Outcomes of Covered Kissing Stent Placement Compared
advertisement

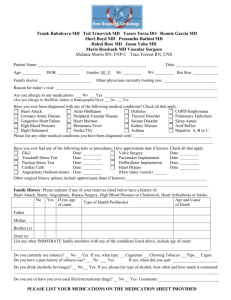
Outcomes of Covered Kissing Stent Placement Compared with Bare Metal Stent Placement in the Treatment of Atherosclerotic Occlusive Disease at the Aortic Bifurcation Saher S. Sabri, MD, Asim Choudhri, MD, Gianluigi Orgera, MD, Bulent Arslan, MD, Ulku C. Turba, MD, Nancy L. Harthun, MD, Klaus D. Hagspiel, MD, Alan H. Matsumoto, MD, and John F. Angle, MD PURPOSE: To review the outcomes with the use of balloon-expandable covered iliac kissing stents as compared with bare metal stents in the treatment of atherosclerotic disease at the aortic bifurcation. MATERIALS AND METHODS: A review of consecutive patients from a single institution with atherosclerotic occlusive disease at the aortic bifurcation treated with balloon-expandable kissing stents was performed between January 1, 2002, and September 1, 2007. Fifty-four patients were identified and divided into two groups: those with bare metal stents and those with covered stents. Technical and clinical success (Fontaine classification), complications, and patency at follow-up were documented. RESULTS: Twenty-six patients (17 men, nine women; mean age, 61 years; age range, 39 –79 years) received covered stents and 28 patients (15 men, 13 women; mean age, 61 years; age range, 38 – 82 years) received bare metal stents. Technical success was achieved in 100% of patients in both groups. Major complications occurred in three of the 26 (11%) with covered stents (P ⴝ .66) and two of the 28 patients (7%) with bare metal stents. The median follow-up was 21 months (20 months for covered stents vs 25 months for bare metal stents; range, 1– 62 months). Twenty-two of the 26 patients (85%) with covered stents had sustained improvement in clinical symptoms during the follow-up period compared with 15 of the 28 patients (54%) with bare metal stents (P ⴝ .02). Primary patency rates at 1 and 2 years were 92% and 92%, respectively, for covered stents and 78% and 62% for bare metal stents (P ⴝ .023). CONCLUSIONS: The use of covered balloon-expandable kissing stents for atherosclerotic aortic bifurcation occlusive disease provides superior patency at 2 years as compared with bare metal balloon-expandable stents. J Vasc Interv Radiol 2010; 21:995–1003 Abbreviations: ABI ⫽ ankle-brachial index, CIA ⫽ common iliac artery, DSA ⫽ digital subtraction angiography, EIA ⫽ external iliac artery, PTA ⫽ percutaneous transluminal angioplasty, TASC ⫽ Trans-Atlantic Inter-Society Consensus ATHEROSCLEROTIC occlusive disease involving the aortic bifurcation and proximal common iliac artery (CIA) has been historically treated From the Division of Angiography, Interventional Radiology, and Special Procedures, Department of Radiology/Box 800170 (S.S.S., A.C., G.O., B.A., U.C.T., K.D.H., A.H.M., J.F.A.) and the Division of Cardiovascular and Thoracic Surgery, Department of Surgery (N.L.H.), University of Virginia Health System, Jefferson Park Ave, Charlottesville, VA 22908. Received August 13, 2009; final revision received January 25, 2010; accepted February 8, 2010. Address correspondence to J.F.A.; E-mail: jfa3h@virginia.edu Inc., and Thoracic Endograft Trials. He is a paid consultant for W.L. Gore, Cook, Bard, Medtronic, Siemens Medical, Crux Medical, and Boston Scientific. J.F.A. has research funded by Atrium Medical and is a paid consultant for Terumo Medical and Siemens Medical. None of the other authors have identified a conflict of interest. A.H.M. has research funded by NIH-HNLBI CORAL TRial Angio-Corelab PI, W.L. Gore, Medtronic, Cook, From the 2008 SIR annual meeting. © SIR, 2010 DOI: 10.1016/j.jvir.2010.02.032 with surgical bypass (1,2). Endovascular treatment with the “kissing stent” technique has shown early clinical results comparable to the surgical option (3–7). However, the longer-term patency rates with aortic bifurcation kissing stents have been disappointing compared with the patency rates of CIA and external iliac artery (EIA) stents (8 –14). Early experience with the use of covered stents in some vascular beds has shown improved patency rates compared with bare metal stents, particularly in the treatment of occlusive lesions involving the superficial femoral artery (15–17). Our 995 996 • Outcomes of Covered Kissing Stents Compared with Bare Metal Stents study reviews our experience with the outcomes of percutaneous placement of expanded polytetrafluoroethylene– covered kissing stents compared with bare metal balloon-expandable stents in the treatment of atherosclerotic occlusive disease at the aortic bifurcation. MATERIALS AND METHODS A retrospective review of consecutive patients from a single institution with atherosclerotic occlusive disease at the aortic bifurcation treated with kissing balloon-expandable iliac kissing stents was undertaken for procedures performed between January 1, 2002, and September 1, 2007, by using a procedural database (Hi-IQ; ConexSys, Albion, Rhode Island). Human investigation review board approval was obtained for this study. Electronic medical records were reviewed for patient demographics, vascular disease risk factors, procedural information, and clinical and imaging follow-up. All study subjects had clinical and angiographic evidence of atherosclerotic occlusive disease involving the aortic bifurcation with unilateral or bilateral CIA stenosis or occlusion. The patients were divided into two groups: those with covered stents and those with bare metal stents. Bare metal stents were used exclusively between January 2002 and November 2004. After November 2004, a commercially available covered stent became available and was applied almost exclusively, in an off-label application. Runoff weighting scores for each limb were recorded on the basis of the reporting standards recommendation of the Society of Interventional Radiology Technology Assessment Committee (18). The clinical status of the patient was assessed with the Fontaine classification (19) at baseline before the procedure, 6 –12 weeks after the procedure, and at the last clinical follow-up. Change in clinical status was designated as “improved,” “no change,” or “worse” on the basis of a change by one or more Fontaine classes. Resting ankle-brachial indexes (ABIs) were obtained in all patients at baseline and at the time of discharge after the procedure. Postprocedure clinical follow-up with ABIs was also performed at 6 –12 weeks after the procedure and then annually. Immediate technical success was defined as less than 30% residual stenosis of the target lesion(s). Initial clinical success was defined as an improvement in ABI from baseline of at least 0.1. Follow-up imaging with computed tomographic (CT) angiography or digital subtraction angiography (DSA) was performed in select patients on the basis of the preferences of the physician performing the clinical follow-up. Patency at follow-up was defined as no evidence of restenosis or occlusion within the originally treated vessel on the basis of follow up CT angiography or DSA and/or the clinical combination of no target vessel revascularization procedures and no more than a 0.15 decrease in follow up ABI. Procedural complications were defined according to the Society of Interventional Radiology Clinical Practice Guidelines (20). Bilateral percutaneous common femoral artery access was obtained, followed by insertion of 6-8-F introducer sheaths in both common femoral arteries for the patients with bare metal stents and 7-F sheaths for patients with covered stents. One patient required left brachial artery access to obtain the diagnostic angiogram. A weight-based bolus of heparin was administrated intravenously or intraarterially to achieve an activated clotting time of more than 220 seconds. Under fluoroscopy, a hydrophilic 0.035-inch guide wire and a 5-F catheter were advanced through the iliac lesions via the common femoral artery access sites. A 5-F multi-sidehole pigtail catheter was advanced proximal to the aortic bifurcation. DSA of the pelvis and both lower extremities was performed by using a power injector in an anteroposterior projection. Oblique images of the pelvis arterial anatomy were also obtained. The introducer sheaths were advanced over the guide wire through the lesions to facilitate delivery of the balloon-expandable stents across the occlusive lesions. Preprocedure dilation with balloon angioplasty was performed as necessary to facilitate stent delivery. The bilateral balloon-expandable stents were positioned over the lesions and the introducer sheaths retracted. Simultaneous stent deployment was performed by using the kissing balloon/stent technique (Figs 1,2). The same type of stent was used in both CIAs. The diameters of the stents selected were usually July 2010 JVIR oversized 10%-20% relative to the treated iliac arteries. If the combined diameter of the stents was greater than the diameter of the distal aorta, then smaller-diameter premounted stents were used at initial stent deployment to keep from overdilating the distal aorta. Postdeployment dilation with larger balloons was then used to make sure the stents opposed the wall both proximally and distally. The artery diameters were measured from the DSA images by using the intrinsic calibration and the quantitative vascular analysis measurement program on the angiographic equipment (Axiom Artis Imaging System; Siemens Medical, Malvern, New Jersey). The proximal ends of the stents were positioned at or above the aortic bifurcation to cover the entire stenotic segment. In patients with unilateral CIA stenoses or occlusions involving the ostium of the ipsilateral CIA, a stent was also placed in the contralateral CIA, and extended a similar distance into the aorta, to ensure its patency. The distance from the proximal end of the stents to the aortic bifurcation was measured and documented in a review by the authors. In the patients with bare metal stents, the balloon-expandable stents used included the Palmaz Genesis (Cordis Endovascular, Warren, New Jersey) and Express LD (Boston Scientific, Natick, Massachusetts) stents. All the stents in the covered stent group were balloon-expandable expanded polytetrafluoroethylene covered stents (iCAST; Atrium Medical, Hudson, New Hampshire). After the procedure, all patients were placed on 81– 325 mg of acetylsalicylic acid a day for life and 75 mg of clopidogrel a day for a minimum of 30 days. The Fisher exact test was used for discrete variables. The Student t test and the Mann-Whitney U test were used for continuous variables evaluation. Ordinal variables analysis was performed by using the Kruskall-Wallis test (nonparametric analysis of variance). Patency of the stents was analyzed by using survival analysis with Kaplan-Meier log-rank test. A P value less than .05 was considered to be indicative of a statistically significant difference. Volume 21 Number 7 Sabri et al • 997 Figure 1. (a) Initial left anterior oblique image from DSA of the pelvis shows bilateral proximal common iliac stenoses (arrows) without involvement of the distal aorta. (b) Bilateral bare metal kissing stents (Express LD) were deployed. (c) Image from DSA performed at 6-month follow-up shows right common iliac in-stent restenosis (arrowheads) secondary to intimal hyperplasia. RESULTS Fifty-four consecutive patients were identified and divided into two groups: those with covered stents and those with bare metal stents. Twenty-six patients (17 men, 9 women; mean age, 61 years; age range, 39 –79 years) received covered stents–-all of which were placed after November 2004. Twentyeight patients (15 men, 13 women; mean age, 61 years; age range, 38 – 82 years) received bare metal stents–-all but four were placed before November 2004 (Table 1). The demographic data and risk factors were similar for both groups. The distribution of the Fontaine classification scores of clinical symptoms were comparable, with 21 of the 26 patients (81%) with covered stents and 21 of the 28 (75%) with bare metal stents having claudication (Fontaine classes II) (P ⫽ .747) (Table 2). Two patients in each group had tissue loss. Treated lesion characteristics on the basis of the TASC II classification of the aortoiliac segments (1) were statistically more advanced in the patients with covered stents, with 10 of 26 patients (38%) classified as having class C and D lesions compared with two of the 28 (7%) with bare metal stents (P ⫽ .0034) (Table 2). Twelve of the 26 patients (46%) with covered stents had CIA occlusions: All of these CIA occlusions were unilateral, with contralateral stenosis in eight patients and a normal contralateral CIA in four. The remaining 14 patients (54%) had bilateral CIA stenoses. Of the 28 patients with bare metal stents, three (10%) had CIA occlusions (one bilateral and two with contralateral stenoses) and 25 (90%) had CIA stenoses (22 bilateral and three unilateral with a contralateral normal CIA). Runoff weighting scores for each limb was recorded on the basis of the reporting standards recommendation of the Society of Interventional Radiology Technology Assessment Committee (19). The distribution of the scores was comparable between both groups. The mean runoff weighting scores for patients with covered stents were 2.0 ⫾ 2.1 on the right and 2.1 ⫾ 1.6 on the left. The mean runoff weighting scores for patients with bare metal stents were 1.6 ⫾ 1.8 on the right and 1.5 ⫾ 1.7 on the left (P ⫽ .134) (Table 2). Immediate technical success was achieved with stenting in 100% of patients in both groups. Major complications, which included vascular dissection requiring additional stent placement and distal embolism, occurred in three of the 26 patients (11%) with covered stents and two of the 28 (7%) with bare metal stents (P ⫽ .66). There were no proceduralrelated mortalities. There was no statistically significant difference between the two groups with regard to stent diameters. Twelve of the 26 patients (46%) with covered stents had one or both iliac stents dilated to only 6 or 7 mm in diameter; in 14 of the 26 patients (54%), the smallest stent diameter was 8 –10 mm. In the patients with bare metal stents, 11 of the 28 patients (40%) had a 6 –7-mm-diameter stent used and 17 (60%) had stents dilated to 8 –10 mm in diameter (P vs patients with covered stents ⫽ .784). The left and right stents were the same size or within 1 mm of each other in every case in both groups. The stents extended more than 1 cm above the aortic bifurcation to cover distal aortic disease in five of the 26 patients (19%) with covered stents and eight of the 28 (28%) with bare metal stents (P ⫽ .53). One patient in the covered stent group had a distal aortic stent placed in addition to the CIA kissing stents. Additional EIA interventions were performed in the same procedural setting in 14 of the 26 patients (54%; 12 underwent stent placement and two underwent percutaneous transluminal angioplasty [PTA]) with covered stents and 12 of the 28 (43%; 10 underwent stent placement and two underwent PTA) with bare metal stents (P ⫽ .586). Additional femoropopliteal revascularization with PTA, stent placement, or bypass grafting was performed in five of the 26 patients (19%) with covered stents and three of the 28 (11%) with bare metal stents (P ⫽ .46). 998 • Outcomes of Covered Kissing Stents Compared with Bare Metal Stents Figure 2. (a– c) Initial anterioposterior images from DSA shows proximal left common iliac occlusion (a) treated with bilateral covered kissing stents (b,c) (iCAST stents, arrows in c). (d) CT angiogram obtained at 12-month follow-up shows patency and absence of intimal hyperplasia. The ABIs before and after the procedure are summarized in Table 3. At baseline, there were no statistically significant differences between the limbs or the groups (P ⫽ .314). The ABIs increased in both study groups after revascularization. ABIs (in the left and right limb) improved from an average of 0.74 and 0.61, respectively, before the procedure to 0.83 and 0.87, respectively, at discharge for the covered stent group and from 0.77 and 0.70 to 0.92 and 0.91, respectively, for the bare metal stent group (covered stent vs bare metal stent groups, P ⫽ .81). Immediate clinical success, based on an immediate improvement in the ABI of more than 0.1, was similar between both groups and achieved in 24 of the 26 patients (92%) with covered stents and 24 of the 28 (86%) with bare metal stents. Clinical follow-up with ABIs was available in all patients. Imaging follow-up was available in 15 of the 26 patients (57%) with covered stents and 19 of the 28 (68%) with bare metal stents. July 2010 JVIR The median follow-up was 21 months (20 months for covered stents vs 25 months for bare metal stents; range, 1– 62 months). Twenty-two of the 26 patients (85%) with covered stents versus 15 of the 28 (54%) with bare metal stents (P ⫽ .02) had sustained improvement in clinical symptoms during the follow-up period on the basis of the Fontaine classification (Table 4). Two of the 26 patients (8%) with covered stents had no initial improvement in symptoms but chose not to undergo any additional procedures during the follow-up period. Two patients in the covered stent group had worsening symptoms during followup, and both required revascularization with thrombolysis of the thrombosed stents followed by balloon angioplasty. Thirteen patients in the bare metal stent group described worsening symptoms during the follow-up period. Of these 13 patients, 12 required additional procedures for target vessel revascularization, including an aortobifemoral bypass graft (n ⫽ 1), additional stent placement (n ⫽ 4), and balloon angioplasty alone (n ⫽ 7). One patient in the bare metal stent group underwent a major amputation. Ten of the 26 patients (39%) with covered stents continued to smoke after stent placement, compared with 13 of the 28 patients (46%) with bare metal stents (P ⫽ .59). There was no significant decrease in ABIs in the covered stent group during the follow-up period, with the ABIs showing little change (0.83 and 0.87 after the procedure and 0.80 and 0.88 at latest follow-up for the right and left limbs, respectively). However, there was a significant decrease in the ABIs for the bare metal stent group, with follow-up ABIs of 0.74 and 0.79 compared with discharge values of 0.92 and 0.91 for the right and left limbs, respectively (P ⫽ .003). With use of Kaplan-Meier analysis, primary patency rates at 1 and 2 years were 92% and 92% for covered stents and 78% and 62% for bare metal stents, respectively (P ⫽ .023) (Fig 3). Overall patency rates (combing both groups) were not affected by patient sex, stent diameter (greater or less than 8 mm), external iliac and/or femoropopliteal interventions, or cessation of smoking. Volume 21 Number 7 Sabri et al Table 1 Summary of Demographics Parameter Covered Stents (n ⫽ 26) Bare Metal Stents (n ⫽ 28) 61 ⫾ 10.2 61.5 ⫾ 12.8 17 9 25 (96) 13 (50) 13 (50) 3 (12) 15 13 25 (89) 11 (39) 13 (46) 1 (4) .612 .584 .999 .342 18 (70) 20 (77) 21 (75) 23 (82) .764 .741 Mean age (y) Sex M F Hypertension Diabetes mellitus Coronary artery disease Renal impairment (creatinine level ⬎2 mg/dL) Hyperlipidemia Smoking history P Value .885 .418 Note.—Numbers in parentheses are percentages. Table 2 Summary of Clinical and Anatomic Findings Parameter Covered Stents (n ⫽ 26) Bare Metal Stents (n ⫽ 28) 21 (81) 5 (19) 21 (75) 7 (25) 7 (27) 9 (35) 6 (23) 4 (15) 13 (46) 13 (46) 2 (7) 0 (0) 0 (0) 8 (31) 1 (4) 2 (7) 4 (15) 0 (0) 14 (54) 0 (0) 22 (78) 3 (11) 2.2 ⫾ 2.1 2.1 ⫾ 1.6 4.3 ⫾ 3.2 1.4 ⫾ 1.7 1.6 ⫾ 1.7 3.1 ⫾ 3.1 Fontaine classification II III–IV TASC II classification A B C D CIA disease Bilateral occlusion Unilateral occlusion with contralateral stenosis Unilateral occlusion with normal contralateral artery Bilateral stenosis Unilateral stenosis with normal contralateral artery Runoff weighting Right Left Right ⫹ left P Value .747 .034 .134 Note.—Numbers in parentheses are percentages. DISCUSSION The management of symptomatic atherosclerotic occlusive disease of the iliac arteries has been dramatically altered by the use of permanent metal endoprostheses (stents). Clinical success rates of 70%–92% at 2 years have been reported for bare metal stents in the CIA (21,22). Patients with CIA origin occlusive lesions, with or without adjacent distal aortic disease, represent a complex subgroup of patients because of the technical challenges as- sociated with stent placement and the variable results with endovascular therapy reported in the literature (11,23–25) Although encouraging results were seen using the kissing balloon technique in 1991 for aortic bifurcation and proximal iliac lesions (26), the longterm benefit from iliac artery angioplasty is limited by elastic recoil of the lesion and arterial dissections. Early application of stents at the aortic bifurcation revealed that kissing stents are • 999 often needed to achieve an adequate angiographic result. Kissing stents are now commonly applied for aortic bifurcation and iliac origin occlusive lesions. Unfortunately, clinical results are still discouraging compared with those seen with focal CIA disease (8,10,11,13,25,27–30). Primary patency rates of 58%– 87% at 2 years are typical of the results reported, which are inferior to the results seen with focal CIA disease (10,13,27). The reasons for the inferior results with the application of kissing stents at the aortic bifurcation compared with single CIA stents remain unclear and are probably multifactorial. The results associated with the use of iliac artery kissing stents have been found to be particularly poor when the stents extend into the aorta far enough to overlap at least one-half the width of a stent (28). A higher incidence of acute stent thrombosis suggests that flow disturbance or increased thrombogenicity or lack or neoendothelialization of the free end of the bare stents within the aortic lumen may be important (30). However, the only factors that have been shown to affect iliac stent patency are stent size less than 7 mm and possibly EIA disease (31). Reconstruction of the aortic bifurcation by using covered stents rather than bare metal stents may provide more laminar flow, decreased thrombogenicity, less chance for prolapse of plaque through the covered stent, and less ingrowth of hyperplastic tissue–-a concept easily extrapolated from the experience with covered iliac stents (32). Several studies have demonstrated the efficacy of using stentgrafts for aorto-iliac occlusive disease, with overall primary patency ranging from 70% to 85% at 1 year (33–37). However, the use of stent-grafts for aortic bifurcation occlusive disease has not been widely adopted mainly due to the required large introducer sheath sizes in the face of potentially small access vessels, costs, and lack of a U.S. Food and Drug Administration–approved covered stent for this specific indication. The covered stents used in this study were balloon-expandable, unlike the other available stent-grafts, which are self-expanding. It also provides the advantage of being able to be delivered through a relatively small access sheath (7 F). The results presented herein dem- 1000 • Outcomes of Covered Kissing Stents Compared with Bare Metal Stents Table 3 Summary of ABIs Parameter Covered stents Before the procedure After the procedure At follow-up Bare metal stents Before the procedure After the procedure At follow-up Right ABI Left ABI 0.74 ⫾ 0.21 0.83 ⫾ 0.23 0.80 ⫾ 0.21 0.61 ⫾ 0.18 0.87 ⫾ 0.22 0.88 ⫾ 0.17 0.77 ⫾ 0.28 0.92 ⫾ 0.17 0.74 ⫾ 0.24 0.70 ⫾ 0.20 0.91 ⫾ 0.21 0.79 ⫾ 0.21 Note.—For covered stents, the P values for right ABIs were .028 for comparisons before and after stent placement and .21 for comparisons after stent placement and at follow-up; the P values for left ABIs were .001 for comparisons before and after stent placement and .82 for comparisons after stent placement and at follow-up. For bare metal stents, the P values for right ABIs were .012 for comparisons before and after stent placement and .003 for comparisons after stent placement and at followup; the P values for left ABIs were .002 for comparisons before and after stent placement and .025 for comparisons after stent placement and at follow-up. Table 4 Findings at Clinical Follow-up Finding Covered stents Clinical improvement Stable Clinical worsening Bare metal stents Clinical improvement Stable Clinical worsening No. of Patients Additional Intervention Performed during Follow-up 22 2 2 None None PTA (n ⫽ 1), surgical bypass (n ⫽ 1) 15 0 13 None NA PTA (n ⫽ 8), stent placement (n ⫽ 3), Surgical bypass (n ⫽ 1), major amputation (n ⫽ 1) Note.—The median follow-up was 20 months for covered stents and 25 months for bare metal stents. NA ⫽ not applicable. onstrate a clinically and statistically significant difference in the patency rates of covered versus bare metal balloon-expandable stents employed in the treatment of atherosclerotic occlusive disease of the aortic bifurcation and proximal CIAs (Fig 3). This improved patency of covered stents was identified despite the increased severity in runoff disease and the more adverse TASC II classification of the aortoiliac disease in the patients with covered stents. A median clinical follow-up of 25 months in the patients with bare metal stents and 20 months in the patients with covered stents suggests that this difference in clinical and patency results is durable. Only two of the 24 patients (8.3%) who experienced immediate benefit in the covered stent group had stent occlusion during the follow-up period. Both patients had occluded EIA stents and ipsilateral internal iliac artery occlusion at follow-up, which may have contributed to the thrombosis of the CIA stent. However, it is difficult to attribute this only to the EIA stents because approximately half of the patients in both study groups received EIA stents. It is worth mentioning that the antiplatelet therapy used in these two patients (81–325 mg of acetylsalicylic acid a day for life and 75 mg of clopidogrel a day for a minimum of 30 days) was similar to that used by the remainder of the covered stent group. None of the other patients in the covered stent group presented with instent restenosis. In-stent restenosis or July 2010 JVIR target vessel occlusion requiring intervention was visible in 38% of the bare metal stents at 24-month follow-up. The superior clinical and patency results seen with covered stents compared with bare metal stents in this patient population is likely due to the prevention of in-stent intimal hyperplasia and the improved laminar flow hemodynamics, which is likely due to a decrease in turbulent flow in the distal aorta (Fig 4). The patency rates associated with iliac artery stents have been reported to be negatively affected by female sex, small vessel size, presence of distal aortic and external iliac disease, and smoking continuation after the procedure (14,24,38,39). With the exception of distal aortic disease, our study failed to show a negative effect on patency for any of the above factors in either group. There was no difference in patency between men and women in either group, the men in the covered stent group did statistically better (P ⫽ .033) than the men in the bare metal stent group, and the women in the covered stent group trended toward better outcomes than the bare metal stent group (P ⫽ .075). Within both groups, the patency of small- (⬍ 8 mm) versus large- (ⱖ 8 mm) diameter stents was not statistically different. The large-diameter stents had better patency in the covered stent group compared with the bare metal stent group (P ⫽ .0087). Small-diameter stents showed a trend toward improved patency in the covered stent group as compared with the bare metal stent group (P ⫽ .0894). Extending the stents proximally above the aortic bifurcation in a “crossing” manner to cover distal aortic disease has been reported to have worse patency rates. Greiner et al (28) reported that the primary and assisted primary patency rates at 2 years for the “noncrossing” group were significantly higher (94.1% and 100%, respectively) than those obtained in the “crossing” group (33.2% and 45.3%, respectively). Sharafuddin et al (39) also reported that the radial mismatch secondary to proximal extension of the stents into the abdominal aorta is a significant determinant of restenosis. However, stents that extended more than 1 cm above the aortic bifurcation remained patent in four of five patients (80%) in the covered stent group Volume 21 Number 7 Sabri et al Figure 3. Kaplan Meier survival curve shows improved patency of the covered stents versus the bare metal stents at 1 and 2 years (92 and 92% vs 84 and 72%, respectively). Figure 4. CT angiogram obtained at 12 months in the coronal plane demonstrates in-stent stenosis in a bare metal stent (arrowheads). versus only two of eight (25%) in the bare metal stent group (Figs 2,4). Our findings do support the previously published data, which indicate that both the presence of distal aortic disease and extension of the stents above the bifurcation tend to produce lower patency rates with bare metal stents. Due to the small sample size in our study (combined, 13 patients), the utility of covered stents in this particular application can only be inferred. Additional EIA interventions, which were performed in 54% of patients in the covered stent group and 43% of patients in the bare metal stent group, had no significant effect on the patency of the stents. However, the two patients in the covered stent group who had occlusion at follow-up both had EIA interventions where the ipsilateral EIA stent was also found to be occluded at the same time. Overall patency was not affected by the cessation of smoking. However, in a subgroup analysis, the treated vascular segment remained patent in nine of the 10 patients (90%) with covered stents who continued to smoke compared with five of 13 patients (38%) with bare metal stents who continued to smoke (P ⫽ .029). These findings likely reflect the overall superiority of the covered stents. Aortoiliac artery stent placement techniques, the clinical indications for intervention, and the treatment of patients with atherosclerotic aortoiliac disease have shown little evolution during the period of this study. The major change that occurred in endovascular therapy that led to this study was the new availability of a Food and Drug Administration–-approved expanded polytetrafluoroethylene– covered, balloon-expandable stent that was used in an off-label fashion to • 1001 treat occlusive disease of the aortoiliac segments. The slightly worse runoff quality and the increased percentage of total occlusion treated in the covered stent group may have been related to an inherent bias among the interventionalists that the covered stents were more likely to provide a more durable clinical result. In addition, the four patients receiving bare metal stents after the date where covered stent usage started were in cases where the operator believed the anatomy was favorable and the use of covered stents was not necessary. As with all retrospective studies of procedures and new technology, substantial biases can alter results and conclusions, but the use of historical controls provided closely matched populations in this study, which helps minimize these biases. The demographic data and cardiovascular risk factors of the two groups were also very similar (Table 1). However, the study remains limited by its nonrandomized, partially retrospective, and single-institution nature. Risk factors for bare metal kissing stent stenosis include the distance the stents extend into the distal aorta, vessel size, and runoff (28,31). Further research is needed to explore why bare metal stents occlude at a higher rate when used in the kissing-stent configuration compared with use in iliac arteries and to determine what benefit covered stents might have in the kissing-stent configuration. Wall motion at the aortic bifurcation is more complicated than in the iliac artery, and wall shear stress may be important to stent outcomes (40). Although the covered stent used in this study is rigid compared with most bare metal stents, it may provide protection from wall shear–induced intimal hyperplasia. Differences in inflammatory response have already been demonstrated in femoral artery stenting compared with stent placement in the iliac arteries or carotid arteries (41), and the response of the aortic bifurcation may be different than that expected in the aorta or the iliac arteries. However, covered stents prevent intimal hyperplasia only in the middle portion of the stent and do not prevent intimal hyperplasia at the ends of the stent (42). In a sheep model study, polytetrafluoroethylenecovered stents had a similar late lumen loss compared to bare metal stents (43). 1002 • Outcomes of Covered Kissing Stents Compared with Bare Metal Stents The most unique aspect of bare metal kissing stents, compared with conventional iliac stent placements, is that there is a free-floating stent in the distal aorta. Although cause and effect have not been shown, the free-floating stent is the most likely culprit for the inferiority of bare metal stents in this setting and points to the potential advantage of covered stents. There is a case report of cytopathology of failed bare metal kissing stents that demonstrated intimal hyperplasia and thrombus within the stents and the free-floating portions of the stents (30). The correlation between the distance a bare metal stent extends into the aorta and early failure is further evidence that the amount of free-floating stent in the distal aorta is an important determinate of patency (28). The data presented herein suggest that covered stents may provide some protection from the effect of having bare metal in the lumen of the distal aorta. In summary, the use of covered balloon-expandable iliac kissing stents, particularly when the stents extend into the aorta, appears to be superior to the use of bare metal balloon-expandable stents at 2 years of follow-up and suggests that employment of this technology for atherosclerotic aortoiliac occlusive disease, in appropriately selected patients, may be warranted. 6. 7. 8. 9. 10. 11. 12. 13. Acknowledgment: The authors acknowledge the tireless efforts of Tammy Amos in the preparation of this manuscript. 14. References 1. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007; 45 (Suppl S):S5–S67. 2. Rutherford RB. Options in the surgical management of aorto-iliac occlusive disease: a changing perspective. Cardiovasc Surg 1999; 7:5–12. 3. Brewster DC. Current controversies in the management of aortoiliac occlusive disease. J Vasc Surg 1997; 25:365– 379. 4. Tegtmeyer CJ, Kellum CD, Kron IL, Mentzer RM Jr. Percutaneous transluminal angioplasty in the region of the aortic bifurcation: the two-balloon technique with results and long-term follow-up study. Radiology 1985; 157: 661– 665. 5. Kuffer G, Spengel F, Steckmeier B. Percutaneous reconstruction of the aor- 15. 16. 17. tic bifurcation with Palmaz stents: case report. Cardiovasc Interven Radiol 1991; 14:170 –172. Palmaz JC, Encarnacion CE, Garcia JJ, et al. Aortic bifurcation stenosis: treatment with intravascular stents. J Vasc Interv Radiol 1991; 2:319 –323. Mendelsohn FO, Santos RM, Crowley JJ, et al. Kissing stents in the aortic bifurcation. Am Heart J 1998; 136:600 – 605. Mouanoutoua M, Maddikunta R, Allagabond S, et al. Endovascular intervention of aortoiliac occlusive disease in high-risk patients using the kissing stents technique: long-term results. Catheter Cardiovasc Interv 2003; 60: 320 –326. Greiner A, Dessl A, Klein-Weigel P, et al. Kissing stents for treatment of complex aortoiliac disease. Eur J Vasc Endovasc Surg 2003; 26:161–165. Mohamed F, Sarkar B, Timmons G, Mudawi A, Ashour H, Uberoi R. Outcome of “kissing stents” for aortoiliac atherosclerotic disease, including the effect on the non-diseased contralateral iliac limb. Cardiovasc Interv Radiol 2002; 25:472– 475. Haulon S, Mounier-Vehier C, Gaxotte V, et al. Percutaneous reconstruction of the aortoiliac bifurcation with the “kissing stents” technique: long-term follow-up in 106 patients. J Endovasc Ther 2002; 9:363–368. Brittenden J, Beattie G, Bradbury AW. Outcome of iliac kissing stents. Eur J Vasc Endovasc Surg 2001; 22:466 – 468. Scheinert D, Schroder M, Balzer JO, Steinkamp H, Biamino G. Stent-supported reconstruction of the aortoiliac bifurcation with the kissing balloon technique. Circulation 1999; 100(19 Suppl): II295–II300. Murphy TP, Khwaja AA, Webb MS. Aortoiliac stent placement in patients treated for intermittent claudication. J Vasc Interv Radiol 1998; 9:421– 428. Kedora J, Hohmann S, Garrett W, Munschaur C, Theune B, Gable D. Randomized comparison of percutaneous Viabahn stent grafts vs prosthetic femoral-popliteal bypass in the treatment of superficial femoral arterial occlusive disease. J Vasc Surg 2007; 45: 10 –16. Saxon RR, Coffman JM, Gooding JM, Ponec DJ. Long-term patency and clinical outcome of the Viabahn stentgraft for femoropopliteal artery obstructions. J Vasc Interv Radiol 2007; 18:1341–1349. Saxon RR, Dake MD, Vogelzang RL, Katzen BT, Becker GJ. Randomized, multicenter study comparing expanded polytetrafluoroethylene-covered endoprosthesis placement with percutaneous transluminal angioplasty in the treat- 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. July 2010 JVIR ment of superficial femoral artery occlusive disease. J Vasc Interv Radiol 2008; 19:823– 832. Sacks D, Marinelli DL, Martin LG, Spies B. Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. Technology Assessment Committee. J Vasc Interv Radiol 1997; 8:137–149. Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 1997; 26: 517–538. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol 2003; 14: S199 –S202. Bosch JL, van der Graaf Y, Hunink MG. Health-related quality of life after angioplasty and stent placement in patients with iliac artery occlusive disease: results of a randomized controlled clinical trial. The Dutch Iliac Stent Trial Study Group. Circulation 1999; 99:3155–3160. Klein WM, van der Graaf Y, Seegers J, et al. Dutch iliac stent trial: long-term results in patients randomized for primary or selective stent placement. Radiology 2006; 238:734 –744. Nawaz S, Overtoom TC, van Sambeck M, et al. Aortoiliac stenting, determinants of clinical outcome. Eur J Vasc Endovasc Surg 1999; 17:351–359. Yilmaz S, Sindel T, Golbasi I, Turkay C, Mete A, Luleci E. Aortoiliac kissing stents: long-term results and analysis of risk factors affecting patency. J Endovasc Ther 2006; 13:291–301. van’t Riet M, Spronk S, Jonkman J, Den Hoed T. Endovascular treatment of atherosclerosis at the aortoiliac bifurcation with kissing stents or distal aortic stents: a temporary solution or durable improvement? J Vasc Nurs 2008; 26: 82– 85. Tegtmeyer CJ, Hartwell GD, Selby JB, Robertson R Jr, Kron IL, Tribble CG. Results and complications of angioplasty in aortoiliac disease. Circulation 1991; 83(2 Suppl):I53–I60. Bjorses K, Ivancev K, Riva L, Manjer J, Uher P, Resch T. Kissing stents in the aortic bifurcation: a valid reconstruction for aorto-iliac occlusive disease. Eur J Vasc Endovasc Surg 2008; 36: 424 – 431. Greiner A, Muhlthaler H, Neuhauser B, et al. Does stent overlap influence the patency rate of aortoiliac kissing stents? J Endovas Ther 2005; 12: 696 –703. Rosset E, Malikov S, Magnan PE, et al. Endovascular treatment of occlusive lesions in the distal aorta: midterm results in a series of 31 consec- Volume 21 30. 31. 32. 33. 34. Number 7 utive patients. Ann Vasc Surg 2001; 15:140 –147. Saker MB, Oppat WF, Kent SA, et al. Early failure of aortoiliac kissing stents: histopathologic correlation. J Vasc Interv Radiol 2000; 11:333–336. Reyes R, Carreira JM, Gude F, et al. Long-term follow-up of iliac wallstents. Cardiovasc Interv Radiol 2004; 27:624 – 631. Lammer J, Dake MD, Bleyn J, et al. Peripheral arterial obstruction: prospective study of treatment with a transluminally placed self-expanding stent-graft. International Trial Study Group. Radiology 2000; 217:95–104. Maynar M, Zander T, Qian Z, et al. Bifurcated endoprosthesis for treatment of aortoiliac occlusive lesions. J Endovas Ther 2005; 12:22–27. Rzucidlo EM, Powell RJ, Zwolak RM, et al. Early results of stent-grafting to treat diffuse aortoiliac occlusive Sabri et al 35. 36. 37. 38. 39. disease. J Vasc Surg 2003; 37: 1175–1180. Nevelsteen A, Lacroix H, Stockx L, Wilms G. Stent grafts for iliofemoral occlusive disease. Cardiovasc Surg 1997; 5:393–397. Ali AT, Modrall JG, Lopez J, et al. Emerging role of endovascular grafts in complex aortoiliac occlusive disease. J Vasc Surg 2003; 38:486 – 491. Sanchez LA, Wain RA, Veith FJ, Cynamon J, Lyon RT, Ohki T. Endovascular grafting for aortoiliac occlusive disease. Semin Vasc Surg 1997; 10:297–309. Sapoval MR, Chatellier G, Long AL, et al. Self-expandable stents for the treatment of iliac artery obstructive lesions: long-term success and prognostic factors. Am J Roentgenol 1996; 166: 1173–1179. Sharafuddin MJ, Hoballah JJ, Kresowiki TF, et al. Long-term outcome following stent reconstruction of the aortic bifurcation and the role of geometric de- 40. 41. 42. 43. • 1003 terminants. Ann Vasc Surg 2008; 22: 346 –357. La Disa JF Jr, Olson LE, Molthen RC, et al. Alterations in wall shear stress predict sites of neointimal hyperplasia after stent implantation in rabbit iliac arteries. Am J Physiol Heart Circ Physiol 2005; 288:H2465–H2475. Schillinger M, Exner M, Miekusch, W, et al. Inflammatory response to stent implantation: differences in femoralpopliteal, iliac, and carotid arteries. Radiology 2002; 224:529 –535. Yuan GJ, Ohki T, Martin ML, et al. The effect of non-porous PTFE-covered stents on intimal hyperplasia following balloon arterial injury in minipigs. J Endovasc Surg 1998; 5:349 –358. Cejna M, Virmani R, Jones R, et al. Biocompatibility and performance of the Wallstent and the Wallgraft, Jostent, and Hemobahn stent-grafts in a sheep model. J Vasc Interv Radiol 2002; 13:823– 830.