.8
25.07
28.9
7.3
3.9
55*
India
1210.19
17.6
22.8
7.4
2.6
50
261
916
42.60
13.05
0.76
53.33
212
940
26.10
166.64
84.33
65.46
Source- (Bihar)
Only 34 percent of women in Bihar had three or more antenatal check-ups, with a worsening
in urban areas and no improvement in rural areas between National Family Health Survey
(NFHS) 2 & 3. During the same period, institutional deliveries rose from 15 percent to 23
percent. Immunization coverage increased from 12 percent to 33 percent and infant mortality
fell from 78 to 62 per 1000 live births between NHFS2 (1998-99) and NHFS3 (2005-06).
However, the proportion of underweight children below the age of three years increased from
8
NIPI Reference Book-Bihar
54 percent to 58 percent. Polio has not been eradicated and tuberculosis is not well
controlled. Approximately 90 percent of the fatal tropical disease Kala-azar in India is in
Bihar.
Table2: Status of Child health in Bihar and NIPI focused districts
NIPI focused State and Districts
Population (census 2011)
Crude Birth Rate (AHS 2010-11)
Estimated delivery
Infant Mortality Rate (AHS 2010-11)
Estimated Infant Death
Bihar
103804637
26.7
2771584
55
152437
Jehanabad
11,24,176
24.9
27992
53
1484
Nalanda
28,72,523
26.3
75547
52
3928
Sheikhpura
6,34,927
28.9
18349
58
1064
35
97005
77
213412
31
868
67
1875
27
2040
80
6044
31
569
76
1395
Neonatal Mortality Rate (AHS 2010-11)
Estimated Neonatal death
U5 CMR (AHS 2010-11)
Estimated Under-5 child death
Source- Annual Health Survey, 2010-11
Table 2: Infant Mortality Rate (SRS-09)
90
83
77
80
70
75
61
60
73
61
71
60
69
58
60
65
56
52
Bihar
50
Orissa
40
Kerala
30
20
11
12
15
14
13
India
12
12
10
0
2003
2004
2005
2006
2007
2008
2009
Source- (SRS 2009)
1.2 Health Systems and Structure
The healthcare services organization in the country extends from the national level to the
village level. From the total organization structure, we can divide the structure of healthcare
system into national, state, district, community, PHC and sub-centre levels. (WHO, 2007)
State level - The organization at the state level is under the State Department of
Health and Family Welfare in each state headed by a Minister. There is also a
Secretariat under the charge of Secretary/Commissioner (Health and Family Welfare)
belonging to the cadre of Indian Administrative Service (IAS). By and large, the
9
NIPI Reference Book-Bihar
organizational structure adopted by the state is in conformity with the pattern of the
Central Government. The State Directorate of Health Services, as the technical wing,
is an attached office of the State Department of Health and Family Welfare and is
headed by the Director of Health Services. But regardless of the job title, every
program officer under the Director of Health Services deals with one or more
subject(s). Every State Directorate has supportive categories comprising of both
technical and administrative staff. (WHO, 2007)
The area of medical education which was integrated with the Directorate of Health
Services at the state, has once again shown a tendency to maintain a separate identity
as Directorate of Medical Education and Research. This Directorate is under the
charge of Director of Medical Education, who is answerable directly to the Health
Secretary/Commissioner of the State. Some states have created the posts of Director
(Ayurveda) and Director (Homeopathy). These officers enjoy a larger autonomy in
day-to-day work, although sometimes they still fall under the Directorate of Health
Services of the state. (WHO, 2007)
Percentage
India: Percentage of Hospitalizations In The Public and
Private Sector Among Those Below The Poverty Line,
According To State
100%
80%
60%
40%
20%
BI
H
AD
ES
PR
RA
AN
DH
HA
R
GU
JA
R
AT
HI
HA
MA
RY
CH
A
AL
NA
PR
AD
ES
KA
H
RN
AT
AK
A
MA
KE
DH
RA
YA
LA
PR
AD
MA
E
HA
SH
RA
SH
T
NO
RA
RT
HE
AS
T
OR
ISS
A
PU
NJ
AB
RA
JA
ST
H
TA
AN
MI
UT
LN
TA
A
DU
R
PR
AD
ES
H
0%
States
Public Facilities
Private Facilities
Source: Pearson M, Impact and Expenditure Review, Part II, Policy Issues, DFID 2002
Regional level – In the state of Bihar, zonal or regional or divisional set-ups have been
created between the State Directorate of Health Services and District Health
Administration. Each regional/zonal set-up covers three to five districts and acts
10
NIPI Reference Book-Bihar
under authority delegated by the State Directorate of Health Services.
The
designation of the officers/in-charge of such regional/zonal organizations differs but
they are generally known as Additional/Joint/Deputy Directors of Health Services in
different States. (WHO, 2007)
District level - In the recent past, states have reorganized their health services
structures in order to bring all healthcare programs in a district under unified
control. The district level structure of health services is a middle level management
organisation and acts as a link between the state and regional structure on one side
and the peripheral level structures such as Primary Health Centres (PHCs) and subcentres (SCs) on the other side. It receives information from the state level which is
then transmitted to the periphery with required modifications to meet the local needs.
Figure 1: District Health Society-Organogram
Source- (Kumar, 2009)
In doing so, it adopts the functions of a manager and brings out various issues of
general, organizational and administrative types in relation to the management of
health services. The district officer with the overall control is designated as the Civil
Surgeon (CS). These officers are popularly known as CSs and are overall in-charge
of the health and family welfare programs in the district. They are responsible for
implementing programs according to policies laid down and finalized at higher levels,
i.e. the state and Centre. These CSs are assisted by ACMOs and program
officers. The number of such officers, their specialization, and status in the cadre of
State Civil Medical Services differ from the state to state. Due to this, the span of
11
NIPI Reference Book-Bihar
control and hierarchy of reporting of these program officers vary from state to state.
(WHO, 2007)
Sub-divisional/Taluka level – At the taluka level, healthcare services are rendered
through the office of Assistant District Health and Family Welfare Officer
(ADHO). Some specialties are made available at the taluka hospital. The ADHO is
assisted by Medical Officers of Health, Lady Medical Officers and Medical Officers
of General Hospital. These hospitals are being gradually converted into Community
Health Centres (CHCs). (WHO, 2007)
Community level – For a successful primary healthcare program effective referral
support is to be provided. For this purpose one Community Health Centre (CHC) has
been established for every 80,000 to 1, 20,000 population, and this centre provides the
basic specialty services in General Medicine, Paediatrics, Surgery, Obstetrics &
Gynaecology. The CHCs are established by upgrading the sub-district/taluka
hospitals or some of the block level PHCs or by creating a new centre wherever
absolutely needed.
PHC level – At present there is one PHC covering about 30,000 (20,000 in hilly,
desert and difficult terrains) or more population. Many rural dispensaries have been
upgraded to create these PHCs. Each PHC has one medical officer, two health
assistants – one male and one female, health workers and supporting staff. To
improve preventive and promotive aspects of healthcare, a post of Community Health
Officer (CHO) was proposed to be provided at each new PHC, but most states did not
take it up. (WHO, 2007)
Sub-centre level – The most peripheral health institutional facility is the sub-centre
manned by one male and one female multi-purpose health worker. At present, in
most places there is one sub-centre for a population of 5,000 (3,000 in hilly and desert
areas and in difficult terrain). (WHO, 2007)
The 73rd and 74th constitutional amendments have given the powers to the local bodies in
some states of India. In the process, different states have adopted different stakeholders for
the benefit of health services, with the help of community participation, which lays stress on
safe drinking water and sanitation at village level. The panchayats are given the power to
look after the welfare of the people. (WHO, 2007)
12
NIPI Reference Book-Bihar
1.3
Health Infrastructure
Although the state has a fairly extensive network of public health facilities it remains grossly
inadequate compared to the Government of India (GoI)/Government of Bihar (GoB) norms.
Furthermore, even the existing facilities lack the basic minimum infrastructure needed for
their optimal functioning. According to information available with the state directorate, only
23 of the 38 districts in the state have a district hospital. Similarly, of 101 sub-divisional
headquarters, only 23 have a sub-divisional hospital. The CHC/ Referral Hospital Network
are virtually nonexistent with the state having only 101 CHCs/Referral Hospitals (70
functional). The state has only 398 PHCs that suggest that each PHC covers an average of 2
lakh population as against the norm of 30,000. A similar situation prevails with regard to
facilities at the Health Sub-Centre level, where the state has 9140 Health SCs i.e. an average
of one Health SC for a population of 9000 as against the norm of 5000. (Madhav, 2010)
Table 3: Health Infrastructure of Bihar
Item
Sub-centre
Primary Health Centre
Community Health Centre
Multipurpose worker (Female)/ANM
Health Worker (Male) MPW(M) at Sub Centres
Health Assistant (Female)/LHV at PHCs
Health Assistant (Male) at PHCs
Doctor at PHCs
Obstetricians & Gynaecologists at CHCs
Physicians at CHCs
Paediatricians at CHCs
Total specialists at CHCs
Radiographers
Pharmacist
Laboratory Technicians
Nurse/Midwife
Required
14959
2489
622
10499
8858
1641
1641
1641
70
70
70
280
70
1711
1711
2131
In position
8858
1641
70
9127
1074
479
634
1565
21
38
17
104
15
439
135
1425
Shortfall
6101
848
552
1372
7784
1162
1007
76
49
32
53
176
55
1272
1576
706
(Source: RHS Bulletin, March 2008, M/O Health & F.W., GOI) (Bihar)
Nine out of ten Additional Primary Health Centers (APHC) that work under the Block
Primary Health Centre were found closed during the field visit. The Ministry of Health and
Family Welfare (MoHFW-GoI) identifies APHC and PHC as PHC in its RHS Bulletin.
According to community members, centers are operational once a week only for
immunization. (Madhav, 2010) While the services provided by the Block PHC and APHC are
primary in nature with specialty services required to be available through the CHC to a
population of 100,000 these are not available at block level in Bihar. Furthermore a survey
13
NIPI Reference Book-Bihar
conducted in one district showed that 17 out of 42 APHCs (40 percent) are without a Medical
Officer (MO). (Madhav, 2010)
APHC provides only weekly consultation and immunization. Maternal and Child healthcare,
which also includes family planning, has emerged as the main function of PHCs as no
deliveries have been carried out at the APHCs and SCs. Only normal deliveries are conducted
at PHCs with complicated cases being referred for further treatment. Hospitals with lady
doctors (6 percent) are in a better position to provide services of internal examination and
other gynecological treatments. (Madhav, 2010)
In Bihar, while Additional PHCs continue to exist on paper, many centres are derelict and
abandoned sites, while others stand devoid of all human resources. These human resources
have been diverted to ‘upgraded PHCs’ that are on par with CHCs in other states. There are
yet other workers who have been contracted out on a public-private partnership (PPP) basis
(Ref-13). Similarly, 20 percent of SCs in Bihar were found to be functioning on an ad hoc
basis out of a primary school building or a room in a construction site, with the auxiliary
nurse midwife operating out of here only on immunization days. (Gill, 2009)
The other health institutions in the state are given below:
Table 4 : Health Institution
Health Institution
Medical College
District Hospitals
Referral Hospitals
City Family Welfare Centre
Rural Dispensaries
Ayurvedic Hospitals
Ayurvedic Dispensaries
Unani Hospitals
Unani Dispensaries
Homeopathic Hospitals
Homeopathic Dispensary
Source- (Bihar)
1.4
Number
8
25
70
12
366
11
311
4
144
11
179
Human Resources
Due to inadequate physical infrastructure, districts face acute shortage in health personnel as
well. A large number of posts of Medical Officers and frontline health workers remain
vacant. In the case of frontline health workers such as Auxiliary Nurse Midwife (ANM),
14
NIPI Reference Book-Bihar
Male Health Workers (MHW), staff nurses and Anganwadi Worker (AWW) the situation is
almost similar or even worse.
Table 5 Public Health Personnel
Category
Medical
Officers
ANM
IPHS Standard
1 Per 10000
Population
1 Per 2500
Population
Source- (Status, 2009)
Required
9500
Sanctioned
5124
Existing
3860
Gap
516
38500
11294
10055
17151
The state of Bihar requires 5488 ANMs, 1157 Lady Health Visitors (LHVs), 70 Public Health
Nurses (PHNs), 76 District Public Health Nursing Officers (DPHNOs), 13818 Staff Nurses,
383 Head Nurses, 114 Assistant Matrons, 48 Matrons and 147 teachers excluding the
additional personnel required for additional SHCs, PHCs and CHCs to be established based
on the norms for population in 2008. (Nursing in Bihar, 2010)
Table 6 Availability of nursing education programmes in India and Bihar
1.5
India
Bihar
%
ANM training or MPHW(F) training Institutes -18
months after 10th class
487
27
5.5
General Nursing and Midwifery(GNM) Training
Institute for three years after 12th class or
intermediate
1805
11
0.6
B.Sc. Nursing colleges for four years after 12th
class with science
1069
Nil
Nil
Post basic B.Sc. Nursing college for two year for
staff nurses with GNM diploma
129
Nil
Nil
M.Sc. (N) College for 2 years after completion of
B.Sc. nursing
Source- (Nursing in Bihar, 2010)
153
Nil
Nil
State Health Budget Trend
The health budget of the Department of Health and Family Welfare has increased from INR
709.31 crore to INR 1331.57 crore from year 2004-05 to year 2007-08. The growth of the
budget has been the highest in 2006-07 at 51.09 percent from the previous year but it
declined to 8.41 percent in 2007-08. There was a sharp increase and then a decrease in the
growth rate of the budget. This sharp increase in budget estimate could be due to the fact that
year 2006-07 was the first year in which the new government in the state presented the
budget. (Bihar DET Report, Apr,2010)
15
NIPI Reference Book-Bihar
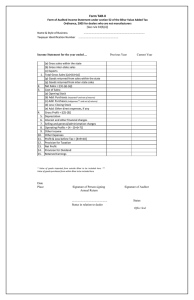
Table 7 Analysis of Health Budget of Bihar (Rupees in Crore)
Particulars
Total Health Budget
Trend of Growth Rate
Total Expenditure budget
Percentage of State Health Budget
to Total State Expenditure Budget
Source –Study of State Finances – RBI
2004-05 2005-06 2006-07 2007-08
709.31
812.94 1228.29 1331.57
14.61
51.09
8.41
28350.46 32227.9 35483.7 36571.55
2.5
2.52
3.46
3.64
There is an increase in the state health budget from 2.50 percent to 3.64 percent in the total
state budget showing a constant increasing trend from 2004-05 to 2007-08. The average
percentage of state health budget to total state budget was 3.03 percent over the period of four
years under consideration of this review. (Bihar DET Report, Apr,2010)
Budget Allocation to Bihar under NRHM
The budget allocation to Bihar under NRHM has increased continuously from INR
398.22 crores in 2005-06 to INR 695.26 crores in 2007-08. The total allocation to the
state under NRHM during this period has been INR 2373.39 crores (Bihar DET
Report, Apr,2010)
The budget allocation increase by 50.47 percent in 2006-07 was the highest year-onyear increase. This could be due to the fact that 2006-07 was the first year of NRHM.
(Bihar DET Report, Apr,2010)
Table 8 Allocation by GoI under NRHM to Bihar State (INR in Crore)
Head
2005-06
2006-07
2007-08
2008-09
Grand Total
Total Allocation under NRHM
398.22
599.21
680.7
695.26
2373.39
RCH Flexipool
123.72
174.32
127.76
213.84
639.64
0
146.62
256.31
186.28
589.21
65.68
51.69
55.14
66.91
239.42
NRHM Flexipool
National Disease Control Programme
Source- Website of MOHFW/NRHM
RCH Flexipool shows a trend of more allocation in the years of 2005-06 to 2006-07.
Later in 2007-08 NRHM Flexipool got more allocation but in 2008-09 RCH Flexipool
again received more allocation. The National Disease Control Program has got in the
range of 10 percent in all the years and the budget allocation decreased from 2005-06
(Bihar DET Report, Apr,2010)
16
NIPI Reference Book-Bihar
Table 9 Public Health Subsidies in Bihar
Share of Public Subsidies by Quintiles (%)
1
2
3
4
5
Ratio I/V
(%)
Rural
Short
Hospitalization
Hospitalization
Share of
Public
Subsidies by
Items (%)
3.9
15.9
28.5
21.3
30.4
7.8
35.4
3.5
11.4
21
23.4
40.8
11.7
51.3
PHC & Others
7.2
9.6
23.6
26.2
33.4
4.6
5.2
Immunization
19.8
22
19.6
19.3
19.3
1
8.1
Total
5.1
13.7
23.7
22.5
35
6.8
100
Urban
Short
Hospitalization
Hospitalization
5.7
20.1
31.9
22.8
19.5
3.4
33.3
3
10.8
21.6
50
14.5
4.8
63.1
PHC & Others
24.3
12.1
20
12.9
30.7
1.3
2.1
Immunization
25.7
20
18.8
14.9
13.9
0.5
1.5
18.8
25
39.7
16.5
3.5
100
Total
4.7
Source- (Srivastava, 2003)
Table 10 Cost drivers of Department of H& FW and NRHM at State Level (Rs in Crore)
Budget Head
Expenditure incurred
during FY 2007-08
544.88
% of Total
Expenditure
41.05
Urban health Services -Allopathy
293.47
22.11
RCH Flexipool- NRHM
174.97
13.18
128.2
9.66
106.14
8
Public Health
29.66
2.23
NRHM Flexipool
12.18
0.92
Direction and Administration
10.1
0.76
National Disease Control Programme
8.53
0.64
Rural Health Services- Other Systems of
medicine
Urban health Services -Other system of
medicine
Training
6.43
0.48
6.17
0.47
4.18
0.31
Maternity and child health
1.48
0.11
Urban family welfare services
0.81
0.06
Research and Evaluation
0.04
0
Rural Health Services-Allopathy
Rural family welfare services
Medical Education, Training and Research
Grand Total
1327.24
Source- State Health Society, Bihar
17
NIPI Reference Book-Bihar
Figure 2 Health Expenditure distribution 2007-08
Urban health
Services -Other
system of medicine
Public Health
1%
Medical Education, 3%
Training and
Research
9%
Direction and
Administration
1%
Rural family welfare
services
11%
H.E. Composition 07-08
Rural Health
Services- Other
Systems of medicine
1%
Urban health
Services -Allopathy
26%
Rural Health
Services-Allopathy
48%
Source: Finance Accounts – 2004-05 to 2007-08
1.6 Important Issues concerning Health in Bihar
Health is a complex sector with deep cross linkages across other social sectors like nutrition,
literacy, poverty, women and child development, panchayati raj, etc. Interventions under
NRHM need to be catalyzed by parallel actions in these sectors. Health is still not a high
priority area and as such needs to be brought under the prime focus, particularly at the state
level. For successful planning and implementation of the Mission activities, it is extremely
important that there is an assured availability of incremental outlay. It is also necessary that
the outlay is made known to the state in time so that these could be factored while preparing
the annual plan. The state also needs to hike its health budget very significantly in order to
meet the target of 2-3 percent of the GDP. (Jha, 2007)
Panchyat Raj Institutions have a very crucial role to play in the entire process. It is, therefore,
imperative that sufficient powers are delegated to them that enable them to lead the process.
The shortage of manpower particularly doctors and paramedical staff willing to work in the
rural areas is expected be a serious challenge. Operationalization of all the healthcare
18
NIPI Reference Book-Bihar
facilities in the light of manpower constraints would be a major challenge for the state. (Jha,
2007)
Substantial Gaps in PHC Infrastructure:
In Bihar, there is an acute shortage of CHCs, PHCs and SCs. The state has a
shortage of 1210 SCs, 13 PHCs, and 389 CHCs. Besides, out of a total of 38 district
hospitals, only 24 are currently functional. (Jha, 2007)
Shortage of Manpower, Drugs and Equipments Necessary for Primary Healthcare
There is also a shortage of essential requirements in terms of manpower, equipment,
drugs and consumables in the primary healthcare institutions. Moreover, there are no
specialists at the CHCs. There is a shortage of 3376 MOs and 19945 ANMs. The
percentage of PHCs having adequate equipment stands at only 6.2 percent compared
to the national figure of 41.3 percent. There is inadequate and erratic availability of
essential drug supplies, ORS packets, weighing scales, etc. There is also a very acute
shortage of gynaecologists and obstetricians to provide maternal health services in the
peripheral areas of the state. (Jha, 2007)
Lack of Training Facilities
The status of training facilities in the state (both in terms of infrastructure and human
resources) remains far from satisfactory at all levels. At the state level, there is only
one training institute {the State Institute of Health and Family Welfare (SIHFW)} that
imparts training to health personnel. The SIHFW is facing a severe shortage of faculty
and related facilities. At the regional level too there is an acute shortage of good
training centres. (Jha, 2007)
Very High Fertility Rate
The total fertility rate in the state is second highest in the country (4.2 compared to the
national figure of 3.0). The birth rate is also second highest in the State (30.4
compared to the national figure of 23.8). Besides, birth order 3 + is 54.4 percent
compared to the national figure of 42 percent. Approximately 51.5 percent of the girls
get married below the age of 18 years as compared to the national figure of 28
percent. The percentage of couples practicing any method of contraception is only 34
percent against the national figure of 53.9 percent. (Jha, 2007)
19
NIPI Reference Book-Bihar
Low Institutional Deliveries and High Level of Maternal Death
The Maternal Mortality Ratio (MMR) in Bihar (371 per 100,000 live births) is the 4th
highest in the country. The high level of MMR can be attributed to low level of
institutional deliveries (23.2 percent compared to national figure of 41 percent), high
level of anaemia among women (63.4 percent compared to national figure of 51.8
percent), low provision of iron and folic acid tablets to antenatal cases (8.1 percent
compared to national figure of 20.4 percent), and low level of complete antenatal
coverage (5.4 percent compared to national figure of 16.4 percent). (Jha, 2007)
Undernutrition in Children and Women
Bihar is a state with lowest per capita income and a very high level of poverty. Diet
surveys carried out by the Department of Women & Child Development indicate that
the state ranks very low in terms of dietary intake (not more than 2000 calories).
Undernutrition is very high in the state, because of low dietary intake, high morbidity
and also closely spaced pregnancies. Approximately 39.3 percent of women are
undernourished (BMI of less than 18.5 kg/m2). The state has very low overweight and
obesity rates in women. The percentage of women with chronic energy deficiency is
also higher (39.3 percent) compared to the national figure of 35.8 percent. (Jha, 2007)
On assessment of weight-for-age in the state, 54.4 percent of children under the age of
three years have been found to be underweight in comparison to the national figure of
47 percent. Assessments of height-for-age about 53.7 percent of the children have
been found to be stunted in comparison to the national figure of 45.5 percent. The
number of infants receiving semi-solid foods at the age of six months is much lower
than the national level and as a result under-nutrition rate in children is much higher
than the national level. About 54.4 percent children are underweight and 81 percent
are anaemic. (Jha, 2007)
Very Low Coverage of Full Immunization
The coverage of routine immunizations and Pulse Polio is low. As per 2001 census,
full immunization in the state was only 11 percent against the national average of 54
percent. As a result, a large number of polio cases are still reported in the state.
Coverage of Vitamin-A dose (10 percent) is also very low in the state. With
improvement in the immunization services in the state, the coverage of immunization
is at present 33 percent (NFHS 3). (Jha, 2007)
20
NIPI Reference Book-Bihar
Low Level of Female Literacy
Low female literacy rate in the state, particularly in rural areas, is one of the major
reasons for poor health conditions in the state. According to the 2001 census, female
literacy rate in the state is 33.57 percent against the national average of 54.28 percent.
Due to illiteracy, there is a lack of awareness among women about antenatal,
intranatal and postnatal care, especially in rural areas. (Jha, 2007)
Poor Status of Family Planning Programs
Key indicators related to Maternal and Child Health (MCH) and Family Planning
clearly show the poor health status in Bihar. Roughly 51.5 percent of the girls in the
state get married below the age of 18 years compared to the national figure of 28
percent. The proportion of couples practicing any method of contraception is 34
percent against the national figure of 53.9 percent. Some of the reasons affecting the
implementation of the Family Planning program in the state are: lack of health
facilities, both in terms of physical infrastructure and skilled human resources to
deliver quality family planning services, evidently low exposure to mass media in
Bihar, leading to lower exposure of family planning messages in the community,
particularly among rural and socioeconomically disadvantaged groups. The program
has also failed in being able to take effective measures to increase the median age at
marriage and first childbirth, etc. (Jha, 2007)
1.7 Initiatives1
A. Three New Medical College & Hospitals proposed by Government of Bihar in
Pawapuri, Bettiah, and Madhepura districts of Bihar.
B. Super Specialty Units in Medical Colleges:
Table 11 New Super Specialty Units in Medical Colleges
DMCH, Darbhanga
Neurosurgery & Cardiology
SKMCH, Muzzafarpur
Neurosurgery & Cardiology
JLMNCH, Bhagalpur
Neurosurgery & Cardiology
PMCH, Patna
Nephrology, Cardiothoracic Surgery,
Gastroenterology, Endocrinology and
Laparoscopic Surgery
Neurosurgery & Cardiology
ANMMCH, Gaya
1
State health Society- Bihar(http://statehealthsocietybihar.org/new-proposed-initiatives.html)
21
NIPI Reference Book-Bihar
C. Super Specialty Hospitals
-
Lok Nayak Jai Prakash Narayan Hospital (Ortho)
-
Rajendra Nagar Hospital (Eye)
-
Gardiner Road Hospital (Haemophilia)
-
Guru Govind Singh Hospital (Maternal & Child)
D. Ultra-Modern Diagnostic Centres:
In the State, Ultra-Modern diagnostic centres include nine Regional Diagnostic
Centres and six Medical College Hospitals that have been set up.
-
Contracts have been awarded to two agencies to operate, maintain and report
24-hours centres.
-
Facilities to be provided - Pathology- Biochemistry, Radiology – Digital Xray, USG, CT Scan, MRI, ECG, and Mammography.
-
The agency will provide required staff, equipment, machine, logistics and
consumables.
-
The agency will ensure installation, maintenance and operation of equipment
with provision of expert technical staff round the clock.
-
Regional Diagnostic Centres will be handed over to the agency.
-
The agency will share a fixed percentage of gross revenue with the
government.
-
There is no cost on the government. Rather, the government will receive
money out of it.
-
The agency will charge rates for diagnostic services from the patients as
applicable at AIIMS, New Delhi.
E. Modular OT
-
To ensure proper upkeep and maintenance of OT equipment it has been
decided to outsource OT equipment to private agencies.
-
Modular O.T. equipment will be provided in six Government Medical College
Hospitals of Bihar on a rental basis.
-
The OT equipment will also be provided on a rental basis to the 25 District
Hospitals.
F. Mahadalit Healthcare
-
The government of Bihar has initiated healthcare services to the people living
in the Mahadalit Tolas who are considered to be the poorest of poor in the
state.
22
NIPI Reference Book-Bihar
-
A survey is to be conducted to identify these Mahadalit Tolas.
-
Health camps will be organized in the identified Mahadalit Tolas.
G. Developing four districts as models (Padmanabhan, 2009)
-
Jehanabad, Gaya, Vaishali and Nalanda districts
-
Develop all facilities in these districts as models
-
Improve patient amenities to IPHS standards and also make them women
friendly.
-
Capacity building of health functionaries to deliver quality healthcare.
-
Mobile nurse trainers to give hands-on training to the nurses and ANMs on
various protocols.
-
Visits to these facilities by the health functionaries of other districts.
I. Drug testing:− Four laboratories accredited by the National Accreditation Board for Testing
and Calibration Laboratory have been selected for testing of the quality of
drugs supply to government health facilities.
− The drug controller will randomly take & collect samples from the drug
depots.
− The collected samples will be sent to the laboratories.
− So far samples of 46 drugs have been sent for quality testing.
H. Biomedical Waste Management:− Hospital Waste Treatment and Disposal Services, in all health facilities right
from Medical Colleges to the PHCs.
− Common biomedical waste treatment facility established for Patna Division
through a Private Firm.
− In the remaining 7 divisions private sector partnership is being approved
through tender. In Muzzafarpur M/s Semb Ramky has been contracted to set
up treatment plant in PPP mode. The agency will collect biomedical waste
generated in the health facilities from 15 districts. In Gaya and Bhagalpur M/s
Synergy is to set up treatment plants for the collection, treatment and disposal
of biomedical waste generated in 15 districts.
− The agency is to provide training to all the health service providers.
23
NIPI Reference Book-Bihar
J. Yoga
− The state government has initiated yoga camps for patients as an alternate
method for treatment.
− Yoga instructors are being selected to organize Yoga Camps in the District &
Sub-Divisional Hospitals.
− Yoga Camps are being organized continuously for six months.
− Every Yoga instructor is paid INR 10,000 per month.
K. School Health
− The government of Bihar has initiated health camps in all the Middle Schools
for regular health checkups of the students.
− Each student will be issued a health card on completion of the check-up.
− Private agencies/NGOs/Institutions are being selected for conducting health
check-ups in schools.
− All the 9 Division Health Quarters were provided INR.1.00 Cr. for the year
2007-08.
L. Rashtriya Swasthya Bima Yojana in Bihar,
− A medical insurance of INR 30,000 would be available to every family living
below poverty line (BPL) against a card worth INR 30. Jagrugta Rath is
equipped with necessary information for families living below poverty line.
Information would also be available to experts who are present to help the
families. (Bhelari, 2011)
− The card provides health coverage of INR 30,000 for five members of a BPL
family every year. The cardholder and his family can visit government and
private hospitals in their district to avail treatment. The cost of medicines
from one day prior to the admission in the hospital to one day after the
discharge, would be covered by the scheme. (Bhelari, 2011)
− The coverage under Rashtriya Swasthya Bima Yojana is provided in
association with Royal Sundaram Insurance Company. The minister and the
principal secretary termed the scheme as a “hassle-free” health insurance
scheme. The card owner would just need to carry the card to the network of
24
NIPI Reference Book-Bihar
hospitals and the expenses for the treatment would be taken care of and the
amount deducted from the card. (Bhelari, 2011)
− This project would cater to five members of every BPL family. The process of
making the cards has already been initiated in various places in all the districts
and thousands of families have already got the card against a fee of INR 30.
(Bhelari, 2011)
− Under the scheme, health smart cards would be distributed among BPL
families. This is a special initiative by the central and the Bihar governments.
(Bhelari, 2011)
1.8 Recent Reforms in Health
The health department’s goal for 2006 was to provide quality and affordable healthcare 24
hours a day at the block level. The year was also declared “Routine Immunization Year” by
the Chief Minister and remarkable progress was made, increasing the rate of immunization
from 12 percent to 33 percent in 12 months. (TOR_Bihar_DFID, 2008)
The government has taken radical measures such as: improved staffing at block PHCs by
relocating from lower level facilities and contracting of 800 general doctors and 400
specialists; improved attendance of doctors by installing telephones in PHCs and contracting
a call centre to monitor their presence. There is zero tolerance of absenteeism and doctors
have been fired for non-attendance. Essential drug lists have been agreed for each type of
facility, drug suppliers and rates have been agreed centrally with orders and payment
decentralized to district levels. There is close monitoring of stocks. As a result of the
presence of both doctors and drugs at the facilities, out-patient attendance has shot up in the
past year, from less than 30 to an estimated over 2000 per month. (TOR_Bihar_DFID, 2008)
Public Private Partnerships (PPPs) have been developed for laboratory diagnostics, radiology
(X rays), mobile medical services and hospital maintenance. Some PHCs have also been
contracted out to NGOs though the experience on this is considered to be ‘mixed’.
(TOR_Bihar_DFID, 2008)
25
NIPI Reference Book-Bihar
Undernutrition in children below the age of three years has increased from 54 percent to 58
percent between NFHS 2 and NFHS 3. The Social Welfare Department (SWD) has
responded to the Supreme Court order for universalisation of ICDS services and subsequently
8000 Anganwadi Centres (AWC) has been sanctioned. The selection of Anganwadi Workers
(AWWs) has been decentralized to Panchayati Raj Institutions (PRIs), and money for local
procurement and distribution of food for the AWCs is now in the hands of the village mothers
committees. Some foods fortified with micronutrients are available. There is a huge challenge
to universalize access to Integrated Child Development Scheme (ICDS), and to ensure that
the services reach children under the age of three years who are at greatest risk from under
nutrition. (TOR_Bihar_DFID, 2008)
There are ambitious plans for a Management Information System (MIS) with a longitudinal
system of recording every child’s nutritional status monthly. There is a massive infrastructure
shortfall, and the department has taken a loan from National Bank for Agriculture and Rural
Development (NABARD) for this purpose. There is a huge need for AWW training. The
Health and Social Welfare departments meet in the State Health Task Force chaired by the
Chief Minister. (TOR_Bihar_DFID, 2008)
The Department of Public Health Engineering has embarked on an ambitious policy reform
and operational plan to address access to water and sanitation. This includes the provision of
toilets for all Anganwadi centres and total sanitation campaign across the state (funded by
GoI). The department is also making efforts to mitigate the chemical contamination of well
water (arsenic, fluoride, iron) especially in eastern Bihar, and exploration of the use of
abundant river water to replace contaminated well water. There is an understanding and
commitment to convergence at the village level as well as between the Department of Health,
Social Welfare and Public Health Engineering. (TOR_Bihar_DFID, 2008)
26
NIPI Reference Book-Bihar
Chapter-2
Maternal & Child
Healthcare in Bihar
27
NIPI Reference Book-Bihar
2. Maternal & Child Healthcare Status in Bihar
2.1 Maternal and Child Health Indicators of Bihar
The total fertility rate of the state is 3.9. The IMR is 52 and MMR is 312 (SRS 2004 - 2006)
both of which are higher than the national average. The sex ratio in the State is 919 females
for every one thousand males (as compared to 933 females for every one thousand males in
the country). Comparative figures of major health and demographic indicators are as
follows: (Bihar)
In 1998-99, the IMR was 78 per 1000 live births in Bihar compared to 68 for all India
(NFHS-2). According to the latest NFHS-3 (2005-06) the figure for Bihar is 62 per 1000
live births. SRS 2009 estimates the IMR of Bihar to be 52 per 1000 live births. (Bihar_NIPI,
2009)
Table 12 Trends in Infant Mortality Rate in Bihar and India
Infant Mortality Rate
Source/Year
Bihar
India
NFHS 2 ( 1998-99 )
78
68
NFHS 3 ( 2005-06)
62
57
SRS 2000
62
71
SRS 2003
60
60
SRS 2006
61
57
SRS 2009
52
50
NRHM Goal by 2010
45
Source: NFHS 2 and 3, SRS Bulletin (1997), SRS (2000, 2003, 2006)
Table 13: Infant mortality rate by sex and residence, 2009 (SRS-09)
India/States/ Union
Territories
Total
Rural
Urban
Total
Male
Female
Total
Male
Female
Total
Male
Female
India
50
49
52
55
54
56
34
32
35
Bihar
52
52
52
53
53
53
40
39
41
Kerala
12
10
13
12
10
14
11
10
11
Source- (SRS 2009)
28
NIPI Reference Book-Bihar
Comparative figures of major health and demographic indicators are as follows: (Bihar)
Table: Status of Child health in Bihar and NIPI focused districts
NIPI focused State and Districts
Population (census 2011)
Crude Birth Rate (AHS 2010-11)
Estimated delivery
Infant Mortality Rate (AHS 2010-11)
Estimated Infant Death
Bihar
103804637
26.7
2771584
55
152437
Jehanabad
11,24,176
24.9
27992
53
1484
Nalanda
28,72,523
26.3
75547
52
3928
Sheikhpura
6,34,927
28.9
18349
58
1064
Neonatal Mortality Rate (AHS 2010-11)
35
31
27
31
Estimated Neonatal death
U5 CMR (AHS 2010-11)
Estimated Under-5 child death
Source- Annual Health Survey, 2010-11
97005
77
213412
868
67
1875
2040
80
6044
569
76
1395
Table 14 RCH II Goals (Bihar State Report)
BIHAR
INDICATOR
INDIA
RCH II/ NRHM
Current status
(2012) goal
Trend (year & source)
Maternal Mortality Ratio
(MMR)
Infant Mortality Rate (IMR)
Total Fertility Rate (TFR)
371 (SRS 01-03)
60 (SRS 2003)
4.2 (SRS 2003)
312 (SRS 0406)
58 (SRS 2007)
3.9 (SRS 2007)
254 (SRS 04-06)
<100
55 (SRS 2007)
2.7 (SRS 2007)
<30
2.1
Table 15 RCH II Outcomes (Bihar State Report)
S.
No.
1
2
3
4
5
6
7
8
Bihar
RCH OUTCOME INDICATOR
India
DLHS–2
(2002–04)
DLHS–3
(2007–08)
DLHS–2
(2002–04)
DLHS–3
(2007–08)
16
26.4
50.4
51
4.3
3.9
16.5
19.1
18.8
20.7
27.7
41.4
40.9
45.9
47
54.1
6
11.8
22.7
24.9
13.4
22
30.3
33.7
24.5
28.4
45.2
47.3
38.3
37.2
21.4
21.5
Mothers who received 3 or more antenatal care
checkups (%)
Mothers who had full antenatal check-up (%)
Institutional deliveries (%)
Children 12-23 months age fully immunised (%)
Children age 6-35 months exclusively breastfed
for at least 6 months (%)
Children with diarrhoea in the last 2 weeks who
received ORS (%)
Use of any modern contraceptive method (%)
Total unmet need for family planning - both
spacing methods and terminal methods (%)
Table 16 Maternal and Child health Profile of NIPI focused districts and Bihar State
Key Indicator
3+ ANC visit
ANC
Child
Bihar
26.4
Nalanda
15
Jehanabad
20
Sheikhpura
23
At least 1 TT injection
58.4
50
54.5
83.5
Received 100+ IFA
9.3
5.5
6.9
5.7
DPT (all 3)
54.2
65.1
55.1
49.2
29
NIPI Reference Book-Bihar
Immunization
Measles
Full
Delivery
Institutional Births
Characteristics
Source: DLHS-3, 2007-08
49.9
69.1
63.9
49.3
41.4
54.2
47.2
38.3
27.7
39.3
42.5
41.6
Under 5 mortality rate (U5MR) in Bihar as per NFHS-3 is 848 per 10000 live births, one of
the highest in India. (Bihar_NIPI, 2009)
Table 17: Trends in Child Mortality Rate in Bihar and India
Under 5 Mortality Rate
Source/Year
NFHS 2 ( 1998-99 )
NFHS 3 ( 2005-06)
SRS 2000
SRS 2003
SRS 2006
NRHM Goal by 2010
Bihar
105.1
84.8
India
95
75
< 50
< 50
Direct estimates of infant and child mortality indicators at district level are not
available, though estimates using census data on children ever born and children
surviving are available but are inconsistent and not reliable. Hence this data is not presented
in this report. The District Level Household Survey (DLHS 2002-03) does not provide
district level infant and child mortality estimates. Thus no reliable estimate of infant
and child mortality is available at the district level. (Bihar_NIPI, 2009)
Table 18 Distribution of Women Receiving Pre-Natal Care by Source of Care
23.5
Govt
Doctor
17.7
Pvt.
Doctor
44.1
NGO
Doctor
2.9
2
20
28
40
3
21.2
15.2
4
7.5
5
Quintiles
ANM/BHW
Others
Total
1
11.8
100
8
4
100
45.5
15.2
3
100
25
57.5
5
5
100
7.7
20.5
64.1
2.6
5.1
100
Total
15.2
Source- (Srivastava, 2003)
21.1
51.5
6.4
5.9
100
30
NIPI Reference Book-Bihar
2.2 Key Achievements in MCH in Bihar
Maternal Health, including Janani Suraksha Yojana (JSY) (Bihar State Report)
−
Number of JSY beneficiaries in the state increased sharply from 0.90 lakh in
06-07 to 8.38 lakh in 07-08 and 10.51 lakh in 08-09.
−
Training on Life Saving Anaesthesia Skills (LSAS): Six medical colleges have
been identified for the purpose, 14 master trainers and 74 MBBS doctors have
been trained in LSAS against a target of 76.
−
Training in comprehensive Emergency Obstetric Care (EmOC): Patna Medical
College has been strengthened as a training site, eight master trainers and 40
MBBS doctors have been trained in EmOC against a target of 76.
−
Skilled Birth Attendant training (SBA): 20 districts have been identified, 150
district level master trainers and 592 SNs/ ANMs have been trained as SBAs,
against a target of 2895.
−
Outsourcing of blood banks in public private partnership model has been
initiated in 4 districts and MoU has been signed in 17 districts.
−
Emergency referral service has been initiated in Patna municipal and sub
urban area.
While the number of institutional deliveries under JSY has increased to 10.51
lakhs in 08-09, Bihar is yet to adequately gear up facilities to meet the load: (Bihar
State Report)
−
The state has operationalized 533 PHCs that operate 24x7 so far against the
target of 821 PHCs by 2010. While monthly NRHM reports submitted by the
state reports all the planned (76) FRUs as
−
Functional - there are only 3 FRUs that fulfil all the three critical criteria of
functionality (as reported during a recent review). A large number of FRUs do
not provide the stipulated range of services due to lack of access to blood
storage facilities and lack of specialist staff.
−
A rapid assessment of functionality of FRUs and 24x7 PHCs was carried out
in the state through GoI/ Development Partner support. There is no indication
that District CMOs & District Program Managers are utilising facility survey
31
NIPI Reference Book-Bihar
findings for comprehensive planning of operationalization of FRU and PHCs,
including linking the same with EmOC and LSAS trainings, placing
anaesthetic drugs, SBA drugs, operationalizing OTs, and establishing Blood
Banks/ Blood Storage facilities at FRUs.
−
There is irrational selection and placement of trained staff with the result that
the existing staff is not used appropriately. Further, LSAS and EmOC trained
doctors are yet to be posted at FRUs.
−
SBA training was initiated but stopped due to the floods. Now there is a need
to immediately begin the training with plans for scaling-up and monitoring the
quality of the training. SIHFW was instructed by the State Health Society
(SHS) for monitoring but the quality of the training is not yet maintained, post
training supervision is weak, and basic protocols in labour room during
delivery are not followed.
−
State and District Level Quality Cell are yet to be created for monitoring the
skilled based training. Evaluation of the trainees needs to be done at the site of
posting/ service provision.
−
Referral transport services need to be strengthened and systematically rolled
out.
Child Health: (Bihar State Report)
−
Integrated Management of Neonatal and Childhood Illness (IMNCI) is ongoing in
23 (out of 38) districts of the state.
−
Six SNCUs are functional in the state and are to be replicated in 23 districts in
year 2009-10.
−
IMNCI trained ANMs run sub centre clinics on Thursday in few districts, which is
to be extended to all districts by 2009-10. The state is considering the option of
decentralised hiring of doctors through Rogi Kalyan Samitis (RKSs) at facilities,
for running the clinics once a month
Neonatal mortality rate or NMR (deaths of newborns within 4 weeks of life per 1000
live births) at 31 (SRS 2007) accounts for 53 percent of the IMR, while early NMR
32
NIPI Reference Book-Bihar
(newborn deaths within one week of life per 1000 live births) at 27 (SRS 2007)
accounts for 87 percent of the NMR. An evaluation of Janani Suraksha Yojana in the
state in December 2008 highlighted that only 11 percent of the beneficiaries surveyed
stayed for at least two days in the health facility after delivery. With the huge off take
in JSY in the state (10.51 lakh beneficiaries in 2008-09), this is clearly a missed
opportunity to address early neonatal mortality. (Bihar State Report)
Other Initiatives (Bihar State Report)
−
Outsourcing of Additional PHCs: 46 APHCs have been handed over to 12 NGOs
covering nine districts.
−
Six GNM and 21 ANM schools have been made functional in the current year.
The state has also developed an online system to monitor service delivery and
logistics availability at the PHCs.
−
Immunization (Bihar State Report)
− As per the various evaluated surveys the immunization coverage shows an
improving trend with full immunization increasing to 41.4 percent in 2007-08
(DLHS 3)
− The state initiative of Muskaan is apparently showing good results including
immunization coverage. There has been very good progress in immunization
training of the health workers (11478/12675)
− District level committees to monitor Adverse Effects Following Immunisation are
constituted in 25 out of the total 38 districts. 90 percent of these committee
members are trained.
2.3
State Schemes to Improve Maternal and Child Health
Ongoing health related programs in Bihar
In order to improve the implementation of several child and related maternal health activities,
certain programs are ongoing currently such as of Janani Evam Bal Suraksha Yojana,
Reproductive and Child Health Care Services, Anaemia Control Program, Vitamin – A
33
NIPI Reference Book-Bihar
Supplementation Program, NRHM, Routine Immunization & Pulse Polio, Mamta and IMNCI
program. (Bihar_NIPI, 2009)
Janani Evam Bal Suraksha Yojana:
Janani Evam Bal Suraksha Yojana under the overall umbrella of the National Rural
Health Mission integrates the benefit of cash assistance with institutional care during
delivery, coupled with antenatal care and immediate post-partum care. This is to
reduce maternal as well as infant mortality. Under this scheme, pregnant women from
BPL families in rural areas will receive INR 1400 and those in urban areas will
receive INR 1000. This is to encourage registration with a clinic and go to a
government or private hospital for delivery. The scheme has been implemented in the
state since July 1, 2006 and so far 3.5 lakh registrations and 89839 deliveries have
taken place. To include the private nursing homes in this scheme, so far 53 private
nursing homes have been accredited. This can be considered a good progress in the
program. (Jha, 2007)
Reproductive and Child Healthcare (RCH) Services
These services basically include three major packages. The first package is for
mothers, which includes early registration, antenatal care, institutional deliveries and
deliveries by SBAs, home-based postnatal care and increased facilities for MTP. The
second package is for newborns which includes skilled care at birth, IMNCI for
common childhood illness and immunization. Other services include increased choice
and availability of family planning services, gender sensitization and gender equality,
and prevention and management of RTIs & STIs etc. (Jha, 2007)
Anaemia Control Program
Decrease in the haemoglobin level which affects the oxygen carrying capacity of
blood is known as anaemia. Under this program, pregnant and lactating mothers are
given IFA (Iron and Folic acid) tablets to prevent anaemia during pregnancy.
Therefore, IFA tablets are distributed to all the pregnant and lactating mothers
through Anganwadi Centres. (Jha, 2007)
Vitamin – A Supplementation Program
34
NIPI Reference Book-Bihar
Government of Bihar and State Health Society have been successful in the
implementation of the Vitamin ‘A’ supplementation Program for pre-school children.
It has, therefore, been decided to undertake the same for the children between the age
group of nine months to five years in all the 38 districts of the state, following the
biannual fixed day strategy linked with Routine Immunization. Children between nine
months and five years of age would be covered with six monthly doses of Vitamin A
syrup. The state has been conducting catch-up rounds of Vitamin-‘A’ and has got
exceptional success in it as its coverage soared to 95 percent. As a long term strategy,
diet management has been included in all training and communication materials. (Jha,
2007)
Routine Immunization & Pulse Polio
The year 2006 was declared Routine Immunization year by the State Government.
The efforts of the year have yielded results, as the dismal figure of 11% complete
immunization has improved to 34 percent and the projected figure by the end of this
year (2007) is 60-70 percent. Polio rounds are also being taken up regularly. The
target of the State Government is that by year 2010, all the districts in Bihar would
provide timely and safe immunization with all antigens (plus 2 dosages of Vitamin
‘A’) to all children between 12-23 months (100 percent coverage) and all pregnant
women with 2 doses of TT (100 percent coverage). Under the Intensive Pulse Polio
Immunization, micro plans including area maps are available and special emphasis
has been given on Information, Education and Communication (IEC) and social
mobilization. (Jha, 2007)
National Rural Health Mission (NRHM)
Bihar is a focused state. It has as its key components provision of a female health
activist in each village (in case of focus State); a village health plan prepared through
a local team headed by the Health & Sanitation Committee of the Panchayat;
strengthening of the rural hospital for effective curative care made measurable and
accountable to the community through Indian Public Health Standards (IPHS);
integration of vertical health & family welfare programs for optimal utilization of
funds and infrastructure and strengthening delivery of primary healthcare. It seeks to
revitalize local health traditions and mainstream AYUSH into the public health
system. It aims at effective integration of health concerns with determinants of health
35
NIPI Reference Book-Bihar
like sanitation & hygiene, nutrition and safe drinking water through a District Plan for
health. (Jha, 2007)
The state has set up institutional arrangements to implement the activities under the
NRHM. If NRHM is implemented effectively, it is expected that the state may have
indicators like other better performing states. (Jha, 2007)
Mamta
Mamta Scheme is an ambitious project aimed at improving the condition of mothers
and newborns in Bihar. Under this scheme, trained midwives would be posted at
hospitals and sub-divisional health centres to take care of mothers and their newborn
babies. The midwives will be paid INR 75 for taking care of a mother and her
newborn. The scheme is expected to attract pregnant women, particularly in rural
areas, to opt for institutional delivery. Besides, the scheme aims to raise awareness
about breast feeding, immunisation and encourage mothers to adopt family planning
methods. The state government and different executing agencies under the National
Rural Health Mission (NRHM) are funding the scheme. (Mamta, 2008)
Home Based Neonatal Care (HBNC)
In the continuum of care, home-based care for the newborn is recognized as a weak
link. The NIPI focus states now recognize that if a difference is to be made in
neonatal and child health, it is important to address and affect what happens in the
home. Since the NRHM already has provided for a voluntary grass root worker, the
ASHA, State Health Societies of the focus states have chosen to build on her presence
and competency to create a structured follow-up system for both the mother and the
newborn.
The intervention:
The intervention consists of three parts. (CHPNC, 2009)
o A special training module (2+5 days) on home-based newborn care.
o An incentive to the ASHA for completion of the PNC check-up routine
o A referral fund to ensure that sick newborns and mothers can be referred to
a facility with proper care available
Under this scheme the ASHA is to visit the home of the beneficiary six times within
the first twenty eight days of birth. The first visit will be during the last phase of the
36
NIPI Reference Book-Bihar
pregnancy (eight month). This will be in addition to the already established antenatal
care that is provided within NRHM, and the main purpose of the first visit is to
motivate the mother for an institutional birth, make sure she is aware of JSY and to
identify any risk factors that the mother may have, indicating that the birth should
take place at a even higher level facility. After the birth, the ASHA will visit the home
on day 1 (in case of home delivery), 3, 7, 15, and 28. In the state of Rajasthan there is
an additional visit at day 42. (CHPNC, 2009)
The ASHA will fill a Postnatal Check-up card (PNC-card) during the visit, which is to
be submitted for validation and payment after the total check-up has been completed.
In addition to basic information such as birth and weight, the card will also provide
information about morbidity and mortality, referrals, immunization, breastfeeding
status etc. (CHPNC, 2009)
37
NIPI Reference Book-Bihar
Chapter-3
Public Private
Partnership
38
NIPI Reference Book-Bihar
3. Public Private Partnership (PPP)
3.1 Key stakeholders in Healthcare’s PPP
There are five key stakeholders in any healthcare service system as shown below.
Implementing a healthcare PPP will have an impact on all these stakeholders and the PPP
itself can be structured along any of the roles where private sector participation is applicable.
(PPP in Healthcare_CII)
Table 19 Stakeholder roles in a Healthcare PPP
Participant Type
Role Description
Public or Private
Entity providing the core services of designing, building and operation
of healthcare units.
Payer
Public or Private
Entity or person paying for the service rendered to the end user. Outof-pocket expenses where the end-user pays for himself/herself still
forms a large part of this segment in India. Formal sector consists of
insurance players both in public and private sectors where the end-user
comes under medical cover.
Beneficiary
Neutral
End-user or the ultimate recipient of the healthcare service. Currently
impacted by high costs as percentage of income and significant
vagaries in quality of service across the country
Regulator
Public
An apex body governing the formal healthcare market in the system.
The role of a central regulator will be key to monitor the expansion
and sustainability of a scalable PPP model
Public or Private
Resource, expertise and management provider for connectivity and
sharing of data on patients, specific medical cases, diagnoses and
treatment techniques is an area of development that can bridge the
quality and accessibility gap across regions in the country.
Provider
IT
Infrastructure
Source- (PPP in Healthcare_CII)
3.1.1 Department for International Development (DFID)
DFID has approved the Bihar health sector reform program Sector Wide Approach to
Strengthening Health (SWASTH) recently with a budget of GBP 145 million. This will be
one of the largest and most integrated health programs of DFID where it will be working with
three departments simultaneously. The Bihar TAST team is all geared up to take on the
challenge of implementation and to improve services through sector reforms in one of the
poorest states of India. (Medha Soni, 2010)
39
NIPI Reference Book-Bihar
3.1.2 Norway- India Partnership Initiative (NIPI)
The Norway- India Partnership Initiative is an outcome of a commitment by the Hon’ able
Prime Minister of Norway and the Hon’ able Prime Minister of India, focusing on the issue
of reducing child mortality and improving child health to attain the Millennium Development
Goal 4 by the year 2015. Norway has contributed USD 80 million over five years for this
purpose to the five states of Orissa, Bihar, Madhya Pradesh, Rajasthan and Uttar Pradesh.
These States together constitute 40 percent of India’s population and contribute almost 60
percent of child deaths in India. The NIPI activities are for five years (2007-2012) and
corresponds with the duration of the NRHM. (NIPI_GoO)
The activities under NIPI are put into operation through UN organizations like UNICEF,
WHO and United Nation’s Office for Project Services (UNOPS). While UNOPS is a local
fund agency and operates through the NIPI Secretariat, UNICEF and WHO have a grant of
USD 20 million and 10 million each respectively for program implementation in the five
focused states. Many of the recent initiatives of UNICEF in child health sector in Bihar are
funded by NIPI. (NIPI_GoO)
Aims & Objectives
With sustained effort by the Government of Bihar, child health indicators have shown
improvement, but extra efforts are needed to achieve the MDG 4. (NIPI_GoO)
NIPI aims at accelerating the child health interventions:
1. Based on block, district, region and state specific situations.
2. Through partnership and collaborative arrangements with professional organizations,
NGOs, local elected bodies and administration within the state.
3. Aimed at making child health visible through catalytic input and create a mechanism
that will ensure sustainability under NRHM processes.
Core Interventions
The core interventions of NIPI are:
Capacity building of frontline workers in home-based newborn and child care and community
mobilization.
Institutional strengthening at block and district level to meet the expanding requirements related
to quality child and related maternal health service delivery. (NIPI_GoO)
Complimenting these, NIPI will support the state and national governments in developing and
optimizing a Management Information System on child health and related maternal health. The
40
NIPI Reference Book-Bihar
Partnership is deeply committed to equity-driven, gender-sensitive, and pro-poor principles
approach and it would endeavour to draw upon and enhance the strong equity rubric of the
NRHM. (NIPI_GoO)
Institutional Mechanism
The institutional mechanism of NIPI is led by a Joint Steering Committee with Secretary,
Health and Family Welfare, Government of India as Chairperson and the Norway
Ambassador to India as the Co-Chair. Additionally, there are representatives of Government
of India, Government of Norway, WHO, UNICEF and the NIPI focus States. At the state
level, activities under NIPI will be implemented by the Bihar government.
3.2 PPP Initiatives by Health Department, GoB
Private Specialists (Status, 2009)
-
From District Hospitals to PHC
Provision of Private specialists in Ophthalmology, ENT, Orthopaedics,
Paediatrics, Gynac. and Surgery
The doctors are to be paid INR.500 per day.
Renowned doctors being contacted
Total number of doctors empanelled is 217 (Source : Data Centre)
Mobile Medical Units (Status, 2009) (MMU)
-
-
-
Scheme of 1 MMU per district launched on July 13 2009
Total Functional MMUs in Bihar till date:- 12
Rest to start operations from November end onwards
Staff per MMU includes Specialist Doctor, Nurse, X-ray Technician, Lab.
Attendant, Para Medic/ Pharmacist cum Van Supervisor, OT Assistant and
Driver.
Services per MMU – Free OPD, Free Drugs, Gynac/ANC clinic, Eye
check up, ENT check up, HIV testing, Pathology, Radiological tests, IEC,
Medical camps etc.
Budget Sanctioned in FY 09-10 is INR16.56 cr.
Rent Per Month INR 4.68 lakhs for one MMU
Dial 108 (Status, 2009)
-
Pilot in Patna city through PPP
In operation from June 3, 2009
2 kinds of Ambulances – Five Advanced Life Support and five Basic Life
Support
41
NIPI Reference Book-Bihar
-
Basic facilities – Drugs, Oxygen, Heart monitor, ventilator and other
supportive medical system
Patient fees- INR300. Very poor patients would receive treatment at lower
rates or for free.
15-20 minutes service availability
GPS fitted
Total number of calls – 3509 (June’09 to Oct’09)
Diagnostic Services (Status, 2009)
-
Free Services to all Patients at the PPP operational centres from PHC to
DH
Free Services to all BPL Patients at the PPP operational centres in the
MCH
Pathology Services (Status, 2009)
In the government hospitals pathology services to the needy patients were not
provided efficiently due to paucity of lab technicians and irregular supplies of
reagents required for pathological tests. The state decided to outsource pathological
services to reputed private labs in order to improve them in the government hospitals.
Two agencies have been selected through a tender process. The agencies have set up
labs at the District Hospitals and sample collection centres at the health facilities
below district levels. In the state 407 centres are operational. More than 4 lakhs tests
have been conducted in the last two years. (PPP_BSHS)
-
Private sector provider operates, maintains and reports through 24-hours
Diagnostic centres
Coverage : 25 District Hospitals, 23 Sub-Divisional Hospitals, 76 Referral
Hospitals and 398 PHCs of Bihar
19 districts each divided among two agencies for Pathology
Agency pays nominal monthly rent for space in DH & SDH
District Hospitals have Labs
Collection Centres at PHCs
Reports within 24 hours
Number of Tests conducted – 5.58 lakhs (Mar 06-Apr 09)
Services started in 407
Radiology Facilities (Status, 2009)
The state had decided to outsource radiology services in all the government health
facilities. About 151 radiology centres have been operationalized. These centres have
42
NIPI Reference Book-Bihar
provided X-ray services to 3.53 lakhs patients in the last two years. Ultrasound
Facilities in the District Hospitals and Sub-divisional Hospital are also being
provided. (PPP_BSHS)
-
38 districts given to one agency to operate, maintain and generate x-ray
films
Functional units – 134
Space provided against nominal rent
No investment by Government
Government doctor reports on films
Reports within 24 hours
Functions under the overall supervision of the Hospital Management
Society (RKS) of the respective Hospital.
Functions under the operational control of District Health Society
Number of Tests conducted – 3.71 lakhs (July 06 to Apr 09)
Services started in 91 centres
Hospital Maintenance Services (Status, 2009)
The support services for the cleanliness of the hospital’s wards and the premises were
not up to the mark and the washing of the bed sheets, linen and other apparel were not
proper due to paucity of adequate numbers of sweepers and washer men. Due to
recurrent powercuts the maintenance of the cold chain of the vaccines was also not
proper. Similarly the diet given to the in-patients was not satisfactory. In order to
improve the support services in the hospitals the state decided to outsource these
services to private agencies and NGOs through a tender process. The following
support services have been outsourced: (PPP_BSHS)
-
Maintenance of Hospital Premises.
Generator Facility.
Cleanliness of Hospitals.
Laundry
Diet for in-patients
Centralized rate contract finalized and each district was given three parties
to choose from. All 38 districts have already started using these services
Outsourced Services – Quality issues (Padmanabhan, 2009)
-
21 contracts were signed by SHS, Bihar with private agencies.
A checklist developed to monitor the quality of services
Registers and checklists have also been prescribed for outsourced agencies
to prevent false claims
Maternal & Child health Improvement (Padmanabhan, 2009)
43
NIPI Reference Book-Bihar
-
APHCs to be made functional with paramedical model
One CEmONC for each district
VHSCs to be formed
Use of HSC untied funds
Community monitoring system
Use of trained anaesthetists by reorientation
Rational distribution of human resources
Encourage the use of self improvement NRHM quality manual by the
health facilities in the state by conduct of regional workshops
Fast tracking ASHA training program
-
Generic Drug Shops
For making drugs available at comparatively cheaper rates to the patients, an initiative
has been taken to set up generic drug shops. Three generic drug shops are being set up
in each of the six Medical College Hospitals; two in each of the 38 District Hospitals
and two in other hospitals. (PPP_BSHS)
Funds have been sent to 23 DHSs for the construction of drug stores. Five drug stores
have been constructed. (PPP_BSHS)
Data Centre: At State & District level:From the state level monitoring is done through the State Data Centre on a daily basis
through telephones. Detailed reports are being posted on the SHSB website. An
option
to
receive
public
feedback
has
been
provided
on
the
website
www.statehealthsocietybihar.org. (PPP_BSHS)
Blood Storage Units:
To ensure provision of quality blood to the needy patients, blood storage units are
being set up in 76 FRUs of the state through the PPP model. While 21 units have been
operationalized by the Bihar AIDS Control Society, the remaining 55 units are in the
process of operationalization in PPP model. (PPP_BSHS)
APHC Outsourcing:
It has been decided to provide 24 x 7 hours services at PHCs. To enable this service
all available staff has been deployed to the PHCs. The APHCs have been outsourced
to private agencies to provide proper OPD services, routine immunization and ANC.
44
NIPI Reference Book-Bihar
Presently about 44 APHCs have been outsourced while outsourcing of the remaining
APHCs is in process. (PPP_BSHS)
Drug Availability (PPP_BSHS)
− Rate Contract for procurement of drugs has been finalized at the state level
and the finalized rates have been provided to the districts.
− The list of free drugs has been expanded to incorporate 33 OPD and 37 IPD
medicines in other hospitals.
− 107 IPD drugs in each hospital of every district.
− In-patient treatments to be free in all District Hospitals
− Doctors instructed to prescribe only generic drugs to patients.
Monitoring & Evaluation: (PPP_BSHS)
− At the state level monitoring is done through the State Data Centre on a daily
basis. Detailed reports are being posted on the SHSB website.
− Officials of the Department visit the health facilities to monitor activities
there.
− DMUs have been instructed to adopt PHCs to ensure better performance.
− Evaluation of Free Drug Distribution Scheme & JBSY is being done through
third party.
− Performance-based ranking of districts is being undertaken on select health
indicators.
3.3
PPP in Rest of India and World on MCH
3.3.1
Chiranjeevi Yojana (CY)
CY was created to significantly reduce maternal and infant mortality by harnessing the
existing private sector and encouraging it to provide delivery and emergency obstetric care at
no cost to families living below the poverty line. Under the scheme the government contracts
private providers that volunteer to render their services by signing a Memorandum of
Understanding with the district government. In return, they receive an advance payment to
commence services and are compensated at about USD 4,500 per 100 deliveries (normal,
caesarean, or with other complications). Any qualified private provider with basic facilities,
45
NIPI Reference Book-Bihar
such as labour and operating rooms, and access to blood bank and anaesthetists can enroll in
the program after a thorough orientation. CY beneficiaries are enrolled through their family
health workers. The scheme uses the existing cards issued to families living below the
poverty line by the rural development department of the state government to access services.
In the first six months since the launch of the scheme, each provider performed an average of
116 deliveries. The institutional delivery rate has increased from 54.7 percent to more than 81
percent in 2005–06. CY’s long-term goal is to achieve an institutional delivery rate of 95
percent by 2012. (CHMI, 2011)
Key program components include:
Benefits Package. CY uses demand-side financing to provide families living below the
poverty line with access to a comprehensive benefits package that covers both direct and
indirect costs, including free delivery (with no condition exclusions), free medicines after
delivery, and transport reimbursement. In addition, it offers support to the attendant in
exchange for lost wages. The payment method and formula encourage providers to reach
a certain volume of work, avoid complicated transaction costs, and create a disincentive
for unnecessary Caesarean section surgeries. The provider compensation package is
designed to account for all potential complications during delivery (estimated at 15
percent of cases). (CHMI, 2011)
Contract Management. CY’s district management authorities require participating doctors
to maintain a case file for each patient they serve. Weekly records of the deliveries
conducted by the providers are submitted to local authorities and the block (sub-district)
health officer, who regularly visits beneficiaries to monitor service quality and address
grievances. Payment to providers is also made through block health officers based on
instructions from district authorities. All districts send a monthly report to state
authorities for review and feedback. (CHMI, 2011)
District Management Capacity. CY employs a decentralized management model that
engages health officials at four government levels (state, district, block, and village) as
facilitators and organizers of health services. To implement the scheme state-wide,
officials at various levels play interlinked and overlapping roles. These roles are divided
into state level (state-wide planning, implementation, and monitoring of the scheme),
district level (district wide implementation, provider enrolment and orientation, provider
compensation, and report collection), block level (registration of beneficiaries, bill
collection from providers, and overall supervision), and village level (motivating
expectant mothers to use institutional delivery and facilitating their visit). (CHMI, 2011)
46
NIPI Reference Book-Bihar
3.3.1 Janani
Janani started a social marketing and social franchise program that uses India's large
private health sector network of practitioner and facilities to provide safe and low-cost
options for family planning, health, and reproductive health services in rural areas.
(CHMI, 2011)
The conventional social marketing infrastructure of shops (more than 31,000 in number)
and stockists sells products (such as contraceptives) in urban and semi-urban areas and
replenishes supplies to rural health franchisee centres and franchisee medical clinics. This
is complemented by a social franchisee program through which doctors in rural areas
provide low-cost clinic-based services. The social franchise has a network of rural health
practitioners who work in partnership with a female family member. She serves as the
conduit between the clinics and rural communities. After receiving Janani training, rural
practitioners are franchised as Titli (Butterfly) Centres, and they sell nonclinical products
and over-the-counter pregnancy tests. Clients needing clinical services are counselled and
referred to the nearby Surya Clinic, which earns the Titli Centres a commission. Under
the private-public partnership of the NRHM the government has accredited 15 of Janani’s
Surya Clinics as authorized sterilization centres, which the government reimburses USD
35 to the clinic for each sterilization. The plan is to set up 40 free clinics at the district
headquarter town by the end of December 2009. More than 40,000 trained networked
rural providers are monitored by project field teams set up by entrepreneurs, and the 620
franchisee medical clinics are supervised by Janani. (CHMI, 2011)
Key program components include: • Social marketing for the underserved. The
conventional social marketing franchise uses shopkeepers (mostly in urban centres) to
deliver primarily nonclinical products such as condoms and oral contraceptives. In
contrast, Janani’s model focuses on expanding service delivery from urban to rural areas,
integrating a strong clinical component and catering to the poorest segments of the
population. (CHMI, 2011)
Profitable franchisee product bundle. The rural health providers find the franchise
profitable and worth belonging to because of a broad mix of income-generating
services including the sale of non-clinical products, charges for over-the-counter
diagnostic tests, and commissions for referring clients needing clinical services to the
Surya clinics. (CHMI, 2011)
47
NIPI Reference Book-Bihar
Formalizing the private sector. Janani has played an important role in bringing rural
providers and private doctors into a formal operational framework. The Surya health
promoters in the network receive training in non-clinical skills to function as the first
point-of-contact in the villages, while the surgical skills of doctors in the Surya
clinics are upgraded to provide quality family planning services and comprehensive
abortion care services. This has effectively complemented the network of shops that
have long worked with the well organized private sector. (CHMI, 2011)
Fostering community-level ownership. Janani seeks to transform participants into
stakeholders at both the rural and urban levels. About half of Janani’s budget is for
communication and education campaigns, a critical component of which is
empowering clients about quality services so they can maintain pressure on providers
for good-quality care. To complement this, Surya health promoters are selected from
within communities. (CHMI, 2011)
3.3.2
Child Helpline International
Child Helpline International (CHI) facilitates the establishment of helpline services in
countries were these facilities and services do not exist and helps scale-up helpline services
that work primarily on a district level. In developing nations where state mechanisms are
unable to reach children in crisis, it has been seen that helpline services provide an efficient
link between children and the system. (CHMI, 2011)
Additionally, CHI also concentrates its efforts on advocacy and child participation. CHI
hopes to bring the issues and concerns of children from around the world to the attention of
policy makers in all corners of the world, ensuring children have a voice and that their voices
are heard. (CHMI, 2011)
Objectives:
To place children on the global telecom agenda
To pass a resolution in International Telecommunication Union (ITU) which makes
helpline services a global strategy in reaching out to children
To allocate funding for bridging the digital divide and ensure that children, especially
the marginalised child, have access to telecom
In 2004, 11.5 million calls were received at child help lines across the globe. By establishing
and scaling-up helpline services, CHI endeavours to bring these services to as many children,
especially the most marginalised, as possible. (CHMI, 2011)
48
NIPI Reference Book-Bihar
In May 2004, the helpline was officially launched in Vietnam. The helpline is a partnership
between Plan Vietnam and the Committee on Population, Children and Families (VNCPFC).
The helpline operates in Hanoi and is now looking to expand to other cities in Vietnam. The
helpline has a free number (1800 1567) which is active from 7a.m. to 9p.m. daily and has,
since its inception, received around 12,000 calls. The helpline number can be directly called
from anywhere in Vietnam, so it is very easy to reach. A large number of phone calls have
been received for advice on domestic violence, child sexual abuse, abandoned children and
child accident etc. (CHMI, 2011)
The helpline has also started on-line counselling services relating to reproductive health,
children’s rights and psychology as an addition to the telephone service already provided. In
addition, two centres for the protection of children have been operational in Ho Chi Minh (in
the south) and Da Nang city (in central Vietnam) to make the helpline more efficient. (CHMI,
2011)
3.3.3
RapidSMS Malawi
RapidSMS works to address serious constraints within Malawi's National Integrated
Nutrition and Food Security Surveillance (INFSS) System, which faces slow data
transmission, incomplete and poor quality data sets, high operational costs and low levels of
stakeholder ownership. (CHMI, 2011)
RapidSMS allows health workers to enter a child’s data, and through an innovative feedback
loop system, it instantly alerts field monitors of their patients’ nutritional status. Automated
basic diagnostic tests are now identifying more children with moderate malnutrition who
were previously falling through the cracks. This system also increases local ownership of the
larger surveillance program through two-way information exchange. Operational costs for the
RapidSMS system are significantly less than the current data collection system. (CHMI,
2011)
The Government of Malawi, pleased by the results of the pilot, plans on scaling RapidSMS
up nationally later in 2010. They are also interested in expanding this to a country wide
campaign to register child births, as well as deploying RapidSMS in other sectors, including
education and HIV/AIDS. (CHMI, 2011)
49
NIPI Reference Book-Bihar
3.3.4 Vietnam’s Nutritious Food Program
The goal of the project is to reduce the incidence and severity of malnutrition among lowincome, vulnerable, and primarily rural children by expanding access to improve feeding
practices, including giving fortified complementary foods to children 6-24 months of age.
Based on an alliance between the government, food producers, and non-government
organizations (NGOs), the project has enabled the National Institute of Nutrition (NIN) to
further develop an innovative model for increasing production capacity by expanding sales,
reducing unit costs, and lowering the price to consumers, thereby improving the prospects for
sustainability. (CHMI, 2011)
Specific objectives are to: (i) expand localized, commercial production of a fortified, low-cost
complementary food; (ii) develop and expand the system of community-based
complementary food sales, distribution, and enhanced nutrition education; (iii) address
barriers to accessing complementary food among the most poor and vulnerable; and (iv)
address policy development and advocacy for long-term support for fortified complementary
food (as part of a range of options that should be available for addressing malnutrition).
(CHMI, 2011)
The expected outcome of the project is increased access of approximately 325,000 poor
children to fortified complementary food. Over 3 years, the project has worked to open
community-based channels for distribution, marketing, and nutrition education in 6 provinces
and 60 districts. (CHMI, 2011)
Vietnam’s Country Investment Plan (CIP) for food fortification prepared under the Asian
Development Bank’s regional Technical Assistance project outlines a 10-year expansion of
this model to reach 25 percent of vulnerable infants between six to 24-months on a national
basis. This project is a strategic first step in the expansion, with a focus on developing
strategies for scaling up and sustainability as well as ensuring that the product and project
benefits reach the poorest and most vulnerable. The new mechanisms for financial
sustainability have been adopted actively by using the strengths of public–private partnership.
(CHMI, 2011)
50
NIPI Reference Book-Bihar
3.3.5 Karra Society for Rural Action
The Karra Society for Rural Action, in partnership with the Government of Jharkhand and
district healthcare facilities, established a referral network in six blocks of Kunti District in
Jharkhand. (CHMI, 2011)
To address this issue, the Karra Society initiated the establishment of quality referral services
for obstetric and infant healthcare facilities in 320 villages of six blocks in the Kunti district.
The project's objective is to create a pool of village health volunteers with awareness on
reproductive and child health, increase the incidence of safe births by facilitating institutional
deliveries, and encourage community ownership by establishing a call centre in each block
for instant access to referrals. (CHMI, 2011)
To help this initiative achieve its goals, the Society has engaged in community mobilization
for health by strengthening Self Help Groups (SHGs), creating a health fund to be used in
case of emergencies, establishing a call centre available 24 hours a day, seven days a week in
each block, and providing transport vehicles for all villages in the network to facilitate quick
referrals. Furthermore, training is conducted for TBAs, SHGs and Sahiyyas (individuals who
educate pregnant women in rural areas). Awareness sessions are also conducted for future
mothers on proper precautions to be taken during pregnancy. (CHMI, 2011)
As the program helps deliver government maternal and child health programs, the
government has decided to partner with the Karra Society and UNICEF to support the design
and development of this model. In 2009, about 1354 patients utilized the Society's services
and 769 were referred to higher levels of care. (CHMI, 2011)
The model appears to be able to successfully control maternal and infant deaths in the region,
documenting about two maternal and 12 neonatal deaths since it began operations. (CHMI,
2011)
3.3.6
Wired Mothers
The study aims to examine the beneficial impact of mobile phones for healthcare on maternal
and neonatal morbidity and mortality, and to seek innovative ways to ensure access to skilled
attendance at delivery through an intervention called "wired mothers". Wired mothers are
pregnant women linked to a Primary Healthcare Unit through mobile phones receiving
standard SMS reminders for care appointments and who can call the primary provider in case
of acute or non acute problems. The study also looks at the health system's response in
51
NIPI Reference Book-Bihar
relation to obstetric emergencies when using mobile phones thereby strengthening
communication between the different levels from TBA to referral hospital. (CHMI, 2011)
Specific objectives
To study the attendance of wired and non-wired women at routine primary healthcare
appointments.
To study the level of facility-based deliveries amongst wired and non-wired women.
To study morbidity amongst wired and non-wired women.
To study the quality of services provided to wired and non-wired women.
To study neonatal morbidity and mortality amongst children delivered by wired and
non-wired mothers.
The project was initiated in January 2009 and completed in December 2010
52
NIPI Reference Book-Bihar
Chapter-4
NIPI Focus Districts’
Profile
53
NIPI Reference Book-Bihar
4. District Profile
4.1 Nalanda
4.1.1 Introduction
Nalanda is one of the important districts of Bihar with an area of 2367 sq.km and a
population of over two million. Bihar Sharif is the district headquarters and the district is
flanked by two important rivers namely Phalgu and Mohane. The decadal growth rate for the
year 1991-01 was estimated at 18.6 percent, the lowest for all the states of Bihar. The sexratio of the district is recorded at 915 females per 1000 male population. The percentage of
SC & ST population stands at 19.4 percent and 0.02 percent respectively, which is much
lower than other districts of Bihar. A marked disparity was noted between male and female
literacy rates, at only 39.6 percent for males compared to 66.9 percent for females.
(Bihar_NIPI, 2009)
The modern district of Nalanda with HQ Bihar Sharif was established on November 9,
1972. Earlier it was Bihar Sharif sub-division of Patna district. (Nalanda_DHP, 2010)
Table 20: Nalanda – At A Glance (Nalanda DHP, 2010)
AREA ( Sq. Kms)
2367 Sq Km
Population(Census 2001)
Total
2370528
Males
1238599 (52.24%)
Females
1131929 (47.75%)
Rural Population
Total
Males
Females
2014948
1052608 (52.23%)
962340 (47.76%)
Urban Population
Total
355580
Males
184094 (51.77%)
Females
171531 (48.23%)
Population Of Scheduled Castes
473786 (19.98%)
Population Of Scheduled Tribes
Density Of Population
Sex Ratio
970
1007
915
54
NIPI Reference Book-Bihar
Table 21: Comparative Population data (2001 Census) (Nalanda_DHP, 2010)
Basic Data
India
Bihar
Nalanda
Population
1027015200
828787
2370528
Density
324
880
1007
Sex- Ratio
933
921
915
Total
65.38
47.53
53.64
Male
75.85
60.32
66.44
Female
54.16
33.57
38.58
Literacy (%)
Demographic
Indicators
Density
Decadal Growth
rate (1991-2000)
Population
Nalanda
Bihar
1007
880
18.64%
28.43%
2370528
8,28,78,796
Male
1238599
43243795
Female
1131929
39754714
0-6 years
461240
16806063
0-6 years - male
237527
8652705
0-6 years female
223713
8153358
SC
19.90%
15.72%
ST
0.04%
0.91%
BPL
58.80%
42.60%
Sex Ratio
Early age of
marriage
915
921
59.60%
51.50%
Literacy
53.64%
47.53%
Male literacy
66.44%
60.32%
Female literacy
38.58%
33.57%
Crude birth rate
31.20%
29.90%
62
60
4.2
4.3
Infant Mortality
rate
Total Fertility
Rate
(Nalanda_DHP, 2010)
These tables show the demographic scenario of Nalanda district. According to
Census of India 2001: (Nalanda_DHP, 2010)
− The size of population of Nalanda district is above 2370528 comprising 2.86
percent of the population of Bihar state in 2.51 percent of the state’s area.
− Very high density of population (1007) which is still rising
− Decadal population growth rate of 18.6 percent as against 28.43percent of the
state as whole. Thus the decadal growth rate of the district is lowest than that of
55
NIPI Reference Book-Bihar
the state.
− Sex ratio of the population is 915 females per thousand males which is less than
the sex ratio of the state. It is difficult to interpret the deficit of 85 females per
thousand males in the district despite outward migration, predominantly of males
in the working ages. A possible explanation seems to be that over the years male
population has benefited more from the epidemiological transition than the
female population.
− Only 15 percent of the population resides in the urban area, and the rest lives in the
rural areas.
General
Information
Nalanda
Bihar
Agriculture
Paddy, Wheat, Potato, Onion,
Vegetables
Paddy, Wheat, Jute,
Maize, Oil Seeds,
Sugarcane, Barley
etc.
Industry
Handloom. Weaving
Ordinance Factory(Under
Construction), Railway Coach
Maintenance Factory (Under
Construction)
Oil refinery,
Fertilizer factories,
Cotton spinning
mills, sugar mills
Prone to flood
Yes
Yes
(Nalanda_DHP, 2010)
Based on these statistics one can say that Nalanda district lacks urbanization and
industrialization. As far as industrialisation is concerned the situation is expected to
improve on completion of the two projects mentioned above. Population density
of this district is 1007 per sq. km. which is also high in comparison to the state density.
Decadal population growth is lowest i n this district in Bihar, which is a positive sign.
(Nalanda_DHP, 2010)
Government Administrative Set-up
The district comprises three sub divisions and 20 blocks. There are also 1084 revenue
villages and 249 gram panchayats. Traditionally the district was divided into 12 C.D.
blocks but eight more blocks were created during last decade. The newly elected
Panchayati Raj is enthusiastic in playing an important role (Nalanda_DHP, 2010)
56
NIPI Reference Book-Bihar
Figure 3: District Health Administrative Setup (Nalanda_DHP, 2010)
General Indicators
Nalanda (HQ Bihar Sharif)
Bihar
Subdivisions
3
9 divisions,
101 subdivisions
Blocks
20
534
Towns
3
No. of
Municipalities
1
Gram Panchayats
249
Revenue Circles
20
Villages
1084
Source: (Nalanda_DHP, 2010)
8471
45,103
57
NIPI Reference Book-Bihar
4.1.2 District Health System
In a study of 593 districts of the country (Jansankhya Sthirata Kosh", www.jsk.gov.in) in
terms of overall rank in health it was found that Nalanda district ranks 509 though on the
basis of under-five mortality it ranked 328. Filaria, Malaria, Kala-azar, skin diseases, and
Tuberculosis are some of the most common diseases in Nalanda district. Hepatitis, Diarrhoea,
Typhoid, Blindness and Leprosy are other high prevalence diseases. (Nalanda_DHP, 2010)
Table 22: Health Indicator
Indicator
Nalanda
Bihar
India
CBR
32
31
1.4
CDR
N.A
8.1
6
IMR
60/1000
61
58
MMR
452/100000
371
301
TFR
4.3
4
2.68
CPR
21.5
Complete
Immunization
38%
32.8
Sources: DLHS3, NFHS3, SRS2007 (Nalanda_DHP, 2010)
Table 23: Institutional Delivery in Nalanda district (PHC wise) (Nalanda_DHP, 2010)
S.
No.
Name of PHC
April
May
June
July
August
Sep.
Oct.
Nov.
Dec.
Jan.
123
138
92
151
221
207
229
208
185
47
1
Asthawan
2
Giriyak
92
78
76
123
146
162
159
160
149
92
3
Rajgir
132
231
237
297
300
201
408
325
352
37
4
Harnaut
150
124
122
139
236
274
280
234
240
249
5
Sarmera
44
25
37
37
48
82
126
89
110
61
6
Noorsarai
101
117
124
180
199
253
318
230
214
150
7
Rahui
95
106
106
124
129
199
213
186
147
107
8
Hilsa_PHC
0
0
0
0
0
0
0
0
0
0
9
Hilsa_Sub
139
146
126
193
277
275
318
214
236
51
10
Chandi
96
118
115
166
292
356
392
289
249
203
11
Ekangarsarai
95
148
140
201
240
248
257
212
214
235
12
Islampur
48
32
52
39
65
107
101
76
79
83
13
Sadar_PHC
0
0
0
0
0
0
0
0
0
0
14
Sadar Hospital
1135
762
853
1141
1797
1656
1398
1058
1534
690
15
Urban Health
Centre
0
0
0
0
0
0
0
18
40
35
2250
2025
2080
2791
3950
4020
4199
3299
3749
2040
Total
58
NIPI Reference Book-Bihar
Figure 4 Nalanda District
Table 24 MCH Indicators in Nalanda district
INDICATORS
MATERNAL HEALTH
Mothers registered in the first trimester
when they were pregnant with last live
birth/still birth (%)
DLHS-2 (2002
- 04)
Total
Rural
DLHS-3 (2007 08)
Total
Rural
NIPI BASELINE
(2008 - 09)
Total
Rural
-
-
25
22.1
42.7
37.40%
Mothers who had at least 3 antenatal care
visits during the last pregnancy (%)
14
13.1
25.2
22.2
38.5
36.6
Mothers who got at least one TT injection
when they were pregnant with their last
live birth / still birth (%)
29.7
27.9
50
47.2
95.3
95.3
Institutional births (%)
27.3
23.4
39.3
34.5
58.6
57.7
Delivery at home assisted by a
doctor/nurse /LHV/ANM (%)
7.5
8.3
7
6.2
20.6
17.9
-
-
27.9
24.2
45.5
42.9
Mothers who received postnatal care
within 48 hours of delivery of their last
child (%)
CHILD IMMUNIZATION AND
VITAMIN A SUPPLEMENTATION
59
NIPI Reference Book-Bihar
Children (12-23 months) fully immunized
(BCG, 3 doses each of DPT, and Polio
and Measles) (%)
Children (12-23 months) who have
received BCG (%)
Children (12-23 months) who have
received 3 doses of Polio Vaccine (%)
Children (12-23 months) who have
received 3 doses of DPT Vaccine (%)
Children (12-23 months) who have
received Measles Vaccine (%)
Children (9-35 months) who have
received at least one dose of Vitamin A
(%)
Children (above 21 months) who have
received three doses of Vitamin A (%)
19
19.8
54.2
53.2
48
48.9
46.4
46.4
88
88.6
97.3
96.9
30.7
29.9
62.8
62.4
73.8
73.8
35.1
28.9
65.1
64.5
71.9
72.9
25.5
25
69.1
69.2
66.8
68
-
-
59.4
58.5
41
43.1
-
-
10.4
11.5
13.1
13.5
0
0
45.3
46.2
44.6
42.6
9.4
0
86.6
86.1
76.4
77.3
-
-
80.9
79.5
82.5
86.4
-
-
28
25.4
9.1
8.3
-
-
28
25
15.80%
14.10%
-
-
30.2
31.6
8.5
8.9
-
-
20.7
20.9
22.5
17.6
-
-
87
87.8
51.5
50.9
TREATMENT OF CHILDHOOD
DISEASES (Children under 3 years,
based on last two surviving children)
Children with Diarrhoea in the last two
weeks who received ORS (%)
Children with Diarrhoea in the last two
weeks who were given treatment (%)
Children with acute respiratory
infection/fever in the last two weeks who
were given treatment (%)
Children who were examined within 24
hours of birth (based on last live birth)
(%)
Children who were examined within 10
days of birth (based on last live birth) (%)
CHILD FEEDING PRACTICES
(Children under 3 years)
Children breastfed within one hour of
birth (%)
Children (age 6 months above)
exclusively breastfed (%)
Children (6-24 months) who received
solid or semisolid food and still being
breastfed (%).
Source- (Bihar_NIPI, 2009)
4.1.3 Health Infrastructure
The District Head Quarter Hospital at Bihar-Sharif together with two referral hospitals,
twenty block PHCs, and 25 APHCs caters to the healthcare needs of the people. There is also
one blood bank and a total of 141 doctors in districts.
60
NIPI Reference Book-Bihar
Table 25: Public Health Care Delivery System: Organisational Structure and Infrastructure
61
NIPI Reference Book-Bihar
Table 26: Health Infrastructure
S.No.
Type of Institutions
Number
Total No. of
Beds*
1
District Hospital
01
120
2
Referral
02
60
3
Block PHCs
20
72
4
APHCs
25
0
5
Sub-centres
305
0
6
Ayurvedic Dispensaries
00
N.A
7
Anganwadi Centres
2246
N.A
8
Others (Pvt. Facility accredited)
04
N.A
9
Blood Bank
01
10
No. of ANMs
650
N.A.
11
No. of Doctors
141
N.A.
(Nalanda_DHP, 2010)
4.1.4 Nalanda Facility Survey Findings
The study done by A N Sinha Institute of Social Sciences for Access Health International in
Sep. 2010 was an attempt to provide insights into the infrastructure available and current
capacity of both governments, corporate and private health services providers of Nalanda
district in neonatal and infant care.
Number of deliveries conducted in the health facility
People prefer government hospitals for delivery due to the facilities that are available
and at no extra cost. Usually a patient in a private hospital incurs an expenditure of
about INR 2500 to INR 3000 for a normal delivery. On the other hand in a
government hospital, the beneficiary receives INR 1400 under the JBSY scheme. As a
result while on an average only 62 deliveries take place in private hospitals, there are
about 260 that take place in a government hospital in a month in Nalanda district
(Ratan, 2010)
62
NIPI Reference Book-Bihar
Average number of deliveries per month
Private Nursing Home/ Private Hospital
Govt. Hospital
62
260
Neonate Outpatients attended
92 neonates
consult the doctor in private hospitals and 80 neonates come to
government hospitals each month. (Ratan, 2010)
Average number of Neonates (OPD) per month
Private Nursing Home/ Private Hospital
Govt. Hospital
92
80
Infant Outpatientss attended
249 Infants come across to consult the doctor in private hospital and 299 infants come
across to the government hospital . (Ratan, 2010)
Average number of Infants (OPD) per month
Private Nursing Home/ Private Hospital
Govt. Hospital
249
299
Consultation Charges for outpatients
INR 61 is the average charge for consultation in a private hospital while in the
government hospital only INR 1or 2 is charged from the outpatient towards
registration. (Ratan, 2010)
Average charge for OPD Consultation (INR)
Private Nursing Home/ Private Hospital
61
Govt. Hospital
1-2
(Only Registration Charges)
Distance covered by patients
Generally 0-1 year old patients travel about 25 kms to consult the doctor in a private
nursing home or private hospital. At the same time patients visiting a government
hospital travel a distance of18 kms for a consultation with the doctor there. (Ratan,
2010)
63
NIPI Reference Book-Bihar
Distance travelled by 0-1 year old Patient to consult the doctor
Private Nursing Home/ Private Hospital
Govt. Hospital
25 Kms.
18 Kms.
Common Ailments of outpatients below the age of one year Fever, vomiting,
diarrhoea, pneumonia, RTI/ARI, cold and cough, loose motions and jaundice where
found in patients at both private and government hospitals while cases of
gastroenteritis, rickets, LBW, paralysis, meningitis and malnutrition have been seen in
private hospitals only. (Ratan, 2010)
Private nursing home/
Private hospital
Govt. hospital
Fever
√
√
Paralysis
√
X
Meningitis
√
X
Jaundice
√
√
Loose Motion
√
√
Cold and Cough
√
√
Diarrhoea
√
√
Pneumonia
√
√
RTI/ ARI
√
√
Gastroenteritis
√
x
Rickets
√
X
Vomiting
√
√
LBW
√
X
Malnutrition
√
x
Common Ailments
Number of Neonate In-patients
Private hospitals for child care in Nalanda is in far better conditions and more in
number than in the other 2 NIPI focused districts. Government hospitals also manage
neonate’s complications to some extent. So the average number of neonate in-patients
in private and public hospital remains almost the same i.e. 28 and 29 respectively per
month. (Ratan, 2010)
Number of Neonates (IPD) per month
Private Nursing Home/ Private Hospital
Govt. Hospital
28
29
64
NIPI Reference Book-Bihar
Common Complications of Neonate In-patients
Common complications like birth asphyxia, jaundice, hypothermia and sepsis & RTI /
ARI are found in the in-patients of private as well as government hospitals while
LBW PEM, gastroenteritis & meningitis are found in the in-patients of private
hospitals only. (Ratan, 2010)
Name of common neonatal complications of inpatient
Private nursing home/
Private hospital
Govt.
hospital
Birth Asphyxia
√
√
Jaundice
√
√
Hypothermia
√
√
Sepsis
√
√
RTI / ARI
√
√
LBW
√
X
PEM
√
X
Gastroenteritis
√
X
Meningitis
√
X
Duration of stay of neonate In-patients in hospital
Government hospitals are not well equipped to handle complications. Only Hilsa subdivision and Sadar hospital manage the complication among neonates at some extent.
So the average length of stay of neonates in a government hospital is about 24 hours
to 2 days in case of complications. On the other hand, private hospitals have proper
facilities and equipment to manage the neonatal complications. So the average length
of stay of neonate in-patients is about 2 to 10 days in Nalanda private hospital. (Ratan,
2010)
Duration of Stay of Neonates (IPD)
Private Nursing Home/ Private Hospital
Govt. Hospital
2-10 Days
24 Hour-2 Days
Hospitalisation cost of Neonate In-patients
The Average expenditure in the hospital that includes the bill and medicine are INR
650 and INR 400 per day respectively while diagnostics costs are above INR 500 per
patient in private hospital of this district. (Ratan, 2010)
65
NIPI Reference Book-Bihar
Hospitalisation cost of Neonates in
inpatient in private hospital
Average Amount
(INR/day)
Terms of expenses
Hospital Bill
650
Medicine cost
400
Diagnostics cost
500
Number of neonatal in-patients between 29 days and 12 months
The number of neonatal in-patients is 26 in private hospitals as against 75 in
government hospitals. This is so because complications or common illness of infants
are managed very well in government hospitals and at no cost. On the other hand the
treatment and hospital bills in a private hospital are unaffordable by poor people. This
results in the government hospitals having more patients of this age than private
hospitals. (Ratan, 2010)
Number of Neonatal in-patients between 29 days and 12-Months per month
Private Nursing Home/ Private Hospital
Govt. Hospital
26
75
Common complication of 29 days-12 months old children inpatients
Complications in neonates between 29 days and 12 months include diarrhoea,
pneumonia, loose motion, RTI / ARI meningitis, and cold & cough. Fever was found
in patients of
both private and government hospitals while cases of jaundice
gastroenteritis, malnutrition and rickets were found in private hospitals only and cases
of hypothermia was found in government hospital only. (Ratan, 2010)
Name of common complication in 29 days - 12 months old children out
patients.
Private Hospital/Nursing Home
Govt. Hospital
Diarrhoea
√
√
Jaundice
√
√
Pneumonia
√
√
Loose Motion
√
√
RTI / ARI
√
√
Mengitis
√
X
Gastroenteritis
√
√
Cold & Cough
√
X
66
NIPI Reference Book-Bihar
Malnutrition
√
√
Fever
√
X
Bronchitis
√
X
Hypothermia
X
√
Rickets
√
X
Duration of stay of neonatal in-patients between the age of 29 days and 12 months
It is observed that 29 days – 12 month old neonatal in-patients stay between 12 hours
to 3 days generally in both private and government Hospitals. Some critical neonatal
patients have stayed up to 16 days in some private hospital. (Ratan, 2010)
Length of stay (LoS) of 29 days – 12 Months old children (IPD) per month
Minimum LoS
Maximum LoS
12 Hours
3 Days
Hospitalisation costs of 29 days – 12 month old neonatal in-patients in private
hospital
The average hospital bill in a private hospital is INR 100-500 per day while INR 100 500 is spent on medicines and INR 150-500 on diagnostics for the in-patient. (Ratan,
2010)
Hospitalisation cost for 29 days-12 month
old neonatal in-patient in private hospital
Terms of expenses
Average Amount
(INR/day)
Hospital Bill
100-150
Medicine cost
100-500
Diagnostics cost
150-500
4.2 Jehanabad
4.2.1 Introduction
Jehanabad is located at the confluence of two small rivers called Dardha and Yamunaiya. It is
the heartland of Magadh and the local dialect is called Magahi. The area is developing now
and the services sector is gaining ground in the district. Jehanabad town is the administrative
headquarter of this district. This district is a part of Magadh division and is only 45 km from
Patna, the state capital. The decadal growth rate for the year 1991-01 was estimated to be
67
NIPI Reference Book-Bihar
28.6 percent, which is more or less the same as the state growth rate. The sex-ratio of the
district is recorded at 928 females per 1000 male population. The percentage of SC & ST
population stands at 18.4 percent and 0.02 percent respectively, which is much lower than
other districts of Bihar. A marked disparity is noted between male and female literacy rates,
the latter being only 40.1 percent compared to the former (70.9 percent). (Bihar_NIPI, 2009)
Table 27: Statistical Profile (based on 2001 census) (Jehanabad_DHP, 2009)
Sl.
No.
Population
1.
Bihar
2.
Male
Female
Total
43153964
39724832
82878796
Jehanabad
480518
443959
924477
3.
Rural Population
420777
391807
812584
4.
Urban Population
59741
52152
111893
5.
Literacy rate
70.29%
40.43%
55.91%
6.
Rural
69.03%
37.94%
53.99%
7.
Urban
78.83%
58.62%
68.42%
History: Description of Jehanabad and its history is found in the famous book "AINA-EAKBARY" wrote by Abul Fazal. The book states that in the 17th century Jehanabad was
badly affected by famine and people were dying of hunger. Moghul emperor Aurangzeb, in
whose times the book was re-written established a "Mandi" for relief of the people and
named it ’JEHANABAD’. (Aggrawal, 2010)
Jehanabad district was carved out of the old GAYA district on August 1, 1986. Earlier it was
a subdivision of Gaya since 1872. It is situated 56 km to the south of the state headquarters,
Patna and 47 km to the north of Gaya by road and is well connected to both the stations via
an electrified rail-route as well. In the year 2001, the district of Arwal was created out of the
district of Jehanabad. (Aggrawal, 2010)
Table 28: Other Important data :- (Jehanabad_DHP, 2009)
1.
Area (in Sq. km.)
941.4 sq.km
2.
Decadal growth rate
28.64%
(1991 to 2001)
3.
Population Density
963 PPSK (Person per sq.km)
4.
Sex Ratio
928 (per 1000 male)
5.
Villages
Populate
- 562
Uninhabited - 43
Total - 605
68
NIPI Reference Book-Bihar
6.
Town
Municipality
02
7.
8.
Rural Families
144199
9.
SC Population
124856
10.
Cultivator
1.40 Lacs
11.
Small and Marginal Farmers
92138
12.
Agriculture Labours
1.78 Lacs
13
Skilled labours/ artisan
7967
14.
House hold Cortege Workers
12661
15.
Other Workers
59716
16.
Net Area under Cultivation
78000 Hec.
17.
Gross Cropped Area
260735.46 acr.
18.
Net Irrigated Area
66450 Hec.
19.
Area under Forest
1030 Hec. (0.41%)
20.
Water Area Fishery
1176..46 Hec.
21.
Total Cattle
2.04 Lacs (1982)
02
Geography: The district covers 941.4 sq. km. of geographical area in South Bihar. The town
of Jehanabad, which is the HQ of the district, is situated at the confluence of rivers Dardha
and Jamuna. Lying between 25-0 to 25-15 degree north latitude and 84-13 to 85-15 degree
eastern longitudes, the district is bounded by districts of Patna in the north, Gaya in the south,
Nalanda in the east and Arwal in the west. (Aggrawal, 2010)
Administration: There is one subdivision - Jehanabad and seven blocks in the district Jehanabad, Kako, Makhdumpur, Ghosi, Ratni Faridpur, Hulasganj and Modanganj. There are
93 Gram Panchayats, seven Panchayat Samities and one Zila Parishad in this district. One
Nagar Panchayat is at Makhdumpur and one Nagar Parishad at Jehanabad, M.P.
constituency - 01, MLA constituency - 3 (Jehanabad_DHP, 2009)
Socio-Economic: The relatively small sized district is a cauldron of conflict as far as the
socioeconomic situation is concerned. There were extreme caste tensions (with an economic
bearing) prevailing in the whole Magadha area (old Gaya district - now broken into 5 districts
of Gaya, Aurangabad, Nawada, Jehanabad and Arwal) and they were manifested in their
worst forms in this district. Thus this place has been badly affected by Naxalism (PWG,
MCC, ML (Lib) etc.) and has seen the emergence of rival outfits such as Ranvir Sena. As a
result this district has witnessed a horrifying spate of large scale carnages in the past which
has resulted in the killing of hundreds of innocent people. Nonhi-Nagwan, Parasbigha,
69
NIPI Reference Book-Bihar
Khagari-Damuha,
Laxmanpur-Baathe,
Rampur-Chauram,
Senari,
Shankarbigha
and
Narainpur - there are numerous villages where big massacres have occurred. (Aggrawal,
2010)
4.2.2 Health System
Janani Suraksha Yojana (JSY):
JSY is the prime strategy in the NRHM with the objective to increase the institutional
deliveries so that the reduction in MMR objective is achieved. The scheme comprises of
payments to the beneficiary and ASHA for food, transportation and motivation. During the
current year the performance and outcome of JSY has been quite encouraging. This scheme
has significantly increased the incidence of institutional deliveries in the district and the same
time, it has also increased the public’s faith in public health facilities. The district had
achieved 120 percent of JSY’s target. In the year 2009-10 a total of 20520 deliveries were
carried out in all PHCs. For the F.Y.2010-11 the district has proposed 18550 deliveries to
improve institutional deliveries in rural areas. (Aggrawal, 2010)
JSY payments were up-to-date in almost all the facilities that were visited. But in few
facilities the payment has not been made due to unreleased funds. All the beneficiaries were
issued cheques at the time of discharge. (Aggrawal, 2010)
Table 29: Health Indicators
Indicator
CBR
Jehanabad
28.6
Bihar
29.2
India
23.8
CDR
8.1
8.1
6
IMR
62
61
58
MMR
371
371
301
TFR
4.6
4
2.68
CPR
Complete
Immunization
33
34.1
56.3
47.2
32.8
44
Sources: DLHS3, NFHS3, SRS2007 (Jehanabad_DHP, 2009)
70
NIPI Reference Book-Bihar
Figure 5 Jehanabad District
Table 30 MCH Indicators in Jehanabad district
INDICATORS
MATERNAL HEALTH
Mothers registered in the first trimester
when they were pregnant with last live
birth/still birth (%)
Mothers who had at least 3 Antenatal care
visits during the last pregnancy (%)
Mothers who got at least one TT injection
when they were pregnant with their last
live birth / still birth (%)
Institutional births (%)
Delivery at home assisted by a
doctor/nurse /LHV/ANM (%)
Mothers who received post natal care
within 48 hours of delivery of their last
child (%)
CHILD IMMUNIZATION AND
VITAMIN A SUPPLEMENTATION
Children (12-23 months) fully immunized
(BCG, 3 doses each of DPT, and Polio
and Measles) (%)
Children (12-23 months) who have
received BCG (%)
NIPI
BASELINE
(2008 - 09)
Total
Rural
DLHS-2 (2002
- 04)
DLHS-3 (2007 08)
Total
Rural
Total
Rural
-
-
26.7
27
36
35.60%
18.7
18.3
30.6
31.2
39.6
39.2
30
29.3
54.5
54.4
98.6*
98.5
31.4
30.2
42.5
43
66.1
66.2
11.9
12
10.6
10.3
31.6
30.4
-
-
31
31.5
39
39
14.1
14
47.2
46.3
51
50.7
36.8
36.8
85.4
87.2
98.7
98.6
71
NIPI Reference Book-Bihar
Children (12-23 months) who have
received 3 doses of Polio Vaccine (%)
Children (12-23 months) who have
received 3 doses of DPT Vaccine (%)
Children (12-23 months) who have
received Measles Vaccine (%)
Children (9-35 months) who have
received at least one dose of Vitamin A
(%)
Children (above 21 months) who have
received three doses of Vitamin A (%)
21.5
21.3
48.7
49.9
73.1
72.9
26.1
27.2
55.1
56.4
71.1
71.5
19.4
19.9
63.9
65
63.6
63.5
-
-
66
66.9
41.2
41
-
-
9.2
9.9
13.7
15.6
0
0
13.6
13.4
34.8
34.8
100
100
74.7
77.7
56.5
56.5
-
-
72.6
72.5
77.1
76.5
-
-
29.8
30
10.4
10.7
-
-
31
31.8
17.2
17.7
-
-
18.6
19.1
20.2
20.5
-
-
10.9
11.4
28.4
25.7
-
-
84.5
84
41.4
39.7
TREATMENT OF CHILDHOOD
DISEASES (Children under 3 years,
based on last two surviving children)
Children with Diarrhoea in the last two
weeks who received ORS (%)
Children with Diarrhoea in the last two
weeks who were given treatment (%)
Children with acute respiratory
infection/fever in the last two weeks who
were given treatment (%)
Children had check-up within 24 hours
after delivery (based on last live birth)
(%)
Children had check-up within 10 days
after delivery (based on last live birth)
(%)
CHILD FEEDING PRACTICES
(Children under 3 years)
Children breastfed within one hour of
birth (%)
Children (age 6 months above)
exclusively breastfed (%)
Children (6-24 months) who received
solid or semisolid food and still being
breastfed (%).
4.2.3 Health Infrastructure
There are 120 Health Sub Centers (HSCs) in the district, of which only 81 HSCs are
functional. However most of them do not have their own building with adequate facilities.
Most facilities also face a shortage of staff due to which they were unable to provide the
services. In some FRUs, BPHCs and APHCs C-section was not conducted due to lack of
specialists. (Aggrawal, 2010)
A total of 52 of the 80 HSCs are being run without their own buildings in private
accommodations which are unfit for an HSC, to say the least. (Jehanabad_NIC)
72
NIPI Reference Book-Bihar
Figure 6: Health Facility in Jehanabad
Source: (Aggrawal, 2010)
73
NIPI Reference Book-Bihar
Table 31: Health Infrastructure
Type of Hospital
No. of
Hospital
No. of
Beds
No. of
Doctors
Sanctioned
No.
of Doctors
working
Sadar Hospital
1
95
13
13
Referral Hospital
2
60
09
4
07
28
24
168
25
56
11
33
81
-
-
-
Block P.H.C
Adi. P.H.C
Health Sub
Centre
(Jehanabad_NIC)
Name of DISTRICT : Jehanabad (Jehanabad_DHP, 2009)
Month's
OPD
Inpatients
No. of
Delivery
Referred
Case
No of
Emergency
Immunization
Mother
Child
Pulse
Polio
7810
198
204
0
742
797
2995
0.00%
May-05
8984
172
179
0
390
1233
6121
0.00%
Jun-05
9905
193
162
0
408
804
3417
0.00%
Jul-05
11273
186
215
0
544
816
3298
0.00%
Aug-05
11957
425
305
0
807
794
3557
0.00%
Sep-05
12156
221
304
0
482
810
3806
0.00%
Oct-05
10856
214
260
0
496
758
3703
0.00%
Nov-05
10379
203
244
0
420
791
4334
0.00%
Dec-05
10363
286
159
0
511
788
4982
0.00%
Jan-06
9137
402
182
0
616
609
3947
0.00%
Feb-06
8893
669
159
0
731
735
5556
0.00%
Mar-06
9054
349
148
0
731
858
5741
0.00%
TOTAL'0506
120767
3518
2521
0
6878
9793
51457
Apr-06
8067
190
151
0
623
944
5638
0.00%
May-06
9632
203
181
0
946
1141
5562
0.00%
Jun-06
10677
242
189
0
1071
1182
5220
0.00%
Jul-06
20048
331
269
0
1704
1484
5140
0.00%
Aug-06
22603
445
281
0
1347
1294
4917
0.00%
Sep-06
24237
386
327
0
1216
806
4863
0.00%
Oct-06
21345
356
303
0
1246
675
4620
0.00%
Nov-06
18749
484
306
0
965
900
6867
0.00%
Dec-06
17370
457
301
0
988
1295
16819
0.00%
Jan-07
15910
521
265
0
1070
995
11101
0.00%
Feb-07
16955
808
230
0
789
1271
13445
0.00%
Mar-07
19704
634
251
0
1223
1466
10093
0.00%
74
NIPI Reference Book-Bihar
TOTAL'0607
205297
5057
3054
0
13188
13453
94285
21738
335
299
35
1278
1993
13247
1.50%
May-07
24349
653
465
158
1737
1883
6375
0.92%
Jun-07
28739
1133
508
233
1559
4046
14052
0.00%
Jul-07
38093
1403
715
235
1723
3966
10872
1.26%
Aug-07
40130
2055
1171
221
2283
4502
15340
1.21%
Sep-07
38828
2768
1551
210
2126
3807
17183
1.00%
Oct-07
40869
3389
1967
168
2690
3168
17838
1.00%
Nov-07
38505
3512
1932
154
2336
2711
17628
0.00%
Dec-07
33522
3587
1711
156
2112
2497
17082
0.91%
Jan-08
35443
3495
1399
107
1990
2572
18572
0.99%
Feb-08
33193
3015
1202
94
1852
2889
21955
1.13%
Mar-08
29771
3240
1065
148
2030
2743
19330
1.33%
TOTAL
'07-08
403180
28585
13985
1919
23716
36777
189474
Apr-08
26667
2818
900
153
2206
1452
16298
1.13%
May-08
35413
3014
864
164
2391
2470
17900
0.00%
Jun-08
36989
2626
864
149
2284
4173
14901
0.95%
Jul-08
43654
3417
1200
157
2594
4209
13055
1.04%
Aug-08
48658
4568
1691
240
3001
4955
11801
1.04%
Sep-08
54762
5114
2131
193
3171
3889
12358
0.81%
Oct-08
43669
5857
2563
185
3315
3064
17165
0.81%
Nov-08
41295
5108
2343
169
2799
2732
15922
0.78%
Dec-08
41527
5401
2232
156
2671
2848
17712
1.14%
TOTAL
'08-09
372634
37923
14788
1566
24432
29792
137112
Total
1101878
75083
34348
3485
68214
89815
472328
(Jehanabad_DHP, 2009)
Table 32: Final Budget of Jehanabad
Sl. Budget
No
Head
1
TB
2
Kala azar
3
Leprosy
4
Filariasis
5
Blindness
6
Child Health
7
Maternal Health
8
Family Planning
9
Institution
Strengthening
Total
(Jehanabad_DHP, 2009)
%
0.44%
2.43%
0.56%
0.22%
1.55%
3.90%
70.51%
17.45%
2.93%
Total Budget
962000
5366460
1245000
496000
3424000
8603648
155552750
38494000
6453000
220596858
75
NIPI Reference Book-Bihar
4.2.4 Jehanabad Facility Survey Findings
The study done by A N Sinha Institute of Social Sciences for Access Health International in
September 2010 was an attempt to provide insights into the infrastructure available and
current capacity of both Governments, corporate and private health services providers of
Jehanabad district in neonatal and infant care.
Number of deliveries conducted in the health facility
People prefer government hospitals to private hospitals or nursing homes due to the
Janani Bal Suraksha Yojana (JBSY). The average number of deliveries per month is
275 in government hospitals while only 16 deliveries occur in private nursing homes
or private hospitals. (Ratan, 2010)
Average number of deliveries per month
Private Nursing Home/ Private Hospital
Govt. Hospital
16
275
Neonate Outpatients attended
There are more neonate consultations (about 83/ month) in private nursing home as
against only 17 neonates consult the doctor at the government hospital during an
illness. (Ratan, 2010)
Average number of Neonates Attended (OPD) per month
Private Nursing Home/ Private Hospital
Govt. Hospital
83
17
Infant Outpatients attended
180 infants consult the doctor at a private nursing home per month while 102 infants
consult the doctor at the government hospital every month for the treatment of their
illness. (Ratan, 2010)
Average number of infants Attended (OPD) per month
Private Nursing Home/ Private Hospital
Govt. Hospital
180
102
76
NIPI Reference Book-Bihar
Consultation Charges for Outpatients
Private nursing homes charge an average of INR 55 for an outpatient consultation for
15 days to one month. On the other hand, government hospitals charge a nominal fee
of INR 1 or 2 towards registration for an outpatient consultation in which medicines,
diagnosis and treatment are provided. (Ratan, 2010)
Normal Charges for Outpatient Consultation (INR)
Private Nursing Home/ Private Hospital
Govt. Hospital
1-2
(Only Registration Charges)
55
Distance covered by patients
Generally 0-1 year old patients travel about 35 kms to consult the doctor in a private
nursing home or private hospital. Patients seeking treatment in a government hospital
travel a distance of 13 kms to consult the doctor there. (Ratan, 2010)
Distance travelled by 0-1 year old patient to consult the doctor
Private Nursing Home/ Private Hospital
Govt. Hospital
35 Kms.
13 Kms.
Common ailments of below one year old out patient
Fever, meningitis, jaundice, loose motion, sepsis, cold and cough, diarrhoea,
dehydration, pneumonia, RTI / ARI, bronchitis etc. are some of the common ailments
in 0-1 year old outpatients who go to a private hospital for treatment. On the other
hand fever, loose Motion, cold & cough, diarrhoea, pneumonia, RTI and bronchitis,
etc. are found in out-patients who get treated at the government hospital. (Ratan,
2010)
Private nursing home/
Private hospital
Govt. hospital
Fever
√
√
Paralysis
√
X
Meningitis
√
X
Jaundice
√
X
Common Ailments
77
NIPI Reference Book-Bihar
Loose Motion
√
√
Sepsis
√
X
Cold and Cough
√
√
Diarrhoea
√
√
Dehydration
√
X
Pneumonia
√
√
RTI/ ARI
√
√
Bronchitis
X
√
Number of Neonate in-patients
It is found that average number of neonates who are provided in-patient treatment for
complications at birth is 83 per month at private hospitals/ nursing homes and 18 at
the government hospital in Jehanabad district. (Ratan, 2010)
Number of Neonates inpatient per month
Private Nursing Home/ Private Hospital
83
Govt. Hospital
18
Common complications of Neonate In-patients
Common neonatal complications seen in in-patients are birth asphyxia, jaundice,
hypothermia and sepsis. Neonate in-patients in government hospitals are seen with
complications of RTI, LBW, meningitis and diarrhoea. (Ratan, 2010)
Name of common neonatal complications of Inpatient
Birth Asphyxia
Private nursing home/
Private hospital
√
Govt. hospital
√
Jaundice
√
√
Hypothermia
√
√
Sepsis
√
√
RTI
√
X
LBW
√
X
Meningitis
√
X
Diarrhoea
√
X
Blood Exchange
√
X
78
NIPI Reference Book-Bihar
Duration of stay of Neonate In-patients
Due to the lack of facilities in government hospitals to treat complications, neonate inpatients generally stay only for one or two days. However there are some private
hospitals in this district that have paediatricians and equipment and therefore allow
neonate in-patients to stay for about three to seven days. (Ratan, 2010)
Length of stay of neonates inpatient
Private Nursing Home/ Private Hospital
Govt. Hospital
3-7 days
24 hrs-2 days
Hospitalisation Cost of Neonate In-patients
The hospital bill and medicine cost for neonate in-patients amounts to INR 500 and
INR 270 per day respectively and diagnostics costs above INR 250 (Ratan, 2010)
Hospitalisation cost of neonate in-patient in
private hospital
Terms of expenses
Average Amount
(INR./day)
Hospital Bill
500
Medicine cost
270
Diagnostics cost
250
Number of 29 days – 12 months old in-patients
The number of in-patients in the age group of 29 to 12 months old neonate in-patients
at 68 is about 3 times more in the government hospital than the 23 patients who visit
private hospitals. (Ratan, 2010)
Number of 29 days-12 month inpatient per month
Private Nursing Home/ Private Hospital
23
Govt. Hospital
68
Common complication of 29 days-12 months old children inpatients
The common complications among neonate in-patients 29 days – 12 months old are
diarrhoea, hypothermia, jaundice, pneumonia, loose motion, fever, cold & cough, RTI
in both private & government hospitals while the cases of LBW, paralysis and snake
biting are seen only in private hospitals. (Ratan, 2010)
79
NIPI Reference Book-Bihar
Name of common complication in 29 days - 12 months old children out patients.
Private Hospital
Nursing Home
Govt. Hospital
Diarrhoea
√
√
Hypothermia
√
X
Jaundice
√
√
Pneumonia
√
√
Loose Motion
√
√
Cold & Cough
√
√
RTI
√
√
Dehydration
X
√
LBW
√
X
Paralysis
√
X
Snake Biting
√
X
Duration of stay of neonate in-patients of the age group 29 days – 12 months
It is observed those 29 days – 12 month old neonate in-patients stay for 12 hours to 5
days in private hospitals or in government hospital. The duration of the stay usually
depends upon the condition and complication of patient. (Ratan, 2010)
Duration of stay of 29 days-12 month inpatient
Private Nursing Home/ Private Hospital
Govt. Hospital
12 hours
5 days
5.16 Hospitalisation Costs for Infant in-patients in Private Hospital.
The daily expenses for care of infant in-patients at a private hospital or nursing home
is approximately INR 100-150 while INR 300 is spent on medicine and INR 185 on
diagnostics (Ratan, 2010)
Hospitalisation cost of Infant in-patients in
private hospital
Terms of expenses
Average Amount
(INR /day)
Hospital Bill
100-150
Medicine cost
300
Diagnostics cost
185
80
NIPI Reference Book-Bihar
4.3 Sheikhpura
4.3.1 Introduction
Sheikhpura district is spread over an area of 689 sq.km. Its headquarters is Sheikhpura. The
district is divided into six blocks namely Ariari, Sheikhpura, Barbigha, Ghatkusumbo,
Chebara and Shekhopur Sarai. Paddy, wheat and lentils are the main crops. The Ganges,
Mohane, Harohar and Kiul are the important rivers that pass through the districts. The
population of the district is a little over five lakhs, with a decadal growth rate for the year
1991-01 being 25.0 percent. The sex-ratio of the district is recorded at 920 females per 1000
male population. The percentage of SC & ST population stands at 19.7 percent and 0.04
percent respectively, which is much less compared to the other districts of Bihar. A marked
disparity is noted between male and female literacy rates, the latter being only 34.1 percent
compared to the former (62.6 percent). (Bihar_NIPI, 2009)
Social: (Sheikhpura_DHP, 2009)
− Sheikhpura district has a strong hold of tradition with a high value placed on joint
family, kinship, caste and community.
− The villages of Sheikhpura have old social hierarchies and caste equations still shape
the local development. The society is feudal and caste ridden.
− 17.84 percent of the population belongs to SC and 0.1 percent to ST. There are at least
9 percent villages where the SC population is more than 40percent. Some of the most
backward communities are Mushahar, Turha, Mallah and Dome.
Area (Hectares)
77705
Population 2009 (Projected Figure)
Total
622177
Males
324054
Females
298126
Population of SC
111003
Population of ST
37
Population Density
762
Sex Ratio
920
(Sheikhpura_DHP, 2009)
Demographic scenario of Sheikhpura district (According to Census of India 2001):
(Sheikhpura_DHP, 2009)
81
NIPI Reference Book-Bihar
− The size of population of Sheikhpura district is above 622177, comprising 0.75
percent population of Bihar (Sheikhpura_DHP, 2009)
− The density of population is (762) which is still rising (Sheikhpura_DHP, 2009)
− Decadal population growth rate of 26.39 percent as against 28.43 percent of the state
as a whole. Thus the decadal growth rate of the district is slightly less than that of the
state. (Sheikhpura_DHP, 2009)
− The sex ratio of the population is 920 females per thousand males which is almost
same as the sex ratio of the state. It is difficult to interpret the deficit of 80 females per
thousand males in the district despite outward migration, predominantly of males in
the working ages. A plausible explanation seems to be that over the years male
population has benefited more from the epidemiological transition than the female
population. (Sheikhpura_DHP, 2009)
Basic Data
India
Bihar
Sheikhpura
Population
1027015247
82878796
525137
Density
324
880
762
Sex Ratio
933
921
920
Literacy (%)
Total
68.38
47.53
49.01
Male
75.85
60.32
66.16
Female
54.16
(Sheikhpura_DHP, 2009)
33.57
33.84
Economic: (Sheikhpura_DHP, 2009)
− The main occupation of the people of Sheikhpura is labour work in crushers
(stone works), agriculture, fisheries and daily wage labour.
− Almost 20 percent of the youth population migrates to the metropolitan cities like
Kolkata, Mumbai, and Delhi etc. in search of jobs.
− The main crops are wheat, paddy, pulses, and o oilseeds.
Villages
Total
310
Uninhabited
52
Inhabited
258
Gram Panchayat
54
Nagar Panchayat
2
Towns
2
82
NIPI Reference Book-Bihar
Blocks
6
Revenue Circles
6
Sub-Division
1
Police Station
9
Police Outposts
2
M.L.A. Constituency
(Sheikhpura_NIC)
2
Based on these statistics one can say that Sheikhpura district lacks urbanization and
industrialization. As elsewhere in Bihar, Sheikhpura suffers from lack of infrastructure
facilities, lack of connectivity, and lack of social development and most people depend on
small-size agricultural land. (Sheikhpura_DHP, 2009)
Figure 7 Sheikhpura District
(Sheikhpura_DHP, 2009)
Table 33 MCH Indicators in Sheikhpura district
INDICATORS
MATERNAL HEALTH
Mothers registered in the first trimester
when they were pregnant with last live
birth/still birth (%)
Mothers who had at least 3 Antenatal care
visits during the last pregnancy (%)
DLHS-2 (2002
- 04)
DLHS-3 (2007 08)
Total
Rural
Total
Rural
NIPI
BASELINE
(2008 - 09)
Total
Rural
-
-
42.9
43.4
51.3
48.6
22.2
21.1
43.2
43.4
40.7
39.5
83
NIPI Reference Book-Bihar
Mothers who got at least one TT injection
when they were pregnant with their last
live birth / still birth (%)
33.2
31.9
83.5
84.2
98.5
98.4
Institutional births (%)
21.2
18.8
41.6
41.3
60.5
59.3
9.2
7.8
5
4.2
8.2
7.8
-
-
44.1
45
36.8
28.8
19.1
20
38.3
41.3
55.6
55.4
50
50
74.5
73.2
95.1
95.1
25.5
27.4
48.3
49.8
70.2
69.6
26.7
31.3
49.2
50.9
72.9
72.8
27.4
30.2
49.3
50.7
67.6
65.8
-
-
49.3
51
42.7
41.3
-
-
8
9.2
19.2
14.7
67.4
61.7
24.5
25.8
25.9
25.8
79.1
75.4
80.2
82.9
76.3
83.1
-
-
76.2
77.5
93.1
93
-
-
39.4
40.2
18.1
17.2
-
-
41.3
42.3
24.4
23.7
-
-
10.5
11.5
10.6
11.4
-
-
12.5
12.9
29.9
26.8
-
-
82.5
82.5
58.4
57.5
Delivery at home assisted by a
doctor/nurse /LHV/ANM (%)
Mothers who received post natal care
within 48 hours of delivery of their last
child (%)
CHILD IMMUNIZATION AND
VITAMIN A SUPPLEMENTATION
Children (12-23 months) fully immunized
(BCG, 3 doses each of DPT, and Polio
and Measles) (%)
Children (12-23 months) who have
received BCG (%)
Children (12-23 months) who have
received 3 doses of Polio Vaccine (%)
Children (12-23 months) who have
received 3 doses of DPT Vaccine (%)
Children (12-23 months) who have
received Measles Vaccine (%)
Children (9-35 months) who have
received at least one dose of Vitamin A
(%)
Children (above 21 months) who have
received three doses of Vitamin A (%)
TREATMENT OF CHILDHOOD
DISEASES (Children under 3 years,
based on last two surviving children)
Children with Diarrhoea in the last two
weeks who received ORS (%)
Children with Diarrhoea in the last two
weeks who were given treatment (%)
Children with Acute Respiratory
Infection/fever in the last two weeks who
were given treatment (%)
Children had check-up within 24 hours
after delivery (based on last live birth)
(%)
Children had check-up within 10 days
after delivery (based on last live birth)
(%)
CHILD FEEDING PRACTICES
(Children under 3 years)
Children breastfed within one hour of
birth (%)
Children (age 6 months above)
exclusively breastfed (%)
Children (6-24 months) who received
solid or semisolid food and still being
breastfed (%).
84
NIPI Reference Book-Bihar
4.3.2 District health System
Government Administrative Set-up
There is one sub division and six blocks in the district. The district has 19 police stations and
54 gram panchayats. There are two railway police stations in Sheikhpura. Traditionally the
district was divided into three blocks but three more blocks were created during the last
decade. A few of the newly created blocks are still in the formation process. The newly
elected Panchayati Raj is enthusiastic to play important role in the district. (Sheikhpura_DHP,
2009)
4.3.3 Health Infrastructure
Table 34: Health Infrastructure
85
NIPI Reference Book-Bihar
Institution
Number
District Hospital
1
Referral Hospital
1
Primary Health Centre
Additional Primary Health
Centre
Health Sub Centre
6
Blood Bank
(Sheikhpura_DHP, 2009)
17
85
02 (in Process)
(Sheikhpura_DHP, 2009)
Table 35: Human Resource
Allopathic Doctor
86
NIPI Reference Book-Bihar
Regular
Contractual
33
17
Lady Doctor
Regular
Contractual
3
1
Pharmacist
Regular
Contractual
8
2
Lab Technician
Regular
Contractual
2
3
Health Educator
Regular
Contractual
13
0
ANM
Regular
Contractual
111
65
Staff Nurse
Regular
Contractual
4
27
Health Worker (Male)
Regular
1
(Sheikhpura_DHP, 2009)
Contractual
0
4.3.4 Sheikhpura Facility Survey Findings
The study done by A N Sinha Institute of Social Sciences for Access Health International in
September 2010 was an attempt to provide insights into the infrastructure available and
current capacity of both Governments, corporate and private health service providers of
Shiekhpura district in neonates and infant care.
Number of Deliveries
On an average 60 deliveries are performed in private hospitals and 290 in government
hospitals. (Ratan, 2010)
Average numbers of Deliveries
87
NIPI Reference Book-Bihar
Private Nursing Home/ Private Hospital
60
Govt. Hospital
290
Average Number of Neonates/ Outpatient Attended
Common people mostly preferred the government hospital for institutional deliveries
primarily because of the government JBSY scheme. JBSY provides medical treatment
and medicines free of cost. However the first choice for treating a neonate is a private
hospital or nursing home as against a government hospital. (Ratan, 2010)
Average number of Neonate Outpatients attended
Private Nursing Home/ Private Hospital
Govt. Hospital
91
60
Outpatient child (Infant attended)
An average 260 infant outpatients visit private hospitals or nursing homes for
treatment in a month while only 180 outpatients visit a government hospital for
treatment. (Ratan, 2010)
Average numbers of Infants Outpatient attended
Private Nursing Home/ Private Hospital
260
Govt. Hospital
180
Consultation Charges for Outpatients The minimum charge for outpatient
consultation in a private hospital or nursing home is INR 40 with a maximum of INR
100. Three visits are covered in one consultation charge. Most nursing homes and
private hospitals provide one month of consultation free. However one doctor charged
once every 15 days while another doctor charged for each visit. (Ratan, 2010)
Normal charge of Outpatient Consultation (INR)
Private Nursing Home/ Private Hospital
76
Govt. Hospital
1.25
Distance covered by patient
88
NIPI Reference Book-Bihar
A patient travels a distance of 23 kms to go to a private nursing home or hospital.
However the distance covered to visit a general hospital is a little less than 18 kms.
(Ratan, 2010)
Distance Travelled by Out Patients
Private Nursing Home/ Private Hospital
23 Km.
Govt. Hospital
18 Km.
Common neonatal ailments
Jaundice, cough & cold, feeding problem, loose motion, pneumonia, fever, diarrhoea,
RTI, sepsis and hypothermia are some of the common neonatal ailments in
Sheikhpura district. (Ratan, 2010)
In-patient care of neonates
Average neonates inpatients care
Private Nursing Home/ Private Hospital
120
Govt. Hospital
53
Neonatal Complications
Different kinds of neonatal complications are found like no crying by the neonate,
sepsis, birth asphyxia, dehydration, meningitis, hypothermia, Pneumonia, RTI, fever,
loose motion and jaundice. (Ratan, 2010)
Duration of stay of Neonate In-patients
Neonate in-patient care in a private hospital can involve a duration of 2-7 days in a
private hospital while in a government hospital the maximum length of stay is about
5 days. (Ratan, 2010)
Length of Stay
Private Nursing Home/ Private Hospital
2-7 days
Govt. Hospital
1-5 days
Hospitalization cost of neonates
89
NIPI Reference Book-Bihar
Neonate hospitalization costs an average of INR 200 per day in a private hospital or
nursing home. Sometimes the cost may even go up to INR 525 for a patient. On the
other hand it is free of cost in government hospitals. (Ratan, 2010)
Average Hospitalization cost
Private Nursing Home/ Private Hospital
Govt. Hospital
200
Free
Number of 29 days to 12months old neonates in in-patient care
An average of 132 neonate patients from different parts of the district visit private
nursing homes and hospitals and 160 patients visit government hospitals. (Ratan,
2010)
Average 29 days-12 months old children inpatient care
Private Nursing Home/ Private Hospital
Govt. Hospital
132
160
Common Complications (29 days to 12 months)
Some of the common complications experienced by neonates of the age group of 29
days to one year are diarrhoea, jaundice, pneumonia, vomiting, sepsis, dehydration,
fever, cold and cough and hypothermia of children. They usually get treated at a
private nursing home or hospital. Neonate patients who visit government hospitals
usually experience complications such as pneumonia, jaundice, LBW, fever, cough
and cold and RTI. (Ratan, 2010)
Common complications
Private Nursing Home/ Private Hospital
Diarrhoea, Jaundice. Pneumonia, Vomiting, Sepsis,
Dehydration, Fever, Cold &Cough and
Hypothermia
Govt. Hospital
Jaundice. Pneumonia, Vomiting,
Fever, Cold &Cough and Low
Birth Weight
Duration of stay (29 days to one year old children)
Neonate infants of the age 29 days to one year may stay for 1-7 days in private
hospitals or nursing homes. Neonates who visit government hospitals stay for 1-5
days for the same condition. (Ratan, 2010)
90
NIPI Reference Book-Bihar
Length of stay( 29 days-12 months old children)
Private Nursing Home/ Private Hospital
Govt. Hospital
1-7 days
1-5 Days
Hospitalization cost (29 days to one year old children)
The daily average hospitalization cost for a neonate inpatient at a private hospital or
nursing home is INR 580. On the other hand it is free of cost for a neonate in patient
at a government hospital. This also includes treatment, diagnostics and medicines that
are provided by the hospital. (Ratan, 2010)
Average Hospitalization cost (INR)
Private Nursing Home/ Private Hospital
580
Govt. Hospital
Free
91
NIPI Reference Book-Bihar
Chapter-5
Maternal & Child
health in NIPI’s focus
Districts
92
NIPI Reference Book-Bihar
5. Maternal and Child Health in NIPI’s focus districts
In this section, the data was collected for “NIPI Baseline Report of Bihar” from the three
NIPI focus Districts; Nalanda, Sheikhpura and Jehanabad and relevant information from
the state level. The districts were selected by NIPI in consultation with the state NRHM for
implementation of the interventions. (Bihar_NIPI, 2009)
5.1
Maternal Health
Maternal healthcare is a concept that encompasses family planning, pre-conception, prenatal,
and postnatal care. The goal of pre-conception care includes providing education, health
promotion, screening and interventions for women of reproductive age to reduce risk factors
that might affect future pregnancies. Antenatal care is the comprehensive care that women
receive and provide for themselves throughout their pregnancy. Women who begin prenatal
care early in their pregnancies have better birth outcomes than women who receive little
or no care during their pregnancies. Postnatal care issues include recovery from childbirth,
concerns about newborn care, nutrition, breastfeeding, and family planning. (Bihar_NIPI,
2009)
5.1.1 Delivery Care
One of the important thrusts of the program is to encourage deliveries under proper
hygienic conditions (delivering under clean conditions, washing hands with
disinfectant before delivery, etc.) and under the supervision of qualified/ experience
health professionals. For each live/still birth during two years preceding the survey,
we had asked the women on the place of delivery, who assisted during the deliveries
in case of home deliveries, characteristics of delivery and any problems that may
have occurred during the delivery process. This section provides the details.
(Bihar_NIPI, 2009)
According to NFHS reports, the percentage of women who have delivered in a health
facility has steadily increased in Bihar and overall in India. In Bihar, institutional
deliveries were only 14.8 percent in 1998-99 (NFHS 2), which has increased by nine
93
NIPI Reference Book-Bihar
percent in 2005-06 (NFHS3). Assistance of trained health personnel during delivery
is critical for maternal and child survival. A steady increase was also noted in the
number of pregnancies assisted by health personnel in both Bihar and India. When
compared to the all-India statistics, Bihar is still lagging behind in terms of both
institutional delivery and births assisted by health personnel. (Figure 4.3)
(Bihar_NIPI, 2009)
A recent DLHS3 reported institutional deliveries at 27.7 percent while NIPI Phase II
survey also clearly indicates that the trend has increased to nearly 40 percent of all
deliveries, which took place in government hospitals (61.6 percent in institutions),
while only 38.4 percent took place at home. (Bihar_NIPI, 2009)
Influence of background characteristics choice of place of delivery
The following section explores the relationship between the place of last delivery
and critical background variables, viz. age of respondent, her education level,
child’s birth order and standard of living level of her household based on Asset
Ownership Index. (Bihar_NIPI, 2009)
Nearly 40 percent women reported the place of delivery as a government health
facility while 21.4 percent women visited private health facility for delivery. Of the
total home deliveries, 23.6 percent took place at the in-laws’ home, 11.9 percent in
p arental home and nearly 2.5 percent took place in others’ homes. The preferences
of health facility for the delivery by the mothers do not have any relation with the
age of mothers. (Bihar_NIPI, 2009)
Table 36: Place of delivery v/s number of living children, NIPI-08
Institutional
Birth
Order
1-2
3-4
5+
Total
Govt
Hospital
N
%
755 39.2
534 41.5
253 40.3
1540 40.1
NGO
N
2
3
0
5
%
0.1
0.2
0
0.1
Home
Private
N
552
202
68
822
%
28.7
15.7
10.9
21.4
In-laws
N
348
340
218
906
%
18.1
26.4
34.9
23.6
Parental
N
226
166
64
456
%
11.7
12.9
10.2
11.9
Other
places
N
%
36
1.9
39
3
21
3.4
96
2.5
Other
N
9
3
3
15
%
0.5
0.2
0.5
0.4
Total All
Births
N
1927
1287
626
3840
%
100
100
100
100
94
NIPI Reference Book-Bihar
Data shows that deliveries in health facilities and a t home do not have any
relation with the education of the mothers while the preference for private
institutional delivery also increases with the education of the pregnant mother.
(Bihar_NIPI, 2009)
The hypothesis that younger women having their first child would rather have a
risk-free institutional delivery rather than have it at home while more experienced
women with children can afford to think otherwise is more or less validated in
the above table. Institutional deliveries come down from 67 percent for women with
1-2 live children to 55.4 percent for those who had more than two children.
(Bihar_NIPI, 2009)
Table 37: Place of delivery v/s economic status of respondents’ household, NIPI-08
Institutional
Delivery at
Govt
place(Public)
Home
Total
Other
NGO
Private
In-laws
Parental
Home
Others
All Births
Wealth
Index
N
%
N
%
N
%
N
%
N
%
N
%
N
%
N
%
Lowest
841
41
1
0
307
15.1
562
27.6
262
13
55
2.7
6
0.3
2034
100
Second
243
44
1
0.2
104
18.7
116
20.9
67
12
18
3.2
6
1.1
555
100
Third
172
38
0
0
124
27.3
94
20.7
51
11
11
2.4
2
0.4
454
100
Fourth
150
36
1
0.2
131
31.5
81
19.5
47
11
5
1.2
1
0.2
416
100
Highest
134
35
2
0.5
156
40.9
53
13.9
29
7.6
7
1.8
0
0
381
100
Total
1540
40
5
0.1
822
21.4
906
23.6
456
12
96
2.5
15
0.4
3840
100
The generic trend was that women with lower economic profile tended to favour
having deliveries at government facilities as against those who belonged to wealthier
households and could afford private treatment. (Bihar_NIPI, 2009)
Arrangement and cost of transport
In more than 70 percent cases, family members, relatives and friends made the
arrangement for transport. Husbands also played an important role in arranging
transport particularly in urban areas for delivery. A significant number of ASHA‟s
95
NIPI Reference Book-Bihar
made arrangement for transport in rural areas of Sheikhpura (18.3 percent), and
Jehanabad (8.4 percent). On an average, the cost of transport worked out to be as
follows: (Bihar_NIPI, 2009)
Table 38: Average transportation expenses (in Rupees), NIPI-08
Jehanabad
N
Mean
Nalanda
Sheikhpura
Total
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
N
789
213
N
44
171
N
833
207
N
648
187
N
117
155
N
765
173
N
635
250
N
134
186
N
769
235
N
2072
217
N
295
169
N
2367
206
On an average, the cost incurred on transportation is less than INR 300 in all the
districts. In urban areas average cost of transportation varies from INR 155 to INR
186 while in rural areas it varies from INR187 to INR 250 in the study districts.
(Bihar_NIPI, 2009)
5.1.2. Institutional delivery
This section elaborates on issues dealing with the nature of delivery and
attending
service provider, incurred costs, health problems/complications
experienced during delivery, nature of advice received post delivery and from
whom, and finally, opinion on quality of service and facility standards.
(Bihar_NIPI, 2009)
Table 39: Nature of Institutional delivery, NIPI-08
Rura
l
Jehanabad
Urba Tota
n
l
Rura
l
Nalanda
Urba Tota
n
l
Rura
l
Sheikhpura
Urba Tota
n
l
Rura
l
BIHAR
Urba
Total
n
Who
conducted
the delivery
Governmen
t Doctor
Private
Doctor
ANM
%
%
N
%
%
N
%
%
N
%
%
N
15.6
17.6
15.2
13.6
13.9
14.1
15.9
15
15.7
15.1
15.2
15
23.2
27.5
24
17.4
19.7
18.7
11.8
15.5
12.5
17.9
20.4
18.5
60.8
54.2
60.4
68.5
65.6
66.7
71.8
69.5
71.4
66.6
63.9
66
Other
0.4
0.7
0.4
0.5
0.8
0.5
0.5
0
0.4
0.4
0.5
0.4
76.5
79.5
85.6
81.1
84.2
89.6
83.4
88.3
84.6
80.7
83.9
Type of Delivery
Normal
79.7
Caesarean
12.5
17
13
9.9
10.7
10.6
7.1
12.3
8.5
10
12.8
10.7
Assisted
7.7
6.5
7.6
4.5
8.2
5.2
3.3
4.3
3.3
6.5
Total
789
44
833
648
117
765
635
134
769
5.4
2,07
2
5.4
2,36
7
295
96
NIPI Reference Book-Bihar
The above table clearly shows that the person actually performing the delivery was
primarily an ANM (66 percent) followed by private doctor (18.5 percent) and
government doctor (15 percent). The trend is similar across the districts and
locality. While most deliveries were normal, incidence of caesarean deliveries was
more in urban areas. Around 5 percent of the deliveries across both urban and rural
areas were assisted deliveries. (Bihar_NIPI, 2009)
Table 40: Cost incurred in institutional delivery1, NIPI-08
Jehanabad
Rupees
Nalanda
Sheikhpura
BIHAR
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
%
%
%
%
%
%
%
%
%
%
%
%
<500
5001000
1001-
12.2
6.8
11.9
12.8
10.3
12.4
18.9
19.4
19
14.4
13.9
14.4
45.4
54.5
45.9
47.1
37.6
45.6
50.2
40.3
48.5
47.4
41.4
46.6
9
6.8
8.9
8.2
1.7
7.2
6.5
4.5
6.1
8
3.7
7.4
1500
15012000
2001-
12
11.4
12
10
22.2
11.9
10.1
8.2
9.8
10.8
14.2
11.2
3.2
0
3
3.1
3.4
3.1
1.7
1.5
1.7
2.7
2
2.6
2500
25013000
3001-
2.9
9.1
3.2
2.9
5.1
3.3
2
6.7
2.9
2.7
6.4
3.1
2.4
2.3
2.4
1.9
3.4
2.1
2.2
4.5
2.6
2.2
3.7
2.4
4000
40015000
5001 +
3
2.3
3
2.9
5.1
3.3
2
2.2
2.1
2.7
3.4
2.8
9.9
6.8
9.7
11.1
11.1
11.1
6.3
12.7
7.4
9.2
11.2
9.4
Total
789
44
833
648
117
765
635
134
769
2072
295
2367
The survey also attempted to understand the cost incurred on institutional delivery
including transportation cost. More than half (52.6 percent) of the mothers spent
less than INR 500 on institutional delivery; another 42 percent mothers spent
INR 501 to 1000 and 5 percent mothers spent INR 1001-1500 on institutional
delivery. The data reveals that delivery expenses in rural areas are more than in
urban areas. (Bihar_NIPI, 2009)
Premature labour was one of the major problems experienced by almost 60 percent of
the women respondents who faced problems. This is consistent across all age groups.
Prolonged labour was another problem faced by a third of the respondents across all
age groups. (Bihar_NIPI, 2009)
97
NIPI Reference Book-Bihar
Table 41: Problem experienced during delivery by women of different age groups, NIPI-08
Institutional Delivery
Premature
labour
1518
1921
2225
2630
3140
4149
Excessive
bleeding
Prolonged
labour
Obstructe
d labour
Breech
presentation
Other
Total
N
%
N
%
N
%
N
%
N
%
N
%
N
56
69.1
11
13.6
31
38.3
10
12.3
3
3.7
2
2.5
81
262
57.8
56
12.4
176
38.9
95
21
22
4.9
25
5.5
453
478
57
89
10.6
320
38.1
169
20.1
42
5
39
4.6
839
425
62.1
64
9.4
233
34.1
124
18.1
47
6.9
25
3.7
684
163
56.4
26
9
86
29.8
48
16.6
8
2.8
10
3.5
289
13
61.9
2
9.5
7
33.3
4
19
0
0
0
0
21
Home Delivery
This section deals with the details of home delivery cases, including reasons behind
choosing to have the baby delivered at home and not in an institution, the actual
place where the delivery took place and whether it was influenced by the
background of the pregnant mother-to-be, the person who actually conducted the
delivery and finally, why this person was chosen to begin with. (Bihar_NIPI, 2009)
Table 42: Reason for home delivery, NIPI-08
Reason
(multiple
response)
Jehanabad
Rura Urba Tota
l
n
l
Nalanda
Rura Urba Tota
l
n
l
Sheikhpura
Rura Urba Tota
l
n
l
BIHAR
Rura Urba Tota
l
n
l
%
%
%
%
%
%
%
%
%
%
%
%
Costs too
much
15.5
9.7
14.8
19.6
16.2
18.9
18.7
18.1
18.5
18
14.8
17.6
Facility not
open
2.2
2.2
2.1
4.1
2
3.7
6
8.4
6.4
4.1
3.7
4.2
Too far/ No
transportation
11.5
6.5
10.8
25.8
17.6
23.2
18.9
8.4
17.5
19.1
12
17.6
Don't trust
facility/poor
quality service
3
1.1
2.8
2.3
10.1
4.7
3.7
6
4.2
3
6.5
4
No one to
accompany
19.7
20.4
19.3
26
21.6
24.7
15.2
14.5
14.9
20.5
19.4
19.8
Did not get
time/no time
32.7
37.6
32.5
28.1
24.3
27.3
32.8
26.5
31.1
31.1
28.7
30.1
1
2.2
0.9
0.9
0.7
0.9
0.9
2.4
1.2
0.9
1.5
1
No female
provider at
facility
98
NIPI Reference Book-Bihar
Husband/famil
y did not allow
12.7
14
13.2
7.9
8.1
8.4
5.8
6
6
8.7
9.3
9
Not necessary
25.9
20.4
25.9
24.9
24.3
25.6
28.9
36.1
30.5
26.6
26.2
27.4
Not customary
4.7
2.2
4.5
3
5.4
3.4
5.5
7.2
6
4.4
4.9
4.6
Other
7.7
15.1
7.8
4.3
4.1
3.9
6.9
8.4
6.8
6.2
8.3
Total
401
401
425
401
401
535
401
401
498
401
401
6
145
8
Out of 3843 women interviewed in three districts, 1458 (39 percent) women
delivered at home. In Nalanda, 41 percent mothers delivered at home followed by 39
percent in Sheikhpura and 34 percent in Jehanabad. (Bihar_NIPI, 2009)
As m e n t i o n e d above, nearly two-fifth of the total surveyed women delivered at
home. They were also asked the reasons why they did not deliver in the health
facility. 30 percent women mentioned they did not have time to go to health facility,
27 percent felt that delivery i n a n institution
is
not necessary, 18 percent
women cited non-availability of transportation facility and another 20 percent
reported nobody was there to accompany them for delivery as the main reason for
their deliveries at home. The most important reason emerging in all the districts for
not going to a health facility for delivery is the lack of time. Q ualitative
discussions have inferred that people generally did not prefer to go to health facility
if there was no serious problem or any complication to the pregnant woman. Non
availability of transportation also emerged as an important reason during the
qualitative discussions. (Bihar_NIPI, 2009)
Table 43: Reasons behind choosing a specific person to conduct the delivery, NIPI-08
Jehanabad
Delivery
Specification
Nalanda
Sheikhpura
BIHAR
R
U
T
R
U
T
R
U
T
R
U
T
%
%
%
%
%
%
%
%
%
%
%
%
Why did you choose the person to conduct delivery?
Past experience
28.9
20.4
28.9
21.1
23.6
22.1
58.7
48.2
58
36
29
36.4
Economical
13
11.8
12.2
15.1
4.7
13.6
0.9
2.4
1
9.7
6.2
8.9
Safe delivery
33.2
32.3
33.2
38.6
43.9
40
17.6
16.9
17.5
29.9
33.6
30.3
Reliability
Behaviour of
the service
provider
Recommended
9.7
10.8
9.2
4.5
4.7
4.9
8.8
14.5
8.8
7.5
9
7.5
1.5
6.5
2.4
14.9
17.6
14
2.3
2
6.6
9.9
6.5
10
11.8
10.4
4.5
3.4
4.1
9.7
16.9
10.7
7.9
9.3
8.2
Other
3.7
6.5
3.8
1.3
2
1.3
2.1
1.2
2
2.3
3.1
2.3
425
469
66
535
433
498
1303
155
1458
Total
401
24
65
99
NIPI Reference Book-Bihar
The reason for choosing a particular person to conduct delivery at home was also
asked. The two most important criteria for selection of the individual was her past
experience (36 percent) and past record of conducting safe deliveries (30 percent).
T h e Person being economical (9 percent) and recommended by somebody (8
percent) were the other reasons expressed for choosing the person to conduct home
delivery. (Table 4.32) (Bihar_NIPI, 2009)
Table 44: Cost incurred in home delivery, NIPI-08
Jehanabad
Amount (in
INR.)
Nalanda
Sheikhpura
BIHAR
R
U
T
R
U
T
R
U
T
R
U
T
%
%
%
%
%
%
%
%
%
%
%
%
< 500
39.3
40.7
37.9
36.1
32.2
35.6
55.2
57.5
55.1
43.6
41.1
43
500 - 1000
52.7
49.4
53.3
54.9
58.7
55.2
32.9
31.3
32.7
46.7
49
46.8
1001 - 1500
4
4.9
4.5
3.5
1.4
3.1
2.4
5
2.9
3.3
3.3
3.4
1501 - 2000
2.8
3.7
2.9
3.5
4.2
3.8
6.2
5
6.2
4.2
4.3
4.4
2001 - 2500
0.3
1.2
0.5
0.7
1.4
0.8
1.2
1
0.7
1
0.8
> 2500
0.9
0.8
1.3
2.1
1.5
2.1
1.3
2.1
1.5
1.3
1.5
Total
351
375
457
65
522
420
63
483
1228
152
1380
24
So far as the amount spent on home deliveries are concerned, 43 percent spent less
than INR500 and another 47 percent spent between INR500 – 1000. In Sheikhpura,
expenditure on most of the home deliveries (55 percent) was less than INR500
while in Jehanabad and Nalanda; it was between INR500- to INR1000 in more than
50 percent cases. (Bihar_NIPI, 2009)
5.1.3 Postnatal Care
The health of a mother and newborn child depends not only on the healthcare she
receives during her pregnancy and delivery, but also on the care she and the infant
receive during the first few weeks after delivery. Postnatal care check-ups soon after
the delivery are particularly important for births that take place in non-institutional
settings. (Bihar_NIPI, 2009)
A large proportion of maternal and neonatal deaths occur during the first 48 hours
after delivery. Hence safe motherhood programs have increasingly emphasized
the importance of postnatal care, recommending that all women receive a check
100
NIPI Reference Book-Bihar
up within the first two days of delivery. The World Health Organisation (WHO)
recognizes several “crucial moments when contact with the health system/informed
caregiver could be instrumental in identifying and responding to needs and
complications” (WHO, 1998). It is most important to have the first postnatal checkup within a few hours of delivery. Another important time for a postnatal check-up
is six weeks (42 days) after the delivery. By this time, a woman’s body should
generally have returned to its per-pregnancy state. To assess the extent of postnatal
care check-ups, women were asked whether any health personnel checked on her
health since her last delivery. (Bihar_NIPI, 2009)
Table 45: Timings of First Post Natal Care, NIPI-08
District
Jehanabad
<4 Hrs
4-23
Hrs
1-2
days
3-41
Days
>41
days
DK/CS
No
Checkup
Total
Nalanda
Sheikhpura
All Districts
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
Rural
Urban
Total
%
%
%
%
%
%
%
%
%
%
%
%
0.2
0.2
0.3
0.2
0
0.2
0.6
0.5
0.3
0.3
0.3
1
1.8
1.1
0.6
0.6
0.7
1.9
1.8
0.8
0.5
0.8
1.5
4.6
2
1.4
1.6
1.5
1.6
1.5
0.3
0.3
0.2
1.8
1.1
1.7
1.2
0.4
1.1
0
0
0
0.5
0.5
0.4
0.5
0.1
0.5
97.2
96.1
0.1
0.4
0.1
0.6
0.4
0.5
0.5
95.1
99.6
95.4
98.1
99
98.3
94.9
92.5
94.5
96
1,192
68
1,260
1,124
184
1,308
1,072
200
1,272
3,388
452
3,840
A majority of women (96 percent) did not receive any postnatal check-up after
their most recent birth within two months of delivery. Only 4 percent of women
received a health check-up within two months of delivery. (Bihar_NIPI, 2009)
Among the small number of mothers who received postnatal care, ANM/Nurse/
Midwife checked 57 percent mothers and doctors checked 33 percent mothers. About
one third (31 percent) of mothers attended a PHC for postnatal check up followed by
21 percent mothers who visited a private hospital/clinic and 20 percent who visited a
government hospital . Around 15 percent mothers received post partum care at home.
(Bihar_NIPI, 2009)
101
NIPI Reference Book-Bihar
Out of the total women who received PNC, 14 percent received PNC in the
government hospital, 27 percent in PHC and 18 percent received PNC at a private
hospital but they all delivered in the same health facilities. About 4 percent women
delivered in a private health facility but they received PNC in government hospital.
Another three percent women received first prenatal check-up in a PHC while they
delivered in a private hospital. In most of the cases women received PNC at the
same place where they delivered. There were some women who received PNC at a
government facility but delivered in private health institution, whil e a negligible
number of women received PNC in a private health facility after delivering in a
government institution. (Table in Annexure) (Bihar_NIPI, 2009)
5.2 Newborn Care
The majority of newborn problems are specific to the perinatal period. They result not
only in deaths but also high m o r b i d i t y and disability. These problems are the result of
poor maternal health, inadequate care during pregnancy, inappropriate management and
poor hygiene during delivery, lack of newborn care and discriminatory care. Death among
newborn infants is so frequent that it is accepted as routine by many families and community
members. If a mother dies during childbirth, her baby has smaller chance of survival.
However if the baby survives he/she is at high risk for neglect, malnutrition and morbidity.
Keeping this in view, the government has launched a nationwide program for the care of
pregnant women and newborns. (Bihar_NIPI, 2009)
The first check of the baby after delivery is very crucial for overall assessment,
exclusive breastfeeding and appropriate care. The study has collected information
regarding first health check-up, contact with care provider within ten days of birth and
vaccination within one month of birth for all babies either delivered at hospital or home.
(Bihar_NIPI, 2009)
The first health check-up of babies that took place within ten days of birth was reported to be
very low in Bihar. Nearly four-fifth (81 percent) of babies did not have contact with any
102
NIPI Reference Book-Bihar
health worker within the first 10 days of birth. Only 11 percent of babies had contact with
any health worker within the first 24 hours of birth. About 19 percent of babies had contact
with a health worker within the first 10 days after birth. The variation in these figures across
the three study districts was minimal. There was minimal variation between rural and
urban areas in this practice except for the urban area of Jehanabad district where little more
than 90 percent babies were not checked. (Table 5.3 & 5.4) (Bihar_NIPI, 2009)
Table 46: Timing of first neonatal check-up by Districts, NIPI-08
JEHANABAD
RURAL
NALANDA
SHEIKHPURA
URBAN
RURAL
URBAN
RURAL
URBAN
N
%
N
%
N
%
N
%
N
%
N
%
<6 Hrs
114
9.5
8
3.2
82
7.3
46
11.7
169
15.8
57
21
6-23 Hrs
14
1.2
2
0.8
11
1
6
1.5
15
1.4
3
1.1
1-2 Days
57
4.8
2
0.8
28
2.5
8
2
43
4
10
3.7
3-4 Day
19
1.6
2
0.8
15
1.3
14
3.6
11
1
5
1.8
5-6 Days
Week or
more
No Checkup
2
0.2
5
0.4
5
0.5
1
0.4
5
0.4
1
0.4
18
1.6
6
1.5
11
1
984
82.3
233
94
965
85.9
314
79.7
818
76.3
195
72
Total
1195
100
248
100
1124
100
394
100
1072
100
271
100
Sheikhpura district of Bihar proved to be the best performer among all the surveyed
districts where 28 percent neonates received check-up in urban areas while 24 percent in
rural areas. At the same time in other districts its ranges between 6-20 percent. (Bihar_NIPI,
2009)
5.2.1
Breastfeeding and Supplementation
Breastfeeding is one of the main pillars of newborn care. Educating mothers on
correct breast-feeding practices and child nutrition is a very important component of
newborn care. In this survey, we explored breastfeeding practices among the eligible
women, the attitude and practice of feeding pre-lacteal liquids, the period of
exclusive breastfeeding and introduction of supplementary feeding. (Bihar_NIPI,
2009)
103
NIPI Reference Book-Bihar
Initiation of breastfeeding immediately after birth is beneficial to both the infant as
well as the mother. More than 96 percent of women in Bihar had breastfed their
children. Little more than half of the mothers received help from somebody
in initiation of breastfeeding. A comparison on breastfeeding between rural and
urban women showed that rural women had received help in initiation of
breastfeeding as compared to urban women. (Bihar_NIPI, 2009)
Table 47: Breastfeeding practices, NIPI-08
JEHANABAD
NALANDA
SHEKIPURA
RURAL
URBAN
RURAL
URBAN
RURAL
URBAN
N
%
N
%
N
%
N
%
N
%
N
%
Yes
1158
96.9
243
98
1070
95.2
384
97.5
1029
96
262
96.7
No
37
3.1
5
2
54
4.8
10
2.5
43
4
9
3.3
1195
100
248
100
1124
100
394
100
1072
100
271
100
Ever breastfed
Anybody helped in initiating the breast feeding
Yes
720
62.2
131
53.9
605
56.5
174
45.3
437
42.5
79
30.2
No
438
37.8
112
46.1
465
43.5
210
54.7
592
57.5
183
69.8
1158
100
243
100
1070
100
384
100
1029
100
262
100
Sources helped in initiating breastfeed
Government
14
1.9
1
Doctor
Private Doctor
51
7.1
17
1.5
4
2.3
7
1.6
13
40
6.6
12
6.9
35
8
8
10.1
0.8
9
2
2.5
Nurse
77
10.7
13
9.9
81
13.4
19
10.9
67
15.3
16
20.3
ANM/ASHA/LHV
67
9.3
7
5.3
98
16.2
22
12.6
42
9.6
7
8.9
Dai
Mother/ Mother-inlaw
Friends/Relatives
62
8.6
19
14.5
47
7.8
14
8
49
11.2
9
11.4
341
47.4
52
39.7
204
33.7
71
40.8
182
41.6
27
34.2
104
14.4
22
16.8
126
20.8
32
18.4
52
11.9
10
12.7
3
0.7
131
100
605
100
174
100
437
100
79
100
Others
4
0.6
720
100
Around two-third o f mothers received support from untrained persons like mother,
mother-in-law and friends. Little more than one tenth of the mothers received
support from a nurse and similar proportion received it from an ANM/ASHA. The
role of government doctors in the initiation of breastfeeding was found to be
negligible with only two percent mothers having received help from them. A
r u r a l -urban analysis of the district showed almost similar results as that of the state.
(Table 48) (Bihar_NIPI, 2009)
104
NIPI Reference Book-Bihar
Eligible mothers from the survey stated that initiation of breastfeeding practices
has taken place within one hour of delivery and before completion of three days from
delivery. Around 13 percent women started breastfeeding the child within one hour of
delivery. (Bihar_NIPI, 2009)
In Bihar around 61 percent of women have delivered in health institutions. At
these health institutions the doctor/nurse/ANM attending to the delivery is expected
to advice women on initiation of breastfeeding soon after birth. However, in Bihar
the percentage of women who initiated breastfeeding within one hour of childbirth
is substantially less than the proportion of institutional deliveries, suggesting that
even in health institutions also early initiation of breastfeeding was not ensured.
(Bihar_NIPI, 2009)
An in-depth interview with ANMs, ASHAs and Anganwadi Workers revealed that
the customary practices for breastfeeding is prominent in the region but varies
from village to village. Although some of the ANMs revealed that they counsel
women on breastfeeding practices most of them were unable to do so due to lack of
time. ASHAs are more close to mothers than any other health workers in rural
areas and they counsel them on breastfeeding practices like give mother’s first
milk to the child, exclusive breast feeding up to six months, how the mother’s milk
enhances the immunity of the child etc. However a change in customary system
will take some time. (Bihar_NIPI, 2009)
There is no significant difference or impact of the gender of child on initiation of
breastfeeding. (Bihar_NIPI, 2009)
Table 48: Initiation of breastfeed and gender of child, NIPI-08
Immediately within
an hour of birth
Same day after an hour of
birth
1-3 days
After 3
days
%
%
%
%
Boy
11.9
35.9
45.2
6.2
Girl
14.3
34.4
44.3
5.8
Gender of child
105
NIPI Reference Book-Bihar
Table 49: Feeding of prelacteal liquids, NIPI-08
JEHANABAD
Rural
NALANDA
Urban
Rural
SHEIKHPURA
Urban
Rural
All Districts
Urban
Rural
Urban
N
%
N
%
N
%
N
%
N
%
N
%
N
%
N
%
Exclusively
breastfeed
13
2.3
3
3.2
16
3.3
5
2.6
15
2.6
2
1.1
44
2.7
10
2.2
Milk (other
than breast
milk)
368
65.5
54
58
349
72.7
135
69.2
458
79.7
148
85.1
1175
72.7
337
73
Plain water
Sugar or
glucose water
Sugar-saltwater
solution
Fruit juice
Infant
formula
Tea
78
13.9
5
5.4
30
6.3
12
6.2
19
3.3
9
5.2
127
7.9
26
5.6
58
10.3
10
11
45
9.4
37
19
20
3.5
9
5.2
123
7.6
56
12
2
0.4
2
2.2
2
0.4
1
0.2
5
0.3
2
0.4
2
0.4
1
1.1
16
3.3
18
1.1
1
0.2
1
0.2
1
0.1
3
0.5
1
1.1
2
0.3
1
0.6
5
0.3
2
0.4
Honey
3
0.5
4
4.3
10
1.7
1
0.6
13
0.8
5
1.1
2
0.3
5
0.3
Janam ghutti
Other
3
34
Total (N)
6
13
562
14
93
0.6
19
4
480
6
3.1
195
48
8.3
575
4
2.3
174
101
6.2
23
1617
462
In the table 49 we looked at the proportion of mothers who had exclusively
breastfed by background variables i.e. gender of the child, age and education of
mothers, number of live children, location of PSU and wealth index. For this
analysis, only mothers of children beyond 6 months of age were considered and all
mothers who were currently breastfeeding but had children who were younger were
not considered. (Bihar_NIPI, 2009)
The situation of exclusive breastfeeding practices is not very encouraging in Bihar.
Among the infants aged more than 6 months, around 27 percent of children
were exclusively breastfed up to 6 months after birth while the remaining mothers
(about 73 percent) discontinued exclusive breastfeeding within 6 months.
(Bihar_NIPI, 2009)
Exclusivity of breastfeeding was not influenced by educational status of women,
locality of residence of women, birth order of the child or economic status of the
family. But exclusive breastfeeding was highest (38.6 percent) among young
106
5
NIPI Reference Book-Bihar
mothers wi t hin t he age group of 15 to 18 years and lowest (16.7 percent)
among oldest mothers. In fact with regard to education of t he mother, economic
profile of the family and number of live children, there is no significant correlation
or trend between mothers residing in urban and rural areas. However urban mothers have
shown a lower proportion of discontinuation of exclusive breastfeeding before six
months of children’s age. (Bihar_NIPI, 2009)
In the table 5.10 we looked at the proportion of mothers who had exclusively
breastfed by background variables i.e. gender of the child, age and education of
mothers, number of live children, and location of PSU and wealth index. For this
analysis, only mothers of children beyond 6 months of age were considered and all
mothers who were currently breastfeeding but had children who were younger were
not considered. (Bihar_NIPI, 2009)
The situation of exclusive breastfeeding practices is not very encouraging in Bihar.
Among the infants aged more than 6 months, around 27 percent infants were
exclusively breastfed up to 6 months after birth while the remaining mothers (about
73 percent) discontinued exclusive breastfeeding within 6 months. (Bihar_NIPI,
2009)
Exclusivity of breastfeeding was not influenced by educational status of women,
locality of residence of women, birth order of the child or economic status of the
family. But exclusive breastfeeding is highest (38.6 percent) among young mothers
in the age group of 15 to 18 years and lowest (16.7 percent) among oldest mothers.
In fact, education of mother, economic profile of family and number of live children,
there seems to have no significant correlation or trend but mothers residing in
urban areas showed a lower proportion of discontinuation of exclusive breastfeeding
before six months of children’s age. (Bihar_NIPI, 2009)
Table 50: Period of exclusive breastfeeding by background variables, NIPI-08
Background variables
< 6 months
6 months and more months
Boys
908
73.9
320
26.1
Girls
813
72.2
313
27.8
107
NIPI Reference Book-Bihar
Total
1721
73.1
633
26.9
Age of the Respondent (in Years)
15-18
35
61.4
22
38.6
19-21
281
73.6
101
26.4
Background variables
< 6 months
6 months and more months
22-25
599
73.1
220
26.9
26-30
508
73
188
27
31-40
283
74.1
99
25.9
41-49
15
83.3
3
16.7
Total
1721
73.1
633
26.9
Years of schooling
1113
73.2
408
26.8
<5
No schooling
44
73.3
16
26.7
5-7
157
69.5
69
30.5
8-9
137
72.1
53
27.9
10-11
196
77.2
58
22.8
12 & Above
74
71.8
29
28.2
633
26.9
319
27.1
Total
1-2
1721
73.1
Number of Live Children
858
72.9
3-4
582
73.7
208
26.3
5+
281
72.6
106
27.4
Total
1721
73.1
633
26.9
Rural
1527
73.6
549
26.4
Urban
194
69.8
84
30.2
Total
1721
73.1
633
26.9
Location of PSU
Wealth Index
Lowest
909
73.9
321
26.1
Second
251
71.3
101
28.7
Middle
205
73
76
27
Fourth
186
73.8
66
26.2
Highest
170
71.1
69
28.9
Total
1721
73.1
633
26.9
5.2.2 Child Morbidity and Treatment
Diarrhoea and ARI have been identified globally as major threats to the survival of
children under the age of five years. This is also true for India, where these two
diseases have been the major causes behind infant mortality. Prevention as well as
108
NIPI Reference Book-Bihar
effective treatment of these diseases depends on a host of individual, household and
community level behavioural factors. One of the objectives of this study is to
estimate the role played by such factors in determining the utilisation of formal
healthcare to cure diarrhoea and certain respiratory illnesses plaguing newborns.
The Reproductive Child Health program includes components like treatment of
diarrhoea
and
ARI
and
health
education
to
mothers
on management of
d iarrhoea and danger signs of ARI. The paramedical and medical staff is trained to
diagnose the cases of pneumonia among the children and treat the cases of
pneumonia and diarrhoea.
All the gover nm ent healt h i nst i tut i ons are
supplied w i t h m edi ci nes necessary for the treatment of pneumonia and diarrhoea.
The major findings of the study are as follows: (Bihar_NIPI, 2009)
Prevalence of illness in children under study
The following section looks at the prevalence of child morbidity and to know about
about the incidence of diarrhoea and fever in children. . The survey involved asking
questions to the mothers on the incidence of these conditions in the two weeks prior to
the survey date. (Bihar_NIPI, 2009)
Table 51: Prevalence of illness in children under study, NIPI-08
Jehanabad
Indicator
Nalanda
Sheikhpura
Rural
Urban
Rural
Urban
Rural
Urban
%
%
%
%
%
%
1.9
1.2
All NIPI Districts
Rural
N
%
Urban
Total
N
%
N
%
47
5.1
175
4.6
112
12.3
443
11.5
% of children with diarrhoea in last two weeks
Yes
5.9
6.1
6.1
7.4
154
4.5
% of children with fever in last two weeks
Yes
6.8
4.8
17.6
19
10.6
9.2
393
11.6
Table 52 shows that around 4.6 percent of children were suffering from diarrhoea
and it is lowest among the children of Jehanabad (1.9 percent for rural and 1.2 for
urban). About 12 percent of children were suffering from fever also and again
Jehanabad secured lowest proportion of children with fever (6.8 percent for rural
and 4.8 percent for urban areas). At the state level there is no significant difference
109
NIPI Reference Book-Bihar
in the prevalence of diarrhoea and fever but both are more in urban areas than in rural
areas. (Bihar_NIPI, 2009)
As per NFHS-3 estimates, in Bihar 6.8 percent of children had ARI in past two
weeks prior to the survey while the national average was 5.8 percent. After NFHS-1
prevalence of diarrhoea in Bihar reduced (17.7 percent) from the national average of
19.2 percent while for NFHS-3 the data in not available. (Bihar_NIPI, 2009)
5.2.3 Summary Observation
Incidence of weighing a baby after birth is reported to be very rare in Bihar. T h e
p r i m a r y r eason for this was revealed from Focus Group Discussion with ANM
and in-depth interview w with ANMs, ASHAs and Anganwadi Workers where
they stated that most of them were not equipped with a proper weighing
machine for weight measurement of the newborn. (Bihar_NIPI, 2009)
It is important to mention that first health check-up within ten days after birth was
reported to be very low in Bihar. At the same time around two-third mothers
received support from non-trained persons like mother/mother in-law, friends and
dais while there should have been more involvement from ANM/ASHA/ AWW.
(Bihar_NIPI, 2009)
In Bihar the percentage of women initiating breastfeeding within an hour of
childbirth is substantially less than the proportion of institutional deliveries,
suggesting that even in health institutions also early initiation of breastfeeding was
not ensured. ASHAs in rural areas are more close to mothers than any other health
workers
and they counsel them on breastfeeding practices like giving mother’s
first milk to the child, exclusive breastfeeding up to six months and improved
immunity of the child due to mother’s milk. (Bihar_NIPI, 2009)
However, ASHAs, AWWs and ANMs are the people who v i s i t the community
and stay there to interact with the general population. They are able to educate the
110
NIPI Reference Book-Bihar
village mothers and train them periodically so as to eliminate the barriers more
effectively. They also offer many incentives to these mothers. (Bihar_NIPI, 2009)
A recent national level survey estimated morbidity among children to be low in the
state or closer to the national level. However many children who suffered from an
illness in the two weeks prior to the survey continued to be ill at the time of the
survey. Although treatment was given to the children, it was given late which could
be dangerous for baby’s life. (Bihar_NIPI, 2009)
Only 35 percent children with diarrhoea received ORS. 16 percent mothers with
children who had diarrhoea in the two weeks prior to the survey revealed that they
did not know what to do when child had diarrhoea. (Bihar_NIPI, 2009)
Respondents utilizing government health care facilities are very low or negligible
which not only costs extra to the poorer population but also push them to visit
quacks and practice home remedy for any illness. (Bihar_NIPI, 2009)
Almost 80 percent mothers stated that they are aware about pneumonia. However on
looking into their awareness on the symptoms, it was found to be inadequate. This
res ul t ed i n t he children receiving much less or somewhat less intake of liquids
and food than normal thereby affecting their health. (Bihar_NIPI, 2009)
The above mentioned situations demand that there be some unified and concerted
effort on the part of all service providers. (Bihar_NIPI, 2009)
5.3 Child Immunization
The immunization of children against six serious but preventable diseases namely,
tuberculosis, diphtheria, pertusis, t e t a n u s , poliomyelitis and measles is the main
component of the child survival programme. As part of the National Health Policy, the
National Immunization Programme is being implemented on a priority basis. The
Government of India initiated the expanded Programme on Immunization (EPI) in 1978 with
111
NIPI Reference Book-Bihar
the objective of reducing morbidity, mortality and disabilities among children from six
diseases. (Bihar_NIPI, 2009)
The Universal Immunization Programme (UIP) was introduced in 1985-86 with the objective
of covering at least 85 percent of all infants against six vaccine prevent abl e diseases by
1990. This scheme was been introduced in every district of the country. The standard
immunization schedule developed for the child immunization programme specifies the age
at which each vaccine should be administrated and the number of doses to be given.
Routine vaccinations received by infants and children are usually recorded on a vaccination
card that is issued for the child. (Bihar_NIPI, 2009)
5.3.1 Vaccination coverage
This section provides the coverage details of different vaccinations including Polio
0, BCG, Polio 1, 2 and 3, Measles and Vitamin A and whether or not coverage
varies across Districts, by sex of the child, location of the PSU, the child’s birth
order or even by the education of the mother. For this analysis, we had taken
children who were 12-23 months of age and the evidence is entirely through service
records, i.e. Immunization card available with the household concerned. (Bihar_NIPI,
2009)
Table 52: BCG and Polio 0‟ coverage by background variables, NIPI-08
BCG
Districts
Polio 0
N
%
N
%
Jehanabad
304
98.7
98
31.8
Nalanda
249
97.3
22
8.6
Sheikhpura
214
95.1
67
29.8
BIHAR
767
97.2
187
23.7
Boy
404
97.6
94
22.7
Girl
363
96.8
93
24.8
RURAL
677
97.1
165
23.7
URBAN
90
97.8
22
23.9
Sex of the Child
Location of PSU
Birth order of child
112
NIPI Reference Book-Bihar
1
197
99
36
18.1
2 to 3
303
96.8
77
24.6
4 to 5
165
95.4
41
23.7
6+
100
98
32
31.4
No education
487
96.6
121
24
Below 5
20
100
6
30
5 to 7
78
98.7
18
22.8
8 to 9
68
98.6
20
29
10 to 11
88
96.7
20
22
12 & above
26
100
2
7.7
Years of schooling
In all the sampled districts as high as 97 percent children received BCG but Polio 0
coverage was near about 24 percent. The coverage of Polio 0 was highest in
Jehanabad (31.8 percent) but much lower in Nalanda (8.6 percent). (Bihar_NIPI,
2009)
Coverage of Polio 0 was marginally higher among girls than boys but not significantly
slow to conclude in favour of any gender bias in coverage. Polio 0 coverage in urban
and rural areas is almost same. (Bihar_NIPI, 2009)
Table 53: Child Immunisation Coverage in NIPI Districts, Bihar
Bihar
Jehanabad
Nalanda
Sheikhpura
%
%
%
%
All Basic Vaccinations
41.4
38.3
54.2
47.2
BCG
81.5
74.5
88
85.4
POLIO3
53.1
48.3
62.8
48.7
DPT3
54.4
49.2
65.1
55.1
MEASLES
54.2
49.3
69.1
63.9
Percentage received at least
one dose of Vitamin A
49.9
49.3
59.4
66
BCG and measles and 3 doses of polio and DPT
Source: District Level Household Survey (2007-2008)
DLHS3 shows that nearly more than half of the children received all three doses
of DPT vaccination in Bihar while equal doses of DPT was recorded in
Sheikhpura
(55.1 percent). Consequently a slightly lower coverage of DPT
113
NIPI Reference Book-Bihar
vaccination was observed in Jehanabad (all three doses of DPT vaccination.) (See
table 54). (Bihar_NIPI, 2009)
Table 54: Immunization coverage – all basic vaccines
District
All Basic
Vaccination
N
%
Jehanabad
157
51
Nalanda
123
48
Sheikhpura
125
55.6
All basic vaccines cover the following:
o BCG
o DPT 1, 2 and 3
o OPV 1, 2 and 3
o Measles
NFHS-3 shows that a third (32.8 percent) of the children in the age group of 1223 months were fully immunised in Bihar. The immunisation figures for Bihar are
worse than the national average. It is also noted that there is a steady increase in the
immunisation coverage over the last two decades. (Bihar_NIPI, 2009)
Outreach of the programmes and availability of the health services at an accessible
place is of utmost importance in delivering a quality service. On interviewing mothers
on the venue of vaccination, varied responses came out from the three districts. In
Jehanabad (20 percent) and Sheikhpura (12 percent) sub centre was the most common
place for women to bring their children for vaccination. However in Nalanda, it was
PHC where (11.5 percent) most of children got vaccinated. The in-law’s home and
parent’s home were next common places for vaccination in Sheikhpura. It was an
altogether different scenario in Nalanda where most of the children were vaccinated in
a SC (nine percent), PHC (11.5 percent) or government hospital (six percent). Taking
Bihar as a whole, PHC (9 percent) and SC (14 percent) were most common, and the
next common places were in law’s home (4 percent) and parent’s home (5 percent).
(Bihar_NIPI, 2009)
114
NIPI Reference Book-Bihar
Table 55: Problems faced by mother/community in vaccinating the child, NIPI-08
DISTRICT
No time from daily
wage work
Distance of Health
Facility/ Vaccination
Centre
Irregular presence
of health
professional
Non- availability of
vaccines
DONT KNOW
NO PROBLEM
FACED
OTHER
Jehanabad
Nalanda
Sheikhpura
Total
Total
Total
N
%
N
%
N
%
300
23.8
349
26.7
319
25.1
286
22.6
243
18.6
235
18.5
125
9.9
142
10.9
97
7.6
112
8.9
184
14.1
55
4.3
93
7.4
63
4.8
185
14.5
566
44.8
561
42.9
562
44.2
8
0.6
8
0.6
9
0.7
115
NIPI Reference Book-Bihar
Chapter-6
Resource Persons
116
NIPI Reference Book-Bihar
6. Resource Persons
6.1 List of Resource Person at State Level
Name
Designation
Sh. Amarjeet
Sinha, I.A.S.
Sh.Sanjay
Kumar, I.A.S.
Principal
Secretry
Executive
Director
Additional
Executive
Director
Dr.D.K.Raman
Sh.Ashok
Kumar Singh,
B.A.S
Sh.Jay Prakash
Singh, B.A.S.
Lalit Bhushan
Ranjan,B.A.S.
Sh.K.L.Das
Sh.P.N.Mishra
Qualification
I.A.S.
08.02.2010
ed_shsb@yahoo.co.in
drdkraman@yahoo.com
B.Sc.(Geology)
Deputy
Collector
Finance
Manager
Account
Manager
Email
I.A.S.
Administrative
Officer
Deputy
Collector
DOJ
10.11.09
administrativeofficer92@gmail.com
23.06.10
jpchullu@gmail.com
22.04.2010
M.A.
(Econimics)
04.02.08
fmshsbihar@gmail.com
Dr.Narendra
Kumar Mishra
State
Programme
Officer
M.B.B.S, M.S.
02.12.09
nkmishra57@gmail.com
Dr.A.K.Tiwary
State Programe
Officer
M.B.B.S.,
H.M. Diploma
02.12.05
draketewary@yahoo.co.in
Dr.M. P.
Sharma
State Programe
Officer
M.B.B.S.
02.12.09
sharma_madan1@yahoo.co.in
Dr.A. K. Shahi
State Programe
Officer
M.B.B.S.
02.12.09
drakshahi@gmail.com
Ms.Rashi
Jayaswal
State Programe
Manager
PGDRM,
PGDHRM
08-022008
rash_san@rediffmail.com
Ms. Jyoti
Verma
Dy. Director M
&E
P.G.D.R.D
02-032010
jyoti26.ranchi@gmail.com
Dr. Jayati
Srivastava
Dy. Director Training
MSW,Ph.D
31.03.10
trainingcellshsb@gmail.com
Mr.Gaurav
Kumar
Dy. Director
MCH
MBA- Public
Health
29-032010
ddmch.bihar@yahoo.com
Mr.Ram Ratan
SPO-RI &
Polio
BS(HB) &
Med.Anatomy
(AIIMS),
PGDCH (CMC
Vellore)
02.03.10
rraiims@gmail.com
Er. Alok
Ranjan
Consultant
cold chaincum-I/c
B.Tech +
M.B.A.
21.12.05
coldchainbihar@gmail.com
hkbihar@gmail.com
117
NIPI Reference Book-Bihar
Housekeeping
Sh. Ranjeet
Samaiyar
Sh Arvind
Kumar
Sh. Atul
Verma
6.2
Consultant
NRHM
MBA (Health)
01.08.08
nrhmbihar@gmail.com
MCA
01.08.08
statehealth_society@yahoo.co.in,
arvindkr05@gmail.com"
PG in
Computer
Science/IT
23.12.05
atulverma10000@gmail.com
System
Analyst-cumData Officer
Data Officercum-I/C
Complaint Cell
List of Resource person at District Level
S.No.
District
D.P.M
1
Jehanabad
Mr.Niwish
Manan
2
Nalanda
Mr. P. P
Chakariyar
3
Patna
4
Sheikhpura
Mr.
Piyush
Ranjan
Mr.
Acharya
Mamat
Code
No.
Office
No.
06112
230414
0612
2300658
06341
225031
Sl.No
Fax
No.
230558
225031
CUG No.
Contact No
9473191879
9835400289
9473191889
9473191889
9473191891
9334122969
Mr. B.
Rai
9473191897
9334269382
Mr.
Pankaj
Kumar
Location
D.A.M
Mr.
Kausal
Jha
Mr.
Nirbhay
Kr.
Designation
Contact No
Mr. Arvind
Kumar
9334956994
9430287252
Mr. Kumar
Manoj
9431261867
9431268013
Mr. Shiv
Krishna Murti
9973448760
Mr. Gautam
9934066861
Mobile
Number
Moic - Ratni Faridipur PHC
9470003325
2
Moic - Jehanabad Sadar PHC
9470003326
3
D.M
9470003327
4
Ghosi MOIC
9470003328
5
ACMO
9470003329
C.S
9470003330
7
Moic - Mukhudumpur PHC
9470003331
8
DS - Sadar Hospital. Jehanabad
9470003332
Jehanabad
Contact No
9939391876
1
6
M & E Officer
9
Moic - Hulasganj PHC
9470003333
10
Moic - Modanganj PHC
9470003334
11
Moic - Kako PHC
9470003335
12
DIO
9470003336
118
NIPI Reference Book-Bihar
2
D.S. - Sub divisional Hospital
,Hilsa
DIO - Nalanda
3
D.M - Nalanda
9470003504
4
Moic - Silow PHC
9470003505
5
D.S. - Sadar Hospital , Nalanda
9470003506
6
C.S. - Nalanda
9470003507
7
Moic - Tharthari PHC
9470003508
8
Moic - Noorsarai PHC
9470003509
9
Moic - Harnaut PHC
9470003510
10
Moic - Islampur (Referal) PHC
9470003511
11
Moic - Ekangarsarai PHC
9470003512
12
Moic - Biharsharif (Sadar) PHC
9470003513
Moic - Chandi PHC
9470003514
14
Moic - Nagarnausa PHC
9470003515
15
Moic - Karai parsurai PHC
9470003516
16
Moic - Hilsa PHC
9470003517
17
Moic - Sarmera PHC
9470003518
18
Moic - Bind PHC
9470003519
19
Moic - Asthawa (Referal) PHC
9470003520
20
Moic - Prwalpur PHC
9470003521
21
Moic - Katarisaria PHC
9470003522
22
Moic - Rahui PHC
9470003523
23
Moic - Giriyak PHC
9470003524
24
Moic - Rajgir (Referal) PHC
9470003525
25
Moic - Bain PHC
9470003526
26
ACMO - Nalanda
9470003527
1
Moic - Chewara PHC
9470003728
2
3
4
5
Moic - Ariari PHC
C.S
D.M
ACMO
9470003729
9470003730
9470003731
9470003732
1
13
6
Nalanda
9470003502
9470003503
Moic - Shekhopursarai PHC
9470003733
7
Moic - Ghatkusumbha
9470003734
8
D.S - Sub. Div. Hos.Sheikhpura
9470003735
9
DIO
9470003736
10
Moic - Barbigha PHC
9470003737
11
Moic - Sheikhpura Sadar PHC
9470003738
1
DIO
9470003548
2
Superintendent Cum HOD, Eye
9470003549
Moic - Asthawa
9470003550
Moic - Athmalgola Phc
9470003551
5
Principal
9470003552
6
HOD, Medicine
9470003553
7
HOD, E.N.T
9470003554
Sheikhpura
3
4
Patna
119
NIPI Reference Book-Bihar
8
Fatuha , MOIC
9470003555
9
HOD, Surgery
9470003556
10
HOD, Orthopadic
9470003557
11
HOD, Plastic Surg.
9470003558
12
HOD, Aneathesia
9470003559
13
HOD, Neuro Serg.
9470003560
14
HOD, P.M.R.
9470003561
15
HOD, O.B.S. & Gyane.
9470003562
16
HOD, PEDIA
9470003563
17
HOD, Readiotherapy
9470003564
18
HOD, Skin, V.D.
9470003565
19
HOD, Psychiatrist
9470003566
20
HOD, F.M.T.
9470003567
21
Superintendent
9470003568
22
Principal
9470003569
23
HOD, Readiotherapy
9470003570
24
HOD, Skin
9470003571
25
HOD, Psychiatrist
9470003572
26
HOD, Aneathesia
9470003573
27
HOD, E.N.T
9470003574
28
HOD, F.M.T.
9470003575
29
HOD, P.S.M.
9470003576
30
HOD, Medicine
9470003577
31
HOD, Surgery
9470003578
32
HOD, O.B.S. & Gyane.
9470003579
33
HOD, Paedia
9470003580
34
HOD, Eye
9470003581
35
HOD, Orthopadic
9470003582
36
S.D.H. G.G.S. Patna
9470003583
37
DS - S.D.H. Danapur PHC
9470003588
38
RDD
9470003599
39
C.S
9470003600
40
DM/ PATNA
9470003601
41
42
Bidhayak Hospita Virchand
Patel Path Patna
Dr. Sushila Prasad New Garden
Hospital 6/C , MOIC
9470003612
9470003614
120
NIPI Reference Book-Bihar
6.3 NGOs in Bihar
NGOs working on Health sector
1.
Adarsh Chikitsha Sewa Sanstha
Parameshara
Rupouli via Jhausharpur (R.S.)
Madhubani - 847403
Bihar
Tel
: –
Fax
: –
E-mail : –
Website: www.indiasocial.org
Contact: Secretary
Activities : ADOLESCENT HEALTH AND NUTRITION; TRAINING; IEC MATERIAL; EDUCATION
2.
Bihar State AIDS Control Society
S.I.H.F.W. Building
Sheikhpura
Patna - 800014
Bihar
Tel
: 0612-2290278
2286437
Fax
: 0612-2282082
E-mail : biharsacs@gmail.com
Website: www.bsacs.org
Activities : AIDS BIHAR; AIDS PREVENTION; HIGH RISK GROUP; SEX WORKER; INNOVATIVE
PROJECT AIDS
3.
4.
5.
6.
Centre for Health & Resource Management
(CHARM)
Main Road
Budha Colony
Patna - 800001
Bihar
Tel
: 0612-2525527
9431493870
Fax
: –
E-mail : shakeel456@rediffmail.com
Website: –
Contact: Executive Director
Activities : CHILD HEALTH; HEALTH COMMUNICATION; HEALTH COMMUNICATION
MATERIAL; COMMUNICATION MATERIAL; FLOOD MEDICAL RELIEF; IEC MATERIALS; AIDS;
KALAZAR CONTROL; SENSITIZATION WORKSHOP; FLASH CARDS
Tel
: 06454-226146
DEEPALAYA (Institute for Mental Health &
Fax
: –
Rehabil.)
Kailashpuri
E-mail : –
Srinagar Hata
Website: –
Purnea - 854301
Contact: Secretary
Bihar
Activities : MENTAL HEALTH; REHABILITATION; SELF HELP GROUPS; HEALTH ISSUES
Tel
: 0612-2271609
EPOS Health (India) Pvt. Ltd. Bihar Office
68/A, Patliputra Colony
Fax
: –
Patna - 800013
E-mail : bjo@epos.in
Bihar
eposhq@epos.in
Website: www.epos.in
Contact: Senior Vice President
Activities : PUBLIC HEALTH; HEALTH COMMUNICATION; HOSPITAL PLANNING; PUBLIC
PRIVATE PARTNERSHIP; HUMAN RESOURCE DEVELOPMENT AND MANAGEMENT; QUALITY
MANGEMENT SYSTEM AND ACCREDITATION; STRATEGIC PLANNING AND MANAGEMENT;
ORGANIZATION SYSTEMS AND DEVELOPMENT
Tel
: 06156-287522
Indian Council of Acupressure Yoga
Radhika Kunj
09934969232
Nechua Jalalpur
Fax
: –
Gopalganj - 841503
E-mail : –
Bihar
Website: –
Activities : ACUPRESSURE; YOGA; NATUROPATHY; HEALTH AWARENESS; HEALTH CAMPS;
TRAINING; ADOLESCENT HEALTH AND NUTRITION; EDUCATION; RESEARCH STUDIES;
121
NIPI Reference Book-Bihar
7.
8.
9.
10.
11.
12.
ADVOCACY
Kurji Holy Family Hospital
Sadaquat Ashram
Patna - 800010
Bihar
Tel
: 0612-2262540/156
2264117
Fax
: –
E-mail : khfhosp2@sancharnet.in
Website: –
Contact: Community Health Project
Activities : HEALTH CARE; EDUCATION; POOR; MARGINALIZED GROUPS; SLUM DWELLER;
COMMUNITY HEALTH
Tel
: –
Monghyr Chakshu Yojana Samiti
Radiant Chemical Compound
Fax
: –
Avantika Road
E-mail : –
Jamalpur P.O.
Website: –
Monghyr - 811214
Contact: President
Bihar
Activities : HEALTH SERVICES; RURAL HEALTH; FREE EYE TEST; LOW COST SPECTACLES
Tel
: 06344-222560
Monghyr Chakshudan Yojana Samiti
Choramba Road
9204086500
Monghyr - 811201
Fax
: –
Bihar
E-mail : –
Website: –
Contact: Secretary
Activities : HOSPITAL; DISPENSARIES MEDICAL
HEALTH; EYE DONATION; CHILD WELFARE
Nari Nidhi
2/29, State Bank Colony-II,
Bailey Road
Patna - 800014
Bihar
RELIEF CAMPS; NURSING MOTHER; CHILD
Tel
: 0612-2593018
9934262978
Fax
: 9430013517 (M)
E-mail : narinidhi_pat@sify.com
Website: –
Contact: Secretary
Activities : CHILD HEALTH; WOMEN HEALTH; SELF HELP GROUPS; REPRODUCTIVE HEALTH;
FEMALE FOETICIDE; AYURVEDA; POLIO ERADICATION AWARENESS; KOPAL; ICDS
Tel
: 9234755878
Priyadarshini Swasthya Sanstha
'Urmila Sadan' Mishri Tola
9939681225
Tekari Road
Fax
: 9334051887
P.O. Mahandru
E-mail : psss1@rediffmail.com
Patna - 800006
Website: –
Bihar
Contact: Secretary
Activities : WOMEN WELFARE; EDUCATION; WOMEN'S HEALTH; REPRODUCTIVE HEALTH;
ICDS; BALIKA SAMRIDDHI YOJANA; CAMPS CHILDREN; KISHORI SHAKTI YOJANA; MAHILA
MANDAL; MAHILA PANCH; MAHILA SAMAKHYA; SANJEEVANI; SWADHAR; SHORT STAY
HOMES; WOMEN IN DISTRESS
Tel
: 0612-2266605
Voluntary Health Association of Bihar
West of Ganga Apartment
236712 (R)
L.C.T. Ghat
Fax
: 0612-2266884
Mainpura
E-mail : bvha@sancharnet.in
Patna - 800001
Website: –
Bihar
Contact: Executive Director
Activities : CHILD HEALTH; WOMEN HEALTH; HEALTH COMMUNICATION; SEMINAR;
PATIENT CARE; HEALTH SERVICES
122
NIPI Reference Book-Bihar
Bihar NGO working on Nutrition
Tel
: 612-2276991
2276735
Fax
:–
E-mail : cbox@careindiabih.org
Website: –
2.CARE India Bihar
House 100, Road 1 E
New Patliputra Colony
Patna - 800013
Bihar
Activities : COMMUNITY
MICRONUTRIENTS
3.The Hunger Project
Bihar Office
Mehman Sarai, First Floor
(Behind Imarat Rizvi)
Bank Road, Patna - 800001
Bihar
NUTRITION;
MATERNAL
NUTRITION;
CHILD
NUTRITION;
Tel
: 0612-2207705
Fax
: 0612-2231826
E-mail : bihar_@thp.org
Website: www.thp.org
Activities : MALNUTRITION; HUNGER; MATERNAL HEALTH; COMMUNITY NUTRITION;
POVERTY; CHILD MORTALITY; PRIMARY EDUCATION; GENDER EQUALITY; AIDS;
PANCHAYATI RAJ; NUTRITIONALLY VULNERABLE GROUPS; WOMEN'S EMPOWERMENT;
ENVIRONMENT; GLOBAL PARTNERSHIP
Ministry of Health & Family welfare funded Field NGOs
BIHAR
Patna
Bihar Voluntary Health
Association,
West of Ganga Apartment,
Mainpura, Patna-800 001
Arpan Gramin Vikas Samiti
Mr. Ram Babu
PO- Maner, Dist Patna- 801108
Ph-9835256391
Patna Zila Gramin Vikas Samiti
Mr. Umesh Kumar
House of Dr. Kapil Deo Narayan Singh,
Rd No. 9, East Patel Nagar, Post- Shastri
Nagar,
Patna- 800023
Ph- 0612-2604300, 9431071556
123
NIPI Reference Book-Bihar
Phualwari Jagriti Kendra
Mr. Dinesh Kumar
Vill – Atwarpur, PO- Kurthoi, Ps
Phulwarisharif, Patna
Ph-2511534
Bhartiya Gramin Vikas Evam Ayurveda
Sewa Sansthan
Dr. Anil Kumar Singh
Kararia Bhawan, East Lohanipur, railway
Hunder Rd. Kadamkuan, Patna-800003
Ph- 0612-268896, 9431457942
Nalanda
Bihar Voluntary Health
Association,
West of Ganga Apartment,
Mainpura, Patna-800 001
Bhartiya Jan Utthan Parishad
Mr. Abhishek Bhartiya
Moh-Kammaruddinganj,
PO- Biharsharif, Dist Nalanda - 803101
Ph- 06112-223373/223887, 9431023131,
9934048651
Nisha Bunai Silai School
Mr Harikant Jha
Quamaruddinganj,
PO- Biharsharif, Dist Nalanda- 803101
Ph- 06112-221890/223877, 9835008979
124
NIPI Reference Book-Bihar
Maahila Samaj Vikas Sansthan
Mrs. Alam Ara
Moh-Sherpur
PO- Biharsharif, Dist Nalanda- 803101
06112-222452
Sarvodaya Vikas Jyoti
Prof Ajay Sharma
At & PO- Barbigha, Dist – Sheikhpura811101
Ph- 06112- 272069/272071, 9934026208
125
NIPI Reference Book-Bihar
Works Cited
(2004). A strategy to improve Maternal and Child care. Government of Orissa, Department of Health
& Family Welfare. Bhubhaneswer: Government of Orissa.
Aggrawal, N. (2010). Monitering report of High Focus District (Jehanabad). Ministry of Health and
Family Welfare, MIS. Jehanabad, Bihar: NRHM.
(2009). An analysis of health status of Orissa in specific refrence to health equity. Orissa Health
Support Project. Bhubaneswar: CITRAN Consulting.
(2009). BASELINE SURVEY ON CHILD AND RELATED MATERNAL HEALTH CARE. DRS Pvt. Ltd, Norway
India Partnership Initiative. New Delhi: NIPI.
Bhelari, A. (2011, Feb. 2). Health cover for Rs 30. (The Telegraph) Retrieved Feb. 2, 2011, from The
Telegraph: http://www.telegraphindia.com/1110202/jsp/bihar/story_13520597.jsp
Bihar. (n.d.). Retrieved Jan. 10, 2011, from Minstry of Health and Family Welfare:
http://mohfw.nic.in/nrhm/state%20files/bihar.htm
Bihar State Report. 2009.
Community and Home Based Post Natal Care. (2009, April 29). Retrieved Jan. 28, 2011, from NIPI:
http://www.nipi.org.in/chpnc
(2009). District Health Action Plan, Sheikhpura. District Health Society, Sheikhpura. Sheikhpura,
Bihar: NRHM.
(2009). District Health Action Plan_Jehanabad . NRHM. Jehanabad, Bihar: Distrct Health
Society_Jehanabad.
(2010). District Health Plan_Nalanda. Nalanda (Patna): NRHM.
(Apr,2010). District Level Funds Flow & Expenditure Analysis under the NRHM in Bihar. India: Grant
Thornton.
Gill, K. (2009). A Primary Evaluation of Service Delivary inder the National Rural Health Mission
(NRHM): Findings from a study an Andhra Pradesh, Uttar Pradesh, Bihar and Rajasthan. Planning
Commision. New Delhi: Goverment of India.
Jha, S. C. (2007). BIHAR: ROAD MAP FOR dEVELOPEMENT OF HEALTH SECTOR. Planning Commision,
Goverment of India. New Delhi: GoI.
Kumar, S. (2009). District Health Action Plan. Retrieved Jan. 14, 2011, from
http://mohfw.nic.in/nrhm/DHAP/DHAP_Bihar/buxar.pdf
Madhav, D. G. (2010). PHC in Rural Bihar: Gaps in Infrastucture and Service Delivary. (G. L. Forgia,
Ed.) India Health Beat , 3 (6), 4.
Mamta. (2008). Retrieved from
http://www.biharonline.gov.in/Site/Content/Government/Schemes.aspx?u=MAMTA
126
NIPI Reference Book-Bihar
Medha Soni. (2010). Pulse. (T. P. Singh, Ed.) Pulse , 3, 8.
Norway- India Partnership Initiative (NIPI). (n.d.). (Department of Health & Family Welfare, GoO)
Retrieved Jan. 31, 2011, from Department of Health & Family Welfare, GoO:
http://203.193.146.66/hfw/External_Aided_Projects.asp?GL=5
(2010). Nursig Servises in Bihar; Current situation, Requrement and Measure to Address shortages.
NHSRC (NRHM). Hyderabad, India: Academy for Nursing Studies & Women’s Empowerment
(ANSWER).
Official Website of Jehanabad District. (n.d.). Retrieved Feb. 21, 2011, from
http://jehanabad.bih.nic.in/rsvyswotanalysis.html
Official website of Sheikhpura district of Bihar. (n.d.). (NIC) Retrieved Feb. 22, 2011, from
Adminstritative Information: http://sheikhpura.bih.nic.in/admin.htm
Padmanabhan, P. (2009). Addreshing Challenges in Bihar. Delhi: NHSRC.
Peters, V. R. (2008). Regulating India's health services: To what end? what future? Social Science &
Medicine , 66, 2133-2144.
Program. (2011, Jan. 25). Retrieved Jan. 28, 2011, from Centre of Market Innovation:
http://healthmarketinnovations.org/program/chiranjeevi-yojana-cy
Public Private Partnership - Outsourcing of Support Services. (n.d.). Retrieved Feb. 23, 2011, from
State Health Society, Bihar: http://statehealthsocietybihar.org/ppp.html
Ratan, N. (2010). Feasibility survey of Bihar (NIPI). A N Sinha Institute of Social Science, NIPI.
Hyderabad: Access Health International.
S. Chakrabarti, A. D. (2000). Improving Private Practisner care of sick children: testing new approach
in rural Bihar. Health Policy & Planning , 15 (4), 400-407.
Srivastava. (2003). Toward a developement Strategy (Bihar). (World Bank) Retrieved Jan. 10, 2011,
from World Bank: http://siteresources.worldbank.org/INTINDIA/Resources/chapter_5.pdf
SRS 2009. (2011). (Ministry of Health & Family Welfare, GoI) Retrieved Jan. 24, 2011, from HMIS
Portal: http://www.nrhm-mis.nic.in
(2009). Status of Health in Bihar. GoB, Department of Health. Patna: DoH (Bihar).
The Emerging Role of PPP in Healthcare Sector. KPMG, CII.
http://www.ibef.org/download/PolicyPaper.pdf.
TOR_Bihar_DFID. (2008, Jan. 30). Retrieved Jan. 11, 2011, from DESIGN AND IMPLEMENTATION OF
BIHAR HEALTH SECTOR REFORM:
http://webarchive.nationalarchives.gov.uk/+/http://www.dfid.gov.uk/procurement/files/ojec8277to
rs.pdf
127
NIPI Reference Book-Bihar
WHO. (2007, August 6). Retrieved Jan. 14, 2011, from Country Health profile and Health SystemIndia: http://www.searo.who.int/en/Section313/Section1519_10853.htm
128
NIPI Reference Book-Bihar
Appendix-I
Funds Flow Mechanism for SHS Bihar
Source- (Bihar DET Report, Apr,2010)
129