AN ACCURATELY REPRESENTED FINITE ELEMENT MODEL OF
advertisement

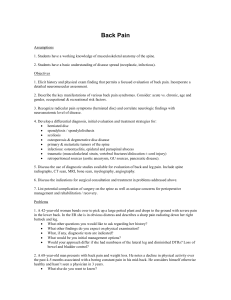
AN ACCURATELY REPRESENTED FINITE ELEMENT MODEL OF LUMBAR MOTION SEGMENT (L2-L3) Ee-Chon Teo and Kim-Kheng Lee School of Mechanical & Production Engineering, Nanyang Technological University, Singapore Corresponding author: Ee-Chon Teo E-mail: mecteo@ntu.edu.sg Abstract In the present study, a three-dimensional geometrical and mechanical accurate finite element model of the human lumbar L2-L3 segment was developed using digitized geometrical data of embalmed lumbar L2 and L3 vertebrae. The direct digitizing process provides an alternative method in capturing the highly irregular geometry of spine as compared to the commonly use of CT/MRI images. All complex anatomical features of the spine such as lamina, superior/inferior facet, pedicle, pars interarticularis, spinous process and transverse process were explicitly represented in the unprecedented finite element model. The analysis accounts for geometrical, material and contact non-linearities. The computed results of lumbar L2-L3 segment were closely correlated with published results in terms of axial displacement, intradiscal pressure, disc bulge, end-plate bulge and tensile stress in the peripheral annulus fiber. 1. Introduction For the past decade, numerical method (such as finite element method) has proved to be a useful adjunct to the experimental approaches for investigating clinical problems of the spine. Investigators have always accentuated the importance on need for more accurate model in terms of geometry, material property and advanced simulation of intervertebral disc to better simulate in vivo and in vitro situations. Though the geometry of lumbar spine is highly irregular, it is important to define the actual geometry of the structure as closely as possible to obtain reasonable results applicable to clinical and in vivo situations. It is well know that the anatomic structure and surface geometry of the vertebrae detect the motion of the spine and its related biomechanical responses. Generally, CT scans or MRI data of patients or cadaveric spine are used for mesh geometry. But the quality of mesh produced using these two methods is not satisfactory as the meshes align inherently with orthogonal plane of images and the undefined borders between the junctions of two adjacent vertebrae. Therefore, the aim of this study is to develop an accurately represented finite element model of lumbar L2-L3 motion segment using direct digizitizing process, which provides another mean for mesh construction. The model was validated against published results under compression loading. The validated FE model was further analyzed to investigate disc and end-plates bulge, intradiscal pressure and stress in the annulus fibers under compressive physiological range of loading with confidence. 2. Material and Methods The 3-D finite element model of the L2-L3 spinal unit was developed based on geometrical data of embalmed lumbar spine obtained using a flexible highly accurate touch-point digitizer of an accuracy of The cadaveric spine was 0.01mm. inspected to be free from spinal disease, metastasis and trauma. Figure 1 shows the steps undertaken to capture its intricate details for mesh generation. compressive displacement of 1.5 mm was applied in 5 increments over the superior surface of the L2 vertebral body (displacement control). 3. Results and Discussion Fig 1: FlowChart The geometrical non-linearity of intervertebral disc is currently modeled by representing the annulus as a composite structure with fiber embedded in solid matrix elements and the nucleus pulposus is modeled as nearly incompressible fluid (Shirazi et al). The nonlinear stress-strain behaviors of the ligaments represented by tension-only cable elements were obtained from literature. In order to appropriately model the changing areas of contact of the facet articulating surface with increments in loading, facet articulation is treated as a moving contact problem. The final FE model (fig 2) consists of 8281 solid 8-noded elements and 817 cable elements with 32,641 degrees of freedoms. As seen from Fig 2, the meshes developed herein are observed to be as regular as possible, of which is an important requirement in finite element analysis. This would be necessary in the study of stress distribution pattern and injury mechanisms in the spine. The predicted results regarding the axial displacement, intradiscal pressure, disc bulge and end-plate bulge shown in the following figures are in good agreement with the previously experimental data in the literature. With increasing prescribed compressive displacement the stiffening behavior of the disc is predicted. Fig 2: FE Model of L2-L3 Motion Segment For analysis, the inferior surface of L3 vertebral body was fixed, and a uniform axial The FE model also predicts the intradiscal pressure increased nearly linearly with increasing compressive load, and these finding compare favourably with published results. With the model validated under static loading, it could serve as a platform for developing more advanced finite element model to better simulate in vivo and in vitro situations. Our focus of future work would be in the development of poroelastic model for lumbar spine to better simulate the fluidflow mechanism for intervertebral disc so as to have a better insight on the nutrition to the disc and pathology of interverterbral disc. References Disc stiffness along the radial direction (bulge stiffness) similarly increased with compressive load. For the normal disc, the end-plate bulge is upwards (convex outward with respect to the nucleus) to provide the volume for the incompressible nucleus. With increasing load, the end-plate bulge increased. 4. Conclusions In conclusion, a well-represented finite element model of L2-L3 motion segment was developed with the adoption of direct digitizing process and advanced modeling technique. The predicted results exhibit nonlinear behaviors except intradiscal pressure, which exhibits a linear relationship with compressive stress. Ng, H.W., Teo, E.C. (2001) J. Spinal Disord, 14: 201-210. SA Shirazi-Adl, SC Shrivastava and AM Ahmed (1984) Spine, 9(2): 120-134. Teo, E.C., Ng, H.W. (2001) J. Biomechanics, 34: 13-21.