Effect of Lidocaine on the Ventricular
Fibrillation Threshold in the Dog
during Acute Ischemia
and Premature Ventricular Contractions
By JOSEPH F. SPEAR, PH.D., E. NEIL MOORE, D.V.M., PH.D.,
and GAIRY GERSTENBLITH, M.D.
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
SUMMARY
The effect of lidocaine on the ventricular fibrillation threshold was investigated in the
anesthetized open-chest dog during paced supraventricular rhythm, during acute ligation
of the anterior descending coronary artery, and during premature ventricular contractions. The minimum current (in milliamperes) required to induce ventricular fibrillation
was determined by passing a train (100 Hz) of 10-14 constant-current pulses through
ventricular epicardial electrodes during the vulnerable period of the cardiac cycle.
Lidocaine was administered intravenously either as a sudden injection or as a "loading"
injection followed by a constant infusion. Following a single injection of 0.7 mg/kg the
blood lidocaine decreased to half its original arterial concentration in 9 min. After the
termination of a 50-60-min constant drip of 70 ,ug/kg/min which was preceded by a
loading injection of 2 mg/kg, the blood lidocaine concentration fell to 50% of its original
value in 31 min. Lidocaine at therapeutic blood levels (1.2-5.5 ug/ml) increased the
fibrillation threshold during paced supraventricular rhythm and reversed the fall in
fibrillation threshold accompanying acute myocardial ischemia and premature ventricular
contractions. The present studies quantify the ability of lidocaine to reduce the vulnerability of the heart to fibrillation during supraventricular rhythm, acute ischemia,
and premature ventricular beats and provide information concerning the metabolism of
lidocaine in the anesthetized dog.
Additional Indexing Words:
Ischemia
Vulnerability
Antiarrhythmia agent
Myocardial infarction
Sudden cardiac death
fibrillation was first described by Wiggers and
Wegria.1 In their investigations of vulnerability, Han et al.2A determined that a decrease in
the ventricular fibrillation threshold is associated with those factors which increase the
degree of nonuniformity of recovery of
excitability of ventricular muscle and predispose the heart to reentry. These same factors
are those associated clinically with a greater
risk of fibrillation. Lidocaine is an important
drug in the management of patients following
acute myocardial infarction.= 6 While it is
accepted that lidocaine does inihibit the
occurrence of postinfarctioii tachyarrhythmias,7 there is some doubt as to whether it has
T HE TECHNIC of passing current
through epicardial electrodes during
early diastole in order to test the vulnerability
of the ventricle or its tendency to undergo
From the Comparative Cardiovascular Studies Unit,
Department of Animal Biology, School of Veterinary
Medicine, and the Hospital of the University of
Pennsylvania, Department of Medicine, University of
Pennsylvania, Philadelphia, Pennsylvania.
Address for reprints: Dr. E. Neil Moore, Comparative Cardiovascular Studies Unit, School of Veterinary
Medicine, University of Pennsylvania, Philadelphia,
Pennsylvania 19104.
Received October 25, 1971; revision accepted for
publication January 27, 1972.
Circulation, Volume XLVI, July 1972
Defibrillation
65
66
a direct effect on the myocardium which
increases the fibrillation threshold. Bacaner8
reported that lidocaine had a negligible effect
on the fibrillation threshold while Shinohara9
reported positive results. In neither of these
studies, however, was the blood lidocaine
concentration monitored during the fibrillation
threshold determinations. In the present
studies the blood lidocaine concentration was
monitored while the ventricular fibrillation
threshold was determined during paced su-
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
praventricular rhythm, during acute ischemia,
and during premature ventricular beats.
Methods
The experiments were performed on 21 dogs,
of both sexes, anesthetized with sodium pentobarbital (30 mg/kg). The animals were maintained
by positive-pressure ventilation at a minute
volume determined from a body weight nomogram. The lead II electrocardiogram (ECG) was
monitored throughout the experiments. Control
experiments demonstrated that open-chest animals can be maintained for 5 hours in acid-base
balance as long as the fibrillation procedures are
carried out at 10-min or longer intervals. Openchest dogs which showed progressive metabolic
acidosis also showed a progressive decrease in
ventricular fibrillation threshold (VFT). In all of
the present experiments data were obtained from
animals which exhibited control VFT which did
not vary by more than 10% for 45 min to 1 hour
before each experimental manipulation. For data
to be acceptable the VFT had to return to control
value after the experimental manipulations.
Lidocaine was administered through a femoral
venous catheter, and arterial samples for blood
lidocaine determinations were obtained from the
abdominal aorta through an indwelling femoral
catheter. Lidocaine whole-blood concentrations
were determined as lidocaine hydrochloride
monohydrate using the gas chromatographic
technic. Lidocaine was administered either in a
single sudden injection (0.7 mg/kg) or in a
constant drip infusion (70 ,ug/kg/min) following a loading injection (2 mg/kg). The drip
infusion was terminated after 50-60 min. The
heart was exposed by a midsternal thoracotomy
and was suspended in a pericardial sling. Bipolar
stimulating electrodes were secured to the right
atrium, and the sinus node was crushed to permit
pacing the heart at a constant basic cycle length
of 380 msec for all experiments.
The ventricular fibrillation threshold (VFT)
was determined by passing a gated train of
impulses through bipolar electrodes sutured on
the right or left ventricule during the vulnerable
SPEAR ET AL.
period of the T wave of the ECG. The electrodes
(1 mm in diameter) were embedded in an acrylic
plaque which maintained their separation at 5
mm. The fibrillation pulses were 4 msec in
duration and occurred at 10-msec intervals (100
Hz). There were 10-14 of these pulses in the train.
They were synchronized to the atrial stimulus and
delivered after every twelfth ventricular response
during the threshold determinations. The current
delivered was measured directly by recording the
voltage drop across a precision 1 kohm resistor in
series with the electrodes. The VFT was
defined as the minimum current in milliamperes
(ma) which induced fibrillation. When fibrillation
ensued, the heart was immediately defibrillated
using a capacitor discharge DC defibrillator. The
placement and duration of the fibrillating train in
each case started within the absolute refractory
period of the beat to be tested and did not extend
beyond the absolute refractory period of the
ventricular beat evoked by the train. The analog
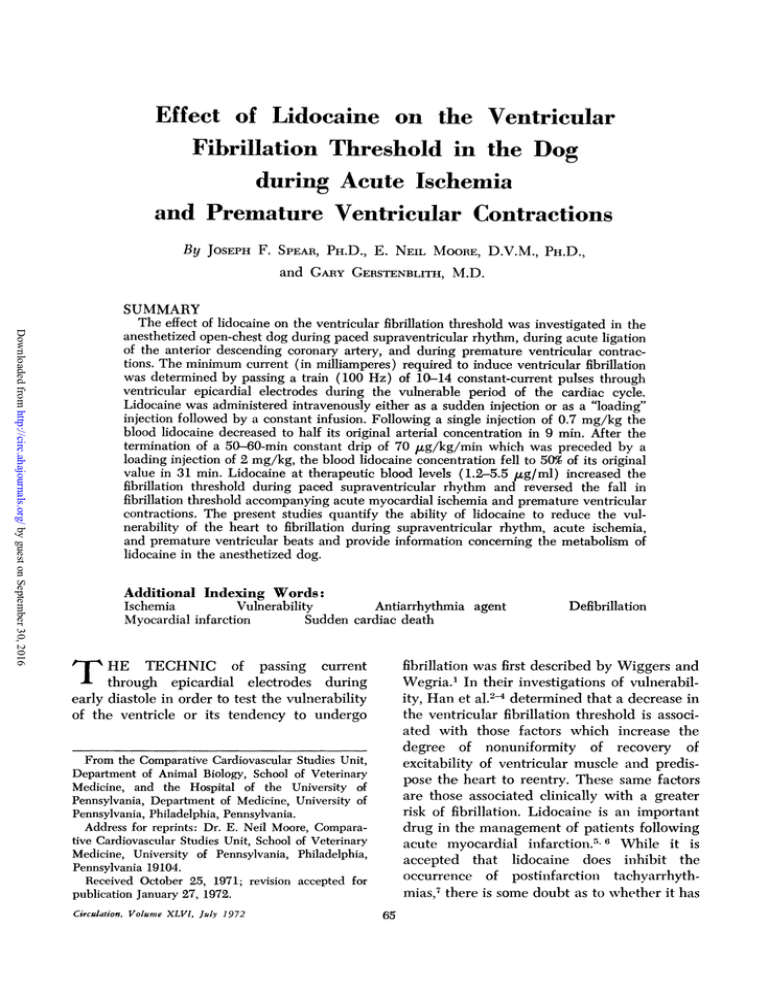
data of figure 1 demonstrates this for a paced
supraventricular beat (A) and for a premature
ventricular contraction (B). The heart was
allowed to recover for 10-15 minutes following
each determination.
In the experiments in which the threshold for
fibrillation was measured following a premature
ventricular beat, the premature beat was evoked
after every 12 normal beats by a single 4-msec
stimulus through the same ventricular electrodes
used for determining the fibrillation threshold.
The premature ventricular beat was the earliest
that could be evoked with a current of twice
threshold intensity delivered during the relative
refractory phase of the preceding normal beat.
The fibrillating train of pulses was then gated to
occur during the vulnerable period of the
premature ventricular beat.
In other experiments the threshold for fibrillation was determined during acute coronary
occlusion. Occlusion was reversibly attained in
the main left anterior descending coronary artery
or one of its large branches using a snare applied
around the vessel near its base. The fibrillating
electrodes were sutured onto the left ventricle.
The electrodes were placed so that they would be
within the ischemic area during the occlusion. For
each fibrillation threshold determination during
acute ischemia the coronary occlusion lasted less
than 2 min. The heart was allowed to recover for
10-15 min following each determination.
Results
Blood Lidocaine Levels foUowing an Intravenous
Injection and following a Constant Infusion
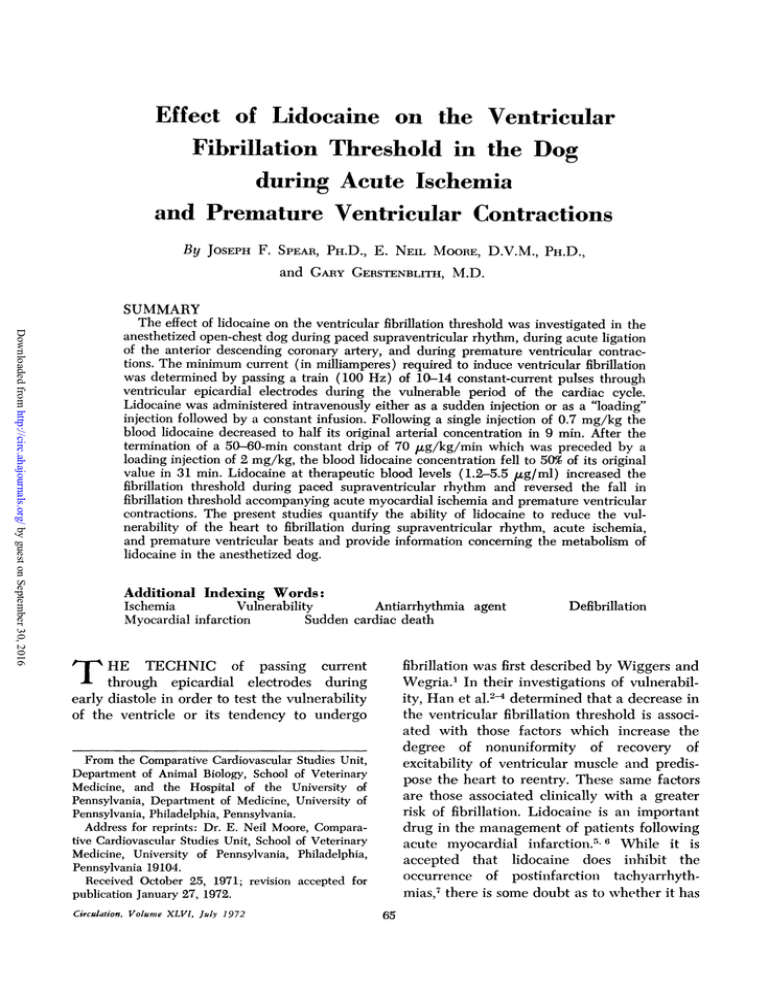
Figure 2 compares the time courses of the
disappearance of lidocaine from the blood
following a sudden injection of 0.7 mg/kg (A)
Circulation, Volume XLVI, July 1972
LIDOCAINE AND VENTRICULAR FIBRILLATION
67
A
ECG
RV
F
S
IIIIlIjj
-
-..
.
.......
.....A....
.0.
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
B
ECG
S
T
P
F
a
tWiUIlIIl
p
F
1111111il
a
-....1-l..
I.
,1
.,
,.
Figure 1
Analog data demonstrating the placement of the train of pulses used to test ventricular fibrillation threshold (VFT) are presented. (A) The procedure for testing the VFT for a paced supraventricular beat. (B) The procedure for testing a premature ventricular beat (PVC). The rapid
phases in the records have been retouched. ECG = lead II electrocardiogram; RV = right
ventricular epicardial electrogram recorded approximately 4 mm from the fibrillating electrodes;
S = the stimulus signal which indicates the timing of the stimulus evoking the premature
ventricular response (P), and the fibrillating train of pulses (F). T p7esents timing signals occurring at 100-msec intervals. On the left of A, the relationship of the fibrillating train to the
T wave in the ECG and in the local electrogram (RV) is shown; on the right, the result of
passing current through the fibrillating electrode is presented. Notice that, although the fibrillating train does evoke a response, the train still does not extend beyond the absolute refractory
period of the evoked response. On the left of B, the fibrillating train (F) is positioned across the
T wave of a stimulated PVC. On the right of B, during the passage of current through the
fibrillating electrodes, the train does not extend beyond the absolute refractory period of the
evoked response.
and following the termination of a constant
infusion of 70 ,ug/kg/min (B). In A, the log
of the arterial blood lidocaine concentration is
plotted against time following a single intravenous injection of lidocaine in seven dogs. To
allow time for intravascular mixing, the first
arterial samples were drawn after 1 or 2 min.
The initial blood concentrations ranged between 6.3 and 1.3 ,ug/ml. The regression line
Circulation, Volume XLVI, July 1972
at the Y intercept in A was 2.7 ,gg/ml, and it
fell to 50% of this value in 9 min. Virtually all
of the lidocaine was removed from the blood
within 30 min after the injection. In B of
figure 2, blood lidocaine concentrations are
plotted against time following the termination
of a constant infusion of intravenous lidocaine
in four dogs. In these dogs an intravenous
"loading dose" of 2 mg/kg was given first; this
A 6A0
70-
5.0-
A
B
0
4.03.0-
A
0.6-
.
a
0 06
80.8
0
z
.'
A
0
0
0
0
j 0.3
0.2-
0.6
0.3~
0.2,
o
10
20 30
40 50 60
7
80
Figure 2
a
a
0.4.
0.1
0.P
0
10
fi
z 0.8_
0
X
W
X
3.
a
1.0
A
f 2.0
32.0Q
z
40
3.0
o
A
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
f-
SPEAR ET AL.
68
0
10
20 30 40 S0 60
TIME (Minutes)
7O 80
Comparison of the disappearance of lidocaine from the blood following a single injection and
following the termination of an infusion. (A) Lidocaine blood concentration afer a single
intravenous injection of lidocaine (0.7 mg/kg) given at time zero. Each symbol represents a
different animal. The linear regression line has a correlation coefficient of 0.617. (B) The time
course of disappearance of lidocaine foUowing the termination of an intravenous infusion of
lidocaine (70 ,ug/kg/mnin). The infusion lasted 50-60 min and was preceded by a loading injection of 2.0 mg/kg. Each symbol represents a different animal; the animals in B were not
the same as those in A. The linear regression line in B has a correlation coefficient of 0.819.
was followed by a constant infusion of 70
,ug/kg/min for 50-60 min. The first arterial
samples ranging between 3.0 and 1.0 gg/ml
were obtained immediately after the termination of the infusion. Notice that the time
course for the disappearance of lidocaine from
the blood for the dogs in B is much longer
than for those in A. In B the half-time for the
disappearance of lidocaine was 31 min.
Effect of Lidocaine
on
the VFT
In each of five animals studied, the VFT for
normal beats was increased following either a
single injection of lidocaine or a constant
infusion of lidocaine. The mean maximum
increase in the fibrillation threshold above
control was 32.0 ma + 10.9 (SD) Figure 3
compares the time course of changes in the
VFT with the time course of changes in the
blood lidocaine concentration following a
single 0.7-mg/kg injection in a representative
experiment. The VFT increased from an average control value of 45 ma to 67 ma following the administration of lidocaine, and the
time course of the changes in VFT correlated
.
with the changes in blood lidocaine concentration. Figure 4 is a similar experiment in which
a constant infusion of lidocaine was administered. In this case, the VFT increased from an
average control value of 35.7 ma to a
maximum of 68 ma during the lidocaine
infusion. The prolonged time that the VFT
was elevated correlated with the prolongation
of the elevation in blood lidocaine concentration. Therefore, following either an injection
or an infusion, the time courses of the
fibrillation threshold changes correlated with
the lidocaine concentration changes.
The late phase of the time course of the
change in VFT in figure 4 exhibits an
"undershoot" before its return to control value.
This phenomenon is also shown in figure 3. It
was also observed in the premature ventricular contraction experiments to be described
later. The "undershoot" occurred in four of
nine animals in which the time courses were
determined. The phenomenon appears to be
real; however, its cause is unknown.
Studies by other investigators have shown
that the VFT is decreased (the heart is easier
Circulation, Volume XLVI, July 1972
LIDOCAINE AND VENTRICULAR FIBRILLATION
o_J
80-
0
X
U)
W
60-
W.
X
i::! 40MJ
-
ax
20
0
10
20
30
40
4.0Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
,
3.0
z
0
0
W
ventricular contractions. The control thresholds are shown at the left of the figure; their
mean value was 31.8 + 8.6 ma. The fibrillation
thresholds were decreased by 68.5% following
the premature ventricular contractions as can
be seen at time zero (mean 10.0 ± 3.6 ma) in
figure 5. Lidocaine was then administered as a
loading injection followed by a constant
infusion in these dogs. The VFT following
PVCs was redetermined at 30 and 60 min
after the beginning of lidocaine administration. Notice that the fibrillation thresholds
following the PVCs were increased during the
administration of lidocaine. The mean values
were 28.3 ± 14.5 ma at 30 min and 23.2 ± 10.7
ma at 60 min. The corresponding mean blood
lidocaine levels for the four dogs at 30 and 60
2.0-
c
p-
0
.-
o)-J
69
80
aC)
10-
0
:c
60
r
0
:-
10
20
30
40
TIME AFTER LIDOCAINE
(Minut es)
Figure 3
A comparison of the time course of changes in the
normal fibrillation threshold and blood lidocaine concentration following a single intravenous injection of
lidocaine (0.7 mg/kg). The control fibrillation threshold
at time zero is the average of three values, which did
not vary by more than 3 ma.
z
40
I_-J
20
O E
m
iL
O-
o
80
100
2.0-
z E
ischemia.4
0
Circulatton, Volume XLVI, July 1972
60
c;
z
0
o
1 Since both of these conditions
can occur during acute myocardial infarction
it was of interest to determine the effect of
lidocaine on the fibrillation threshold under
these conditions. Figure 5 demonstrates the
effect of lidocaine on the VFT following
experimental premature ventricular contractions (PVC) in four dogs. The fibrillation
electrodes were located on the anterior
epicardial surface of the right ventricle. After
control fibrillation thresholds were determined
during paced supraventricular rhythm, the
VFT was measured following premature
40
3.0-
to fibrillate) following premature ventricular contractions and following acute
10
20
O
3 1.0-
a
020
40
60
80
100
TIME AFTER LIDOCAINE STARTED
(Minutes)
Figure 4
A comparison of the time course of changes in the
normal fibrillation threshold and blood lidocaine concentration following a loading injection of 2.0 mg/kg
foUowed by
an intravenous infusion of 70 ,ig/kg/min
of lidocaine. The infusion was terminated at 47 nmii.
The control fibrillation threshold at time z.ero is the
average of three values twhich did not vary by nmore
than 3 ma.
SPEAR ET AL.
70
50-
P.V.C.
CONTROL
40.
0
J
0
I
W 30-
a:
r
z
N
2020-
-J
--Im lo.
u
l_
1
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
0
20
40
60
TIME AFTER LIDOCAINE
(Minutes)
Figure 5
The effect of lidocaine' on the fibrillation threshold
during premature ventricular contractions (PVC). The
control fibillation thresholds are shown at the left.
The values at time zero are the fibrillation thresholds
during PVCs before lidocaine was administered. The
fibrillation thresholds for PVCs during lidocaine administration (loading injection of 2.0 mg/kg followed
by an infusion of 70 ,tg/kg/min for 60 min) are shown
at 30 and 60 min. The lines connect data points for
the same animals.
minutes were 5.8 + 3.5 and 3.2 ± 1.6 ,ug/ml,
respectively.
Figure 6 demonstrates the effect of lidocaine on the VFT during acute coronary
artery occlusion in six dogs. The fibrillating
electrodes were located within the region of
the left ventricle supplied by the coronary
artery which was to be occluded. At the left of
the figure the control fibrillation thresholds are
shown. Their mean value was 53.0 ± 3.8 ma.
During acute ligation of the anterior descending coronary artery the VFT decreased by
52.3% to a mean value of 24.8 + 3.9 ma
(values at time zero in fig. 7). A single
injection of lidocaine was then given in each
case and the fibrillation thresholds were
redetermined during acute occlusion at 4
and 14 min after the administration of
lidocaine. Notice that at 4 min after the
administration of lidocaine, the mean VFT
during ischemia was increased to 56.9 ± 13.2
ma, and at 14 min the mean value was
52.1 + 13.7 ma. The corresponding blood
lidocaine concentrations were 3.3 ± 2.4 ,ug/ml
at 4 min and 1.3 + 0.7 ,ug/ml at 14 min after
the injection of lidocaine.
In order to determine more precisely the
time course of the effects of a single injection
of lidocaine on the VFT following ischemia,
two series of ischemic VFT determinations
were performed in the same animal following
injections of lidocaine given 2 hours apart.
The data were then pooled to construct figure
7. The VFT determinations for the two runs
were staggered in time following the injections so that the pooled data produced
experimental points at shorter time intervals
than could be practical during a single run.
The data of figure 7 show that the time course
of the changes in the ischemic fibrillation
threshold follows closely the time course of
the changes in blood lidocaine concentration
following an intravenous injection.
100
-
0
-J
I
CONTROL
ISCHEMIA
8060
z
40
U
W
20-
-4
0
5
15
10
0
TIME AFTER LIDOCAINE
(Minutes)
Figure 6
The effect of lidocaine on the fibrillation threshold
during acute coronary artery occlusion (acute ischemia).
The control fibrillation thresholds are shown at the
left. The values at time zero are the fibrillation
thresholds during acute ischemia before lidocaine was
administered. The fibrillation thresholds during acute
ischemia following lidocaine administration (single injection of 0.7 mg/kg) are shown at 4 and 14 min.
During each ischemic threshold determination coronary artery occlusion lasted for less than 2 min. The
lines connect data points for the same animals.
Circulation, Volume XLVI, July 1972
LIDOCAINE AND VENTRICULAR FIBRILLATION
00I
ZC)
I
°CD
LL
8040-
-J
o0
l
A
5
Il
1
0
20
40
60
80
I.51
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
cJ)
z
o
_
W
1.0-
c"
U
0
AM
aB O. 50
20
40
60
80
TIME AFTER LIDOCAINE
(Minutes)
Figure 7
A comparison of the time course of changes during
ischemia of the fibrillation threshold and blood lidocaine concentration following a single intravenous
bolus (0.7 mg/kg). The fibrillation threshold data
points were obtained during two runs in the same
animal. During each ischemic threshold determination,
the coronary artery occlusion lasted for less than
2 min.
A comparison of figures 5 and 6 presents an
additional phenomenon of interest. The control VFT determinations are different in these
figures. This difference is related to the
experimental protocol. The VFT measurements of figure 5 were obtained on the right
ventricle and those of figure 6 on the left
ventricle. The higher fibrillation threshold of
the left ventricle compared to the right
ventricle was first reported by Shumway.10 In
our study of 54 control right ventricular
.fibrillation threshold determinations in 10
dogs, and 41 control left ventricular determinations in eight dogs, the right ventricular
threshold was 23.2 + 9.2 ma and the left was
51.8 + 4.3 ma.
Circulatton, Volume XLVI, July 1972
71
Discussion
Lidocaine rapidly diffuses throughout the
body tissues following intravenous administration.12 The liver is the principal site of the
metabolism of lidocaine in man.13 Following
relatively large intravenous lidocaine infusions
in man,14 the blood concentration decreases
with a half-time of 30 or 40 min. Figure 2
demonstrates that the blood concentration of
lidocaine decreases at a more rapid rate
following a single injection than following the
termination of a constant infusion. The lower
blood concentration following a single injection is primarily a result of its dilution as it
diffuses from the vascular space to the
body tissues; some metabolism also occurs.
During a constant infusion, the blood lidocaine has time to equilibrate with the body
tissues, and its disappearance from the blood
is related primarily to its rate of metabolism.
This is supported by the fact that the
disappearance of lidocaine in figure
2B behaves more as a monoexponential
(r = 0.819), while in figure 2A its time course
of disappearance is more complex (r = 0.617).
However, in either case the effects of lidocaine
on the ventricular fibrillation threshold
-(VFT) correlated with the blood lidocaine
level.
Figures 3 and 4 demonstrate that lidocaine
increases the VFT during paced supraventricular rhythm, and that the time course of the
effect is related to the time course of the blood
lidocaine concentration. The effect appears
immediately after lidocaine administration
and rapidly diminishes as the blood lidocaine
concentration decreases. Bacaner's findings8
that lidocaine's effect on the VFT is negligible
are probably related to the rapid disappearance of lidocaine from the blood following a
single injection. In his experiments, the
fibrillation thresholds were measured at least
30 min after the injections, at a time when
the blood levels must have been greatly reduced.
Following premature ventricular contractions, there is an increase in the degree of
dispersion of recovery of the myocardial
tissues, and consequently a decrease in the
72
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
VFT.4 Figure 5 demonstrates the decreased
fibrillation threshold accompanying PVCs.
Even during premature ventricular contractions, lidocaine still increased the fibrillation
threshold. Therefore, not only does lidocaine
inhibit the occurrence of tachyarrhythmias as
has been described clinically,7 but it also has a
direct effect on the myocardium and prevents
the increased vulnerability to fibrillation
which is associated with premature ventricular
contractions.
Shumway'0 and Hanll reported that the
ventricular fibrillation threshold is decreased
during acute ischemia. Figures 6 and 7
demonstrate the decrease in VFT found in our
experiments during ischemia. Note also that
lidocaine more than reverses the decrease in
VFT during acute ischemia, and that the time
course of the effects are related to the time
course of arterial blood lidocaine concentration. All of the effects described for lidocaine
occurred within the therapeutic dose range
(1.2-5.5 mg/ml) for this drug.
An occasional PVC in a heart which is
otherwise free of myocardial disease is usually
not serious even when it falls on the T wave of
a preceding beat; i.e., experience in patients
with failing pacemakers15 and during catheter
pacing of the heart16 have shown that PVCs
can be electrically evoked on the T wave of
preceding beats without causing fibrillation.
The amount of current delivered during
artificial pacing in the human heart at normal
heart rates is less than is necessary to induce
ventricular fibrillation during the vulnerable
period of the normal dog heart (20-50 ma).
These observations suggest that spontaneous
PVCs occurring on T waves are not the only
factor involved in the tendency of fibrillation
to occur in acute myocardial infarction. There
is also recent evidence that fibrillation can
occur following myocardial infarction without
being induced by a PVC.17 However, fibrillation appears to be most likely when premature
ventricular beats fall on the T waves in hearts
which exhibit abnormally large degree of
nonuniform recovery in excitability or otherwise exhibit conditions which predispose them
SPEAR ET AL.
to the sustained reentry which precedes
fibrillation.2' 4
Several recent studies have suggested the
electrophysiologic mode of action of lidocaine.
Studies using microelectrodes'8' 19 show that
besides diastolic depolarization lidocaine decreases the action potential duration and
effective refractory period of Purkinje fibers
without affecting action potential amplitude
or rate of depolarization. Lidocaine also
decreases the dispersion of action potential
durations and prevents the occurrence of
multiple action potentials following single
stimuli. In general, these factors would tend to
decrease nonuniform recovery of excitability
and decrease the opportunity for reentry to
occur. This is undoubtedly related to lidocaine's ability to increase the ventricular
fibrillation threshold.
The basis for the threshold undershoot
phenomenon during the disappearance of
lidocaine is unknown. Whether this is an
artifact of the technic cannot be determined
from our experiments. It may be that during
the disappearance of lidocaine from the
cardiac tissues some regions recover from its
effects before others and thus make the system
transiently more nonhomogeneous and, therefore, more susceptible to fibrillation, than
compared to control situations.
Our studies suggest that lidocaine's effectiveness in treating patients with acute myocardial infarction is not only due to its ability
to decrease the occurrence of ectopic activity,
but also is related to its direct effect on the
myocardium decreasing its vulnerability to
develop fibrillation.
Acknowledgments
The authors wish to thank Mr. Ralph Iannuzzi for
technical assistance, and Dr. M. Meyer, Dr. R. N.
Boyes, and Mr. Paul Kamp of Astra Pharmaceutical
Products, Inc., for providing lidocaine and for
analyzing the blood lidocaine samples.
References
1. WIGGERS CJ, WEGRLA R: Ventric-ular fibrillation
due to single, localized induction and condenser shock applied during the vulnerable phase
of ventricular systole. Amer J Physiol 128:
500, 1940
Circulation, Volume XLVI, July 1972
LIDOCAINE AND VENTRICULAR FIBRILLATION
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
2. HAN J, MOE GK: Nonuniform recovery of
excitability in ventricular muscle. Circ Res 14:
44, 1964
3. HAN J, MILLETT D, CHZZONrrn B, MOE GK:
Temporal dispersion of recovery of excitability
in atrium and ventricle as a function of heart
rate. Amer Heart J 71: 481, 1966
4. HAN J, GARCIA DE JALON PD, MOE GK:
Fibrillation threshold of premature ventricular
responses. Circ Res 18: 18, 1966
5. LowN B, FAxHRO AM, HOOD WB JR, THoRN
GW: Coronary Care Unit. JAMA 199: 188,
1967
6. JEwrTT DE, KISHON Y, THOMAS M: Lignocaine
in the management of arrhythmias after acute
myocardial infarction. Lancet 1: 266, 1968
7. PITT A, LiPP H, ANDERSON ST: Lignocaine
given prophylactically to patients with acute
myocardial infarction. Lancet 1: 612, 1971
8. BACANER MB: Quantitative comparison of bretylium with other antifibrillatory drugs. Amer J
Cardiol 21: 504, 1968
9. SHINOHARA Y: Ventricular fibrillation threshold
(VFRT) in experimental coronary occlusion:
Comparative studies on the effect of G-I-K
solution and some new antiarrhythmic agents.
Jap Circ J 32: 1269, 1968
10. SHUMWAY NE, JOHNSON JA, SnsH RJ: The
study of ventricular fibrillation by threshold
determinations. J Thorac Surg 34: 643, 1957
11. HAN J: Ventricular vulnerability during acute
Circulation, Volume XLVI, July 1972
12.
13.
14.
15.
16.
17.
18.
19.
73
coronary occlusion. Amer J Cardiol 24: 857,
1969
SUNG CY, TRUANT AP: The physiological
disposition of lidocaine and its comparison in
some respects with procaine. J Pharmacol Exp
Ther 112: 432, 1954
STENSON RE, CONSTANIINO RT, HARRISON DC:
Interrelationships of hepatic blood flow, cardiac output, and blood levels of lidocaine in
man. Circulation 43: 205, 1971
BROMAGE: PR, RoBsON JG: Concentrations of
lidocaine in the blood after intravenous,
intramuscular, epidural and endotracheal administration. Anesthesiology 16: 461, 1961
KASTOR JA, LEINBACH RC: Pacemakers and their
arrhythmias. Progr Cardiovasc Dis 13: 240,
1970
CASTILLO C, CASTELLANOS A: Retrograde activation of the His bundle in the human heart.
Amer J Cardiol 27: 264, 1971
DHURANDHAR RW, MACMILLAN RL, BROWN
KWG: Primary ventricular fibrillation complicating acute myocardial infarction. Amer J
Cardiol 27: 347, 1971
DAVIS LD, TEMTE JV: Electrophysiological
actions of lidocaine on canine ventricular
muscle and Purkinje fibers. Circ Res 24: 639,
655, 1969
BIGGER TJ, MANDEL WJ: Effect of lidocaine on
the electrophysiological properties of ventricular muscle and Purkinje fibers. J Clin Invest
19: 63, 1970
Effect of Lidocaine on the Ventricular Fibrillation Threshold in the Dog during
Acute Ischemia and Premature Ventricular Contractions
JOSEPH F. SPEAR, E. NEIL MOORE and GAIRY GERSTENBLITH
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Circulation. 1972;46:65-73
doi: 10.1161/01.CIR.46.1.65
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX
75231
Copyright © 1972 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://circ.ahajournals.org/content/46/1/65
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles
originally published in Circulation can be obtained via RightsLink, a service of the Copyright
Clearance Center, not the Editorial Office. Once the online version of the published article for
which permission is being requested is located, click Request Permissions in the middle column
of the Web page under Services. Further information about this process is available in the
Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/