VIEWPOINT
Deciphering Harm Measurement
Gareth Parry, PhD
Amelia Cline, BSPH
Don Goldmann, MD
I
MPROVEMENT IN HEALTH CARE QUALITY AND SAFETY CAN
be notable when measurement criteria are clear, evidence is strong, and policy and interventions are focused.
Despite this potential, progress in reducing patient harm
in hospitals has been slow.1 In an effort to catalyze progress, the Department of Health and Human Services (HHS)
is funding a national program, Partnership for Patients (P4P),
with the ambitious goal of reducing “preventable hospitalacquired conditions” by 40% by 2013, focused initially on
9 complications.2 Although the program’s goal formally
includes only preventable harm, the HHS notes “the Partnership will target all forms of harm” and provide guidance
to hospitals for reducing “all-cause harm.” Simultaneously,
the list of “serious reportable events” for which the Centers
for Medicare & Medicaid Services will modify physician and
health care institution payment is increasing. However, delay
in defining a measurement strategy for harm has slowed progress and has created confusion. The need to reach consensus on robust, pragmatic measures for assessing and tracking harm rates has therefore become urgent.
Harm Measures
The terms harm, adverse events, and injuries are often used
interchangeably. The Canadian Disclosure Guidelines3 provide particularly useful definitions: harm is “an outcome that
negatively affects a patient’s health and/or quality of life”;
an adverse event is “an event which results in unintended
harm to the patient, and is related to the care and/or services provided to the patient, rather than to the patient’s underlying medical conditions.”
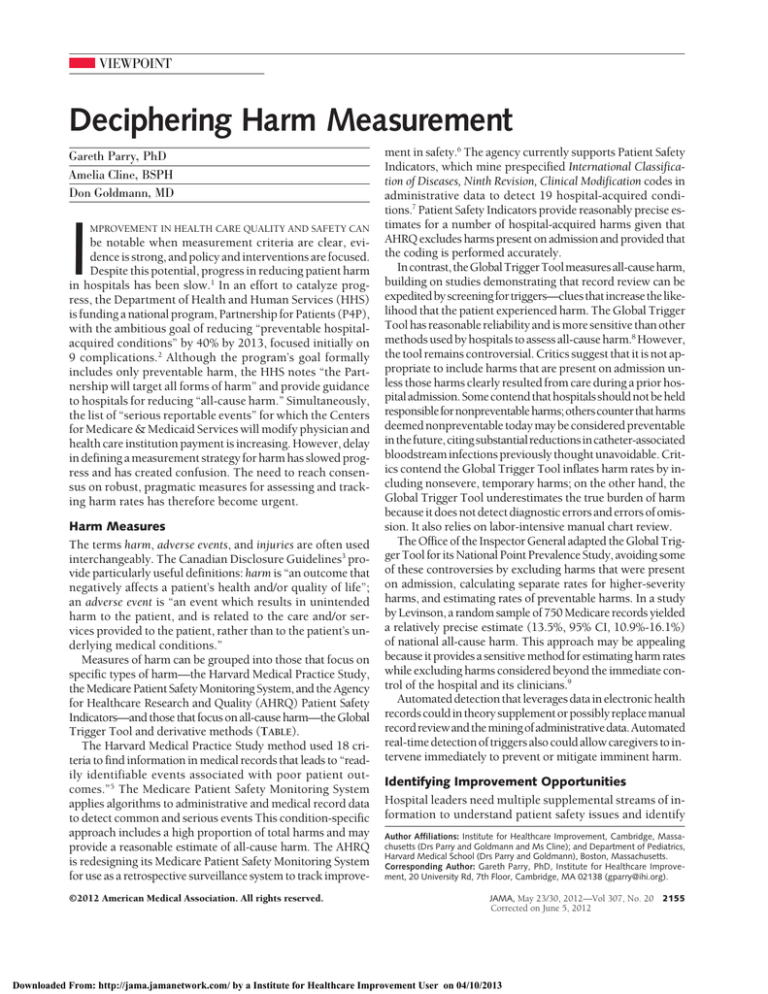
Measures of harm can be grouped into those that focus on
specific types of harm—the Harvard Medical Practice Study,
the Medicare Patient Safety Monitoring System, and the Agency
for Healthcare Research and Quality (AHRQ) Patient Safety
Indicators—and those that focus on all-cause harm—the Global
Trigger Tool and derivative methods (TABLE).
The Harvard Medical Practice Study method used 18 criteria to find information in medical records that leads to “readily identifiable events associated with poor patient outcomes.”5 The Medicare Patient Safety Monitoring System
applies algorithms to administrative and medical record data
to detect common and serious events This condition-specific
approach includes a high proportion of total harms and may
provide a reasonable estimate of all-cause harm. The AHRQ
is redesigning its Medicare Patient Safety Monitoring System
for use as a retrospective surveillance system to track improve©2012 American Medical Association. All rights reserved.
ment in safety.6 The agency currently supports Patient Safety
Indicators, which mine prespecified International Classification of Diseases, Ninth Revision, Clinical Modification codes in
administrative data to detect 19 hospital-acquired conditions.7 Patient Safety Indicators provide reasonably precise estimates for a number of hospital-acquired harms given that
AHRQ excludes harms present on admission and provided that
the coding is performed accurately.
In contrast, the Global Trigger Tool measures all-cause harm,
building on studies demonstrating that record review can be
expedited by screening for triggers—clues that increase the likelihood that the patient experienced harm. The Global Trigger
Tool has reasonable reliability and is more sensitive than other
methods used by hospitals to assess all-cause harm.8 However,
the tool remains controversial. Critics suggest that it is not appropriate to include harms that are present on admission unless those harms clearly resulted from care during a prior hospital admission. Some contend that hospitals should not be held
responsiblefornonpreventableharms;otherscounterthatharms
deemed nonpreventable today may be considered preventable
in the future, citing substantial reductions in catheter-associated
bloodstream infections previously thought unavoidable. Critics contend the Global Trigger Tool inflates harm rates by including nonsevere, temporary harms; on the other hand, the
Global Trigger Tool underestimates the true burden of harm
because it does not detect diagnostic errors and errors of omission. It also relies on labor-intensive manual chart review.
The Office of the Inspector General adapted the Global Trigger Tool for its National Point Prevalence Study, avoiding some
of these controversies by excluding harms that were present
on admission, calculating separate rates for higher-severity
harms, and estimating rates of preventable harms. In a study
by Levinson, a random sample of 750 Medicare records yielded
a relatively precise estimate (13.5%, 95% CI, 10.9%-16.1%)
of national all-cause harm. This approach may be appealing
because it provides a sensitive method for estimating harm rates
while excluding harms considered beyond the immediate control of the hospital and its clinicians.9
Automated detection that leverages data in electronic health
records could in theory supplement or possibly replace manual
record review and the mining of administrative data. Automated
real-time detection of triggers also could allow caregivers to intervene immediately to prevent or mitigate imminent harm.
Identifying Improvement Opportunities
Hospital leaders need multiple supplemental streams of information to understand patient safety issues and identify
Author Affiliations: Institute for Healthcare Improvement, Cambridge, Massachusetts (Drs Parry and Goldmann and Ms Cline); and Department of Pediatrics,
Harvard Medical School (Drs Parry and Goldmann), Boston, Massachusetts.
Corresponding Author: Gareth Parry, PhD, Institute for Healthcare Improvement, 20 University Rd, 7th Floor, Cambridge, MA 02138 (gparry@ihi.org).
JAMA, May 23/30, 2012—Vol 307, No. 20
Corrected on June 5, 2012
Downloaded From: http://jama.jamanetwork.com/ by a Institute for Healthcare Improvement User on 04/10/2013
2155
VIEWPOINT
Table. Summary of Approaches Used to Measure Patient Harm in the United States
Outcome Measure
Method Summary
Features
Medicare
Department of
patient
Health and
safety
Human
monitoring
Services
system
Patient
Safety Task
Force, CMS
Method
Creator
Specified unintended harms,
injuries, or loss that is
more likely associated
with a patient’s
interaction with the health
care delivery system than
from an attendant
disease process
Full medical records are sent to 2 clinical data
abstraction centers and are screened by
trained abstractors for specific types of adverse
events using an electronic data collection
software program (MedQuest)
Administrative data are then used to identify specific
postdischarge events; eg, readmissions and
30-d postoperative mortality
Focuses on events that are likely to be
documented and discoverable in the
medical record, likely associated
with a specific process of care,
commonly responsible for serious
morbidity or mortality, preventable or
repairable; no assessment of
preventability or severity
PSIs
AHRQ
Adverse events: resulting
from exposure to the
health care system, likely
amenable to prevention
by changes to the system
Review by mining administrative data
Each of the 19 PSIs include a set of ICD-9-CM
codes specified by AHRQ, and these codes are
mined from a hospital’s administrative data
Rates of each PSI are calculated using
AHRQ-defined denominators
PSIs are harm-specific and do not
comprise an aggregate measure of
all-cause harm preventability not
formally assessed
June 2009 adoption of
present-on-admission codes
improved specificity
Global
Trigger
Tool
Institute for
Healthcare
Improvement
Adverse events: unintended
physical injury resulting
from or contributed to by
medical care that requires
additional monitoring,
treatment, or
hospitalization or that
results in death
2-Stage manual medical record review
Primary stage: 2 trained clinical providers (eg,
nurse, clinical pharmacist) independently review
records for 53 specific triggers and any
resultant adverse events
Disagreements are resolved by consensus
Secondary stage: harms detected on primary
review are reviewed by a trained physician,
who is the final arbiter
Severity of harm is rated using the modified
NCC MERP scale4
Aggregate measure of all-cause harm
Harms related to health care present on
admission, temporary harms, and
nonpreventable harms are included
Office of
Inspector
General
Harm
Detection
Method
Office of
Inspector
General,
adaptation
of the
Global
Trigger Tool
Adverse events: harm as a
result of medical care or
occurring in a health care
setting
2-Stage medical record review
Primary stage: records are screened for potential
adverse events using 5 methods, including a
modified version of the Global Trigger Tool’s
53 triggers
Secondary stage: full record review by a physician
team to confirm harm in flagged records and
assessment of the preventability and severity
of harms
Aggregate measure of all-cause harm
Temporary harms, nonpreventable
harms, and harms present on
admission excluded from
overall rate.
Abbreviations: AHRQ, Agency for Healthcare Research and Quality; CMS, Centers for Medicare & Medicaid Services; ICD-9-CM, International Classification of Diseases, Ninth Revision,
Clinical Modification; NCC MERP, National Coordinating Council for Medical Errors Reporting and Prevention; PSI, Patient Safety Indicator.
improvement opportunities. For example, voluntary reporting supplements formal assessment of harm rates by providing valuable information regarding near misses and failureprone systems, while promoting a culture of safety. Morbidity
and mortality reviews, executive walk-rounds, root-cause
analyses, and failure modes and effects analyses can yield
important clues to improving hazardous systems.
Conclusions
The Centers for Medicare & Medicaid Services and the AHRQ
are well positioned to speedily clarify which measures and
methods can most effectively evaluate progress toward the
P4P goals. Until then, despite its imperfections, the Office
of the Inspector General approach may be the best available method for determining national harm trends.
While awaiting consensus, individual hospitals can apply a portfolio of measurement methods, including those
outlined in this Viewpoint, according to their own safety
priorities. Condition-specific measures (including Patient
Safety Indicators and real-time surveillance of specific harms)
are valuable for within-organization improvement. However, hospitals will need to address multiple types of harm
before substantial improvement in all-cause harm rates will
be observed. Delay in measuring the effect of best practices
on harm rates will postpone the day when the nation can
celebrate significant improvement in patient safety.
2156
JAMA, May 23/30, 2012—Vol 307, No. 20
Corrected on June 5, 2012
Conflict of Interest Disclosures: All authors have completed and submitted the
ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Disclaimer: The Institute for Healthcare Improvement (IHI) developed the Global
Trigger Tool and provides training materials at no charge.
Additional Contributions: We thank Carol Haraden, PhD, and Frank Federico, RPH,
both of the IHI, for their valuable comments and suggestions on this article. Neither were compensated for their contribution.
REFERENCES
1. Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ.
Temporal trends in rates of patient harm resulting from medical care. N Engl J Med.
2010;363(22):2124-2134.
2. Partnership for patients: better care, lower costs. healthcare.gov. http://www
.healthcare.gov/compare/partnership-for-patients. Updated December 14, 2011.
Accessed March 15, 2012.
3. Disclosure Working Group. Canadian Disclosure Guidelines. Edmonton, Alberta: Canadian Patient Safety Institute; 2008.
4. Medication errors council revises and expands index for categorizing errors: definitions of medication errors brroadened [news release]. National Cooridinating Council for Medication Error Reporting and Prevention; June 12, 2001. http://www
.nccmerp.org/press/press2001-06-12.html. Accessed May 2, 2012.
5. Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. N Engl J Med. 1991;324(6):370-376.
6. Metersky ML, Hunt DR, Kliman R, et al. Racial disparities in the frequency of
patient safety events. Med Care. 2011;49(5):504-510.
7. AHRQ Quality Indicators Toolkit for Hospitals. Agency for Healthcare and Research Quality; January 2012. http://www.ahrq.gov/qual/qitoolkit/index.html. Accessed May 2, 2012.
8. Classen DC, Resar R, Griffin F, et al. “Global trigger tool” shows that adverse
events in hospitals may be ten times greater than previously measured. Health
Aff (Millwood). 2011;30(4):581-589.
9. Levinson DR. Adverse Events in Hospitals: National Incidence Among Medicare Beneficiaries. Washington, DC: Office of Inspector General; November 2010.
http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf. Accessed May 2, 2012.
©2012 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Institute for Healthcare Improvement User on 04/10/2013