Thermal Perception Threshold Testing for the Evaluation of Small
advertisement

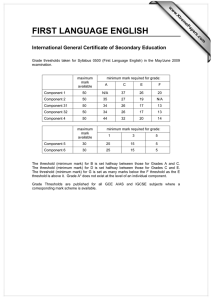
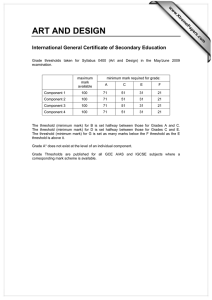
Original Article Industrial Health 2000, 38, 366–371 Thermal Perception Threshold Testing for the Evaluation of Small Sensory Nerve Fiber Injury in Patients with Hand-Arm Vibration Syndrome Norikuni TOIBANA1, Hisataka SAKAKIBARA2*, Mamoru HIRATA3, Takaaki KONDO4 and Hideaki TOYOSHIMA4 1 Tokushima Kensei Hospital, 4–9–1, Shimosuketou-machi, Tokushima 770-0963, Japan Nagoya University School of Health Sciences, 1–1–20, Daiko-minami, Higashi-ku, Nagoya 461-8673, Japan 3 Osaka Prefectural Institute of Public Health, 1–3–69, Nakamichi, Higashinari-ku, Osaka 537-0025, Japan 4 Nagoya University School of Medicine, 65 Tsurumai-cho, Showa-ku, Nagoya 466-8550, Japan 2 Received May 8, 2000 and accepted July 17, 2000 Abstract: The aim of the present study was to investigate whether thermal perception threshold testing is a useful method that could replace pain threshold testing in the evaluation of small sensory nerve fiber injury in vibration-induced neuropathy. Vibration, pain, and thermal (warm and cold) perception thresholds were examined on both middle fingers of 50 patients with hand-arm vibration syndrome and 29 healthy controls of similar age. The patients were divided into three subgroups according to the Stockholm Workshop sensorineural scale. Thermal (warm and cold) thresholds as well as vibration and pain thresholds were significantly more deteriorated among the patients than in the controls. Among the patients, warm thresholds elevated and cold thresholds lowered according to the Stockholm Workshop scale. Thermal thresholds were significantly correlated with pain thresholds, and the sensitivity of the thermal threshold testing tended to be greater than that of the pain threshold testing. The present findings indicate that thermal threshold testing for warm and cold perception can be a useful substitute for pain threshold testing to examine small nerve fiber injury in vibration-induced neuropathy. Key words: Thermal threshold, Vibration-induced neuropathy, Pain threshold, Sensory nerve Introduction Peripheral nerve impairments in the hand are often encountered among workers exposed to hand-transmitted vibration. These neurological abnormalities include numbness and tingling of the fingers, damaged skin sensory perception, reduced grip force, and occasionally impaired manipulative dexterity. Histopathological studies have demonstrated demyelinating neuropathy with severe destruction and loss of the myelin sheath, and remarkable loss of nerve fibers in finger skin specimens from vibrationexposed subjects1, 2). Nerve conduction measurements have *To whom correspondence should be addressed. shown reduced sensory and motor nerve conduction velocities in vibration-exposed hands3, 4), which are associated with impaired vibration perception thresholds and reduced grip force5, 6). Vibration perception threshold testing is widely accepted as a useful measure for screening or diagnosing vibrationinduced sensory nerve impairments7). Such testing is thought to evaluate the function of large sensory nerve fibers such as myelinated A-β fibers. On the other hand, some studies indicate that thermal perception is also damaged among vibration-exposed workers, implying that small nerve fibers, including unmyelinated C fibers and myelinated A-δ fibers, are impaired in vibration-induced neuropathy8, 9). An animal experiment with rats has demonstrated that vibration exposure THERMAL PERCEPTION IN HAND-ARM VIBRATION SYNDROME produced transient changes in non-myelinated fibers of the plantar nerve as well10). Recently, Stockholm Workshop 94 has recommended thermal threshold testing as a suitable measure of the function of unmyelinated C fibers and myelinated A-δ fibers7). In Japan, vibration and pain perception thresholds are examined in order to evaluate vibration-induced sensory nerve injury. However, there are some questions about pain threshold testing from the ethical point of view7), so that it would be better to find a substitute for it. Thermal threshold testing is one candidate for such a substitute, because it is supposed to examine the function of small sensory nerve fibers, just as in pain threshold testing. Hence, the present study investigated whether thermal threshold testing could be a useful substitute for pain threshold testing in the evaluation of vibration-induced neuropathy. In this study, the authors examined thermal (warm and cold) thresholds as well as vibration and pain thresholds of patients with handarm vibration syndrome and healthy controls, and compared the effectiveness of these sensorineural tests. Materials and Methods The subjects were 50 male patients with hand-arm vibration syndrome and 29 healthy male controls. The patients had been under treatment for hand-arm vibration syndrome, and the controls were healthy volunteers who had not been occupationally exposed to hand-arm vibration. These subjects were selected from among those without complications causing peripheral neuropathies such as diabetic, chemical and druginduced neuropathies, cerebral vascular diseases, other neurological diseases, or severe injuries to the hand. Subjects were also limited to those who consumed less than 80 ml a day of alcohol equal to ethanol. There was no significant difference in age between the patients and the controls (mean ± standard deviation: 60.3 ± 3.5 and 60.3 ± 3.3, respectively). The patients had VWF (n=39, 78%), finger numbness or tingling (n=41, 82%), coldness in the hands (n=48, 96%), and joint pain in the hand and arm (n=40, 80%). The controls did not have VWF, finger numbness or tingling, but some complained of coldness in the hand (n=4, 14%) and joint pain in the hand and arm (n=6, 21%). Thermal (warm and cold) perception thresholds were measured on the palmar surface of the distal phalanx of both middle fingers using a thermo-esthesiometer11). The plate temperature of the thermo-esthesiometer was initially set to the finger skin temperature of each subject, which had been measured just before using an infrared thermometer (IT340S, Horiba Manufacturing, Japan), and then it 367 automatically increased or decreased at the rate of 0.2°C/s. Warm or cold perception thresholds were determined as the temperature at which each subject started to feel warm or cold in the finger tested. The measurements were performed twice in a random order. The value closer to the initial skin temperature was adopted as the subject’s threshold. The values of warm and cold thresholds and differences between warm threshold and finger temperature, between cold threshold and finger temperature, and the neutral zone between warm threshold and cold threshold were evaluated as indices of thermal perception testing. Vibration perception thresholds at 125 Hz and pain perception thresholds were also measured on the same finger. The former was done with a vibrometer (AU-02B, Rion, Japan). The level of vibration generated by the vibrometer can be changed from − 10 dB to 40 dB in increments of 2.5 dB. The 0 dB is set at 0.218 m/s2 r.m.s for 125 Hz. The latter was measured using a syringe needle (gauge 23) with weights of 1, 2, 3, 5, 7, 10 or 15 grams in each syringe. These measurements were carried out in summer under room temperatures between 26°C and 28°C to keep fingers warm. About four subjects, including both patients and controls, were examined in the morning and another four subjects were tested in the afternoon. Subjects rested in the test room for about 20 or 30 min before they were examined. All subjects were given full explanations about the present study and consented to participation. Examinations were made in the following order. First, the palmar surface skin temperature of both middle fingers was measured using an infrared thermometer (IT340S, Horiba Manufacturing, Japan). As the finger skin temperature of a few patients was lower then 30°C, their hands were warmed with a heater to above 30°C. Second, vibration perception thresholds at 125 Hz were measured. Third, pain perception thresholds were examined, and thermal perception thresholds were tested last. The same physician examined all subjects. The differences in test values between the patients and the controls were compared with Student’s t-test, χ2 test, or Fisher’s exact test. Comparisons among subgroups of the patients classified according to the Stockholm Workshop sensorineural scale12) were made with multiple comparison by Scheffe’s method. Results Comparison of examination results of patients and controls As shown in Table 1, both warm and cold thresholds in the patients were significantly more deteriorated than in the controls (p<0.01). The differences between warm threshold 368 N TOIBANA et al. Table 1. Examination results of patients with hand-arm vibration syndrome and healthy controls Right middle finger Skin temperature (°C) Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Vibration threshold (≥10 dB) Pain threshold (≥5 g) Left middle finger Skin temperature (°C) Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Vibration threshold (≥10 dB) Pain threshold (≥5 g) Vibration syndrome patients (n=50) Controls (n=29) 32.0 ± 1.1 43.7 ± 3.6** 18.7 ± 6.8** 11.6 ± 3.5** 13.3 ± 6.6** 25.0 ± 9.0** 49 (98%)** 43 (86%)** 32.5 ± 1.3 35.6 ± 2.6 29.4 ± 3.3 3.2 ± 2.3 3.0 ± 2.9 6.2 ± 4.1 3 (10%) 4 (14%) 32.1 ± 1.1 43.4 ± 3.2** 18.7 ± 6.6** 11.3 ± 3.2** 13.6 ± 6.9** 25.0 ± 9.0** 50 (100%)** 41 (82%)** 32.4 ± 1.2 35.3 ± 1.9 29.4 ± 2.4 2.9 ± 1.7 3.0 ± 2.3 5.9 ± 3.1 3 (10%) 4 (14%) **p<0.01: significant difference between patients and controls. WPT, CPT and FST stand for warm perception threshold, cold perception threshold, and finger skin temperature, respectively. and finger temperature and between cold threshold and finger temperature, and the neutral zone between warm threshold and cold threshold were also significantly greater in the patients (p<0.01). Finger skin temperatures did not differ significantly between the patients and the controls. Significantly increased vibration and pain thresholds were also encountered in the patients (p<0.01). The cut-off value for vibration threshold in the present study was set at 10 dB or more, and that for pain threshold was set at 5 g and over. These were determined as the point where specificity was around 90% in the control subjects under study. Examination results according to Stockholm Workshop sensorineural scale The patient subjects were divided into three subgroups according to the Stockholm Workshop sensorineural (SN) scale. In this study, the scale was defined as follows: 0 SN (without numbness), 1SN (with numbness but without reduced sensory perception as defined in the 2+3 SN category), and 2+3 SN (with numbness and impaired sensory perception of 15 dB or more in vibration threshold and 10 g and over in pain threshold). Age and finger temperature did not differ among the three subgroups (Table 2). With higher SN scale, warm thresholds Table 2. Examination results of patients with hand-arm vibration syndrome according to Stockholm Workshop sensorineural (SN) scale 0 SN 1 SN 2+3 SN Right middle finger Age (years) Skin temperature (°C) Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Vibration threshold (≥10 dB) Pain threshold (≥5 g) (n=13) 60.6 ± 2.6 32.1 ± 1.1 41.1 ± 4.1 22.3 ± 5.4 9.0 ± 3.9 9.8 ± 5.2 18.7 ± 8.5 13 (100%) 9 (69%) (n=18) 61.0 ± 3.3 32.1 ± 1.3 43.7 ± 2.7 19.4 ± 6.7 11.7 ± 2.6 12.7 ± 6.8 24.4 ± 7.7 17 (94%) 15 (83%) (n=19) 59.5 ± 3.6 32.0 ± 1.1 45.4 ± 3.0* 15.6 ± 6.5* 13.4 ± 3.1* 16.7 ± 6.1* 29.8 ± 7.9* 19 (100%) 19 (100%)* Left middle finger Age (years) Skin temperature (°C) Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Vibration threshold (≥10 dB) Pain threshold (≥5 g) (n=16) 61.3 ± 2.8 32.4 ± 1.1 42.4 ± 3.4 21.0 ± 6.0 10.0 ± 3.3 11.4 ± 5.9 21.4 ± 8.3 16 (100%) 11 (69%) (n=18) 60.7 ± 3.3 32.1 ± 1.1 43.2 ± 3.3 20.3 ± 6.4 11.1 ± 3.1 11.9 ± 6.5 22.9 ± 8.4 18 (100%) 14 (78%) (n=16) 58.9 ± 3.6 31.7 ± 1.2 44.7 ± 2.4 14.7 ± 5.9* 13.0 ± 2.7* 17.9 ± 6.7* 30.8 ± 8.5* 19 (100%) 16 (100%) *p<0.05; statistical difference from 0 SN. WPT, CPT and FST stand for warm perception threshold, cold perception threshold, and finger skin temperature, respectively. Industrial Health 2000, 38, 366–371 369 THERMAL PERCEPTION IN HAND-ARM VIBRATION SYNDROME Table 3. Specificity and sensitivity of thermal, vibration and pain perception threshold testing Specificity Sensitivity 89.7% 89.7% 89.7% 93.1% 93.1% 86.2% 89.7% 86.2% 89.7% 93.1% 94.0% 94.0% 94.0% 94.0% 92.0% 96.0% 90.0% 96.0% 90.0% 96.0% Vibration perception threshold (≥10 dB) Right finger Left finger 89.7% 89.7% 98.0% 100.0% Pain perception threshold (≥5 g) Right finger Left finger 86.2% 86.2% 86.0% 82.0% Thermal perception threshold Warm threshold (≥38.5°C) Cold threshold (≤27°C) WPT − FST (≥5.5°C) CPT − FST (≥5.5°C) WPT − CPT (≥12°C) Right Left Right Left Right Left Right Left Right Left WPT, CPT and FST stand for warm perception threshold, cold perception threshold, and finger skin temperature, respectively. increased and cold thresholds decreased. The differences between warm threshold and finger temperature and between cold threshold and finger temperature, and the neutral zone between warm threshold and cold threshold, tended to be greater according to the SN scale. The warm and cold thresholds and these differences were significantly different between the 0 SN and the 2+3 SN (p<0.05). Specificity and sensitivity of thermal threshold, vibration threshold and pain threshold testing As the cut-off value was set at the point where specificity was around 90% in the control subjects, the sensitivity of warm and cold threshold testing in the patients was 94% (Table 3). On the other hand, the sensitivity of vibration threshold testing was 98% and 100% for the right and left hand, respectively, and that of pain threshold testing was 86% and 82%. Thus, the sensitivity of thermal threshold testing tended to be greater than that of pain threshold testing. Correlation of thermal thresholds with vibration threshold and pain threshold Table 4 shows Spearmann’s correlation coefficients of warm and cold thresholds with vibration and pain thresholds. Thermal thresholds (both warm and cold thresholds) were more closely linked with pain thresholds than with vibration thresholds. Table 4. Spearman’s correlation coefficients among thermal, vibration and pain perception thresholds Right middle finger Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Left middle finger Warm threshold (°C) Cold threshold (°C) WPT − FST (°C) CPT − FST (°C) WPT − CPT (°C) Vibration threshold Pain threshold 0.439** − 0.157 0.469** 0.204 0.350** 0.457** − 0.215 0.429** 0.285* 0.390** 0.206 − 0.100 0.165 0.171 0.193 0.428** − 0.349** 0.398** 0.456* 0.468** **p<0.01, *p<0.05. WPT, CPT and FST stand for warm perception threshold, cold perception threshold, and finger skin temperature, respectively. Discussion The present study showed that thermal perception thresholds for warmth and cold as well as vibration and pain perception thresholds were significantly more deteriorated among patients with hand-arm vibration syndrome than in healthy controls, which agrees with previous studies8, 9, 13–16). These findings suggest that both small and large sensory nerve fibers are impaired in vibration-induced neuropathy. Animal experiments have also demonstrated damage to small and large nerve fibers in the vibration-exposed extremities10, 17, 18). The present study also demonstrated that indices of thermal thresholds tended to worsen among patients according to the Stockholm Workshop sensorineural scale; a deterioration of thermal thresholds in the 2+3 SN (moderate and severe) group were significantly greater than in the 0 SN group. This finding indicates that thermal threshold testing could reflect the severity of the nerve damage. Hirosawa et al.8) similarly reported that thermal thresholds were deteriorated in vibration-exposed patients with advanced nerve damage. The results by Strömberg et al.16) showed that temperature sense in vibration-exposed workers did not have a clear tendency to worsen with higher Stockholm Workshop scale, but it was likely to be more severely impaired in vibrationexposed workers with numbness than in those without it. In the present study, a significant correlation was found between thermal and pain thresholds, while such relations were not as close between thermal and vibration thresholds. This is physiologically reasonable because both thermal and pain sensations are mediated through unmyelinated C-fibers 370 and myelinated A-δ fibers, and heat above 45°C and cold below 15°C are perceived as heat pain and cold pain via pain nerve fibers as well19). It, therefore, seems that thermal threshold testing could be a substitute for pain threshold testing in examining the impairments of small sensory nerve fibers. In fact, the greater sensitivity of thermal threshold testing in the present study suggests that the thermal threshold testing might even be superior to pain threshold testing. There are some differences among studies concerning the sensitive indices of thermal thresholds testing for the evaluation of vibration-induced nerve impairments. Some studies pointed out that the neutral zone between the warm and cold threshold was a sensitive indicator of nerve damage8, 9), while others reported that cold thresholds were more useful than warm or heat thresholds in the detection of vibration-induced neuropathy9, 13). One study indicated that heat threshold testing did not detect any significant impairment in vibration-exposed workers20). On the other hand, others showed that warm perception in particular were impaired in vibration-exposed workers8, 16). In the present study, the patients were almost equally damaged in warm and cold thresholds and the neutral zone, judging from the sensitivity in the tests. These differences in the sensitive indices among studies could result from differences in the subjects examined. For example, it is supposed that patients with severe nerve injury will have abnormalities in almost all indices of thermal thresholds. It is possible that the present patients were such severe cases because most of them had increased vibration thresholds. Another possibility is that the differences are due to differences in the methods of measuring thermal thresholds, as some studies have indicated that thermal thresholds are affected by the starting temperature21, 22). Further studies are necessary to determine a sensitive indicator of thermal threshold testing for evaluating vibration-induced neuropathy. As mentioned above, vibration and pain thresholds are measured in Japan to evaluate vibration-exposed neuropathy, but some controversy still surrounds the ethics of pain threshold testing. The present study has demonstrated that thermal threshold testing for warm and cold perception can reflect the severity of vibration-induced neuropathy and would be a useful substitute for pain threshold testing. Measurements of vibration thresholds for detecting the dysfunction of large nerve fibers, and thermal thresholds for testing impairments in small nerve fibers would be suitable for the evaluation of vibration-exposed nerve impairments. N TOIBANA et al. Acknowledgements We are much obliged to Prof. Hideki Mito of Kansai Welfare University for the use of his thermo-esthesiometer. This study was partly supported by a grant-in-aid for scientific research from the Japan Ministry of Education, Science, and Culture. References 1) Takeuchi T, Futatsuka M, Imanishi H, Yamada S (1986) Pathological changes observed in the finger biopsy of patients with vibration-induced white finger. Scand J Work Environ Health 12, 280–3. 2) Takeuchi T, Takeya M, Imanishi H (1988) Ultrastructural changes in peripheral nerves of the fingers of three vibration-induced persons with Raynaud’s phenomenon. Scand J Work Environ Health 14, 31–5. 3) Brammer AJ, Pyykkö I (1987) Vibration-induced neuropathy: Detection by nerve conduction measurements. Scand J Work Environ Health 13, 317– 22. 4) Sakakibara H, Kondo T, Miyao M, Yamada S (1994) Digital nerve conduction velocity as a sensitive indication of peripheral neuropathy in vibration syndrome. Am J Ind Med 26, 359–66. 5) Färkkilä M, Pyykkö I, Jäntti V, Aatola S, Starck J, Korhonen O (1988) Forest workers exposed to vibration: A neurological study. Br J Ind Med 43, 826– 9. 6) Sakakibara H, Hirata M, Hashiguchi T, Toibana N, Koshiyama H, Zhu SK, Kondo T, Miyao M, Yamada S (1996) Digital sensory nerve conduction velocity and vibration perception threshold in peripheral neurological test for hand-arm vibration syndrome. Am J Ind Med 30, 219–24. 7) Anonymous (1995) Clinical and laboratory diagnostics of neurological disturbances in workers using handheld vibrating tools. In: Stockholm Workshop 94, Handarm vibration syndrome: Diagnostics and quantitative relationships to exposure, Proceedings. eds. by Gemne G, Brammer AJ, Hagberg M, Lundström R, Nilsson T, 187–93, Sweden’s National Institute of Occupational Health, Solna. 8) Hirosawa I, Watanabe S, Fukuchi Y, Nishiyama K, Hosokawa M (1983) Availability of temperature sense indices for diagnosis of vibration disease. Int Arch Occup Environ Health 52, 215–22. Industrial Health 2000, 38, 366–371 THERMAL PERCEPTION IN HAND-ARM VIBRATION SYNDROME 9) Ekenvall L, Nilsson BY, Gustavsson P (1986) Temperature and vibration thresholds in vibration syndrome. Br J Ind Med 43, 825–9. 10) Lundborg G, Dahlin LB, Hansson H-A, Kanje M, Necking LE (1990) Vibration exposure and peripheral nerve fiber damage. J Hand Surg 15A, 346–51. 11) M i t o H , S h i m i z u T ( 1 9 8 1 ) E x p e r i m e n t a l thermoesthesiometer incorporating peltier thermal modules —its rationale and instance of applications—. Acta Med Kinki Univ 6, 125–30. 12) Brammer AJ, Taylor W, Lundborg G (1987) Sensorineural stages of the hand-arm vibration syndrome. Scand J Environ Health 13, 279–83. 13) Virokannas H, Virokannas A (1995) Temperature and vibration perception thresholds in workers exposed to hand-arm vibration. Cent Eur J Pub Health 3 (Suppl), 66–9. 14) Zamyslowska-Szmytke E (1998) Efficacy of vibration, electric current and thermal perception tests in diagnosis of hand-arm vibration syndrome. Int J Occup Med Environ Health 11, 247–54. 15) Lindsell CJ, Griffin MJ (1999) Thermal thresholds, vibrotactile thresholds and finger systolic blood pressures in dockyard workers exposed to handtransmitted vibration. Int Arch Occup Environ Health 371 72, 377–86. 16) Strömberg T, Dahlin LB, Rosén I, Lundborg G (1999) Neurophysiological findings in vibration-exposed male workers. J Hand Surg 24B, 203–9. 17) Chang KY, Ho ST, Yu HS (1994) Vibration induced neurophysiological and electron microscopical changes in rat peripheral nerves. Occup Environ Med 51, 130– 5. 18) Ho ST, Yu HS (1989) Ultrastructural changes of the peripheral nerve induced by vibration: An experimental study. Br J Ind Med 46, 157–64. 19) Guyton AC (1981) Somatic sensations: I. the mechanoreceptive sensations. In: Textbook of medical physiology (sixth edition). ed. by Guyton AC. 597– 625, Saunders, Philadelphia. 20) Nilsson T, Lundström R, Burström L, Hagberg M (1995) Assessment of heat pain perception in relation to vibration. Cent Eur J Pub Health 3 (Suppl), 70–2. 21) Hilz MJ, Glorius S, Beric A (1995) Thermal perception thresholds: Influence of determination paradigm and reference temperature. J Neur Sci 129, 135–40. 22) Ruffell CM, Griffin MJ (1995) Effect of starting temperature on the repeatability on thermotactile thresholds. Centr Eur J Publ Hith 3 (Suppl), 81–5.