An Illustrative Communication Strategy for Emergency Contraception
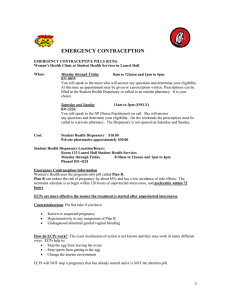
advertisement

An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 1 An Illustrative Communication Strategy for Emergency Contraception Step 1: Analyze the Situation Health and Commodity Context *The majority of the information in this section is a global-level analysis for purposes of illustration. The country-specific situation analysis should be focused on the local context. Health Context Women of reproductive age in developing countries have an increased risk of unintended pregnancy and STI/HIV infection. Each year there are an estimated 75-79 million unintended pregnancies worldwide, 46 million of which end in induced abortion, and about 20 million of which are considered unsafe abortions in non-medical settings (Singh et. al., 2009). There are an estimated 215 million women with an unmet need for contraception (Guttmacher Institute, 2008). Although globally contraceptive use has steadily increased in the past three decades, use in some of the poorest areas of the world, such as sub-Saharan Africa, remains low. It is estimated that less than one-fifth of couples in sub-Saharan Africa are using contraception (UN, 2011). There is global consensus that contraception has direct and indirect influences on a number of health outcomes including maternal, neonatal and infant health and community health (Kerber, 2007; Ronsman and Graham, 2007). According to the “Demographic and Health Surveys (DHS) Analytical Studies 22” published in September 2011, the proportion of pregnancies that were mistimed or unwanted was between 5% and 30% across 20 countries analyzed between 2002 and 2011. The countries studied represented sub-Saharan Africa, Asia, the Middle East, Europe and Eurasia, and Latin America and the Caribbean. 34% of all pregnancies in these countries ended in an unintended birth or an induced abortion. One in three unintended births was from An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 2 contraceptive failure. Some women are at higher risk of unintended pregnancy than others – including young unmarried women and adolescents; women at risk of domestic- and gender-based violence; and women using condoms or traditional methods as their main contraceptive method. Many unplanned pregnancies occur within a year after first sexual intercourse. Studies have found a delay of about one year on average between starting sexual activities and first use of modern contraceptives. Adolescents also struggle with condom negotiation, and many young women report that their first sex experience was coerced.1 In addition, women living in unstable settings are at high risk of unwanted pregnancies. A study by United Nations High Commissioner for Refugees (UNHCR) revealed that 54% of women that survived rape in refugee camps in seven countries did not receive ECPs within 120 hours of an incident in 2007; also, reproductive health assessments in northern Uganda and Jordan revealed that ECPs are not provided in a consistent manner for unwanted pregnancies, including to survivors of sexual violence. While most public health efforts are focused on encouraging men and women to use a regular contraceptive method, it is also important to offer a “back-up” or “last minute” method in case a regular method fails, no method was used or sex was forced. Offering an option to women who have accidentally had unprotected sex or have been forced into sex is a public health priority to address the risk of unintended pregnancies, which in turn can lead to abortion, child neglect or abandonment. Commodity Context Emergency contraception is an important component of a comprehensive family planning program. It offers a reliable option to address the needs of the populations most at risk of unintended pregnancies. Depending on the formulation used and timing of use, ECPs can reduce a 1 Demographic and Health Surveys (DHS) in Ghana, Kenya, Namibia, and Brazil show that the proportion of currently pregnant women under age 20 who reported that their pregnancies were mistimed or unwanted was 46%, 50%, 55%, and 58%, respectively FHI – Adolescents and ECPs 2005. An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 3 woman’s risk of becoming pregnant from a single act of intercourse between 75 and 89% (ICEC/FIGO March 2012). While several products can be used as emergency contraception2, the levonorgestrel-alone ECP is the only one that is widely available in developing countries. It commonly consists of a packet containing two tablets of 0.75 mg each, labeled to be taken 12 hours apart. Recent research has shown, however, that the full dose of 1.5 mg can also be taken at once and does not cause more side effects than two 0.75 mg doses 12 hours apart. ECPs can be used up to 5 days after unprotected sex but are generally more effective the sooner they are used. Extensive research on how ECPs work suggests that interference with ovulation is the primary and possibly the only mechanism of action.3 ECPs do not have any effect after fertilization; ECPs cannot terminate or interrupt an established pregnancy and will not stop a fertilized egg from implanting in the uterus, nor have they been shown to harm a developing embryo. ECPs are safe and appropriate for dispensing by a pharmacist or drug seller without a prescription. Additionally, they are available directly from pharmacists informally even in many developing countries where they are registered as a prescription product. Dedicated ECPs are available from over 90 different manufacturers – and can be purchased at central level (i.e. by central procurement agencies) for as low as US $1 per pack (depending on quantities ordered; packs typically contain one complete “dose,” consisting of one or two pills, depending on the brand and formulation). There are more than 100 ECPs brands used around the world and the most common types include Postinor, Pregnon, NorLevo, and Escapelle. More information on ECPs brands, types and manufacturers is available on the International Consortium for Emergency Contraception (ICEC) website at: 2 Two other compounds have been approved for emergency contraceptive use in some contexts; In addition, IUDs can be used after unprotected sex to prevent the pregnancy; and certain regular contraceptive pills can also be used using what is called the Yuzpe method. 3 Some evidence suggests that ECPs may also function by preventing the egg and sperm from meeting though there is no definitive conclusion. International Consortium for Emergency Contraception (ICEC)/International Federation of Gynecology and Obstetrics (FIGO). Mechanism of action: how do levonorgestrel-only emergency contraceptive pills (LGNECPs) prevent pregnancy? March 2012 An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 4 http://www.cecinfo.org/country-by-country-information/status-availability-database/ec-pill-types-and-countries-of-availability-by-brand Audience and Communication Analysis Access to ECPs varies across different country contexts and is influenced by a number of cultural, social, and political elements. A recent global synthesis of existing demand creation evidence for ECPs found that there are three significant barriers to address in order to increase provision of ECPs (Health Communication Capacity Collaborative, 2013): Low awareness, knowledge and acceptability at individual, community and societal level: DHS data show that the percentage of women who have heard about ECPs as a contraceptive option is systematically lower than for other modern FP methods. Women’s awareness of ECPs continues to be below 10% in Senegal and Zambia, and across the globe, knowledge of ECPs is only around 20% (ICEC 2011a). Even in countries like Kenya where the method is better known (56% of women report having heard about ECPs), usage remains low. Among those who have heard about it, misconceptions remain. A study in Kenya found that among those who knew about the method, one-third believed that it causes abortion, and only about two-thirds knew the correct timeframe for using the method (PSI Kenya, 2009). This indicates the need for continued education and awareness-creation on ECPs across a number of settings. Provider knowledge and skills: An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 5 There is a great variability of knowledge levels among providers around the world. Responses collected through an extensive literature review conducted in June 2011 by the Population Council (Williams, 2011), showed a range in knowledge, from 34% of urban Ghanaian physicians, to 90% or more of providers in Turkey (Sevil et al 2006), Indonesia (Syahlul and Amir 2010), Barbados, and Jamaica (Yam et al., 2007). Two studies in Nigeria (Ebuehi et al., 2006; Oriji and Omietimi, 2011) also show substantial variability among doctors, nurses, and other health care providers in correct administration of ECPs and the biological mechanism of action. In Mexico, a Population Council article showed significant pharmacist confusion between ECPs and mifepristone, the abortion pill (Population Council, 2012). In Bangladesh, as many as 54% of providers incorrectly classified ECPs as a product that can cause abortion before they participated in training (Khan and Hossain 2008). This misunderstanding was also prevalent among a smaller proportion of providers in Turkey, Ghana, and Nigeria (Uzuner et al 2005; Steiner et al 2000; Ebuehi et al 2006), and 42% of providers interviewed in Pakistan were “unsure” whether ECPs could cause abortion or not (Abdulghani et al 2009). These findings are also similar among opinion leaders, religious leaders and even some government officials; even in developed countries like the US, ECPs are still confused with mifepristone. A study from Kenya and Ethiopia (Judge et al., 2011) also found that although knowledge of ECPs as an option to prevent pregnancy after unprotected sex was high, knowledge about the actual biological mechanism was low, leading to confusion on how to administer them. A 2007 study from Uganda found that the majority of health care providers surveyed knew about ECPs and generally had favorable impressions, but many had outdated or inadequate clinical information (Byamugisha et al., 2007). These knowledge gaps affect the providers’ comfort and ability to properly counsel potential ECP clients. Provider bias and negative attitudes: There are also barriers related to attitudes and beliefs by providers that, if addressed, could increase access to and coverage of ECPs. For example, in Ethiopia a study by DKT found evidence of bias among pharmacists concerning the administration of ECPs to certain populations, such as adolescents and unmarried women, and concerns over repeat use. For example, there is widespread belief among providers and women that repeat use will cause long term health problems, especially related to fertility, despite evidence that suggests no increased risk (Halpern et al., 2010). An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 6 Pharmacists in several countries report not being willing to stock ECPs on the ground of personal beliefs because they think it causes abortion, or because they think it increases promiscuity or discourages clients from using a barrier method. Other aspects influencing availability and use of ECPs: The type and number of products registered and distributed in the country (choice). The price levels and availability (is there a public sector offer or a socially marketed product or only commercial products). The inclusion of ECPs in national family planning programs, including essential medicine lists, policies and distribution systems. The status of ECPs (prescription vs. over-the-counter). Policy restrictions on age (who can access ECPs). The number and reach of outlets providing ECPs (clinics and pharmacies). Example of Table to Organize Key Information End-user/community members (e.g. women of reproductive age, women at high risk of GBV) Current Behaviors Primary Barriers to Desired Behavior Primary Benefits of Desired Behavior Each year there are an estimated 75-79 million unintended pregnancies worldwide, 46 million of which end in induced abortion. Limited availability of ECPs Offers a reliable option to address the needs of the populations most at risk of unintended pregnancies In addition, women living in unstable settings are at high risk of unwanted pregnancies. 54% of women that survived rape in Limited awareness and promotion Fear of side effects including: Causes abortion, infertility, or An Illustrative Communication Strategy for Emergency Contraception: Step 1 (Analyze the Situation) 7 Providers (incl. public and private, pharmacy, clinicand community-based) refugee camps in seven countries did not receive ECPs within 120 hours of an incident in 2007. menstrual changes Low levels of promotion and administration/prescription of ECPs Low levels of knowledge of ECPs regarding biological mechanism and side effects Method easily incorporated into current family planning counseling Unwillingness to stock/prescribe ECPs because of association with abortion Commodity produced by over 90 different manufacturers – feasible availability Low confidence levels of prescribing/administering ECPs Provider bias – provides ECPs only to certain populations