American Journal of Infection Control 41 (2013) S97-S104
Contents lists available at ScienceDirect
American Journal of Infection Control
American Journal of
Infection Control
journal homepage: www.ajicjournal.org
Original research article
The crucial role of wiping in decontamination of high-touch environmental
surfaces: Review of current status and directions for the future
Syed A. Sattar PhD a, *, Jean-Yves Maillard PhD b
a
b
Centre for Research on Environmental Microbiology, Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada
Pharmaceutical Microbiology, Cardiff School of Pharmacy and Pharmaceutical Sciences, Cardiff University, Cardiff, UK
Key Words:
Wiping
Towelettes
Disinfection
Nosocomial pathogens
Infection control
The testing and label claims of disinfectants to wipe high-touch environmental surfaces rarely reflect
their field use where contact times are in seconds with only microliters of the disinfectant deposited on
a unit surface area. Therefore, such products must be properly assessed with mechanical/chemical action
combined. We critically review current wipe test methods and propose future approaches.
Copyright Ó 2013 by the Association for Professionals in Infection Control and Epidemiology, Inc.
Published by Elsevier Inc. All rights reserved.
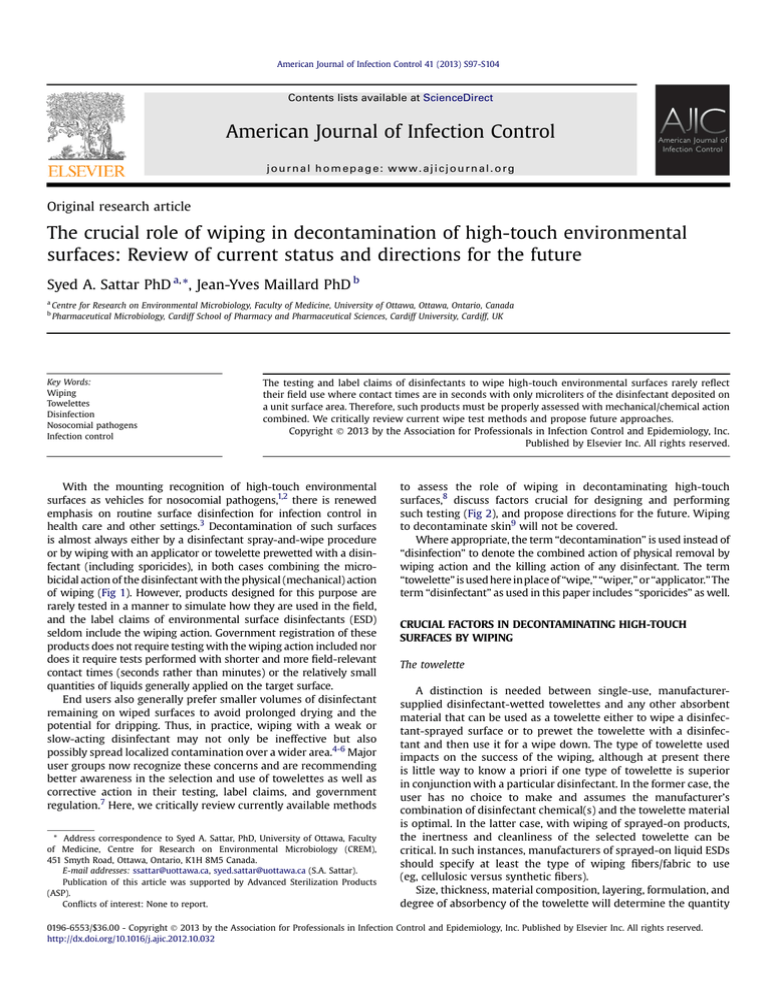
With the mounting recognition of high-touch environmental
surfaces as vehicles for nosocomial pathogens,1,2 there is renewed
emphasis on routine surface disinfection for infection control in
health care and other settings.3 Decontamination of such surfaces
is almost always either by a disinfectant spray-and-wipe procedure
or by wiping with an applicator or towelette prewetted with a disinfectant (including sporicides), in both cases combining the microbicidal action of the disinfectant with the physical (mechanical) action
of wiping (Fig 1). However, products designed for this purpose are
rarely tested in a manner to simulate how they are used in the field,
and the label claims of environmental surface disinfectants (ESD)
seldom include the wiping action. Government registration of these
products does not require testing with the wiping action included nor
does it require tests performed with shorter and more field-relevant
contact times (seconds rather than minutes) or the relatively small
quantities of liquids generally applied on the target surface.
End users also generally prefer smaller volumes of disinfectant
remaining on wiped surfaces to avoid prolonged drying and the
potential for dripping. Thus, in practice, wiping with a weak or
slow-acting disinfectant may not only be ineffective but also
possibly spread localized contamination over a wider area.4-6 Major
user groups now recognize these concerns and are recommending
better awareness in the selection and use of towelettes as well as
corrective action in their testing, label claims, and government
regulation.7 Here, we critically review currently available methods
* Address correspondence to Syed A. Sattar, PhD, University of Ottawa, Faculty
of Medicine, Centre for Research on Environmental Microbiology (CREM),
451 Smyth Road, Ottawa, Ontario, K1H 8M5 Canada.
E-mail addresses: ssattar@uottawa.ca, syed.sattar@uottawa.ca (S.A. Sattar).
Publication of this article was supported by Advanced Sterilization Products
(ASP).
Conflicts of interest: None to report.
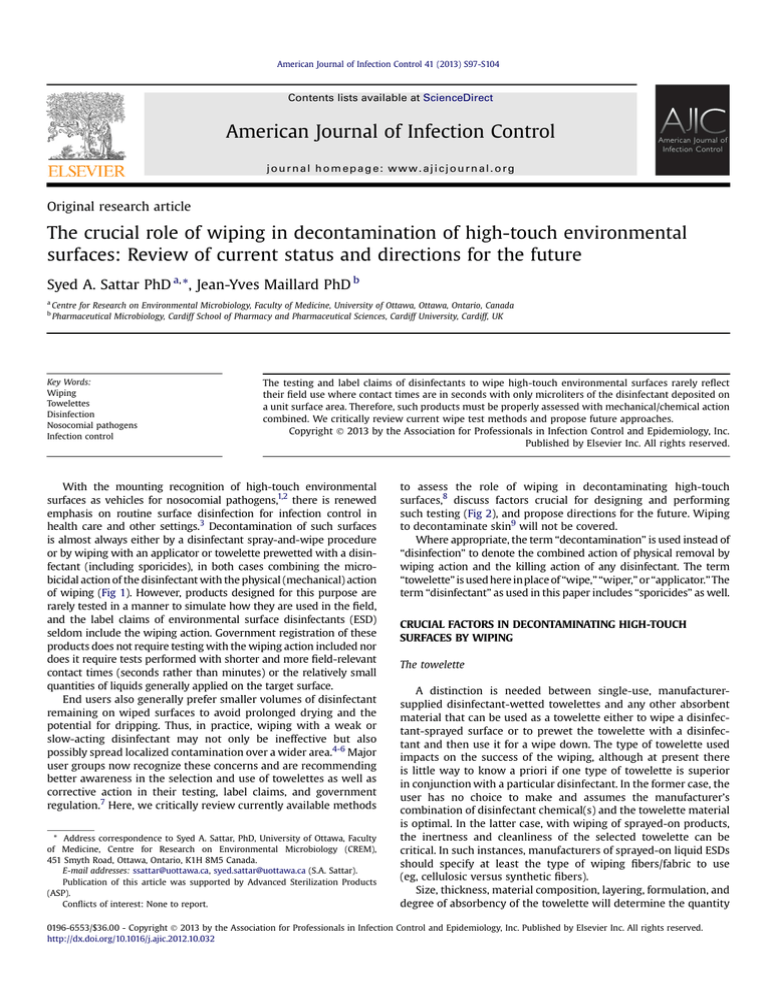
to assess the role of wiping in decontaminating high-touch
surfaces,8 discuss factors crucial for designing and performing
such testing (Fig 2), and propose directions for the future. Wiping
to decontaminate skin9 will not be covered.
Where appropriate, the term “decontamination” is used instead of
“disinfection” to denote the combined action of physical removal by
wiping action and the killing action of any disinfectant. The term
“towelette” is used here in place of “wipe,” “wiper,” or “applicator.” The
term “disinfectant” as used in this paper includes “sporicides” as well.
CRUCIAL FACTORS IN DECONTAMINATING HIGH-TOUCH
SURFACES BY WIPING
The towelette
A distinction is needed between single-use, manufacturersupplied disinfectant-wetted towelettes and any other absorbent
material that can be used as a towelette either to wipe a disinfectant-sprayed surface or to prewet the towelette with a disinfectant and then use it for a wipe down. The type of towelette used
impacts on the success of the wiping, although at present there
is little way to know a priori if one type of towelette is superior
in conjunction with a particular disinfectant. In the former case, the
user has no choice to make and assumes the manufacturer’s
combination of disinfectant chemical(s) and the towelette material
is optimal. In the latter case, with wiping of sprayed-on products,
the inertness and cleanliness of the selected towelette can be
critical. In such instances, manufacturers of sprayed-on liquid ESDs
should specify at least the type of wiping fibers/fabric to use
(eg, cellulosic versus synthetic fibers).
Size, thickness, material composition, layering, formulation, and
degree of absorbency of the towelette will determine the quantity
0196-6553/$36.00 - Copyright Ó 2013 by the Association for Professionals in Infection Control and Epidemiology, Inc. Published by Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.ajic.2012.10.032
S98
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
Fig 1. Possible scenarios for decontaminating high-touch environmental surfaces by
wiping (modified from Sattar and Springthorpe29).
of a disinfectant retained in and released from it. The physical
structure of the towelette also influences the degree of contact it
makes with the surface as well as its cleaning/abrasion of that
surface and the capacity it has to pick up and hold soils, microbes,
and particles as the surface is wiped. It can, therefore, also influence
the level of redeposition of any previously accumulated microbes or
soil onto the most recently wiped surface area. Its chemical structure as well as prior use history and the degree of soil load it carries
influence whether and to what extent the towelette interacts with
the disinfectant chemicals. Such interactions weaken the disinfecting power by partial or complete neutralization of the disinfectant(s). The more surface contacted and the more soil acquired,
the weaker the disinfectant becomes. Towelettes employed in the
wiping of disinfectant-sprayed surfaces are often used for repeated
wiping with no or only cursory washing/decontamination in
between. Even those towelettes marketed as single use are often
used repeatedly and beyond their capacity to disinfect the surface
they are wiping. Thus, the level of the active(s) brought in contact
with the target surface and the inherent ability of the towelette
to react with and neutralize the active(s) in the disinfectant10 are
key factors that must be considered to prevent spread of microbial
contamination over wider areas. In specific settings, the use of
prewetted towelettes was shown to be better than a spray-andwipe procedure in decreasing bioburden from surfaces.11
Target nosocomial pathogens
In health care settings in particular, the types and levels of
pathogen contamination on high-touch environmental surfaces is
often unknown. Also, nosocomial pathogens vary widely in their
susceptibility to ESD depending on their biology, growth phase,
environmental conditions such as relative humidity (RH) and air
temperature, nature of the surface, and type and level of the
associated soil. Therefore, for routine wiping to be effective, it must
be designed and executed to cover as wide a variety of commonly
encountered pathogens as possible. The advent of sporulating
Clostridium difficile as an important nosocomial pathogen is now
a significant challenge for environmental decontamination in general12,13; the higher microbicide resistance of its spores14 requires
the use of towelettes with sporicidal chemicals.6
Regulatory agencies in North America (US Environmental
Protection Agency [EPA]; Health Canada)15,16 and Europe (European
Committee for Standardization [CEN])17 accept, with some exceptions (EPA and viruses), the use of surrogates of nosocomial pathogens to permit label claims for ESD. The criteria for choosing
a surrogate in testing towelettes would be the same as those
Fig 2. The combined effect of various factors impacting the outcome of decontamination of high-touch surfaces by wiping with a towelette.
currently employed in carrier testing of ESD, and the surrogate to be
selected should withstand the initial drying of the inoculum on the
carrier to be used for wiping. Safety, ease of handling, and ready
quantitation of viability are also important considerations. In
addition, the surrogate must be reasonably resistant to common
types of ESD to make label claims meaningful.18,19 Table 1 is a list of
recommended surrogates with justifications for inclusion in the
testing of towelettes. The listed surrogates represent all 5 major
groups of nosocomial pathogens and belong to biosafety levels 1
and 2.20 Several of those are already widely accepted in testing
chemical microbicides in general.21
The wiping action
The type and frequency of wiping action as well as the pressure
exerted during wiping can profoundly influence the outcome of
decontamination, and they also are among the more difficult
variables to control in the field. However, any standardized testing
of towelettes and wiping action must precisely control all these
factors for reproducible data on towelette performance and assess
all tested products under the same test conditions.
Surface to be wiped
A combination of use history, topography, accessibility, orientation, and inherent disinfectant demand of the target surface will
determine the efficiency of wiping and also the level of contact
between the target pathogen(s) and ESD. The surface to be wiped
must not only permit direct contact between the target pathogen(s)
and ESD but also allow for a sufficiently long dwell time to achieve
the desired level of decontamination. In general, the ease of
decontamination by wiping is directly related to the degree of
smoothness of the surface. However, if a representative environmental surface is to be selected for standardized evaluation of
wiping performance and decontamination efficacy, it should be one
with an uneven topography and also widely available.22
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
S99
Table 1
Surrogates recommended for the testing of towelettes
Organism (ATCC number)
Category
Biosafety
level
Nosocomial
pathogen?
Staphylococcus aureus (6538)
Gram-positive
coccus
2
Yes
Acinetobacter baumannii (19606)
Gram-negative
bacillus
2
Yes
Candida albicans (10231)
Nonfilamentous or
yeast-like fungus
2
Yes
Aspergillus niger (64958)
Filamentous fungus
2
Yes
Mycobacterium terrae (15755)
Environmental
mycobacterium
2
Rare cases of
human infections
Bacillus subtilis (19659)
Aerobic spore former
1
No
Clostridium difficile (43598)
Anaerobic spore
former
2
Yes
Feline calicivirus (VR-782)
Small, nonenveloped
virus
2
No
Comment(s)
A common nosocomial pathogen; frequently used as a surrogate for
testing microbicides against vegetative bacteria (ASTM 2011).21,40
Survives well on drying of inocula on carriers.
Higher intrinsic resistance to microbicides than other gram negatives
and also withstands drying well. Increasingly important as
a nosocomial pathogen.41
An opportunistic nosocomial pathogen. Widely used as a surrogate
for testing ESD and topicals against nonfilamentous fungi
(ASTM 2011).21
Aspergillus42 and other species of filamentous fungi are emerging
nosocomial pathogens. The conidia of A niger are used in testing ESD
against filamentous fungi (ASTM 2011).21
Several species of nontuberculous or environmental mycobacteria are
increasingly being incriminated in health care-acquired infections.43
Mycobacteria in general also show a higher resistance to ESD.
M terrae is now widely accepted as a surrogate for testing the
mycobactericidal activity of microbicides (ASTM 2011).21,44
Commonly used as a surrogate to test chemicals against aerobic
spore-forming bacteria.
Now a significant nosocomial pathogen. EPA now requires ESD to be
tested against nontoxigenic strains of these spores for label claims of
sporicidal activity.45
Safe and relatively easy to culture and assay for infectivity in vitro;
withstands drying well,46 and also shows relatively high resistance to
ESD; a good surrogate for nosocomial viral pathogens including
human noroviruses.29
ATCC, American Type Culture Collection.
Contact time between ESD and target pathogen(s)
Product performance criterion
As mentioned above, the contact time between the towelette
and the target surface during normal wiping is often no longer than
a few seconds.4,23 Therefore, the desired level of reduction in
microbial contamination with a combination of wiping and disinfection must be achieved within that brief period for the decontamination to be effective under actual use conditions.
For government registration, an ESD should achieve a 3- to
5-log10 reduction in the viability of tested organisms (except for
bacterial spores), depending on the test method acceptable to the
target regulatory agency. This level of product performance is based
more on practicality than on any documented links between log10
kill and reductions in the rates of nosocomial infections spread via
high-touch environmental surfaces. A recent study of environmental surfaces in patient wards found the highest counts
of heterotrophic bacteria to be about 2.0 103 colony-forming
units/in2 (3 102 colony-forming units/cm2) on the bedrails24;
the numbers of nosocomial pathogens such as methicillin-resistant
Staphylococcus aureus were barely detectable on the bedrails at the
same site. These numbers are of the same level of magnitude as
those previously reported in the literature.25
Should an ESD assessed in a towelette test achieve the same
level of performance for registration without wiping or a higher
level because of the combined action of disinfection and the
physical action of wiping? As stated before, wipe testing is generally more demanding because of the much shorter contact times as
well as the lower volumes of disinfectant deposited over a unit
surface area. This critical issue should perhaps be discussed
together with the regulatory community once sufficient data from
well-designed and standardized wipe-testing studies become
available. For wiping of food-contact surfaces, the EPA requires
a 5-log10 reduction in the viability of the tested bacteria.26
Disinfectant
Whereas environmental surfaces in health care facilities may
be wiped down after terminal fumigation of a ward, or after
applying a disinfectant powder for a spill, most commonly used
ESDs are liquids. The speed and spectrum of microbicidal action of
any such liquid are both crucial for successful decontamination by
wiping. A combination of the chemical action of ESD and the
physical action of wiping must achieve the desired level of
reduction in contamination ideally against common nosocomial
vegetative bacteria, mycobacteria, viruses, and fungi. For spray-on
products, it may be feasible to wait for the label-recommended
contact time of several minutes before wiping is initiated. For
products that are applied with a single-use, manufacturer
supplied towelette, the wiping and contact occur simultaneously,
and so it is critical that the ESD act within a few seconds. Towelettes claiming residual microbicidal activity on the wiped surface
will require careful evaluation and potential benefits as well as
any risks the long-term use of such products may entail in
promoting antimicrobial resistance.
As mentioned above, effective wiping of surfaces suspected of
contamination with spore formers such as Clostridium difficile
would require sporicidal ESD.6 The relationship between detergent activity and microbicidal efficacy in the formulation is critical; an imbalance will lead to inefficient bioburden removal from
surfaces and the release of pathogens from the towelette.6
Recovery of test organism(s) from the carrier
Efficient recovery of the organism used for experimental
contamination of the carrier is critical for a quantitative and
reproducible assessment of the combined effect of disinfection and
wiping. Flat and relatively small carriers are the most desirable for
ease of wiping and complete immersion of the carrier into
S100
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
a relatively small volume of eluent-neutralizer; this is especially
important when testing against viruses. The eluent and disinfectant
neutralizer must first be tested for efficiency as well as safety to the
test organism(s) and cell cultures when working with viruses.22
The human factor
Even when the most effective product is used, the degree of
diligence on the part of the housekeeping staff will ultimately
determine the success of the wiping action. It is now well documented that the wiping of high-touch environmental surfaces is
either neglected altogether or carried out in too cursory a manner
to be effective.27 Improper wiping can be counterproductive by
spreading localized contamination over a wider area.5,6 It should be
noted that wiping is a generic term that means different things to
different individuals. Properly conducted wipe testing should give
guidance on the types and extent of wiping that might be valuable
inclusions in product labeling.
contamination and may spread it over a wider area during the
decontamination if not killed effectively at the point of contact.
Therefore, it is imperative that the combined action of disinfection
and wiping be fast and efficient enough to reduce the pathogen
load to as low a level as possible to avoid spreading the pathogen
over a wider area.4,5 The potential for such pathogen spread over
a wider area during wiping is particularly high with inappropriate
detergent/microbicide ratio and the ability of certain towelette
materials to release microbial contamination.6
CURRENTLY AVAILABLE PROTOCOLS FOR TESTING OF
TOWELETTES
RH and air temperature together can determine the rate of loss
of wetness on the towelette itself and, therefore, the amount of ESD
delivered to the point of contact with the contaminated surface.
This points to the need for proper packaging of towelettes by
manufacturers and appropriate care in the storage and use of the
packaged towelettes by the end user. RH and air temperature can
also influence the rate of evaporation of liquids from environmental
surfaces, thus affecting microbicidal efficacy on surfaces.
Table 2 lists the available wipe test protocols with their attributes in relation to the critical factors listed above and summarizes
the information from 4 peer-reviewed studies published thus far.
With some exceptions (EPA 2001),26 test protocols currently available to assess disinfecting towelettes for regulatory purposes are
semiquantitative at best, and they also do not incorporate crucial
and field-relevant factors such as pressure and the relatively short
contact during wiping nor can they properly control for the ratio
between the volume of the disinfectant applied and the unit surface
area being wiped.
Currently, AOAC International and ASTM International are the
only 2 standards-setting organizations with published methods for
testing towelettes for their microbicidal activity (Table 2). They are
similar in their basic design and also subject to the same limitations. There is also a dearth of towelette test methods in peerreviewed literature.
Disinfectant/towelette ratio
A LOOK AT THE FUTURE
Marketed single-use towelettes generally have a relatively
constant ratio between an individual towelette and the volume of
disinfectant soaked in it as long as the canister or pouch is properly
closed, stored, and used within its recommended shelf life. Much
greater variability occurs when a dry towelette is wetted with
a disinfectant on site or when a disinfectant is first sprayed on a
surface and it is then wiped. For economy and for environmental
and human safety,8 the most desirable approach would be to have
just enough disinfectant to wet the towelette and to deliver moisture to the surface to be decontaminated without it dripping. How
long the towelette remains damp enough during use would depend
on the type and level of volatile organics (eg, ethanol) the ESD
contains but also on the end user for those towelettes that need
activation with water prior to use.
Any future attempts at developing standardized protocols to
assess the decontaminating potential of towelettes should consider
the following:
Should towelettes be tested against individual types and species
of pathogens? We consider such an approach unnecessary and
impractical. Instead, carefully chosen surrogates should be used
to maintain the cost of product development competitive while
keeping the product label uncomplicated and user-friendly. In
particular, the “fear-factor” should never be the basis for selecting
a pathogen for testing and label claims, especially in the absence of
any credible evidence for its ability to survive on and be transmitted
by high-touch environmental surfaces.19 It should be noted that it is
also possible to evaluate ESD against defined cocktails of microorganisms,28 a somewhat more complex but necessarily more realistic approach.
If and what type of soil load should be used in testing the decontaminating activity of towelettes? Pathogens discharged by infected
hosts are always contained in body fluid of one kind or another.
The organic and inorganic materials in such body fluids represent
the “soil load,” which not only affords protection to the pathogen but
can also react with the disinfectant and quench its microbicidal
activity. In addition, even brand new environmental surfaces often
exert a demand on ESD, and those frequently cleaned also contain
residual amounts of soil. Therefore, the decontaminating potential of
towelettes should be tested in the presence of a reasonable amount
of added soil load to better simulate the impact of the factors noted
above. The ingredients of any soil load selected should be available
readily and widely at a reasonable cost from reputable sources; they
also must be compatible with any organism used in the testing.29
Should test organisms be recovered from the towelette used for
decontamination? Recovering the test organism from the contaminated towelette is neither easy nor needed. Efficient elution of
microbes from towelettes is often difficult because of their porous
Relative humidity and air temperature
Ratio between disinfectant volume and surface area to be wiped
In addition to the volume of disinfectant soaked in a towelette,
the efficiency of surface decontamination is related to the total area
rubbed with a given towelette. As a towelette moves over the
surface there is depletion of the disinfectant in it and also simultaneous accumulation of microbial and other contamination from
the surface being wiped. In other words, a towelette could rapidly
lose its decontaminating potential if used beyond its “capacity.”
Therefore, label directions must provide the user with guidance
on the surface area to be decontaminated with a given towelette
for optimal effectiveness.
Potential for microbial transfer
Surface contamination is rarely uniform and is likely to be
concentrated in certain “spots.” Wiping a contaminated surface
for infection control inevitably dislodges wet or dried microbial
Table 2
Listing of available methods to test towelettes for decontamination of high-touch, hard, nonporous surfaces
Source
Standards-setting organizations
AOAC International’s Standard 961.0235
Comments
A bacterial inoculum, with or without an added soil load, is dried on several
microscope slides. Depending on the test, 10-60 slides are then sprayed
individually with a disinfectant. At the end of the contact time, each slide
is separately placed in a neutralizer-containing recovery medium. For a “pass,”
10/10 slides must show no growth, and no more than 1 “failure” allowed with 60
slides.
Can be used to generate data to register aerosol/trigger-sprayed disinfectants in the
United States. Requires additional details, eg, better standardization of the
starting bacterial inocula and conditions for drying them on the carriers, to
reduce variability in results. The volume of the liquid sprayed per unit surface
areas may be higher than that normally used in the field. The recommended
contact time of 10 minutes is also not in line with normal use. The large number
of carriers required in each test makes the procedure time-consuming and labor
intensive. The carrier surface is relatively smooth and thus easier to disinfect.
This method cannot differentiate between mechanical bacterial removal by wiping
and the killing action of the disinfectant in the towelette. It is also subject to
individual variations in the wiping procedure.
Designed for use with vegetative bacteria, mycobacteria, and filamentous fungi for
testing precleaned or soiled surfaces. Although the contact time is not specified,
wiping of 10 carriers with 1 towelette would extend it well beyond what is
relevant in the field. The carrier surface is relatively smooth.
ASTM International’s Work Item 3290836
This quantitative method, which uses Petri plates as carriers for dried inocula of
vegetative bacteria, is soon expected to become a standard of ASTM.
ASTM International’s standard E236237
To wipe carriers (glass slides) with towelettes impregnated or presaturated with
a disinfectant. After specified contact time, each carrier is placed in a neutralizercontaining recovery medium and incubated. As an option, the used towelette, or
a portion of the liquid expressed from it, is also cultured for surviving test
organisms.
This phase 2, step 2 test incorporates a back and forth wiping procedure across 4 test
areas, simulating in-use conditions. It also aims to evaluate the sustained activity
of various disinfectant ingredients on surfaces.
Four-field test: CEN test under
development38
Peer-reviewed publications
Three stage-test4-6,11
US Environmental Protection Agency
US EPA39
Draft Interim Guidance for Nonresidual
Sanitization of Hard Inanimate Food
Contact Surfaces Using Presaturated
Towelettes26
This test is currently being considered, and the final details are not available yet;
thus, comments cannot be made on how the wiping process and the transfer of
microbial contamination are strictly controlled.
This “three-step” method to test removal, killing, and transfer of bacteria was
designed after close observations of the use of commercial towelettes on hightouch surfaces in an intensive care unit of a hospital. Control or test towelettes are
mounted on the tip of a drill to wipe a metal disk; the drill rotation (set at 60
rpm), contact time (set at 10 seconds), and contact pressure (set from 100 g to
300 g) are controlled. The used towelette is brought into contact with an agar
medium containing a neutralizer to assess the extent of transfer of viable
organisms to a clean surface.
The method originally described by Williams et al4 was used to measure the
efficacy of a number of different towelettes against MRSA. This quantitative
method incorporates a reasonably short contact time of 10 seconds based on
field use of wiping. The starting inoculum on each disk usually >6-log10 of cfu
represented a high level of contamination. Also, contacting the used towelette
with an already moist surface of agar, potentially over-estimated the extent of
bacterial transfer.
Whereas Williams et al.4,5 compared the efficacy of different commercially
available towelettes against MRSA, Panousi et al11 compared the efficacy of
prewetted towelettes with that of disinfectant spray-on towelettes. Siani et al6
measured the sporicidal activity of a number of towelettes against C difficile
spores. In this study, towelettes varied widely in their ability to remove the
spores. None showed the required level of sporicidal action even after a 5minute contact. There was repeated transfer of the spores from all but 1 type of
towelette. In fact, the detergency in the towelettes released more cfu of the
spores.
This quantitative study with a relatively short contact time points to the
importance of proper testing of “sporicidal” claims of towelettes to avoid
enhancing the risk of spread of the spores over a wider area during wiping.
Overall, used towelettes with weak disinfection activity can transfer viable bacteria
upon as many as 8 consecutive adpressions.
Uses the feline calicivirus as a surrogate for human norovirus to assess virucidal
activity of presaturated or impregnated towelettes on hard, nonporous surface
disinfection. Virus suspension, with an added soil load, is spread on inside bottom
surface of glass Petri plates and dried. Ten carriers (Petri dishes) are wiped with 1
towelette. Product effectiveness criterion is a 4-log10 reduction in virus viability
as compared with the controls.
AOAC standard 961.0235 adapted to wiping glass, metallic, plastic, or ceramic
carriers contaminated with either Staphylococcus aureus or Escherichia coli, with
a soil load. Other organisms to be listed on label could also be tested. Product
performance criterion is 99.999% (5 log10) in viability of test organism.
Acceptable for data submission to EPA for registration of a product as a virucide.
Although the contact time is not specified, wiping of 10 carriers with 1 towelette
would extend it well beyond what is relevant in the field. The carrier surface is
relatively smooth and thus easier to disinfect.
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
Summary of procedure
The method is quite flexible and based on a reasonably short contact time of 30
seconds. It is also quantitative because it clearly specifies the level of microbial
load on the carriers at the start and gives a clear product performance criterion.
Inclusion of E coli as a test organism may be inappropriate because it does not
withstand drying well.
S101
(Continued on next page)
CFU, Colony-forming units; MRSA, methicillin-resistant Staphylococcus aureus.
Can be used to generate data to register presaturated towelettes in the United
States. Requires additional details, eg, better standardization of the starting
bacterial inocula and conditions for drying them on the carriers, to reduce
variability in results. Individual variations in wiping procedure may also impact
the results.
Method for Disinfection Using
Presaturated Towelettes26
AOAC standard 961.02 method35 adapted for work with Mycobacterium bovis (BCG).
Glass slides inoculated with the test organism (with soil load) and dried. Ten
slides are then wiped with 1 towelette. The glass slides are then placed in
a neutralizer-containing recovery medium and incubated.
A bacterial inoculum, with or without an added soil load, is dried on several
microscope slides. Depending on the test, 10-60 slides are then wiped with
a disinfectant-soaked towelette. At the end of the contact time, each slide is
separately placed in a neutralizer-containing recovery medium. For a “pass,”
10/10 slides must show no growth, and no more than 1 “failure” is allowed with
60 slides.
Summary of procedure
Source
Table 2
Continued
Towelette test for mycobacteria15
Comments
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
Suggested contact time is 10 minutes which is too long for the way towelettes are
used in the field. The test may take as long as 60 days to complete because of the
slow growth of M bovis. The carrier surface is relatively smooth.
S102
nature and the potential for irreversible microbial attachment to
individual fibers30; applying strong shearing forces may cause
microbial inactivation. Furthermore, relatively large volumes of an
eluent/neutralizer are required to properly immerse the entire
towelette for microbial recovery. Sufficiently large volumes of such
eluates are generally difficult to process when working with
viruses. Properly discarding used towelettes, even if they contain
residual levels of contamination, should pose virtually no threat to
patients and staff. The approach of squeezing out the disinfectant
from the test towelette before or/and after use and testing a portion
of the properly neutralized liquid for its microbicidal activity has
been used, but its relevance and practicability remain questionable.
Should product labels not specify the ratio between disinfectant
volume and the surface area to be decontaminated by wiping? The
volume of disinfectant in individual presoaked towelettes marketed commercially remains fairly constant. However, the end user
is hardly ever provided with guidance on how large a surface area
to be decontaminated with a given towelette. Such information is
crucial because the disinfecting power of a towelette is rapidly
depleted during its application with the accumulation of soil and
also because of the evaporation of any liquid disinfectant in it.
There are additional factors to consider when dealing with
towelettes to be used for decontaminating surfaces prewetted with
a disinfectant. Towelettes used in such situations may vary widely in
their nature, absorbency, degree of cleanliness, and potential to react
with and neutralize the disinfectant. These factors individually or in
combination could impact the outcome of decontamination. Here
also, an end user is not provided with clear guidance on the type of
towelette to be used and the unit surface area to be decontaminated
with it. The testing and label claims of presoaked towelettes as well
as those for decontaminating prewetted surfaces must take these
factors into consideration to better inform the end user and thus
ensure greater success in infection prevention and control.
What controls should be included in testing the decontaminating
activity of towelettes: Apart from the usual sterility checks on culture
media and reagents, a wipe test must include the following controls:
(1) the number of viable organisms placed on each carrier to be
wiped; (2) assessment of loss in viability of the test organism during
the initial drying of the carriers; (3) physical removal of the test
organism from the carrier by a control or blank towelette; this control
is needed to differentiate between the microbicidal action of the
disinfectant and the simple removal of the contamination by the
wiping action alone. However, obtaining towelettes without the
disinfectant already soaked in them may be difficult. In case such
“blanks” become available, the challenge will also be to soak them
in a control fluid because of the strong hydrophobicity of the fabric.
Addition of a mild detergent and overnight soaking may help
provided the control fluid is proven to be safe for the test organism(s).
Alternatively, the disinfectant-soaked test towelette can be brought
into contact with the contaminated carrier for 5 to 10 seconds
without any wiping action to assess the effect of exposure to the
disinfectant alone in the towelette.31 Although only relatively small
volumes of test disinfectant may be left on wiped carriers, it still
is necessary to confirm that its microbicidal activity has been effectively neutralized immediately at the end of the contact time.
DISCUSSION
Even though high-touch environmental surfaces may on occasion introduce pathogens directly into patients, more commonly
bare or gloved hands become the vehicles after contact with hightouch environmental surfaces.12 Towelettes used for the decontamination of high-touch surfaces have a role to play in decreasing
microbial bioburden from surfaces if they can demonstrate they can
remove and/or kill target microorganisms from surfaces and
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
prevent the transfer of microbial contamination. The use of sporicidal towelettes combined with appropriate education of the end
users and proper auditing can substantially decrease the nosocomial spread of C difficile.32
However, the label claims of disinfectants for wiping of hightouch environmental surfaces are not tenable either on scientific
or practical grounds. Such claims are based on unrealistically long
contact times, absence of wiping action, and testing against a limited
number of relatively disinfectant-sensitive nosocomial pathogens.
This situation continues to generate a false sense of security and loads
the environment with potentially unsafe chemicals while exposing
patients and caregivers to undue health risks.9 In spite of the
mounting evidence for the spread of nosocomial pathogens through
high-touch environmental surfaces13 and the benefits of decontaminating such surfaces12,33 for infection prevention and control,
the frequency and quality of such decontamination remain woefully
inadequate.27 Indeed, cursory wiping of high-touch surfaces with
weak or slow-acting ESD may spread localized contamination over
a wider area, thus making routine housekeeping counterproductive.
Pathogens can be readily transferred between hands and hightouch environmental surfaces.12,34 Therefore, effective infection
control requires both regular hand hygiene as well as the decontamination of high-touch surfaces.3 Although towelettes are also
marketed for the decontamination of hands,9 they are excluded
from consideration here because of fundamental differences in test
protocols for their evaluation.
Some disinfectants in towelettes may damage hands on
repeated contact. Manufacturers provide instructions for suitable
gloves to be worn when wiping. Also, any sharps or pieces of broken
glass must first be safely removed from any surface to be wiped.
This critical review of the current situation is meant to focus on
the urgent need for better protocols to test towelettes to ensure the
development/marketing of more efficient products and thus aid in
improved infection prevention. Whereas the convenience of use is an
important factor in the increasing popularity of disinfectant-wetted
towelettes, they also contribute to workplace safety and reduce the
use of disinfectant chemicals. In certain applications, prewetted
towelettes offer better bioburden control compared with spray-on
towelettes.11 Vertical surfaces (eg, light switches) and round ones
(eg, bedrails) can be more readily and conveniently decontaminated
using towelettes than by spraying of disinfectants. On the other hand,
prespraying then wiping of surfaces has the advantage of being able
to extend the contact time and to provide a larger amount of ESD per
unit area. Proper testing protocols are required to back up claims of
either product type and to provide adequate instructions for use
in preventing the spread of pathogens.
Here, we reviewed the use of towelettes mainly against bacterial
pathogens, viruses, and endospores based on the available literature. There is no information on the efficacy of towelettes against
bacterial biofilms.
Acknowledgment
The authors thank Susan Springthorpe of CREM for her critical
review of the manuscript and Jason Tetro of CREM for providing
much assistance in the search for relevant literature.
References
1. Otter JA, Yezli S, French GL. The role played by contaminated surfaces in the
transmission of nosocomial pathogens. Infect Control Hosp Epidemiol 2011;32:
687-99.
2. Shaughnessy MK, Micielli RL, DePestel DD, Arndt J, Strachan CL, Welch KB, et al.
Evaluation of hospital room assignment and acquisition of Clostridium difficile
infection. Infect Control Hosp Epidemiol 2011;32:201-6.
3. Dancer SJ. The role of environmental cleaning in the control of hospitalacquired infection. J Hosp Infect 2009;73:378-85.
S103
4. Williams GJ, Denyer SP, Hosein IK, Hill DW, Maillard J-Y. The development of
a new three-step protocol to determine the efficacy of disinfectant wipes on
surfaces contaminated with Staphylococcus aureus. J Hosp Infect 2007;67:329-35.
5. Williams GJ, Denyer SP, Hosein IK, Hill DW, Maillard J-Y. Limitations of the
efficacy of surface disinfection in the healthcare setting. Infect Control Hosp
Epidemiol 2009;30:570-3.
6. Siani H, Cooper C, Maillard J-Y. Efficacy of “sporicidal” wipes against Clostridium
difficile. Am J Infect Control 2011;39:212-8.
7. Royal College of Nursing. The selection and use of disinfectant wipes. London, 2011. Available from: http://www.rcn.org.uk/__data/assets/pdf_file/0011/
382538/003873.pdf. Accessed September 24, 2012.
8. Huslage K, Rutala WA, Sickbert-Bennett E, Weber DJ. A quantitative approach
to defining “high-touch” surfaces in hospitals. Infect Control Hosp Epidemiol
2010;31:850-3.
9. Larson EL, Cohen B, Baxter KA. Analysis of alcohol-based hand sanitizer
delivery systems: efficacy of foam, gel, and wipes against influenza A (H1N1)
virus on hands. Am J Infect Control 2012;40:806-9.
10. Goldsmith MT, Latlief MA, Friedl JL, Stuart LS. Adsorption of available chlorine
and quaternary by cotton and wool Fabrics from disinfecting solutions. Appl
Microbiol 1954;2:360-4.
11. Panousi MN, Williams GJ, Girdlestone S, Maillard J-Y. Use of alcoholic wipes
during aseptic manufacturing. Lett Appl Microbiol 2009;48:648-51.
12. Kundrapu S, Sunkesula V, Jury LA, Sitzlar BM, Donskey CJ. Daily disinfection of
high-touch surfaces in isolation rooms to reduce contamination of healthcare
workers’ hands. Infect Control Hosp Epidemiol 2012;33:1039-42.
13. Weber DJ, Rutala WA, Miller MB, Huslage K, Sickbert-Bennett E. Role of hospital
surfaces in the transmission of emerging health care-associated pathogens:
norovirus, Clostridium difficile, and Acinetobacter species. Am J Infect Control
2010;38:S25-33.
14. Perez J, Springthorpe VS, Sattar SA. Activity of selected oxidizing microbicides
against the spores of Clostridium difficile: relevance to infection control. Am J
Infect Control 2005;33:320-5.
15. US Environmental Protection Agency. 2012 Antimicrobial testing methods &
procedures (ATMP). Available from: http://www.epa.gov/pesticides/methods/
atmpindex.htm. Accessed on February 08, 2013.
16. Health Canada Guidance Document. Disinfectant drugs. 2007. Public Works
and Government Services Canada. Available from: http://www.hc-sc.gc.ca/dhpmps/alt_formats/hpfb-dgpsa/pdf/prodpharma/disinf_desinf-eng.pdf. Accessed
September 22, 2012.
17. European Commission. Technical guidance document in support of the directive
98/8/EC concerning the placing of biocidal products on the market: guidance on
data requirements for active substances and biocidal products. European
Commission, Brussels, Belgium. Available from: http://ihcp.jrc.ec.europa.eu/our_
activities/public-health/risk_assessment_of_Biocides/doc/TNsG/TNsG_DATA_
REQUIREMENTS/TNsG-Data-Requirements.pdf. Accessed September 22, 2012.
18. Sattar SA. Hierarchy of susceptibility of viruses to environmental surface
disinfectants: a predictor of activity against new and emerging viral pathogens.
J AOAC Int 2007;90:1655-8.
19. Sattar SA. Promises and pitfalls of recent advances in chemical means of preventing the spread of nosocomial infections by environmental surfaces. Am J
Infect Control 2010;38:S34-40.
20. US Centers for Disease Control and Prevention. Biosafety in microbiological
and biomedical laboratories. 5th ed. CDC, Atlanta, GA. Available from: http://
www.cdc.gov/biosafety/publications/bmbl5/index.htm. Accessed September
22, 2012.
21. ASTM International. Standard quantitative disk carrier test method for determining the bactericidal, virucidal, fungicidal, mycobactericidal & sporicidal
activities of liquid chemicals. Document E-2197. West Conshohocken [PA]:
ASTM International; 2011.
22. Springthorpe VS, Sattar SA. Carrier tests to assess microbicidal activities of
chemical disinfectants for use on medical devices & environmental surfaces.
J AOAC International 2005;88:182-201.
23. Berendt AE, Turnbull L, Spady D, Rennie R, Forgie SE. Three swipes and you’re
out: how many swipes are needed to decontaminate plastic with disposable
wipes? Am J Infect Control 2011;39:442-3.
24. Sexton JD, Tanner BD, Maxwell SL, Gerba CP. Reduction in the microbial load on
high-touch surfaces in hospital rooms by treatment with a portable saturated
steam vapor disinfection system. Am J Infect Control 2011;39:655-62.
25. Page K, Wilson M, Parkin IP. Antimicrobial surfaces and their potential in
reducing the role of the inanimate environment in the incidence of hospitalacquired infections. J Mater Chem 2009;19:3819-31.
26. US Environmental Protection Agency 2001. Draft Interim guidance for nonresidual sanitization of hard inanimate food contact surfaces using pre-saturated
towelettes. Available from: http://www.epa.gov/oppad001/towelette.htm. Accessed September 25, 2012.
27. Carling PC, Bartley JM. Evaluating hygienic cleaning in health care settings: what
you do not know can harm your patients. Am J Infect Control 2010;38:S41-50.
28. Sabbah S, Springthorpe S, Sattar SA. Use of a mixture of surrogates for infectious bioagents in a standard approach to assessing disinfection of environmental surfaces. Appl Environ Microbiol 2010;76:6020-2.
29. Sattar SA, Springthorpe VS. Disinfection of environmental surfaces to interrupt
the spread of nosocomial pathogens: a critical look at use patterns & expectations. In: Rutala WA, editor. APIC preconference symposium on “Disinfection, Sterilization & Antisepsis: Principles, Practices, Current Issues & New
Research, ” Tampa, FL; 2007. p. 82e96.
S104
S.A. Sattar, J.-Y. Maillard / American Journal of Infection Control 41 (2013) S97-S104
30. Downey AS, Da Silva SM, Olson ND, Filliben JJ, Morrow JB. Impact of processing
method on recovery of bacteria from wipes used in biological surface sampling.
Appl Environ Microbiol 2012;78:5872-81.
31. Hernández A, Carrasco M, Ausina V. Mycobactericidal activity of chlorine
dioxide wipes in a modified prEN 14563 test. J Hosp Infect 2008;69:384-8.
32. Carter Y, Barry D. Tackling C difficile with environmental cleaning. Nursing
Time 2011;107:22-5.
33. Boyce JM, Havill NL, Lipka A, Havill H, Rizvani R. Practices. Infect Control Hosp
Epidemiol 2010;31:99-101.
34. Cheeseman KE, Denyer SP, Hosein IK, Williams GJ, Maillard J-Y. Evaluation of
the bactericidal efficacy of three different alcohol handrubs against 57 clinical
isolates of Staphylococcus aureus. J Hosp Infect 2009;72:319-25.
35. AOAC Official Method 961.02. Germicidal spray products as disinfectants.
Official method of analysis, 2009. Gaithersburg [MD]: AOAC International;
2009.
36. ASTM International. New test method for quantitative petri plate method
(QPM) for testing antimicrobial towelette products. Work item 32908. West
Conshohocken [PA]: ASTM International; 2012.
37. ASTM International. Standard practice for evaluation of pre-saturated or
impregnated towelettes for hard surface disinfection. Document E2362. West
Conshohocken [PA]: ASTM International; 2009.
38. CEN. Quantitative test method for the evaluation of bactericidal activity on
non-porous surfaces with mechanical action employing wipes or mops in the
medical area: test method and requirements (phase 2, step 2). CEN TC 216:
Draft 11e20118. Brussels [Belgium]: CEN; 2011.
39. US Environmental Protection Agency. Pre-saturated or impregnated towelettes confirmatory virucidal effectiveness; test using feline calicivirus as surrogate for norovirus. Available from: http://www.epa.gov/oppad001/pdf_files/
towelettes_confirmatory_virucidal.pdf. Accessed September 25, 2012.
40. US Environmental Protection Agency. 2012 Product performance test guidelines,
OCSPP 810.2200: Disinfectants for use on hard surfaces: efficacy data recommendations. Available from: http://www.regulations.gov/#!documentDetail;
D¼EPA-HQ-OPPT-2009-0150-0014. Accessed September 22, 2012.
41. Karageorgopoulos DE, Falagas ME. Current control and treatment of multidrugresistant Acinetobacter baumannii infections. Lancet Infect Dis 2008;8:7517-62.
42. Krishnan S, Manavathu EK, Chandrasekar PH. Aspergillus flavus: an emerging
non-fumigatus Aspergillus species of significance. Mycoses 2009;52:206-22.
43. Alexander S, John GT, Jesudason M, Jacob CK. Infections with atypical
mycobacteria in renal transplant recipients. Indian J Pathol Microbiol 2007;
50:482-4.
44. Sattar SA. Testing of chemicals as mycobactericidal agents. Chapter 6.3. In:
Fraise A, Maillard J-Y, Sattar SA, editors. Principles and practice of disinfection,
preservation and sterilization. 5th ed. Oxford [England]: Wiley-Blackwell; 2013.
45. US Environmental Protection Agency 2009. Guidance for the efficacy evaluation of products with sporicidal claims against Clostridium difficile. Available
from: http://www.epa.gov/oppad001/cdif-guidance.html. Accessed September
22, 2012.
46. Mattison K, Karthikeyan K, Abebe M, Malik N, Sattar SA, Farber JM, et al.
Survival of calicivirus in foods & on surfaces: experiments with feline calicivirus as a surrogate for norovirus. J Food Protect 2007;70:500-3.