Designing a Critical Care Nurse–Led Rapid Response Team Using
advertisement
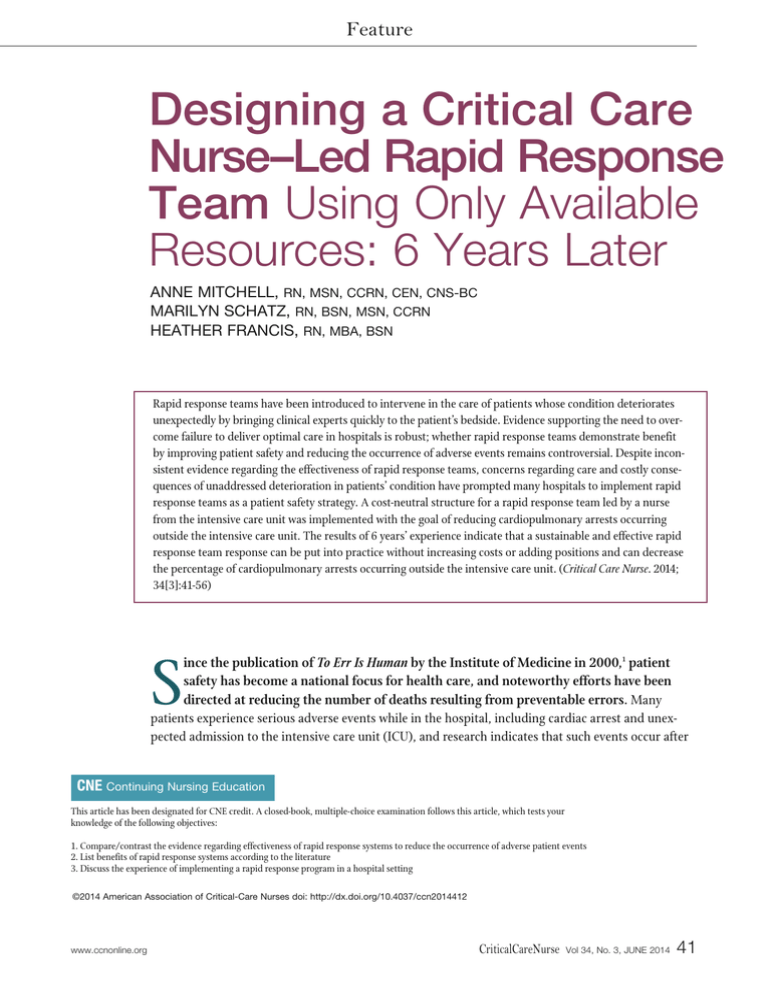
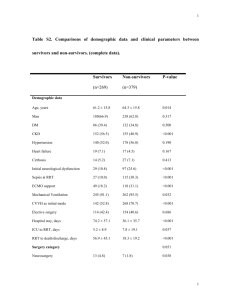
Feature Designing a Critical Care Nurse–Led Rapid Response Team Using Only Available Resources: 6 Years Later ANNE MITCHELL, RN, MSN, CCRN, CEN, CNS-BC MARILYN SCHATZ, RN, BSN, MSN, CCRN HEATHER FRANCIS, RN, MBA, BSN Rapid response teams have been introduced to intervene in the care of patients whose condition deteriorates unexpectedly by bringing clinical experts quickly to the patient’s bedside. Evidence supporting the need to overcome failure to deliver optimal care in hospitals is robust; whether rapid response teams demonstrate benefit by improving patient safety and reducing the occurrence of adverse events remains controversial. Despite inconsistent evidence regarding the effectiveness of rapid response teams, concerns regarding care and costly consequences of unaddressed deterioration in patients’ condition have prompted many hospitals to implement rapid response teams as a patient safety strategy. A cost-neutral structure for a rapid response team led by a nurse from the intensive care unit was implemented with the goal of reducing cardiopulmonary arrests occurring outside the intensive care unit. The results of 6 years’ experience indicate that a sustainable and effective rapid response team response can be put into practice without increasing costs or adding positions and can decrease the percentage of cardiopulmonary arrests occurring outside the intensive care unit. (Critical Care Nurse. 2014; 34[3]:41-56) ince the publication of To Err Is Human by the Institute of Medicine in 2000,1 patient safety has become a national focus for health care, and noteworthy efforts have been directed at reducing the number of deaths resulting from preventable errors. Many patients experience serious adverse events while in the hospital, including cardiac arrest and unexpected admission to the intensive care unit (ICU), and research indicates that such events occur after S CNE Continuing Nursing Education This article has been designated for CNE credit. A closed-book, multiple-choice examination follows this article, which tests your knowledge of the following objectives: 1. Compare/contrast the evidence regarding effectiveness of rapid response systems to reduce the occurrence of adverse patient events 2. List benefits of rapid response systems according to the literature 3. Discuss the experience of implementing a rapid response program in a hospital setting ©2014 American Association of Critical-Care Nurses doi: http://dx.doi.org/10.4037/ccn2014412 www.ccnonline.org CriticalCareNurse Vol 34, No. 3, JUNE 2014 41 failure to rescue.2,3 Several studies have established that up to 84% of patients show signs of clinical deterioration 6 to 8 hours preceding cardiac arrest.3-7 Clinicians often fail to appreciate or report antecedent signs of deterioration or to intervene if signs of deterioration are indeed recognized.3,4,8 The inability of clinicians to recognize a decline in a patient’s condition and prevent unintended injury or death constitutes failure to rescue, which has been incorporated as a measure of medical and nursing care.4,6-10 Reasons for failure to rescue include limitation of monitoring techUp to 84% of patients show signs nology to specialty of clinical deterioration 6 to 8 hours units; failure to preceding cardiac arrest. report or respond to abnormal findings on assessment; variation in individual judgment, training, and experience; low sensitivity and fidelity of periodic assessments in general care areas; and inability of frontline staff to initiate early interventions independently.8,11 Because cardiac events are often not sudden and early signs of deterioration in a patient’s condition are not always recognized, rapid response systems (RRSs) have been introduced to intervene in the care of declining patients by bringing clinical expertise and timely interventions to the bedside.3,8,12 Litvak and Pronovost13 suggest that some patients in general care areas have their condition deteriorate despite adequate clinical care whereas other patients may be misclassified on admission and the level of care provided is inadequate to meet the patient’s needs, so rapid response teams (RRTs) are necessary to rescue them. In 2004, the Institute for Healthcare Improvement (IHI), through its Saving 100000 Lives Campaign, challenged Authors Anne Mitchell is a clinical nurse specialist in the emergency department and intensive care unit at Banner Baywood Medical Center, Mesa, Arizona. Marilyn Schatz is a clinical manager in the intensive care unit at Banner Baywood Medical Center. Heather Francis is the director of nursing of the intensive care unit, dialysis, at Banner Baywood Medical Center. Corresponding author: Anne Mitchell, RN, MSN, CCRN, CEN, CNS-BC, Banner Baywood Medical Center, 6644 E. Baywood Avenue, Mesa AZ 85206 (e-mail: anne.mitchell@ bannerhealth.com). To purchase electronic or print reprints, contact the American Association of CriticalCare Nurses, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org. 42 CriticalCareNurse Vol 34, No. 3, JUNE 2014 the health care community to create a culture of patient safety. In 2006, the IHI recommended the deployment of RRTs as 1 of 6 innovative strategies to improve patients’ outcomes.1,14 In 2005, the first International Consensus Conference of Medical Emergency Teams convened experts in patient safety, critical care, and hospital medicine to standardize nomenclature, describe patients who might benefit from RRTs, and identify characteristics of an RRS.2 They identified 3 models of RRSs: medical emergency teams (MET) led by a physician, RRTs led by a nurse (usually a critical care nurse), and critical care outreach (CCO) teams led by a nurse, which in addition to responding to RRT calls, provide surveillance for patients recently discharged from the ICU. Although the optimal composition of a RRT is not known, members of the team typically include physician or nurse team leads, respiratory therapists, critical care nurses, and nursing supervisors.3,8,15 Although most RRTs are staff activated, many hospitals now provide family and patients access to the RRT in accordance with the 2009 Joint Commission National Patient Safety Goals.16 Family-activated RRT call rates are reported to be low and often relate to communication issues between providers and patients’ families or pain management.11,17-20 In 2011, the Society of Critical Care Medicine surveyed hospitals to determine their experience with patient and family activation of RRSs.20 Of the 25 participating hospitals, 67% used a nurse-led RRT model and 90% afforded patients and their families access to the RRT. The volume of family or patient calls ranged from 0 to 24 calls per year and appeared to be related to the size of the facility. A lack of understanding of the plan of care or perceived lack of a quick response to changes in the patient’s condition were reported as primary causes for family RRT activation.20 Impact of RRTs on Patients’ Outcomes Evidence of the impact of RRTs or METs on the safety and survival of hospitalized patients is contradictory, with researchers in some studies reporting decreased rates of cardiac arrests, unplanned ICU admissions, and hospital mortality, whereas researchers in other studies reported no difference.8,21-26 Bristow and colleagues21 reported a reduction in the number of unplanned ICU admissions, but no difference in cardiac arrest rates when they compared 1 hospital that had a MET with 2 hospitals that did not. In a prospective controlled trial www.ccnonline.org that examined the effect of a MET on postoperative patients, Bellomo and colleagues22 concluded that the availability of a hospital-wide MET 24 hours a day, 7 days a week reduced both the incidence of postoperative adverse outcomes and mortality rates. In an observational study, DeVita and colleagues23 reported that use of a MET decreased the mean monthly incidence of cardiopulmonary arrest by 17%. A single-center 5-year study examined the effect of a MET on time to treatment and mortality rates of patients diagnosed with shock and showed substantial reductions in time to central catheter placement, fluid and antibiotic administration, and mortality rates after implementation.25 In a prospective before and after trial in a community hospital, using an RRT led by a physician’s assistant, Dacey et al27 reported that cardiac arrests per 1000 discharges decreased from 7.6 before RRT implementation to 3.0 afterward. After initiation of a CCO model, McFarlan and Hensley17 noted a 36% reduction in the rate of non-ICU cardiac arrest whereas Thomas and colleagues,11 using a nurse-led RRT, reported a 56% decrease in cardiac arrest outside the ICU. One year after implementation of an RRT, Jolley et al18 reported a 21% decrease in the occurrence of cardiac arrests outside of the ICU but noted no change in hospital mortality rates. After execution of a MET in a 300-bed teaching hospital, Buist and colleagues,28 after adjusting for case mix, noted a 50% decrease in the incidence of unexpected cardiac arrests and a reduction in mortality from 77% to 55%. Howell did not use an ICU-trained RRT but instead focused on systematic detection of patients’ clinical deterioration and notification of the usual care providers to determine if patients’ outcomes improved.29 They reported that a rapid response by this type of team was independently associated with decreases in unexpected mortality and cardiac arrests occurring outside of the ICU, proposing this as a cost-effective option for facilities with limited critical care resources.29 Using an intensivist-led CCO model that also included an ICU fellow and provided 48 hours or more of post-ICU surveillance, Al-Qahtani and colleagues30 evaluated non-ICU cardiac arrests 2 years before and 3 years after implementation. They noted a decrease in non-ICU arrests from 1.4 to 0.9 per 1000 hospital admissions and a decrease in hospital mortality from 22.5 to 20.2 per 1000 hospital admissions. In spite of strong face validity and widespread adoption in many hospitals, measurable benefit after www.ccnonline.org implementation of an RRT has not been reported by all investigators. In a large, multicenter randomized controlled trial, the MERIT study investigators randomly assigned 23 hospitals to MET implementation or usual care for 6 months and found no reduction in cardiac arrests, ICU admissions, or unexpected deaths.24 After a systematic review and analysis of studies evaluating RRT effectiveness, Chan and colleagues26 reported that implementation of an RRT in adult populations was associated with a 33.8% reduction in rates of cardiopulmonary arrests outside the ICU but did not decrease hospital mortality. After completing a systematic review of RRSs, Winters and colleagues31 concluded that although METs were associated with reductions in hospital mortality and cardiac arrest rates, the results should be interpreted with caution because of limitations (wide confidence intervals, lack of heterogeneity, nonrandomization) in the quality of the studies they reviewed. However, Winters et al8 recently published a second systematic review of RRSs as a patient safety strategy, Evidence on the impact of rapid response again noting teams (RRTs) or medical emergency that RRSs teams (METs) on the safety and survival decreased the of hospitalized patients is contradictory. rate of adult and pediatric arrests outside the ICU but benefits were not consistently realized by all facilities. They suggested several possible explanations for some RRSs not realizing benefits: unknown optimal team membership, ineffective monitoring and identification of patients in deteriorating condition, and limited availability of resources.8 However, they did conclude that the beneficial effects of RRSs are becoming more apparent with increased implementation. Results of these studies reporting mortality and non-ICU cardiopulmonary arrest data are summarized in Table 1. Some authors suggest that RRT benefits include more than measurements of mortality rates and numbers of cardiac arrests. Rosen and colleagues32 reported reductions in non-ICU codes and mortality rates during a 3-year period within a 26-hospital collaborative after each facility implemented a type of RRS. They described unanticipated benefits related to RRS use, including improved staff satisfaction, the opportunity to discuss and change code status, and identification of new areas for quality improvement.32 After comparing outcomes for patients admitted to the ICU via RRT intervention CriticalCareNurse Vol 34, No. 3, JUNE 2014 43 Table 1 Reference Summary of studies of rapid response systems that reported comparison data Type of team Findings Bristow et al, 2000 MET Fewer unanticipated ICU admissions, no difference in in-hospital cardiac arrest rates or mortality, higher rate of do-not-resuscitate orders Buist et al,28 2002 MET Reduction in cardiac arrest rate, decrease in hospital mortality rate Bellomo et al, 2004 MET Decrease in postoperative adverse outcomes, mortality rate, and length of stay in hospital DeVita et al,23 2004 MET Decrease in cardiopulmonary arrest rate, no change in proportion of fatal arrests Hillman et al,24 2005 (MERIT) MET No significant difference in unexpected deaths, incidence of cardiac arrest, unplanned ICU admissions 21 22 Sebat et al,25 2007 Dacey et al,27 2007 McFarlan and Hensley, 2007 MET (emergency department physician and intensivist) Decreased time to central catheter placement, infusion of fluids, ICU admission, first antibiotic administration and profound reduction in mortality for patients identified with shock RRT led by physician assistant Decreased in-hospital cardiac arrest rate and unplanned ICU admissions 17 RRT Decrease in cardiac arrests in non-ICU areas Thomas et al, 2007 RRT Decrease in cardiac arrests on medical-surgical units, decrease in nonICU cardiac arrests Jolley et al,18 2007 RRT Decrease in arrests and non-ICU arrests, no difference in deaths/1000 discharges 11 Howell et al,29 2012 Patient’s usual primary care team, no critical care training Reduction in unexpected mortality, no difference in overall in-hospital mortality rate, decrease in non-ICU arrests MET Decrease in non-ICU cardiopulmonary arrest, decrease in non-ICU mortality rate (anticipated and unanticipated) Rosen et al,32 2013 Variable team composition among 26-hospital collaborative Decrease in non-ICU arrests, nonsignificant decreases in ICU codes and all-cause mortality rates Jones et al,33 2010 MET (patient’s on-call physician and ICU nurses) Decrease in non-ICU cardiac arrests Al-Qahtani et al,30 2013 Chan et al, 2010 Meta-analysis of 18 studies Reduction in cardiac arrests outside ICU, not associated with lower hospital mortality rates Winters et al,8 2013 Meta-analysis of 18 high-quality studies and 26 lower-quality studies Decrease in cardiac arrests in non-ICU areas, benefit not realized in all rapid response systems 26 Abbreviations: ICU, intensive care unit; MET, medical emergency team; RRT, rapid response team. versus patients transferred to the ICU by usual processes, Jaderling et al34 suggested that RRTs represent an important mechanism for identifying complex cases in which patients are in need of ICU care. They noted that although 30-day mortality did not differ, the RRT patients were older, had more severe comorbid conditions, and were almost 3 times as likely to have a diagnosis of severe sepsis.34 Additional benefits of RRTs listed by Thomas et al11 include improved patient safety, improved identification by nurses of signs of deterioration, increased satisfaction of physicians and patients, and increased job satisfaction among nurses. 44 CriticalCareNurse Vol 34, No. 3, JUNE 2014 Some researchers, addressing the inconsistent results of RRT studies, suggest that RRT benefit takes time, perhaps several years, to become evident as it involves a cultural change for an institution. RRT success also appears to be linked to practice; if the RRT is widely adopted by clinicians, it appears more effective.35,36 A higher call intensity, or “dose rate,” more than 25 RRT calls per 1000 admissions, is reported to be associated with decreases in cardiac arrest rate,37 and conversely when the RRT rate decreases, the cardiac arrest rate increases.36 The RRT must be used to be effective, and if it is not used, benefits may not be manifested.3,15,24,37 www.ccnonline.org The complexity of the intervention and the lack of benchmarking tools to facilitate comparisons of RRS outcomes among hospitals may contribute to the inconsistent evidence of RRT effectiveness.24,38 It is assumed but not established that RRSs are rapid and responsive.38 To that end, Olgesby et al38 proposed a “score to door time,” the time from the first recorded abnormality that should have triggered RRS activation to ICU admission, as a standardized measure of RRS effectiveness. Delays greater than 4 hours were associated with higher Acute Physiology and Chronic Health Evaluation (APACHE) scores at ICU admission.38 Attempting to improve the effectiveness of the RRT, a group of investigators placed automated vital sign monitors on patients in general care areas that provided electronic prompts to escalate care when abnormalities were detected. They reported increases in the detection of respiratory abnormalities, increased RRT calls, and improved survival of patients receiving RRT intervention.39 Wake Forest University initiated an RRS comprising the patient’s on-call physician and critical care nurses hired into RRS positions to identify patients who are not responding to treatment.33 Owing to a 17% decline in RRS use, policy was changed to mandate RRS activation for any patient meeting the criteria for physiological instability, resulting in a 34% increase in RRS calls and a 35% decrease in cardiopulmonary arrests occurring in the general care areas.33 The authors concluded that by mandating RRT activation, fear of criticism on the part of nurses initiating RRS was eliminated, resulting in increased call rates and improved outcomes.33 In addition to vital signs criteria, judgment that prompt assistance was needed at the bedside was emphasized to staff as an important criterion for RRT activation by Beitler and colleagues.40 As a result, they reported significant reductions in hospital-wide mortality, out-ofICU mortality, and out-of-ICU cardiopulmonary arrests.40 Although outcomes vary from study to study, the beneficial effects of RRTs are becoming clearer as the intervention is more universally applied. Benefit has been reported in many hospital settings using a variety of RRS models even though this has not firmly translated into a consistent reduction in overall hospital mortality.8,19,23,28,29,41 Perceptions and Function of RRTs To determine the value of RRTs as perceived by nurses and physicians using them, investigators www.ccnonline.org surveyed staff in hospitals with established programs. They found that nurses working in facilities with wellfunctioning and integrated RRTs did not hesitate to activate it.42-44 Conversely, teams not viewed as cohesive and supportive were less likely to be called because the nursing staff was not confident the team would support their decision to activate the response.42 Nurses with RRT experience indicate that they initiate RRTs for 3 primary reasons: (1) the patient exhibits signs and symptoms that were either unexpected or significantly different from baseline; (2) the nurse, despite the absence of objective data, The RRT must be used to be effective, thought that something was and if it is not used, benefits may not wrong; and (3) be manifested. the nurse was convinced that the patient needed immediate intervention and was either unable to reach the physician or unable to obtain appropriate interventions as perceived by the nurse.42 Nurses with access to a robust RRT state that if they were changing jobs or a family member required hospitalization, they would select a facility offering an RRT.32,42,43 Surveys of medical residents and nurses indicate that both agree that the presence of a MET improves patient safety, although the nurses perceived that more strongly than did the residents.42-45 Benin and colleagues45 conducted qualitative open-ended interviews with nurses, physicians, RRT members, and house staff to evaluate their view of RRT impact within a hospital setting. Nurses reported a sense of security and empowerment derived from knowing that skilled backup was available, a perception echoed by physicians and administrators.45 Additional positive benefits included increased morale among nurses, real-time redistribution of nurses’ workload, triage of patients needing intensive care, and immediate access to expert help.45 After conducting interviews with RRT members, physicians, and staff, and observing actual RRT events, Leach and Mayo12 defined 5 attributes associated with well-functioning and effective RRTs: an organizational culture supportive of innovation and committed to patient safety, expertise of team members, dedicated RRT positions, communication, and familiarity among RRT members. Easy access to RRT activation and a respectful, nonjudgmental response by the RRT members have also been identified as structural elements critical to RRT success.46-48 CriticalCareNurse Vol 34, No. 3, JUNE 2014 45 Development of a Facility-Based RRT In 2005, administrators at a nonteaching, 275-bed community hospital within a large health care system (Banner Baywood Medical Center, Mesa, Arizona) resolved to follow the IHI recommendations by implementing a hospital RRT. They tasked the facility’s code blue committee with the responsibility for model selection, process development, and implementation. Table 2 When to activate the rapid response team Nurse is concerned about patient Respiratory distress or threatened airway (respiratory rate >30/min or <6/min or acute change in oxygen saturation <90% despite administration of oxygen) or change in breathing pattern Acute change in blood pressure to <90 mm Hg, heart rate to <40/min or >130/min, or 20% change from baseline Acute change in level of consciousness Model Selection After a review of the literature and IHI recommendations for RRSs and evaluation of available resources, a nurse-led RRT model was selected. The RRT implementation had to be budget neutral. No positions existed that could be solely dedicated to the RRT, and creating new RRT nursing positions was not an option. The selected RRT membership included the nursing house supervisor, the shift lead respiratory therapist, and the nurse manager of the ICU, who was designated as team lead. Typically none of these individuals had patient assignments and all could respond quickly to an RRT call. If the ICU nurse manager could not avoid a patient assignment, they were directed to delegate another ICU nurse to respond, assign other ICU nurses to monitor their patients while off the unit, or notify the nursing supervisor that they were unable to respond but were available for phone consultation. Procedure Criteria for calling the RRT similar to the criteria used by other hospitals were developed (Table 2), but staff were encouraged to activate the RRT any time they had concerns about a patient’s condition.3,15,18,23,27,29,30,41,47 To activate the RRT, staff called the same emergency phone number used to broadcast a cardiac arrest. A beeper paging system was tried about a year after RRT implementaEasy access to RRT activation and a tion to reduce respectful, nonjudgmental response by hospital noise, the RRT members are critical to success. but overhead paging of RRT calls was resumed because of some dead zones within the facility. The RRT responded to all inpatient units, diagnostic areas, a rehabilitation unit located within the facility, as well as outpatient areas such as endoscopy, medication and pain clinics, and a chest pain unit. In the event of simultaneous RRT calls, the clinical nurse 46 CriticalCareNurse Vol 34, No. 3, JUNE 2014 Urine output <50 mL in 4 hours without history of renal dysfunction Failure to respond to treatment specialist or the ICU director of nursing would respond. If they were unavailable, the ICU nurse manager and the nursing supervisor decided who would respond to which call and would request additional respiratory therapy support if needed. An emergency protocol for orders common to urgent patient situations was developed for use by the RRT (Table 3). The cardiovascular, internal medicine, surgery, and anesthesia medical committees approved the emergency protocol and operationalization of the RRT. As RRT lead, the ICU nurse manager was encouraged to communicate assessment findings and recommendations directly to the patient’s primary provider, who was always contacted. However, if the RRT event concluded before contact with the provider, and transfer to a higher level of care was not indicated, the patient’s primary nurse assumed responsibility for communicating findings to the responding physician. Initially, ICU transfer was ordered by the attending physician, but after the initiation of an intensivist program, this became a collaborative decision between the intensivist and the attending physician. Documentation of RRT call data was recorded by the nursing supervisors on a form created for that purpose and became a permanent part of the medical record (Figure 1). The RRT call rates, cardiac arrests outside the ICU, and outcome data were reviewed bimonthly by the code blue and RRT committee and reported annually to the hospital quality committee. Education All hospital clinical staff and physicians were educated about the purpose and process of RRT activation www.ccnonline.org Table 3 Rapid response team’s emergency protocol: symptomatic/unstable – systolic blood pressure ≤90 mm Hg, change in level of consciousness, nausea/vomiting, dizziness, lightheadedness, diaphoresis, saturations decreased from normal, tachypnea Complaint Interventions Sudden onset of chest pain Call physician Obtain stat EKG, physician to interpret Apply O2 at 2-4 L via nasal prongs; titrate O2 to maintain SpO2 ≥92% Nitroglycerin 0.4 mg SL for unrelieved chest pain q 5 minutes x 3 Nitroglycerin infusion for CP unrelieved by SL NTG, start 5 μg/min Sustained symptomatic ventricular tachycardia Pulse present: Call physician Titrate O2 to maintain SpO2 ≥92% Obtain 12-lead EKG (physician to interpret), continuous monitoring Amiodarone 150 mg in 100 mL D5W IV over 10 minutes (15 mg/min); followed by amiodarone 900 mg in 500 mL D5W IV infusion at 1 mg/min Cardiovert if patient becomes unstable/symptomatic If becomes pulseless, call code blue; follow ACLS guidelines Symptomatic bradycardia Call physician Titrate O2 to maintain SpO2 ≥92% (flow maximum 4 L/min) Obtain 12-lead EKG, physician to interpret Atropine 0.5 mg IV; may repeat x 1 Apply transcutaneous pacemaker if dysrhythmia persists Acute respiratory distress Call physician Titrate O2 to maintain SpO2 ≥92% (verify O2 flow with physician) Notify respiratory therapist Stat ABG Call ED physician to intubate if patient’s condition critical Order stat portable CXR if suspected pneumothorax, hemothorax, or other chest abnormality For life-threatening dysrhythmias associated with placement of a Swan-Ganz catheter in the right ventricle Notify the physician Withdraw Swan-Ganz catheter into the right atrium (after verifying that the balloon is deflated) For symptomatic tachycardia Call physician Initiate ACLS guidelines for synchronized cardioversion if patient’s condition becomes unstable For symptomatic hypotension Call physician Initiate fluid bolus of 250 mL normal saline H/H if bleeding suspected Abbreviations: ABG, arterial blood gas analysis; ACLS, Advanced Cardiovascular Life Support; CP, chest pain; CXR, chest radiograph; D5W, 5% dextrose in water; ED, emergency department; EKG, electrocardiogram; H/H, hemoglobin/hematocrit; IV, intravenous; NTG, nitroglycerin; O2, oxygen; q, every; SL, sublingual; SpO2, oxygen saturation by pulse oximetry; stat, urgent. (Figure 2). Designated members of the RRT received training on use of the emergency protocol and expectations of RRT roles, with a strong emphasis on providing positive reinforcement to staff members initiating the response. No specific education on the clinical management of urgent patient situations was deemed necessary for the 4 ICU nurse managers. They had a mean of 21 years of ICU experience, maintained Advanced Cardiac Life Support (ACLS) certification, and had already informally consulted on non-ICU patients in deteriorating condition when requested by other nurse managers. This approach allowed more rapid implementation of the RRT program and decreased RRT initiation costs. www.ccnonline.org Findings Before RRT Implementation Before RRT implementation, a retrospective chart review was conducted of inpatients sustaining a cardiopulmonary arrest during the preceding year to evaluate the presence of antecedent physiological abnormalities. A systolic blood pressure less than 90 mm Hg, a heart rate greater than 100 beats per minute, and a respiratory rate greater than 20 breaths per minute were grouped together and considered abnormal vital signs. Oxygen saturation less than 90% was considered abnormal, and a level of consciousness recorded as less than the patient’s baseline was considered altered mental status. New onset or worsening of pain was determined by the patient’s CriticalCareNurse Vol 34, No. 3, JUNE 2014 47 RAPID RESPONSE TEAM RECORD Date: _______________________ Time called: __________ Team called by: ❒ Nurse Patient label Room#/location: __________________ Arrival time: ______________ ❒ Therapist ❒ House officer Code status_________ Event ended: ____________ ❒ Attending ❒ Other ____________ PRIMARY REASON FOR CALL ❒ Staff concerned/worried: ❒ Acute significant bleed Specify: _______ ❒ Acute mental change ❒ SBP less than 80 mm Hg ❒ Failure to respond to treatment ❒ Symptomatic hypertension ❒ New neuro deficit VITAL SIGNS: HR____________ ❒ ❒ ❒ ❒ ❒ ❒ RR less than 8 Symptomatic bradycardia RR greater than 24 Seizures SpO2 less than 90% HR greater than 130 BP______________ RR______________ Situation/background: TEMP_____________ RECOMMENDATIONS/INTERVENTIONS Airway/Breathing ❒ Oral airway ❒ Suctioned ❒ Nebulizer treatment ❒ Intubated ❒ NPPV ❒ Bag mask ❒ O2 Mask/nasal ❒ ABG ❒ CXR ❒ No intervention Circulation ❒ Fluid bolus ❒ Blood ❒ EKG ❒ NPPV ❒ Defibrillation ❒ Cardioversion ❒ No intervention Admitting DX: History: MEDICATIONS: ASSESSMENT: OTHER INTERVENTIONS (Specify): Follow-up report: Outcome: ❒ Potential code avoided ❒ Other: __________________________________________________________ ❒ Stayed in room ❒ Transferred to ICU ❒ Transferred to telemetry ❒ Remote telemetry PHYSICIAN NOTIFIED: __________________________________ Time: _______________________________ SIGNATURES OF TEAM MEMBERS: MD:________________________________________________________ RN:________________________________________________________ RT:_________________________________________________________ Figure 1 Form used to document rapid response calls. Abbreviations: ABG, arterial blood gas analysis; BP, blood pressure; CXR, chest radiograph; DX, diagnosis; EKG, electrocardiogram; HR, heart rate; ICU, intensive care unit; MD, physician; NPPV, noninvasive positive-pressure ventilation; O2, oxygen; RN, nurse; RR, respiratory rate; RT, respiratory therapist; SBP, systolic blood pressure; SpO2, oxygen saturation by pulse oximetry; TEMP, body temperature. report of pain. Patients exhibited signs of deterioration a mean of 4.53 hours before cardiac arrest. A change in vital signs, occurring in 74% of patients, was the most common abnormality noted before cardiac arrest. The next most common abnormality was oxygen desaturation in 42% of patients, followed by an alteration in mental 48 CriticalCareNurse Vol 34, No. 3, JUNE 2014 status in 37% of patients. New or increased pain was noted in a small number of patients. Most patients exhibited more than 1 indication of deterioration in clinical condition. The percentage of cardiac arrests occurring outside of the ICU was 83%. The cardiac arrest rate was 1.84 and the hospital mortality rate was 1.42 per 1000 discharges. www.ccnonline.org Findings After RRT Implementation House supervisor Lead respiratory therapist Intensive care unit’s nurse manager Assessment of patient Transfer to higher level of care Collaborates with attending physician Make recommendations and patient remains on present unit If patient’s condition worsens or you become concerned—recall critical rescue No. of inpatient codes Figure 2 Algorithm showing the process for activating the rapid response team. 7 17 6 14 12 5 10 4 8 3 6 2 4 1 No. of rapid response calls In mid-February 2006, the RRT officially became operational. By year’s end, a total of 106 RRT calls had been made and 20 inpatients had experienced cardiac arrest. In 2006, the cardiac arrest rate per 1000 discharges was 1.7 and the percentage of non-ICU cardiac arrests decreased from 83% to 12.7%, a substantial reduction. The number of cardiac arrests declined as the number of RRT calls increased (Figure 3). By the close of 2007, the percentage of cardiac arrests occurring outside the ICU was 64% and declined further to a relatively constant rate, ranging between 45% and 53% through 2012 (Figure 4). The actual number of cardiac arrests increased during the 6-year period, related to the addition of 68 ICU and inpatient beds and a higher patient volume. The cardiac arrest rate initially decreased for the first 2 years of implementation to 1.7 but increased to 3.4 by 2012 after changes in the method of collecting and reporting this data were implemented within the health care system. Hospital mortality rate showed a small downward trend from 1.44 per 1000 discharges in 2005 to 1.25 per 1000 discharges in 2012. The number of RRT calls increased almost every year, peaking at 444 calls in 2011, ending at 358 calls for 2012, reflective of a 5% decrease in 2012 hospital discharges. The RRT “dose” rate increased from 7.5 per 1000 discharges in 2007, the first full year of RRT operation, to as high as Page rapid response team 2 0 0 February March April May June Inpatient codes Juy August September October November December Rapid response calls Figure 3 Inpatient codes versus rapid response calls in 2006. Rapid response calls started in February, and there were no inpatient codes in December. www.ccnonline.org CriticalCareNurse Vol 34, No. 3, JUNE 2014 49 90 60 80 40 60 50 30 40 20 30 20 Number of non-ICU cardiac arrests Percentage of non-ICU cardiac arrests 50 70 10 10 0 0 2005 2006 2007 2008 2009 2010 2011 2012 Year % of non-ICU cardiac arrests No. of non-ICU cardiac arrests Figure 4 Percentage versus number of cardiac arrests not occurring in the intensive care unit (ICU). Data point for the number of non-ICU cardiac arrests in 2005 was not available. 20.3 per 1000 discharges in 2011. The RRT call duration decreased from a mean of 40 minutes the first year to a mean of 24.3 minutes by 2012. Telemetry activated the RRT most often, followed by the medical and surgical units. Although the telemetry units placed the most RRT calls, the “other” category, which includes the outpatient areas, rehabilitation unit, medical imaging, cafeteria, hospital lobby, and other areas, demonstrated an increased call rate during the 6-year period, while telemetry calls decreased The RRT included the nursing house slightly. Most supervisor, the shift lead respiratory calls occurred therapist, and the nurse manager of the between the ICU, who was designated as team lead. hours of 7 AM and 3 PM, but calls during evening and night hours have trended upward (Figure 5). Disposition of RRT patients after an RRT event remained consistent during the 6 years (Figure 6). More than half, up to 58%, of RRT patients transferred to the ICU after an RRT event, 10% to 20% transferred to telemetry, and 30% to 40% remained in their room. A small number of RRT patients from outpatient areas 50 CriticalCareNurse Vol 34, No. 3, JUNE 2014 were taken to the emergency department. Initially the most common reason for the RRT call was a change in vital signs, but over time, nurses’ concern for the patient became the most common reason and a change in vital signs became the second most common trigger. Discussion Although the goal of RRT implementation was to reduce the incidence of cardiac arrests outside the ICU, the precipitous decrease during the first year, from 83% to 12.7%, was greater than anticipated. Likely reasons for this decrease included the implementation of the RRT, the opening of a newly constructed 26-bed ICU, nearly double the size of the former ICU, and the addition of 56 new telemetry and surgical beds. Typically many patients in the emergency department waited from 2 to 24 hours or more for inpatient bed placement. The addition of the new beds improved patient flow, decreased length of stay in the emergency department, and facilitated patients’ placement on monitored units. In 2007, the second year of RRT implementation, 64% of arrests occurred outside the ICU, a 23% decrease www.ccnonline.org 80 70 Percentage of calls 60 50 40 30 20 10 0 0 2006 2007 2008 2009 Year 2010 2011 2012 2011 2012 Time of day 7 AM-2:59 PM 3 PM-10:59 PM 11 PM-6:59 AM Figure 5 Percentage of calls and time of day. 70 60 Percentage of patients 50 40 30 20 10 0 2006 2007 2008 2009 2010 Year Stayed in room Transferred to telemetry unit Transferred to intensive care unit Transferred to emergency department (outpatients) Figure 6 Disposition of patients after rapid response team was called. www.ccnonline.org CriticalCareNurse Vol 34, No. 3, JUNE 2014 51 from 2005, and comparable to decreases reported by others.8,11,17,26,28 The percentage of non-ICU arrests declined to 56% in 2008 and to 47.6% by 2009, thereafter ranging from 45% to 48% until 2012 when it increased slightly to 53.4%. As hospital volume increased after the addition of 68 beds, the actual number of cardiac arrests increased and then remained fairly constant through 2012. After declining to 1.7 per 1000 discharges for the first 2 years, the cardiac arrest rate increased, in spite of a sustainable reduction in the number of cardiac arrests occurring outside the ICU and a slight decline in hospital mortality rate. After the initial increase, the arrest rate stabilized between 3.4 and 4.5 per 1000 discharges through 2012. An aging population may have contributed to the increase; however, changes made to definitions and disease code classifications during the third year were most likely responsible for the difference in cardiac arrest rates between the first 2 years and the last 4 years. Because the RRT dose rate was less than the recommended 25 per 1000 discharges, using the RRT more often may have resulted in a more observable decrease in the overall arrest rate. The number of RRT events has increased since RRT inception while the duration of calls has decreased. Several factors influenced the increase in RRT use. Intentional promotion of RRT by sharing its success with nursing and medical staff encouraged RRT use, and keeping the ICU nurse manager free of patient assignments accommodated the increased call volume. Although no formal data were obtained, anecdotal reports from nursing staff and managers indicated that they viewed the RRT as a support for the bedside nurse, a patient safety measure, a mechanism for improving The percentage of cardiac arrests occurring communicaoutside the ICU decreased from 83% to tion with 12.7% in the year after implementation of providers, and the RRT, although a new ICU twice the size a tool for facilof the old ICU opened that year too. itating care and ICU transfer for a declining patient. This theme, consistent with previously reported data, was also observed by administrators and most providers.3,35,42,43,46 The mean RRT call duration of 24 minutes in 2012 is similar to what some others have reported.15,32,46,48,49 Factors contributing to shorter RRT calls include familiarity with the RRT process, development of cohesiveness and trust among 52 CriticalCareNurse Vol 34, No. 3, JUNE 2014 team members, and acquisition of expertise by both nurses from general care areas and RRT members through repeated experience of the RRT process.12,46 This ICU consistently reports the highest mean APACHE scores within the 24-hospital system. The 4 telemetry units, including the stroke unit, have a total of 104 beds and receive the majority of ICU transfers, contributing to their higher number of RRT calls. Two things may be responsible for the decline in telemetry RRT calls in the past few years: the addition of education in nursing orientation focused on patients in deteriorating condition and skill gained in managing declining patients through repeated RRT exposure. Initially the RRT was conceived as a resource for inpatients, although it was never specifically stated that the team would not respond to other areas. As the RRT has become a familiar part of the hospital culture, it has been adopted by all areas of the hospital. The increased volume of RRT use in “other” areas of the hospital such as the kitchen, gift shop, lobby, as well as ancillary departments such as outpatient diagnostics and endoscopy is responsible for the higher number of “other” category calls. Multiple factors contribute to a successful RRT, but nursing satisfaction with the process is a key factor in developing an effective RRT. Supportive feedback from the RRT members and favorable experiences with RRT events reinforce staff use. Because failure of bedside staff to call the RRT when activation criteria are present has been associated with adverse events, the RRT should support the staff initiating the response and consider no call inappropriate.11,24,49 If nurses fear disapproval, believe they have adequate resources to manage the patient, or presume they should be able to handle the patient themselves, initiation of the RRT is unlikely.42,49 Nonjudgmental appraisal of RRT occurrences mitigates fear of reproach for unwarranted calls. An “unnecessary” call still offers opportunities for teaching and mentoring less-experienced clinicians. The nurse may require help even if the patient did not. Easy access to skilled assistance, an immediate response to a patient in unstable condition, expedited patient transfer to a higher level of care, patient stabilization, and confirmation of the bedside nurses’ judgment underscores the benefit of RRT activation to staff.42,44,45 The RRT event may also encourage discussions regarding end-of-life decisions and facilitate a “do-not-resuscitate” order for patients www.ccnonline.org and families struggling with end-of-life decisions.30,32,50 As nurses experience these advantages, the RRT will become incorporated into usual nursing practice.47 Monitoring RRT data and processes are essential to preserve RRT effectiveness by confirming success or identifying deficiencies. Data analysis has confirmed the need to exclude the ICU nurse manager from patient assignments. If RRT call volume increases, call duration lengthens, or the RRT assumes additional responsibilities such as outreach or surveillance, back-up strategies using the clinical nurse specialist or ICU director of nursing may be insufficient, and dedicated positions may be a consideration. Implications for Practice Our experience indicates that a team of clinical experts responding to the bedside of patients in deteriorating condition results in a reduction in non-ICU cardiopulmonary arrests, and this reduction is sustainable over time. Creating and maintaining a successful RRT, without the use of additional resources, is possible if the team members are experienced in the rescue and management of critically ill patients and are routinely free of patient assignments. The ICU nurses leading the RRT should be ACLS certified and proficient critical care nurses. Barriers that prevent bedside staff from activating the RRT need to be identified and conquered in order to promote its use, increase the call rate, and realize benefits. The RRT must be incorporated into hospital culture to be effective. Providing repeated education and sharing RRT outcomes with nurses, clinical staff, physicians, and administrators can perpetuate its use and achieve a higher dose rate, which can maximize RRT impact. The leadership team of the hospital must support an organizational culture that values patient safety and promotes innovative strategies focused on the reduction of adverse outcomes. Ongoing monitoring of RRT call volume, duration, and outcomes is essential to ensure that designated resources are adequate to maintain patient flow, ICU staff supervision, program success, and sustainability. Conclusion Although RRSs have been described as a “bandaid” for managing patients in general care areas whose condition deteriorates, this patient safety strategy is contributing to the ability of hospitals to rescue patients with www.ccnonline.org signs of deterioration and reduce the occurrence of preventable adverse events.8,13 The implementation of an RRT program that uses the ICU nurse manager as the team leader can produce sustainable decreases in the percentage of cardiac arrests occurring outside the ICU without the expense of dedicated resources. Over time, experience with the rapid response process can decrease the duration of the call, which allows accommodation for increases in RRT volume. For now, the RRT seems to be a good strategy for improving patient safety. As Don Berwick14 stated, “the names of the patients whose lives we save can never be known. Our contribution will be what did not happen to them.” CCN Financial Disclosures None reported. Now that you’ve read the article, create or contribute to an online discussion about this topic using eLetters. Just visit www.ccnonline.org and select the article you want to comment on. In the full-text or PDF view of the article, click “Responses” in the middle column and then “Submit a response.” To learn more about rapid response teams, read “Rapid Response Teams: Qualitative Analysis of Their Effectiveness” by Leach and Mayo in the American Journal of Critical Care, May 2013;22:198210. Available at www.ajcconline.org. References 1. Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building A Safer Health System. Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academy Press; 2000. 2. DeVita M, Bellomo R, Hillman K, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006;34:24632478. 3. Jones D, DeVita M, Bellomo R. Rapid response teams. N Engl J Med. 2011;365:139-146. 4. Schein RM, Harzday F, Pena M, Ruben B, Strung C. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388-1392. 5. Franklin C, Matthew J. Developing strategies to prevent in-hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247. 6. Hillman KM, Bristow PJ, Chey T, et al. Antecedents to hospital deaths. Intern Med J. 2001;331:343-348. 7. Buist M, Jarmolowski E, Burton R, Bernard S, Waxman B, Anderson J. Recognizing clinical instability in hospital patients before cardiac arrest or unplanned admission to intensive care. Med J Aust. 1999;171:22-25. 8. Winters B, Weaver S, Pfoh E, Yang T, Pham J, Dy S. Rapid response systems as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:417-425. 9. Clark S, Aiken L. Failure to rescue: needless deaths are prime examples of the need for more nurses at the bedside. Am J Nurs. 2003;103(1):42-47. 10. Silber J, Sankey W, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. Med Care. 1992;30:615-629. 11. Thomas K, VanOyen M, Rasmussen D, Dodd D, Whildin S. Rapid response team: challenges, solutions, benefits. Crit Care Nurs. 2007;27(1):20-27. 12. Leach L, Mayo A. Rapid response teams: qualitative analysis of their effectiveness. Am J Crit Care. 2013;22:198-209. 13. Litvak E, Pronovost P. Rethinking rapid response teams. JAMA. 2010; 304:1375-1376. 14. Institute of Healthcare Improvement. 5 Million Lives Campaign. http:// www.ihi.org/Engage/Initiatives/Completed/5MillionLivesCampaign /Pages/default.aspx. Accessed March 14, 2014. CriticalCareNurse Vol 34, No. 3, JUNE 2014 53 15. Scherr K, Wilson D, Wagner J, Haughian M. Evaluating a new rapid response team. AACN Adv Crit Care. 2012;23(1):32-42. 16. The Joint Commission. 2009 Joint Commission: Hospital national patient safety goals. http://www.unchealthcare.org/site/Nursing/servicelines /aircare/additionaldocuments/2009npsg. Accessed March 3, 2013. 17. McFarlan S, Hensley S. Implementation and outcomes of a rapid response team. J Nurs Care Qual. 2007;22(4):307-313. 18. Jolley J, Bendyk H, Holaday B, Lombardozzi K, Harmon C. Rapid response teams: do they make a difference? Dimens Crit Care Nurs. 2007;26(6): 253-260. 19. Bogert S, Ferrell C, Rutledge D. Experience with family activation of rapid response teams. Medsurg Nurs. 2010;19:215-222. 20. SCCM Update. Patient and family activation of rapid response teams. Crit Connect. 2011;April/May:18-19. 21. Bristow P, Hillman K, Chey T, Daffurn K, et al. Rates of in-hospital arrests, deaths, and intensive care admissions: the effect of a medical emergency team. Med J Aust. 2000;173:236-240. 22. Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004;32(4):916-920. 23. DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL; Medical Emergency Response Improvement Team (MERIT). Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. Qual Saf Health Care. 2004;13:251-254. 24. Hillman K, Chen J, Cretikos M, Bellomo R, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365:2091-2097. 25. Sebat F, Musthafa A, Johnson D, et al. Effect of a rapid response system for patients in shock on time to treatment and mortality during 5 years. Crit Care Med. 2007;35(11):2568-2575. 26. Chan P, Jain R, Nallmothu B, Berg R, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18-26. 27. Dacey M, Mirza E, Wilcox V, et al. The effect of a rapid response team on major clinical outcome measures in a community hospital. Crit Care Med. 2007;35(9):2076-2082. 28. Buist M, Moore G, Bernard S, Waxman B, Anderson J, Hguyen T. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. Br Med J. 2002;321:1-5. 29. Howell M, Long N, Folcarelli P, et al. Sustained effectiveness of a primary team-based rapid response system. Crit Care Med. 2012;40:2562-2568. 30. Al-Qahtani S, Al-Dorzi H, Tamim H, et al. Impact of an intensivist-led multidisciplinary extended rapid response team on hospital-wide cardiopulmonary arrests and mortality. Crit Care Med. 2013;41:506-517. 31. Winters B, Pham J, Hunt E, Guallar E, Berenholtz S, Pronovost P. Rapid response systems: a systematic review. Crit Care Med. 2007; 35(5):1238-1243. 32. Rosen M, Hoberman A, Ruiz R, Sumer Z, et. al. Reducing cardiopulmonary arrest rates in a three-year regional rapid response system collaborative. Joint Comm J Qual Patient Saf. 2013;39:328-336. 33. Jones C, Bleyer A, Petree B. Evolution of a rapid response system from voluntary to mandatory activation. Jt Comm J Qual Patient Saf. 2010;36: 266-270. 34. Jaderling G, Bell M, Martling C, Ekbom A, Bottai M, Konrad D. ICU admittance by a rapid response team versus conventional admittance, characteristics, and outcome. Crit Care Med. 2013;41:725-731. 35. Santamaria J, Tobin A, Holmes J. Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. Crit Care Med. 2010;38(2):445-450. 36. Jenkins S, Lindsey P. Clinical nurse specialists as leaders in rapid response. Clin Nurse Spec. 2010;24:24-30. 37. Jones D, Bellomo R, DeVita M. Effectiveness of the medical emergency team: the importance of dose. Crit Care. 2009;13:313-317. 38. Oglesby K, Durham L, Welch J, Subbe C. “Score to door time,” a benchmarking tool for rapid response systems: a pilot multi-centre service evaluation. Crit Care. 2011;15:R180-R186. 39. Bellomo R, Ackerman M, Bailey M, et al. A controlled trial of electronic automated advisory vital signs monitoring in general hospital wards. Crit Care Med. 2012;40:2349-2361. 40. Beitler J, Link N, Bails D, Hurdle K, Chong D. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Crit Care. 2011;15:R269-R279. 41. Butner S. Rapid response team effectiveness. Dimens Crit Care Nurs. 2011; 30(4):201-205. 42. Donaldson N, Shapiro S, Scott M, Foley M, Spetz J. Leading successful rapid response teams: a multisite implementation evaluation. J Nurs Adm. 2009;39(4):176-181. 54 CriticalCareNurse Vol 34, No. 3, JUNE 2014 43. Sarani B, Sonnad S, Bergey M, et al. Resident and RN perceptions of the impact of a medical emergency team on education and patient safety in an academic medical center. Crit Care Med. 2009;37(12):3091-3096. 44. Shapiro S, Donaldson N, Scott M. Rapid response teams seen through the eyes of the nurse. Am J Nurs. 2010;110(6):28-34. 45. Benin A, Borgstrom C, Jenq G, Roumainis S, Horwitz L. Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators. BMJ Qual Saf. 2012;21:391-398. 46. Hatler C, Mast D, Bedker D, et al. Implementing a rapid response team to decrease emergencies outside the ICU: one hospital’s experience. Med Surg Nurs. 2009;18:84-90. 47. Grimes C, Thornell B, Clark A, Viney M. Developing rapid response teams: best practice through collaboration. Clin Nurse Spec. 2007;21(2):85-92. 48. Chamberlain B, Fonley K, Maddison J. Patient outcomes using a rapid response team. Clin Nurse Spec. 2009;23:11-12. 49. Shearer B, Marshall S, Buist M, et al. What stops hospital clinical staff from following protocols? An analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi-campus Australian metropolitan healthcare service. BMJ Qual Saf. 2012;21:569-575. 50. Downar R, Rodin D, Barua R, et al. Rapid response teams, do not resuscitate orders, and potential opportunities to improve end-of-life care: a mulitcentre retrospective study. J Crit Care. 2013;28:498-503. www.ccnonline.org CCN Fast Facts CriticalCareNurse The journal for high acuity, progressive, and critical care nursing Designing a Critical Care Nurse–Led Rapid Response Team Using Only Available Resources: 6 Years Later Facts • Rapid response teams (RRTs) have been introduced to intervene in the care of patients whose condition deteriorates unexpectedly by bringing clinical experts quickly to the patient’s bedside. • Evidence supporting the need to overcome failure to deliver optimal care in hospitals is robust; whether RRTs demonstrate benefit by improving patient safety and reducing the occurrence of adverse events remains controversial. • Despite inconsistent evidence regarding the effectiveness of RRTs, concerns regarding care and costly consequences of unaddressed deterioration in patients’ condition have prompted many hospitals to implement RRTs as a patient safety strategy. • A cost-neutral structure for an RRT led by a nurse from the intensive care unit (ICU) was implemented with the goal of reducing cardiopulmonary arrests occurring outside the ICU. • No positions existed that could be solely dedicated to the RRT, and creating new RRT nursing positions was not an option. The selected RRT membership Table When to activate the rapid response team Nurse is concerned about patient Respiratory distress or threatened airway (respiratory rate >30/min or <6/min or acute change in oxygen saturation <90% despite administration of oxygen) or change in breathing pattern Acute change in blood pressure to <90 mm Hg, heart rate to <40/min or >130/min, or 20% change from baseline Acute change in level of consciousness Urine output <50 mL in 4 hours without history of renal dysfunction Failure to respond to treatment included the nursing house supervisor, the shift lead respiratory therapist, and the nurse manager of the ICU, who was designated as team lead. • Criteria for calling the RRT similar to the criteria used by other hospitals were developed (see Table), but staff were encouraged to activate the RRT any time they had concerns about a patient’s condition. • To activate the RRT, staff called the same emergency phone number used to broadcast a cardiac arrest. The RRT responded to all inpatient units, diagnostic areas, a rehabilitation unit located within the facility, as well as outpatient areas such as endoscopy, medication and pain clinics, and a chest pain unit. • All hospital clinical staff and physicians were educated about the purpose and process of RRT activation. Designated members of the RRT received training on use of the emergency protocol and expectations of RRT roles, with a strong emphasis on providing positive reinforcement to staff members initiating the response. • The number of RRT events has increased since RRT inception while the duration of calls has decreased. Several factors influenced the increase in RRT use. Intentional promotion of RRT by sharing its success with nursing and medical staff encouraged RRT use, and keeping the ICU nurse manager free of patient assignments accommodated the increased call volume. • Anecdotal reports from nursing staff and managers indicated that they viewed the RRT as a support for the bedside nurse, a patient safety measure, a mechanism for improving communication with providers, and a tool for facilitating care and ICU transfer for a declining patient. This theme, consistent with previously reported data, was also observed by administrators and most providers. • The results of 6 years’ experience indicate that a sustainable and effective RRT response can be put into practice without increasing costs or adding positions and can decrease the percentage of cardiopulmonary arrests occurring outside the ICU. CCN Mitchell A, Schatz M, Francis H. Designing a Critical Care Nurse–Led Rapid Response Team Using Only Available Resources: 6 Years Later. Critical Care Nurse. 2014;34(3):41-56. www.ccnonline.org CriticalCareNurse Vol 34, No. 3, JUNE 2014 55