- American Journal of Orthodontics and Dentofacial
advertisement
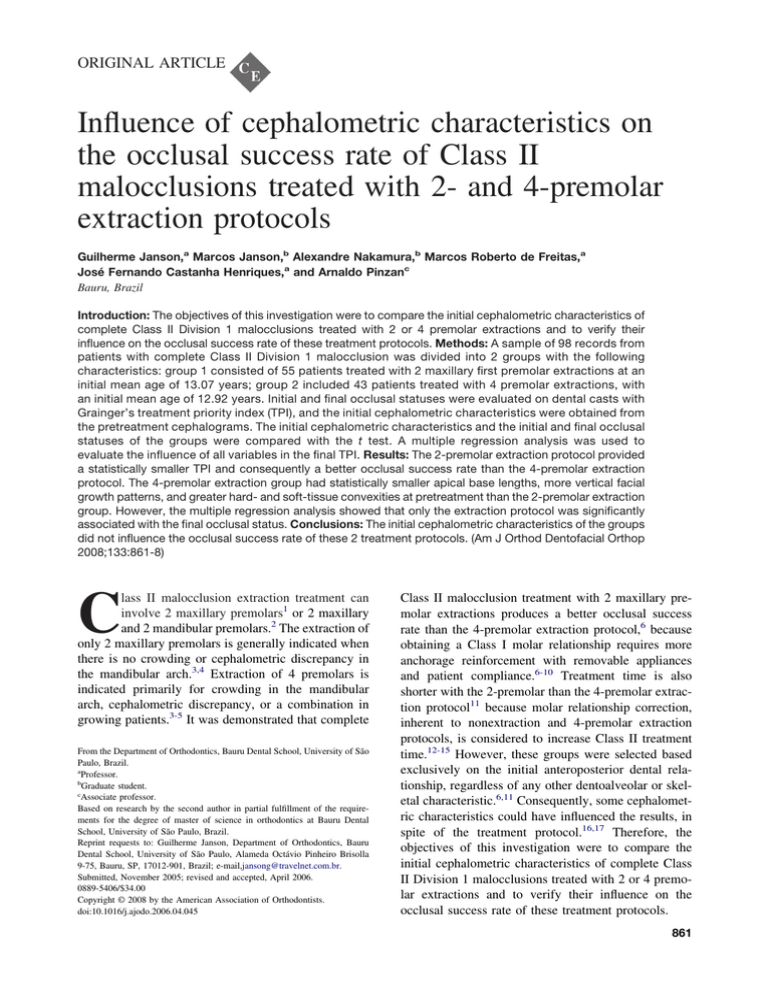
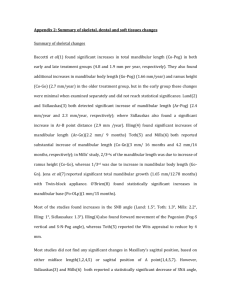
ORIGINAL ARTICLE Influence of cephalometric characteristics on the occlusal success rate of Class II malocclusions treated with 2- and 4-premolar extraction protocols Guilherme Janson,a Marcos Janson,b Alexandre Nakamura,b Marcos Roberto de Freitas,a José Fernando Castanha Henriques,a and Arnaldo Pinzanc Bauru, Brazil Introduction: The objectives of this investigation were to compare the initial cephalometric characteristics of complete Class II Division 1 malocclusions treated with 2 or 4 premolar extractions and to verify their influence on the occlusal success rate of these treatment protocols. Methods: A sample of 98 records from patients with complete Class II Division 1 malocclusion was divided into 2 groups with the following characteristics: group 1 consisted of 55 patients treated with 2 maxillary first premolar extractions at an initial mean age of 13.07 years; group 2 included 43 patients treated with 4 premolar extractions, with an initial mean age of 12.92 years. Initial and final occlusal statuses were evaluated on dental casts with Grainger’s treatment priority index (TPI), and the initial cephalometric characteristics were obtained from the pretreatment cephalograms. The initial cephalometric characteristics and the initial and final occlusal statuses of the groups were compared with the t test. A multiple regression analysis was used to evaluate the influence of all variables in the final TPI. Results: The 2-premolar extraction protocol provided a statistically smaller TPI and consequently a better occlusal success rate than the 4-premolar extraction protocol. The 4-premolar extraction group had statistically smaller apical base lengths, more vertical facial growth patterns, and greater hard- and soft-tissue convexities at pretreatment than the 2-premolar extraction group. However, the multiple regression analysis showed that only the extraction protocol was significantly associated with the final occlusal status. Conclusions: The initial cephalometric characteristics of the groups did not influence the occlusal success rate of these 2 treatment protocols. (Am J Orthod Dentofacial Orthop 2008;133:861-8) C lass II malocclusion extraction treatment can involve 2 maxillary premolars1 or 2 maxillary and 2 mandibular premolars.2 The extraction of only 2 maxillary premolars is generally indicated when there is no crowding or cephalometric discrepancy in the mandibular arch.3,4 Extraction of 4 premolars is indicated primarily for crowding in the mandibular arch, cephalometric discrepancy, or a combination in growing patients.3-5 It was demonstrated that complete From the Department of Orthodontics, Bauru Dental School, University of São Paulo, Brazil. a Professor. b Graduate student. c Associate professor. Based on research by the second author in partial fulfillment of the requirements for the degree of master of science in orthodontics at Bauru Dental School, University of São Paulo, Brazil. Reprint requests to: Guilherme Janson, Department of Orthodontics, Bauru Dental School, University of São Paulo, Alameda Octávio Pinheiro Brisolla 9-75, Bauru, SP, 17012-901, Brazil; e-mail,jansong@travelnet.com.br. Submitted, November 2005; revised and accepted, April 2006. 0889-5406/$34.00 Copyright © 2008 by the American Association of Orthodontists. doi:10.1016/j.ajodo.2006.04.045 Class II malocclusion treatment with 2 maxillary premolar extractions produces a better occlusal success rate than the 4-premolar extraction protocol,6 because obtaining a Class I molar relationship requires more anchorage reinforcement with removable appliances and patient compliance.6-10 Treatment time is also shorter with the 2-premolar than the 4-premolar extraction protocol11 because molar relationship correction, inherent to nonextraction and 4-premolar extraction protocols, is considered to increase Class II treatment time.12-15 However, these groups were selected based exclusively on the initial anteroposterior dental relationship, regardless of any other dentoalveolar or skeletal characteristic.6,11 Consequently, some cephalometric characteristics could have influenced the results, in spite of the treatment protocol.16,17 Therefore, the objectives of this investigation were to compare the initial cephalometric characteristics of complete Class II Division 1 malocclusions treated with 2 or 4 premolar extractions and to verify their influence on the occlusal success rate of these treatment protocols. 861 862 Janson et al American Journal of Orthodontics and Dentofacial Orthopedics June 2008 MATERIAL AND METHODS The sample was retrospectively collected from the files of the orthodontic department at Bauru Dental School, University of São Paulo. Ninety-eight patients (56 male, 42 female), who satisfied the inclusion criteria were selected. The sample was divided into 2 groups according to the extraction protocol. Group 1 consisted of 55 patients (31 male, 24 female) treated with 2 maxillary first premolar extractions at an initial mean age of 13.07 years (SD 1.42; range, 9.42-15.17 years). Group 2 included 43 patients (25 male, 18 female) with an initial mean age of 12.92 years (SD 1.73; range, 10.67-18.33 years). These patients were treated with the following extraction combinations: 30 were treated with 4 first premolar extractions, 11 were treated with maxillary first premolar and mandibular second premolar extractions, 1 was treated with 4 second premolar extractions, and 1 was treated with maxillary first and second premolar extractions in the left and right quadrants, respectively, and mandibular first premolar extractions. The groups were well matched by age and sex. Specific inclusion criteria required all patients initially to have complete (fullcusp) bilateral Class II malocclusion (molar relationship),7,18,19 regardless of any other dentoalveolar or skeletal characteristic. Additionally, the subjects had all permanent teeth up to the first molars and no dental anomalies of number, size, or form. Lateral headfilms were obtained in centric occlusion with passive lip posture at the pretreatment stage. The lateral cephalograms for each subject in both groups were traced on acetate paper by 1 investigator (M.J.) and digitized (Accugrid XNT, model A30TL.F, Numonics, Montgomeryville, Pa). These data were then stored on a personal computer and analyzed with Dentofacial Planner software (version 7.02, Dentofacial Software, Toronto, Ontario, Canada) (Fig 1). Because the headfilms had been taken with different machines, the enlargement factors, from 6% to 9.8%, were corrected with the cephalometric software. It was not possible to use every subject from our previous study, because the initial ages of the groups had to be matched for the cephalometric study, and the initial lateral cephalograms of some subjects were not available.6 Therefore, a new comparison of the initial and final occlusal statuses of these subjects had to be conducted. We used Grainger’s treatment priority index20 (TPI). The TPI index provides weighted subscores for overjet, vertical overbite or open bite, tooth displacement, and posterior crossbite, as well as summary scores reflecting the overall severity of the malocclusion. With the exception of rotation and displace- Fig 1. Unusual cephalometric measurements: 1, Mx1PP: perpendicular distance from the maxillary central incisor edge to the palatal plane; 2, Mx6-PP: perpendicular distance from the mesial cusp tip of the maxillary molar to palatal plane; 3, Mx6-ANSperp: distance between the mesial point of the maxillary first molar and the anterior nasal spine-perpendicular line; 4, Md1-MP: the perpendicular distance from mandibular central incisor edge to the mandibular plane; 5, Md6-MP: the perpendicular distance from the mesial cusp tip of the mandibular molar to mandibular plane; 6, Md6-Pogperp: distance between the mandibular first molar mesial point and the pogonion-perpendicular line; 7, overjet: the horizontal distance from the maxillary incisor edge to the mandibular incisor edge, measured parallel to the Frankfort horizontal plane; 8, overbite: the vertical distance from the maxillary incisor edge to the mandibular incisor edge, measured perpendicular to the Frankfort horizontal plane; 9, molar relationship: distance between the mesial surface of maxillary first molar and the mandibular first molar, measured parallel to the Frankfort horizontal plane (positive value when the maxillary molar was anterior to the mandibular molar); 10, canine relationship (OP): distance between the maxillary canine cusp tip and the mandibular canine cusp tip, measured parallel to the functional occlusal plane; 11, NAP angle formed by nasion, A-point, and pogonion (not illustrated). ment, all TPI components are measured along a continuous scale from positive to negative values. Thus, mandibular overjet and open bite are scored as negative overjet and negative overbite, respectively. A constant corresponding to the first molar relationship is added to the TPI score. Total scores on the TPI range Janson et al 863 American Journal of Orthodontics and Dentofacial Orthopedics Volume 133, Number 6 from 0 to 10 or more, with higher scores representing more severe malocclusions.21,22 The TPI components are defined as follows.21,22 1. Overjet is the anterior distance from the most mesial part of the labial surface of the maxillary central incisor to the labial surface of the opposing mandibular incisor, measured perpendicularly to the coronal plane. 2. Overbite or open bite (with the dental models in centric [convenience] occlusion) is the amount of vertical overlap of the maxillary central incisor over the mandibular central incisor taken as a ratio of the total crown height (cervix to incisal edge) of the mandibular incisor. 3. Tooth displacement is the sum of the number of teeth noticeably rotated or displaced from ideal alignment, plus twice the number of teeth rotated more than 45° or displaced more than 2 mm. 4. First molar relationship is a constant comprising the severity of the malocclusion, based on the relationships between the maxillary and mandibular first molars. 5. Posterior crossbite is the buccolingual deviation in occlusion of the postcanine teeth. The measurement is positive for buccal crossbite (first molar positioned too far buccally) and negative for lingual crossbite. Crossbite is also scored as the number of teeth deviating from ideal cusp-to-fossa fit by a cusp-to-cusp relationship or worse.21,22 In the 2-premolar extraction subjects, it was assumed that a Class II molar relationship at the end of treatment would be classified as a neutral relationship in the TPI because this is the correct posterior tooth arrangement in a normal relationship of the anterior teeth in this treatment approach. Mandibular crowding of the initial dental study models was calculated as the difference between arch length (circumference, from left to right first molars) and the sum of tooth widths from first molar to first molar, in millimeters. In a well-aligned arch, arch length was equal to the sum of the tooth widths. Negative values indicated crowding.23 Forty pairs of dental study models (20 of each group) were remeasured by the same examiner (data obtained from the previous study6), and 20 randomly selected radiographs were retraced and redigitized by the same examiner (M.J.). The casual error was calculated according to Dahlberg’s formula (S2 ⫽ ⌺d2/2n),24 where S2 is the error variance and d is the difference between the 2 determinations of the same variable. The systematic error was evaluated with dependent t test25 at P ⬍0.05. Statistical analyses Intergroup compatibility for initial age and sex distribution was evaluated with t and chi-square tests, respectively. The cephalometric variables at pretreatment were compared between the groups with t tests. A multiple regression analysis was used to evaluate the influence of all variables in the final TPI (FTPI). Statistical analyses were performed with Statistica software (Statistica for Windows, version 6.0, Statsoft, Tulsa, Okla) at P ⬍0.05. RESULTS Of the 29 variables, only 4 had systematic errors: Md6-Pogperp, overbite, canine relationship, and nasolabial angle (definitions are given in Fig 1). Four variables showed casual errors greater than 1 mm or 1°, and only 2 variables were greater than 2°. The groups were compatible for initial age, sex distribution, and initial TPI (ITPI) (Table I). Group 1 had larger basal bones (Co-A, Co-Gn, Go-Gn, Co-Go), more protrusive mandible (SNB angle), more horizontal growth pattern (FMA, SNGoGn), less protruded mandibular incisors (Md1-NB), larger Class II canine anteroposterior discrepancy (canine relationship OP), and less convex profile (NAP) than group 2 (Table II, Fig 2, A). Of all variables, only the extraction protocol was significantly associated with the FTPI, according to the multiple regression analysis (Table III). DISCUSSION The purpose of this investigation was to evaluate whether the initial cephalometric characteristics of the groups in a previous study, whose occlusal outcomes were compared, could have influenced the results.6 In that study, the results showed a better occlusal success rate for the 2-premolar extraction protocol compared with the 4-premolar extraction protocol. The groups in the previous study were chosen primarily for complete bilateral Class II malocclusion, independently of the associated cephalometric skeletal characteristics. Therefore, the same subjects were selected for this evaluation, except those without an initial cephalometric radiograph. Additionally, to match the groups’ initial ages, some other records were discarded. This resulted in the records of 98 patients. Table I shows that the groups were compatible for initial age, sex distribution, and ITPI. Although the groups were not compatible for initial amount of crowding, this variable was taken into account in the multiple regression analysis. The FTPI of group 1 was statistically smaller than that of group 2, demonstrating a greater occlusal success 864 Janson et al Table I. American Journal of Orthodontics and Dentofacial Orthopedics June 2008 Compatibility and results of the occlusal comparison between the groups Group 1 (n ⫽ 55) 2 extractions Group 2 (n ⫽ 43) 4 extractions Variable Mean (SD) Mean (SD) P value Crowding (mm) Age (y) Sex 0.76 (1.30) 13.02 (1.42) 3.44 (2.69) 12.92 (1.73) 0.000*† 0.773† Male 31 (56.36%) ITPI FTPI Female 24 (43.63%) Male 25 (58.13%) 8.17 (1.80) 0.67 (0.72) Female 18 (41.86%) 8.16 (1.04) 1.87 (1.66) 0.843‡ 0.970† 0.000*† *Statistically significant: †t test; ‡chi-square test. Table II. Pretreatment comparison between groups (t test) Variable Maxillary component SNA angle (°) Co-A (mm) Mandibular component SNB angle (°) Co-Gn (mm) Go-Gn (mm) Co-Go (mm) Maxillomandibular relationship ANB angle (°) Facial pattern FMA (°) SN.GoGn (°) Sn.PP (°) LAFH (mm) Maxillary dentoalveolar component Mx1.NA (°) Mx1-NA (mm) Mx1-PP (mm) Mx6-PP (mm) Mx6-ANSperp (mm) Mandibular dentoalveolar component Md1.NB (°) Md1-NB (mm) Md1-MP (mm) Md6-Pogperp (mm) Md6-MP (mm) Dentoalveolar relationships Overjet (mm) Overbite (mm) Molar rel (mm) Canine rel OP (mm) Hard- and soft-tissue profile Nasolabial angle (°) NAP (°) Group 1 (n ⫽ 55) 2 extractions Mean (SD) Group 2 (n ⫽ 43) 4 extractions Mean (SD) P value 81.13 (3.92) 85.40 (5.96) 79.84 (3.86) 82.77 (4.67) 0.108 0.020* 76.74 (2.75) 107.71 (6.32) 69.68 (4.40) 50.81 (4.60) 74.52 (2.83) 104.03 (5.33) 67.52 (4.54) 48.03 (4.02) 0.000* 0.003* 0.020* 0.002* 4.39 (2.81) 5.33 (3.02) 0.115 26.60 (4.94) 32.84 (5.55) 5.66 (3.33) 64.28 (5.68) 30.51 (5.17) 37.24 (5.44) 7.02 (3.38) 65.73 (5.55) 0.000* 0.000* 0.050 0.210 26.11 (9.98) 6.51 (3.95) 28.25 (2.87) 23.48 (2.86) ⫺27.13 (2.66) 27.84 (7.51) 6.83 (3.12) 28.80 (2.63) 23.30 (2.46) ⫺26.66 (3.15) 0.345 0.657 0.333 0.752 0.420 24.74 (6.00) 4.77 (2.37) 38.89 (2.88) ⫺30.95 (2.49) 27.93 (2.21) 25.69 (5.30) 6.13 (2.21) 39.94 (2.77) ⫺29.61 (3.25) 28.88 (2.19) 0.419 0.005* 0.071 0.023* 0.036* 7.21 (2.73) 4.15 (2.82) 3.69 (0.77) 4.04 (1.52) 7.36 (2.67) 4.27 (2.00) 3.81 (0.58) 3.30 (0.94) 0.776 0.812 0.377 0.006* 111.07 (13.32) 6.41 (6.79) 108.51 (13.76) 9.37 (6.73) 0.355 0.034* *Statistically significant; rel, relationship. rate for the former, as was obtained in the previous study.6 There could be some criticism in using Grainger’s TPI20 for evaluation of the pretreatment and posttreat- ment occlusal statuses rather than the more recent and currently mostly used peer assessment rating (PAR) index.26-30 The first reason for this was that the TPI was used in the previous study and because the PAR index Janson et al 865 American Journal of Orthodontics and Dentofacial Orthopedics Volume 133, Number 6 Table III. Results of the multiple regression analysis with FTPI as the dependent variable Variable 1. Extraction protocol 2. Initial age 3. Mandibular crowding 4. Mx1-NA 5. Sex F ⫽ 6.982 R 0.441 0.467 0.497 0.515 0.524 R2 P 0.194 0.000 0.218 0.092 0.247 0.062 0.265 0.127 0.275 0.284 P ⫽ 0.000014 FTPI ⫽ 0.44 (number of extracted premolars) ⫹ 0.16 (initial age) ⫹ 0.11 (mandibular crowding) ⫹ 0.04 (Mx1-NA) ⫹ 0.26 (sex score *) ⫺ 3.12. *Male ⫽ 1; female ⫽ 2. A B Fig 2. The software (Dentofacial Planner version 7.02), used to measure the variables, can create a mean tracing for each group at each stage; therefore, A and B are based on superimpositions of these mean tracings to illustrate pretreatment and posttreatment differences between the groups. A, Superimposition on the sella-nasion line at sella of pretreatment mean tracings for group 1 (black) and group 2 (red); B, same superimposition of posttreatment mean tracings for group 1 (black) and group 2 (red). has some limitation in evaluating the posterior segment’s anteroposterior relationship, as pointed out earlier.31-33 To overcome this deficiency, it has been suggested that there should be a different PAR index to separately evaluate Class I, Class II, and Class III malocclusions.34 In this study, an efficient index to evaluate the posterior segment’s anteroposterior discrepancy was crucial because this is where the major differences are between the treatment success rates of these 2 treatment protocols.6,11 The initial cephalometric difference between the groups that could have increased treatment difficulty for the 4-premolar extraction group would be the more vertical growth pattern (FMA and SN.GoGn) of group 2 (Table II).35,36 The apical bases were also statistically larger in group 1 and could have influenced the occlusal success rate. This is why a multiple regression analysis was conducted, with the FTPI as the dependent variable, as will be discussed. The more vertical growth pattern and the more protruded mandibular incisors in group 2 help to explain why these patients were preferably treated with 4-premolar extractions, as usually indicated in these situations.37-39 Nevertheless, more protruded incisors would not affect the occlusal success rates of the 2 treatment protocols. This parameter refers to the relationship of the mandibular incisors to the mandible and the cranial base, and not to the interdental maxillomandibular relationship. The mandibular molars were more anteriorly positioned and had greater dentoalveolar height in group 2. Probably, the anterior positioning of the first molars was a factor for greater crowding in this group. Because group 2 had a greater vertical growth pattern, greater dentoalveolar height would also be expected.40-44 The initial Class II intercanine anteroposterior relationship was statistically greater in group 1 and differs from the previous results in the dental casts that showed similar anteroposterior discrepancies.6 This might have resulted from difficulty in locating the canines in the lateral headfilms.45,46 However, this would increase treatment difficulty in group 1 866 Janson et al and would not help to explain the smaller occlusal success rate of group 2. The more convex skeletal facial profile (NAP) in group 2 was consequent to its statistically nonsignificant greater anteroposterior basal bone discrepancy and greater mandibular retrusion. Although greater facial convexity might be considered less attractive than a straighter profile,47-49 it is unlikely to play a role in the occlusal success rate in the correction of Class II malocclusions. Results of the multiple regression analysis showed that only the extraction protocol was significantly associated with the FTPI (Table III). Other variables that helped to explain the variation in the FTPI were initial age, mandibular crowding, linear anteroposterior position of the maxillary incisors (Mx1-NA), and sex. However, individually, the association of these variables with the FTPI was not statistically significant. These results demonstrate that it is not the cephalometric characteristics that play a primary role in complete Class II treatment success rate but, rather, the treatment protocol. The 4-premolar extraction treatment protocol demands more anchorage reinforcement to correct the anteroposterior molar relationship than the 2-premolar extraction protocol.2,50 Usually, anchorage reinforcement is provided by removable extraoral appliances that require patient compliance. Consequently, the 4-premolar extraction protocol requires more patient compliance than the 2-premolar protocol.51,52 Therefore, the treatment success rate will greatly depend on patient compliance. It is known that malocclusions associated with a vertical growth pattern or a severe skeletal Class II basal relationship have poorer prognoses in orthodontic treatment.35,53-55 This poor prognosis refers to the final esthetic result and not specifically to the occlusal success rate in correcting the posterior segment Class II anteroposterior discrepancy, as previously suggested6,9,56 and as shown by our results. Group 2, with a statistically significant more vertical growth pattern, initially had a more convex facial profile and also ended up similarly; this was less esthetically pleasing than a straighter profile57-60 (Fig 2). Therefore, these results do not contradict any concept but, rather, show that these cephalometric parameters do not influence the occlusal success rate of Class II malocclusions treated with 2- or 4-premolar extraction protocols. When deciding between these 2 protocols, one must remember that these cephalometric variables will influence the esthetic prognosis but not the occlusal success rate. Although it is reasonable that an accentuated vertical facial pattern and a skeletal Class II relationship have poorer prognoses for facial balance, it is American Journal of Orthodontics and Dentofacial Orthopedics June 2008 misleading to think that these factors will also influence the occlusal success rate in complete Class II malocclusions treated by the investigated treatment protocols. Our results show that the most important factor in a better occlusal success rate in the treatment of complete Class II malocclusions is the treatment protocol and not any cephalometric parameter. Therefore, when the clinician must decide between these 2 treatment protocols for a complete Class II malocclusion, the greater difficulty of the 4-premolar extraction protocol will play a greater role in the decision than the cephalometric parameters—ie, growth pattern and apical base discrepancy. CONCLUSIONS The most relevant differences between the groups were that the 4-premolar extraction group had statistically smaller apical base lengths, more vertical facial growth pattern, and greater hard- and soft-tissue convexities at pretreatment than did the 2-premolar extraction group. These different cephalometric characteristics of the groups did not influence the occlusal success rates of the 2 treatment protocols. REFERENCES 1. Cleall JF, Begole EA. Diagnosis and treatment of Class II, division 2 malocclusion. Angle Orthod 1982;52:38-60. 2. Strang RHW. A textbook of orthodontia. Philadelphia: Lea & Febiger; 1950. 3. Rock WP. Treatment of Class II malocclusion with removable appliances. Part 4. Class II, division 2 treatment. Br Dent J 1990;168:298-302. 4. Bishara SE, Cummins DM, Jakobsen JR, Zaher AR. Dentofacial and soft tissue changes in Class II, division 1 cases treated with and without extractions. Am J Orthod Dentofacial Orthop 1995; 107:28-37. 5. Arvystas MG. Nonextraction treatment of Class II, Division 1 malocclusions. Am J Orthod 1985;88:380-95. 6. Janson G, Brambilla AC, Henriques JFC, Freitas MR, Neves LS. Class II treatment success rate in 2- and 4-premolar extraction protocols. Am J Orthod Dentofacial Orthop 2004;125:472-9. 7. Andrews LF. The straight wire appliance. Syllabus of philosophy and techniques. San Diego: Larry F. Andrews Foundation of Orthodontic Education and Research; 1975. 8. Bryk C, White LW. The geometry of Class II correction with extractions. J Clin Orthod 2001;35:570-9. 9. Janson G, Dainesi EA, Henriques JFC, Freitas MR, Lima KJRS. Class II subdivision treatment success rate with symmetric and asymmetric extraction protocols. Am J Orthod Dentofacial Orthop 2003;124:257-64. 10. Kessel SP. The rationale of maxillary premolar extraction only in Class II therapy. Am J Orthod 1963;49:276-93. 11. Janson G, Maria FRT, Barros SEC, Freitas MR, Henriques JFC. Orthodontic treatment time in 2- and 4-premolar-extraction protocols. Am J Orthod Dentofacial Orthop 2006;129:666-71. 12. Chew MT, Sandham A. Effectiveness and duration of two-arch fixed appliance treatment. Aust Orthod J 2000;16:98-103. American Journal of Orthodontics and Dentofacial Orthopedics Volume 133, Number 6 13. Robb SI, Sadowsky C, Schneider BJ, Begole EA. Effectiveness and duration of orthodontic treatment in adults and adolescents. Am J Orthod Dentofacial Orthop 1998;114:383-6. 14. Turbill EA, Richmond S, Wright JL. The time-factor in orthodontics: what influences the duration of treatments in National Health Service practices? Community Dent Oral Epidemiol 2001;29:62-72. 15. Vig KWL, Weyant R, Vayda D, O’Brien KD, Bennett E. Orthodontic process and outcome: efficacy studies—strategies for developing process and outcome measures: a new era in orthodontics. Clin Orthod Res 1998;1:147-55. 16. Buchin ID. Borderline extraction cases. Facial esthetics and cephalometric criteria as the determinants in the extraction decision. Part 2. J Clin Orthod 1971;5:421-34. 17. Kim JC, Mascarenhas AK, Joo BH, Vig KWL, Beck FM, Vig PS. Cephalometric variables as predictors of Class II treatment outcome. Am J Orthod Dentofacial Orthop 2000;118:636-40. 18. Wheeler TT, McGorray SP, Dolce C, Taylor MG, King GJ. Effectiveness of early treatment of Class II malocclusion. Am J Orthod Dentofacial Orthop 2002;121:9-17. 19. Creekmore TD. Where teeth should be positioned in the face and jaws and how to get them there. J Clin Orthod 1997;31:586-608. 20. Grainger RM. Orthodontic treatment priority index. Vital health and statistics, series 2, number 25. Washington, DC: National Center for Health Statistics; 1967. 21. Corruccini RS, Potter RHY. Genetic analysis of occlusal variation in twins. Am J Orthod 1980;78:140-54. 22. Corruccini RS, Whitley D. Occlusal variation in a rural Kentucky community. Am J Orthod 1981;79:250-62. 23. Richardson ME. Late lower arch crowding: the role of the transverse dimension. Am J Orthod Dentofacial Orthop 1995; 107:613-7. 24. Dahlberg G. Statistical methods for medical and biological students. New York: Interscience Publications; 1940. 25. Houston WJB. The analysis of errors in orthodontic measurements. Am J Orthod 1983;83:382-90. 26. Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod 1989;11:309-20. 27. Shaw WC, Richmond S, O’Brien KD, Brook P, Stephens CD. Quality control in orthodontics: indices of treatment need and treatment standards. Br Dent J 1991;170:107-12. 28. Richmond S, Shaw WC, O’Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR index (peer assessment rating): reliability and validity. Eur J Orthod 1992; 14:125-39. 29. Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR index (peer assessment rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod 1992;14:180-7. 30. Richmond S, Andrews M, Roberts CT. The provision of orthodontic care in the general dental services of England and Wales: extraction patterns, treatment duration, appliance types and standards. Br J Orthod 1993;20:345-50. 31. Parkinson CE, Buschang PH, Behrents RG, Throckmorton GS, English JD. A new method of evaluating posterior occlusion and its relation to posttreatment occlusal changes. Am J Orthod Dentofacial Orthop 2001;120:503-12. 32. Al Yami EA, Kuijpers-Jagtman AM, van’t Hof MA. Occlusal outcome of orthodontic treatment. Angle Orthod 1998;68:439-44. 33. Kerr WJS, McColl JH. Use of the PAR index in assessing the effectiveness of removable orthodontic appliances. Br J Orthod 1993;20:351-7. Janson et al 867 34. Hamdan AM, Rock WP. An appraisal of the peer assessment rating (PAR) index and a suggested new weighting system. Eur J Orthod 1999;21:181-92. 35. Fogle LL, Southard KA, Southard TE, Casko JS. Treatment outcomes of growing Class II Division 1 patients with varying degrees of anteroposterior and vertical dysplasias, part 1. Cephalometrics. Am J Orthod Dentofacial Orthop 2004;125:450-6. 36. Vaden JL. Nonsurgical treatment of the patient with vertical discrepancy. Am J Orthod Dentofacial Orthop 1998;113:567-82. 37. Bishara SE, Cummins DM, Jakobsen JR. The morphologic basis for the extraction decision in Class II, division 1 malocclusions: a comparative study. Am J Orthod Dentofacial Orthop 1995;107: 129-35. 38. Vaden JL. Alternative nonsurgical strategies to treat complex orthodontic problems. Semin Orthod 1996;2:90-113. 39. Tweed CH. The application of the principles of the edgewise arch in the treatment of malocclusion. Part I. Angle Orthod 1941;11:5-11. 40. Janson GRP, Metaxas A, Woodside DG. Variation in maxillary and mandibular molar and incisor vertical dimension in 12-yearold subjects with excess, normal, and short lower anterior face height. Am J Orthod Dentofacial Orthop 1994;106:409-18. 41. Schendel SA, Eisenfeld J, Bell WH, Epker BN, Mishelevich DJ. The long face syndrome: vertical maxillary excess. Am J Orthod 1976;70:398-408. 42. Fields HW, Proffit WR, Phillips C. Facial pattern differences in long-faced children and adults. Am J Orthod 1984;85:217-23. 43. Lopez-Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open-bite malocclusion: a longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod 1985;87:175-86. 44. Sassouni V. A classification of skeletal facial types. Am J Orthod 1969;55:109-23. 45. Baumrind S, Frantz RC. The reliability of head film measurements. 1. Landmark identification. Am J Orthod 1971;60:111-27. 46. Vincent AM, West VC. Cephalometric landmark identification error. Aust Orthod J 1987;10:98-104. 47. Gebeck TR, Merrifield LL. Orthodontic diagnosis and treatment analysis— concepts and values. Part I. Am J Orthod Dentofacial Orthop 1995;107:434-43. 48. Turkkahraman H, Gokalp H. Facial profile preferences among various layers of Turkish population. Angle Orthod 2004;74: 640-7. 49. Scott SH, Johnston LE Jr. The perceived impact of extraction and nonextraction treatments on matched samples of African American patients. Am J Orthod Dentofacial Orthop 1999; 116:352-60. 50. Nangia A, Darendeliler MA. Finishing occlusion in Class II or Class III molar relation: therapeutic Class II and III. Aust Orthod J 2001;17:89-94. 51. Graber TM. Current orthodontic concepts and techniques. Philadelphia: Saunders; 1969. 52. Perez CA, Alba JA, Caputo AA, Chaconas SJ. Canine retraction with J hook headgear. Am J Orthod 1980;78:538-47. 53. Musich DR. Orthodontics and orthognathic surgery: principles of combined treatment. In: Graber TM, Vanarsdall RL, editors. Orthodontics: current principles and techniques. St Louis: Mosby; 1994. 54. Tweed CH. Evolutionary trends in orthodontics: past, present and future. Am J Orthod 1953;39:81-108. 55. Tweed CH. The Frankfort-mandibular incisor angle (FMIA) in orthodontic diagnosis, treatment planning and prognosis. Angle Orthod 1954;24:121-69. 868 Janson et al 56. King GJ, McGorray SP, Wheeler TT, Dolce C, Taylor M. Comparison of peer assessment ratings (PAR) from 1-phase and 2-phase treatment protocols for Class II malocclusions. Am J Orthod Dentofacial Orthop 2003;123:489-96. 57. Paquette DE, Beattie JR, Johnston LE Jr. A long-term comparison of nonextraction and premolar extraction edgewise therapy in “borderline” Class II patients. Am J Orthod Dentofacial Orthop 1992;102:1-14. American Journal of Orthodontics and Dentofacial Orthopedics June 2008 58. Shelly AD, Southard TE, Southard KA, Casko JS, Jakobsen JR, Fridrich KL, et al. Evaluation of profile esthetic change with mandibular advancement surgery. Am J Orthod Dentofacial Orthop 2000;117:630-7. 59. De Smit A, Dermaut L. Soft-tissue profile preference. Am J Orthod 1984;86:67-73. 60. Kerr WJ, O’Donnell JM. Panel perception of facial attractiveness. Br J Orthod 1990;17:299-304.