Localized Cutaneous Infections in Immunocompetent Individuals
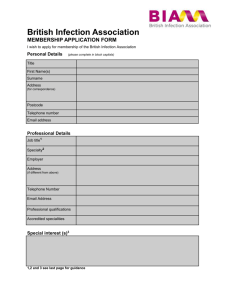
advertisement

Resident Short Reviews Localized Cutaneous Infections in Immunocompetent Individuals Due to Rapidly Growing Mycobacteria John Fowler, MD; Steven D. Mahlen, PhD, D(ABMM) Rapidly growing mycobacteria (RGM) cause skin infections that are refractory to standard antibiotic regimens. Although typically associated with disseminated cutaneous or other systemic infections in immunocompromised patients, RGM sometimes cause localized cutaneous infections in immunocompetent hosts. These infections are almost always associated with precedent skin trauma and inoculation, and therefore have been implicated in outbreaks involving contaminated tattoo ink and inadequately sterilized acupuncture needles. Histologic features often include suppurative granulomatous inflammation, and microorganisms are rarely visualized with stains for acid-fast bacilli. The differential diagnosis includes granulomatous fungal and non-RGM bacterial infections as well as noninfectious suppurative or sarcoidlike conditions. Because no pathognomonic histologic features exist for cutaneous RGM infections, clinical suspicion and appropriate workup are essential to reach an accurate and timely diagnosis. Most localized cutaneous RGM infections in immunocompetent individuals respond well to either clarithromycin or amikacin, in combination with surgical debridement. (Arch Pathol Lab Med. 2014;138:1106–1109; doi: 10.5858/arpa.2012-0203-RS) terium smegmatis group and other rarely pathogenic groups1 (Table). Bacilli of the M smegmatis group, first discovered by Sigmund Lustgarten in the smegma of a man with a penile ulcer, were described in 1885.2 Fifty-three years later, a report of a strain of RGM now known to be M fortuitum isolated from a human postinjection abscess was published by da Costa Cruz.3 In 1953, Moore and Frerichs4 recovered a novel acid-fast bacillus from a knee abscess and subsequently named it M abscessus; and in 1972, Stanford et al5 published their findings regarding an RGM isolate from postinjection abscess outbreaks. This isolate, named M chelonae, was thought by some to be the same organism as M abscessus, but modern classification techniques have demonstrated these to be separate species. Accepted for publication July 16, 2013. From Pathology and Area Laboratory Services, Madigan Army Medical Center, Tacoma, Washington (Dr Fowler); and the Bacterial Diseases Branch, Walter Reed Army Institute of Research, Silver Spring, Maryland (Dr Mahlen). The authors have no relevant financial interest in the products or companies described in this article. The views expressed in this paper are those of the authors and do not reflect the official policy or position of the Department of the Army, the Department of Defense, or the US government. Reprints: Steven D. Mahlen, PhD, D(ABMM), 503 Robert Grant Ave, Bacterial Diseases Branch, Walter Reed Army Institute of Research, Silver Spring, MD 20910-7500 (e-mail: steven.mahlen@ us.army.mil). CLINICAL FEATURES The RGM typically cause disseminated cutaneous infections in immunocompromised hosts, but have also been implicated in lung, bone, joint, ocular, and prosthetic heart valve infections.6–8 In most cases, patients with disseminated cutaneous nontuberculous mycobacterial (NTM) infections are taking low-dose systemic corticosteroids. The most commonly implicated RGM in these instances are M chelonae or M abscessus.1,9 On rare occasion, RGM cause cutaneous infections in immunocompetent hosts. In contrast to cutaneous RGM infections in the immunocompromised, these infections are associated with precedent skin trauma, such as puncture wounds or injuries sustained in motor vehicle accidents. Patients with localized cutaneous infections caused by RGM and other NTM typically present with tender violaceous papules, plaques, nodules, or cellulitis at sites of skin penetration or trauma that, despite treatment with standard antibiotic regimens, have not regressed. Gram stain and routine cultures may be negative, and it is not until after a protracted course that NTM infection is considered. The majority of solitary lesions occur on the lower extremities, but the upper extremities, trunk, and rarely head and neck may also be involved.9,10 Additionally, there are a number of reports of cutaneous M chelonae infections in immunocompetent hosts due to subcutaneous inoculation with contaminated tattoo ink,8,11,12 after acupuncture,13,14 and after mesotherapy.15 Mycobacterium abscessus, M chelonae, Mycobacterium conceptionense, and M fortuitum have all been isolated in postoperative infections after plastic surgery procedures.16,17 Myalgia, fatigue, and night sweats were observed in one immunocompetent patient with tattoo-associated M chelo- 1106 Arch Pathol Lab Med—Vol 138, August 2014 Cutaneous Rapidly Growing Mycobacteria Infection—Fowler & Mahlen R apidly growing mycobacteria (RGM) are defined as nontuberculous species that grow on laboratory media within 7 days.1 There are currently 70 recognized species of RGM that are classified into 6 groups based on genetic relatedness, pigmentation, and biochemical properties. Approximately 80% of disease in humans due to RGM is caused by the nonpigmented Mycobacterium chelonae, Mycobacterium abscessus, and Mycobacterium fortuitum, with the remainder caused by RGM of the pigmented Mycobac- Clinical Manifestations of Rapidly Growing Mycobacteria (RGM) Infections by Group Clinical Manifestationsa Mycobacterium fortuitum group Mycobacterium chelonae/Mycobacterium abscessus group Mycobacterium mucogenicum group Mycobacterium smegmatis group Early-pigmented RGM Mycobacterium mageritense/Mycobacterium wolinskyi group a Localized skin and soft tissue infections, disseminated cutaneous disease (rare), bone and joint infections, lung infections (rare), central nervous system disease (rare, M fortuitum), keratitis, iatrogenic infections Localized skin and soft tissue infections, disseminated cutaneous disease, lung infections (M abscessus in particular), keratitis (M chelonae, M abscessus, otitis media (M abscessus), iatrogenic infections Iatrogenic infections Localized skin and soft tissue infections, bone infections, lung infections (M smegmatis) Iatrogenic infections Localized skin and soft tissue infections, bone infections Data derived from Brown-Elliot BA, Wallace RJ. Mycobacterium: clinical and laboratory characteristics of rapidly growing mycobacteria. In: Versalovic J, Carroll KC, Jorgensen JH, Funke G, Landry ML, Warnock DW, eds. Manual of Clinical Microbiology. 10th ed. Washington, DC: ASM Press; 2011:525–538.1 nae infection,11 but constitutional symptoms often are not present during localized cutaneous infections with these organisms.9 HISTOPATHOLOGY Biopsy of cutaneous RGM infections can show a variety of patterns, depending on the stage at which the biopsy is performed and the immune status of the patient. Suppurative mixed granulomatous inflammation is typically present in immunocompetent patients (Figure 1). In a report of an iatrogenic M abscessus outbreak, Rodrı́guez et al18 separated the histopathologic findings into 3 categories: nodular or diffuse inflammation with mixed granulomas containing abscesses surrounded by epithelioid and Langhans giant cells, neutrophilic abscesses with a subtle granulomatous response, and deep dermal and subcutaneous granulomatous inflammation without neutrophils. Of these patterns, the most commonly observed was the mixed pattern with a robust granulomatous response. The authors observed that broad abscesses with a weak-to-absent granulomatous response were more characteristic of biopsies from immunocompromised patients, and that acid-fast bacilli were more likely to be seen in these instances. In 82% of the biopsies, clear vacuoles surrounded by neutrophils or epithelioid cells were present, and of these nearly one-third contained clumps of acid-fast bacilli (Figure 2). These findings are corroborated by Gable et al,19 who describe a pattern of suppurative infection with a variable degree of granulomatous inflammation in 6 immunocompromised patients with cutaneous RGM infections. Of these cases, 2 had pseudocysts containing microorganisms. This pattern has been suggested to be unique to the RGM.20 Other studies characterizing the histopathologic features of NTM in immunocompetent patients show mixed results: Dodiuk-Gad et al21 reported granulomas in 36% of biopsies from immunocompetent hosts, whereas Bartralot et al22 reported granulomas in 83%. Acid-fast bacilli were observed in even fewer cases. Other patterns observed include robust tuberculoid, palisading, or sarcoidlike granulomas, as well as nongranulomatous patterns, such as necrotizing folliculitis, panniculitis, and nonspecific chronic inflammation.22 Because biopsy does not necessarily demonstrate microorganisms or granulomatous inflammatory reaction, and because RGM infections may not always be detected on standard wound cultures, a clinical suspicion for RGM or other NTM is essential for accurate and timely diagnosis. In such cases, a clinical history of skin infection that follows Arch Pathol Lab Med—Vol 138, August 2014 penetrating skin trauma, lacks response to standard antibiotics, or has negative standard wound cultures should prompt further investigation to include acid-fast bacilli stains and cultures. In cases where mycobacterial infection is suspected but the Ziehl-Neelsen stain is negative, it may be useful to perform a Fite stain, which differs in that tissue sections are deparaffinized using a mixture of mineral oil and xylene rather than xylene alone. This method is considered to be less harsh, preventing loss of the organism’s acid-fast properties, and typically is used to detect Mycobacterium leprae. However, no recent studies have been published that evaluate the sensitivity of modified versus standard acid-fast stains for diagnosis of cutaneous RGM infections. DIFFERENTIAL DIAGNOSIS The differential diagnosis for each of the granulomatous patterns encountered in cutaneous RGM infections is broad. Suppurative versus nonsuppurative granulomatous inflammations raise divergent differential diagnoses, and in both cases, the cause of the granulomas may be either infectious or noninfectious. As with any suppurative cutaneous skin infection—particularly following trauma to the skin— bacterial infection due to more commonly encountered organisms such as Staphylococcus aureus and Streptococcus pyogenes must be considered in the differential diagnosis. These cases are usually excluded by culture and successful empirical treatment. If standard wound cultures are negative and empirical treatment is unsuccessful, then RGM infection should be considered. Suppurative granulomas are associated with a myriad of infectious conditions, including blastomycosis, coccidiomycosis, paracoccidiomycosis, phaeohyphomycosis, cryptococcosis, cat-scratch disease, nocardiosis, actinomycosis, and other atypical mycobacterial infections.23,24 Additional stains for microorganisms should be considered if there is a possibility that these infectious agents are present. Periodic acid–Schiff and Gomori methenamine silver will facilitate visualization of the causative microorganisms in blastomycosis, coccidiomycosis, and paracoccidiomycosis, whereas specific histochemical stains are typically not needed for visualizing the diverse pigmented fungal organisms that cause phaeohyphomycosis, but periodic acid–Schiff and Gomori methenamine silver may still be useful. Cryptococcal microorganisms are highlighted by mucicarmine and Fontana-Masson, and Warthin-Starry highlights rare bacilli in the necrotic granulomas of cat-scratch disease.23 Nocardia Cutaneous Rapidly Growing Mycobacteria Infection—Fowler & Mahlen 1107 histochemical stains and cultures will be negative in these cases, and other findings, such as a history of sarcoidosis or the presence of polarizable material or keratin debris within granulomas, would favor a diagnosis other than RGM infection. Tuberculoid granulomas are seen in tuberculosis, leprosy, leishmaniasis, and other conditions.24 A Ziehl-Neelsen histochemical stain will highlight microorganisms within granulomas in M tuberculosis cutaneous infections, and wound cultures for mycobacteria should not show growth by 7 days. Mycobacterium leprae is best visualized using a Fite stain, though microorganisms often are not readily visualized in tuberculoid leprosy, and a wound culture will fail to grow microorganisms. Cutaneous leishmaniasis may show amastigotes within macrophages using hematoxylin-eosin, but these organisms are not always readily visualized in biopsies of later lesions. If the clinical history suggests cutaneous leishmaniasis or leprosy, polymerase chain reaction may be useful for their detection. Figure 1. Mycobacterium chelonae infection of the hand following accidental incision on the lid of a metal can. There is diffuse granulomatous inflammation with focal suppuration surrounding vacuoles within the dermis, and the epidermis shows irregular acanthosis and parakeratosis (hematoxylin-eosin, original magnification 310). Figure 2. Vacuole containing numerous Mycobacterium chelonae bacteria (Fite acid-fast bacilli, original magnification 3100). stains gram positive in a beaded pattern and is also partially acid fast. This can be confounding, as the RGM—when detected on Gram stain—will stain with a beaded pattern that may be mistaken for gram-positive bacilli.1 Definitive diagnosis often requires culture of the wound, particularly when other atypical mycobacterial infections such as Mycobacterium marinum are in the differential diagnosis. Noninfectious causes of suppurative granulomas include superficial granulomatous pyoderma and ruptured cysts and follicles.24 Lesions of superficial granulomatous pyoderma tend to occur on the trunk but may also occur at surgical sites.25 A recent case report of facial superficial granulomatous pyoderma following surgical scar revision demonstrates the potential similarity of superficial granulomatous pyoderma and RGM infection with regard to clinical presentation and histologic appearance.26 In this case, appropriate histochemical stains and negative cultures aided in establishing the correct diagnosis. Sarcoidlike granulomas raise the differential diagnosis of sarcoid and foreign body giant cell reaction. However, 1108 Arch Pathol Lab Med—Vol 138, August 2014 LABORATORY IDENTIFICATION Isolation of the RGM is best accomplished by culture at 288C to 308C.1 Once colonies are isolated, additional testing for definitive speciation is performed. Before the widespread use of molecular testing, biochemical and antimicrobial susceptibility tests were used to classify the RGM. For example, the M fortuitum and M chelonae/M abscessus groups are strongly positive for the arylsulfatase reaction at 3 days, in contrast to Mycobacterium wolinskyi and the M smegmatis group. Other tests, such as nitrate reduction, carbohydrate utilization, and growth in 5% NaCl, can help distinguish among species. Though historically these tests have been useful in a clinical context, molecular methods are now preferred for clinical identification.1 Therefore, biochemical testing is reserved as an adjunct to new species characterization and not used routinely for diagnosis. Molecular identification methods have shown their usefulness for differentiating among RGM. These methods have the advantage of producing accurate results that are rapidly available. In one method, 2 main hypervariable domains on the 5 0 end of the 16S rRNA gene (region A and region B) are analyzed for signature sequences that differentiate among species.1,27 Two of the major RGM, M chelonae and M abscessus, are identical in these regions, but differ in the 3 0 end of the 16S rRNA gene. Sequence differences within the heat shock protein gene (hsp65) are very useful in differentiating among species that have a high degree of similarity in the 16S rRNA gene, including M chelonae and M abscessus. Additionally, the hsp65 gene is amenable to polymerase chain reaction restriction enzyme analysis, which does not rely on growth rates or nutritional requirements for initial identification and is relatively inexpensive. However, it is a relatively complex test that, as of 2011, has not been approved by the Food and Drug Administration and therefore requires extensive in-house validation. The utility of sequencing the rpoB gene has more recently been demonstrated in instances where neither the 16S rRNA nor the hsp65 gene differentiated among the RGM species.1 TREATMENT AND PROGNOSIS Several factors must be considered when treating NTM skin infections, such as immune status and number of cutaneous lesions. If multiple lesions are present, or if Cutaneous Rapidly Growing Mycobacteria Infection—Fowler & Mahlen surgical debridement would result in cosmetically or functionally unacceptable results, medical therapy alone may suffice. Although M chelonae and M abscessus historically have been considered to be particularly resistant to antibiotics as compared with M fortuitum,2 more recent evidence suggests that clarithromycin is reliably active against M chelonae and M abscessus but not M fortuitum.9 In cases of M fortuitum infection, amikacin is the antibiotic of choice.2,9 The results of one small clinical trial published in 1993 by Wallace et al28 showed that monotherapy with clarithromycin was effective in treating disseminated infection from M chelonae in immunocompromised patients; however, it is questionable whether these results could be extrapolated to immunocompetent patients, as both the mechanism of infection and the hypothetical virulence of the infectious agents are likely different between the 2 groups. Regardless, monotherapy should be undertaken with caution, as development of resistance to individual agents has been reported.9 Moreover, Uslan et al9 have noted higher levels of resistance to previously favored antibiotics of multiple different classes. Development of resistance to the cell wall synthesis inhibitors in particular is conjectured to be due to asymmetric and time-regulated cell elongation and division that leads to variable sensitivity of the RGM to these antibiotics,29 which may partially explain the protracted course of RGM infections. With localized cutaneous NTM infections, it may be reasonable to delay treatment until susceptibility test results are available, whereas delay of treatment may not be feasible in cases of disseminated disease. In immunocompetent hosts, complete surgical excision, if possible, may be curative,17 though cure is most reliably achieved with a combination of medical and surgical therapy.9,10,16 This is in contrast to disseminated cutaneous infection in immunocompromised hosts, for whom prognosis can be quite poor even with adequate treatment.30 References 1. Brown-Elliot BA, Wallace RJ. Mycobacterium: clinical and laboratory characteristics of rapidly growing mycobacteria. In: Versalovic J, Carroll KC, Jorgensen JH, Funke G, Landry ML, Warnock DW, eds. Manual of Clinical Microbiology. 10th ed. Washington, DC: ASM Press; 2011:525–538. 2. Brown-Elliot BA, Wallace RJ. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev. 2002;15(4):716–746. 3. da Costa Cruz JC. Mycobacterium fortuitum: um novo bacilo acidoresistente patogenico para o homen [Mycobacterium fortuitum: new acid fast bacillus pathogenic for man]. Acta Med (Rio de Janeiro). 1938;1:298–301. 4. Moore M, Frerichs JB. An unusual acid fast infection of the knee with subcutaneous, abscess-like lesions of the gluteal region: report of a case study with a study of the organism, Mycobacterium abscessus. J Investig Dermatol. 1953;20(2):133–169. 5. Stanford JL, Pattyn SR, Portaels F, Gunthorpe WJ. Studies of Mycobacterium chelonae. J Med Microbiol. 1972;5(2):177–182. Arch Pathol Lab Med—Vol 138, August 2014 6. Freitas D, Alvarenga L, Sampaio J, et al. An outbreak of Mycobacterium chelonae infection after LASIK. Ophthalmology. 2003;110(2):276–285. 7. Grange JM. Mycobacterial infections following heart valve replacement. J Heart Valve Dis. 1992;1(1):102–109. 8. Preda VA, Maley M, Sullivan JR. Mycobacterium chelonae infection in a tattoo site. Med J Aust. 2009;190(5):278–279. 9. Uslan DZ, Kowalski TJ, Wengenack NL, Virk A, Wilson JW. Skin and soft tissue infections due to rapidly growing mycobacteria: comparison of clinical features, treatment, and susceptibility. Arch Dermatol. 2006;142(10):1287–1292. 10. Escalonilla P, Esteban J, Soriano ML, et al. Cutaneous manifestations of infection by nontuberculous mycobacteria. Clin Exp Dermatol. 1998;23(5):214– 221. 11. Goldman J, Caron F, de Quatrebarbes J, et al. Infections from tattooing: outbreak of Mycobacterium chelonae in France. BMJ. 2010;341:c5483. 12. Kappel S, Cotlair J. Inoculation of mycobacterium chelonae from a tattoo. J Am Acad Dermatol. 2011;64(5):998–999. 13. Lee WJ, Kang SM, Sung H, et al. Non-tuberculous mycobacterial infections of the skin: a retrospective study of 29 cases. J Dermatol. 2010;37(11):965–972. 14. Woo PC, Li JH, Tang W, Yuen K. Acupuncture mycobacteriosis. N Engl J Med. 2001;345(11):842–843. 15. Regnier S, Cambau E, Meningaud JP, et al. Clinical management of rapidly growing mycobacterial cutaneous infections in patients after mesotherapy. Clin Infect Dis. 2009;49(9):1358–1364. 16. Lim JM, Kim JH, Yang HJ. Management of infections with rapidly growing mycobacteria after unexpected complications of skin and subcutaneous surgical procedures. Arch Plast Surg 2012;39:18–24. 17. Panossian A, Cohen MJ, Posalski I. Upper extremity Mycobacterium chelonae cutaneous infection. Plast Reconstr Surg. 2011;127(6):163e–165e. 18. Rodrı́guez G, Ortegón M, Camargo D, Orozco LC. Iatrogenic Mycobacterium abscessus infection: histopathology of 71 patients. Br J Dermatol. 1997; 137(2):214–218. 19. Gable AD, Marsee DK, Milner DA, Granter SR. Suppurative inflammation with microabscess and pseudocyst formation is a characteristic histologic manifestation of cutaneous infections with rapid-growing mycobacterium species. Am J Clin Pathol. 2008;130:514–517. 20. Meyers WM. Mycobacterial infections of the skin. In: Ashworth TG, ed. Tropical Pathology. Vol 8. 2nd ed. Berlin, Germany: Springer; 1995:291–378. 21. Dodiuk-Gad R, Dyachenko P, Ziv M, et al. Nontuberculous mycobacterial infections of the skin: a retrospective study of 25 cases. J Am Acad Dermatol. 2007;57(3):413–420. 22. Bartralot R, Pujol RM, Garcı́a-Patos V, et al. Cutaneous infections due to nontuberculous mycobacteria: histopathological review of 28 cases: comparative study between lesions observed in immunosuppressed patients and normal hosts. J Cutan Pathol. 2000;27(3):124–129. 23. Hirsh BC, Johnson WC. Pathology of granulomatous diseases: mixed inflammatory granulomas. Int J Dermatol. 1984;23(9):585–597. 24. Weedon D. The granulomatous reaction pattern. In: Weedon D, Strutton G, Rubin AI, Houston M, Davie B. Weedon’s Skin Pathology. 3rd ed. London, United Kingdom: Churchill Livingstone; 2010:169–194. 25. Quimby SR, Gibson LE, Winkelmann RK. Superficial granulomatous pyoderma: a clinicopathologic spectrum. Mayo Clin Proc. 1989;64(1):37–43. 26. Persing SM, Laub D. Superficial granulomatous pyoderma of the face: a case report and review of the literature. Eplasty. 2012;12:e56. 27. Patel JB, Leonard DG, Pan X, Musser JM, Berman RE, Nachamkin I. Sequence-based identification of mycobacterium species using the MicroSeq 500 16S rDNA bacterial identification system. J Clin Microbiol. 2000;38(1):246–251. 28. Wallace RJ, Tanner D, Brennan PJ, Brown BA. Clinical trial of clarithromycin for cutaneous (disseminated) infection due to Mycobacterium chelonae. Ann Intern Med. 1993;119:482–486. 29. Aldridge BB, Fernandez-Suarez M, Heller D, et al. Asymmetry and aging of mycobacterial cells lead to variable growth and antibiotic susceptibility. Science. 2012;335(6064):100–104. 30. Bartralot R, Garcı́a-Patos V, Sitjas D, et al. Clinical patterns of cutaneous nontuberculous mycobacterial infections. Br J Dermatol. 2005;152:727–734. Cutaneous Rapidly Growing Mycobacteria Infection—Fowler & Mahlen 1109