2011 Supraventricular tachycardia causing heart failure
advertisement
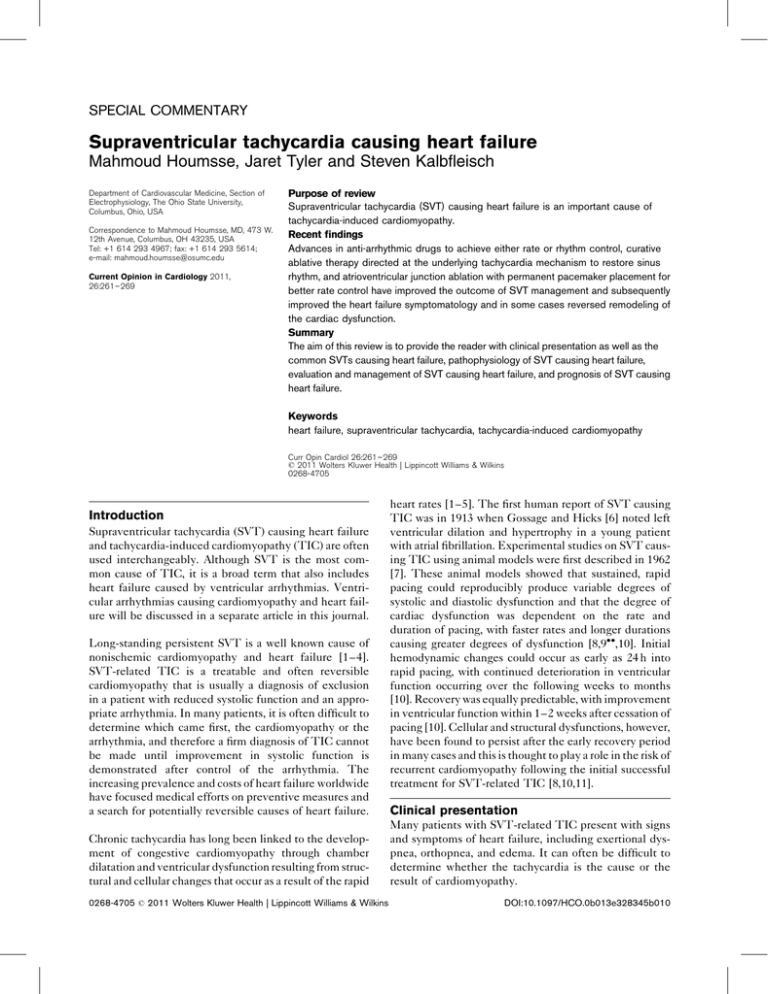
SPECIAL COMMENTARY Supraventricular tachycardia causing heart failure Mahmoud Houmsse, Jaret Tyler and Steven Kalbfleisch Department of Cardiovascular Medicine, Section of Electrophysiology, The Ohio State University, Columbus, Ohio, USA Correspondence to Mahmoud Houmsse, MD, 473 W. 12th Avenue, Columbus, OH 43235, USA Tel: +1 614 293 4967; fax: +1 614 293 5614; e-mail: mahmoud.houmsse@osumc.edu Current Opinion in Cardiology 2011, 26:261–269 Purpose of review Supraventricular tachycardia (SVT) causing heart failure is an important cause of tachycardia-induced cardiomyopathy. Recent findings Advances in anti-arrhythmic drugs to achieve either rate or rhythm control, curative ablative therapy directed at the underlying tachycardia mechanism to restore sinus rhythm, and atrioventricular junction ablation with permanent pacemaker placement for better rate control have improved the outcome of SVT management and subsequently improved the heart failure symptomatology and in some cases reversed remodeling of the cardiac dysfunction. Summary The aim of this review is to provide the reader with clinical presentation as well as the common SVTs causing heart failure, pathophysiology of SVT causing heart failure, evaluation and management of SVT causing heart failure, and prognosis of SVT causing heart failure. Keywords heart failure, supraventricular tachycardia, tachycardia-induced cardiomyopathy Curr Opin Cardiol 26:261–269 ß 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins 0268-4705 Introduction Supraventricular tachycardia (SVT) causing heart failure and tachycardia-induced cardiomyopathy (TIC) are often used interchangeably. Although SVT is the most common cause of TIC, it is a broad term that also includes heart failure caused by ventricular arrhythmias. Ventricular arrhythmias causing cardiomyopathy and heart failure will be discussed in a separate article in this journal. Long-standing persistent SVT is a well known cause of nonischemic cardiomyopathy and heart failure [1–4]. SVT-related TIC is a treatable and often reversible cardiomyopathy that is usually a diagnosis of exclusion in a patient with reduced systolic function and an appropriate arrhythmia. In many patients, it is often difficult to determine which came first, the cardiomyopathy or the arrhythmia, and therefore a firm diagnosis of TIC cannot be made until improvement in systolic function is demonstrated after control of the arrhythmia. The increasing prevalence and costs of heart failure worldwide have focused medical efforts on preventive measures and a search for potentially reversible causes of heart failure. Chronic tachycardia has long been linked to the development of congestive cardiomyopathy through chamber dilatation and ventricular dysfunction resulting from structural and cellular changes that occur as a result of the rapid 0268-4705 ß 2011 Wolters Kluwer Health | Lippincott Williams & Wilkins heart rates [1–5]. The first human report of SVT causing TIC was in 1913 when Gossage and Hicks [6] noted left ventricular dilation and hypertrophy in a young patient with atrial fibrillation. Experimental studies on SVT causing TIC using animal models were first described in 1962 [7]. These animal models showed that sustained, rapid pacing could reproducibly produce variable degrees of systolic and diastolic dysfunction and that the degree of cardiac dysfunction was dependent on the rate and duration of pacing, with faster rates and longer durations causing greater degrees of dysfunction [8,9,10]. Initial hemodynamic changes could occur as early as 24 h into rapid pacing, with continued deterioration in ventricular function occurring over the following weeks to months [10]. Recovery was equally predictable, with improvement in ventricular function within 1–2 weeks after cessation of pacing [10]. Cellular and structural dysfunctions, however, have been found to persist after the early recovery period in many cases and this is thought to play a role in the risk of recurrent cardiomyopathy following the initial successful treatment for SVT-related TIC [8,10,11]. Clinical presentation Many patients with SVT-related TIC present with signs and symptoms of heart failure, including exertional dyspnea, orthopnea, and edema. It can often be difficult to determine whether the tachycardia is the cause or the result of cardiomyopathy. DOI:10.1097/HCO.0b013e328345b010 262 Cardiac failure TICs have been associated with essentially any SVT that is frequent and fairly persistent. The most common supraventricular arrhythmias causing TIC are atrial fibrillation and atrial flutter; however, the subgroups of paroxysmal SVT (PSVT) such as atrial tachycardia (Fig. 1a), atrioventricular nodal re-entrant tachycardia (AVNRT), and atrioventricular re-entrant tachycardia (AVRT) (especially the ‘permanent junctional reciprocating tachycardia (PJRT)’ variant, Fig. 2a) can also be a cause [9,11,12,13]. SVT-related TIC can occur over a range of ages, from in-utero to the elderly, and is generally thought to take months of a fairly persistent arrhythmia to develop [14,15]. The type of arrhythmias causing TIC varies with the age of the patient, with certain forms of PSVT being more common in younger patients and atrial fibrillation and flutter being more common in older patients. Although no absolute heart rate cutoff exists, many consider persistent rates greater than 100 beats/min are necessary to develop relatively early-onset left ventricular dysfunction; however, even slower incessant arrhythmias could lead to the insidious development of heart failure if left unchecked over long periods [11]. Animal models have been studied extensively in the assessment of SVT-related TIC. These studies have shown that rapid pacing can cause reduction in systolic function and cardiac output with a secondary increase in filling pressures and systemic vascular resistance and that cessation of pacing reverses cardiomyopathy [16–19]. Such findings have also been described in numerous clinical reports of SVT-related TIC. In these clinical cases, termination of the tachycardia resulted in an improvement in clinical symptoms, reduction in left ventricular chamber size, and an increase in left ventricular systolic function [20]. The degree of left ventricular dysfunction has clearly been shown to correlate with the rate and duration of the tachycardia, but ironically, in a clinical setting, very rapid arrhythmias rarely lead to TIC because these patients usually develop rate-related symptoms and present for treatment early before a myopathy develops [21]. One of the most important factors for the development of TIC is the total tachycardia burden over time. In patients with relatively slow and asymptomatic tachycardias, the arrhythmia may be incessant and the patient may not present until heart failure symptoms develop. Other factors that may also contribute to the development of TIC include the type of arrhythmia, atrioventricular relationship during the arrhythmia, pattern of the arrhythmia (paroxysmal vs. persistent), irregularity of the QRS complexes, and presence of underlying heart disease [22]. Pathophysiology Before reviewing the available data regarding the gross and cellular changes that occur in SVT-related TIC, it is Key points Long-standing persistent supraventricular tachycardia (SVT) is a well known cause of nonischemic cardiomyopathy and heart failure, which is known as tachycardia-induced cardiomyopathy (TIC). SVT-related TIC is a treatable and often reversible cardiomyopathy that is usually a diagnosis of exclusion, evaluation, and management of SVT causing heart failure. The most common supraventricular arrhythmias causing TIC are atrial fibrillation and atrial flutter. Standard workup for cardiomyopathies should include a thorough history and physical, laboratory assessment, echocardiogram, and ischemic evaluation. If initial workup is negative, then TIC should be considered. Many patients with SVT-related TIC present with signs and symptoms of heart failure, including exertional dyspnea, orthopnea, and edema. It can often be difficult to determine whether the tachycardia is the cause or the result of cardiomyopathy. The goal of treatment is to control the tachycardia through rate or rhythm control, thereby improving a patient’s symptoms, reversing ventricular dysfunction, and preventing future cardiomyopathy. Despite the apparent normalization of systolic function with control of the tachycardia, cellular and structural abnormalities of the myocardium may persist and cause early recurrence of cardiac dysfunction when optimal medical therapy of cardiomyopathy and heart failure is stopped. A small subset of treated SVT-related TIC patients had sudden cardiac death after resolution of ventricular dysfunction, supporting the observation of enduring cellular and molecular abnormalities. Indefinite heart failure medical treatment and frequent follow-up of SVT-related TIC patients should be implemented after tachycardia control or elimination. Implantable cardioverter defibrillator therapy needs to be considered for primary prevention in patients who have persistent reduction or recurrence of depressed left ventricular ejection fraction, despite control of the tachycardia. important to keep in mind that the interaction between the myocardial cellular and extracellular matrix (ECM) via the basement membrane is essential to generate and maintain adequate left ventricular contractility. Pacing-induced TIC in animal models results in enlargement of the cardiac chamber, thinning of the chamber wall with an elevation in wall stress, and decline in the cardiac pump performance as a result of a significant increase in myocardial water accumulation [2,23,24]. In animal studies, SVT-related TIC also resulted in changes in cellular function and ECM composition (see below) in Supraventricular tachycardia causing heart failure Houmsse et al. 263 Figure 1 Paroxysmal atrial tachycardia and curative ablative therapy of incessant repetitive pulmonary vein tachycardia (a) Paroxysmal atrial tachycardia originating from right superior pulmonary vein (RSPV). This was confirmed during electrophysiology study. The P wave axis mimics a sinus node P wave, but the rhythm is clearly abnormal, indicative of an incessant repetitive pulmonary vein tachycardia. (b) Curative ablative therapy of incessant repetitive pulmonary vein tachycardia. Twelve-lead electrocardiogram during radio frequency ablation at the right superior pulmonary vein. Immediately after the onset of the ablation, there was termination of the atrial tachycardia with restoration of sinus rhythm as seen in the last four beats. the heart, and these changes demonstrated significant reversal after tachycardia termination [25,26]. (3) distortion of the sacrolemma–basement membrane interface, which promotes extracellular remodeling and scar formation. Cellular changes are ECM changes are as follows: (1) significant increase in myocyte length, (2) significant reduction in the anchoring of the myocyte to the basement membrane, and (1) SVT-causing TIC resulted in a reduction in collagen concentration and cross-linking, diminished myocyte 264 Cardiac failure Figure 2 ECG of a supraventricular tachycardia patient during sinus rhythm (a) Twelve-lead ECG of a 29-year-old man with frequent and nearly incessant paroxysmal supraventricular tachycardia. This ECG demonstrates a classic long RP tachycardia, the differential diagnosis of which includes permanent junctional reciprocating tachycardia (PJRT), atypical atrioventricular node re-entrant tachycardia (AVNRT) and atrial tachycardia (AT). Electrophysiologic testing is required to differentiate the tachycardia type, but, clinically, the incessant nature of the tachycardia is most consistent with either PJRT or AT. In this case, the patient was found to have PJRT and the accessory pathway was successfully ablated near the coronary sinus ostium. (b) Twelve-lead ECG of the same PJRT patient during sinus rhythm: please notice the short PR interval without pre-excitation (no delta wave). PJRT patients almost never have a delta wave. Therefore, the lack of a delta wave does not rule out atrioventricular re-entrant tachycardia (AVRT). basement membrane adhesion capacity, and increased proteoglycans. (2) These changes improved with the resolution of SVT and resulted in an increased collagen concentration and a normalization of myocyte adhesion capacity and proteoglycan distribution. Incessant SVT-related TIC was also associated with significant structural alterations to the myocardial capillary vasculature and myocyte injury. These alterations in capillary structure and distribution were associated with an increase in coronary vascular resistance, reduced myocardial blood flow, and an increase in capillary diffusion distances. These changes in capillary structure and myocardial blood flow may explain, at least in part, the ventricular dysfunction and myocardial injury observed with chronic SVT [27]. Spinale et al. [28] reported on their observations of subendocardial injury in SVT-related TIC. Their findings showed the potential relationship between the structural changes in capillary vasculature, abnormal myocardial blood flow and subsequent subendocardial injury, and Supraventricular tachycardia causing heart failure Houmsse et al. 265 left ventricular remodeling induced by SVT-related TIC. Changes in mitral valve function have also been reported in TIC. Most of these reports describe functional mitral regurgitation as a result of changes in the left ventricular chamber geometry [29,30], annular dilatation [31], and papillary muscle tethering [32,33], leading to decreased leaflet coaptation in the septal–lateral orientation [34]. Stephens et al. [35] did report on structural changes in the mitral valve leaflet during TIC. These changes include greater cell density, loss of leaflet-layered structure, and greater collagen and elastic fiber turnover. Evaluation The incidence and prevalence of SVT-related TIC are not exactly known; however, as it is treatable, and often reversible, it should be aggressively pursued as a possible cause of a cardiomyopathy if any significant history of a dysrhythmia is present. Although arrhythmias have been shown to be a contributing factor in approximately 6% of hospital heart failure admissions, the percentage of patients having an arrhythmia as the primary cause of a their cardiomyopathy would be expected to be considerably smaller. Unexplained cardiomyopathy work-up needs to be comprehensive, including common causes (ischemic heart disease, hypertensive heart disease, and valvular heart disease) and uncommon causes [infiltrative heart disease, toxic insults (e.g., alcohol, chemotherapy), familial disease, tachycardia-induced cardiomyopathy]. Idiopathic cardiomyopathy is the final diagnosis if the above work-up is negative. The diagnosis of a pure TIC is really one of exclusion and requires the presence of an appropriate arrhythmia and the absence of other significant cardiac disease. Even with the existence of underlying cardiac disease, the presence of a persistent tachycardia can lead to worsening cardiac function and the patient may have a combined cardiomyopathy, with TIC playing at least a partial role. There is no definitive test for a TIC and the real evidence that a TIC was present can only be seen after 2–3 months of follow-up by demonstrating improvement in left ventricular function after appropriate arrhythmia control. The approach to a patient with new, systolic cardiomyopathy includes a thorough history and physical and guided diagnostic tests. While taking the history, one needs to keep in mind that some SVTs are much more common in specific clinical settings. Some variables that can influence the type of tachycardia involved in the development of a TIC are listed below. (1) Age: SVT can occur at any age, but the relative proportion of different types of SVT is strongly influenced by the age of the patient. Re-entrant tachycardias due to accessory pathways, such as PJRT are more common in younger patients, as are incessant atrial tachycardias. Atrial fibrillation and flutter (Fig. 3) are much more common in older patients (>60 years old) and those with underlying cardiac disease. Porter et al. [36] evaluated 1856 patients with PSVT and found that there was a strong relationship between age and PSVT mechanism; AVRTs were more common in younger patients, whereas the prevalence of AVNRT increased with age. Figure 3 Twelve-lead ECG of a right atrial flutter Please note saw tooth flutter waves. Negative P wave in leads II, III, and aVF. 266 Cardiac failure (2) Sex: AVRTs tend to be more common in men, whereas AVNRT and atrial tachycardias are seen more commonly in women [36]. (3) Co-morbidities: Re-entrant forms of PSVT are usually found in patients without structural heart disease. An exception to that rule is that some forms of congenital heart disease, such as Ebstein’s anomaly, have an increased prevalence of accessory pathways and associated AVRTs [37]. Atrial fibrillation and flutter are more commonly seen in patients with other co-morbidities such as diabetes mellitus, hypertension, valvular disease, coronary artery disease, and sleep apnea [38–41]. A 12-lead ECG can detect an arrhythmia and a presumptive diagnosis of the tachycardia type can be often be made on the basis of certain ECG features. ECGs can also reveal substrate for arrhythmias (e.g., pre-excitation) and suggest other nonarrhythmia-related causes of cardiomyopathy including ischemic disease, left ventricular hypertrophy and hypertensive heart disease, and infiltrative diseases such as amyloidosis. The basic ECG, however, cannot determine the overall arrhythmia burden; therefore, long-term monitoring with either a Holter monitor or an auto-event recorder is needed. Analysis of the 12-lead ECG can assist in understanding the possible mechanism of an SVT causing TIC. Some features that should be evaluated when looking at the ECG are listed below. (1) Heart rate: heart rate is not reliable in predicting the mechanism of a tachycardia, but it is important in predicting the risk of developing a TIC. Although it has been shown in experimental studies that the faster the rate the greater the likelihood of developing a TIC [42], in clinical practice it is usually the slower, asymptomatic incessant arrhythmias that typically lead to development of a TIC [9]. (2) Persistent SVT vs. PSVT: Truly paroxysmal tachycardias rarely lead to a TIC, as they rarely cause enough tachycardia burden to result in reduced left ventricular function. Incessant tachycardia has been defined as continuous tachycardia or continuous paroxysms of tachycardia separated by a few normal sinus beats [43]. A classic incessant SVT is PJRT. This is an arrhythmia that is caused by a slowly conducting accessory pathway usually located near the coronary sinus ostium. These patients may have truly incessant tachycardia with essentially no periods of sinus rhythm or they may have frequent episodes of PSVT that last for long periods and result in a large tachycardia burden (see Fig. 2a). Long-term monitoring is usually the best way to determine whether a tachycardia is frequent or incessant, but, in some cases, the 12-lead ECG can reveal that an arrhythmia is frequent and repetitive, as is demonstrated by the ECG shown in Fig. 1a. (3) Long RP vs. short RP tachycardia: The RP-to-PR ratio is not diagnostic of any tachycardia type but does help in creating a differential diagnosis of the possible tachycardia types. Long RP tachycardias are far more likely to be incessant, and the differential diagnosis of these includes PJRT, atypical AVNRT, and atrial tachycardia. A very short RP tachycardia or a tachycardia in which the P wave is not identifiable is most consistent with either typical AVNRT or orthodromic reciprocating tachycardia. These tachycardias are usually infrequent and paroxysmal in nature and therefore rarely lead to a TIC. (4) P wave morphology: The typical normal sinus rhythm P wave morphology is positive in the lateral limb leads I, aVL, and positive in the inferior limb leads II, III, and aVF. It is often biphasic in lead V1 and positive in the rest of the precordial leads. A P wave morphology different from a sinus rhythm P wave is indicative of an abnormal rhythm mechanism. A description of the various P wave morphologies and location of the tachycardia focus is beyond the scope of this review. However, some basic rules regarding P wave morphology and tachycardia location are as follows: (a) A negative P wave morphology in the inferior limb leads (II, III, and aVF) predicts that the origin of the tachycardia’s activation of the atrium is from the inferior portion of the atrium, often in close proximity to the coronary sinus ostium. (b) A negative P wave morphology in the lateral limb leads (I and aVL) is indicative of a left atrial location for the tachycardia focus. Standard workup for cardiomyopathies should include a thorough history and physical, laboratory assessment, echocardiogram, and ischemic evaluation. If initial workup is negative, then TIC should be considered. Cardiac MRI is increasingly being utilized for assessment and diagnosis of unexplained cardiomyopathies. MRIs can noninvasively assess for infiltrative myopathies such as sarcoidosis and hemochromatosis, myocarditis, obstructive causes including valvulopathies and hypertrophic cardiomyopathies, ischemic disease and scar burden, and high-output states including intracardiac shunts, along with potential arrhythmogenic causes such as right ventricular dysplasia. Potential limitations are patients with prior cardiac rhythm devices. Treatment/follow-up The goal of treatment is to control the tachycardia through rate or rhythm control, thereby improving a patient’s symptoms, reversing ventricular dysfunction, Supraventricular tachycardia causing heart failure Houmsse et al. 267 and preventing future cardiomyopathy. This management strategy can be obtained through: (1) anti-arrhythmic drugs to achieve either rate or rhythm control, (2) curative ablative therapy directed at the underlying tachycardia mechanism to restore sinus rhythm, and (3) atrioventricular junction ablation with permanent pacemaker placement for better rate control. Any of these approaches can help improve or normalize symptoms. Which approach to use is dependent on the patient’s comorbidities, degree of cardiac dysfunction, clinical status, type of tachycardia, and risk profile for either drug or ablation therapy. In PJRT patients who develop TIC, antiarrhythmic therapy often fails to suppress or control the tachycardia. Meiltz et al. [13] followed 49 patients with PJRT for 49þ/ 38 months after RF ablation. In this series, eight of the 49 cases had incessant PJRT that was complicated with TIC. RF ablation was successful in ablating the arrhythmia in all eight cases (four patients required two ablation sessions) and regression of left ventricular systolic dysfunction was observed during follow-up in all cases. Radio frequency ablation has also been shown to be effective in treating focal atrial tachycardias (AT) associated with TIC. Medi et al. [9] followed 331 patients with focal AT after RF ablation. In that series, approximately 25% of the tachycardias were incessant, and approximately one-third of patients with an incessant tachycardia had evidence of a TIC. Most of the patients with TIC were young (39 22 years), and the arrhythmiarelated heart rates in the TIC patients tended on average to be slower than the atrial tachycardia rates in those without a TIC. This last finding most likely relates to the fact that patients with rapid tachycardia rates tend to present earlier for care and therefore are less likely to develop a cardiomyopathy. After successful ablation, left ventricular systolic function returned back to normal in 97% of patients at a mean of 3-month follow-up. Rate control for atrial fibrillation or flutter can be obtained with a cocktail of atrioventricular node slowing medications. Nearly all patients should be placed on a betablocker unless otherwise contraindicated. Additional rate controlling medications include digoxin, calcium channel blockers, and even amiodarone in some resistant cases when there is a desire to avoid an atrioventricular junction ablation and pacemaker implant. No standard rate control goal exists; however, most practitioners aim for a resting heart rate 80 beats/min or less, moderate exercise heart rates less than 120 beats/min, and average heart rates less than 100 beats/min on a 24 h Holter. Recurrent unchecked tachycardia has been shown to accelerate a decline in ventricular dysfunction; thus frequent assessments of rate control with Holter and event monitors is warranted in many patients [12,44]. Additionally, effective rate control can periodically be assessed with an in-office 6-min walk or outpatient exercise treadmill evaluation. In patients with left ventricular dysfunction and atrial fibrillation with rapid rates refractory to medical therapy, atrioventricular junction ablation with placement of a pacemaker has been shown to significantly improve cardiac function in appropriately selected patients. In many of these patients, placement of a bi-ventricular (Bi-V) pacing system may be preferred and lead to greater improvement in cardiac function compared with right ventricular pacing alone. The improvement in cardiac function after atrioventricular junction ablation and pacing may not only be due to heart rate control but may also be related to the regularization of the rhythm [45,46]. In at least one study of patients with refractory atrial fibrillation and heart failure, curative pulmonary vein isolation ablation was shown to be superior to atrioventricular junction ablation with Bi-V pacing based on both subjective and objective follow-up assessments [47]. In the modern era when potentially curative approaches are available, these should be considered prior to palliative approaches such as atrioventricular junction ablation, especially in younger patients where long-term device therapy may be problematic. For atrial flutter, which is more easily cured with ablation than atrial fibrillation, studies have shown improvement in the ejection fraction in approximately 60% of patients with reduced left ventricular function prior to the ablation. In many of these patients, the improvement in ejection was great enough to eliminate the need for implantation of a primary prevention defibrillator [13]. Conclusion Despite the apparent normalization of systolic function with control of the tachycardia, cellular and structural abnormalities of the myocardium may persist. This is supported by observations of precipitous decline in systolic function with recurrent arrhythmias, whereas the initial process took months or years to develop [12]. Such early recurrence of cardiac dysfunction is thought to be secondary to persistent cellular abnormalities, structural disarray, and diastolic dysfunction that persisted well after the tachycardia was treated and systolic function normalized [9,21,44]. This is further supported by an observed decline in systolic function with cessation of cardiac remodeling medications (i.e., beta-blockers and angiotensin-converting enzyme inhibitors) even in the absence of tachycardia recurrence [48]. Finally, a small subset of treated SVT-related TIC patients had sudden 268 Cardiac failure cardiac death after resolution of ventricular dysfunction, supporting the observation of enduring cellular and molecular abnormalities [12]. Therefore, medical treatment should be indefinite, with close observation and frequent follow-up of SVT-related TIC patients. Implantable cardioverter defibrillator therapy needs to be considered for primary prevention in patients who have persistent reduction of left ventricular ejection fraction despite control of the tachycardia, but this decision should generally be made after the patient has been given enough time, usually 3 months or more, to allow recovery of cardiac function. 15 Ott P, Kelly PA, Mann DE, et al. Tachycardia-induced cardiomyopathy in a cardiac transplant recipient: treatment with radiofrequency catheter ablation. J Cardiovasc Electrophysiol 1995; 6:391–395. References and recommended reading 21 Fishberger SB, Golan S, Saul JP, et al. Myocardial mechanics before and after ablation of chronic tachycardia. Pacing Clin Electrophysiol 1996; 19:42. Papers of particular interest, published within the annual period of review, have been highlighted as: of special interest of outstanding interest Additional references related to this topic can also be found in the Current World Literature section in this issue (p. 274). 1 Gaasch WH, Zile MR. Evaluation of myocardial function in cardiomyopathic states. Prog Cardiovasc Dis 1984; 27:115–132. 2 Damiano RJ, Tripp HF, Asano T, et al. Left ventricular dysfunction and dilatation resulting from chronic supraventricular tachycardia. J Thorac Cardiovasc Surg 1987; 94:135–143. 3 4 Gillette PC, Smith RT, Garson A Jr, et al. Chronic supraventricular tachycardia: a curable cause of congestive cardiomyopathy. JAMA 1985; 253:391– 392. Packer DL, Bardy GH, Worley SJ, et al. Tachycardia induced cardiomyopathy: a reversible form of left ventricular dysfunction. Am J Cardiol 1986; 57:563– 570. 16 Morgan DE, Tomlinson CW, Qayumi AK, et al. Evaluation of ventricular contractility indexes in the dog with blood ventricular dysfunction induced by rapid atrial pacing. JACC 1989; 14:496. 17 O’Brien PJ, Ianuzzo CD, Moe GW, et al. Rapid ventricular pacing of dogs to heart failure: biochemical and physiological studies. Can J Physiol Pharmacol 1990; 68:34. 18 Ohno M, Cheng CP, Little WC. Mechanism of altered patterns of left ventricular filling during the development of congestive heart failure. Circulation 1994; 89:2241. 19 Wilson JR, Douglas P, Hickey WF, et al. Experimental congestive heart failure produced by rapid ventricular pacing in the dog. Circulation 1987; 75:857. 20 Tomita M, Spinale FG, Crawford FA, Zile MR. Changes in left ventricular volume, mass, and function during the development and regression of supraventricular tachycardia-induced cardiomyopathy. Circulation 1991; 83:635–644. 22 Gopinathannair R, Sullivan RM, Olshansky B. Tachycardia-mediated cardio myopathy: recognition and management. Curr Heart Failure Rep 2009; 6:257–264. An outstanding overview of TIC. It is a very comprehensive review that takes the reader from the cellular level changes to bedside preventive and therapeutic interventions. 23 Spinale FG, Hendrick DA, Crawford FA, et al. Chronic supraventricular tachycardia causes ventricular dysfunction and subendocardial injury in swine. Am J Physiol 1990; 259:H218–H229. 24 Wilson JR, Douglas P, Hickey WF, et al. Experimental congestive heart failure produced by rapid ventricular pacing in the dog: cardiac effects. Circulation 1987; 75:857–867. 25 Zellner JL, Spinale FG, Eble DM, et al. Alterations in myocyte shape and basement membrane attachment with tachycardia induced heart failure. Circ Res 1991; 69:590–600. 26 Spinale FG, Zellner JL, Johnson WS, et al. Cellular and extracellular remodeling with the development and recovery from tachycardia-induced cardiomyopathy: changes in fibrillar collagen, myocyte adhesion capacity and proteoglycans. J Mol Cell Cardiol 1996; 28:1591–1608. 5 Zellner JL, Spinale FG, Eble DM, et al. Alterations in myocyte shape and basement membrane attachment with tachycardia-induced heart failure. Circ Res 1991; 69:590–600. 6 Gossage AM, Hicks B. On auricular fibrillation. Q J Med 1913; 6:435–440. 27 Spinale FG, Grine RC, Tempel GE, et al. Alteration in the myocardial capillary vasculature accompanies tachycardia-induced cardiomyopathy. Basic Res Cardiol 1992; 187:65–79. 7 Whipple GH, Sheffield LT, Woodman EG, et al. Reversible congestive heart failure due to chronic rapid stimulation of the normal heart. Proc N Engl Cardiovasc Soc 1962; 20:39–40. 28 Spinale FG, Hendrick DA, Crawford FA, et al. Chronic supraventricular tachycardia causes biventricular failure and subendocardial injury. Am J Physiol 1990; 259:H218–H229. 8 Khasnis A, Jongnarangsin K, Abela G, et al. Tachycardia-induced cardiomyopathy: a review of literature. PACE 2005; 28:710–721. 29 Kono T, Sabbah HN, Rosman H, et al. Left ventricular shape is the primary determinant of functional regurgitation in heart failure. J Am Coll Cardiol 1992; 20:1594–1598. Medi C, Kalman JM, Haqqani H, et al. Tachycardia-mediated cardiomyopathy secondary to focal atrial tachycardia: long-term outcome after catheter ablation. J Am Coll Cardiol 2009; 53:1791–1797. Focal incessant or frequent paroxysmal atrial tachycardia was associated with only 10% TIC. Patients who had slower ventricular rate during incessant or frequent paroxysmal atrial tachycardia had higher incidence of developing TIC. This was higher in young men. Ninety-seven percent of the patients with TIC restored their left ventricular function by 3-month follow-up. 9 10 Shinbane JS, Wood MA, Jensen DN, et al. Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. JACC 1997; 29:709– 715. 11 Nerheim P, Birger-Botkin S, Piracha L, Olshansky B. Heart failure and sudden death in patients with tachycardia-induced cardiomyopathy and recurrent tachycardia. Circulation 2004; 110:247–252. 12 Pizzale S, Lemery R, Green MS, et al. Frequency and predictors of tachy cardia-induced cardiomyopathy in patients with persistent atrial flutter. Can J Cardiol 2009; 25:469–472. This study is very important due to multivariable analysis of the predictors of reversibility of left ventricular dysfunction. The only independent predictor of the reversibility of left ventricular dysfunction after successful ablation of atrial flutter was ventricular response more than 100 beats/min. It also emphasizes the need for assessment of left ventricular function in 3–4 months. 13 Meiltz A, Weber R, Halimi F, Zimmermann M, et al., for the RETAC (Réseau Européen pour le Traitement des Arythmies Cardiaques). Permanent form of junctional reciprocating tachycardia in adults: peculiar features and results of radiofrequency catheter ablation. Europace 2006; 8:21–28. 14 Harrigan JT, Kangos JJ, Sikka A, et al. Successful treatment of fetal congestive heart failure secondary to tachycardia. N Engl J Med 1981; 304:1527–1529. 30 Sabbah HN, Rosman H, Kono T, et al. On the mechanism of functional mitral regurgitation. Am J Cardiol 1993; 72:1074–1076. 31 Boltwood CM, Tei C, Wong M, et al. Quantitative echocardiography of the mitral complex in dilated cardiomyopathy: the mechanism of functional mitral regurgitation. Circulation 1983; 68:498–508. 32 He S, Fontaine AA, Schwammenthal E, et al. Integrated mechanism for functional mitral regurgitation. Circulation 1997; 96:1826–1834. 33 Otsuji Y, Handschumacher MD, Schwammenthal E, et al. Insight from threedimensional echocardiography into the mechanism of functional mitral regurgitation: direct in vivo demonstration of altered leaflet tethering geometry. Circulation 1997; 96:1999–2008. 34 Timek TA, Dagum P, Lai DT, et al. Pathogenesis of mitral regurgitation in tachycardia-induced cardiomyopathy. Circulation 2001; 104 (Suppl I):I-47–I53. 35 Stephens EH, Timek TA, Daughters GT, et al. Significant changes in mitral valve leaflet matrix composition and turnover with tachycardia-induced cardiomyopathy. Circulation 2009; 120:S112–S119. TIC causes significant changes in the mitral valve composition including cells, interstitial matrix, and myofibroblast phenotyping. TIC will induce greater cell density and loss of leaflet layered structure. Collagen and elastic fiber turnover was greater in TIC, as was the myofibroblast phenotype. Compositional differences between TIC and control leaflets were heterogeneous by annular segment and leaflet region, and related to regional changes in leaflet segment length with TIC. 36 Porter MJ, Morton JB, Denman R, et al. Influence of age and gender on the mechanism of supraventricular tachycardia. Heart Rhythm 2004; 1:393– 396. Supraventricular tachycardia causing heart failure Houmsse et al. 269 37 Iturralde P, Nava S, Sálica G, et al. Electrocardiographic characteristics of patients with Ebstein’s anomaly before and after ablation of an accessory atrioventricular pathway. J Cardiovasc Electrophysiol 2006; 17:1332– 1336. 38 Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991; 22:983– 988. 39 Benjamin EJ, Levy D, Vaziri SM, et al. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994; 271:840–844. 40 Krahn AD, Manfreda J, Tate RB, et al. The natural history of atrial fibrillation: Incidence, risk factors, and prognosis in the Manitoba follow-up study. Am J Med 1995; 98:476–484. 41 Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation 2004; 110:364–367. 42 Armstrong PW, Stopps TP, Ford SE, De Bold AJ. Rapid ventricular pacing in the dog: pathophysiologic studies of heart failure. Circulation 1986; 74:1075–1084. 43 Saoudi N, Cosio F, Waldo A, et al. Classification of atrial flutter and regular atrial tachycardia according to electrophysiologic mechanism and anatomic basis: a statement from a joint expert group from the Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. J Cardiovasc Electrophysiol 2001; 12:852–866. 44 Erbel R, Schweizer P, Krebs W, et al. Sensitivity and specificity of twodimensional echocardiography in detection of impaired left ventricular function. Eur Heart J 1984; 5:477. 45 Felker GM, Thomson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med 2000; 342:1077. 46 Daoud EG, Weiss R, Bahu M, et al. Effect of an irregular ventricular rhythm on cardiac output. Am J Cardiol 1996; 78:1433–1436. 47 Khan MN, Jais P, Cummings J, et al. Pulmonary-vein isolation for atrial fibrillation in patients with heart failure. N Engl J Med 2008; 359:1778–1785. 48 Ilkhanoff L, Gerstenfeld EP, Zado ES, Marchlinski FE. Changes in ventricular dimensions and function during recovery of atrial tachycardia-induced cardiomyopathy treated with catheter ablation. J Cardiovasc Electrophysiol 2007; 18:1104–1106.