The Common Risk Factor Approach (CRFA)
advertisement

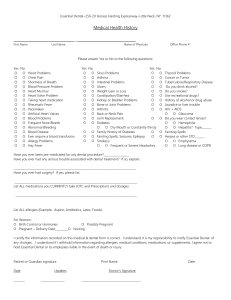
The Common Risk Factor Approach (CRFA) to Oral Health Promotion Carol Chapman, CDA, RDH, MS Continuing Education Units: 2 hours Online Course: www.dentalcare.com/en-US/dental-education/continuing-education/ce435/ce435.aspx Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or procedures into their practice. Only sound evidence-based dentistry should be used in patient therapy. The subsequent information will provide a synopsis and description of the major modifiable behavioral risk factors for chronic and oral disease and how these risk factors can be addressed in a cohesive health promotion program. Upon the completion of this course, dental professionals will be able to create an oral health promotion program using the CRFA. Conflict of Interest Disclosure Statement • Ms. Chapman reports no conflicts of interest associated with this work. ADA CERP The Procter & Gamble Company is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at: http://www.ada.org/cerp Approved PACE Program Provider The Procter & Gamble Company is designated as an Approved PACE Program Provider by the Academy of General Dentistry. The formal continuing education programs of this program provider are accepted by AGD for Fellowship, Mastership, and Membership Maintenance Credit. Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement. The current term of approval extends from 8/1/2013 to 7/31/2017. Provider ID# 211886 1 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Overview The Common Risk Factor Approach (CRFA) is a method used to create cross-disciplinary health promotion programs sharing common risk factors for disease. Many of the behavioral risk factors negatively impacting oral health also have a detrimental effect on overall health. Addressing risk factors in a collaborative health promotion program is not only an efficacious approach to health; it highlights the important mouth-body connection. The subsequent information will provide a synopsis and description of the major modifiable behavioral risk factors for chronic and oral disease and how these risk factors can be addressed in a cohesive health promotion program. Learning Objectives Upon completion of this course, the dental professional should be able to: • Define the Common Risk Factor Approach (CRFA). • Identify common risk factors for chronic and oral disease. • Explain how social determinants affect disease onset and progression. • Describe the levels of disease prevention. • Explain the role of oral bacterial plaque in the mouth-body connection. • Describe the affect of modifiable behaviors on oral disease. • Provide a rationale for using the CRFA. • Give examples of CRFA in practice. • Create an oral health promotion program using the CFRA. Course Contents Introdcution • Introduction • Risk Factors and the Common Risk Factor Approach (CRFA) to Disease • History of the Common Risk Factors for Chronic Diseases Framingham Heart Study • Determinants of Health Explanation of the Impact of Social Determinants on Risk Factors for Disease • Levels of Prevention Identification and Comparison of "Upstream" and “Downstream” Health Interventions • The Mouth-Body Connection • The Four Major Modifiable Behavioral Risk Factors Tobacco Use, Harmful Alcohol Use and an Unhealthy Diet as Risk Factors for Oral and Systemic Disease Oral Biofilm as a Risk Factor for Cancers, Cardiovascular Diseases, Diabetes and Respiratory Disease • CRFA in Action Examples of CRFA in Practice •Conclusion • Course Test Preview • References • About the Author The United States is an aging society. In 2009, the number of people 65 years of age or older numbered 39.6 million. By 2030, there will be approximately 72.1 million older Americans.1 With the aging population comes an increase in chronic and degenerative diseases. Chronic diseases often emerge later in life as a result of years of exposure to detrimental behavioral risk factors. Addressing these detrimental modifiable behaviors at any stage in life will greatly reduce the burden chronic and degenerative diseases have on our society. Risk Factors and the Common Risk Factor Approach (CRFA) to Disease Definition of a Risk Factor The World Health Organization (WHO) describes a risk factor as “any attribute, characteristic or exposure of an individual that increases the likelihood of developing a disease or injury.”2 Identification of Common Risk Factors for Chronic Non-communicable Diseases (NCDs) and Oral Disease According to the WHO, use of tobacco, harmful alcohol use, an unhealthy diet, and poor oral 2 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Figure 1. The Four Major Chronic Noncommunicable Diseases (NCDs). Figure 2. Framingham Heart Study. 5 8 hygiene are risk factors for oral diseases.3 These factors are also linked to cancers, cardiovascular diseases, diabetes and respiratory diseases, the four major chronic non-communicable diseases (NCDs). Annually, NCDs account for almost twothirds of deaths worldwide and are the number one cause of disability.4 NCDs are long-lasting conditions that cannot be cured but can be controlled. diseases. Mid twentieth century, with the emergence and utilization of vaccines and antibiotics, infectious diseases came under control and were replaced by an upsurge in chronic and degenerative diseases. Researchers were discovering a substantial increase in the number of men diagnosed with cardiovascular disease (CVD).6 This upsurge shifted the focus of epidemiologic studies to the little known etiologic factors related to emerging chronic and degenerative diseases. Description of the CRFA Designing health promotion programs with common risk factors for disease, such as NCDs and oral diseases, is the focus of applying the Common Risk Factor Approach (CRFA) to oral health promotion. ‘Killing two birds with one stone’ is an apt idiom for the efficacious method of CRFA. Framingham Heart Study One of the most famous studies of the time, the Framingham Heart Study, was a longitudinal cohort study undertaken in Framingham, MA. It began in 1948 and continues today. This unique study examined the health determinants, also known as the risk factors, associated with chronic disease. History of the Common Risk Factors for Chronic Diseases Researchers recruited 5,209 male and female volunteers from 28 to 62 years of age to assess common factors associated with the development of CVD.7 Information from physical examinations Until the 1950s, epidemiologic research concentrated on the eradication of infectious 3 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Figure 3. Dahlgren and Whitehead's Model of the Social Determinants of 9 Health. and lifestyle interviews were analyzed using multivariate regression models. These models were able to identify specific risk factors contributing to the overall risk of CVD. Since 1948, surviving subjects have returned every two years for physical examinations and laboratory tests. The second generation, the children and their spouses of the original cohorts, were enrolled in 1971. In 2002 a third generation, the grandchildren of the original cohort were enlisted. This first of a kind study enlightened the medical community to the multifactorial features of chronic and degenerative diseases. Prior to this study many CVDs, such as arthrosclerosis, were seen as a natural part of the aging process. “circumstances in which people are born; grow up, live, work, and age, as well as the systems put in place to deal with illness.”10 Described as “the causes of the causes,”11 these determinants affect the ability of an individual to attain and maintain health. The wider arches involve issues such as health policies, access to care, and conditions under which people live and work. Explanation of the Impact of Social Determinants on Risk Factors for Disease Determinants of health can be addressed at an individual level or at a community level. In dentistry, most health promotion is addressed at an individual level in hopes of changing individual lifestyle factors. For health promotion, including dental health promotion, to have a more farreaching affect it should be directed at the wider sphere of determinants, such as the social and community networks. To reduce the negative impact of detrimental modifiable behavioral risk factors, more emphasis needs to be placed on the social environments in which these negative behaviors arise. Determinants of Health Description and Identification of the Social Determinants for Disease Health is an amalgamation of many factors. The Dahlgren and Whitehead's model (1991) depicted in Figure 3 shows a core of individuals grouped together with some of the non-modifiable risk factors for disease such as age, gender and heredity.9 Radiating from the center are concentric arches of the determinants, the risk factors, affecting health. Dahlgren and Whitehead described these layers as the “policy rainbow.” These determinants not only interact with the individual but interact with each other in a complex relationship. The wider bands of determinants, those outside the social and community networks, are characterized as the Levels of Prevention Identification and Description of the Levels of Prevention Primary, secondary and tertiary are the three levels of prevention used to avert and control diseases in populations. Primary prevention is targeted at reducing the incidence of disease. It focuses on curtailing risk factors. Primary 4 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Figure 4. The Natural History Disease Model. 14 Figure 5. Upstream Downstream Dental Healthcare. prevention is the most effective and efficient form of healthcare. Health promotion plays a key role in primary prevention by “enabling people to increase control over the determinants of health and thereby improve their health.”12 Secondary prevention is directed at the presymptomatic or early stage of disease, decreasing the number of existing cases of disease. Secondary prevention reduces the prevalence of disease. Limiting disability and improving function following disease or its complications is the goal of tertiary prevention. 14 in the river upstream? Health promotion is an upstream approach aimed at limiting the need for downstream, or secondary and tertiary prevention. The Mouth-Body Connection The mouth and body are viewed as separate biologic entities by many Americans. Traditionally medicine and dentistry have been seen as fields unrelated to each other. Medicine and dentistry are studied in different schools and have separate professional associations but both professions are related by human anatomy. Published in 2000, Oral Health in America: A Report of the Surgeon General was the first time a Surgeon General addressed the important connection between oral health and general health.15 The report stated that “oral health is a critical component of overall health and must be included in the provision of health care and the design of community programs.” David Satcher, the former Surgeon General, in the preface of Oral Health in America advocated for the construction of a “framework for action that integrates oral health into overall health.”16 Identification and Comparison of “Upstream” and “Downstream” Health Interventions Primary prevention has been referred to as treating people ‘upstream.’ It is a term attributed to John McKinlay, a medical sociologist. He tells a tale of a man standing by a swiftly running river when a drowning person floats past. The man jumps in the river and rescues the individual. No sooner had he rescued that person when another drowning individual comes floating by. Repeatedly the man rescues and revives drowning people. The man becomes so involved in rescuing drowning people that he overlooks the most important factor, who is pushing people The WHO declares, “Oral health promotion and oral disease prevention should embrace what is termed ‘the common risk factor approach,’ leading 5 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 to the integration of oral health promotion into broader health promotion.”17 International and national organizations agree the CRFA framework is the most effective method for health promotion. disorders, especially cervical caries.24 When smoking is accompanied by alcohol consumption, it produces an even greater negative effect. People who smoke and also drink alcohol have a risk of oral cancer greater than the risk of those who only smoke or those who only drink alcohol.25 The Four Major Modifiable Behavioral Risk Factors Healthy People is a nationwide disease prevention and health promotion plan created by the United States Department of Health and Human Services (DHHS).26 Every ten years Healthy People sets out goals and objectives aimed at attaining health for Americans for the decade to come. There are 42 topic areas in Healthy People 2020. One of these areas addresses tobacco use. Of the 20 objectives directed at tobacco use, objective TU-10 seeks to “Increase tobacco cessation counseling in health care settings.”27 More specifically, TU-10.3 speaks to dentistry and the obligation dental professionals have to address tobacco use. The intention of the objective is to, “Increase tobacco cessation counseling in dental care settings.” Healthy People realizes dental health care providers are in an ideal position to help current tobacco users to quit and to provide incentives to prevent the onset of tobacco use. It is well-documented tobacco use, harmful alcohol use, and an unhealthy diet are risk factors for cancers, CVDs, respiratory diseases and diabetes.18 The role oral biofilm plays in the development of NCDs is a recently studied relationship.19 Attaching a specific risk factor to a specific NCD is an impossible task. First, there is often a lag time between exposure to a risk factor and the development of a health condition. Secondly, there is usually more than one risk factor associated with a health condition, and thirdly, the exposure to risk factors is often linked to more than one health condition. Risk factors act synergistically to accelerate the onset or worsen already existing NCDs. Tobacco Use, Harmful Alcohol Use and an Unhealthy Diet as Risk Factors for Oral and Systemic Disease Tobacco Use All forms of tobacco use pose a threat to oral health as well as general well-being. The Centers for Disease Control and Prevention (CDC) affirms “tobacco use is the leading preventable cause of disease, disability and death”20 and is the number one risk factor for NCDs. The CDC points to cigarette smoking as being responsible for “more than 480,000 deaths per year in the United States, including an estimated 41,000 deaths resulting from secondhand smoke exposure. For every person who dies from a smoking-related disease, about 30 more people experience at least one serious illness from smoking.”21 Statistics from the WHO project “tobacco use will kill 1 billion people worldwide in the 21st century.”22 Harmful Alcohol Use Like tobacco, excessive intake of alcohol is also a risk factor for NCDs. Harmful alcohol use, as defined by the National Institute of Alcohol Abuse and Alcoholism is, “Failure to fulfill major role obligations at work, school, or home, continued drinking even in situations where it is physically hazardous, recurrent alcohol–related legal problems and continued drinking despite persistent or recurrent social or interpersonal problems it may cause.”28 The CDC states, “Excessive alcohol use includes binge drinking, heavy drinking, any alcohol use by people under the minimum legal drinking age, and any alcohol use by pregnant women.”29 The CDC goes on to say “heavy drinking for men is defined as consuming 15 drinks or more per week. For women, heavy drinking is defined as consuming 8 drinks or more per week.” Related to oral health, tobacco use is associated with stained teeth, reduction of taste, periodontal disease, oral cancer, decreased wound healing and a decrease in the body’s immune response to infection.23 In addition, long-term smoking is associated with reduced salivary flow rate (SFR) leading to an increase in oral and dental Alcohol abusers have a much higher rate of periodontal disease, decayed teeth, and precancerous lesions.30 Alcohol abuse also delays the healing process and negatively effects blood clotting factors. Tooth decay is related to the high 6 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 sugar and acid content in many alcoholic drinks. Alcohol abuse can also inhibit proper oral hygiene measures. Failing to brush and floss teeth regularly can result in tooth decay and periodontal disease. The Oral Cancer Foundation states, “The dehydrating effect of alcohol on cell walls enhances the ability of tobacco carcinogens to permeate mouth tissues.”31 In addition, “nutritional deficiencies associated with heavy drinking can lower the body’s natural ability to use antioxidants to prevent the formation of cancers.” Lastly, the Oral Cancer Foundation suggests cirrhosis of the liver leads to a change in texture of throat and esophagus tissue that may increase the likelihood of developing oral cancer. The body needs the right kind of fat, mainly monounsaturated and polyunsaturated fatty acids and very limited amounts of saturated fats. Poultry, olive and canola oil and plant foods like nuts and avocados are examples of foods containing monounsaturated fats. Fatty fish such as salmon and mackerel, as well as corn and soybean oils contain polyunsaturated fats. Saturated fats found in meat and dairy products such as cheese, butter, and milk should be limited. Too much saturated fat may elevate blood cholesterol thereby increasing the risk for CVDs as well as some cancers. The American Heart Association (AHA) recommends less than 30% of total calories for the day come from fat and only 10% of the 30% should come from saturated fat.37 Unhealthy Diet Unhealthy diets are those that have increased fat, sugar and sodium and are low in the intake of fruit and vegetables.32 Dietary excess, termed overnutrition, are the intake of excessive amounts of nutrients and are a form of malnutrition. Overnutrition can result in obesity and contribute to the NCDs of cancer, CVD, and diabetes as well as dental caries.33 Limiting the intake of foods that have refined grains, saturated fats, and added sodium and sugars is the healthiest choice. Following the Dietary Guidelines for Americans, developed by the U.S. Department of Agriculture (USDA) is the soundest choice for overall nutrition.34 ChooseMyPlate.gov, established by the USDA in conjunction with the DHHS, is an excellent website to evaluate a patient’s diet for nutritional counseling. It is also a resource for nutritional information to use in a health promotion program. Sugar Sugar is a carbohydrate. The body uses carbohydrates to make glucose, the fuel for the body’s cells.38 Glucose is blood sugar converted from glycogen stored in the liver and muscles; when released into the bloodstream, it provides energy for the cells. Insulin from the pancreas helps control the amount of glucose in the body. There are varying amounts of carbohydrates in food products. The glycemic index is used to measure the effect of foods containing carbohydrates on blood glucose level. The lower the glycemic index the slower the digestion process. This results in a gradual release of glucose into the bloodstream. A food with a high glycemic index causes the hormone insulin to be released to reduce the glucose level. Less than 100 mg/dL when fasting and less than 140 mg/ dL two hours after eating is considered a normal sugar level.39 The more glucose in the body, the more insulin is released into the bloodstream. A consistently elevated glucose level puts individuals at risk for insulin resistant type 2 diabetes and CVD. Fat Some intake of fat is needed in the diet. Fats are required for many important functions in the body. Fats insulate our body, protect vital organs, act as messengers, help proteins do their jobs, and start chemical reactions that help control growth, immune function, reproduction and other aspects of basic metabolism.35 Problems arise when excessive amounts of fat, especially saturated fats, are consumed. Fat contains 9 calories per gram, compared to protein and carbohydrates containing only 4 calories per gram.36 This means smaller amounts of energy-dense fats should be eaten. “There is convincing evidence, collectively from human intervention studies, epidemiological studies, animal studies and experimental studies, for an association between the amount and frequency of free sugars intake and dental caries.”40 Added sugar is found in many processed foods. There is no nutritional benefit from eating foods with added sugar. Research shows the average American consumes 22 teaspoons of 7 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 added sugar a day.41 The AHA recommends limiting sugar intake to no more than 100 calories per day (about 6 teaspoons) for women and no more than 150 calories per day (about 9 teaspoons) for men. One regular 12-ounce soda contains 9 teaspoons of sugar. Drinking one regular soda a day would put most men and all women over the recommended daily limit. Products that list any type of sugar as the first or second ingredient should be avoided. National Cancer Institute, there are more than 100 different types of cancer. Worldwide, deaths from cancer are estimated to reach 13.1 million by 2030 with about 30% of cancers attributable to modifiable behavioral risk factors. Cancer is the result of cell mutation. The determined life span of cells is regulated by messages received from the genes inside the cell. Certain genes tell the cell how to make different proteins. Some proteins signal the cell to multiply; others encourage the cell to stop multiplying. Mutated cells send incorrect messages leading to an increased production of proteins that signal abnormal cell proliferation, diminished cell differentiation, and inhibition of cell death. The result is a tumorous growth. Sodium Many Americans are unaware of how much dietary sodium they are eating. Excessive intake of sodium increases the risk for hypertension, a major contributor to CVD.42 Seventy-five percent of sodium Americans consume comes from processed and restaurant foods.43 The USDA recommendation for daily sodium intake is 2,400 mg. For persons 51 years of age and older and for persons of any age who are African American or have hypertension, diabetes, or chronic kidney disease the recommended daily intake is 1,500 mg. About half of the U.S. population, including children, and the majority of adults, should not exceed 1,500 mg of sodium a day. Close to 43,250 Americans will be diagnosed with oral or pharyngeal cancer this year. It will cause over 8,000 deaths, killing roughly 1 person per hour, 24 hours per day. Of those 43,250 newly diagnosed individuals, only slightly more than half will be alive in 5 years.”46 Poor oral hygiene has been recognized as a possible risk factor for oral and pharyngeal cancer.47 One theory suggests chronic infection, such as periodontitis, may promote normal cells to mutate. The inflammatory process signals cells to proliferate. The more proliferation that occurs, the more chance there is for mutation. The mutation of cells takes a long time to occur so eliminating risk factors, such as poor oral hygiene, can halt the process. Oral Biofilm as a Risk Factor for Cancers, Cardiovascular Diseases, Diabetes and Respiratory Disease Oral Biofilm In 2000, the Oral Health in America: A report of the Surgeon General reported, “You are not healthy without good oral health.”16 The connection between oral health and general health is a recently studied association. Oral biofilm begins with the formation of the pellicle and ends with the complex formation of mature biofilm. Recent research suggests the host response to pathogenic organisms contained in oral biofilm may be a risk factor for the four major NCDs, cancer, CVDs, respiratory diseases and diabetes.44 A new association between oral cancer and oral hygiene was addressed in a recently published study in the Cancer Prevention Research, a journal of the American Association for Cancer.48 Researchers found inadequate oral health to be correlated with oral human papillomavirus (HPV) infection. The study controlled for the number of oral sex partners and smoking and still discovered that inadequate oral health was an independent risk for oral HPV infection. Results showed HPV infection was 55% higher among those self-reporting poor to fair oral health. According to one of the researchers, Dr. Thanh Cong Bui, “Poor oral health is a new independent risk factor for oral HPV infection. The good news is, this risk factor is modifiable by maintaining good oral hygiene and good oral health, and one Cancer As defined by the National Cancer Institute, “cancer is a term used for diseases in which abnormal cells divide without control and are able to invade other tissues.”45 Cancer is not just one disease but various diseases named according to the site of origin. According to the 8 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 can prevent HPV infection and subsequent HPVrelated cancers.” respiratory infection whereas COPD is a longstanding chronic infection. These infections can be severely debilitating and are a major cause of death. Chronic lower respiratory disease is the third leading cause of death in the United States.52 Cardiovascular Disease When oral hygiene is inadequate, undisturbed bacterial plaque produces harmful toxins that stimulate an acute inflammatory response known as gingivitis. This inflammatory reaction requires constant stimulation to remain active. If the bacterial plaque is removed, the gingivitis subsides. If it is not removed, gingivitis can develop into a chronic inflammatory response, periodontitis. Not only are the teeth’s supporting structures destroyed in the presence of chronic inflammation but research suggests that CVDs may be associated with the inflammatory response. The two most common types of pneumonia are community-acquired pneumonia (CAP) and nosocomial, also known as hospital-acquired, pneumonia. CAP is not usually associated with oral microorganisms but nosocomial pneumonia is linked to microorganisms found in the oral cavity. Patients at the highest risk for nosocomial pneumonia are patients who are unable to perform self-oral care such as medically compromised, institutionalized or hospitalized patients. Inflammation is a complex defense mechanism producing a variety of cellular and chemical reactions. Bacteremia occurs when bacteria from the mouth enter the bloodstream via epithelial tissue. The more inflammation present, the more permeable the epithelial tissue becomes. Several species of bacteria related to periodontitis, in particular Porphyromonas gingivalis, have been found in the atheromatous plaque in the arteries of the heart.50 Atheromatous plaque is the yellow coating on the innermost surface of an artery produced by lipid deposits. These deposits cause arteries to narrow, reducing blood flow, and may result in a heart attack or stroke. Inflammatory mediators, the cytokines interleukin-1 beta (IL‑1), interleukin-6 beta (IL-6) and tumor necrosis factor (TNF), are produced by a broad range of cells and can enter circulating blood, attach to the atheromatous plaque in the arteries, and be a factor in clot formation. These proteins are also thought to interact with the vessel wall, contributing to the swelling and narrowing of the heart’s arteries. The inflammation in the atheromatous plaque is also promoted by C-reactive protein (CRP), a marker for heart disease, as well as the protein fibrinogen produced in the liver. Fibrinogen and CRP are also associated with blood clots formation. COPD is a pulmonary disease affecting airflow.53 People with COPD often have compromised protective systems in their lungs making it difficult to eliminate inhaled oral pathogens. If oral pathogens are not expelled from the lungs, the result may be proliferation of the bacteria resulting in lung infections or worsening already existing lung condition. The host response to periodontal infection has four mechanisms associated with the origination and development of respiratory disease. First, the protective mechanisms of the lungs usually prevent colonization of inhaled oral pathogens. But if a large number of microorganisms are inspired, a particularly virulent pathogen is inhaled or the host has a suppressed immune system, infection can occur. Second, enzymes in saliva associated periodontal disease may alter the lungs mucosal surfaces promoting the adhesion and proliferation of inspired bacteria. Third, enzymes may break down salivary pellicles on pathogens and deter their clearance from the lungs. Lastly, cytokines derived from periodontal tissues may alter the epithelium in the lungs encouraging infection from inhaled pathogens. Appropriate oral hygiene is essential for susceptible populations such as individuals with compromised respiratory function and immunocompromised individuals. Respiratory Disease Research studies suggest periodontal disease is a risk factor for respiratory diseases such as pneumonia and chronic obstructive pulmonary disease (COPD).51 Pneumonia is an acute Diabetes Diabetes mellitus is a metabolic disorder associated with the body’s inability to produce 9 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 CRFA in Action insulin or to produce enough insulin.54 Either situation results in elevated levels of blood glucose. Type 1, Type 2 and gestational diabetes are the three major categories of diabetes. Gestational diabetes, by definition, is diabetes diagnosed during pregnancy. Gestational diabetes usually subsides following delivery but women identified with gestational diabetes are at an increased risk of developing type 2 diabetes later in life. Type 1 diabetes is an autoimmune disease where the immune system attacks and destroys the insulin-producing beta cells in the pancreas. By far, approximately 95% of persons in the U.S. with diabetes, have type 2 diabetes. In the past, type 2 diabetes was referred to as adult-onset diabetes. This term is no longer applicable due to the dramatic increase in adolescents and children being diagnosed with type 2 diabetes.55 The root cause of this increase is a sedentary lifestyle in combination with an unhealthy diet. The Rationale for Using the CRFA to Promote Oral Health The common risk factors between general and oral health provide a rationale for dental health professionals to partner with community members to develop health promotion programs that will benefit a multitude of individuals. Dental health professionals provide oral care instruction and education to patients all the time. Although providing this information on a one-to-one basis is certainly beneficial, the challenge is to take that information to a wider community audience. A community health promotion program is a win-win for dental health providers as well as the recipients of the program. Dental health professionals have an opportunity to promote dentistry and the important position dentistry holds in the community, and the recipients are the beneficiaries of a wealth of health care information. Diabetes affects and is affected by several oral conditions and diseases. Xerostomia is often a symptom of undetected diabetes. Burning mouth syndrome, taste disorders, infections, such as candidiasis, and dental decay are all related to xerostomia. Diabetes can also lower systemic resistance to infection and make already existing oral health problems more severe. Examples of CRFA in Practice Women, Infants, and Children (WIC) Program Dental health professionals can partner with a local Women, Infants, and Children (WIC) program. WIC is a special federal supplemental nutrition program. It serves low-income women, infants and children up to age five who are at nutritional risk.58 Dental health intervention can be as simple as providing pamphlets to a center on oral care for infants and children as well as oral care during pregnancy. Participants in the WIC program are individuals with some of the greatest need for information on nutrition and oral care. Children from families with a lower socioeconomic status are at the highest risk for dental decay. Pamphlets should be culturally sensitive and provided in several languages to meet the needs of the population being served. A step further would be to set up a booth at the WIC center a day or two a month for several hours to interact with the WIC participants. Dental assisting, dental hygiene, or dental students could use this opportunity to fulfill community service hours mandated by their educational programs. Being present at the facility allows time for students to demonstrate with typodonts the correct brushing and flossing techniques and to answer questions WIC participants may have about dental issues. According to the CDC periodontal disease is more common in people diagnosed with diabetes. Adults, aged 45 years or older, with poorly controlled diabetes, were 2.9 times more likely to have severe periodontitis than those without diabetes.56 The likelihood increases to 4.6 times among individuals who smoke and have poorly controlled diabetes. Many studies suggest that oral bacteria and the inflammation associated with periodontitis play a role in the ability to control blood sugar levels. Conversely, poor glycemic control is related to elevated levels of inflammatory mediators. Research suggests reduction of oral inflammation may have a positive effect on the diabetic condition.57 Individuals with diabetes and periodontal disease have two chronic conditions, each of which may affect the other. The solution to control of both is daily brushing and flossing, frequent professional re-care appointments, and educational reinforcement. 10 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Depending on the regulations of the center, fluoride varnish could be applied to the children attending with their mothers. revisited. The newest trend is e-cigarettes. The risks of using this type of device are not wellknown but the addictive potential of nicotine is very well-documented. The nicotine cartridges used in the e-cigarettes are flavored and appear to be harmless to young adults. Intervention by a dental health professional on the risks of e-cigarettes would be beneficial. See dentalcare. com course Electronic Cigarettes the Past, Present and Future. Diabetes Many communities sponsor Juvenile Diabetes Research Foundation (JDRF) walks throughout the year to raise money and awareness for what was formerly termed juvenile diabetes. Juvenile diabetes is now known as type 1 diabetes. Although the etiology of type 1 and type 2 diabetes differs, the oral conditions suffered by persons with either type of diabetes are the same. Dental health professionals could distribute information on oral care and the risk factors associated with diabetes and oral disease. Information on JDRF walks can be found at http://www2.jdrf.org/site/ PageServer?pagename=walk_homepage. The CDC has developed a model entitled, “the Coordinated School Health Program (CSHP).” This model serves as a guide to meet the health and safety needs of K-12 students. The CSHP model has eight components designed to encourage health and learning. Improving the oral health of school children can be integrated into each of the eight components of the CSHP model. A more detailed description of how this can be accomplished is provided at http://www. astdd.org/docs/BPA2attachmentschoolcshpB.pdf. Schools Although volunteering is not a solution to the lack of access to dental care that many children in the U.S. experience, volunteering during February, Children’s Dental Health Month, at a local elementary school to give a presentation on oral health benefits the children. Covering several topics such as nutrition, brushing and flossing, and visiting the dental office is an introduction for many children to basic oral care. Make it a fun interactive experience. Dental professionals can dress in costumes; create a nutrition game or make-up a brushing song. There are also many other times during the year a school would accommodate a presentation and work with the dental health professionals. Special Programs Your community may have an adult center where individuals with learning disabilities or special needs attend a daytime program. Presenting a program to these persons is always welcomed. Mentally and physically challenged adults are often in the greatest need of instruction. If caregivers provide oral care for the adult, if possible, instruction and written information should also be given to the caregivers. The Parent Teacher Association (PTA) may be the place to promote the very controversial topic of HPV vaccines. According to the CDC, the HPV vaccines are given as a series of three shots over six months.60 Cervarix and Gardasil are vaccines that protect against cervical cancers in women. Only one vaccine, Gardasil, is offered for males. For the best protection, all three doses have to be given and have to have time to create an immune response before being sexually active with another person. The vaccination is recommended for preteens at about age 11 or 12 years. The same types of HPV that infect the genital areas can infect the mouth and throat causing cancers of the head and neck area. Recent studies have associated HPV with a high risk of tonsilar cancer.61 There are also special needs schools and programs that often get overlooked during Children’s Dental Health Month. Whether your community has schools with special needs classes or there is a separate school for special needs students, it is always appreciated by the school staff when someone takes the time to cater to the needs of the students in those programs. Middle and high school presentations could focus on tobacco use. The dangers of smoking and using chew tobacco have been emphasized for many years but as each new generation reaches middle and high school age the topics need to be 11 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Figure 6. Integrating Oral Health into the Coordinated school Health Program Model. Celebrations Halloween is a time of year when children receive a large supply of candy. A dental office could have a candy exchange. The office could set up a program where candy could be exchanged for a small monetary reward or gift. The exchange could be by the pound or by a designated number of pieces of candy. The candy could then be donated to our military troops overseas. Organizations such as Operation Gratitude gladly accept donations. Information about Operation Gratitude can be found at http://www. operationgratitude.com/. 59 When children come to the office for the exchange, they could receive a toothbrush, floss and information on oral care. This information can also be shared with the accompanying adult. The staff might also give a tour of the office. A candy exchange promotes good nutrition, proper oral hygiene and also promotes the office. Conclusion For the most part, dental health promotion has been isolated from other health promotion initiatives. Clinical dental preventive and educational approaches alone can only achieve 12 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 limited results. The dental profession needs to adopt an integrated common risk factor approach with groups concerned about reducing NCDs. Dental health professionals are in a position to couple with community stakeholders to address modifiable behavioral risk factors with appropriate health promotion information. Taking this combined approach can greatly reducing the morbidity and mortality from chronic diseases and decrease the incidence of oral diseases. Although many of the suggestions for coupling with community stakeholders are volunteer initiatives, for real change to occur changes should be long-term sustainable programs. Dental health professionals can work within and between their professional organizations to find enduring solutions. 13 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 Course Test Preview To receive Continuing Education credit for this course, you must complete the online test. Please go to: www.dentalcare.com/en-US/dental-education/continuing-education/ce435/ce435-test.aspx 1. Which statement best describes a risk factor? 2. Chronic non-communicable diseases can be cured. Worldwide, the number one cause of disability is chronic non-communicable diseases. a. b. c. d. a. b. c. d. The etiology of a disease. A feature that predicts the course of a disease. An attribute that increases the probability of disease The intervention to cease the worsening of a disease. Both statements are true. Both statements are false. The first statement is true and the second statement is false. The second statement is true and the first statement is false. 3. Which type of research study is the Framingham Heart Study? 4. Risk factors are also known as __________ of health. 5. Which risk factor is modifiable? 6. Which type of prevention is directed at the presymptomatic or early stage of disease? 7. Tertiary prevention reduces the negative impact of an already established disease by restoring function and reducing disease-related complications. Tertiary prevention is the most effective and efficient form of healthcare a.Cross-sectional. b. Longitudinal cohort. c. Retrospective case-control. d. Randomized controlled trial. a.rates b.agents c.values d.determinants a.Age b.Gender c.Heredity d. Oral biofilm a.Primary b.Secondary c.Tertiary d.Quaternary a. b. c. d. Both statements are true Both statements are false The first statement is true; second statement is false The first statement is false; second statement is true 14 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 8. Which was the first to address the important connection between oral health and general health? a. b. c. d. 9. Healthy People 2020 World Health Organization The Framingham Heart Study Oral Health in America: A Report of the Surgeon General According to the CDC, which is the number one risk factor for NCDs? a. b. c. d. Tobacco use Poor oral hygiene An unhealthy diet Harmful alcohol use 10. Which entity provides 10-year national objectives for improving the health of all Americans? a. b. c. d. Healthy People Institute of Medicine World Health Organization Centers for Disease Control and Prevention 11. All of the following have increased rates of occurrence due to harmful alcohol use except one. Which one is the exception? a.Malocclusion b. Decayed teeth c. Periodontal disease d. Precancerous lesions 12. Saturated fats are found in fatty fish such as salmon. Polyunsaturated fats are founds in dairy products such as cheese. a. b. c. d. Both statements are true Both statements are false The first statement is true and the second statement is false The second statement is true and the first statement is false 13. The American Heart Association (AHA) recommends limiting sugar intake to no more than __________ calories per day for women. a.50 b.100 c.150 d.500 14. According to the USDA, which is the recommended daily amount of sodium for an individual with hypertension? a. b. c. d. 1,000 1,500 2,000 2,400 mg mg mg mg 15. Which acute respiratory disease is associated with the inhalation of oral pathogens? a.Asthma b.COPD c.Tuberculosis d. Nosocomial pneumonia 15 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 16. Which type of cell is destroyed in type 1 diabetes? a.Beta b.Delta c.Alpha d.Langerhans 17. Which undertaking utilizes a community approach to oral health promotion? a. b. c. d. Application of fluoride varnish at a WIC center Instructing a patient in the correct flossing technique Providing oral care pamphlets in the dental office reception area Performing an oral cancer screening during a recall prophylaxis appointment 18. Which HPV vaccine is offered to males? a.Gardasil b.Cervarix c.Heptavax d.Menomune 16 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. Department of Health and Human Services. Aging Statistics. Accessed July 9, 2014. World Health Organization. (2014). Risk factors. Accessed July 9, 2014. World Health Organization. (2012). Oral health. Accessed July 9, 2014. World Health Organization. Global Health Observatory (GHO). NCD mortality and morbidity. Accessed July 9, 2014. Somai M. Tunisian Center for Public Health. Global Burden of Diseases: Tunisia. September 21, 2013. Accessed July 20, 2014. Framington Heart Study. Epidemiological Background and Design: The Framingham Study. Accessed July 9, 2014. Framington Heart Study. History of the Framington Heart Study. Accessed July 9, 2014. Framingham Heart Study. Accessed June 19, 2014. Bambra C, Gibson M, Sowden A, et al. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010;64:284e29. Centers for Disease Control and Prevention. Social Determinants of Health. Accessed July 9, 2014. Commission on Social Determinants of Health. Achieving Health Equity: from root causes to fair outcomes. p.4. Accessed July 9, 2014. The Bangkok Charter for Health Promotion in a Globalized World. Health Promot. Int. (2006) 21 (suppl 1): 10-14. Accessed 9, 2014. Rosecrance J, Cook T. Upper Extremity Musculoskeletal Disorders: Occupational Association and a Model for Prevention. CEJOEM 1998; 4(3):214-231. Accessed July 9, 2014. Williams D. Reducing global oral health inequalities - a call to action. Accessed September 12, 2014. National Institute of Dental and Craniofacial Research. Oral Health in America: A Report of the Surgeon General (Executive Summary). Chapter 1: The Meaning of Oral Health. Accessed July 9, 2014. National Institute of Dental and Craniofacial Research. (2000). Oral Health in America: A Report of the Surgeon General (Executive Summary). Preface from the Surgeon General U.S. Public Health Service. Accessed July 9, 2014. Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention--WHO recommendations for improved evidence in public health practice. Community Dent Health. p. 1. 2004 Dec; 21(4 Suppl):319-329. Accessed July 9, 2014. World Health Organization. Noncommunicable diseases and mental health. Scaling up action against noncommunicable diseases: how much will it cost? September 2011. Accessed July 9, 2014. Petersen PE, Integrated prevention of oral and chronic disease - the challenges to dental public health. (2006) Keynote lectures. p.1. Accessed September 4, 2014. National Conference of State Legislatures. State Smoke-Free Laws and Health. Last updated July, 2013. Accessed July 9, 2014. U.S. Department of Health and Human Services. The Health Consequences of Smoking, 50 Years of Progress: A Report of the Surgeon General, 2014. Accessed July 9, 2014. World Health Organization. Tobacco Free Initiative (TFI). WHO report on the global tobacco epidemic, 2011. Accessed August 4, 2014. National Institute of Dental and Craniofacial Research. Chapter 3: Diseases and Disorders. Accessed August 4, 2014. Rad M, Kakoie S, Brojeni F, Pourdamghan N. Effect of Long-term Smoking on Whole-Mouth Salivary Flow Rate and Oral Health. J Dent Res Dent Clin Dent Prospect. 2010; 4(4):110-114. Accessed August 4, 2014. National Institute on Alcohol Abuse and Alcoholism. Alcohol Alert. Alcohol and Tobacco. Jan 2007;71. Accessed September 10, 2014. HealthyPeople.gov. About Healthy People. Revised September 7, 2014. Accessed September 10, 2014. HealthyPeople.gov. Tobacco Use. Revised September 7, 2014. Accessed September 10, 2014. Gmel G, Rehm J. Harmful Alcohol Use. National Institute on Alcohol Abuse and Alcoholism. Accessed August 5, 2014. 17 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 29. Centers for Disease Control and Prevention. Alcohol and Public Health. Frequently Asked Questions. Revised: March 14, 2014. Accessed July 9, 2014. 30. Obrochta J, McClue E, Frese P. Oral Implications of Chemical Dependency & Substance Abuse for the Dental Professional. dentalcare.com. Accessed August 4, 2014. 31. The Oral Cancer Foundation. The Alcohol Connection. Accessed July 9, 2014. 32. World Health Organization. Global Health Observatory (GHO). Unhealthy Diet. Accessed August 4, 2014. 33. Chopra M, Galbraith S, Darnton-Hill I. A global response to a global problem: the epidemic of overnutrition, Bulletin of the World Health Organization 2002;80:952-958. Accessed August 4, 2014. 34. United States Department of Agriculture. Dietary Guidelines for Americans. Accessed September 4, 2014. 35. National Institute of General Medical Sciences. Inside Life Science. What Do Fats Do in the Body? Posted: December 15, 2010. Accessed August 4, 2014. 36. Low-Energy-Dense Foods and Weight Management: Cutting Calories While Controlling Hunger, Research to Practice Series, No. 5. CDC. Accessed July 9, 2014. 37. USDA. Dietary Guidelines for Americans 2005. Chapter 6 Fats. Revised: July 9, 2008. Accessed July 9, 2014. 38. Gebel E. Diabetes Forecast. How the body Uses Carbohydrates, Proteins, and Fats. March 2011. Accessed September 4, 2014. 39. American Nutrition Association. Nutrition Digest. 2010;36(4). Accessed July 9, 2014. 40. Moynihan P, Petersen PE. Diet, nutrition and the prevention of dental diseases. Public Health Nutr. 2004 Feb;7(1A):201-26. 41. Corliss J. Eating too much added sugar increases the risk of dying with heart disease. Harvard Health Publications. Harvard Medical School. February 6, 2014. Accessed July 9, 2014. 42. Srinath Reddy K, Katan MB. Diet, nutrition and the prevention of hypertension and cardiovascular diseases. Public Health Nutr. 2004 Feb;7(1A):167-86. 43. U.S. Food and Drug Administration. Sodium in Your Diet: Using the Nutrition Facts Label to Reduce Your Intake. Revised: June, 20 2014. Accessed July 9, 2014. 44. National Institute of Dental and Craniofacial Research. Part Three: What is the Relationship Between Oral Health and General Well-Being? Accessed August 4, 2014. 45. National Cancer Institute. What is Cancer? Revised March 7, 2014.Accessed September 12, 2014. 46. The Oral Cancer Foundation. Oral Cancer Facts. Rates of Occurrence in the United States. Accessed September 5, 2014. 47. Kim J. Amar S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology. Sep 2006; 94(1): 10–21. 48. Science Daily. American Association for Cancer Research (AACR). Poor oral health linked to cancer-causing oral HPV infection. August 21, 2013. Accessed September 9, 2014. 49. Lockhart PB, Bolger AF, Papapanou PN, et al., Periodontal Disease and Atherosclerotic Vascular Disease: Does the Evidence Support an Independent Association? A Scientific Statement from the American Heart Association. J Oral Microbiol. 2010 Dec 21; 2. 50. Leishman SJ, Do HL, Ford PJ. Cardiovascular disease and the role of oral bacteria. J Oral Microbiol. 2010; 2:10. 51. Prasanna SJ. Causal relationship between periodontitis and chronic obstructive pulmonary disease. J Indian Soc Periodontol. 2011 Oct-Dec;15(4): 359–365. 52. Centers for Disease Control and Prevention. FastStats. Leading Causes of Death. Revised: July 2014. Accessed September 9, 2014. 53. Juvelekian G, Stoller J. Lung Summit: Advances in Pulmonary Medicine, Critical Care Medicine, and Mechanical Ventilation. September 18-20, 2014. Chronic Obstructive Pulmonary Disease. Accessed August 5, 2014. 54. National Diabetes Information Clearinghouse (NDIC). Diabetes Overview. Revised: April 2, 2014. Accessed August 5, 2014. 55. The Merck Manual Professional Edition. Diabetes Mellitus (DM). Revised: June 2014. Accessed August 5, 2014. 18 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014 56. Centers for Disease Control and Prevention. Diabetes Public Health Resource. 2011 National Diabetes Fact Sheet. Accessed July 9, 2014. 57. Mealy B. Periodontal disease and diabetes; A two-way street. J Am Dent Assoc 2006; 137(10 supplement):26S-31S. 58. United States Department of Agriculture. Women, Children and Infants. Revised: August 28, 2014. Accessed September 10, 2014. 59. Association of State & Territorial Dental Directors. Best Practice Approaches. Improving Children's Oral Health through Coordinated School Health Programs. Revised May 26, 2011. Accessed September 7, 2014. 60. Centers for Disease Control and Prevention. Human Papillomavirus (HPV). HPV Vaccines. Last Revised: January 29, 2013. Accessed July 9, 2014. 61. Ramqvist T, Dalianis T. Oropharyngeal cancer epidemic and human papillomavirus. Emerg Infect Dis. 2010 Nov;16(11):1671-7. About the Author Carol Chapman, CDA, RDH, MS Carol Chapman, CDA, RDH, MS instructs first and second year students in the dental hygiene program at Florida SouthWestern State College (formerly Edison State College) in Fort Myers, FL. Her didactic instruction includes courses in patients with special needs and community dental health. Additionally, Carol is a contracted writer with Elsevier. Prior to employment at Florida Southwestern State College, Carol worked in private practice for 23 years as a dental hygienist and also has experience in dental assisting. Email: cchapman@fsw.edu 19 ® ® Crest + Oral-B at dentalcare.com Continuing Education Course, November 1, 2014