Dentaltown Magazine www.dentaltown.com
What Are Your
Core Values?
Substance Use Disorder:
When Your Patient Has an Addiction
The Dilemma of
Dental Aid Therapists
Howard Speaks, page 22
by Dr. William Kane, page 106
by Fred Joyal, page 30
September 2012
September 2012 » Volume 13, Issue 9 » Equipment
3.0
Earn up to
CE Credits
This Issue
Continuing Education:
Step-by-Step Layering for
Anterior Composite Buildup
by Dr. Anthony Tay, page 94
Profile: BISCO
Continuing Education:
CBCT Use in Endodontics
A Division of Farran Media, LLC
by Dr. Paul A. Jones, page 84
IT’777777
…777'7
7777
:98767554327107/4.-,+*
Outstanding wear resistance
Enhanced color stability
)('&(8754227342.%7$#"! 347+#
$5 22.$7,013.7 %7!24#7% %#7$#"!#2.+42*
:987675547%.432 57 %#7013.7#"!#2.+4
,47#"1.% +.#%7#
7, %5.%-742+,4+.$27
%7!43
#3" %$4
Low shrinkage of only 1.6 vol.%
Non-sticky
Prolonged working time under ambient light
42.-%437 %#7! 3+.$542*
Excellent polishability and polish retention
Tooth-like modulus of elasticity
557':::'&:'&:
TRY ®SO NOW
FOR JUST
REF 2646 3. 57.+ 8 X 0.25 Caps
(2 X A1, 2 X A2, 2 X A3, 2 X A3.25)
1 X 1g Grandio SO Heavy Flow
syringe A2, 1 X Dimanto Polisher
$58
VOCO · 555 Pleasantville Rd Suite 120 NB · Briarcliff Manor, NY 10510 · www.vocoamerica.com · infousa@voco.com
FREE FACTS, circle 10 on card
FREE FACTS, circle 15 on card
FREE FACTS, circle 32 on card
FREE FACTS, circle 14 on card
contents
September 2012
76
Practice Management
SDD for the DDS
Dr. Joe Steven Jr. shows how to successfully schedule same-day dentistry for the
benefit of your patients and your production numbers.
80
Cosmetic
Take-home Versus In-office
Whitening Techniques
Dr. Joseph Banker discusses the best techniques for getting pearly whites pearly white.
84
101
Honest Feedback – A Trip to 3M
Continuing Education
Cone Beam CT in Endodontics
Dr. Paul Jones describes CBCT’s advantages and limitations with cases to support.
22
Howard Speaks
Practice with Purpose
This month, Dentaltown Magazine Publisher
Dr. Howard Farran talks about getting back to
the basics by identifying your core values.
28
Professional Courtesy
64
Let Your Patients Do
the Bragging
Tom Hopkins shows you how to
provide patients with ideas like
posting reviews, writing testimonials or giving them several business
cards to take to their friends.
30
Second Opinion
70
Townies recall their recent trip to 3M’s
headquarters to give input on upcoming
products.
102
Selling Dentistry
Finance
Financial Mistakes to
Avoid in Your 30s and 50s
Dr. Douglas Carlsen tells of common financial mistakes to dodge at
these key times in a dentist’s life.
Roundtable Discussion
Midnight in Hong Kong: A Meeting
of the (Impassioned) Minds
Dr. Howard Farran, John Christensen, Dr.
Rhonda Savage and Patrick Tessier gather
for an impromptu roundtable at the World
Dental Forum, discussing a common interest: passion.
106
The Magical Mystery Office Tour
Dentaltown Magazine Editorial Director
Dr. Thomas Giacobbi encourages you to
think about your office through the eyes of
a patient taking a tour.
Townie Trip
Addiction
When Your Patient Has an Addiction
Dr. William Kane points out how to identify
if a patient has an addiction and how to aid
in treatment.
The Dilemma of Dental Aid Therapists
Fred Joyal, founder of 1-800-DENTIST, writes
about the pros and cons of the position.
56
Corporate Profile
BISCO
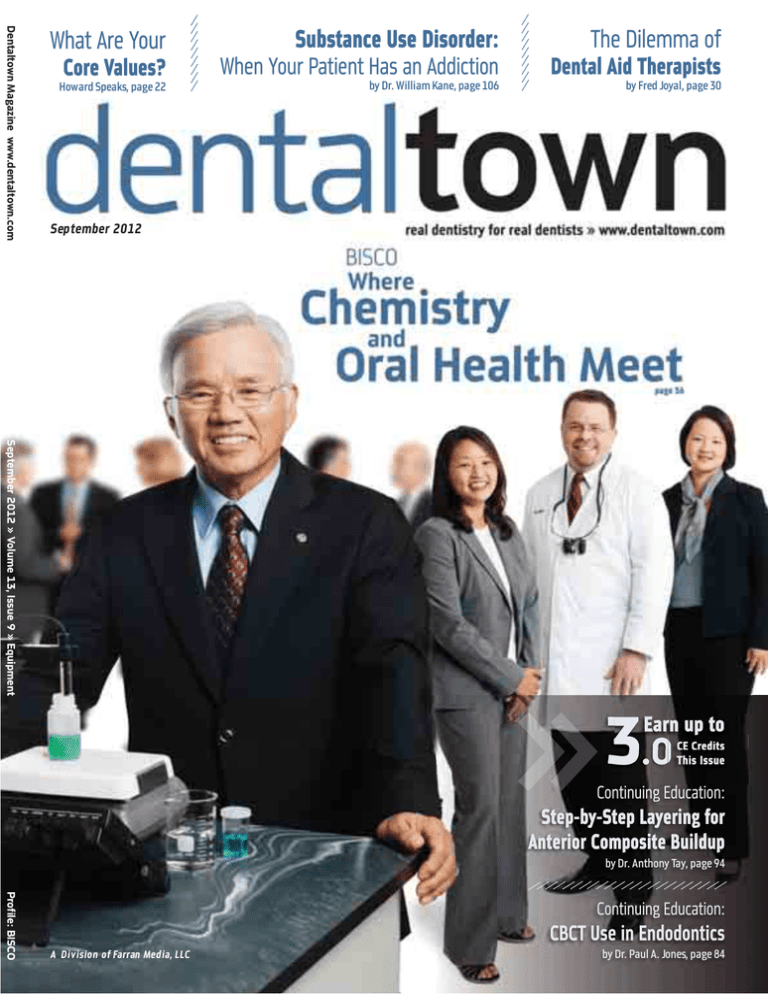
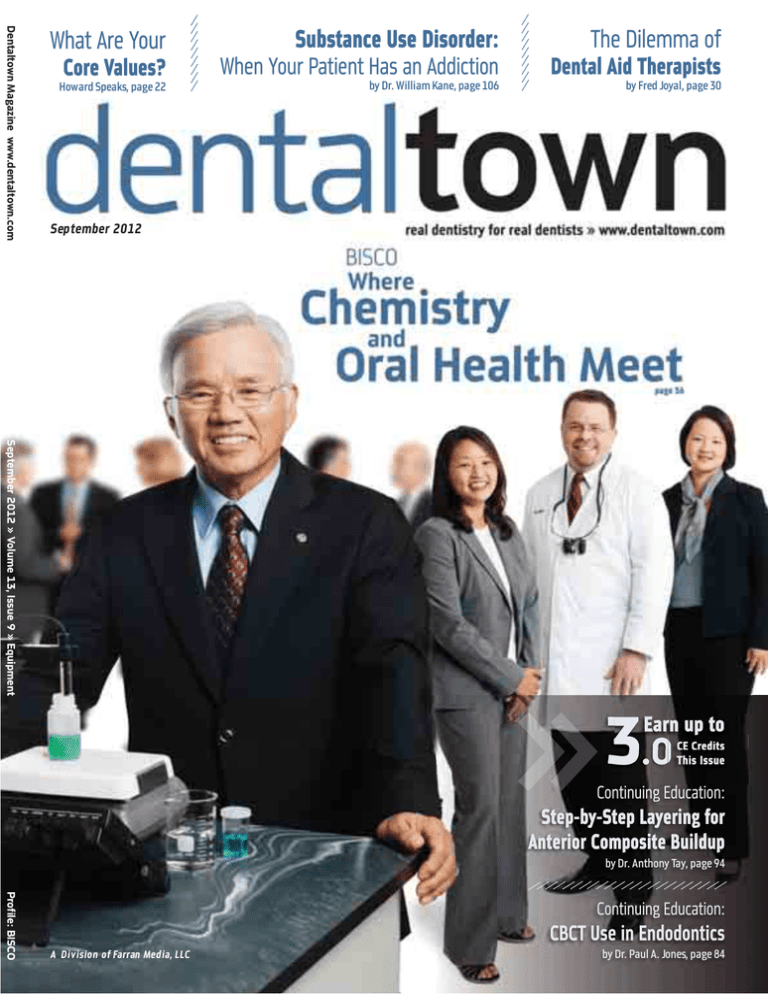
On cover, from left: BISCO President Byoung Suh, PhD,
MS, FADM; Director of Business Operations, Julie Suh;
Executive Vice President Paul L. Child Jr., DMD, CDT;
and Director of Professional Relations, Carolyn D. Suh.
continued on page 10
6
SEPTEMBER 2012 » dentaltown.com
INNO VATIVE
INNOVATIVE
T
DE
DEPTH
REDUCTION BURS
De
Developed
veloped bbyy Dr.
Drr. Rober
Robertt W
Winter,
interr, Prosthodontist/Master
dontist/Master Cer
Ceramist,
raamist,
amist, ffor
or
or outcome-based
outcome based prepar
preparation
raation
atio design.
MINIMAL
.3mm / .5mm / .7mm
RWMIN
! ! ! CONVENTIONAL
EXTENSIVE
.5mm / .7mm / .9mm
RWCONV
R
! ! ! .8mm / 1.0mm / 1.2mm
RWEXT
! ! structure is required
! of the tooth
.3mm - .4mm
.8mm - 1.0m
-1
1.0mm
0mm
1.1mm - 1.3mm
By Y
Your
our
o Side in De
Dentistr
Dentistryy
DENTAL
DENT
TAL
A INSTRUMENTATION
INSTRUMENTA
ATION
T
To
T
o order
order call 800.841.4522
or fax 888.610.1937.
website:
BrasselerUSA.com
Visit our w
ebsite:: BrasselerUSA
Depth reduction b
ur concepts and philosoph
ative Design clinics
bur
philosophyy presented in Restor
Restorative
aavailable
va
vailab
v
le through Spear campus lear
ning progr
ams:: www
.speareducation.com.
learning
programs:
www.speareducation.com.
©2012 Brasseler USA. All rights rreserved.
eserved.
FREE FACTS, circle 1 on card
B-3
B-3705-TOWN-09.12
705-TOWN-09.12
Introducing CEREC Omnicam
®
Quite simply the most perfect
CAD/CAM camera ever
CEREC® Omnicam’s innovative and
elegant design combines industry
leading ease of use with high precision
and powder free convenience.
Designed for
Access
ColorStreaming for
Confidence
Powder Free for
Convenience
Slim, rounded camera tube allows
easy rotation of the camera in the
intraoral space. Tiny camera tip
guarantees the best lens positioning
anywhere in the mouth.
As the camera moves over teeth,
a photorealistic clinical image is
displayed in full-color with crisp
clarity and impeccable detail.
Works without the aid of any
powder or opaquing agent.
CEREC Omnicam is easy to
learn, convenient and fast, yet
maintains Sirona’s highest
level of precision.
For more information and to schedule
an in-office demonstration, contact your
Patterson Representative directly,
or call 800.873.7683.
FREE FACTS, circle 52 on card
GLOBAL
NUMBER
contents
September 2012
continued from page 6
Hygiene & Prevention
114
In This Issue
Unblocking the Nose
116
94
Continuing Education
Simplified Step-by-Step Layering Technique for
Aesthetic Anterior Composite Buildup
Dr. Anthony Tay explains the process to make anterior composite buildups easy.
In This Issue
12 Dentaltown.com Highlights
16 Continuing Education Update
62 New Products
75 Product Profile
Message Boards
36
Perio Reports
• Mouth Breathing Reduces
Exercise Capacity
• Mouth Breathing Changes
Facial Morphology
• Humming Increases Nasal Nitric
Oxide Production
• Mouth-Breathing Kids Have Bad Breath
• Infant Sleep Disordered Breathing
Leads to Childhood Behavior Problems
• Snoring Associated with Craniofacial
Development
120
Profile in Oral Health
Mouth Vs. Nasal Breathing
Cosmetic
More Single Tooth Isolation
Anterior Composites
A Townie offers colleagues a collection of impressive single tooth
isolation anterior composite cases.
124
Product Profile
NTI: Prophies, Parafunction and
Your Patients
126
Hygienetown.com Message Board
Zest Anchors
52
113 Ad Index
128 Dentally Incorrect
Sleep Study Standard
of Care?
Sleep Apnea and Sleep Disordered
Breathing Cause More than
Hypoxemia
One dentist thinks treating snoring
without a diagnosis is malpractice.
Do you agree?
Hygienists discuss the importance of sleep
apnea to a patient’s overall health, and their
role in it.
Sleep Medicine
Dentaltown (ISSN 1555-404X) is published monthly on a controlled/complimentary basis by Dentaltown.com,
LLC, 9633 S. 48th St., Ste. 200, Phoenix, AZ 85044. Tel. (480) 598-0001. Fax (480) 598-3450.
USPS# 023-324 Periodical Postage Paid in Phoenix, Arizona and additional mailing offices.
POSTMASTER: Send address changes to: Dentaltown.com, LLC, 9633 S. 48th St., Ste. 200, Phoenix, AZ 85044
©2012 Dentaltown.com, LLC. All rights reserved. Printed in the USA.
Publications Mail Agreement #40902037
Return undeliverable Canadian addresses to Station A, P.O. Box 54, Windsor ON N9A 6J
e-mail: cpcreturns@wdsmail.com
10
SEPTEMBER 2012 » dentaltown.com
improve
improve yyour
our pra
practice
ctice with
keating
kea
atting dental
dent
enttal
a zirconia.
z
uncompromising
uncompro
omising esthetics.
estheticcs outstanding
ta
strength
sstrength. flawl
flawless
less fit
332KDZ
2KDZ Bruxe
Bruxe102/1.-,+,*)(',&&.%2$1*'2#".
102/1.-,+,*)(',&&.%2$1*'2#".
22",!".+#2
22",!".+#2 &,#2,1-*),2)%2")%2$,),+".%2
&,#2,1-*),2)%2")%2$,),+".%2
22)2..1#2-.1',+#2.'1&2.+#".#,-2)%
22)2..1#2-.1',+#2.'1&2.+#".#,-2)%
221*+#2,#+2.1$.-#2$*12*+#.1,*12+,)!&.2),#+2
221*+#2,#+2.1$.-#2$*12*+#.1,*12+,)!&.2),#+2
22)%21,%!.+
22)%21,%!.+
332KDZ
02*12",!"2.+#".#,-2-+.+22&#1
2KDZ Ultra
Ultra02*12",!"2.+#".#,-2-+.+22&#1
22,+2#".2)+.12)%(&.1.%2*1,#.2
22,+2#".2)+.12)%(&.1.%2*1,#.2
22*1-.&,)2*)221)22++#1-#1.22
22*1-.&,)2*)221)22++#1-#1.22
221*,%.+21.-,+.2$,#2)%2)-*'1*',+,)!2
221*,%.+21.-,+.2$,#2)%2)-*'1*',+,)!2
22,#&,#2..12#,'.
22,#&,#2..12#,'.
32KDZ
32KDZ Max02
".2'11,!.2*$22!1.#2'#.1,&+2
Max02
".2'11,!.2*$22!1.#2'#.1,&+2
22.21.++2/2.'2#*2*12.&&2$,##,)!2
22.21.++2/2.'2#*2*12.&&2$,##,)!2
22$1'.*12#*21*,%.2.-.#,*)&2+#1.)!#"2
22$1'.*12#*21*,%.2.-.#,*)&2+#1.)!#"2
22)%2.#
22)%2.#
ALL OF OUR PRODUCTS ARE
PROUDLY
PROUDL
LY MADE IN IRVINE, CA
C
ALL OR
OR CLICK
CLICK FOR
FOR A PICKUP
PICKUP TODAY
TODA
CALL
AY
800.433.9833 | www.keatingdentalarts.com
www.keatingdenttalarts
a
.com
FREE FACTS, circle 30 on card
".2+,#-"2#*2&&(-.1',-+2,+2*)2212.#,)!2
".2+,#-"2#*2&&(-.1',-+2,+2*)2212.#,)!2
.)#&2,1-*),221*,%.+22$',&2*$2
.)#&2,1-*),221*,%.+22$',&2*$2
-1*)2)%21,%!.2*#,*)+2#"#21.2,)%,-#.%2
-1*)2)%21,%!.2*#,*)+2#"#21.2,)%,-#.%2
$*12&&2*+,#,*)+2,)2#".21-"2-"2*$2#".+.2
$*12&&2*+,#,*)+2,)2#".21-"2-"2*$2#".+.2
+#1*)!2,#&2)%2,*-*'#,&.21.+#*1#,*)+2
+#1*)!2,#&2)%2,*-*'#,&.21.+#*1#,*)+2
1.2$&#21,-.%2)%2,&&2&&*2*2#*21,)!2*12
1.2$&#21,-.%2)%2,&&2&&*2*2#*21,)!2*12
1-#,-.2#*22).2&..&2*$2.+#".#,-+2)%2
1-#,-.2#*22).2&..&2*$2.+#".#,-+2)%2
1*$,#,&,# W
1*$,#,&,#
We’re
ee’re into cutting edge crown
and bridge! Are you?
YOUR FIRST KDZ
$50 YOUR
CROWN OR BRIDGE CASE UP
OFF TO
TO 3 UNITS!
*To
*T
To redeem,
redeem, write “Dentaltown” on your
form.
Offer
RX for
m. Of
fer cannot be combined with
offer
promotion.
any other of
fer or pr
omotion. $50 Off
Off
dentaltown.com
highlights
▼
CASEPRESENTATION
Lack of Keratinized Tissue
Around Implants
How would you graft this edentulous patient?
Keratinized Tissue
DENTALTOWNFEATURES
MESSAGEBOARDS
▼
Monthly Poll
Need Help with Permanent SSC
Cosmetic Dentistry
When times are tough and finances are
tight, you might need to do a permanent
SSC now and again.
Have you attended any
cosmetic-related CE in 2012?
A. Yes B. No
▼
Permanent SSC
Would Mid-level Providers Increase
My Income?
Mid-level providers are a hot topic. Profit
will certainly increase their acceptance,
or will it?
Mid-level
CONNECTWITHUS
Find Dentaltown on Facebook
www.facebook.com/dentaltown
Follow Dentaltown on Twitter
www.twitter.com/dentaltown
Comments
Dentaltown Magazine is based on an interactive publishing model. After you read this magazine, jump online to
Dentaltown.com and post your comments and feedback
about the articles. (Editor’s Note: See “Message from the
Online Community Manager” for more details.)
Online CE
Posterior Composites Made Easy
– Lee Ann Brady, DMD
Wouldn’t it be great if placing posterior composites was
easy? We spend a lot of time investing in new materials
and techniques to accomplish this goal. This program looks at aspects of
placing a posterior composite from the initial prep through completion to
identify key technique aspects that improve the predictability of placement, and the success of the finished restoration.
continued on page 14
12
SEPTEMBER 2012 » dentaltown.com
RS !
PE
SU
U
N-UP” BON
“SIG
A Value
up to
.00
$912
Purchase !
• FREE List
!
p
-u
et
S
d/or
• FREE
r Patient an
rint Fees fo
P
F
ngs !
F
li
O
ai
%
M
0
•5
borhood
gh
ei
N
t”
n
ie
“New Pat
&%$#"! #$#" %"$#" ! !$! #"#
$ !"$#"! Our Systems have
been PROVEN
for years to get
Dentists a steady
stream of New
“Fee-ForService” Patients
and increase
their Referrals!
Call Today for a FREE information
packet to qualify you for the
“Free Bonus” of $912.00
PUBLISHING, INC.
“I wanted to let you know
about the fantastic response we got
from our very first mailing of your
newsletters. My husband and I are
in our 25th year and have done many
direct marketing pieces over the
years. Although we got responses,
we never had so much positive
response so quickly from any mailing ! We were
swamped with “New Patient” phone calls for appointments
and many comments from our regular patients on how
much they liked the newsletter !
And to think, that this Great Response was from our
very first mailing with you, in February 2010 when we
had the biggest snow storm the northeast has seen in
many years !
With Stoneybrook, I had confidence that you would do
it and do it right because you are so experienced. That took
the worry out of it for me, and of course, it ended up that
you were right !”
Drs. Jennifer and Jim Rice, Nellysford, VA
dentaltown.com
continued from page 12
▼
highlights
SEP
2012
Message
from the
Online
Community
Manager
Letters to the Editor
We often get asked the question: “Why doesn’t Dentaltown have a Letters to the Editor section?” Well, the fact is, we
do – we just do things a little differently around here.
At the end of each online article in the magazine section of Dentaltown.com, you’ll find an “add comment” link. By clicking that, you can share your thoughts and questions with all the readers of Dentaltown… and of course, the editor.
Your opinion is important and because we don’t want to be the only ones who get to hear it, we want your feedback to be
the start of a message board conversation. Dentaltown prides itself on bringing you quality content, much of which is
derived from these online exchanges. This transparency ensures our magazine includes the relevant topics you and your
peers are talking about.
If you have questions
If what you read in the magazine leaves you intrigued and you want to ask quesabout the site, call me at
tions, you can ask them directly of the author at the end of the online version of
480-445-9696 or e-mail me
the article. If you have a specific interest in the topic or case, or maybe are strugat kerrie@farranmedia.com.
gling with a technique, you can even upload your own case images and ask specific questions regarding your practice.
See you on the
message boards,
Maybe you want to validate an opinion or practice by sharing an example of how
Kerrie Kruse
you use the same strategies. Maybe you want to caution a treatment technique
Online Community
because of a personal experience you had in your practice. Regardless of your
Manager
motivation, collaborative feedback is what makes the Dentaltown community
the best community for dental professionals.
Dentistry’s Most Effective New Patient Attraction System
INCREASE YOUR
NEW PATIENTS
15% - 45%
WITHOUT SPENDING ONE DIME
ON ADDITIONAL ADVERTISING
For more than 25 years Jay Geier’s Scheduling Institute has
been helping thousands of dentists grow their practices,
and it all starts with increasing their new patients.
Call 877.215.8225
Go to www.SchedulingInstitute.com
FREE FACTS, circle 34 on card
14
SEPTEMBER 2012 » dentaltown.com
“2012 will be my best year ever
thanks to Six Month Smiles!”
- Dr. Noel Ananthan, Streetsville, ON, Canada
Will 20
2012
012 be your
y
your
best y
year ev
ever?
er?
Adult patients in your practice no longer need to be stuck
with crooked teeth. The award-winning Six Month Smiles
System includes short treatment times & clear braces,
giving patients the most attractive option to finally have the
smile they’ve always wanted.
BEFORE
DURING
2012 Course Schedule:
Chicago
Sept. 14-15
San Francisco
Sept. 28-29
Indianapolis
Oct. 12-13
Washington, DC
Oct. 26-27
Las Vegas
Nov. 2-3
Miami
Nov. 9-10
Phoenix
Nov. 16-17
Houston
Nov. 30-1
Los Angeles
Dec. 7-8
AFTER SIX MONTH
M
SMILES
Call us at (585) 571-4729
e-mail: Seminars@SixMonthSmiles.com
www.SixMonthSmilesTownies.com
FREE FACTS, circle 8 on card
Straight Teeth. Less Time. Clear Braces.
continuing education
update
»
What’s New in Continuing Education?
by Howard M. Goldstein, DMD, Director of Continuing Education
▼
▼
▼
▼
September is time to go back to school. But at
Understanding Color
Dentaltown, the school is anywhere and anytime you
want with our ever-expanding roster of quality online
and Shade Matching
CE courses!
in Dentistry
There have been several new releases added to
by Dr. Lane Ochi
Dentaltown’s CE course listings in the last couple
of weeks.
Dentaltown.com
Understanding Color and Shade Matching in
search Color and Shade Matching
Dentistry by Lane Ochi DDS, FACD, FICD
Prosthodontist and frequent Dentaltown.com
Message Board contributor Dr. Lane (Velogeek) Ochi
The Power of the
delves into how one uses color to get that perfect shade
Question... How to
match. Color is an integral part of aesthetic dentistry.
Move Your Patients
If the color of a restoration is off, the mistake can be
from Denial to Action
glaringly evident and the result is an unhappy patient.
by Mary Osborne
Most dental schools do not do an adequate job in
Dentaltown.com
teaching color theory. Color theory is a language that
search The Power of the Question
conceptually and perceptually describes the elements
of color and their interactions.
Unfortunately, understanding color is tricky. Slight
variances in shade play with our eyes, our minds, and,
Dental Marketing
ultimately, our dentistry. The illumination in the denSummit Series
tal treatment room, optical illusions, color blindness
by Howie Horrocks
and fatigue are among the dental professional’s ongoand Mark Dilatush
ing obstacles to successful shade matching. Dr. Ochi
will enlighten the dentist and ceramist on the dimenDentaltown.com
sions of color, the effect of metamerism and other phesearch Dental Marketing Summit
nomenon using actual examples from his own cases.
By being fluent in the language of color, we can
sharpen our perception of color, better understand existing color dynamics, make better
Treating
predictions and communicate more clearly
Worn
about color.
Smiles
A review of these concepts as rules
by Dr. John Nosti
and guidelines will be presented in a
manner that can be utilized to resolve
Dentaltown.com
complex aesthetic problems.
search Worn Smiles
The Power of the Question... How to
Move Your Patients from Denial to Action
by Mary Osborne
Internationally known speaker Mary Osborne will
help you become a more effective communicator
by learning to follow up on difficult questions and comments from patients. You will
continued on page 18
16
SEPTEMBER 2012 » dentaltown.com
Meet
M
eet TThe
he Latest
L atest Additions
Additions TTo
o TThe
he G
Gendex
ende x FFamily
amily
NE
NEW
W from
f rom G
Gendex!
ende x!
Your
Y
our IImaging
maging Future
Fu t ur e S
Starts
tar t s TToday!
ooday!
EEmbodied
mbodied in
in a sturdy,
sturdy, ergonomic
ergonomic design,
design, tthese
hese ddynamic
ynamic
eextraoral
xtraoral iimaging
maging ssystems
ystems ddeliver
eliver hhigh-quality
igh-qualit y rrepeatable
epeatable
rradiographic
adiographic results
results using
using efficient
ef ficient tools
tools such
such as
as EasyPosition™
EasyPosition™
aand
nd eeasy-to-use
asy-to-use ttouchscreens.
ouchscreens.
Cone Beam
Beam 3D
3D Imaging
Imaging Systems
Systems
P Cone
Panoramic X-ray
X-ray Systems
Systems
P Panoramic
Intraoral
Intraoral X-ray
X-ray Systems
Systems
Digital
Sensors
Digital IIntraoral
ntraoral S
en s o r s
Digital
X-ray
Digital X
hosphor PPlates
lates
-ray PPhosphor
2012
12 Gendex Dental Systems, 906.9044/09.12Rev2
©20
LLearn
earn m
more
ore aabout
bout tthe
he G
GXDP-300,
XDP-300, G
GXDP-700
XDP-700 and
and tthe
he
gendex.com
ndex.com
ffull
ull line
line of
of G
endex iimaging
maging ssolutions
olutions at
at ge
Gendex
Gendex Dental Systems
www
.gendex.com
www.gendex.com
Call toll-free: 1-888-339-4750
FREE FACTS, circle 46 on card
Intraoral
Intraoral Cameras
C am e r a s
Imaging
Imaging Software
Soff tware
continuing education
update
continued from page 16
learn how to check out assumptions; ask clarifying questions; and provide
information in a way that is clear, concise and relevant to the needs of
each patient.
In spite of our best efforts to educate patients about the need for dental care, many patients delay and avoid treatment that we know can help
them. We struggle to understand what gets in their way, and how to motivate them to take action. We sometimes get tired of being seen as the person with the bad news, rather than someone who is there to help them.
The process of making choices about health is complex, but it does
not have to be a mystery. This course will provide participants with a sixstep cycle for helping patients make healthy
choices. You can help your patients move
“In spite of our best efforts to educate
through this process without using manipulation, fear or nagging. You can learn to ask claripatients about the need for dental care,
fying questions, and give information that
many patients delay and avoid treatment
connects with the values of each individual.
This course will help you become a better listhat we know can help them.”
tener in your personal life, as well as your professional life. It will challenge your assumptions
and offer you language that is both authentic and powerful. It will help
you develop long-term, trusting relationships with your patients. It will
allow you to close the gap between what they think they want from you,
and what you know you can do for them.
A couple of months ago we released the best and most popular course
on dental marketing there is – Dental Marketing Summit Series by
Howie Horrocks and Mark Dilatush.
This series is designed and delivered to assist any dentist with the total
understanding necessary to promote dentistry properly, effectively and
efficiently. Participants will receive personalized marketing plans and the
book Unlimited New Patients – Volume 3 as part of their course material.
And released in January 2012 and rapidly becoming Dentaltown’s
most popular CE course – Treating Worn Smiles by John Nosti.
Ever wondered how Dr. John Nosti turns those worn-down teeth
back into a beautiful smile as he has shown so many times on our message boards? Join Dr. Nosti as he reviews the main causes of occlusal
breakdown in patients and discusses ways to engage your patients and get
them enrolled in their treatment, as well as review his treatment protocol
from start to finish on these complex cases. Unlike many teaser courses,
this one-hour presentation is fast-paced and teaches you what you need
to know to start your functional cosmetic practice today!
Enjoy learning from the comfort of your home! ■
To search for a course:
1. Go to the Dentaltown.com CE page at: http://dentaltown.com/onlinece
2. Enter your keywords in the box at the left
3. Click the “Search Courses” button (Do not press “Enter” or “Return”)
18
SEPTEMBER 2012 » dentaltown.com
The bulk fill flowable
strong enough
3M, ESPE and Filtek are trademarks of 3M or 3M Deutschland GmbH. Used under license in Canada.
© 3M 2012. All rights reserved. 1. Compressive strength. 2. In vitro data on file.
to be called Filtek™
From one of the most trusted innovators of restorative
solutions comes Filtek™ Bulk Fill Flowable Restorative.
s5PTOSTRONGERTHANTHELEADINGBULKlLLmOWABLE1,2
s.EARLYTWICETHEWEARRESISTANCEOFLEADINGBULKlLLmOWABLES2
s#HOICEOFDELIVERIESEASYTOUSECAPSULESORSYRINGES
s/RANGECOLORISEASYTOIDENTIFYANDASKFOR
s&LOWABLEVISCOSITYMAKESITEASYTOACHIEVEGOODADAPTATION
Filtek
™
Stronger is better.
Bulk Fill
Flowable Restorative
www.3MESPE.com/filtekbulkfill
FREE FACTS, circle 31 on card
dentaltown
staff
Editorial Advisory Board
Editorial Director
Thomas Giacobbi, DDS, FAGD • tom@farranmedia.com
Hygienetown Editorial Director
Trisha O’Hehir, RDH, MS • trisha@farranmedia.com
Editor
Benjamin Lund • ben@farranmedia.com
Associate Editor
Chelsea Knorr • chelsea@farranmedia.com
Assistant Editor
Krista Houstoun • krista@farranmedia.com
Creative Director
Amanda Culver • amanda@farranmedia.com
Graphic Designer
Corey Davern • corey@farranmedia.com
Vice President of Sales & Business Development
Pete Janicki • pete@farranmedia.com
Regional Sales Managers
Mary Lou Botto • marylou@farranmedia.com
Steve Kessler • steve@farranmedia.com
Geoff Kull • geoff@farranmedia.com
Executive Sales Assistant
Leah Harris • leah@farranmedia.com
Circulation Director
Marcie Donavon • marcie@farranmedia.com
Circulation Assistant
Kami Sifuentes • kami@farranmedia.com
Marketing Director/Online Community Manager
Kerrie Kruse • kerrie@dentaltown.com
Marketing & Events Coordinator
Marie Leland • marie@farranmedia.com
Director of Continuing Education/Message Board Manager
Howard M. Goldstein, DMD • hogo@dentaltown.com
I.T. Director
Ken Scott • ken@farranmedia.com
Internet Application Developers
Angie Fletchall • angie@farranmedia.com
Nick Avaneas • niko@farranmedia.com
MultiMedia Specialist
Devon Kraemer • devon@farranmedia.com
Publisher
Howard Farran, DDS, MBA • howard@farranmedia.com
President
Lorie Xelowski • lorie@farranmedia.com
Controller
Stacie Holub • stacie@farranmedia.com
Receivables Specialist
Kristy Corley • kristy@farranmedia.com
Seminar Coordinator
Colleen Hubbard • colleen@farranmedia.com
20
SEPTEMBER 2012 » dentaltown.com
*Continuing Education Advisory Board Member
Rebecca Bockow, DDS
Krieger Aesthetic & Reconstructive Dentistry
Seattle, WA
William Kisker, DMD, FAGD, MaCCS*
Dental Care of Vernon Hills
Vernon Hills, IL
Lee Ann Brady, DMD
Arrowhead Dental Professionals
Glendale, AZ
Kenneth Koch, DMD
Real World Endo
Wilmington, DE
Dennis Brave, DDS
Real Word Endo
Wilmington, DE
Arnold Liebman, DDS
Dr. Arnold I. Liebman
Brooklyn, NY
Doug Carlsen, DDS
Golich Carlsen
Denver, CO
Stan Mcpike, DDS
Stan Mcpike, DDS
Jonesboro, AR
Howard M. Chasolen, DMD
Sarasota, FL
John Nosti, DMD, FAGD, FACE
Advanced Cosmetic and General Dentistry
Mays Landing, NJ
Mark Fleming, DDS*
Belmont Dental Care
Scottsdale, AZ
Krzysztof Polanowski, DDS
Stomapol
Serocka, Wyszkowa, Poland
Seth Gibree, DMD, FAGD
North Georgia Smiles
Cumming, GA
Jay Reznick, DMD, MD
Southern California Center for Oral and
Facial Surgery
Tarzana, CA
Stephen Glass, DDS, FAGD*
Advanced Dentistry of Spring
Spring, TX
Lloyd Ritchie Jr., DDS
Lloyd K. Ritchie Jr., DDS
Pensacola, FL
Howard Golan, DDS, JD, MWCLI
Golan Family Dentistry
New Hyde Park, NY
Donald Roman, DMD, AFAAID
Roman Dental Arts
Paramus, NJ
Brian Gurinsky, DDS, MS
Brian Gurinsky, DDS, MS
Denver, CO
Tom Schoen, DDS
Schoen Family Dentistry
Wabasha, MN
Eyad Haidar, DMD
Weston Dentistry
Weston, MA
Timothy Tishler, DDS
Northbrook Dental Care, Ltd.
Northbrook, IL
Joshua Halderman, DDS
Northstone Dental Group
Columbus, OH
Glenn van As, BSc, DMD
Canyon Dental
North Vancouver, British Columbia, Canada
Glenn Hanf, DMD, FAGD, PC
McDowell Mountain Ranch Dentistry
Scottsdale, AZ
© 1999–2012 Dentaltown.com, LLC. All rights reserved. Printed in the USA.
Copyrights of individual articles appearing in Dentaltown reside with the individual authors. No article appearing in Dentaltown
may be reproduced in any manner or format without the express written permission of its author and Dentaltown.com, LLC.
Dentaltown.com message board content is owned solely by Dentaltown.com, LLC. Dentaltown.com message boards may not be
reproduced in any manner or format without the expressed written consent of Dentaltown.com, LLC.
Dentaltown makes every effort to report clinical information and manufacturer’s product news accurately, but cannot assume responsibility for the validity of product claims or typographical errors. Neither do the publishers assume responsibility for product names, claims,
or statements made by contributors, in message board posts, or by advertisers. Opinions or interpretations expressed by authors are their
own and do not necessarily reflect those of Dentaltown.com, LLC.
The Dentaltown.com “Townie Poll” is a voluntary survey and is not scientifically projectable to any other population. Surveys are presented to give Dentaltown participants an opportunity to share their opinions on particular topics of interest.
LETTERS: Whether you want to contradict, compliment, confirm or complain about what you have read in our pages, we want to hear
from you. Please visit us online at www.dentaltown.com.
WHAT A
DIFFERENCE
A DAY MAKES
10.
10.9
4.8
4.
.8
G-CEM™ Automix
5.3
3
3.9
3.
†
RelyX Unicem Clicker
Maxcem Elite†
4.2
4..2
1.8
1..8
G-CEM™ - Str
Stronger
ronger
o
by Design
G-CEM’ss advanced formulation provides
G-CEM’
provides higher tensile
strength
str
ength within the critical first 24 hours.
Which material would you trust?
G-CEM™ Capsules Now
G-CE
Indicated for Post & Core
Indicat
Cem
Cementation with our
G Elongation Tips!
NEW GC
FREE FACTS, circle 45 on card
'#!MERICA)NCs8FTUUI4USFFU"MTJQ*-ttXXXHDBNFSJDBDPNtXXXHDBNFSJDBDPNUSBJOJOHtª($"NFSJDB*OD
*OUFSOBMUFTUJOHEBUBPOGJMFp/PUBSFHJTUFSFEUSBEFNBSLPG($"NFSJDB*OD
howard speaks
column
» Practice with Purpose
by Howard Farran, DDS, MBA, Publisher, Dentaltown Magazine
In the July 2012 issue of Dentaltown Magazine, I
wrote about the importance of a purpose-driven life and
the difference between people who have a passion for
what they do vs. the poor souls who trade time for
money. I wrote a little about giving your team a purpose
as well, but I saved the bigger idea for this column,
which is giving your entire practice purpose. Not just
your staff, not just you, not just the chairs and the bricks
and the mortar, but the driving philosophy of your
entire practice.
Your practice’s purpose gives you clear-cut direction.
If you take a team of people who place a high value on
profitability, every decision they make will go toward
maximizing profits. On the other hand, you might have
a group of people who highly value customer care and
will do and spend almost anything to make sure their customers are well taken care of. Put those two groups
together and you’re going to see some battles. One team
might want to hold back on spending money in order to
lower overhead, while the other team really wants to
implement something new to offer customers at the
expense of the bottom line.
That’s why it is so important for companies – large
and small – to make their values and their purpose crystal clear. That’s where a mission statement comes in. Yes,
even though you might consider yourself “just a dental
practice,” you need a mission statement. A mission statement explains to your customers and your team what
your goal is and why your business exists.
Southwest Airlines’ mission statement
says, “Southwest Airlines is a company
that is for anyone and everyone that
wants to get from point A to point B by
flying. Our service and philosophy is to
fly safe, with high frequency, low-cost
flights that can get passengers to their
destinations on time and often closer to
their destination. We fly in 58 cities
and 30 states and are the world’s
largest short-haul carrier and
we make sure that it is run
efficiently and in a
economical way.” In
a rather succinct 80
words Southwest Airlines lays out exactly what it does,
and if you’ve ever flown Southwest, it’s apparent that its
employees take this mission statement to heart.
Other mission statements use broad strokes. Take
Sears’ for instance: “To grow our business by providing
quality products and services at great value when and
where our customers want them, and by building positive,
lasting relationships with our customers.” Pretty broad
(actually, a little too broad… and maybe a bit vague), but
that’s OK, because when you delve into your company’s
list of core values, you can further define your mission.
And in case you were wondering, Dentaltown’s
mission statement is: “To better dentistry by connecting dental professionals through traditional and innovative media.”
Now that you’ve explained who you are and what
you do, it’s time to explain the “how” through developing
your core values. Core values are extremely important.
Without them, your team members will make all of their
decisions based on what they think is best – which may
not actually jibe with the practice’s philosophy. You can’t
afford contradiction and infighting; everyone needs to be
on the same page and adhering to the same values, otherwise you’re not going to move forward. Your company
needs to make clear to the entire team what it values and
how it will conduct business.
Some companies have five core values, some have 25.
We spent months developing the core values for
Dentaltown and my dental practice, Today’s Dental, and
whittled our list to what we thought are the 12 most
important values we, as a company and a dental practice,
needed to adhere to. If someone doesn’t “get” my corporate
culture, I can get them right out the door permanently.
First off, we all decided it was important to create a
fun, positive and professional environment. People
don’t want to come to work and deal with all the catty,
tacky garbage people tend to bring into an office, which
eventually makes people feel bad. These are your teammates and they’re your allies.
We require our teams to be passionate, enthusiastic
and determined to make a difference. Try as hard as you
can but you can’t train people to be these three things.
You must make sure you’re hiring people who carry these
traits and be prepared to jettison those who do not.
continued on page 24
22
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 47 on card
howard speaks
column
continued from page 22
Find us on Facebook
www.facebook.com/dentaltown
Be humble. This is something a lot of people have
trouble with – myself included. When you’ve gone to
school for eight years and you come out ready to champion the oral health of your town, it comes with a little
bluster. But just because you’re a doctor and you make the
big bucks, and you’re talking to the mother of a caries-ridden two-year-old and she’s pouring Mountain Dew into
his mouth, doesn’t mean you get to be a high-falootin’
jerk. You have to be a leader. You can’t chastise her or
make her feel bad. I have had patients who have come in
and said, “If I don’t give her Mountain Dew she’ll cry.”
You’ve got to be calm, take the high road and say, “OK,
but what is your baby doing right now? She’s crying
because she has a toothache, and it could be caused by the
Mountain Dew. You’re not a bad person. You just did
what you thought was right, but it’s my job to empower
you to make higher quality decisions so that your daughter keeps her teeth for the rest of her life.” Remember, you
exist to teach, not criticize.
“Empower your staff. Be helpful.
Coach them. Invest in training your
team and when they are finished
training, get them some more!”
You have to embrace and drive innovation. You have
to adopt all technology that makes you do dentistry faster,
easier, of a higher quality and at a lower cost. Macroeconomics is made up of three things – people, technology
and capital. You have to embrace all new technology.
You’ve got to follow the golden rule (“Treat others
like you would want to be treated”); the common thread
found at the heart of every major religion. Simple enough,
right? Not really… Let’s say your child was injured or sick
and you needed to take her to the emergency room. Your
child might be scared and might start asking the nurse
questions. Would you really want to hear the nurse say,
“I’m sorry, I can’t talk about this with you. The controlfreak doctor says I can’t talk to you like a human.” Nobody
wants to hear that, and certainly nobody wants to say that,
but when someone calls up your practice and your front
desk can’t explain what they think because you’ve got them
gagged, there’s something wrong.
Mistakes will be made. Be accepting and accountable, and move forward. You’re not perfect, doc. Nobody
is. There’s a reason why we call it a “dental practice” –
nobody’s perfected it, and nobody ever will. We are our
own worst critics; if someone screws up, help them realize their mistake, redirect if it’s needed and then move
forward. You don’t laugh at them or chastise them or
belittle them. Mistakes are an opportunity to learn.
Speaking of which…
Never stop learning. This is a favorite of mine
because if your practice chooses to adopt this particular
core value, I can help you and your team along by shamelessly promoting Dentaltown.com’s awesome line-up of
online continuing education courses. You don’t have to
take notes. You don’t have to get a hotel. You don’t have
to buy an airline ticket. And all of our courses will not
just benefit you but your whole team. Why don’t you do
something educational and morale boosting for your
team like Terrific Tuesdays, when every Tuesday you
spring for pizza and the whole staff stays in and watches
a one hour-long online CE course given by the best
instructors around the world? It’s important to continue
improving your knowledge base and your skills. Keep
learning new techniques that will start making your practice money, like sleep dentistry or implants.
If you’re on my team, you need to be honest and
respectful. Integrity is everything. You have to report your
cash because if you don’t your staff thinks it’s OK to steal
from the IRS, therefore it’s OK to steal from you. You have
to warranty all your work. You have to be honest. If you
screw up, you tell a patient, hey I’m a human and I just
broke the bur off into your nerve and this is what I did.
Don’t cover it up. Don’t lie. It just makes things worse. Be
honest, get it all out front.
You have to balance life and work and be fully
present in both. To take this a little further, I’ve got my
four Bs: my body, my babies, my business and my babe.
If you don’t take care of your body, then babies, business and babe don’t matter because you’ll be dead. You
stay healthy in order to be there for your family and
your business. So many of us are workaholics. We
ignore our families until they want nothing to do with
us and we get upset when they eventually only love us
because we give them money (because that’s the only
part of you you really ever gave them). It disappoints
me when dentists take personal calls from their spouses
all day long but won’t let their staff take personal calls
from their spouse or their children. When your kid is
having a crisis, you reschedule all of your appointments,
but when your hygienist’s child is facing a crisis, you
raise hell and start making threats. It’s an awful double
standard. Remember, treat other people how you want
to be treated.
continued on page 26
24
SEPTEMBER 2012 » dentaltown.com
#(&$($#
(
(
(((%$(%(%$$#$"(CO.
( ( (
(
(
(
before
after
results like these...
...consistently.
continuous refrigeration
heat is any whitening gel’s worst enemy.
FREE FACTS, circle 44 on card
The warmer gels get, the less potent they become.
( ( $("($("$%"
(
( (
((
KöR® (('&%$#"%"!(%( ($&#(
refrigerate an entire line of whitening gels from the
#"$(( (( "$#(( "$%(( (( ##%#(( $&#((
(( %"!(( $&#(( %$(( (( $#"$(( "(( #((
$(#%#("
(
(
% $#"$(%"!(#
(
( $ (
$
( (
( $("#(
(
(
of many ways KöR Whitening relies on science and
( (
( (
( ( $ (("$
( (
!%($(&#((&%##($&#(#
The Science of Whitening™
dr.
dr. rod
rod kurthy
k ur
Developer
D e ve l o p e r & W
Whitening
hi tening SScience
cience EExpert
x
888-816-7764
###"$# $
howard speaks
column
continued from page 24
Strive to make everyone feel safe, valued and
important. I’ve witnessed dysfunctional staff meetings
where the doctor barks orders or makes a decision before
talking to the staff, and the whole team just looks at him,
their eyes as wide as saucers, and before anyone can ask a
question the team is dismissed and everyone runs away.
That is so dysfunctional. I remember the last time I ever
held a staff meeting like this. I told my staff we were buying a CEREC milling unit and my assistant Jan spoke up
and said, “That’s the stupidest thing I’ve ever heard in my
life.” It wasn’t because she thought buying a CEREC was
a bad idea, it was because our office needed to be
updated. After that meeting, we argued about this for
about a month. Eventually, and with some long-term
financial planning, we all got what we wanted. The point
of this story is, in that month while Jan and I butted
heads, not once was she afraid that she was going to lose
her job because she stood up to me. My team knows I’m
not going to fire them or abuse them for standing up to
me. We can disagree and have heated debates, but they
must be done in a respectful way so nobody fears losing
their job just because they disagree with me. You need
this in a practice because it allows your team ownership
of all of the decisions that are made.
Be remarkably helpful. Give a man a fish and you
feed him for a day. Teach a man to fish and you feed him
»
Howard Live
Howard Farran, DDS, MBA, is an international speaker
who has written dozens of published articles. To schedule Howard to speak to your next national, state or local
dental meeting, e-mail colleen@farranmedia.com.
2012
29
SEP
Excellence in Dentistry
2-3
OCT
Asteto Dent Labs
6OCT
American Orthodontic Society
Dallas, Texas
www.profitabledentist.com
Jennifer Jones – 812-949-9043
Newark, New Jersey
mdaich@aol.com
Memphis, Tennessee
Barbara Zuniga – 800-448-1601
bzuniga@orthodontics.com
www.orthodontics.com
26
SEPTEMBER 2012 » dentaltown.com
for a lifetime. Empower your staff. Be helpful. Coach
them. Invest in training your team and when they are
finished training, get them some more! I can’t say enough
about online CE. Your hygienists and assistants should
know exactly what is going on with a root canal. If you
want your receptionist telling people how much a root
canal costs, she should at least know what a root canal is.
Have her take a CE course on Dentaltown.com. In one
hour, she can learn what a root canal is, know how to
make one better and faster and then when she’s done
with the root canal course, she can explain what she
learned to patients (and tell them how good you are at
it). Empower everyone with knowledge – it’s the best
help you can give.
Our final core value prompts our team to create
opportunities to make our customers feel special. In
these turbulent economic times, why are you taking off
your gloves and mask and slinking back to your office
while the local anesthetic sets in? You need to take these
golden opportunities to bond with your patients, share
things with them and listen to them. At the very least,
review their social network. Why not?! They’re just going
to be sitting there soaking up the Novocain anyhow. Say to
them, “By the way, how’s the rest of the family? I haven’t
seen your husband in a while. When’s the next time he’s
going to come see me?” Review the treatment plan – not
just of your patient in the chair, but of their family as well.
Say, “OK, your kids are nine and 10. We talked about
sending them for an orthodontic consult when your
daughter is 12 and your little boy is 13…” Engage them.
Bring up their pano, their digital X-rays. Stay in that operatory to teach. Ensure everyone in your office is a teacher.
Give everybody a purpose to teach, you want a measurable
impact on the improvement on everyone’s oral health from
when you graduated from school to when you retire.
Being clear about your purpose is one thing, but
actually following your own core values is another.
You might spend a year coming up with your company’s
mission and core values, but without consistent follow
through, they won’t mean a damn thing. When you
review your employees, you must hold them accountable
to all of your practice’s values. The staff should also have
the freedom to police each other. If someone’s behavior
isn’t in line with any of your core values, that person
needs to be called out and be held accountable for their
actions. Everyone should have the opportunity to change
their ways, but if someone on the team is consistently
not adhering to any of your company’s values, perhaps
it’s time that person find another practice whose values
are more in line with his or her own. ■
43210/.-,1+*),3('32+'&(')%3
3
3 3
3
$/#-%3"/#!%3$
3
3 0( 0%
10/.-,/
!
+ + +
+
+
+
+ +
+
+
+
+ +
+
+
+
+
+ +
+ +
+
+ +
+
+
+
+
+ +
+
+ +
+
+ +
+ +
+
+
#
# &$#(#)%##('#&(##%
(&#
#
#
# #
# #
#
#
%#%#%(#)('&#
#%
#
#
#
# #
#
# &#&#
# # ##
('#&'&#'(#'
#
# #
& ! &#%'#'(#
# # #
& '#%
#
'##
# # #$('#
#
#
#(#""#'!'&(#(#(#%'#
# #
#
# # #
#
%'#(&#
#
# ''(!%& ('
$/#-3#(
3
03/
3
(/-(+'
01#/-( 03/'&3+1)((')
3
3
(),3+'&3#-10')-,#
3
3
-1/3-,('
3
+'#(#-0'- !300-(+'/
3
3310#*
33
-#
)('&%$&#"%'!
#
#(#(##%#(#&3
# #
#
#
# # 3
"
3"310
3
3
*&03$$"
3
+
(#(-3+*130#(-03+13/
3 3
3 3 33*#3-+&/!3/-33-+3
3
3 3
3 3
'&3+*-3+103+13+'-/-3!+*13&0/
3 3
3 3
3
3
013+13*1,/#0
3 3
FREE FACTS, circle 42 on card
professional courtesy
column
»
The Magical Mystery Office Tour
by Thomas Giacobbi, DDS, FAGD, Editorial Director, Dentaltown Magazine
Do you give tours of your dental office? I was
asked this question recently while taking a tour of Adec’s manufacturing facilities in Newberg, Oregon. I
suspect your initial reaction was similar to mine: “Is
that something that patients would want to do?” and
“I don’t have time for something like that.” I am not
advocating that you turn your office into a museum
with guided tours, rather that you think about your
office through the eyes of a patient taking a tour.
The A-dec tour left me with a very positive
impression of their company for the following reasons: Every inch of each factory building was swept
clean, the workstations were organized and every
employee we passed along the way had a smile on
their face. Notice the first things I mentioned about
the tour had nothing to do with how they make the
chairs? Our patients are no different. Since I’m a
geek dentist, I had tremendous appreciation for the
process of building a dental chair and delivery unit
from the ground up. It is a fascinating orchestration
of separate processes that come together in an exquisite way. The principals of Just-in-Time management are at work and nearly every job can be
tracked to a specific order. The employees are clearly
empowered and loyal – the younger employees have
been there 10 years!
Another fine example is the Innovation
Center at 3M headquarters in Minnesota.
This building serves as a center for visitors
from many different industries from all over
the world. It is a showcase of the many
technologies that 3M has available to create
the products that we use every day inside
and outside of our dental offices. The tour
is more than just look and see – it is an
education about their company, its history
and the culture of innovation. If you went into
engineering instead of dentistry, this
could be a dream job. Once again,
many of the employees I have
encountered during my numerous visits have many years of
service under their belts.
28
SEPTEMBER 2012 » dentaltown.com
Let’s turn this discussion back to our dental
practices and ask a few essential questions:
• Would you be happy to give any patient a
complete tour of your office at any time?
• Are there any locations within your office
that you would not be proud to show due
to a lack of organization or cleanliness?
• How many team members do you have that
would make great tour guides?
• Would your tour guide be able to share the
culture of your practice?
• Do you have a written mission statement?
Are your team members familiar with this
document?
• When your patient meets other team members along the way, would they be impressed
by their attitude and commitment to the
practice?
• Could you (the Dr.) demonstrate or describe
the things you do behind the scenes to
ensure that your patients receive the best
care possible?
• Is there anything that you do in the practice
you would not want a patient to see?
To be clear, I am not suggesting that your
office must be filled with brand new equipment
or that you must be as rich as a multi-billion
dollar company. The self-examination that the
answers to these questions will provide is a great
way to find out if you are working in the practice
of your dreams. Ask your team members to give
each other a tour of the office with a critical eye.
If you would like to really learn something about
your office, ask three or four team members to
each do a video tour of the office with their cell
phone camera or one that you provide. Be sure
they work separately as this will provide different
perspectives. Their videos will provide new
insights into the strengths and weaknesses of
your practice. If you learn something new about
your practice with this exercise, or if you have
any comments to share, please send an e-mail to:
tom@dentaltown.com. ■
Bluephase Style
®
LED Curing Light
Very small, cures all.
The latest advancement in LED curing lights
s0ATENTED0OLYWAVE™TECHNOLOGYTOCUREALLDENTALMATERIALS1
s3PECIALLYDESIGNEDLIGHTPROBEFOREASYACCESSTOPOSTERIORTEETH
s#ORDLESSORCORDEDUSE
&ORMOREINFORMATIONLOGONTOivoclarvivadent.com/bluephasestyle
100% CUSTOMER SATISFACTION
GUARANTEED!
ivoclarvivadent.com
Call us toll free at 1-800-533-6825 in the U.S., 1-800-263-8182 in Canada.
©2012 Ivoclar Vivadent, Inc. Bluephase and Polywave are trademarks of Ivoclar Vivadent.
1
All materials known to date in the range of 385 – 515 nm
FREE FACTS, circle 35 on card
second opinion
column
» The Dilemma of Dental Aid Therapists
by Fred Joyal
There is an ever-increasing amount of buzz
about dental aid therapists, especially in light of the
recent Frontline coverage on access to care and corporate dentistry. I’m going to try to distill this down
to its essentials.
First, let me say that this is an issue dentists need to
confront head-on; otherwise government is going to
feel the pressure to solve the access to care issue for you.
As you might know, there are several states that are
training dental aid therapists already (DATs, as I will
call them), and more are considering it.
The issue as I see it has five different interrelated
elements. They are:
1. Access to affordable dental care for about onethird of the population;
2. Lack of basic understanding of oral health in
about two-thirds of the population;
3. The rising cost of dental school and subsequent
student debt;
4. Ignorance of the total economic impact of the
dental health crisis;
5. The scarcity mindset of many dentists.
Access to Care
This is both a geographic and economic problem.
Many people cannot afford even basic dentistry. They
are unlikely to have any dental “insurance,” and if
gasoline goes up 50 cents, every bit of their discretionary income disappears, if they had
any to start. I know that they might still
spend money unwisely – on tattoos,
cigarettes and things like that – but
you won’t change that about people. I believe in focusing on what
realistically can be changed, rather
than pointlessly pontificating about
what people should do.
Access to care is also tied directly to
the next two elements.
Dental Health Education
People are woefully ignorant of how and why to
take care of their teeth. At
the lower income levels
people are also often
misinformed, believing, for example, that since
deciduous teeth are going to fall out anyway, there is
no need to take care of them. But it is not just the
lower class. At every income stratum millions of people do not appreciate the essential nature of oral
health. This will not be solved by some educational
program or ad program. It would take hundreds of
millions of dollars and a really effective campaign.
Who is going to do that? The ADA? Not a chance.
They’d have to increase dues by $1,000 a year. 1800-DENTIST, a large voice to consumers, already
spends $50 million a year, and it’s a blip on the
screen in terms of changing awareness.
Dental School Tuition
The average cost of dental school, including tuition
and living expenses, now exceeds $100,000 per year.
Students typically graduate with debt in excess of
$250,000, and the interest rate for graduate student
loans is double what it is for undergrads. The money
that was once used to buy a practice is now used to service that debt. And directly related to access to care is the
fact that a new dentist is not going to practice in an
underserved area like rural Tennessee for two reasons:
one, she doesn’t want to make $70,000 a year and only
do extractions, and two, she doesn’t want to live there.
When I talk to dental students, they all want to practice
within 10 miles of where they would like to live. They
give almost no consideration to how many other dentists are already there, which is why we have such a wide
disparity across the country in providers per capita.
Economic Impact
States and counties are just starting to realize that
when they cut state aid for dentistry the problem and
cost doesn’t go away (shocking!), but the burden is
shifted to ERs, where treatment costs an average of 10
times as much, virtually all of it paid by the county.
The exponential savings of preventive care is never
more evident than in dentistry, but few legislatures get
this. And even fewer are calculating the impact on
absenteeism and productivity of employees with dental
pain. And even worse is the downward spiral created
in children’s lives when tooth pain keeps them out of
school, affecting their learning, and inevitable tooth
loss limits their job opportunities.
continued on page 32
30
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 22 on card
second opinion
column
continued from page 30
Scarcity
Despite the fact that 30 to 50 percent of the population
doesn’t see a dentist regularly, many dentists complain that there
isn’t enough opportunity, and worry that dental aid therapists
will take away even more income from them than the recession
has. I believe that dentistry is the most abundant profession in
the country, but that requires adaptability. We need to evolve
how our services are delivered.
I sincerely believe that dental aid therapists have the potential to address all these issues. Before you fetch the pitchforks,
hear me out.
First, it is never going to be feasible for most dentists to treat
the underserved segment of the population. We are coming up on
a shortage of dentists as it is, due to population growth outpacing
graduates – by some estimate a shortfall of 35,000 dentists by
2025. And few of you can treat patients for 25 percent of your
normal fees without eventually closing your doors.
Second, the only way people learn anything is when they are
listening. When it comes to taking care of their teeth, this happens when they are in a dental office. DATs will bring millions
more people into dental care, and begin this education process.
Furthermore, and this is no small point, many people with dental issues put off seeing a dentist precisely because they know
that the diagnosis will be serious, as will the cost. It’s human
nature. Many will believe that going to a DAT will be safer,
because she won’t be able to do the whole treatment. And gradually they will be drawn into preventive care.
Which leads to my third point: The more people visiting
someone about their teeth, the more dentistry will be diagnosed and treated, especially if they are also being educated. I
believe billions more in dentistry will be done. What this is
called in marketing terms is “broadening the category.” Just as
Invisalign did not destroy orthodontics, but instead created
millions more cases with patients who would never have put
brackets on their teeth, and whitening vastly expanded the cosmetic veneer market, this can happen in all of dentistry, if the
proper gateway is created.
DATs will tend to be smaller, storefront-type facilities, which
will also create greater awareness. They will work hours that are
more convenient to the lower classes.
Governments will see the real economic benefit of this at
some point, and start to support it more intelligently. (OK, I’m
a wide-eyed optimist on this one.)
We will never get all dentists to agree on this. And societies see
their primary job as preserving dentists’ income, so they will not
get behind it. But it’s coming. And it will not destroy dentistry.
(They’ve had DATs in New Zealand for 90 years – no disaster yet.)
So you can fight it, or see it as an opportunity.
I know the argument is that people will not be getting good,
professional dentistry. But they already aren’t. Just as supervised
neglect is better than unsupervised neglect, infrequent treatment
continued on page 34
FREE FACTS, circle 16 on card
32
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 37 on card
second opinion
column
continued from page 32
is better than none. And pretending that the problem
will solve itself with proper education is a pipe dream.
Here’s my recommendation: Embrace this, and as a
dentist, create three or four dental aid therapist clinics
in your area that essentially feed you cases as they arise
from patients who cannot be treated by the DAT. (OK,
maybe start with just one!)
This is also what we call “a technology play” in
business. These clinics will often be one or two person operations, where appointing, billing and record
management could be a challenge. With the right
technology you can manage them centrally. Your current PMS and phone system will handle it, most
likely. Beyond that, you can also do remote diagnosis
with each of those facilities – the technology is
already there, with intra-oral cameras, digital radiography and Skype.
Lastly, instead of fighting it, get involved in the
training and regulation of DATs, so that states are not
just making up rules that could botch the whole process.
There are four stages of societal change: ignorance,
denial, violent resistance and finally acceptance. The
sooner we get to acceptance, the sooner this crisis
abates, and the faster the dental category broadens.
If I’m wrong, tell me why. I’m all ears. Feel free to
write me at fred@1800dentist.com. ■
Author’s Bio
Fred Joyal co-founded 1-800-DENTIST in 1986. As the company’s CEO, he has written more than 200 television and radio commercials and interacted with
thousands of the most successful dentists across the country. Under Fred’s leadership, 1-800-DENTIST has matched millions of consumers with the right
dentist, giving him unique insight into the mindset of the modern dental patient. Fred launched GoAskFred.com, a free online marketing resource, to share
his expertise. He is also the author of Everything is Marketing: The Ultimate Strategy for Dental Practice Growth, which is available at www.goaskfred.com.
You can reach Fred at fred@1800dentist.com.
Stands out for blending in.
No wonder it’s called the “Miracle Match” composite. Just one shade of
Estelite Sigma Quick® invisibly blends with up to 10 shades to match its
surroundings, eliminating the need to stock excess inventory. See how one
shade will change your world!
Try a FREE sample today by visiting www.themiraclematch.com.
FREE FACTS, circle 27 on card
34
SEPTEMBER 2012 » dentaltown.com
Upgrade to
Brilliance
Improve your performance. Add fluid
maneuverability and see colors accurately
for better tissue analysis. Compared to
conventional halogen lights, A-dec LED
delivers 25% more illuminance at one-fifth
of the power consumption.
If you already own an A-dec light, you may
be eligible for special savings. For details
about an upgrade, talk to an A-dec Customer
Service Representative at 1.800.547.1883.
Earn a CE credit by attending Dentalcompare’s
live webinar LED Lighting for the Operatory
(Sept. 25 at 1 p.m. PDT). For details and
registration, go to a-dec.com/LEDwebinar.
To learn how A-dec LED
gives you exceptional
performance and
unparalleled ergonomics,
visit a-dec.com/LED.
FREE FACTS, circle 38 on card
© 2012 A-dec Inc.
All rights reserved.
cosmetic
townie clinical
»
More Single Tooth Isolation
Anterior Composites
Dentaltown Message Board > Cosmetic Dentistry > Cosmetic Dentistry > More Single Tooth Isolation Anterior Composites
▼
A Townie offers colleagues a collection of impressive single tooth isolation anterior composite cases.
satchdds
Member Since: 04/19/02
Post: 1 & 2 of 68
Fig. 1: Nineteen-year-old with leaky resin done by her pediatric dentist after ortho.
Surpass, supreme and seam-free.
F ig. 1
F ig. 2
F ig. 3
F ig. 5
F ig. 6
Fig. 2: From the lingual.
Fig. 3: Closer.
F ig. 4
▼
Interested in other discussions
regarding similar techniques? Check
out the following message boards:
My Single Tooth
Isolation Technique
Search: Tooth Isolation
Composite Mock Up
of Anterior Wear Case
Search: Anterior Composite
Fig. 4: Showing her the decay.
Fig. 5: Perfect isolation.
Fig. 6: Buildup prior to any trimming. This was bonded
with Surpass, layers of different supreme. C-1 B as the base,
A-1 E next with the incisal GT for the translucency. Then GT
translucent over the A1E as enamel layer.
Fig. 8: I did take off more from the incisal after this
photo. I think it came out pretty good for a hack like me.
[Posted: 1/25/2012]
Figs. 9-16: She is getting married next month in Key West.
I told her to replace this a few years ago at her initial exam. I
whitened her last month and now we are ready to bond.
F ig. 9
F ig. 10
F ig. 7
F ig. 8
F ig. 11
continued on page 38
36
SEPTEMBER 2012 » dentaltown.com
The
Th
he Lightest
Lighttest is no
now
ow even
Lighter!
The Lightest Mini LED!
r
r
r
r
r
SEE it Even Better –
45 Day, NO Obligation Trial
1.800.345.4009
www.DesignsForVision.com FREE FACTS, circle 33 on card
cosmetic
townie clinical
continued from page 36
F ig. 12
F ig. 13
F ig. 14
F ig. 15
F ig. 16
F ig. 17
Fig. 17: Surpass, seam-free, Filtex WB, WE and some YT… how much do you all charge
for this service? ■
JAN 12 2012
twmdds
Member Since: 02/16/04
Post: 3 of 68
Satch, I love the technique and use it all the time. Thanks for teaching. ■ Tom
JAN 25 2012
continued on page 40
UPCOMING
COURSES
THE HOTTEST TOPICS IN DENTISTRY!
INCREASE YOUR PRODUCTION IMMEDIATELY
The Absolute Best Value in Dental CE Offered Anywhere!
Presented by: Louis Malcmacher DDS MAGD
October 24 –
Houston, TX
Course objective:
Learn HANDS-ON about the most trusted and cutting edge advances in general dentistry
including operative dentistry, prosthodontics, CAD-CAM, lasers, Botox and dermal fillers, esthetic
dentistry, oral medicine, lowering overhead control, total case acceptance and much more!
October 31 –
Orange County, CA
November 2 –
Los Angeles, CA
Tuition only $97 per doctor, $47 per team member,
or $197 per office (doctor plus up to 4 team members)
7 AGD PACE Participation CE credits.
November 7 –
Phoenix, AZ
"Dr. Louis Malcmacher is a combination of the genius of Dr. Gordon
Christensen and the entertainment of the Madow Brothers. We loved
the Hottest Hands-On Topics course!" – Dr. Robert Fields, Van Nuys, CA
November 14 –
Chicago, IL
SIGN UP
Before October 1, 2012. Limited Attendance
Call Today! 1-800-952-0521 or visit: CommonSenseDentistry.com
FREE FACTS, circle 4 on card
38
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 26 on card
cosmetic
townie clinical
continued from page 38
satchdds
Member Since: 04/19/02
Posts: 4 & 5 of 68
F ig. 18
F ig. 19
F ig. 20
F ig. 21
F ig. 22
F ig. 23
F ig. 25
Figs. 18-19: # 9 and 10 from F ig. 24
today. I coded these. MFL, F. I
charged for the facial twice.
Fig. 20: #9 isolated.
Fig. 22: #10 isolated.
[Posted: 2/7/2012]
Fig. 26: Today’s rubber fun.
Met this kid last week. Pepsi addiction. Since our conversation he has only had four cans
(with meals).
Figs. 27-28: Prior to trimming.
Fig. 29: 2, 3, 5 and 7. 8 is next.
Fig. 30: Prepping #8. Still loaded with dk.
Fig. 34: And his #1 with b dk... this one is for Murph... full quadrant except 4 and 6. ■
F ig. 26
F ig. 27
F ig. 28
F ig. 29
F ig. 30
F ig. 31
F ig. 32
F ig. 33
F ig. 34
FEB 7 2012
continued on page 42
40
SEPTEMBER 2012 » dentaltown.com
You went to dental school to become a dentist.
Now Dr. Farran teaches you and your staff
the business of dentistry.
Dr. Howard Farran is sharing his proven techniques to
increase your productivity and build your business.
With this special, you’ll also receive a bonus DVD
with Howard’s off-the cuff comments from his
Howard Speaks series, bloopers from his live lecture
and dental forms you can use in your practice today!
All for only
To order:
call 480-445-9712 or
visit www.dentaltown.com/onedaymba
cosmetic
townie clinical
Raj D
Member Since: 06/03/03
Post: 6 of 68
continued from page 40
Satch, beautiful work as usual. I recently started using rd for composites after years
of using it only for endo. It makes life easy! Are you allowed to bill out the same surface twice like you did on numbers 9 and 10? Thanks for posting. ■
FEB 7 2012
skuzma2dds
Member Since: 08/06/07
Post: 7 of 68
deserteagle
Member Since: 09/20/06
Post: 12 of 68
Great work… and really great showcase. Certainly a great technique for longevity. ■
FEB 7 2012
Good work, Satch. Usually when I use the 212 retainer it won’t stay firm. How do you
stabilize the retainer? Do you put some flowable on the lingual? ■
FEB 7 2012
satchdds
Member Since: 04/19/02
Post: 13 of 68
Fig. 35: Emergency patient… lucky I have six chairs. Her son wanted mommy to try his
cookie… that’s her story.
F ig. 35
F ig. 36
F ig. 37
continued on page 44
FREE FACTS, circle 5 on card
42
SEPTEMBER 2012 » dentaltown.com
TM
SELF-ETCH BONDING SYSTEM
T
Shear Bond Strengths
Surpass
Scotchbond MP+
Optibond FL
All Bond 2
®
®
Brush & Bond
®
SE Bond
Excite ®
®
®
®
Dentin
Enamel
58.2
60.1
37.7
39.2
48.2
49.2
36.1
42.1
33.7
18.8
43.7
28.5
22.1
23.4
.
Order your supply today:
T: 1.877.APEX123 | www.apexdentalmaterials.com
FREE FACTS, circle 39 on card
cosmetic
townie clinical
continued from page 42
F ig. 38
F ig. 39
F ig. 40
Fig. 38: I had to lock the clamp with composite buttons. ■
FEB 7 2012
ponderosa
Member Since: 08/30/07
Post: 14 of 68
satchdds
Member Since: 04/19/02
Posts: 15, 17, 20 & 21 of 68
Nice work, Satch. Are you using a mylar matrix and wedge for the interprox at all? ■ Gary
FEB 7 2012
Not usually a wedge but occasionally the gingival interproximal area needs a mylar. I take
it out as soon as I cure the composite to build up the contact and contours.
[Posted: 2/8/2012]
Here is an older guy with some decay on the facial of #10, with a 30-year-old crown.
Since I have a rubber dam on I can now etch the porcelain with Ultradent Porcelain Etch. I
hate sandblasting in the mouth... yuck. The porcelain is then treated with Apex Interface followed by surpass 2 and 3. The filling was done with Injectafil from a Centrix needle tip.
Almost zero finishing was needed.
continued on page 46
FREE FACTS, circle 17 on card
44
SEPTEMBER 2012 » dentaltown.com
Award Winning Digital Sensors & Practice Management Software
3
Limited Time Offers
Expires: Sept. 30, 2012
OPTION 3
OPTION 2
Digital Sensors
OPTION 1
Excellent–Good
Image Quality
–Clinicians Report, September 2011
&
An independent, nonprofit, dental education and product testing
foundation. For the full report, call (800) 704-8494
& Practice
Management
Software
Practice
Management
Software
Digital
D gi
Digita
Sensors
Sen
Interest
Interest FREE Financing
for12 Months
With any sensor bundle purchase*
FREE
F
“Paperless”
“Paperl
les Software
With any Practice Management
Software Purchase*
Purchase these award-winning
products together or separately.
Combining DentiMax Practice Management
software with DentiMax digital sensors makes for
one very powerful system—allowing you to view
digital x-rays while treatment planning at the
same time. However, if your office is already
married to either a practice management or
digital sensor system, DentiMax can make your
partial system complete.
*Offers cannot be combined with any other offer. Expires September 30, 2012.
Call for important qualification information and terms and conditions.
Complete
Bundle
FREE
Apple iPad 3
&
Interest
Interest
In
er t FREE Financing
for12 Months
With Complete Sensor & Practice
Management Software Bundle.*
Call Today!
(800) 704-8494
FREE FACTS, circle 19 on card
cosmetic
townie clinical
continued from page 44
F ig. 41
F ig. 42
F ig. 43
Fig. 41: Porcelain etch on the crown.
[Posted: 2/15/2012]
Fig. 44: This is #7 on a case that we are doing implants on an accident to his centrals
that I just posted. Someone asked if I ever needed a mylar. Deep decay like this for the gingival area. Then remove the mylar as in the picture after the mylar one.
Fig. 45: Mylar in place.
F ig. 44
F ig. 45
F ig. 46
F ig. 47
F ig. 48
F ig. 49
Fig. 46: Mylar removed.
Figs. 47-48: Lingual view before trimming.
Fig. 49: The tissue between 7 and 8 is bad because we just pulled #8 and grafted him last
week. Cantilever pontic off of a fractured # 9. See my other thread about the trampoline.
[Posted: 2/20/2012]
Figs. 50-54: This guy is a contractor. He lost his balance while installing a toilet and
kissed it. Not kidding. That’s his story.
F ig. 50
F ig. 51
F ig. 52
F ig. 53
F ig. 54
F ig. 55
continued on page 48
46
SEPTEMBER 2012 » dentaltown.com
Premier® Implant Cement™
Secure Retention.
0REMIER )MPLANT #EMENT OFFERS THE
STRENGTH AND DURABILITY OF RESIN CEMENTS ASSURING LONGTERM
PERFORMANCE FOR PERMANENT IMPLANTRETAINED RESTORATIONS AND
LONGTERMPROVISIONALSPremier Implant Cement will not wash out!
Retrievability.
0OLYMER ELASTICITY AND A NONEUGENOL FORMULA
MAKE 0REMIER )MPLANT #EMENT IDEAL FOR LONGTERM TEMPORARIES
ANDANYIMPLANTRETAINEDCROWNSTHATMAYREQUIREADJUSTMENTOR
RETREATMENT 7ITH NO CHEMICAL BONDING CROWNS CAN BE REMOVED
MOREEASILYnIFNEEDED
Easy to Use. 4HEAUTOMIXSYRINGEENSURESCONTROLLEDDOSINGAND
THE UNIQUE TWOSTAGE AUTOCURING MAKES SEATING THE RESTORATION AND
REMOVINGEXCESSCEMENTQUICKANDSIMPLE
NEW! Premier® Implant Cement™ Value Pack
3 - 5ml syringes and 25 mix-tips
Secure retention and retrievability
in one unique cement.
Save over 25% per syringe!
Premier® Dental Products Company s 888-670-6100 s www.premusa.com s#OSMETICs%NDORestoratives(YGIENE0ERIOs)NSTRUMENTSs0ROSTHETIC
"AIL#!!NINVITROANDVIVOEVALUATIONOFVARIOUSIMPLANTCLEANINGINSTRUMENTS
FREE FACTS, circle 20 on card
cosmetic
townie clinical
continued from page 46
F ig. 56
F ig. 57
F ig. 58
Fig. 55: Prior to bonding with surpass. ■
FEB 20 2012
mling
Member Since: 11/20/08
Post: 22 of 68
What’s your technique for getting such nice contacts? ■
FEB 20 2012
satchdds
Member Since: 04/19/02
Post: 23 of 68
I just build the composite against the thin and stretched r.d. The contact is as long as I
make it. Very different than a contact made with a mylar. It’s more like the contact you get
with plumbers tape. ■
FEB 21 2012
mling
Member Since: 11/20/08
Post: 24 of 68
So you stretch the dam thin, place your composite, shape it and cure it, all while holding the dam tight? ■
FEB 21 2012
satchdds
Member Since: 04/19/02
Posts: 25, 28 & 31 of 68
Sorry, no. I don’t need to hold the dam after it is stretched over the tooth. It is very thin.
You just need to practice free-hand sculpting.
[Posted: 2/28/2012]
Crazy I keep getting these wrap around lesions…
F ig. 59
F ig. 60
F ig. 61
F ig. 62
F ig. 63
F ig. 64
Fig. 59: Another Pepsi please.
Fig. 60: This shot is for Dino…
Fig. 61: This is #7 as you can see #6 and 8 are prepped.
Fig. 62: #7 finished not trimmed.
Fig. 63: Building the contact for #8. As usual surpass, seam-free and Filtek Ultra.
Fig. 64: #6 isolated.
Out the door a happy girl!
continued on page 50
48
SEPTEMBER 2012 » dentaltown.com
$#"!
"#"$
$#"! "#"$
!" # ""#$" *)('&)%*$#)"!$ !)'%&$) #
(((*%!#*'%&!(%!*)
"""
Dental Supply, LLC
*)('&%($&#"
!$' "%($)"
%&'$'"$&%"
"""*""
""""
$
$
$$$
$
FREE FACTS, circle 25 on card
cosmetic
townie clinical
continued from page 48
[Posted: 2/29/2012]
Figs. 65-66: I did this kid’s right side a couple of weeks ago… decay on 9, 10, 11, 12,
14 and a rotted wizzy.
F ig. 65
F ig. 66
F ig. 67
F ig. 68
F ig. 69
F ig. 70
F ig. 71
F ig. 72
F ig. 73
Fig. 67: # 9 with a 9 clamp.
Fig. 68: 9 unfinished.
Fig. 69: #7 with a 212.
Fig. 71: #11 loaded with sub g decay.
Fig. 72: #11 with a 9 clamp.
Fig. 73: And #16 with its goober. ■
FEB 29 2012
newdoc7
Member Since: 09/03/06
Post: 32 of 68
Nice! Are you placing the rubber dam after you prep? Thanks. ■
FEB 29 2012
satchdds
Member Since: 04/19/02
Post: 33 of 68
FEB 29 2012
Find it online at: www.dentaltown.com
50
SEPTEMBER 2012 » dentaltown.com
search Single Tooth Isolation
▼
»
Yes, otherwise I would tear the dam. I prep with a split dam in the posterior. ■
Imagine the
esthetics of a layered restoration
3M, ESPE and Lava are trademarks of 3M or 3M Deutschland GmbH. Used under license in Canada. © 3M 2012.
All rights reserved. VITA and VITA SYSTEM 3D-MASTER are not trademarks of 3M. 1. Compared to other zirconias. 2. Data on file.
from all-zirconia.
The unique formula of Lava™ Plus High Translucency
Zirconia provides significantly higher translucency1 and
unprecedented beauty—without compromising strength.
sThe patented shading system enables highly esthetic all-zirconia or
traditionally layered restorations.
sExcellent color match to the VITA® Classical Shade Guide and
VITA SYSTEM 3D-MASTER® Shades.
sHigh strength allows tooth-preserving 0.5 mm minimum wall thickness—
requiring 3X less occlusal preparation than lithium disilicate glass ceramic
because of its 3X greater strength.2
Lava Plus zirconia is the beautifully durable material of choice.
www.3MESPE.com/LavaPlus
FREE FACTS, circle 40 on card
Receive $50 OFF
a Lava Plus restoration
at www.3MESPE.com/LavaPlus/Coupon
Lava Plus
™
High Translucency Zirconia
sleep medicine
message board
Sleep Study Standard of Care?
»
Dentaltown Message Boards > TMD & Occlusion, Sleep Apnea/Snoring and Appliance Therapy > Sleep Apnea/Snoring > Sleep Study Standard of Care
fishdrzig
Member Since: 10/25/02 Post: 1 of 24
drbglass
Member Since: 10/16/01 Post: 2 of 24
One dentist thinks treating snoring without a diagnosis is malpractice. Do you agree?
Is obtaining the results of a sleep study ordered by an MD standard of care prior to
making a snoring appliance? FEB 22 2012
The study doesn’t necessarily have to be ordered by an MD, but it is standard of care that
the diagnosis be made by a physician. FEB 22 2012
drbksmith
Member Since: 08/25/02 Post: 3 of 24
And a diagnosis of snoring (benign or primary to rule out sleep apnea) can only be made
after a sleep study. FEB 22 2012
fishdrzig Member Since: 10/25/02 Post: 4 of 24
Excuse my ignorance, but if a sleep study is not done and an anti-snore device is made,
what could be some problems that arise for the patient? I ask because I have a patient who
needs to know why and thought I would pick the Dentaltown brains on this forum. Thank
you for your time. FEB 22 2012
drbksmith Member Since: 08/25/02 Posts: 6 & 15 of 24
Actually, the follow up sleep study is the most important, as you want to make sure the
problem is corrected. Of course, you don't know what the problem is if you don’t do a study
before. Tell your patient that there is a condition called “silent apnea,” where you solve the
snoring, while apnea remains. Patients can think they are fine, when in fact, they aren't.
[Posted Feb. 22, 2012]
There are many apneics walking around who have been made silent with a Silent Nite
some dentist made without knowing what he or she was doing. They think they’re “cured”...
and maybe they are, but they might never know. The appliance, other than known side
effects, probably won’t cause any problems, but it’s the proverbial Band-Aid over a squamous
cell carcinoma. Why would you take a chance? FEB 22 2012
drbglass Member Since: 10/16/01
Post: 16 of 24
Do you think it would be treating below the standard of care to treat gingivitis with
homecare without X-rays or probing for a complete diagnosis? You could eliminate the sign
of gingival inflammation, and unwittingly allow the bone loss to continue. In this case, the
lack of diagnosis cost the patient their teeth because of the fact that periodontal disease is on
a continuum, and you only treated what you “saw.”
Obstructive disorders are on a continuum as well. If you only treat what you “see,” you
can eliminate the snoring but unwittingly allow the more significant underlying issue to
continue, which can lead to even more significant comorbidities. In this case, the patient has
the potential to lose more than a tooth.
Simply stated: Treating snoring without a diagnosis is malpractice. FEB 22 2012
continued on page 54
52
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 11 on card
sleep medicine
message board
manro1
Member Since: 11/16/07
Post: 17 of 24
continued from page 52
Barry, not arguing here, just thinking out loud: If treating snoring only is malpractice,
why is it that anyone can buy an over-the-counter snoring appliance? FEB 23 2012
drbglass Member Since: 10/16/01
Post: 19 of 24
For continued discussion on sleep
apnea, visit these message board
threads on Dentaltown.com.
NTI and Sleep Apnea
Search: Sleep Apnea
Sleep, etc.
Search: Sleep
Great question – and the one I appreciate everyone is thinking about when we teach
what is required. No need to be concerned about seeming argumentative. Not at all...
great question.
I have no idea what the FDA was thinking when it allowed those appliances to be sold;
and why in the world the sleep docs haven’t gone crazy trying to stop it. But that doesn’t take
the responsibility of diagnosis away from the health practitioner. It seems strange that
puresleep.com should be allowed to mistreat patients – I get it. But I sure don’t want to be
compared with any of them; either in the diagnostic portion or the treatment considerations
including managing occlusal changes and other untoward effects. FEB 23 2012
Find it online at: www.dentaltown.com
search Sleep Study
»
Register Now for Early Bird Pricing
www.towniemeeting.com
54
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 12 on card
bisco
corporate profile
In 1981, Dr. Byoung I. Suh (initials B.I.S forming the first
three letters of “BISCO”) had a vision for better resins.
With focused research and a dedicated team, BISCO
pioneered dental adhesion technology and many of the
dental products you rely on today can be traced back to
a humble lab in northern Illinois. Dentaltown Magazine
spoke with Dr. Suh and his team to learn more about
BISCO’s history and its future.
Respondents
President, Byoung Suh, PhD, MS, FADM
Director of Clinical Education, Douglas Brown DDS, FAGD
Executive Vice President, Paul L. Child Jr., DMD, CDT
Director of Sales and Marketing, Tom Czervionke
Director of Professional Relations, Carolyn D. Suh
Director of Business Operations, Julie Suh
Director of Research & Development, Janet L. Zuffa, PhD
56
SEPTEMBER 2012 » dentaltown.com
by Benjamin Lund, Editor, Dentaltown Magazine
If you were to bump into a dentist on the street who didn’t
know about BISCO, how would you describe your company
to him or her?
Child: BISCO is an international dental restorative company that
produces well-known products such as the All-Bond family of adhesives, Duo-Link resin cement, Z-Prime Plus and TheraCal LC. We specialize in making high-quality products that are chemical-based and
required for successful adhesion to teeth and other dental substrates.
BISCO is expanding into all areas of dentistry that are restorative-based
and where we can provide products that are both innovative and better.
bisco
corporate profile
period of time, assuring that materials are always fresh and will
function at peak performance. Furthermore, BISCO is a direct
selling company which allows the pricing of our products to be
very competitive, thereby providing our customers the very
best value for their purchases.
Who would you say is your typical customer?
Tell us about how BISCO got its start? Tell us a little
about your evolution. Why did Dr. Byoung Suh
choose dentistry?
Carolyn D. Suh: During the 1970s, Dr. Suh had been
working in the dental industry, synthesizing his own BisGMA
resin and developing Adaptic-like, self-cured composites. In
1981, he decided to start his own dental company because he
felt that dentistry needed new dental adhesives that would bond
to dentin and to metal, and had some chemistry-based solutions
in mind. By 1990, BISCO introduced All-Bond, followed by
the improved version, All-Bond 2, in 1991, which revolutionized adhesive dentistry into what it is today.
To what do you attribute BISCO’s successful penetration in dentistry?
Carolyn D. Suh: BISCO’s success has always been attributed to Dr. Suh’s understanding of chemistry, and his dedication
to research and knowledge of adhesion dentistry. His commitment to teaching and sharing information with dentists and
other lecturers, as well as his dedication to the highest standards
for quality products, has helped BISCO achieve its success over
the last 30 years.
How does BISCO set itself apart from its competition?
Czervionke: Categorically, there are many similarities among
products currently marketed in dentistry. BISCO takes great
pride in developing products that not only provide the dentist
with the highest level of quality but also offers the
added assurance and confidence in the product
they are using. It’s commonly known that there
is a high degree of science at the core of every
BISCO product, but more importantly, there is an
even higher degree of integrity at the foundation of
each developed product. It’s not about just marketing a product, but rather marketing the best product possible to meet the needs of the dentist and
the patient.
In addition, BISCO also develops and manufactures almost all their products in the United
States. Products are virtually made-to-order, so
products are not warehoused for any extended
Czervionke: Generally speaking, there really is not a “typical”
customer per se. BISCO’s customers come from all levels of
experience, backgrounds and demographics. A common thread
among BISCO’s customers is that they have high standards for
the products they purchase and they have come to expect and
consistently receive this from BISCO products. BISCO is certainly not the largest or most visible dental company, but we have
a very strong and loyal customer base, which continues to grow.
Tell me about research and development of your
products. How does it happen from start to finish?
Zuffa: New product ideas come from many sources…
market research, customer requests, literature searches and
patents. The products we develop stem from all of these things
coupled with BISCO’s desire to keep scientific integrity at the
forefront of what we do. When we talk about the product development process, it is an iterative process... something that we
have refined over the years. Requirements change as we develop
the product, but we keep our focus on maintaining the quality
of the products that we produce.
In general, it works like this: We have an idea that needs to
be tested and we look at all the implications of the development,
even though it is very early in the process (so we look at the technical, market, economic and manufacturing implications). Once
those things have been demonstrated, we work on the development – can we make the product meet the market requirements?
Is the product safe and effective, stable under the storage conditions? After that, we work on implementation. We follow a traditional Stage-Gate model of product development, coupled
with the Design Control requirements spelled out by the FDA.
The final stages of design transfer have to do with the actual
continued on page 58
57
dentaltown.com « SEPTEMBER 2012
bisco
corporate profile
continued from page 57
product realization and manufacture of the material, packaging,
advertising, etc. When we are ready, we “launch” another great
new product to market. Of course, we analyze post-launch feedback to make sure that we have done our jobs correctly.
How can a dentist get involved in the development of
your products?
Carolyn D. Suh: Many of BISCO’s product development
ideas come from the feedback and input from our customers
and our KOLs (key opinion leaders) who use our products and
understand how BISCO can help improve clinical dentistry by
utilizing our strong research and chemistry-based knowledge.
We also have implemented a group called the BISCO Institute
for Education & Innovation, a focus group formed of local dentists who meet at BISCO to discuss and evaluate new ideas and
innovations to help improve everyday dentistry.
How is BISCO branding itself today? What are you
implementing to ensure your brand is the most
pervasive in the dental profession, nationally and
internationally?
Child: BISCO is branding itself as the premier dental
restorative company to go to regarding innovation, integrity and
unquestionable products at competitive prices. We take pride in
knowing our customers trust us 100 percent with their patients’
best care in mind. We are expanding this message of trust and
loyalty to new customers every day through education and direct
contact. BISCO will continue to grow and become a major
source for all dentists worldwide for their needs.
What’s BISCO’s current business philosophy?
Julie Suh: BISCO’s business philosophy is best reflected in
our key core value – integrity. Highest standards for our products, science-based product innovation, respect for others and
promoting knowledge to benefit the industry are all aspects of
integrity for BISCO. These values reflect the ethics of a true scientist, our founder, Dr. Suh. It is with these values that Dr. Suh
has led BISCO for the last 30 plus years. Our business is not
driven by numbers, it is driven by the desire to promote excellence and continual progress in dentistry for the benefit of our
customers through products developed and activities conducted
with integrity.
Tell me about your team. What’s the culture like
at BISCO?
Julie Suh: Our employees are all part of the BISCO family.
About one-third of our employees have been with the company
for more than 15 years. We celebrate birthdays, anniversaries,
weddings and births, and provide support to each other in times
of need. While we maintain a professional atmosphere and
strong business processes at BISCO, there is no corporate
bureaucracy or formality to hinder our business operations. Our
decision-making is usually by consensus, with just enough controversy to keep our decisions sharp. With almost everyone
working in one location, working relationships are direct and
personal, and communication is easy and quick.
Tell me about your management team. What experience do all of you have under your belts?
Julie Suh: Our management team consists of eight directors
that report to our President Dr. Byoung Suh, or our Executive
Vice President Dr. Paul Child, along with our Vice President of
Finance and Administration Minsook Suh. The BISCO management team has experience working in small, medium and
large companies (Fortune 500); public and private companies; a
variety of industries; and of course, our clinicians have clinical
experience. Our sales and marketing managers and directors
have had significant experience in the dental industry before
coming to BISCO, including companies such as GC America,
Lifecore and Clinician’s Report. Our scientific directors have
had relevant experience in medical device or polymer chemical
companies. It is this diversity of experience in related industries
that has allowed our management team to bring a variety of best
practices to BISCO operations.
What can a practice expect when it purchases a
product from BISCO?
Czervionke: Consistency of product, high quality and outstanding value – these would be the three main deliverables when
purchasing a BISCO product. In addition, BISCO makes every
effort to provide the highest level of customer care and service.
BISCO’s technical staff is extremely well-trained in product
knowledge and is able to assist a dental practice with a wide variety of product or procedural questions. BISCO consistently
receives high marks in the ability to service our customer’s needs.
How do you work with clinicians to ensure they are
using your products in the best way possible?
Czervionke: Utilizing the resources and expertise of clinicians and industry leaders is essential in the development and
continued on page 60
58
SEPTEMBER 2012 » dentaltown.com
BISCO’s new SELECT HV ETCH is a 35% high viscosity phosphoric acid etchant containing Benzalkonium
Chloride (BAC), designed for the “selective etch” or “hybrid” technique – etching enamel margins without
etching dentin. It can also be used for everyday total-etch restorative procedures. SELECT HV ETCH is
formulated for optimized handling and accurate pin-point placement performance.
• High Viscosity, ideal for enamel etching
20%
OFF
Like us on:
Dentistry courtesy of
Dr. Michael Morgan.
Rx Only
MC-10121SE
YOUR FIRST
PURCHASE
of a SELECT HV ETCH
Bulk Syringe Kit or
a 4-5g Syringe Package.
• Available in a convenient bulk syringe
with refillable syringes
• Contains Benzalkonium Chloride (BAC),
an antimicrobial agent
800.247.3368
www.bisco.com
Offer expires 10/15/2012. Promo code 12A09.
U.S. customers only. Discounts cannot be
combined with any other offer.
FREE FACTS, circle 6 on card
bisco
corporate profile
continued from page 58
implementation of dental products. BISCO makes every effort
to work with clinicians at all stages of product development,
from concept to post-market surveillance, to achieve the desired
success and to provide the best possible materials to meet the
demand of the clinician.
What is the protocol if a dentist is experiencing any
difficulty with one of your products? Are there people on staff who can speak the doctor’s language?
Brown: BISCO sales professionals take pride in their accumulated knowledge. This knowledge is a valuable asset to our
dentist/dental-auxillary customer. Our sales professionals are
trained on solution-based delivery of this knowledge. You have
challenges; we have solutions! Expect prompt, pragmatic and
professionally delivered solutions to clinical challenges.
Customer service professionals will immediately ask specific
diagnostic questions and have dentists immediately available
when needed to serve as clinical resources such as the Director
of Clinical Education, Director of Research and Development,
and always, Dr. Byoung Suh, BISCO’s founder.
How does BISCO keep in touch with its customers?
Czervionke: Unlike many of our competitors, BISCO
being a direct selling organization allows us the distinct advantage of providing regular and personal contact with our customers in a variety of ways. In addition to strong telemarketing
capabilities, BISCO maintains a strong presence in attending
tradeshows, seminars and workshops. BISCO also routinely
communicates with customers via newsletters, direct mail programs, and electronic and social media, in an effort to keep our
customers current on new products, promotional opportunities
and clinical information as well. BISCO is currently in the
process of completing a new upscale Web site, which will pro-
“BISCO products
allow the clinician
and auxillary to
standardize
clinical protocols
for effective
delivery of
adhesion over
and over again.”
vide customers with easy access to a variety of informative and
useful product, technique and procedural data.
What is an interesting story about a customer interaction you had?
Dr. Byoung Suh: At the Greater New York meeting five
or six years ago, Adrian Jurim, a ceramist and master dental
technician, approached me and requested that I develop a zirconia primer due to a recent experience he had. He relayed a
story of a patient who’d had full-mouth reconstruction, all
with zirconia as the substrate. A few weeks after final cementation, both maxillary canines became dislodged, and the
patient swallowed them! Due to this request and story, we
developed and launched a zirconia primer, Z-Prime Plus,
which bonds chemically to zirconia.
In your opinion, how does incorporating BISCO products impact a doctor’s overall practice?
Brown: Incorporating BISCO products will make one a better dentist. BISCO chemistry is proven, reliable and simple.
BISCO products allow the clinician and auxillary to standardize
clinical protocols for effective delivery of adhesion over and over
again. BISCO’s universally compatible adhesives and cements
provide significant cost savings for the office and guaranteed
clinical effectiveness!
Think about the company’s most significant accomplishment. Can you tell us all about it?
Dr. Byoung Suh: BISCO’s most significant accomplishment is not one of commercial or financial success, but that
we have stayed true to my philosophy of business that has
always been to put research, science and integrity first. By
staying true to this business philosophy, BISCO is regarded
worldwide as a company of integrity and the products
are accepted as truly science-based materials by practitioners around the world.
What are you most excited about in the upcoming year?
Dr. Byoung Suh: I am excited about BISCO’s possible expansion into the regenerative line of products,
designed specifically to lay the foundation for rebuilding
tooth structure. This follows the successful launch of
TheraCal LC, the first light-cured calcium silicate product to help remineralize tooth structure by stimulating
hydroxyapatite growth. In addition, I am also excited to
see BISCO products reach more dentists worldwide so
that we can share the benefits of our science-based products with more patients.
If you would like more information about BISCO,
visit www.bisco.com or call 800-247-3368. 60
SEPTEMBER 2012 » dentaltown.com
new product
profiles
CEREC Omnicam
Sirona Dental Systems introduces the new CEREC Omnicam. Its revolutionary design
features a new, ergonomic handpiece and special optics to guarantee unsurpassed intraoral access. New ColorStreaming allows continuous capture of the oral cavity as well
as displaying the 3D data in full color – an industry first. The system is completely
powder-free while still retaining Sirona’s high standards for precision. Additionally, the
Omnicam records 2D and 3D data; captures half-arch and full-arch impressions
quickly; and automatically eliminates substandard images. For more
information or to schedule a free demonstration,
visit www.cereconline.com.
SR Phonares II
Ivoclar Vivadent recently launched the SR
Phonares II, the next generation of ultra-premium composite denture teeth. As the newest
addition to Ivoclar Vivadent Removable, SR
Phonares II have an optimized shape, shade and
strength. The existing range of 22 anterior tooth
moulds has been extended to include two new
mandibular anterior moulds, L54 and L55, and
the shades of the Phonares teeth have been precision matched to the A-D shade guide and
include all 16 A-D and four innovative bleach
shades. For more information, call 1-800-5336825 or e-mail mail@ivoclarvivadent.com.
New Products
www.dentaltown.com
Newly Designed Task-Vision
LED Reading Glasses
Task-Vision LED Reading Glasses have a
freshly designed EZ slide cover for changing the batteries. This means no more
screws or hard-to-open covers, the ability
to change the batteries in seconds and
greater ease for people with arthritic fingers. Contemporary black frame, aspheric
lenses (distortion free) and lithium batteries are included. For more information on
the LED Reading Glasses that provide 50
hours of continuous use, call 800-2575782 or visit www.visionusasupplies.com.
62
SEPTEMBER 2012 » dentaltown.com
▼
If you would like to submit a new product for consideration to appear in this section, please
send your press releases to Assistant Editor Krista Houstoun at krista@farranmedia.com.
DCB Abrasives
Offering outstanding effectiveness on extremely hard materials, KOMET DCB (diamonds with
ceramic bond) abrasives feature a ceramic bond interspersed with a high content of diamond
grit. The grinding instruments are suitable for work on all types of ceramics, including zirconium oxide and aluminum oxide, as well as on hard dental alloys, achieving fine surfaces without applying pressure.
The abrasive line now includes a small-diameter (4.8mm), 13mm-long cylinder-shape grinder,
the DCB 2, in addition to the 6.5mm-in-diameter, 13mm-long cylinder-shape version, DCB 2 C.
The array of DCB instruments also includes the DCB 1 flame-shape abrasive, the DCB 3 and
3C tapered-cylinder grinders, the DCB 4 and 4C flat-edge (12mm in diameter), the DCB 5
knife-edge (22mm in diameter) disc configurations, and the DCB six cup-shaped abrasive.
For more information about Komet’s DCB
abrasives, please call 888-566-3887 or
visit www.komet-usa.com.
new product
profiles
Estelite Sigma Quick
Aptly called the “Miracle Match” composite, just one
shade of Estelite Sigma Quick invisibly blends into its surroundings with up to 10 shades, eliminating the need to
stock excess inventory and reducing surplus costs. Ideal for
both anterior and posterior restorations, this chameleonlike composite handles as beautifully as it looks. For more
information, visit www.themiraclematch.com.
Flexipalette
Flexipalette is an assortment of three photographic contrastors created to enhance digital photography for aesthetic cases. Flexipalette is patient-friendly as it is made
out of a bendable copper sheet 100 percent overmoulded
with Plastimed – a medical-grade plastic rubber that’s
latex free, safe and hypoallergenic. For more information
call 877-755-6868 or visit www.smilelineusa.com.
FREE FACTS, circle 51 on card
63
dentaltown.com « SEPTEMBER 2012
selling dentistry
feature
T
op professionals in nearly every field of selling understand the value of good clients
above and beyond the direct business they get from them. Each client’s business not
only adds to your personal bottom line, but it can lead to even more business through
referrals. The same goes for dental practices. Every satisfied patient can be the source of
many more patients whose business generates additional revenues for your practice.
The key is to understand how to leverage the satisfaction of your current patients for
its maximum value. It’s a very simple, yet critical aspect of business and something that
deserves dedicated effort by you and every member of your staff. In fact, it’s a good idea
to remind everyone on your staff, both verbally and visually, that they should constantly
be seeking opportunities to generate the contact information for potential new patients.
Some dental practices do this so naturally that you would have to pay careful attention to determine exactly the steps they are implementing to grow their practices through
their patients. Let me suggest a couple of things you can easily do to get started on a program of growth that’s rooted in your existing, satisfied patients.
First, ask the existing patients what they would tell others about their
experience with your practice. Either you or your staff member should
make a quick note of that (or even have the patient jot down their
thoughts on a piece of your stationery, sign and date it). Then, post
it on a bulletin board in your waiting room. It’s critical that the
patient understands they’re giving you permission to display their
endorsement. Truly satisfied patients will be happy to do this.
continued on page 66
by Tom Hopkins
64
SEPTEMBER 2012 » dentaltown.com
into a
We turned that
The beautifully translucent
Z Crown™ Solid
Full Contour Zirconia
Call ttoday
C
oday and get y
your
firstt Z Cr
Crown™
our firs
own™
$99,, rregularly
value!
S
Solid
ffor
or only $99
egularly a $125 v
alue!
877-954-6243
8
77-954-6243
WWW.BAYSHOREDENTALSTUDIO.COM | customerservice@bayshoredentalstudio.com
FREE FACTS, circle 13 on card
selling dentistry
feature
continued from page 64
Some will even embellish their messages with small illustrations, if they’re artistically
inclined. Keep a cup of colorful markers or stickers of gold stars and such handy for them
to use for this purpose. This is way more beneficial to your practice than crayons and paper
in the lobby. The more fun you can make it for them, the more likely they’ll do it.
Once you have 15, 20 or more of these endorsements, put them into binders and place
them throughout your office. Once patients become familiar with this process, they’ll look
forward to seeing what others have said (or drawn) and tell friends and
relatives to look for their endorsements when they come in for treatment. It becomes a point
of interest in coming to your office and something they’ll talk about with others in the daily
course of their lives. And, the more they talk about you, the further the word of your excellent service spreads throughout the community.
Consider taking pictures of just the smiles on patients’ faces to add to their endorsements.
Maybe call your booklet “The Book of Smiles,” so patients will know how to refer to it. The
mental image you’re creating is of happy people with healthy teeth. Isn’t that exactly what you
want to have pop into their minds when they think of you?
With the ease of use of technology today, you could even
“You should be so proud of the level have your staff capture a quick video of some patients talking
about how great your service is. You would then show this
of service you provide that you are never video on a screen in your waiting room or while patients are
hanging out, relaxing in the operatory.
hesitant to ask patients to tell their friends,
Another way of letting your patients brag for you is to
loved ones and associates about it.” use our “Higher Authority Close” and have your patient,
especially if they’re a prominent person in the area, actually
talk with other prospective patients for you. To do this, you
would need to have a satisfied patient agree to make a call on your behalf. Perhaps they have
mentioned knowing someone with a particularly large extended family in the community
or being active in a social group in the area. Ask them to mention their positive experience
with your practice and suggest the others consider going there as well.
People who are active in the community are used to networking for themselves. When
they find a good resource, they’re usually eager to share it with others in their network.
Always be considerate of higher authorities’ time and don’t ask them to make calls for you
frequently – just ask when they have influence over a key group of potential new patients.
You should be so proud of the level of service you provide that you are never hesitant to
ask patients to tell their friends, loved ones and associates about it. You might even say,
“Since you’re so happy with how well we’ve served your needs (or your family’s needs), you
wouldn’t mind telling a few friends or relatives about it, would you?” When it’s stated that
way, most people will not mind agreeing to do it. The trick is in getting them to follow
through because within 15 seconds of leaving your office most people will have at least five
other things on their minds.
So, what do you do to increase the odds that they’ll tell others about you? You could give
them a to-do list-type of note pad or sticky note pad that shows right on it in the first position – “Tell the next person I talk with about how great Dr. So-and-So is.” Always include
your phone number. Add the Web site if they can sign up as new patients online. And, include
your photo on the note pad as another trigger to remind your happy clients to do this.
Some businesses I know of will give out three, five or even more items like this and
have a staff member follow up with the patients within the week to find out who they
gave them to. They would then ask for a mailing address to send a brochure, coupon or
additional information about your practice. Repeat mailings would be sent at least six
times in a year in order to become a familiar face to those people. It takes a minimum of
six contacts with people who are not already clients for them to start to remember your
name or face and make the connection to your type of service.
continued on page 68
66
SEPTEMBER 2012 » dentaltown.com
CS
CS 7600
7600
The
T
he w
world’s 1st intelligent plate imaging system
Coming
Coming together
together tto
o iimprove
mprove yyour
our w
workflow
orkflow
Finally al
he p
ieces ffit
it iinto
nto p
lace. SSetting
etting a n
ew standard
standard in
in d
ental
Finally
alll tthe
pieces
place.
new
dental
iimaging,
maging, tthe
he iintelligent
ntelligent C
S7
60 0 g
o es b
eyond tthe
he essentials
essentials o
op
CS
7600
goes
beyond
off ttop
p
er formance, speed
speed and
and image
image quality.
quality. Using
Using exclusive
exclusive SScan
can & G
o
performance,
Go
technology*, the
the system
system automates
automates tasks
tasks and
and eliminates
eliminates tthe
he rrisk
isk
technology*
o eenhance
nhance p
roductivity an
d eefficiency.
fficienc y.
of p
late mi
x-ups tto
of
plate
mix-ups
productivity
and
d ssecured
ecured w
orkflow
t Truly
Truly aautomated
utomated an
and
workflow
n aass llittle
ittle aass 5 sseconds
econds
Outstanding iimages
mages iin
t Outstanding
with all
all tthe
he benefits
benefits of
of digital
digital
Film-like w
orkflow with
t Film-like
workflow
can be
be used
used cchairside
hairside o
n a ccentral
entral llocation
ocation
Compact design
design that
that can
t Compact
orr iin
*Available
*Available as
as an
an o
option
pt i o n
Learn
Learn more
more at
at www.carestreamdental.com/cs7600dt12
w w w.carestreamdental.com/cs760 0dt12
© Carestream
Carestream Health,
Health, Inc.
Inc. 2012.
2012.
7873
7873 DE
DE 76
76 AD
AD 0812
0 812
FREE FACTS, circle 24 on card
FEATURING
NEW SC AN
& GO
TECHNOLOG
Y
selling dentistry
feature
continued from page 66
I used to do this in my real estate career. I found it interesting how many people would
eventually come to me to buy or sell a home and tell me that they recognized me. That sense
of familiarity made them feel comfortable calling me when they had a need even though they
had never met me.
Another idea to gain new patients is to include your business card and a
satisfied
patient endorsement in every piece of mail you send out. This
“When you have a patient who
includes your water bill, your electric bill and so on. Again, I received
calls from people at the water department office because they had
expresses that fear, yet continues to
seen my information repeatedly. In fact, one woman gave my busicome to you, you know you’re
ness card to a relative who was thinking about moving into the area.
Neither person knew a good real estate agent, but the clerk at the
providing them not only great dental
water department happened to have my card in her desk.
The simplest method for using a satisfied client’s name is to
services but a great experience.”
have him or her write you a letter about how happy he or she is
with the decision to come to you for dental services. Once you’ve
gotten his or her issues resolved, you have earned the right to ask for a more formal testimonial letter. All you have to do is say these words: “Mr. or Ms. Client, I’m so pleased that
you are enjoying the benefits of our services. And I so appreciate the opportunity I have of
serving your needs.” (By the way, if they aren’t perfectly satisfied with both the results and
your level of service, don’t waste your time on this.) “Since you’re so happy, you wouldn’t
mind dashing off a short letter about our experience together that I might show to another
prospective patient, would you?”
See how nice that is? And if you’ve done your job properly, he or she will be happy
to approve it for your usage with those other potential patients. It’s painless for them and
priceless for you.
As you know, some people have a tremendous amount of fear about going to the dentist.
When you have a patient who expresses that fear, yet continues to come to you, you know
you’re providing them not only great dental services but a great experience. Don’t be afraid to
ask them to write up or record something about that particular benefit of your service. Don’t
just listen for generalized statements of satisfaction from your patients. Pay attention to pain
points – fears, bad past experiences, and so on. Once you have served them well and satisfied
their needs, encourage them to help others with similar fears to overcome them and gain the
benefit of good dental health. As nice as it would be to have a small army of happy patients
saying, “Dr. So-and-So is great,” the more specific they can be about what makes you great,
the more likely you are to get new patients. Someone who hears their message about “I used
to be afraid of going to the dentist, but …” or “I had no pain or discomfort at all” their ears
will perk up and they’ll pay attention. They’ll want to know of this wonderful place of painfree dentistry, someone having a relaxing and enjoyable visit to the dentist and so on.
Work on the ways you can encourage clients to do the bragging for you and you’ll soon
find yourself generating more revenue, but doing so with more ease than ever before. ■
Author’s Bio
Tom Hopkins is a world-renowned expert and authority on selling and salesmanship. His simple yet powerful strategies have been proven effective
in many industries, including the dental industry, and during all types of economic cycles. The foundation of his training includes both the “people
skills” of proper communication and the nuances that impact every situation where trying to persuade others. Tom’s style of delivery is practical and
entertaining – making the strategies easy to remember and implement. Learn more about how Tom Hopkins can help you increase revenues in your practice at
www.tomhopkins.com/blog. To reach Tom, please e-mail him at tomhopkins@tomhopkins.com
Details about Tom’s speaking schedule can be found at: www.tomhopkins.com/live_events.shtml.
68
SEPTEMBER 2012 » dentaltown.com
A Better Way to Isolate
Isolite simultaneously increases
patient comfort while lowering
the stress typically associated
with the meticulous placement
of bonded restorations.
Working with Isolite,
I would say that
my average time to
complete preparation
and restoration
is cut by one third.
— Michael I. Barr, DDS
U Isolates two quadrants simultaneously
U A leap forward in comfort for patient & professional
U Unprecedented patient safety
U 30% faster procedures
U Better isolation = better dentistr y!
Take a video tour at www.isolitesystems.com
and learn how Isolite can benefit your practice.
Or call 800-560-6066 to speak with an Isolite representative.
U S E C O D E D T N 2 012
to receive special offer.
FREE FACTS, circle 54 on card
finance
feature
FINANCIAL MISTAKES TOs AVOIDs
in Your
by Douglas Carlsen, DDS
I provided “Obstacles to Savings” in my April Dentaltown
article. This month, I’d like to hone-in further on the mistakes both young and nearing-retirement dentists make.
Video supplements on this month’s topic are available.
Go to YouTube and search “Doug Carlsen Channel.”
Alternatively, on the Dentaltown Web site, on the right hand
column click on “Message Boards,” then “Finance,” then
“Personal Finance.”
The Thirties
Spending Without a Budget
The newly minted dentist, after years of no income suddenly has compensation that is much higher than the
national average. It’s high time to celebrate! Family responsibilities are normally few. Extracurricular spending could
involve dining out, entertainment, clothing, travel, new
sports equipment, and of course, that new BMW. The dark
side of this new financial independence involves taxes, credit
cards, auto loans and student loans.
Here’s a quick way to broadly budget without spreadsheets or entering transactions into Quicken or Mint. Figures
used below are approximate for the young dentist.
For the single employed dentist list the following:
• Monthly take-home pay
30 50
&
• Subtract out your monthly rent; auto loan payment; student loan payment; medical insurance
payment; an additional $350 for auto insurance,
repairs and fuel; $250 per month for groceries; and
$500 per month for utilities including cell phone,
cable and Internet.
For the single dentist who has purchased a practice, use
the same numbers as above with the following changes:
- Instead of take-home pay, use 65 percent of your
net income (all taxes will average about 35 percent).
- Include your practice loan payment minus the
interest to your expenses.
For married dentists, use the above figures, yet double
amounts for auto and groceries.
What’s left over is your “play money.” Be sure to know
what this amount is. It’s most often between $500 and $2,000
per month. This money is for clothing, hobbies, sports, dining out, sporting events, concerts, gifts and vacations. If you
have a firm mental idea of your total monthly “play money,”
it will be much easier to not overspend.
Paying Bills Late
Habitually paying bills or credit cards late can severely
sabotage one’s retirement savings. Maintaining a balance
continued on page 72
70
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 2 on card
finance
feature
continued from page 70
of $25,000 with 18 percent interest on credit cards, which
is not unusual for a dentist, denies the dentist $465,000 in
lost investment potential over a 30-year career. Second,
late payments leave a negative mark on your credit score,
which translates to higher costs for office, equipment and
home purchase.
Third, you lose the goodwill of dental suppliers, labs,
attorneys, tax and financial planners, and usually your staff.
Worst of all, you lose confidence in yourself.
Money Secrets
For married dentists, secret accounts and not being open
about debt and purchases is a huge no-no and often ends in
divorce. Well before marriage, put everything on the table.
The biggest risk to your financial wellbeing is divorce. I tell
clients to add six years to their working career for each
divorce, and that’s conservative.
Emergency Fund in Place
A mistake many dentists make is not having an emergency fund in place before any other savings. Emergencies
happen when least expected. A single bike or ski accident
or other disability can cause years of financial turmoil.
Disability insurance normally covers only about half of your
net income and doesn’t begin for 90 days. Those 90 days
can cut your income to zero or less for the entire year,
requiring three to five years to pay off the debt accumulated. An emergency fund of $40,000+ for a dental family
is essential.
Maintaining a High Debt-to-income Ratio
A prudent rule of thumb is Brian Hufford’s 25 percent
rule regarding total debt.1 That is, one should not have
more than 25 percent of family net income in personal
and practice loan payments. If a young doctor earning
$200,000 per year has student debt of $250,000 at six percent interest with payments of $2,900 per month, that’s
$35,000 per year and 17.5 percent of the family’s income.
With two car loans totaling $1,000 per month, or
$12,000 per year, we creep up to $47,000 per year in debt
payment. That’s 23.5 percent. Sorry, a home mortgage is
out of reach.
continued on page 74
1.
Brian C. Hufford, CPA, CFP, “Maximize Your Wealth: Improving Upon the Reality of Your Finances,” AGD
Impact, February 2010.
You’d never give your customers
the same solution. Neither would we.
Our Practice Finance Specialists will prescribe solutions that fit your practice, helping you with
acquisition financing or practice debt refinancing. In addition, we can help with buy-ins or
buyouts, expansions, relocations or new practice start-ups.
branch
usbank.com/PRACTICEFINANCE
Subject to normal credit approval. Some restrictions may apply. Deposit products offered by U.S. Bank National Association. Member FDIC. © 2012 U.S. Bank MMWR19030
FREE FACTS, circle 9 on card
72
SEPTEMBER 2012 » dentaltown.com
HIGHEST RATED
FASTEST SELLING
IT SPEAKS FOR ITSELF!
R
R
R
R
TOP
An independent non-profit dental education and product testing foundation gave Stylus ATC
“Excellence” and “Choice” ratings.
Midwest® Stylus™ ATC. Thousands of dental professionals have switched
to it, making it the fastest selling handpiece in the nation.* Numerous
industry recognized editorials have said it’s the best handpiece available.
$#"! !!"!!"!!!"!"
$!"!!!""!" !!"!!
!!!$
* SDM Data
FREE FACTS, circle 28 on card
MADE IN AMERICA
finance
feature
continued from page 72
High student loan debt makes it imperative in most
instances for the young dentist not to purchase a home
until after the practice purchase and only when student
loans are either paid off completely or at a very low payment. There is enough stress on doctors in the first several
years of owning a practice. To have monthly totals of
$3,000 for student loans, a $3,000 mortgage, a practice
loan of $6,000 and auto loans of $1,000, all totaling
$13,000 per month, makes me sweat just writing!
Please heed my warning: To establish a lifestyle of
revolving auto, home, practice and credit card debt severely
debilitates one’s ability to grow wealth. Doctors in their late
40s still paying student loans with revolving credit card debt
have a very long road ahead to financial freedom.
The Fifties
one can do in one’s 50s to leverage debt for increased retirement savings. Practice loans, second homes and new mortgages on the primary residence severely hamper savings.
Cash is king in one’s 50s. A 55-year-old dentist recently
asked when he can finally buy that Porsche he’s dreamed of
for years. The answer: anytime, as long as he pays in cash.
Beating the Market
Taking risk to “catch up” with a portfolio that’s suffered
over the years is poor strategy. Holding only individual
stocks, commodities or putting all your eggs into real estate
is not the answer.
Make sure to buy the whole market, not just what you
feel might be the “hot” areas. Work with a financial planner
or a discount broker that practices within the American Law
Institute’s Prudent Investor Rule. In part it states:
Divorce
I list divorce as a mistake, yet there is often no mistake.
It’s tough to place fault and it is devastating mentally.
Financially, it’s the worst disaster a dentist can face other
than permanent disability without insurance. For all professionals, divorce is common.
Fortunately or not, those who stay married tend to have
more wealth. According to Thomas Stanley, PhD, author
of The Millionaire Next Door series, “Among the 944 millionaires surveyed nationwide for Stop Acting Rich, 91 percent were married to the same spouse on average for 36
years. Fully two-thirds have never been divorced.2
30-year Fixed Mortgage
Taking out a 30-year fixed loan as you approach retirement will normally increase your retirement income need
substantially. Without a mortgage, most dentists require in
the neighborhood of $150,000 per year pre-tax income.
Add in a mortgage and the income level increases anywhere from $30,000 to $60,000. In real retirement dollars, that’s $600,000 to well over $1,000,000 in additional
funds. In years, it’s three to five more years of work. The
reason for the new mortgage is often other debt.
Debt
The dentist’s 50s is the time of life when income and
potential savings are maximized. Normally the home is
either paid off or nearly paid off, college fees are under
control or gone, the practice is stable, and the dentist can
save significantly more than any other life decade.
Please don’t fall prey to your ability to access more
credit. Lenders love older practicing dentists. There’s little
2.
From Stanley’s blog downloaded at http://www.thomasjstanley.com/blog-articles/417/Dont_
Criticize_the_1%3B_Emulate_Them.html on June 25, 2012.
74
SEPTEMBER 2012 » dentaltown.com
Fiduciaries and other investors are confronted with potent
evidence that the application of expertise, investigation,
and diligence in efforts to “beat the market” ordinarily
promises little or no payoff, or even a negative payoff after
taking account of research and transaction costs.3
How best to invest now? From CBS MoneyWatch
bloggers Allan Roth and Larry Swedroe: “Decide on an
asset allocation between stocks and bonds that’s appropriate for you, ignore the scary headlines, and stick to your
strategies during the tough times. Find some way to overcome your fear when the market goes down. After all,
you're not just investing for the next year or two – you’re
investing for the next 20 to 30 years.”4 ■
3.
4.
Larry Swedroe, The Only Guide to Winning Investment Strategy You’ll Ever Need, 2005,
Truman Talley Books, New York, NY, page 50.
Downloaded from http://www.cbsnews.com/8301-505146_162-39945431/5-biggest-retirement-planning-mistakes/ on June 25,2012.
Author’s Bio
Dr. Douglas Carlsen has delivered independent
financial education to dentists since retiring from his
practice in 2004 at age 53.
For Dentists’ Financial Newsletter, visit www.golichcarlsen.com
and find the “newsletter” button at the bottom of the home page.
Additional Carlsen Dentaltown articles are at:
www.towniecentral.com. Search “Carlsen.”
Videos available at:
www.youtube.com/user/DrDougCarlsen.
Contact Dr. Carlsen at drcarlsen@gmail.com or 760-535-1621.
product
profile
Zest Anchors
Zest Locator Overdenture Attachments
For 40 years Zest Anchors has been in the design and manufacturing of overdenture attachments. Zest pioneered self-aligning attachments to combat the
damage done by the improper seating of overdentures.
Zest’s Locator Attachment is designed with the primary benefits of ease of
insertion and removal, customizable levels of retention, low vertical profile and
exceptional durability. Its most critical design feature is its innovative ability to
pivot, which increases the Locator’s resiliency and tolerance for the high mastication forces an attachment must withstand and allows it to compensate for the path
of insertion even with up to 40 degrees of divergence between implants.
During seating, while the Locator male pivots inside the denture cap, the system’s
self-aligning design centers the male on the attachment before engagement. These two
actions in concert allow the Locator to self-align into place, enabling patients to easily seat their
overdenture without the need for accurate alignment and without causing damage to the attachment components. This self-aligning feature also increases the durability of the Locator
Attachment. Once seated, the male remains in static contact with the attachment while the denture cap, which is processed into the overdenture, has a full range of rotational movement over
the male for a genuine resilient connection of the prosthesis without any loss of retention.
The Locator System offers both Locator males and extended range males, which provide
clinicians with a variety of retention level options to suit their patients’ needs and enables clinicians to accommodate various paths of insertion depending on implant positions. Locator
males allow for insertion of the overdenture with up to 20 degrees of divergence between
implants and are available with one and a half, three or five pounds of retention forces.
Extended range males allow for insertion of the overdenture with up to an extensive 40
degrees of divergence between implants and are available with zero, one, two or four pounds
of retention forces.
With the Locator Attachment’s unique design, the overall restorative height of the overdenture is significantly reduced on all brands of endosseous implants. With a total attachment height
of only 3.17mm (male plus 1mm cuff height) for an externally hexed implant, the Locator saves
a minimum of 1.68mm of interocclusal space compared to other overdenture attachments. The
Locator Attachment also has twice the amount of retention surface area compared to other overdenture attachments available. Its unique dual-retention feature, which includes inside and outside retention, ensures long lasting performance and predictable durability.
Zest offers three Locator Attachments for the various types of overdenture treatments.
The Locator Implant Attachment is the premier attachment for implant-retained, tissuesupported overdentures and is available for virtually every implant system. When a treatment
plan calls for an overdenture bar, the Locator Bar Attachment provides the same self-aligning
feature, superb retention, a low-profile design and long-lasting durability. It is also offered in
three options for the fabrication of a resilient attachment on an implant-supported cast alloy
or milled titanium bar. The Locator Root Attachment is a supra-radicular design with a
choice of a straight post and 10- or 20-degree angled posts to accommodate divergent roots.
A special cast-to version is also available.
Locator has become the overdenture attachment that is embraced by clinicians worldwide.
It is currently available for more than 350 different implants produced by more than 70 manufacturers, meaning that almost any implant platform has a compatible Locator Attachment
to fit. Now, patients all over the world are enjoying a better quality of life, without the worry
of ill-fitting dentures.
For more information, call 800-262-2310 or visit www.zestanchors.com. Locator Implant Attachment
Locator Bar Attachment
Locator Root Attachment
75
dentaltown.com « SEPTEMBER 2012
practice management
feature
by Joe Steven Jr., DDS
T
here have been volumes written about increasing dental office production,
and many dental speakers talk about that all the time. We’ve read or heard
about doing quadrant dentistry instead of one tooth at a time numerous
times. There’s no lack of information out there about improving case acceptance via better communication skills. And of course, I always recommend offering more
services to our patients, which increases our busyness level and production.
For one reason or another, many dentists cannot or refuse to offer more services, yet
they are still intent on increasing their daily production numbers. There is another way,
which is actually quite simple for any dentist to do – more same day dentistry (SDD).
I recall a seminar I attended years ago where the speaker was advocating setting daily
production target goals, which is always a good idea. But, he went a little too far I
believe. He said at the end of a regular work day, the appointment secretary had to print
out a schedule for the next day with the production numbers next to each patient’s
name. If those numbers didn’t total up to their targeted goal, her work day was not over.
She had to stay and rework the schedule by calling other patients and working them in
or moving patients around if need be so that the numbers would total their goal. Boy,
does that sound like a fun job!
76
SEPTEMBER 2012 » dentaltown.com
practice management
feature
I address that issue all the time at my seminars and regard that advice as
being very misguided because we all know that at 8:15 the next morning,
much of that schedule can change with unforeseen cancellations or rescheduling needs for various reasons. So, what would be the point of staying late
the night before to put together the “ideal” schedule?
Taking care of the appointment schedule is the most difficult duty in any
dental office, and we doctors really have no idea how difficult it is. I’ve had
assistants help out up front when needed if we were short-handed up there,
and they often come back and say that they could never do that job. It does
take a very special individual who can balance many spinning plates at the
same time. You have to know the patients and have a feel of how responsible
individual patients are concerning their appointments. You have to understand dental procedures and know the time factors associated with them. You
also need to know and calculate the doctor’s capabilities of handling a busy
schedule. Some doctors don’t want a busy schedule, and that’s okay, but don’t
complain when your numbers are not up where you would like them to be.
I’ve heard from many offices that the doctor will not interrupt a regularly
scheduled patient’s appointment time by working in an emergency patient. I
understand that noble concept, but many times it is necessary and it usually
results in increased production.
So, what is SDD all about? Simply put, it means doing dentistry the same
day it is diagnosed whenever possible. If an emergency patient comes in with
a terrible toothache and you make the diagnosis of a root canal, post, buildup and crown, if at all feasible, do as much as you can that day! That work is
“icing on the cake,” adding production dollars to the daily schedule that
weren’t there before.
The same thing happens when we take a patient from the hygiene exam
room to the doctor’s treatment room after diagnosing a simple filling that
needs to be done. We have done that for years when we are aware that we
have an opening on the doctor’s side. And it’s not just the doctor being aware,
the whole team needs to be on top of that and move these patients over and
do same-day dentistry when possible. Most patients greatly appreciate that
service because they avoid taking more time off from work.
Over the years, I’ve heard countless stories from patients who complained
about how their previous dentist would only work on one tooth at a time, or
they would have multiple consultation appointments prior to being treated,
or their doctor kept referring them out for different procedures. People want
to get things done and move on. SDD can be ideal for many of our patients
and greatly appreciated while improving our profitability. Many doctors all
around the country complain about how the economy has affected the busyness in their practices, resulting in openings in their schedule throughout the
day. Many times SDD will solve that problem.
We have to address the big “elephant in the room” to really cover this
topic properly, and I’m sure many of you reading this have already wondered about this concern: How do you do this if the doctor is only working out of one or two operatories? We can’t expand our offices over night,
but with some creative flexibility, all of us can accommodate more patients
on a daily basis.
Once again, a very astute person at the front desk has the best grasp of
what is going on daily and needs to be offering guidance throughout the
day. With the use of radio headsets in our office, the ladies up front always
She said no
to her smile
makeover...
continued on page 78
77
dentaltown.com « SEPTEMBER 2012
practice management
feature
continued from page 77
suggest possibilities to the clinical staff for doing SDD. They might call
back with a message saying something like, “Mary can’t make it today, so
you have time to do that emergency root canal on Bill right now.” Or, they
might tell the assistants they can move Tom over to hygiene after their
crown seat because there’s an opening in the hygiene room. Everyone has
to be flexible and aware of what’s going on with the schedule every hour.
Another thing that I’ve capitalized on in the past, before we expanded
our office to a total of nine treatment rooms five years ago, is the old “rotating game”! For nearly 30 years, we increased our daily production by rotating patients. Some might not consider this VIP treatment, but it certainly
is for those emergency patients who we can care for on the same day.
Actually, Linda Miles, one of our great consultants is the only other speaker
I’m aware of who has recommended this same concept for increasing daily
production while taking better care of more patients.
Here’s how it works. Let’s say an emergency patient comes in with a terrible toothache. Both of the doctor’s chairs are already filled with prescheduled patients. After giving anesthetic to one of those patients I would
say to that patient, “Jim, we just had a patient come in with a terrible
toothache. It’s going to take about 10 minutes for you to get real numb.
Would you mind having a seat out front for a few minutes, and let me get
that patient out of pain right away?” After he agrees, and they always do,
then we seat the emergency patient, make the diagnosis, anesthetize, and
then rotate again. The previous patient is now ready for treatment, and we
have made the best use of our time.
I have to admit that I am not always politically correct when playing
the rotating game, and we do pick and choose which patients we feel we
can rotate. But, the majority of patients are great candidates for doing this,
and actually regard us as being very compassionate and caring for all our
patients. You will get comments such as, “I’ve been there before, so go
ahead and take care of him!” Or they’ll say something like, “That’s great to
know that if I ever come in with a toothache, that you’ll take care of me
right away also, so go ahead!” It’s a win-win for everyone.
With our expanded office we seldom ever find the need to do that anymore, but occasionally we do. If I had not played the “rotating game” over
all those years prior to our expansion, my net income would have suffered
dramatically. When we work in more procedures like that, our office overhead has already been met, so this additional production represents a much
higher profit per procedure. If you want to increase your profits immediately remember SDD for the DDS, and it works for DMDs also! ■
Author’s Bio
Dr. Joe Steven graduated from Creighton Dental School in 1978 and has been in solo practice in Wichita, Kansas, up until June, 2007 at which
time his daughter, Dr. Jasmin Rupp joined him. He is president of KISCO, a dental products marketing company, providing “new ideas for dentistry,” and is the editor of the KISCO Perspective Newsletter. Dr. Steven, along with Dr. Mark Troilo, presents the “Team Dynamics” seminar.
Dr. Steven also presents four other seminars: “Efficient-dentistry,” “Efficient-prosthetics,” “Efficient-endo” and “Doctors Only.” Dr. Steven also provides
the KISCO Select Consulting Program to dentists in the form of a monthly audio CD recording. He offers a coaching consulting program called the KISCO’s
21 Club. Contact info: jsteven@kiscodental.com; 800-325-8649; www.kiscodental.com.
78
SEPTEMBER 2012 » dentaltown.com
Then she
said
Introducing...
TM
Not every patient can afford veneers, especially in today’s economy.
Until now, there hasn’t been a more affordable solution that you can
stand behind clinically.
Duo:PCH™ changes that.
Porcelain Composite Hybrid is an entirely new esthetics category,
combining the convenience of a composite build-up with the
finishing beauty of porcelain.
Here’s how it works:
s
Customize the porcelain shells.
s
Place the composite build-up.
s
Seat the porcelain shells.
You’ll create beautiful, long-lasting and stain-resistant porcelain
finishes. Now, Duo:PCH gives more patients than ever a chance at a
beautiful new smile.
To get started, call DenMat at 888-237-7281
or visit denmat.com.
Treating more smiles. Beautifully.
Get started treating more patients
today with the comprehensive
Duo:PCH Starter Kit, including
28 porcelain shells.
©2012 DenMat Holdings, LLC.
World Rights Reserved
801314300 8/12 CO
FREE FACTS, circle 21 on card
yes!
cosmetic
feature
by Dr. Joseph Banker
Whitening is one of the most common cosmetic
procedures. Studies have shown that people with
whiter teeth look younger and there is a correlation
between high self-esteem and a bright, confident smile.
There is a debate between the benefits and risks of takehome versus in-office whitening techniques.
There are many in-office whitening systems that
were purchased with the best intentions. Like your
treadmill, many of these have found a nice spot in
the corner collecting dust. Some systems use a light
source and some do not. What they all have in common is that they are designed to achieve rapid
whitening results.
I really want to “like” in-office whitening procedures. They are easy, profitable, your staff can perform most of the procedures, and you can see
another patient at the same time (or surf the Web
depending on your level of motivation). But, it scares
me – not the whitening, but the side effects.
As a practitioner, it’s often a stressful task to use
in-office whitening systems when the risks and benefits are often unpredictable. A patient comes in for
this elective procedure, and begins by signing a consent form, taking an NSAID, applying sunblock and
donning the protective glasses. Ready to go? Not
quite. We have to cover every bit of soft tissue before
we apply a highly potent whitening gel to the teeth.
Once it’s finally under way, we give the patient a
bell to ring if he or she feels any discomfort. It might
be a little zap or it can feel as painful as someone
sticking an ice pick in his or her tooth. Patients then
sit and wait, and wait, and wait. Will they get
through it or will they need to stop halfway?
Once the whitening process is complete, we
remove the isolation. Oops, the isolation leaked and
there’s a white line on the gums? Don’t worry, it
won’t stay white. It will turn bright red, and after it’s
done sloughing off, it will look normal again. The
continued on page 82
80
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 36 on card
cosmetic
feature
continued from page 80
patient’s teeth will most likely be dehydrated, so now
he or she is advised to stay away from red wine, dark
sauces, tea, coffee, among other things, for the next
day or two so they don’t stain. Sometimes this is the
worst case, but there have been cases when patients
will call the next day complaining that their gums are
blistering. Maybe the light was a little too close and
burned the tissue (while you were surfing the Web).
There are plenty of cases when the procedure
goes smoothly, but the whitening was inadequate.
The patient needs to return for another session or
continue whitening at home. The results are white
teeth, but the complications of in-office whitening
can be significant.
Let’s consider an alternative. Professionally fabricated whitening trays with a whitening gel appropriate for the specific case. Quality trays can easily
be fabricated by a well-trained staff member. Trays
should be made from accurate models with smooth,
sharply trimmed gingival margins. I can’t stress the
importance of quality trays enough. If dental
experts are going to charge an appropriate fee for
this service, the product must look and feel like
something special.
Not every patient should receive the same
whitening gel. There are many systems available
with various ingredients designed to desensitize,
but all have one common ingredient – peroxide.
There are also a couple of different types of peroxide to use – hydrogen peroxide or carbamide peroxide in varying concentrations. Whatever gel you
dispense, an appropriate concentration for each
case should be selected.
The amount of time and frequency that the gel is
applied should also be varied. Personally, I like 22percent gel for up to one hour for most patients, but
I always instruct my patients to remove the trays at
the first sign of sensitivity. I would prefer that they
waste gel rather than have discomfort.
Recently, I had a new patient come to me
because she had been unsuccessful in her attempts to
have her teeth whitened by two previous dentists.
She was getting married in three months and desperately wanted whiter teeth. Her previous attempts
The #1 Botox & Dermal Filler Training Course in Dentistry!
®
BOTOX & DERMAL
FILLER
THERAPY
For Every Dental Practice
AMERICAN
ACADEMY
of
FACIAL
ESTHETICS
TM
TM
Register before
Oct. 1, 2012 and save
up to $700 off tuition
Featuring:
Dr. Louis Malcmacher, Dr. James Jesse,
and the faculty of the
American Academy of Facial Esthetics
Limited Attendance!
Sign Up Today!
Upcoming Courses:
• Sep. 14-15
• Sep. 21-22
• Sep. 28-29
• Sep. 28-29
• Sep. 28-29
• Oct. 12-13
• Oct. 12-13
• Oct. 19-20
• Oct. 19-20
• Oct. 26-27
• Nov. 2-3
16 AGD
PACE CE
Credits
Jacksonville, FL
St. Louis, MO
Birmingham, AL
Loma Linda, CA
Detroit, MI
Minneapolis, MN
Scottsdale, AZ
San Antonio, TX
Salt Lake City, UT
Dallas, TX (Level I & II)
Seattle, WA
More 2012 dates can be found on our website!
AACD and AGD members receive
an additional savings off tuition!
Call Today! 1-800-952-0521
or visit: FacialEsthetics.org
OUR #1 SELLING BOTOX AND DERMAL FILLER THERAPY DVD’S – NEW 3 VOLUME SET!
®
These over the shoulder treatment DVD’s will give you a solid foundation of facial esthetic techniques.
Two hours of AGD PACE CE credit for each DVD!
Limited time offer - order before Oct. 1, 2012 and save up to $150!
FREE FACTS, circle 3 on card
82
SEPTEMBER 2012 » dentaltown.com
cosmetic
feature
included one in-office whitening procedure, but she
experienced significant pain and had to stop after
only 10 minutes. Her second attempt was a takehome system that she could also not tolerate due to
teeth and gum pain. She needed well-made trays and
a concentration of gel appropriate for her very sensitive teeth. I instructed her use a 10-percent gel (her
previous attempt was 22 percent) and she used it for
only 10-15 minutes per day for two months. This
was a very slow procedure that required a significant
amount of gel and excellent patient compliance, but
she comfortably obtained the results that she wanted
and was happy to show off her white smile at her
wedding. This is a great example of how this procedure can be modified to suit each individual’s needs.
Many of the over the counter (OTC) products
look similar to those that we dispense. It is important
to educate patients on the difference between OTC
products and professionally dispensed products. We
have the ability to use materials that are far more effective, but require our supervision to prevent potential
damage. If patients are reluctant to have professional
whitening, I encourage them to try an OTC product.
In most cases, they ultimately return for treatment.
I asked 40 local dentists their opinions on inoffice versus take-home techniques. The overwhelming majority agree with me. They have
varying results from in-office techniques and prefer
the predictability of take-home techniques. I am
sure there are plenty of offices that have great success with in-office techniques, but they seem to be
the minority.
There is no shortage of data evaluating whitening techniques. A 2012 study by The International
Journal of Periodontics and Restorative Dentistry
that compared the efficacy of take-home versus inoffice techniques, among others, stated that there
were no significant differences in the results, regardless of the technique. The study also found the use
of the light did not change the results of the inoffice whitening.
Other studies have shown that the heat from the
lights might contribute to dehydration of the teeth and
therefore might cause the temporary appearance of a
whiter tooth. The heat from the light can also contribute to pulpal sensitivity and soft-tissue irritation.
The time a whitening agent is in contact with the
teeth and the duration that it is kept in contact are
the main variables that affect whitening. They are
also the two variables that affect the most common
side effect, sensitivity.
“To me, it really comes down
to predictability. I perform predictable
procedures with consistent results.”
Regardless of the technique used, the results
were virtually identical and there was no significant
difference in the longevity of the resulting whitened
teeth. It is an individual preference to select the
technique that is best for the dental professional and
the patient.
To me, it really comes down to predictability. I
perform predictable procedures with consistent
results. I don’t like to do a costly elective procedure
and have less-than-ideal results, including pain or an
unsatisfied patient. I have been able to achieve comfortable whitening that can be customized for every
patient to obtain great results and maintained for
years. This leads to happy, satisfied patients as well
as referrals.
It is safe to say that what works best in one practice might not be the best for another. For now, I’ll
stick to the take-home technique, but I will keep an
open mind and look forward to predictable, faster,
comfortable techniques. ■
Author’s Bio
Dr. Joseph Banker of Creative Dental Care is a veteran cosmetic dentist who has been named "Top Dentist" by New Jersey Monthly Magazine
for four consecutive years. He studied at the UMDNJ, and trained at The Las Vegas Institute for Advanced Dental Studies and the Rosenthal
Institute of NYU. He is a member of the American Academy of Cosmetic Dentistry, The Crown Council and a number of other dental organizations. Dr. Banker treats patients from all over the country at his office in Westfield, New Jersey. Dr. Banker has contributed to numerous media outlets
including Newsweek, Shape Magazine, Dentaltown Magazine, and has previously served as a dental consultant for the show Extreme Makeover. For more
info, visit www.creativedentalcare.com.
83
dentaltown.com « SEPTEMBER 2012
continuing education
feature
“The best way to show that a stick is
crooked is not to argue about it or to
spend time denouncing it, but to lay a
straight stick alongside it.” – D. L. Moody
by Paul A Jones, DDS, MS
Abstract
Cone Beam CT (CBCT) is an excellent tool in endodontic diagnosis and treatment planning. This course defines CBCT, compares
the types of devices available, and discusses which ones are best in
endodontics. It lists the advantages and disadvantages of CBCT. It
shows how much radiation a patient receives compared to other medical and dental X-rays.
The types of endodontic cases where a CBCT is indicated are
listed. Several cases are presented where CBCT more clearly revealed
the cause of the problem than conventional two-dimensional X-rays.
CBCT sometimes prevents subjecting patients to exploratory surgery
or endodontic access on hopeless teeth. Like the operating microscope,
clinicians who utilize CBCT would not want to practice without it.
Educational Objectives
At the end of this program, participants will be able to:
1. Define cone beam CT and then describe the types of machines
available.
2. Understand the amount of radiation a patient receives from
CBCT compared to other types of medical and dental X-rays.
3. Describe when taking a CBCT is appropriate in endodontics.
4. Compare the advantages and disadvantages of CBCT over conventional 2D radiography.
5. Understand the limitations of CBCT with regard to artifacts.
6. Explain who is responsible for detecting and reporting potential pathology on CBCT scans.
This written self-instructional program is designated for 1.5 hours of CE credit by Farran Media. Participants will receive verification
shortly after Farran Media receives the completed post-test. See instructions on page 90.
Farran Media is an ADA CERP Recognized provider. ADA CERP is a service of the American Dental
Association to assist dental professionals in identifying quality providers of continuing dental
education. ADA CERP does not approve or endorse individual courses or instructors, nor does it
imply acceptance of credit hours by boards of dentistry.
84
SEPTEMBER 2012 » dentaltown.com
Approved PACE Program Provider
FAGD/MAGD Credit
Approval does not imply acceptance
by a state or provincial board of
dentistry or AGD endorsement.
12/01/2004 to 12/31/2012
continuing education
feature
Two-dimensional X-rays have been an integral part of
endodontic diagnosis and treatment planning for over a century
but they have limitations. Three-dimensional cone beam computed tomography (sometimes called cone beam volumetric
tomography), or CBCT, now allows viewing the anatomy and
pathology of the teeth and bone in all three dimensions in thin
slices at any angle, and accurate measurement of the teeth and
other structures.
What is Cone Beam CT?
In CBCT a cone-shaped X-ray beam is rotated around the
head of the patient, exposing a sensor to multiple views of the
teeth and jaws. A computer then renders those scans into a volume of images of the region of interest (ROI) that are then
reconstructed to allow viewing slices at any angle or thickness.
More importantly, CBCT allows viewing anterior teeth in the
sagittal (anterior posterior) plane and posterior teeth in the coronal plane (from the mesial and distal) as well as slicing them axially (at right angles to the long axis of the teeth); these views are
essentially unobtainable in periapical radiography. CBCT also
displays bone, defects or lesions in bone, as well as anatomic
structures to be avoided in surgery like the inferior alveolar
nerve, the mental foramen and the maxillary sinus. Because of
the dimensional accuracy of the scan, teeth and bone can be
measured in sub-millimeter distances.
CBCT differs from spiral (fan) beamed medical CT in that it
is lower in cost and in the amount of radiation exposure to the
patient. CBCT devices are classified by the size of the area imaged
called the field of view (FOV). Large FOV machines image the
entire skull; medium FOV machines image both jaws; and small or
limited FOV image one quadrant or one jaw. The minimum cube
of data displayed is called voxel (volumetric pixel) and is analogous
to the square pixel in digital photography. The voxel size also represents the minimum slice thickness achievable by the scan.
In general, the larger the field of view, the greater the
absorbed radiation dosage to the patient and the larger the voxel
size. Because endodontic diagnosis and treatment planning is
usually concerned with imaging one quadrant of teeth and with
fine detail, small FOV machines are most appropriate in
endodontics. When looking for cracks and periapical lesions, the
smallest voxel size is best. Although new machines are constantly
becoming available, 76 microns (0.076mm) is the smallest voxel
size currently on the market. The average width of the periodontal ligament space and the diameter of the tip of a size 20-K file
are both 200 microns (0.20mm).
CBCT is a valuable aid in endodontics in the following
situations:
• Difficult endodontic diagnosis where suspected apical
lesions are not seen on periapical X-rays (PA) and the clinical exam is inconclusive.
• Difficult root and canal anatomy to help determine the
number, shape, curvature and length of roots and canals.
• Endodontic retreatment cases where cause of failure is unclear.
• Locating suspected cracks in roots or bone loss caused by them.
• Procedural accidents (perforations, file separations).
• Internal and external tooth/root resorption.
• Traumatic injuries to teeth and bone.
• Measuring the length of teeth, the width of bone and the
distance from anatomic structures like the inferior alveolar canal and maxillary sinus to the apex when planning
endodontic surgery.
ALARA – “As Low As Reasonably Achievable” – is the guiding principle in all radiology. Due to the slightly higher radiation, CBCT should only be used when the clinical exam and
conventional radiographs don’t demonstrate enough information for adequate diagnosis and treatment planning. Young
patients are much more susceptible to the effects of radiation
than adults who are more susceptible than senior citizens.
Anyone who orders or takes a CBCT is responsible for all
pathology visible on the scan. All slices in all three-dimensions
should be carefully reviewed for pathology, not just the region of
interest. Just as those who perform oral surgery or endodontics
are held to the standard of care of a specialist, those who take or
order a CBCT are held to the standard of care of an oral maxillofacial radiologist. Until one becomes proficient in reading
CBCT scans, they should also be reviewed by someone who is.
The AAOMR (http://www.aaomr.org/) presents courses in
CBCT interpretation that are quite good.
How Much Radiation Does a Patient Receive
from CBCT?
Effective radiation dosage can be expressed a number of
ways. Micro Sievert (μSV) is the unit most cited in current literature. The most meaningful to the patient is probably days of
normal background radiation.
Chart 1 was created from Ludlow1 and White & Pharoah.2 It
illustrates the various dosages of different brands of CBCT
machines and traditional X-rays. Note that a cross-country airline
trip exposes a patient to radiation dosages higher than some dental
CBCT scans and that radiation from medical CT is much higher
than most dental CBCT machines, especially the small FOV.
Advantages of CBCT over 2D X-rays
Maxillary posterior teeth are sometimes difficult to visualize
due to anatomic overlap of the zygomatic arch, buccal roots,
maxillary sinus, palatal roots and palatal bone. They are more
easily visualized on CBCT than with conventional PA. Multiple
1:
2:
Ludlow, J.B., 2009. Dosimetry of the Kodak 9000 3D Small FOV CBCT and Panoramic Unit. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 107, e29.
Oral Radiology: Principles and Interpretation, White & Pharoah Mosby, Inc. 2009
continued on page 86
85
dentaltown.com « SEPTEMBER 2012
continuing education
feature
continued from page 85
periapical X-rays taken at different angles will sometimes show the
anatomy but small FOV CBCT scans of the maxilla expose the patient
to radiation doses similar to two to three periapical X-rays and more
clearly displays the anatomy and pathology.
Seltzer & Bender3 in 1961 demonstrated that defects created in the
cancellous portion of the jaw were not visible with 2D X-rays unless
they invaded the cortical plate. By displaying a thin slice at any angle
through both the cancellous and cortical bone, CBCT often shows
bone loss from apical periodontitis that is not visible on 2D intraoral
periapical radiography.
Lofthag & Hansen4 in 2007 concluded “…in selected cases, e.g.,
when there is no detectable pathology in periapical radiographs
although clinical tests indicate so, or when endodontic surgery is
planned for multi-rooted teeth, additional radiographic examination
using a 3D technique… should be considered.” Estrela et al.5 in 2008
concluded that detection of apical periodontitis was significantly better
with CBCT than with periapical or panoramic radiography.
Fig. 1 shows two cases demonstrating that principle. The PA didn’t
clearly show the periapical lesions but the CBCTs did.
Fig. 2 illustrates the value of CBCT in making a diagnosis. The
clinical exam didn’t differentiate which tooth was causing the patients
symptoms. The PA didn’t show an obvious periapical lesion. CBCT
3:
4:
5:
Fig. 1
Fig. 2
Bender IB, Seltzer S. Roentgenographic a direct observation of experimental lesions on bone. J.A.D.A. 62:152 Feb. 1961.
Lofthag-Hansen, S., Huumonen, S., Gröndahl, K., Gröndahl, H.-G., 2007. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
103, 114–119.
Estrela, C., Bueno, M.R., Leles, C.R., Azevedo, B., Azevedo, J.R., 2008. Accuracy of Cone Beam Computed Tomography and Panoramic and Periapical Radiography for Detection of Apical Periodontitis. J Endod 34, 273–279.
86
SEPTEMBER 2012 » dentaltown.com
continuing education
feature
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
clearly shows a lesion at the apex of #15 on both the sagittal and
coronal slices.
The PA (Fig. 3) doesn’t show a lesion but the CBCT (Fig. 4)
clearly shows not only a lesion on the mesial buccal root but also
that the cause is probably a previously untreated MB2 canal.
Nurbakhsh et al.6 reported using CBCT to study maxillary
sinus mucositis adjacent to teeth with apical periodontitis.
Maxillary sinusitis can sometimes be confused with endodontic
periapical pathology and visa versa. Fig. 5 is a case where the patient
was diagnosed by his ENT with a sinus infection. The PA didn’t
show which tooth was the cause but the CBCT clearly showed that
the abscessed upper first molar was the cause of the sinus infection.
Lower molars sometimes have three distinct roots.7 Figs. 6 and
7 show a case where the CBCT clearly shows that to be the case but
the PA does not.
Maxillary incisors very rarely have more than one root. Fig. 8 is
a case where the periapical X-ray didn’t show that but the CBCT did.
Figs. 9 and 10 are a case where the tooth remained symptomatic
after root canal treatment. The PA didn’t reveal the cause of the
6:
7:
Nurbakhsh, B., Friedman, S., Kulkarni, G.V., Basrani, B., Lam, E., 2011. Resolution of Maxillary Sinus
Mucositis after Endodontic Treatment of Maxillary Teeth with Apical Periodontitis: A Cone-Beam Computed
Tomography Pilot Study. J Endod 37, 1504–1511.
Song, J.S., Choi, H.-J., Jung, I.-Y., Jung, H.-S., Kim, S.-O., 2010. The Prevalence and Morphologic
Classification of Distolingual Roots in the Mandibular Molars in a Korean Population. J Endod 36, 653–657.
Fig. 9
Fig. 10
continued on page 88
87
dentaltown.com « SEPTEMBER 2012
continuing education
feature
continued from page 87
Fig. 11
Fig. 14
Fig. 12
Fig. 15
problem but the CBCT did. Note that only two of the four
canals were located and treated.
The mesial roots of lower molars sometimes have three
canals. Fig. 11 shows how CBCT shows three canals in the
mesial root of a lower second molar; the periapical doesn’t.
Patel et al.8 concluded that “the advent of cone beam computed tomography has considerably enhanced the clinician’s
capability of diagnosing internal root resorption.” Root resorption is sometimes difficult to see clearly on PA. Fig. 12 is a case
where CBCT much more clearly shows the extent of the internal resorptive defect on the palatal root of an upper first molar
that is not evident on the PA.
Cracked teeth and roots are notoriously difficult to diagnose
and treatment plan. Bernardes et al.9 concluded that “cone-beam
volumetric tomography was better than conventional radiography in the diagnosis of root fractures.”
Kajan & Taromsari10 concluded “CBCT can be an ideal alternative in the diagnosis of root fracture in the field of endodontics.” CBCT can only reveal cracks that are at least twice as wide
as the minimum voxel size of the scan according to the Nyquist
Theorem. Even if the crack is too small to be seen on a CBCT,
the bone loss caused by the bacteria contained in cracks is often
easier to demonstrate on CBCT than on periapical radiographs.
Fig. 13 is a case where the bone loss caused by a crack on the
distal of the lower second molar is visible on the CBCT but not
8:
9:
10:
11:
Fig. 13
on the periapical. Note that the crack in the root is not visible
on the CBCT so it must be narrower than twice the 76 micron
voxel size of the scan, or about the diameter of the tip of an ISO
size 15/02 endodontic file.
Fig. 14 is an upper canine where the crack in the root can
clearly be seen on the axial view of the CBCT, so it must be
wider than twice the voxel size. Notice that the crack and the
bone loss are also seen on the periapical X-ray.
The vertical bitewing suggests a short root canal filling in
the mesial buccal root of the upper first molar might be the
cause of the problem and that retreatment or apical surgery
might be indicated. Cone beam CT clearly shows the palatal
root has a vertical fracture, making the prognosis hopeless
(Fig. 15).
The results of traumatic injuries to teeth and bone are often
easier to see on CBCT than on conventional periapical X-rays.
Fig. 16 is a case of two lower incisors re-implanted by an emergency room physician that look OK on the PA. CBCT clearly
shows that they were not re-implanted in the sockets but rather
between the alveolus and the soft tissue.
Kovisto et al.11 concluded “the CBCT scan is an accurate,
non-invasive method to evaluate the position of the mandibular
canal.” CBCT allows tracing and accurate measurement of the
inferior alveolar nerve. This case (Fig. 17) shows that the nerve
is over 6mm from the apex of the lower first molar’s mesial root,
Patel, S., Ricucci, D., Durak, C., Tay, F., 2010. Internal Root Resorption: A Review. J Endod 36, 1107–1121.
Bernardes, R.A., de Moraes, I.G., Húngaro Duarte, M.A., Azevedo, B.C., de Azevedo, J.R., Bramante, C.M., 2009. Use of cone-beam volumetric tomography in the diagnosis of root fractures. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod 108, 270–277.
Kajan ZD, & Taromsari M. Value of cone beam CT in detection of dental root fractures. Dentomaxillofac Radiol. 2012 Jan;41(1):3-10.
Kovisto, T., Ahmad, M., Bowles, W.R., 2011. Proximity of the Mandibular Canal to the Tooth Apex. J Endod 37, 311–315.
88
SEPTEMBER 2012 » dentaltown.com
continuing education
feature
making periapical surgery less risky than if the nerve was nearer
the apices.
In Fig. 18 the apices of the lower molars are touching the
inferior alveolar nerve, increasing the risk of parasthesia caused
by apical surgery.
Fig. 19 demonstrates the various artifacts on CBCT than can
be confused with pathology. Metal restorations and radiopaque
root canal fillings cause beam hardening and streak artifacts due
to photon starvation that appear like decay in the crowns of teeth
and cracks in the roots. One must be careful when first interpreting CBCT scans not to misinterpret these as pathology.
Procedural accidents like root perforations and file separation are better visualized by CBCT than periapical X-rays. Fig.
20 is a case where the cause of non-healing is not apparent on
the PA but a post perforation to the buccal mid root is clearly
visible on the CBCT.
12:
Although Cone Beam CT is being utilized by more than
one-third of the endodontists in the U.S., it is not yet the standard of care. It should not be used for routine screening of all
patients or taken on all cases.12
Summary
CBCT is a valuable tool in endodontics in cases where
the clinical exam and traditional two-dimensional radiographs fail to produce a diagnosis; in retreatment cases;
where unusual anatomy, cracks, trauma and resorptive
defects are present or suspected; or where apical surgery is
planned. A CBCT will sometimes prevent subjecting patients to
needless operative or surgical procedures to make a diagnosis
and treatment plan of hopeless teeth. Like the operating
microscope, clinicians who utilize CBCT would not want to
practice without it. Use of cone-beam computed tomography in endodontics Joint Position Statement of the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology, 2011. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod 111, 234–237.
Fig. 16
Fig. 17
Fig. 18
Fig. 19
Fig. 20
Author’s Bio
Dr. Paul A Jones has limited his practice to endodontics since 1978. He has been using Cone
beam CT in his private practice since 2009, where he has taken and read more than a thousand CBCT scans. He has taken or given more than 100 hours of continuing education in
Cone beam CT, read scores of articles and books, and contributed to a chapter in a textbook on the subject. He is a member of the American Academy of Oral and Maxillofacial Radiologists, the American
Association of Endodontists, and the American Dental Association.
continued on page 90
89
dentaltown.com « SEPTEMBER 2012
continuing education
feature
continued from page 89
Post-test
Claim Your CE Credits
Answer the test in the Continuing Education Answer Sheet and submit it by mail or fax with a processing fee of $36. We invite you to view all of our CE
courses online by going to http://www.dentaltown.com/onlinece and clicking the View All Courses button. Please note: If you are not already
registered on www.dentaltown.com, you will be prompted to do so. Registration is fast, easy and of course, free.
1. Which size field of view (FOV) scan is most appropriate in
endodontics?
a. Small or limited FOV.
b. Medium FOV.
c. Large FOV.
d. Medical CT.
2. What is the number of days of natural background radiation
a patient receives from a single limited FOV Kodak 9000
CBCT scan?
a. Zero to one.
b. One to five.
c. Five to 10.
d. Ten to 20.
3. What is the ability to see periapical lesions in cancellous
bone on cone beam CT scans compared to periapical X-rays?
a. Less.
b. About the same.
c. More.
d. It depends on the size of the lesion.
4. An axial slice on a cone beam CT is:
a. Parallel to the floor.
b. From ear to ear.
c. From front to back.
d. At an oblique angle.
5. The distance from the apex of a lower tooth to the inferior
alveolar canal can be measured accurately to within a tenth
of a millimeter on cone beam CT.
a. True
b. False
a. They might only be visible if they are wider than twice the
minimum voxel size of the scan.
b. They will be visible even if there are metal posts or
radiopaque fillings in the root canals.
c. The bone loss adjacent to the cracks in roots is often visible on scans even if the cracks themselves aren’t.
d. They are more easily visualized on CBCT than on periapical X-rays.
8. Who is responsible for detecting and reporting to the patient
any pathology visible on a cone beam CT scan?
a. An oral maxillofacial radiologist.
b. The practitioner who orders the scan.
c. The owner of the facility that takes the scan.
d. All of the above.
9. As a person ages from a child to an adult to a senior citizen,
which is true about their susceptibility to any potential
adverse effects of radiation?
a. Less susceptible.
b. More susceptible.
c. About the same.
d. Depends on the weight of the patient.
10. Cone beam CT is now the standard of care in endodontics,
and if available in the office should be taken on all cases.
a. Both parts of the statement are true.
b. The first part is true but the second false.
c. The first part is false but the second true.
d. Both parts of the statement are false.
6. Dental decay can easily be identified by a CBCT on teeth
where there are several large metal restorations on other
teeth in the quadrant.
a. True
b. False
Legal Disclaimer: The CE provider uses reasonable care in selecting and providing content
that is accurate. The CE provider, however, does not independently verify the content or
materials. The CE provider does not represent that the instructional materials are error-free
or that the content or materials are comprehensive. Any opinions expressed in the materials are those of the author of the materials and not the CE provider. Completing one or
more continuing education courses does not provide sufficient information to qualify participant as an expert in the field related to the course topic or in any specific technique or
procedure. The instructional materials are intended to supplement, but are not a substitute
for, the knowledge, expertise, skill and judgment of a trained healthcare professional. You
may be contacted by the sponsor of this course.
7. Which statement about detecting cracks in teeth and roots is
not true about cone beam CT scans?
Licensure: Continuing education credits issued for completion of online CE courses may
not apply toward license renewal in all licensing jurisdictions. It is the responsibility of each
registrant to verify the CE requirements of his/her licensing or regulatory agency.
90
SEPTEMBER 2012 » dentaltown.com
continuing education
feature
Continuing Education Answer Sheet
Instructions: To receive credit, complete the answer sheet and mail it, along with a check or credit card payment of $36 to:
Dentaltown.com, Inc., 9633 S. 48th Street, Suite 200, Phoenix, AZ 85044. You may also fax this form to 480-598-3450. You will
need a minimum score of 70 percent to receive your credits. Please print clearly. This course is available to be taken for credit
September 1, 2012 through its expiration on September 1, 2015. Your certificate will be e-mailed to you within 3-4 weeks.
Cone Beam CT in Endodontics by Paul A Jones, DDS, MS
License Number ______ ______ ______ ______ ______ ______ ______ ______ ______ _______
CE Post-test
Please circle your answers.
AGD# _____________________________________________________________________________________
Name _____________________________________________________________________________________
Address ___________________________________________________________________________________
City___________________________________________ State __________ ZIP _________________________
Daytime phone_____________________________________________________________________________
E-mail (required for certificate) _________________________________________________________________
Check (payable to Dentaltown.com, Inc.)
1.
a
b
c
d
2.
a
b
c
d
3.
a
b
c
d
4.
a
b
c
d
5.
a
b
6.
a
b
7.
a
b
c
d
8.
a
b
c
d
9.
a
b
c
d
10.
a
b
c
d
Credit Card (please complete the information below and sign; we accept Visa, MasterCard and American Express.)
Card Number _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____
Expiration Date – Month / Year ______ ______ / ______ ______ ______ ______
Signature ________________________________________________________________________________________ Date ____________________
Yes, I would like to continue receiving Denaltown Magazine free of charge
(Signature required for subscription - free to U.S. only)
Field of practice (optional)
No, thank you.
Program Evaluation (required)
Please evaluate this program by circling the corresponding numbers: (3 = Excellent to 1 = Poor)
1. Course objectives were consistent with the course as advertised
3
2
1
2. Course material was up-to-date, well-organized and presented in sufficient depth
3
2
1
3. Instructor demonstrated a comprehensive knowledge of the subject
3
2
1
4. Overall, I would rate this course
3
2
1
5. Overall, I would rate this instructor
3
2
1
For questions, contact Director of Continuing Education Howard Goldstein at hogo@dentaltown.com
General Dentist
Anesthesiology
Consultant
Cosmetic Dentistry
Dental Assistant
Dental Company Rep.
Dental Education
Dental Lab Tech
Dental Student
Dental Hygiene Student
Endodontics
Endodontic Resident
Front Office
Hygienist
Implantology
Oral & Maxillofacial Surgeon
OMS Resident
Oral Pathology
Orthodontics
Orthodontic Resident
Pediatric Dentistry
Pediatric Resident
Periodontics
Periodontic Resident
Prosthodontics
Public Health
Radiology
Speaker
TMD Specialist
Other
91
dentaltown.com « SEPTEMBER 2012
FREE FACTS, circle 49 on card
continuing education
feature
by Dr. Anthony Tay
Abstract
Fig. 1: Anterior composite buildup with the simplified layering technique.
This article describes a simplified approach toward step-by-step layering of the anterior composite restoration. An understanding toward
natural aesthetic from composite buildup and the ideal dimensions of
individual layers will be presented. This will allow the practitioners
to learn the skills required to confidently place anterior composite
buildup in a conservative, aesthetic and predictable manner.
A common scenario that general dental practitioners face involves
the rehabilitation of lost dental tissue in the anterior teeth. This can be
in response to dental trauma from an accident or replacement of a
defective restoration. With today’s composite material in the dental
market, it is possible to restore the lost dental tissue in a conservative
and predictable approach. For this purpose, this presentation describes
a simplified technique for such aesthetic anterior composite buildup.
The individual steps will be described logically, including the layering
details. To create surface anatomies that will mimic nature and lifelike
aesthetics, the protocols for finishing and polishing will be given. With
some practice, such anterior composite buildup can be routinely
placed in a conservative, aesthetic and predictable manner.
Educational Objectives
At the end of this program, participants will be able to:
a. Understand the workflow required for anterior composite
buildup in a simplified manner.
b. Determine the thickness of the different composite layers for
ideal aesthetic outcome.
This written self-instructional program is designated for 1.5 hours of CE credit by
Farran Media. Participants will receive verification shortly after Farran Media receives
the completed post-test. See instructions on page 99.
94
SEPTEMBER 2012 » dentaltown.com
Approved PACE Program Provider
FAGD/MAGD Credit
Approval does not imply acceptance
by a state or provincial board of
dentistry or AGD endorsement.
12/01/2004 to 12/31/2012
continuing education
feature
c. Restore a fractured anterior tooth with minimal adjustment and finishing, using a putty matrix.
d. Create primary, secondary and tertiary anatomies for aesthetic anterior restoration.
e. Understand and master the polishing techniques for teeth
of different surface textures.
composite restoration should first be attempted to replace the
lost dental tissue.
In emergency situations, two common techniques are usually employed, i.e., freehand composite buildup or palatal
“gloved finger matrix” techniques. The “gloved finger matrix”
technique involves placing the clean-gloved index finger behind
the palatal surface of the tooth, and using it as a matrix for the
Introduction
initial placement of the composite. This technique allows a betOne of the most common aspects of a general dental practi- ter control of the subsequent layering process than the freehand
tioner’s work involves the rehabilitation of lost dental tissue in technique. However, since it is not precise in its dimension and
the anterior teeth. This can sometimes be a result of accident form, it requires experience and practice to get a satisfactory
trauma, or simply a replacement of a defective restoration that aesthetic outcome.
was placed previously. With the advancement in adhesive techFor routine situations, however, when there is no urgency of
nology, coupled with the improvement in mechanical property time, I prefer the commonly used silicon putty matrix technique.
of the restorative composite material, such rehabilitation can
1. For the situation of the fractured anterior dental tissue,
now be routinely done in a fairly conservative and predictable
this will involve taking an impression of the dental arches,
manner, often without the consideration for conventional
followed by an extra-oral wax-up of the fractured site. The
prosthodontics. This minimalist approach reduces the destrucdetails of the wax-up are then captured and transferred to
tion of healthy tooth structure, while preserving the remaining
a silicon putty matrix (Virtual, Ivoclar Vivadent), to form
tooth strength and extending to its longevity. With this in mind,
the scaffold for the composite layering process.
composite restoration of the lost anterior dental tissue thus takes
2. For the situation of the defective restoration replacement,
on an increasingly important role.
the wax-up stage might not be necessary if the existing
There are many composite materials in the market, with as
restoration has a satisfactory form and outline. This can thus
many clinical techniques dedicated to their applications. Central
be directly captured and transferred to the silicon putty
to most of these techniques involves the comprehension of the
matrix, before the actual composite rehabilitation treatment.
theoretical, practical and clinical aspects of the composite rehaIn such cases, the silicon putty matrix is very useful as it
bilitation. A theoretical understanding of the mechanical prop- allows stable placement of the initial composite layer. In addierty of the composite, its translucency, chroma and opacity, tion, its highly accurate impression nature allows the capturing
allows the practitioner to modulate the composite layering and of the wax-up details in a precise manner and minimizes the
thickness successfully. The practical aspect involves the familiar- eventual occlusal adjustment.
ization of the material’s handling, the sensitivity to ambience
Prior to the commencement of the clinical restorative prolight and the best tools to manipulate it to the practitioner’s cedure, the tooth shade is taken to assist in the composite
advantage. Finally, the all-important clinical restorative steps shade selection, for the creation of invisible margin between
must be staged and streamlined to ensure maximum efficiency composite and tooth structure. This is critical, as the tooth
dehydrates with prolonged period of moisture control, and its
for the practitioner and his practice.
In this article, I describe a simplified layering technique for value subsequently increases. When this happens, the tooth
will appear more opaque. Hence, any
aesthetic anterior composite buildup, using
attempt to match this higher opacity with
3M ESPE Filtek Supreme Ultra (Filtek
the composite restoration immediately, will
Z350XT in the Asia Pacific region) restoracause a visual mismatch of the tooth-comtive composite. Filtek Supreme Ultra is a
posite complex upon rehydration of the
nano-filled composite that is suitable for both
tooth a few hours later.
anterior and posterior uses.
After the shade taking process is completed, a suitable local anesthesia may be
Tooth Preparation
given, followed by rubber dam isolation.
A central incisor was used in this presTooth preparation involves the placement of
entation, with an enamel-dentine fracture
buccal and palatal bevels to assist in the aessimulated at the mid-body section, withthetic blending of the composite to the
out the pulp being exposed. In such cliniFig. 2: A central incisor with a simulated
cal setting, when no sign of irreversible enamel-dentine fracture. Rubber dam is tooth, as well as increasing the surface area
for composite bonding. This is followed by
pulpitis or pulpal necrosis is encountered, placed to mimic moisture control.
continued on page 96
95
dentaltown.com « SEPTEMBER 2012
continuing education
feature
continued from page 95
etching, priming and bonding of the prepared tooth surface,
according to the practitioner’s preferred choice and system of
etchant, primer and bonding agent. In this presentation, 3M
ESPE Scotchbond Etchant Gel and 3M ESPE Adper
Singlebond 2 primer adhesive were used, according to the
manufacturer’s instruction. The tooth surface is now ready
for composite restoration.
Composite Layering
To begin, the silicon putty matrix that was made prior to the
clinical procedure is now being used to construct the palatal surface with composite. This layer will determine the palatal
dimension of the tooth, and allow the buildup of the remaining
layers anteriorly. A thin layer of A1E (3M ESPE Filtek Supreme
Ultra A1 Enamel shade) composite is placed on the putty surface, corresponding to the missing dental tissue of the affected
incisor. A common error that practitioners encounter is to layer
the composite on the putty in either excess or inadequate cervico-coronal width. Excess width will result in excessive composite flash at the beveled palatal margin, while inadequate width
might cause reduced adhesive contact with the beveled palatal
margin. A better approach, just prior to any composite placement here, is to place and approximate the putty matrix to the
affected incisor and inscribe the beveled palatal tooth margin
onto the putty matrix surface, via a sharp explorer.
The A1E composite is then placed in thin amount onto the
matrix surface, between 0.3 to 0.5mm in thickness, and slightly
extended beyond the inscribed line of the sharp explorer. A
microbrush and a ball burnisher are most suitably used to ensure
Fig. 3
Fig. 5
an even thickness of the layer. It is important to keep this layer
thin to minimize polymerization shrinkage of the composite,
and to allow slight translucency for visual effect. The putty with
the composite is transferred back onto the palatal surface of the
incisor, with a gentle pressure on the putty directed towards the
palatal surface of the tooth, to allow the approximation of the
composite to the beveled palatal margin of the tooth.
Following 20 seconds of light-curing, the putty is gently
peeled away to reveal the adhesion of the composite to the
tooth unaided. The composite should reveal slight translucency, which will assist in the reproduction of incisal halo subsequently. For more dramatic translucency, CT (3M ESPE
Filtek Supreme Ultra Clear Translucent shade) composite can
sometimes be used instead of A1E here. This can result in a
greater incisal halo effect.
An optional, but useful step involves the use of flowable
composite to fill in any potential void created between the
palatal composite layer and the palatal beveled tooth margin.
This will reduce any trapped air bubbles. In this illustration, a
thin layer of 3M ESPE Filtek Supreme Ultra Flowable
Restorative shade A2 is placed and light-cured for 20 seconds.
Next, the mesial and distal walls are built up to the required
dimensions with A1E and lightcured for 20 seconds. In the clinical intra-oral setting, this dimension is usually determined by
the immediate neighboring teeth contacts (Fig. 6). The tooth is
now effectively converted to a large Class V cavity.
The dentine mass is reproduced with the layering of A3D
(3M ESPE Filtek Supreme Ultra Dentine A3 shade) composite
within this new Class V cavity.
Fig. 6
Fig. 7
Fig. 8
Fig. 9
Fig. 4
Fig. 3: A sharp explorer, such as a Ash No. 6 probe, can be used to inscribe the
palatal tooth margin onto the silicon putty (Virtual, Ivoclar Vivadent) surface.
Fig. 4: Microbrush is used to even the surface of the palatal composite layer
(A1E), as well as to minimize trapped air bubble.
Fig. 5: First layer completed with A1E.
Fig. 6: A2 Flowable is placed between the composite and palatal bevel margin
interface.
Fig. 7: Mesial and distal walls completed with A1E.
Fig. 8: Three hyperchromatic mamelons, built up with A3D, are clearly visible.
Fig. 9: CT placed to simulate the desired incisal halo.
96
SEPTEMBER 2012 » dentaltown.com
continuing education
feature
To mimic the higher chroma of the natural dentine, the dentine composite shade chosen should be ideally one or two shades
darker than the enamel composite shade. This also allows the
dentine composite layer to be seen clearly through the subsequent buccal enamel composite layer. In this illustration, the
enamel shade chosen was A1, while the dentine shade was A3.
When placing the A3D composite, care should be taken to
ensure a smooth transition slightly onto the buccal bevel of the
natural tooth, to mask any visible restorative margin. At the
same time, three distinct mamelons are placed at the incisal
third to mimic that seen in a natural central incisor.
For optimum aesthetic, the overall dentine shade composite should be kept 0.5mm short of the intended buccal
enamel surface (in a palato-buccal manner), to allow the final
buccal placement of 0.5mm of enamel shade composite.
There are a few ways to make this thickness assessment, such
as using a sectioned buccal silicon putty matrix or just visual
estimation. Recently, a new tool called LM-Arte Misura (LM
Arte instruments from Style Italiano) was developed to make
this assessment of final enamel composite thickness more predictable. The dentine composite is now ready to be lightcured for 20 seconds.
For the creation of incisal halo, we next placed CT composite between the mamelons and around the mamelons (slightly
within the incisal, mesial and distal margins of this “Class V cavity”). This is light-cured for 20 seconds.
To complete the final enamel layering, we placed 0.5mm
thickness of A1E composite onto the buccal surface. It is important to keep this layer thin and evenly spread out so that we can
Fig. 10
Fig. 11
minimize the finishing process. I recommend the use of size
three brush, with a thin amount of wetting resin on the brush
(Brush & Sculpt, Cosmedent) to ensure a uniform spread of the
layer, improve handling characteristic and minimal trapping of
air bubbles. Avoid using bonding agent in place of wetting resin,
as bonding agent may contain HEMA and thus can affect the
polymerization and also the final color of the composite. We followed this with 20 seconds of light-curing.
Finishing
Primary and Secondary Anatomy:
Anatomies creation should ideally be done after the lightcuring of the final enamel composite layer. Gross-contouring is
done using coarse and medium coarse discs (Soft-lex, 3M ESPE)
to achieve the desired primary anatomy. For buccal secondary
anatomy, there are many techniques available. I favor the technique from Dr. Newton Fahl Jr., using a pencil to mark vertical
and horizontal lines on the tooth. This serves as a guide for the
rotary contouring. With the line markings, a long flame-shaped
diamond bur is used in a controlled manner, to reproduce the
three subtle developmental lobes as well as the two triangularshaped shallow depression at the incisal third of the buccal surface. A silicon polishing cup (Astropol P, Ivoclar Vivadent) is
used to smooth the transition of the secondary anatomy created.
Tertiary Anatomy:
If tertiary anatomy is desired, especially in young teeth that
require perikymata characterization, the same long flame-shaped
bur can be used to achieve this effect. This bur should be placed
parallel to the buccal surface, and moved between mesial and distal slowly one or two times, at a very slow rotary speed with
feather-light pressure. It is important to use magnification for this
purpose, as there is a tendency for many practitioners to overdo
it. The tertiary anatomy, when created, is smoothened again with
Astropol P, to make the appearance subtle and natural.
Polishing
Fig. 12
Fig. 13
The restoration is finally polished with aluminum oxide
polishing paste (Enamelize, Cosmedent) and felt polishing disc
(FlexiBuff, Cosmedent) at slow-medium speed, light-medium
pressure, to achieve the desired luster. In my experience, I favor
the use of electric micromotor, with slow-speed conventional
Fig. 10: Completed layering.
Fig. 11: Computer overlay image of the desired pencil line markings on the tooth
image of Figure 10. This gives us the guide for producing primary and secondary anatomy.
Fig. 12: Primary, secondary, tertiary anatomies created.
Fig. 13: Completed – Natural tooth color reproduction.
continued on page 98
97
dentaltown.com « SEPTEMBER 2012
continuing education
feature
Fig. 14
continued from page 97
Fig. 15
Fig. 14: Completed – Subtle incisal halo resent.
Fig. 15: Completed – Harmonious blending of the different layers.
Fig. 16: Completed – Palatal tooth margin clinically invisible.
Fig. 17: Completed – Developmental grooves created in a natural manner.
Fig. 18: Left model shows a smooth but matte surface. Right model shows a
smooth and highly shiny surface. No surface resin glaze is needed.
Fig. 18
Fig. 16
Fig. 17
contra-angled handpiece for this polishing stage. The high
torque from the electric micromotor allows the polishing to be
done in a controlled manner without causing micro-gouging of
the polished surface.
to a high shine with Enamelize and FlexiBuff. The results show
that a matte or shiny surface can be easily created, depending on
the aesthetic outcome desired. Both models, with the slightly
different polishing protocols, do produce a clinically acceptable
smooth surface, as seen in older teeth.
Alternative Finishing and Polishing Method
In older teeth that have lost their surface microtexture
(perikymata) and acquired a smooth and sometimes shiny surface, tertiary anatomy is not indicated. Instead, after the secondary anatomy stage, this restoration can be polished with 3M
ESPE Soflex Fine and Superfine polishing discs, at mediumhigh rotary speed, to achieve a matt, smooth surface. If high
shine is desired, Enamelize and FlexiBuff can subsequently be
used with the technique described above.
In this simple demonstration, two composite tooth models
were built up to identical dimensions, using 3M Filtek Supreme
Ultra Body A2 shade (A2B). They were finished to the secondary anatomy stages (under the section Finishing – Primary and
Secondary Anatomy). Both models were then subjected to further
polishing with 3M ESPE Softlex fine and superfine polishing
discs. However, only the right model was additionally polished
1.
2.
3.
4.
5.
Devoto W, Saracinelli M, Manauta J. “Composite in everyday practice: how to choose the right material
and simplify application techniques in the anterior teeth.” Eur J Esthet Dent. 2010 Spring;5(1):102-24.
Fahl Jr, N “Mastering Composite Artistry to Create Anterior Masterpieces - Part 2.” Journal of Cosmetic
Dentistry 2011: 42-55, Winter.
Fahl Jr, N “Mastering Composite Artistry to Create Anterior Masterpieces - Part 1.” Journal of Cosmetic
Dentistry 2010: 56-68, Fall.
Dietschi D “Layering concepts in anterior composite restorations.” J Adhes Dent. 2001 Spring;3(1):71-80.
Dietschi D “Optimising aesthetics and facilitating clinical application of free-hand bonding using the ‘natural layering concept.” Br Dent J. 2008 Feb 23;204(4):181-5.
98
SEPTEMBER 2012 » dentaltown.com
Conclusion
A simplified layering technique, as described here, allows
practitioners to create natural-looking anterior composite with
predictability. With the improvement of the restorative composite over the years, we must, as dedicated caregivers to our
patients, take advantage of this, and be able to offer minimally
invasive and conservative restorative treatment. With practice,
we will be able to do so confidently. Author’s Bio
Dr. Anthony Tay received his Bachelor of Dental Science
from the University of Melbourne, Australia, in 2005. He
returned to Singapore in 2006, where he has been involved
in full-time metropolitan private practices. As a general practitioner, he
delivers a comprehensive range of dental services, with special interest
in composite rehabilitation, restorative dentistry and minimal intervention dentistry. He is a current committee member of the Academy of
Cosmetic Dentistry (Singapore) and the Continuing Dental Education
committee of the Singapore Dental Association, and is actively involved
in continuing dental education for his peers. He can be contacted at
dr.anthonytay@gmail.com
continuing education
feature
Post-test
Claim Your CE Credits
Answer the test in the Continuing Education Answer Sheet and submit it by mail or fax with a processing fee of $36. We invite you to view all of our CE
courses online by going to http://www.dentaltown.com/onlinece and clicking the View All Courses button. Please note: If you are not already
registered on www.dentaltown.com, you will be prompted to do so. Registration is fast, easy and of course, free.
1. Which of the following about the use of silicon putty matrix
is true?
a. It allows the stable placement of the initial composite layer.
b. It captures the wax-up details to allow accurate transfer of
tooth form and dimension.
c. It minimizes finishing and occlusal adjustment.
d. All of the above
2. What is the role of the sharp explorer in this presentation?
a. To inscribe the palatal tooth margin onto the silicon
putty matrix so that the palatal composite layer can be
predictably placed.
b. To allow the creation of perikymata at the finishing stage.
c. To stabilize the composite layering when using the light-cure.
3. Shade-taking of the tooth is taken before the placement of
the rubber dam...
a. because the eyes become tired and lose the ability to differentiate chroma at the end of the restorative procedure.
b. because the tooth dehydrates and its value increases for a
few hours after rubber dam placement, resulting in inaccurate shade match.
c. because the debris and saliva from the tooth preparation
after rubber dam placement can interfere with the perception of hue.
4. What can be done to create invisible margins between the
composite and tooth structure?
a. Place bevels on the tooth preparation margin.
b. Select a composite shade that is similar to the tooth structure, prior to dehydration from rubber dam placement.
c. All of the above
5. Why is flowable composite useful in this presentation?
a. It fills in any potential void between the initial palatal
layer of composite and the palatal tooth margin, thereby
reducing any air bubble trapped.
b. It is used as a bulk-fill agent.
c. It provides the halo effect.
6. When restoring anterior composite with the technique
described in this article, the dentine shade should ideally be:
a. The same shade as enamel shade.
b. One or two shades darker than enamel shade.
c. One or two shades lighter than enamel shade.
7. After the placement of the dentine composite layer, what is
the ideal thickness of the buccal, final enamel layer of composite for optimum aesthetic?
a. 0.5mm
b. 1.0mm
c. 1.5mm
d. 2.0mm
8. Which of the following about the role of the wetting resin
is false?
a. It reduces air bubbles being trapped during layering.
b. It improves the handling of the composite.
c. It improves the polishing quality of the composite.
9. For anterior restoration, secondary and tertiary anatomies
should be created…
a. after the light-curing of the final enamel composite layer.
b. before the light-curing of the final enamel composite layer.
c. before the light-curing of the dentine composite layer.
10. Old teeth tend to appear smoother and shiner than young teeth.
a. True
b. False
Legal Disclaimer: The CE provider uses reasonable care in selecting and providing content
that is accurate. The CE provider, however, does not independently verify the content or
materials. The CE provider does not represent that the instructional materials are error-free
or that the content or materials are comprehensive. Any opinions expressed in the materials
are those of the author of the materials and not the CE provider. Completing one or more
continuing education courses does not provide sufficient information to qualify participant
as an expert in the field related to the course topic or in any specific technique or procedure.
The instructional materials are intended to supplement, but are not a substitute for, the
knowledge, expertise, skill and judgment of a trained healthcare professional. You may be
contacted by the sponsor of this course.
Licensure: Continuing education credits issued for completion of online CE courses may
not apply toward license renewal in all licensing jurisdictions. It is the responsibility of each
registrant to verify the CE requirements of his/her licensing or regulatory agency.
continued on page 100
99
dentaltown.com « SEPTEMBER 2012
continuing education
feature
continued from page 99
Continuing Education Answer Sheet
Instructions: To receive credit, complete the answer sheet and mail it, along with a check or credit card payment of $36 to:
Dentaltown.com, Inc., 9633 S. 48th Street, Suite 200, Phoenix, AZ 85044. You may also fax this form to 480-598-3450. You will
need a minimum score of 70 percent to receive your credits. Please print clearly. This course is available to be taken for credit
September 1, 2012 through its expiration on September 1, 2015. Your certificate will be e-mailed to you within 3-4 weeks.
Simplified Step-by-Step Layering Technique for Aesthetic
Anterior Composite Buildup by Dr. Anthony Tay
License Number ______ ______ ______ ______ ______ ______ ______ ______ ______ _______
CE Post-test
Please circle your answers.
AGD# _____________________________________________________________________________________
1.
a
b
c
2.
a
b
c
3.
a
b
c
4.
a
b
c
5.
a
b
c
6.
a
b
c
7.
a
b
c
8.
a
b
c
9.
a
b
c
10.
a
b
Name _____________________________________________________________________________________
Address ___________________________________________________________________________________
City___________________________________________ State __________ ZIP _________________________
Daytime phone_____________________________________________________________________________
E-mail (required for certificate) _________________________________________________________________
Check (payable to Dentaltown.com, Inc.)
d
d
Credit Card (please complete the information below and sign; we accept Visa, MasterCard and American Express.)
Card Number _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____
Expiration Date – Month / Year ______ ______ / ______ ______ ______ ______
Signature ________________________________________________________________________________________ Date ____________________
Yes, I would like to continue receiving Denaltown Magazine free of charge
(Signature required for subscription - free to U.S. only)
Field of practice (optional)
No, thank you.
Program Evaluation (required)
Please evaluate this program by circling the corresponding numbers: (3 = Excellent to 1 = Poor)
1. Course objectives were consistent with the course as advertised
3
2
1
2. Course material was up-to-date, well-organized and presented in sufficient depth
3
2
1
3. Instructor demonstrated a comprehensive knowledge of the subject
3
2
1
4. Overall, I would rate this course
3
2
1
5. Overall, I would rate this instructor
3
2
1
For questions, contact Director of Continuing Education Howard Goldstein at hogo@dentaltown.com
100
SEPTEMBER 2012 » dentaltown.com
General Dentist
Anesthesiology
Consultant
Cosmetic Dentistry
Dental Assistant
Dental Company Rep.
Dental Education
Dental Lab Tech
Dental Student
Dental Hygiene Student
Endodontics
Endodontic Resident
Front Office
Hygienist
Implantology
Oral & Maxillofacial Surgeon
OMS Resident
Oral Pathology
Orthodontics
Orthodontic Resident
Pediatric Dentistry
Pediatric Resident
Periodontics
Periodontic Resident
Prosthodontics
Public Health
Radiology
Speaker
TMD Specialist
Other
townie trip
feature
Since dental product manufacturers want to make products with dentists in mind, 3M
took full advantage of the available Townie think tank. Several Townies traveled to 3M’s
headquarters in Minnesota to give the company feedback on upcoming products and equipment.
Dr. Don McNamara says,
Naturally, the 3M folks were wonderful and really rolled out the red carpet for us Townies. The
Innovation Center was a great place for the lecture portions and the tour of the facility was like visiting a science museum.
As with all Townie gatherings, the real meat of the meeting was the opportunity to spend some quality time with great Townies from the U.S. and Canada. When a 3M speaker would toss out an
idea or want to brainstorm some concepts for improving a product, there were some great ideas
offered by those in attendance. I mean, when you’re talking the pros and cons of CAD/CAM products with the likes of McClure and Fleming, you get great, accurate feedback!
Dr. Tim Goodheart states,
It’s sort of mind-boggling to learn just how many products 3M invented, developed and sells. For
me personally, it was very impressive to see just how much time, effort and company talent it puts
into its dental division and products. Regardless of whether a dentist chooses to use 3M products, I
think dentistry ought to take great satisfaction in the fact that a high-tech, top quality, innovative
company such as 3M considers dentistry to be an important part of its present and future and puts
a large chunk of the companies’ resources into improving things for dentists and patients.
Dr. Tim Burke says,
3M embodies a collection of qualities which are, in my experience, unparalleled. I have prior experience with corporate culture – before dental school I spent more than four years in quality control
with Kraft foods, and my ex worked for Lever Brothers while I was in school. While they are obviously both world-class businesses, their R&D departments can’t compare with 3M and its culture
of teamwork and cooperation. It is their synthesis and integration of widely disparate technologies
that permit them to continually develop and market products while others stand by and wonder
what happened.
I’m sure people have talked about the “Trifecta” of bond, cement and materials. That was a huge hit
for the dental end. I can see some of the materials that we were sent to evaluate will likewise turn out
to be popular – the retraction paste and polishing systems have great potential, and should do well.
The “Paradigm” line was a wise addition, in spite of all the razzing it took for confusing nomenclature. 3M has a solid name, and a value line carrying it will likely be accepted more readily than an
unknown generic.
I think we really gave them some things to think about – not always what they wanted to hear –
but at least it was honest. More, they really did seem to value the input as we spoke to some of them
about topics we discussed last year. ■
101
dentaltown.com « SEPTEMBER 2012
roundtable
discussion
It was a dark and humid night on Victoria Harbour. The
choppy water lapped against the hull of the alluring Aqua Luna
junk boat as four top dental industry CEOs watched the
Symphony of Lights laser show illuminate buildings on Hong
Kong Island and the Kowloon peninsula. After the harbor
cruise, the four disembarked the Aqua Luna and sauntered over
to Hullett House, an English Colonial building on Canton
Road, for a traditional Cantonese feast. There, Dr. Howard
Farran, John Christensen, Dr. Rhonda Savage and Patrick
Tessier assembled around a table for a spirited evening.
The gathering conjured themes of Woody Allen’s recent hit,
Midnight in Paris, where a group of high-profile writers rendezvoused in an enchanting place and time. What brought liter-
ary leaders like Hemmingway, Fitzgerald, Stein, Porter, Dali and
Picasso to Paris in the 1920s? The same thing that brought these
four dental thought leaders together nearly a century later on
this particular night in Hong Kong: a passion for creating meaningful lives and professions; the thrill of collaborating and vetting ideas with like-minded people.
In a quest for continuous improvement of the dental profession, each traveled from the U.S. to Hong Kong for the World
Dental Forum, an international dental event where more than 500
participants from seven countries gather to share innovative
approaches to dentistry from around the world. As the evening progressed, and the brainstorming between the four garnered momentum, a fundamental link between the four became evident: passion.
continued on page 104
102
SEPTEMBER 2012 » dentaltown.com
WHAT IIS
PA
?
Your PASSION
COSMETIC
C DENTISTR
DENTISTRY
RY
With
you can easily deliver up
to 8 units of lab quality veneer s with our direct
composite stentt in about an hourrr.. Boost your
" #!" !# !! %$#%$"#$#
ective new-patient magnet.
which is an efffeec
TM
EZVeneers
en
V
ass looww as $
TM
EZZ ENEERS
SERVING
SER
RVING
V
Y
YOUR
OUR
O
COMMUNITY
To help you treat the under ser ved,, you maay
prescribe our top quality removable products at
ver y attractive feees,, through our ver y competitive
Pre-Pay Program.
m.. Expand your patient base,
ityy.
grow your practice and help your community
ass low as $
DIGITAL
DIGIT
TAL
A DENTISTR
D
DENTISTRY
RY
LAVATM
Ultimate
Send in your digital
gital impression fo
or a restoration
milled on our industrial 5-axis machines fo
or a
%$#"! ! %%$!!"#$! !#$###
e.max
FMZ™
onnlly $
& More!
y
These are our everyday fees, not one
one-time introductor y
prices. We are committed to earning your business with
$
"#$ !#!$!! #$ !"#
afffo
ordable feees.. If you’re passionate about dentistr y like we
are, give us a call...
WE’LL FUEL
EL
PASS
Your PASSION
FREE FACTS, circle 23 on card
Dental
Dental Laborat
Laboratory
ory USA
Boston
888-659-5913
Los Angeles
800-859-0822
Chicago
866-963-6856
Seattle
877-711-8778
www.moderndentalUSA.com
roundtable
discussion
continued from page 102
What is Passion?
we’ve become the largest dental community in the world! I insist
that passion was, is and always will be a fundamental tenet to my
success, so much so that I made ‘be passionate, enthusiastic and
determined to make a difference’ one of the core values expected
from every employee of my company.”
In the opening scene of the movie Heights, Glenn Close’s
character lectures her university students on passion. “That is
the problem with us today,” she warns, “we can’t remember what
it’s like to be consumed with desire. We have forgotten passion!
… for Christ sake, take a risk sometime this weekend!”
For these leaders in dentistry, this kind of deep, risk-taking zeal Dr. Rhonda Savage:
permeates all aspects of their lives. It’s a character trait. The line Passion to Elevate Practice Management
“Today my area of expertise focuses on dental practice manbetween their personal life and their professional life blurs because
their jobs aren’t just jobs; they are purposes, they are life-long agement,” said Dr. Savage. “But even before purchasing Linda
quests for improving the world around them – they are passions. Miles and Associates (now Miles Global), dentistry was my true
calling. My passion for this profession
And passion doesn’t have a pause button.
was so strong that it led me to be an
But what is passion, exactly?
active duty dental officer in the U.S.
Psychologist Robert Vallerand defined
Navy. After that, like Dr. Farran, I also
passion as “a strong inclination or
started my own practice.
desire towards a self-defining activity
“In dental school, they teach us
that one likes (or even loves), finds
enough to succeed clinically, but when
important, and in which one invests
it comes to the business side of the dentime and energy … these activities
tal practice, we all could use some help.
come to be so self-defining that they
I may have been passionate about
represent central features of one’s idenimproving the smiles of my patients,
tity,” (Dr. Robert J. Vallerand, 2007).
Above: Godfrey Ngai speaking at World Dental Forum
Vallerand’s progressive research Below, from left: John Christensen, Dr. Rhonda Savage, but my quest soon turned into becoming a resource for dentists who needed
posits that passion improves perform- Dr. Howard Farran and Patrick Tessier
help with systems, accountability and
ance in all aspects of life. Dr. Farran,
communication. When we give aid to
Dr. Savage, Mr. Tessier and Mr.
a dental practice to help its bottom line,
Christensen can all attest to this. All
the staff and doctor(s) can treat all of
four were invited to discuss their pastheir patients to the best of their ability.
sions at this impromptu roundtable,
“I am currently the CEO of Miles
and how each were driven to create
Global and I focus on helping dental
organizations that make important
offices become more successful. My
contributions to the world of dentistry.
goal is to encourage and empower other
dentists. I’m very attentive and make
Dr. Howard Farran:
great
recommendations,
while making the whole team feel
Passion to Build a Dental Community
extremely
inspired.
My
passion
is to do all I can to ensure their
“Early on in my life, my goal was to become a dentist,” said
Dr. Farran. “I aggressively achieved that goal, but once I did, I growth and trigger them to be even more successful.”
yearned for something more. It didn’t take long for me to experience the isolation common to many practicing dentists. I felt Patrick Tessier:
like I was on my own island doing my own dentistry with Passion to Aid the Dental Profession
nobody to bounce ideas off of until I could go on a fishing trip
“I joined the dental laboratory business a dozen years ago,”
with the friends I’d made in dental school. I was driven to find said Tessier. “As a mechanical engineer with an MBA, I immedia way to communicate with my peers all the time instead of ately fell in love with the dental profession. All of my education
when it was convenient for a handful of us to get together. and experience have been fully utilized, but the most impressive
Thank God for the Internet!
aspect of the dental business is the fundamental fact that den“I created Dentaltown so no dentist would ever have to prac- tistry helps people; there is a real-time direct connection with
tice solo again. I realized that if dentists could collaborate easily doctors and patients.
and effectively, then ideas for improvement could be shared by
“When I was introduced to Modern Dental Laboratory a
all and could have a dramatic result for the participants. With decade ago, I knew almost immediately that importing the highmore than 150,000 Dentaltown members worldwide today, quality work from Modern could improve the lives of our clients
104
SEPTEMBER 2012 » dentaltown.com
roundtable
discussion
and their patients. My fundamental business
model separating manufacturing from customer
service allows MDL USA to offer world-class
quality products with white glove service and
great pricing.
“As my import business grew, the quality
difference became very clear. Doctors loved the
work. Comments like ‘after 25 years, I now
enjoy restorative’ became common. I began to
realize we were actually helping improve dentistry by allowing the doctor to focus on treating the patient, not
fussing with the lab work.
“It makes me very proud to think we are helping dentists
deliver the very best dental health care they possibly can. Every
day I get to count my blessings: that I was fortunate to be introduced to this business by Mr. George Obst of DSG; that I was
lucky to meet Mr. Godfrey Ngai of Modern Dental; that every
day I get to work with my friends at MDL USA to serve our
dentist clients and help them deliver
great health care. I think it is our
human duty to do the very best with
skills and abilities we have. It is my
passion to make the most of my blessings and try to make a positive difference in the world.
John Christensen:
Passion to Spread the Word
“When I graduated from Northwestern University’s Advertising/
Marketing Graduate School in 1980 and started my agency,
chrisad, I accepted any type of client who would pay the bills,”
said Christensen. “Almost immediately, dentists began contacting me and we began conducting fairly extensive patient-consumer research by testing various advertising approaches.
“The first couple dental clients did not do well. I later
understood the reason for this was not the marketing but rather
the aspects of practice management that no amount (nor quality) of marketing could overcome. The third dental client’s practice was optimally configured, their early marketing sparked a
yet unheard of growth, and before I knew it, I had dozens of
dentist clients in the San Francisco Bay Area.
“I had no idea that no other marketing firm had ever specialized in dentistry. What excited me the most was that with every
marketing step my company took, and every bit of data we
uncovered, we knew we were pioneers. Every day revealed a new
breakthrough – even today, after 32 years of exclusively working
with dentists, with the largest database in the world of in-prac-
Left: Modern Dental Lab Tour led by
Godfrey Ngai
Below: Howard A. Ngai, Dr. Howard Farran
and Dr. Chan
Below, left: U.S. delegation on Modern
Dental Lab tour.
tice patient-consumer behavior, working
in four nations and with 100-million
mail marketing pieces out each year, we
are still experiencing similar exciting
breakthroughs.
“I never view my job as work, but as
a fun game because I know the outcome
is 100 percent certain, I will never give
up on any client and will passionately
stand by their side until they attain it. It’s a great deal of fun!”
What is Your Passion?
Does your work “consume you with desire”? Do you take
risks to attain those desires? Great leaders answer “yes” to both
of these questions. Passion is a type of energy that is manifested
from inside; a force to be tapped into, accessible to all. When
someone is truly passionate about what they do, like these dental giants, others are drawn to you. Your passion, whether it is to
build a dental community, to permeate into a practice, to help
the dental community or to spread the word, attracts the attention of your patients and employees. It inspires and enlivens
them. The excitement that your passion generates will keep your
patients retuning again and again and will keep your staff
around for years on end.
Deep down, we all have passion for what we do. We’d like for
you to share your passion with the Dentaltown community. Please
share your story here: www.dentaltown.com/whatisyourpassion. The next World Dental Forum will be held in Paris, France in 2014. To learn more, call 877-711-8778.
105
dentaltown.com « SEPTEMBER 2012
addiction
feature
ne, DDS, MBA
by William T. Ka
The focus of this article will be on indentifying the dental patient with a substance use disorder (SUD) or an addictive disease, as these terms are basically the same. Additionally, it will
cover how an addictive disease affects all aspects of a patients’ life.
Identification and Understanding Addictive Diseases
When our patients seek our skill and care for their oral health needs, they bring a variety of
interesting needs with them. These needs can be emotional, psychological, financial and physical issues that must be addressed prior to and along the way in the dentist/patient relationship.
By the fourth year of dental school, we have discovered this.
At a patients’ initial appointment, they fill out a health history, giving us an insight into their
current and past medical and dental health. Certain diseases, conditions and patient behavior
give us information regarding the patients’ systemic health and will assist us in making the
appropriate diagnosis and dental treatment plan.
When examining a patients’ social history, dental professionals should routinely ask about
the use, frequency and quantity of alcohol, tobacco and other drugs, as well as any history of
addiction, alcoholism or substance abuse. However, a West Virginia survey of dental professionals states that 36 percent of respondents acknowledged not doing so.1
1.
Tufts Health Care Institute Program on Opioid Risk Management. Executive Summary. The Role of Dentists in Preventing Opioid Abuse. March 11-12,
2010. Available at: www.thci.org/opoid/mar10doc/executivesummary.pdf
continued on page 108
106
SEPTEMBER 2012 » dentaltown.com
Selling A Practice Shouldn’t Be
As Scary As A Trip To The Dentist.
NAPB Turns Scary Into Simple
At the National Association of Practice Brokers (NAPB),
we’re experts in dental practice brokerage and transitions and
have decades of experience successfully transitioning thousands
of practices nationwide. We are your Go-To Teeam in ‘Simply’
selling your practice successfully.
Contact
Contact uuss at 888.407.2908 for
for more
more iinformation
nformation oorr vvisit
isit uuss aatt www.buyandsellapractice.info
www
w.b
. uyandsellapractice.info
f
FREE FACTS, circle 29 on card
addiction
feature
continued from page 106
The prevalence of substance abuse is so high that every health care provider in the U.S. sees
patients either at risk themselves or experiencing negative effects of substance use by a friend,
family member or co-worker.2 Addiction is an “equal opportunity” disease that can be present in
patients from all walks of life.
In broad terms, substance use can be described as use, misuse, abuse, addiction. Use is of
course the proper application of say an opioid for post-operative pain following a dental procedure. Misuse would be taking the same opioid for “non medical” use. The next term abuse is
when one has too many drinks on their birthday, or takes more pain medication than actually
prescribed to obtain a more profound or euphoric effect. Finally, addiction is when the individual will continue using the substance despite adverse consequences.
A short and to-the-point definition of addiction is as follows: “Addiction is a medical disorder with a complex etiology, multiple manifestations and a varied clinical course.”3 A recent definition states: “Addiction coops the brain’s neuronal circuits necessary for insight, motivation
and social behaviors. This functional overlap results in addicted individuals making poor choices
despite awareness of the negative consequences; it explains why previously rewarding life situations and the threat of judicial punishment cannot stop curtailing addictions.”4 Patients with an
addiction have “mental mismanagement” where poor decisions
are the norm, not the exception. As the disease progresses, all
Certain patients with addictions
areas of the patients’ life continue on a downward fashion.
Addictive diseases are chronic and progressive and can be fatal
will complain of extreme dental
if not adequately treated. Dental professionals may have difficulty
identifying a patient whose disease state is in the early to middle stages.
pain and extreme anxiety to
Also, one may have difficulty addressing an addictive disease in
the later stages with patients since they are almost always in
secure narcotic prescriptions
denial that they indeed are suffering from an addiction.
Unfortunately dental professionals have not been trained to conduct screening and intervention techniques when patients present with addictive diseases. This is certainly an area that could
be addressed more aggressively by organized dentistry and dental education. In a busy general or
specialty practice, this type of screening is hard to implement.
Certain factors should be considered when looking at a patient’s health and social history.
Certain medical and dental professionals may have a greater suspicion their patient may have
other substance use disorders if they are heavy smokers or smokeless tobacco users. This is certainly a point to consider! Substance use disorders and addictions can negatively affect certain
organ systems such as the hemopoetic, the cardiovascular and the digestive systems.
A patient reporting a past history of hypertension, recent pneumonias and pancreatitis often
have an alcohol abuse or dependence. The patient presenting with complex health histories will
often require a medical consult which can reveal more information than perhaps the patient has
reported. Additionally, patients tend to underreport certain conditions for a variety of reasons.
If a patient lists allergies to several commonly prescribed narcotic pain medications this should
cause some reason for concern.
Frequently, patients with addictions seek episodic emergency care. This may bring someone
new to your practice seeking relief from a painful dental condition. One can also observe established patients interest in their oral health deteriorate over time along with the progression of the
disease. These patients may be more apt to respond to a dental professional’s brief screening or
intervention since a relationship has been established.
A new emergency patient in addition to the painful condition concerning them may have
heightened fears and anxieties concerning dental treatment. Very often the front office can pick
2.
3.
4.
Madden, T.E.: CDA Journal, Vol 36: No. 2: Feb 2008 (119-121)
Vaillant, G.E.: Principles of Addiction Medicine, 3rd edition, 2003, (p.3)
Volcow, N.D., Baler, R.D., Goldstien,R.Z., Neuron 69, Feb 24, 2011 (p599)
108
SEPTEMBER 2012 » dentaltown.com
addiction
feature
up on this and alert the clinical team and ultimately the dentist. When the patient is examined,
health and social history reviewed, radiographs interpreted and a diagnosis made, often the treating dentist will have a fairly good idea of what is going on.
This is where the “red flags” may start to appear. Certain patients with addictions will complain of extreme dental pain and extreme anxiety to secure narcotic prescriptions. Some of these
patients are master manipulators and can get what they want rather easily. When they are successful, they will continue to have these or other pain issues and also refer their “network” of friends
and family. Others whose disease has progressed are far less skilled in manipulation. It takes a seasoned dental professional to resist the skillful manipulation of these “dentist shopper” patients.
Another “red flag” may pop up when the patient presents with a mouth with multiple
pathologies present and the patient blames this condition on several outside factors. These may
include, “The dentist I had in the Army, or previous dentist have done all these horrible things
to me.” These stories can be very “interesting,” but the bottom line is the patient takes no personal responsibility for the condition of their mouth.
The reality is, patients with addictions can and do have real painful dental emergency conditions that really do require treatment. This is really a “slippery slope” for the dental professional
– what are the choices? Generally dentists would want to eliminate the painful condition yet not
participate in enabling the addiction to continue.
Here are some things to consider:
• Am I comfortable with treating this patient? If the answer is yes, proceed with caution, if
your gut-level feeling tells you no, refer the patient.
• Although not the focus of this article, should you decide to treat this patient, offer immediate relief of pain, profound local anesthetic and perhaps an extraction, an I and D, or
open up the tooth initiating endodontic therapy. If the patient accepts and you can do
this, at least the acute painful condition can be eliminated. However if they reject this
treatment and attempt to steer you towards prescribing a powerful narcotic this can be the
game changer!
• Since the patient may be exhibiting various degrees of “mental mismanagement,” adequate informed consent documents should be in place as well as written post operative instructions.
• Become familiar with substance abuse treatment facilities in your community. A great
source of information could be patients in recovery that you are successfully treating.
Treating a Dental Patient in Active Addiction
Most general dentists and dental specialists have patients present with painful conditions that
require rather urgent treatment. Sometimes these patients are easy to treat and other times those
presenting with complex medical issues may not be so easily treated. Patients presenting in our
practices with addictive diseases fall into the later, and are far more difficult to manage and treat.
Patients with addictions can present with unpredictable and maladaptive behaviors. They
could have even possibly created their own iatrogenic dental pathology. This group of patients will
have dependability problems such as keeping appointments and following treatment recommendations. Generally, they will also have exaggerated fears and anxieties regarding dental treatment.
The ultimate goal of treating a patient in acute pain whether they have an addictive disease
or not is to treat and eliminate the painful condition. The goal for some patients in active addictive disease would be to utilize the dentist to continue to support their addiction through liberal
prescribing practices. We must be diligent not to allow perpetuation of their addiction.
In general terms, our goal when treating patients in active addiction is to stabilize the oral
health. Attempting to proceed with extensive dental treatment in these patients prior to adequate
treatment of the addiction will be frustrating. This would be similar to attempting to proceed
with extensive periodontal and restorative dentistry on a patient with untreated hypertension and
diabetes and expecting a good outcome.
continued on page 110
109
dentaltown.com « SEPTEMBER 2012
addiction
feature
continued from page 109
Dentists are often the first healthcare providers to identify suspicious indicators such as hypertension, advanced periodontitis or other symptoms such as possible addictive diseases. We routinely inform our patients of our findings and make appropriate referral to their primary health
care provider for evaluation of these conditions.
How to handle a patient you feel has an addiction can be challenging, and depends on where
the patient is in the disease spectrum. This is where dentists struggle to adequately address the
addictive disease to the patient. There are no easy answers here. A good source of information
would be patients in your practice who are in recovery or perhaps a dental colleague in recovery.
If you decide you will treat a patient with an active addiction, you should realize they will be
more difficult and take longer to treat. Again, there are no simple answers or check lists for treating these patients. The first priority of course is an accurate diagnosis of the dental pathology. Also
there may be several areas of the patients’ mouth that may need attention. After informing the
patient of your findings, next is your decision on the treatment to present to the patient.
Since these patients may be under the influence of their drug of choice or requiring more of
the drug, informed consent is a challenge. Adequate written informed consent and written postoperative instructions are a must. One could place in the post-operative instructions that “lost or
stolen” analgesic prescriptions will not be replaced, and that no refills will be called in.
It is often advisable to have a physician consult if time would permit. If you suspect the
patient has used IV drugs, antibiotic prophylaxis is indicated. It is not a good idea or appropriate
to treat a patient that is intoxicated, unless of course there is dental trauma involved. It is a general rule of thumb not to treat a patient who has used cocaine or methamphetamine within the
last 24 hours; this of course is unrealistic to expect a patient to do this. Adequate pre-operative
screening including adequate vital signs should allow you to make the decision to treat immediately or defer or refer the proposed treatment.
Perhaps the best treatment plan if time would allow is
to attempt to immediately eliminate the painful condition.
This treatment could consist of an extraction, opening the
tooth for endodontic therapy or even an emergency I and
D and area of acute swelling. This would not work in the
case of extreme swelling involving trismus.
If the patient accepts this treatment and you proceed,
thorough written post-operative instructions should be
presented. This would include the number of days postoperatively you feel they may have some discomfort, the
amount of pain medicine we will prescribe and that you
must see them in the office if the pain persists after two
to three days.
Now on to the actual clinical procedure. We all have
our ways of treating emergency patients in our practices.
Again, several of these patients will have exaggerated fears
and anxieties as well as increased drug tolerances and
cross-tolerances. These are the folks when the Nitrous
Oxide is at 50% plus will tell you they are not feeling any
different! So, lots of topical anesthetic, gentle administration of profound local anesthetic and even the use of a
long-acting local anesthetic.
Perform the extraction as gently as possible, open the
tooth, remove the pulp, medicate and take the tooth out of
occlusion, or excise and drain in your normal fashion. Consider the use of a glucocortical steroid such as Decedron in
addition to appropriate antibiotic and analgesic therapy.
110
SEPTEMBER 2012 » dentaltown.com
addiction
feature
Selecting the appropriate post-operative analgesic for patients with an active addictive disease is challenging. If the patients’ drug of choice is ethyl alcohol they may have certain degrees
of liver impairment. Since several of the commonly used analgesics contain acetaminophen
(Tylenol) in addition to codeine or hydrocodone these analgesics should be carefully considered.
Additionally, patients with liver impairment can have delayed wound healing. These patients
may be more prone to developing alveolar osteitis (dry sockets).
If the patients’ drug of choice is an opioid, they have increased tolerances to opioid analgesics. In fact, they may actually require a higher dose of the analgesic to achieve adequate pain
relief. This is a “slippery slope” for most dentists and a great time for a physician consult.
Generally we have a good idea how long our patients will require post-operative analgesics. Since
most dental pathology is generally of the inflammatory nature, we should also strongly consider
the use of non-steroidal anti-inflammatory (NASIDS) agents. Also, inform the patient you will
not call in any refills of their analgesics without them first coming back to the office.
If the patients’ drug of choice is in the stimulant category of cocaine or methamphetamine,
one should be careful with the use of epinephrine in local anesthetic. This could be a problem
if the patient has used the drug recently and an inadvertent intravascular injection was to take
place. This is where the increased time involved with caring for these patients is evident.
In states where medical marijuana is legal, certainly patients are presenting to dental offices
in acute painful conditions. These patients may be under the influence of the medical marijuana
and perhaps making adequate informed consent decisions could be difficult as with all patients
in active addiction. Also, since the method of administration involves smoking or use of a nebulizer, this could cause perhaps an increase in alveolar osteitis (dry sockets) following extractions.
Post-operative analgesics may also be difficult to prescribe due to tolerances and cross-tolerances
since there are over 300 active chemicals in cannabis.
Since patients with addictive diseases exhibit “mental mismanagement” as well as various
states of denial, they may not be ready to address their addictions. Dentists have an ethical obligation to treat patients in pain yet not enable an addiction to continue. This is very challenging.
We should attempt to discuss our concerns with our patients in a non-threatening fashion. For
example: “I’m concerned you could be getting in over your head with your drug (or alcohol) use.
Here’s the name of a person at a treatment center. I suggest you go talk to them to see if they
can help you.” It helps to have a name and a little of what the patient can expect. For example,
“Someone there should be able to see you in the next 24 hours – they’ll help you find a place
you can afford.”5
Unfortunately training in screening and brief interventions is not included in dental school
curriculums for substance abuse and tobacco addictions. Some of this training needs to be more
available. Patients with addictive diseases will present in our practices, these patients are “medically compromised” and must receive adequate oral health care. Often these patients complete
adequate treatment for their addiction and live very productive personal and professional lives
in recovery. ■
5.
American Dental Association. Oral health topics: Drug use talking with your patients—dentists version. “wwwlada.org/2663aspx#talking”. Accessed April 29,2011.
Author’s Bio
Dr. William T. Kane graduated from the University of Missouri – Kansas City School of Dentistry in 1980. He maintains a general practice in
rural Dexter, Missouri. In addition to practicing dentistry, Dr. Kane’s interest and passion have been in the area of recovery and wellness. Since
1987, Dr. Kane has been the Chairman of the Dentist Well–Being Committee for the Missouri Dental Association. Additionally, Dr. Kane served
as a member of the Dental Wellness Advisory Committee (DWAC) with the American Dental Association. Dr. Kane is very familiar with issues facing patients
with addictive diseases and has published and presented on these topics. He also completed an MBA in 1992 from Southeast Missouri State University.
In the fall of 2010, Dr. Kane received his Fellowship in the American College of Dentists.
111
dentaltown.com « SEPTEMBER 2012
Advertisement
With a 20-Year History,
This is Fastbraces®:
The One-wire System of Braces
Conventional Braces
FASTBRACES®
Divergent roots between
two crooked teeth
Fastbraces® is a unique business system developed by Dallas orthodontist, Dr. Anthony Viazis. From the earliest
stages of his career, Dr. Viazis was driven to conceive an alternative to traditional braces that was fast, safe and
more affordable. Dr. Viazis believed that teeth could be straightened more efficiently by moving the crown and root
of the tooth simultaneously.
Traditional braces move teeth into position in two stages,
usually over a period of about two years. In the first year, the
crown of the tooth is moved into alignment. In the second year,
treatment addresses the position of the root of the tooth. The
brackets used at Fastbraces® work on a different mechanical
principle altogether. The patented system uses an innovative
bracket and specially shaped wire to correct the position of the
root of the tooth from the beginning of treatment, realigning
the root and crown together rather than in two separate phases.
The bracket used at Fastbraces® is a unique, T-shaped “triangular” bracket with an elevated slot and unique elbow design.
The shape of the bracket is critical because it literally changes
the equation. The square shape of conventional brackets defines
the distance between the brackets and that distance determines
the flexibility of the wire. The triangular shape of the patented
bracket typically doubles the distance between the individual
brackets, which increases the flexibility of the wire eight times.
The extra distance between brackets is what allows a square wire
between brackets to engage, and the “elbows” help deliver
torqueing and tipping forces to the root from the beginning of
treatment. According to Dr. Viazis, that fundamental difference
allows treatment to be completed in about a year, or as little as
three months in select cases. Research at various universities over
the years has independently verified many of the Fastbraces®
112
SEPTEMBER 2012 » dentaltown.com
technology benefits. The new Fastbraces®Clear™ ceramic brackets offer the same technology advantages of moving teeth as the
Fastbraces® metal brackets with the added benefit of an aesthetic
cosmetic solution.
Fastbraces® providers around the world have the benefit of
24/7, 365-days-a-year live support when they have a patient in
the chair and a technical question arises. Providers receive the
patented brackets used at Fastbraces® for each case. They also email photos of the teeth to Fastbraces® after each patient visit. A
convenient customized tooth recording system at Fastbraces®
makes it easy to track and record each tooth’s movement.
Providers pay a flat fee per patient record and receive thorough
training and ongoing support.
Fastbraces offers free doctor training with a two-day handson course. For that reason, Fastbraces® “University” has opened
its doors to dentists and specialists from all over the world. In an
environment reminiscent of ancient Greek academies, where science was ever evolving and discussed openly through dialogue
and free flow of information, Fastbraces® “University” is such a
place for free orthodontics learning. Dentists considering
becoming Fastbraces® providers are invited to contact the
Fastbraces® information line at 1-888-TOP-WIRE or 1-972867-9473 (international) to inquire about free training, or visit
www.fastbracesuniversity.com or www.fastbraces.com. ad
index
ADINDEX
Our advertisers make it possible for us to bring Dentaltown to you each month free of charge. Support these advertisers by
using the reader service numbers listed below and the reply card. Also, almost all of the advertisers provide telephone
numbers in their advertisements for your convenience and fast response. Our advertisers want to hear from you.
ADVERTISER
PAGE #
3M Dental Products – Filtek
3M Dental Products – LAVA
A-dec, Inc.
ADS
AMD LASERS, LLC
American Academy of Facial Esthetics
Apex Dental Materials, Inc.
The Argen Corporation
Bayshore Dental Studio, Inc.
Biolase Technology, Inc.
BISCO, Inc.
Brasseler USA
Burbank Dental Laboratory
Carestream Dental
Common Sense Dentistry
Danville Materials
Darby Dental Supply
Demandforce, Inc.
DenMat Holdings, LLC
DentiMax, LLC
Dentist Identity
DENTSPLY Midwest
Designs for Vision, Inc.
DUX Dental
Evolve Dental
Flexite Company
Flow Dental Corporation
GC America
Gendex Dental Systems
George Vaill
Glidewell Laboratories
Isolite Systems
019
051
035
061
001
082
043
002-003
065
BC
059
007
033
067
038
027
049
004, 005
077, 079
045
032
073
037
127
025
042
044
021
017
110
039
069
CIRCLE #
31
40
38
–
15
3
39
32
13
41
6
1
37
24
4
42
25
14
21
19
16
28
33
43
44
5
17
45
46
–
26
54
Ivoclar Vivadent, Inc.
Keating Dental Arts
Keller Laboratories, Inc. – IPS
Keller Laboratories, Inc. – NTI
Lighthouse PMG
LSK121 Oral Prosthetics
Misch Instruments
Modern Dental Laboratory
National Association of Practice Brokers
New Patients, Inc.
North American Bancard
Officite, LLC
The Online Practice
Orthoworld, LLC
Premier Dental
Pulpdent Corporation
Ribbond, Inc.
Rondeau Seminars
The Scheduling Institute
Sirona Dental Systems
Six Month Smiles
Stoneybrook Publishing, Inc.
Tokuyama Dental
US Bank
VOCO America, Inc.
Xlear, Inc.
029
011
023
125
071
031
063
103
107
055
IBC
Insert
081
092-093
047
115
128
053
014
008-009
015
013
034
072
IFC
117
35
30
47
48
2
22
51
23
29
12
7
–
36
49
20
50
18
11
34
52
8
–
27
9
10
53
009
003
005
IFC
007
BC
60
58
59
57
55
56
IMPLANT SUPPLEMENT
Burbank Dental Laboratory
Glidewell Laboratories
Glidewell Laboratories
Implant Direct
Shatkin F.I.R.S.T., LLC
Zest Anchors, Inc.
Scan the tag on the right using your smart phone for access to any additional
information you may need about an ad or visit www.dentaltown.com/rsc.
113
dentaltown.com « SEPTEMBER 2012
hygiene and prevention
in this section
Unblocking the Nose
by Trisha E. O’Hehir, RDH, MS,
Hyginetown Editorial Director
The first step in switching from mouth breathing to nose
breathing is making sure the nose is clear. Many mouth
breathers experience nasal congestion and even blame their
mouth breathing on this congestion. Strange as it might seem,
mouth breathing causes nasal congestion. It’s a vicious cycle –
the more one mouth breathes, the more congested the person
is and therefore the more he or she breathes through the
mouth. Mouth breathers are also overbreathing, leading to
lower carbon dioxide levels. The brain responds to low carbon
dioxide levels by producing more mucous in the nasal passages, making nose breathing difficult. Therefore the mouth
breathing continues.
Since reduced carbon dioxide levels cause the nose to
block, unblocking the nose can be done by increasing the carbon dioxide levels in the body to reverse the process. Slowing
down the breathing will elevate the carbon dioxide levels. A
simple six-step exercise outlined in the book Close Your Mouth
by Buteyko Breathing instructor Patrick McKeown will
unblock the nose.
The steps are as follows:
1. Sit up straight.
2. Take a small breath in through your nose, if possible,
and a small breath out. If your nose is quite blocked,
take a tiny breath in through the corner of your mouth.
3. Pinch your nose with your fingers and hold your
breath. Keep your mouth closed.
4. Gently nod your head or sway your body until you feel
that you cannot hold your breath any longer. (Hold
your nose until you feel a strong desire to breathe.)
5. When you need to breathe in, let go of your nose and
breathe gently through it, in and out, with your
mouth closed.
6. Calm your breathing as soon as possible.
This exercise can be repeated several times until the nose is
unblocked. Wait 30 seconds before repeating the exercise. With
the nose unblocked, nasal breathing is possible and the switch
can be made from mouth breathing to nose breathing. Inside This Section
116
120
124
126
114
SEPTEMBER 2012 » dentaltown.com
Perio Reports
Profile in Oral Health: Mouth Vs. Nasal Breathing
Product Profile: Prophies, Parafunction and Your Patients
Message Board: Sleep Apnea and Sleep Disordered Breathing
Cause More than Hypoxemia
»
YOURSELF
You might not be getting the fluoride release you think!
By incorporating xylitol-coated calcium and phosphate in a permeable resin matrix that does not separate,
Pulpdent has developed a sustained time-release varnish with uniform dosage that delivers 10 times
more fluoride than the leading varnish brand.
4-Hour Cumulative Fluoride Release
Fluoride Release (mcg)
In micrograms relative to 50.0 +/- 1.0 mg solid weight
1000
900
800
700
600
500
400
300
200
100
0
5% Sodium Fluoride with CXP™
CXP™ = Xylitol-coated Calcium and Phosphate
for unsurpassed fluoride release.
Premier
embrace
Preventech Colgate
Enamel Pro* Vella*
Prevident*
3M
Vanish*
*Not a trademark of Pulpdent Corporation
Yapp R, Powers JM. Fluoride Ion Release from Several Fluoride
Varnishes. Dent Advis Res Rpt 45:1, March 2012.
There’s more to Embrace than fluoride release
• Contains bioavailable calcium, phosphate and fluoride
• Does not separate - no mixing required
• Ensures predictable, uniform dose
• Pleasing taste encourages patient compliance
Call or email today for a free sample: 617.926.6666 / 800.343.4342 / sales@pulpdent.com
FREE FACTS, circle 50 on card
hygiene and prevention
perio reports
Mouth Breathing Reduces Exercise Capacity
Mouth breathing leads to functional, structural, postural, biomechanical, occlusal and behavioral impairments.
More males suffer with mouth breathing than females.
Those who mouth breathe adapt a forward head posture by
bending their head forward and extending their neck to
reduce airway resistance.
Researchers at the State University at Campinas School
of Medical Sciences in Campinas, Brazil compared exercise
capacity and respiratory muscle strength between mouth
and nose breathing in children eight to 12 years of age. Of
the 92 study subjects, 30 were mouth breathers and 62 were
nose breathers. For the exercise section, children completed
a six-minute walk test according to the American Thoracic
Society recommendations.
Mouth breathing children were recruited from the
Mouth Breather Clinic of the Otolaryngology Department
of the State University. Nose breathers were recruited from a
nearby elementary school. Clinical and endoscopy examinations were completed on all students to evaluate the
nasopharanyx and adenoids.
Inhalation and exhalation muscle function was measured prior to and during exercise. Measurements were made
with a mechanical pressure gauge that was connected to a
plastic mouthpiece. A 15-minute rest period was allowed
between measurements taken at rest and during the walk.
Forward head posture was not a significant predictive
factor for muscle function during exercise. Mouth breathing showed significantly less respiratory muscle strength
compared to nose breathing.
Clinical Implications: Recognize and reverse mouth
breathing in your patients as early as
possible to enhance breathing biomechanics and enhance exercise inhalation
and exhalation muscle strength. Perio Reports Vol. 24, No. 9
Perio Reports provides easy-to-read research summaries on topics of specific
interest to clinicians. Perio Reports research summaries will be included in each
issue to keep you on the cutting edge of dental hygiene science.
www.hygienetown.com
Okuro, R., Morcillo, A., Ribeiro, M., Sakano, E., Conti, P., Ribeiro, J.:
Mouth Breathing and Forward Head Posture: Effects on Respiratory
Biomechanics and Exercise Capacity in Children. J Braz Pneumol
37(4):471-479, 2011.
Mouth Breathing Changes Facial Morphology
In the oral cavity, a balance of functions should exist
between breathing, suckling, swallowing, chewing and
speech. Debate still exists about the impact of mouth breathing on development of orofacial structures. Despite the fact
that bone is the second hardest substance in the body, it is
susceptible to small, continuous forces from muscles. Mouth
breathing results in changed tongue positioning from the
palate to the floor of the mouth, resulting in inferior positioning of the mandible and changes in neck and facial musculature changing dental and facial characteristics.
Researchers at the Medical University in Lucknow, India
evaluated cephalometric tracings to compare landmarks in a
group of 100 children ages six to 12 years. Mouth breathers
accounted for 54 children in the group and nose breathers
accounted for 46 subjects. Significant differences were evident
between nose breathers and mouth breathers for facial development. Mouth breathers showed significant increase in facial
height, mandibular plane angle and angle of the mandible.
The palatal plane to mandibular plane angle was greater in
mouth breathers. There was mandibular retrusion in relation
to the spine in mouth breathers compared to nose breathers.
At as early as three years of age, mouth breathing and low
tongue posture produce an elongation of the lower anterior
facial height, which is more commonly detected after age
five. Posterior rotation of the mandible in mouth breathers
leads to the increased facial height. Palatal changes are also
evident as the maxillary arch narrows and the height of the
palate increases.
Clinical Implications: Early intervention with mouth breathers will prevent morphological changes associated with
Long Face Syndrome. Malhotra, S., Pandey, R., Nagar, A., Agarwal, S., Gupta, V.: The Effect of Mouth Breathing on Dentofacial Morphology of Growing Child. J of Indian Soc Pedod Prev Dent 30(1): 27-31, 2012.
continued on page 118
116
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 53 on card
hygiene and prevention
perio reports
continued from page 116
Mouth-Breathing Kids Have Bad Breath
Mouth breathing results in many facial changes in a
growing child, including changes in the dental arches,
tooth position, facial bone structure, palatal development, chin positioning and lips. Those who mouth
breathe complain of dry mouth, halitosis, restless sleep,
snoring, drooping shoulders, daytime sleepiness, flaccid
lips and protrusion of the anterior teeth.
Researchers at the Metropolitan University de Santos
in Sao Paulo, Brazil evaluated bad breath in a group of
55 children between the ages of three and 14 years. Of
this group, 22 were mouth breathers and 33 were nose
breathers. Nose or mouth breathing was determined by
clinical evaluation of the following signs: long face,
drooping eyes, thin upper lip, dry lips, hypotonic lips,
inverted lower lip, narrow nostrils, high-arched palate,
inadequate lip seal and anterior open bite. A mirror test
was used placing a flat double-sided mirror under the
nostrils to see vapor formation from the nose or the
mouth. A water test involved having the children hold
water in the mouth without swallowing for three minutes. If unable to keep the mouth closed for three minutes, they were considered a mouth breather.
Halitosis was measured using a portable sulfite
monitor. Of the 20 children with no odor, 18 were
nose breathers and 2 were mouth breathers. Of the 35
with bad breath, 15 were nose breathers and 20 were
mouth breathers. Mouth breathing significantly influenced bad breath.
Humming Increases Nasal Nitric Oxide Production
Nitric oxide is produced and released in the nasal airways during nose breathing. It is released from nasal tissue
and inhaled into the lungs. Nitric oxide is not produced or
released with mouth breathing. In healthy sinuses nitric
oxide levels are high. Congested airways lead to lower levels of nitric oxide and mouth breathing. Nitric oxide is
important for many things including smooth muscle relaxation and vasodilation.
Researchers at the Karolinska Institute in Stockholm,
Sweden hypothesized that humming would produce oscillating airflow-enhancing nasal airflow, resulting in higher
release of nitric oxide in the nasal passages. Ten healthy,
non-smoking subjects participated in the study measuring
nitric oxide in exhaled air from both the nose and the
mouth. Measurements were taken at rest with gentle
breathing and again while humming.
Humming resulted in a 15-fold increase in nasal nitric
oxide levels compared to relaxed breathing. During relaxed
nasal breathing, nitric oxide levels were 189 nl/minute and
increased to 2,818 nl/minute with humming. Nitric oxide
levels with relaxed mouth breathing averaged 103
nl/minute and were 104 nl/minute for mouth breathing
and humming. Air needs to pass through the nasal passages
to trigger the release of nitric oxide. With mouth breathing
and humming there was no increase in nitric oxide levels.
Nose breathing produces more nitric oxide than mouth
breathing. When humming is added to nose breathing,
nitric oxide production increases significantly.
Clinical Implications: Encourage mouth breathing
patients to hum with the tongue resting on the palate to
ensure nose breathing. This will increase nitric oxide
production while practicing lips together posture,
tongue on the palate nasal breathing. Clinical Implications: Check to see if your child
patients mouth breathe and have bad breath.
Changing the mouth breathing to nose breathing
may eliminate the bad breath and provide many
other benefits as well. Motta, L., Bachiega, J., Guedes, C., Laranja, L., Bussadori, S.: Association between Halitosis and
Mouth Breathing in Children. Clinics (Sao Paulo) 66 (6): 939-942, 2011.
118
SEPTEMBER 2012 » dentaltown.com
Weitzberg, E., Lundberg, J.: Humming Greatly Increases Nasal Nitric Oxide. Am J Respir Crit Care
Med 166(2):144-145, 2002.
hygiene and prevention
perio reports
Snoring Associated with Craniofacial Development
Children who nose breathe show normal craniofacial growth. Those who mouth breathe show
abnormal craniofacial development, malocclusion,
narrowing and deepening of the palate, tendency
toward open bite and/or cross bite, protrusion of
maxillary incisors and changes in head position
relative to the neck.
Researchers at the University
of Sao Paulo in Brazil evaluated
27 children ages seven to 14 years
to determine any relationship
between cephalometry used by
orthodontists and polysomnography, the gold standard when testing for obstructive sleep apnea.
Fifteen of the children were
mouth breathers and 12 were nose breathers. Mouth
breathing was identified by parents reporting child
sleeping with an open mouth, dribbling on the
pillow three times or more per week or adenoid
obstruction identified with nasofibroscopy.
Infant Sleep Disordered Breathing Leads
to Childhood Behavior Problems
Sleep disordered breathing (SDB) ranges from snoring to
obstructive sleep apnea (OSA), with mouth breathing as a
common clinical sign. SDB occurs in children as young as six
months. SDB causes abnormal gas exchange, interferes with
sleep and restorative processes, and disrupts cellular and
chemical balance. Dysfunction of the prefrontal cortex
impairs attention, executive function, behavioral inhibition,
self-regulation of affect and arousal, and other socio-emotional behaviors. Neurological effects may be irreversible as
sleep is so critical to brain development in infants and
young children. Attention-deficit/hyperactivity disorder is
also linked to SDB.
Three hallmark signs of SDB are snoring, mouth breathing and witnessed apnea. Researchers from Albert Einstein
College of Medicine in Bronx, New York, and University of
Overnight polysomnograms were performed on all
the children.
All of the mouth breathers snored and only one
child in the nose breathing group snored. The
mouth breathers all had lower oxygen saturation levels than nose breathers. The mouth-breathing children were more likely to have a retruded mandible
than nose breathers. Other measurements showed
mouth breathers to have more inclined occlusal
planes, steeper mandibular planes and smaller airways compared to nose breathers. Snoring was the
most important variable associated with abnormal
craniofacial morphology. Early detection and treatment of mouth breathing can change the child’s
facial development, oxygen saturation to brain and
muscles, and general quality of life.
Clinical Implications: Dentists and dental
hygienists should be checking children for mouth
breathing and snoring, which are signs of potential developmental and sleeping problems. Juliano, M., Machado, M., de Carvalho, L., Zancanella, E., Santos, G., Prado, L., Prado,
G.: Polysomnographic Findings are Associated with Cephlometric Measurements in MouthBreathing Children. J Clin Sleep Med 15(5): 554-561, 2009.
Michigan in Ann Arbor, Michigan, analyzed the data from
more than 11,000 children in the Avon Longitudinal Study
of Parent and Children. A total of 14,541 pregnant mothers in the county of Avon in the southwest of England
entered this study between April and November of 1991.
Data up to age seven was analyzed. Mothers reported on
SDB symptoms and completed strengths and difficulties
questionnaires at ages four and seven. The incidence of SDB
in this group was identified in clusters accounting for 55
percent of the sample. The clusters reflected the onset and
end or not of the SDB symptoms. Early SDB symptoms had
a strong, persistent effect on subsequent behavior problems
in the children.
Clinical Implications: Begin checking infants as young as six months for sleep disordered breathing, in particular
mouth breathing and snoring. Bonuck, K., Freeman, K., Chervin, R., Xu, L.: Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 years. Pediatrics 129(4): e857-e865, 2012.
119
dentaltown.com « SEPTEMBER 2012
hygiene and prevention
profile in oral health
by Trisha E. O’Hehir, RDH, MS
and Amy Francis, RDH, OM
Abstract
Nose breathing and mouth breathing both bring
oxygen into the lungs but with different consequences
and different oxygen absorption levels. Dental and dental hygiene education in the past touched only briefly on
problems associated with mouth breathing, primarily dry,
inflamed oral tissues around maxillary anterior teeth. There
is now evidence that mouth breathing has far more serious
and long-lasting implications than drying of oral tissues. A
simple five-step screening process identifies factors affecting
nasal breathing.
Objectives
At the end of this program, participants will be able to:
1. Understand physiologic differences between nasal breathing and mouth breathing.
2. Describe symptoms of mouth breathing.
3. Understand the impact of mouth breathing on malocclusion.
4. List the five steps in the mouth-breathing screening exam.
5. Recognize the role of RDHs in preventing mouth breathing.
120
SEPTEMBER 2012 » dentaltown.com
hygiene and prevention
profile in oral health
Humans are designed to be nose breathers, but for a variety
of reasons the switch can be made to mouth breathing, with serious consequences. The nose and mouth have different functions. Each nostril functions independently and synergistically
to filter, warm, moisturize, dehumidify and smell the air. It’s like
having two noses in one. Breathing through the mouth provides
none of these benefits of nose breathing and a lengthy list of
adverse effects. The problems associated with mouth breathing
begin in the mouth by changing the tongue rest position, thus
changing the normal growth pattern of the palate, both maxillary and mandibular jaws and the airway.1 Inadequate skeletal
growth leads to crowded teeth, a high-vaulted palate and abnormal occlusion, called the Long Face Syndrome. In mouth
breathers, the tongue rests down and forward, not in the palate
as it should, leading to tongue thrust, abnormal swallowing
habits and speech problems. A significant problem with mouth
breathing is reduced oxygen absorption leading to a cascade of
sleep, stamina, energy level and ADHD problems. Dryness of
the oral and pharyngeal tissues from mouth breathing leads to
inflamed tonsils, tonsil stones, dry cough, swollen tongue, halitosis, gingivitis and caries. Mouth breathers chew with their
mouths open, swallowing air, leading to gas, bloating, flatulence
and burping. Lips become flaccid with mouth breathing because
they don’t close regularly to provide the necessary lip seal.
Dental and dental hygiene education in the past touched
only briefly on problems associated with mouth breathing, primarily dry, inflamed oral tissues around maxillary anterior teeth.
Adding to that knowledge, there is now evidence that mouth
breathing has far more serious and long-lasting implications
than drying of oral tissues.
Many misconceptions about mouth breathing persist today.
In some circles, mouth breathing and nose breathing are thought
to be equivalent and in athletics, mouth breathing is still
assumed to be better than nose breathing. Assuming that mouth
breathing and nose breathing are no different ignores basic physiologic facts about the exchange of oxygen and carbon dioxide.
Today professional athletic teams are being coached to train with
their mouths closed, focusing on nose breathing to increase
endurance, stamina and muscle memory. Another misconception is assuming more oxygen is absorbed with a big inhale
through the mouth doesn’t take into consideration the fact that
oxygen is absorbed on the exhale, not the inhale. Sleep medicine
writings assume mouth breathing and sleep apnea are not connected, which is not supported by scientific evidence. Mouth
breathing and obstructive sleep apnea (OSA) are connected.4
Dental professionals are in a perfect position to evaluate
mouth and nose breathing, check for tongue rest position and
intervene early with young children to assure normal skeletal
development and help mouth breathers of all ages become nose
breathers. Understanding the physiology of breathing and
implementing a simple five-step screening system raises awareness of the significance of this problem and provides an opportunity to implement far-reaching changes in patients’ lives.
Mouth Breathers are prone to:
nasal congestion
watery, itchy eyes
runny nose
allergies
asthma
enlarged tonsils
bad breath
tonsil stones
dry cough
snoring
sleep disturbances
fatigue
low energy level
ADHD
tongue thrust
abnormal swallowing habits
aerophagia
bloating
burping
flatulence
hiccups
acid reflux
heartburn
poor palate development
crooked teeth
recessive chin
Long Face Syndrome
speech problems
weak, flaccid lips
fibromyalgia
chronic fatigue syndrome
silent aspiration
pneumonia
bronchitis
bed wetting
frequent urination at night
Physiology of Breathing
The purpose of breathing is to deliver oxygen to the cells
of the body and to remove excess carbon dioxide. The body
requires approximately two to three percent oxygen and the
atmospheric level is 21 percent so there is no need to store oxygen. The body’s requirement for carbon dioxide is 6.5 percent
and the atmospheric content is 0.03 percent, so the body has to
produce and store carbon dioxide in the lungs and blood.
Carbon dioxide is produced as a byproduct of exercise and
digestion of food. Carbon dioxide has several functions in the
body: facilitate release of oxygen from hemoglobin, trigger
breathing, maintain blood pH by buffering with bicarbonate or
carbonic acid and prevent smooth muscle spasms. All of these
functions are reduced or impaired in mouth breathers.
Breathing is subconscious with each inhale determined not
by the need for oxygen, but by the level of carbon dioxide in the
alveoli of the lungs and blood. As carbon dioxide builds up in
the body, the pH of the blood drops. This pH change is monitored by chemoreceptors in blood vessels that will signal the
brain to trigger the next breath. Normal respiration follows a
gentle wave pattern with 10 to 12 breaths per minute, providing
five to six liters of air per minute. Mouth breathers often have a
respiration rate above 12 breaths per minute and those with
asthma and serious medical conditions have rates of 20 respirations per minute or higher.
Breathing through the nose controls the amount of air taken
in and, more importantly, controls the amount of air exhaled.
1.
4.
Souki, B., Pimenta, G., et al: Prevalence of malocclusion among mouth breathing in children: do expectations meet reality? Int J Pediatr Otorhinolaryngol 73(5):767-773, 2009.
Juliano, M., Machado, M., et al: Polysomnographic findings are associated with cephalometric measurements in mouth-breathing children. J Clin Sleep Med 15(5):554-561, 2009.
continued on page 122
121
dentaltown.com « SEPTEMBER 2012
hygiene and prevention
profile in oral health
continued from page 121
Oxygen is absorbed on the exhale, not on the inhale. The backpressure created in the lungs with the slower exhale of nose
breathing compared to mouth breathing allows more time for
the lungs to transfer oxygen to the blood. The exchange of oxygen in the blood requires the presence of carbon dioxide.
Approximately 98 percent of oxygen is carried in hemoglobin.
Carbon dioxide levels need to be at five percent in the alveoli
and arterial blood before the oxygen molecules are released from
hemoglobin to reach brain and muscle cells. Lower than five
percent carbon dioxide levels lead to an elevation in blood pH
and the oxygen “sticks” to the hemoglobin, this is the Bohr
Effect, first described in 1904 by physiologist Christian Bohr.
Nitric oxide is released in the nasal cavity and inhaled with
nose breathing. Nitric oxide increases the efficiency of oxygen
exchange. With nitric oxide, blood oxygen increases by 18 percent. Mouth breathing bypasses the nitric oxide.
Seventy-five percent of the inhaled oxygen is exhaled.
During strenuous exercise, 25 percent of the oxygen inhaled is
exhaled. Mouth breathing to take in more air does not increase
the level of oxygen in the blood, which is already 97-98 percent
saturated. Mouth breathing with big breaths actually lowers the
carbon dioxide level in the lungs and the blood leading to lower
levels of oxygen released from the hemoglobin to body cells.
Taking in more air doesn’t deliver more oxygen to the cells of the
body. A balanced pH of the blood is achieved with proper oxygen-carbon dioxide exchange. Nasal breathing will increase oxygen in the lungs, blood and cells. Excessive carbon dioxide loss
through mouth breathing decreases oxygen levels in the lungs,
blood and cells.
mouth. Others believe they are nose breathers, but if you watch
them, their mouth is open most of the time. Sitting still, they
might have their mouth closed, but if they get up and walk
across the room, their mouth is open. Telltale signs of mouth
breathing are an addiction to chap stick or lip balm. An open
mouth leads to drooling, both awake and asleep, causing
chapped lips and a tendency for mouth breathers to lick their
lips frequently. Closed mouth lip seal is efficient at keeping
saliva in and air out but chronic mouth breathers find it very difficult to hold their lips together. Mouth breathing at night
causes drooling and dries the oral tissues so the mouth, teeth,
tissue and throat are all dry upon waking. If someone wakes
with a dry mouth, he or she is likely a mouth breather at night,
which means he or she is also mouth breathing during the day.
The tongue normally rests against the palate, without touching the teeth. With mouth breathing, the tongue drops down
and forward. It might in fact be that the down and forward
tongue position triggers mouth breathing. Mouth breathing is
impossible with the tongue resting against the palate. A simple
tool to self-test for mouth breathing is the square plastic bag
closers used on plastic bread bags. Place the square plastic chip
between the lips and have the person go about their daily activities. If the chip falls out, they are mouth breathing.
Mouth Breathing – What Goes Wrong
Five-step screening for mouth breathing
122
SEPTEMBER 2012 » dentaltown.com
»
Several things go wrong with mouth breathing, beginning
with oxygen/carbon dioxide exchange, the change in tongue rest
position and swallowing air. The low carbon dioxide levels associated with mouth breathing trigger the activation of breathing
faster than usual, leading to over breathing or hyperventilation.
Signs of Mouth Breathing
With less oxygen being delivered to the brain, muscles and all
Determining if someone is a mouth breather is not always the cells of the body, the body functions less than optimally.
easy. Some people admit they always breathe through their Sleep is often disturbed and of poor quality, leaving the mouth
breather tired in the morning and feeling fatigued mid-afternoon. Attentiondeficit hyperactivity disorder (ADHD)
is also linked to mouth breathing.11 This
dryness and lack of air filtration in
Lips together at rest – yes or no?
mouth breathing causes enlarged and
inflamed tonsils and adenoids and
increased risk of upper respiratory tract
Nasal breathing – yes or no?
infections. Lower levels of carbon diox(check each nostril for air intake)
ide cause smooth muscle spasms associated with gastric reflux, asthma and
Tongue posture at rest – up, down, middle?
bedwetting. Smooth muscle is found
throughout the body in the respiratory
system,
digestive system, circulatory
Frenum length – adequate or tight? (mouth open wide should measure three fingers
system,
all
hollow organs and all tubes
stacked vertically, with the tongue on the roof of the mouth, opening is two fingers.
and
ducts.
Less than that indicates a tight lingual frenum.)
The tongue resting in the palate
provides
passive pressure, stimulating
Palatal width – adequate or narrow? (measure with a cotton roll, cross-arch on the
stem
cells
located in the palatal suture
palate between bicuspids.)
and within the periodontal ligaments
hygiene and prevention
profile in oral health
around all the teeth to direct normal palatal growth. When the
tongue rests in the palate, the teeth erupt around the tongue,
producing a healthy arch form. The lateral pressures from the
tongue counters inward forces from the buccinator muscles.
When the tongue is down and forward, the buccinator muscles
continue to push unopposed, causing the upper arch to collapse.
Children who mouth breath have an underdeveloped, narrow
maxilla with a high vault.2 They develop a retrognathic
mandible and generally have a long face. Harvold et al. surgically blocked noses in monkeys and they all developed malocclusions from mouth breathing.3 Mouth-breathing-related
problems of skeletal development will set children up for
obstructive sleep apnea later in life.4
It might seem logical that mouth breathing occurs because
the nose is congested, but that is not always the case. The brain
of a mouth breather thinks carbon dioxide is being lost too
quickly from the nose and stimulates the goblet cells to produce
mucous in the nose to slow the breathing.5 This creates a viscous
circle of mouth breathing triggering mucous formation, nasal
passage blocking, leading to more mouth breathing. So in fact,
mouth breathing can cause nasal congestion leading to more
mouth breathing.
In some cases, mouth breathing is caused by ankyloglossia,
or a tight lingual frenum keeping the tongue from effectively
moving in the mouth to assist in chewing and swallowing and
comfortably resting on the palate.6 Unless a frenectomy is done,
mouth breathing will continue. Ankyloglossia can be diagnosed
and treated in the first few days after birth.7 However, many
cases are ignored until significant problems have developed.
Early intervention prevents subsequent problems.8
Changing from Mouth to Nose Breathing
Bringing a person’s mouth breathing to his or her attention
starts the process of breaking the habit. Some people will change
back to nose breathing when made aware of it. To remind people to keep their lips together, paper tape is often used by
breathing coaches. It may sound strange, but easy-to-remove
paper tape helps people experience the many benefits of nose
2.
3.
5.
6.
7.
8.
9.
10.
11.
Malhorta, S., Pandey, R., et al: The effect of mouth breathing on dentofacial morphology of growing child.
J Indian Soc Pedo Prev Dent 30(1):27-31, 2012.
Harvold, E., Tomer, B., Vargervik, K., Chierici, G.: Primate experiments on oral respiration. Am J
Orthod 79(4):359-372, 1981.
Bresolin, N., Shapiro, P., et al. Mouth breathing in allergic children: it’s relationship to dentofacial development. Am J Orthod 83 (4):334-340, 1983.
Olivi, G., Signore, A., Olivi, M., Genovese, M.: Lingual frenectomy: functional evaluation and new
therapeutical approach. Eur J Paediatr Dent 13: 101-106, 2012.
Fiorotti, R., Bertolini, M, Nicola, J., Nicola, E.: Early lingual frenectomy assisted by CO2 laser helps
prevention and treatment of functional alterations caused by ankyloglossia. Int J Orofacial Myology 30:
64-71, 2004.
Suter, V., Bornstein, M.: Ankyloglossia: facts and myths in diagnosis and treatment. J Perio 80: 12041219, 2009.
Cartwright, R., et al. Snoring Control Using a New Tongue-Retaining Oral Appliance” Journal of Sleep,
Vol. 27, 2004, 412.
Singh, G., Lipka, G.: Case Report: introducing the wireframe DNA appliance. J Am Acad Gnathol
Ortho 26(4): 8-11, 2009.
Bonuck, K., Freeman, K., Chervin, R., Xu, L.: Sleep-disordered breathing in a population-based cohort:
behavioral outcomes at 4 and 7 years. Pediatrics 129(4): e857-e865, 2012.
breathing for themselves. Be sure they can breathe through their
nose before taping. Best to test this during the day before trying
it overnight while sleeping. Try the tape yourself before suggesting it to a patient. A variety of oral appliances are available that
position the tongue to the roof of the mouth, close the lips and
encourage nose breathing.9 In many cases, the tongue might
need to be exercised since it’s been laying on the floor of the
mouth and doesn’t have the stamina to rest on the palate all day
or all night. Orofacial myofunctional exercises are important at
this stage. These exercises are essential for those receiving a
frenectomy to treat ankylosglossia. In adult cases of life-long
mouth breathing, orthodontics to expand the palate may be necessary to make room for the tongue.10
Screening for mouth breathing is easy and takes very little
time with the five-step process. The first three steps are easily
answered with observation and questions to the patient. First,
are the lips together, second, can the person breathe through
their nose and third, where is their tongue at rest? The next two
steps require measurement, first the mouth opening and second
the mouth open with the tongue touching the roof of the
mouth. Most people can open the width of three fingers stacked
vertically. With the tongue on the roof of the mouth, they
should be able to open at least two fingers. Less than that and
there is a problem with the lingual frenum, either ankyglossia or
a tight lingual frenum. The last screening step is to measure the
maxillary cross arch distance between the bicuspids. The distance should be equal to a standard cotton roll.
The earlier mouth breathing is recognized and converted to
nose breathing, the fewer and less serious the problems will be.
Dental hygienists are the ideal dental professionals to screen for
mouth breathing. Despite the fact that people are more often
asked to open their mouths in a dental office, checking for a
closed mouth is essential to oral and general health. Author Bios
Trisha O’Hehir is currently the Editorial Director for
Hygienetown.com and Perio Reports. She received her
education at the University of Minnesota and her fourdecade career has included roles as clinician in the USA and Zurich,
Switzerland, faculty at the Universities of Minnesota, Washington,
Arizona and Louisville, international speaker, writer, instrument
designer, inventor and entrepreneur.
Amy Francis is both a dental hygienist and an orofacial
myologist, teaching people how to breath, chew and swallow. Amy was working in clinical practice when she went on
for more training by completing her orofacial myology certification program in 2010 in Los Angeles. Amy spoke at the
2011 Townie Meeting on the importance of nose breathing.
Amy lives and works in Lake Havasu, Arizona.
123
dentaltown.com « SEPTEMBER 2012
product
profile
Prophies, Parafunction and Your Patients
by Anita McMillen, RDH
Over the past 25 years, I’ve seen patients in my chair for prohys or SRP that exhibit the artifacts of parafunction. Whether
I’m noting the chart about a fractured crown on #3 or wear
facets on anteriors, the one constant is that patients are almost
never aware of their clenching or grinding. After I notify
patients that they brux, they typically tell me that they don’t. My
observation is usually met with a chorus of ‘no one has ever said
they heard me grind my teeth.’ Then I use my mirror or
the monitor to show them what I’m seeing.
Sometimes I’ll ask them to clench their
teeth together as hard as they can and
hold that position. Then I’ll ask what
they heard. After that, most patients
accept they are indeed parafunctioners.
After they’ve arrived at that determination, I’ll begin asking about symptoms
such as TMD, headaches, migraines and
face, neck or head pains that are often
associated with parafunction. Most
patients don’t see any correlation
between their bruxism and painful
symptoms, so I help connect the dots
for them.
I ask patients if they have had a night
guard in the past. I find that they need to be educated on why
they are wearing an occlusal guard while they sleep. Oftentimes,
patients balk when I mention occlusal guards, complaining that
they’re too bulky and cumbersome. This allows me to go into
depth about the NTI-tss Plus. I discuss its small size, unique
design and benefits experienced from wearing it. I tell them that
it usually only covers four teeth so it’s easy to wear, and also that
it’s different from traditional night guards because it guarantees
canine and posterior separation not only during excursions but
also during a centric clench. I usually ask them to clench their
teeth together with their hands on their temples. Doing this,
they can feel the muscles tense and bulge beneath their fingers.
Then I have them do it again with a tongue depressor between
their central incisors. They feel the decreased intensity of the
clenching and you can almost see the light bulb go off for them.
Sometimes patients take issue with the cost of an appliance.
Unfortunately, too often, splints are not covered by insurance. I
assure patients that the NTI’s unique design is durable, easy to
wear and might not only alleviate their symptoms but also
reduce the need for expensive dental work in the future. It will
protect their teeth and restorations, decreasing the need for
pricey crowns and future root canals.
I am able to allay many of their concerns by
sharing my own experience with the NTI.
Much of my life I’ve suffered from facial, neck
and head pain. Throughout the years I tried
many different treatments, including mouth
guards, with little to no relief of my symptoms. My pain was caused from nocturnal
clenching and the full coverage guards did
not relieve the pain. Like many other
clenchers, these full coverage appliances
made my symptoms worsen. About five
years ago, I heard about the NTI-tss Plus
and Dr. Greg Hillery prescribed one for me.
Almost overnight, my pain was eliminated.
It wasn’t too long before I
realized that most of my clenching occurred during the day
while working chairside with
patients. Knowing that, I started
wearing both a nighttime and
daytime appliance. This is very
helpful when patients comment
that they “cannot wear an appliance during the day because their
job dictates that they speak on the phone with customers.” At
this point I ask them if they are having a hard time understanding my speech and I lower my mask to show them I am wearing
my daytime NTI.
For me the NTI has been a godsend. I’m still practicing and
I wear it daily. Using my own experience and showing my
patients the actual device in my mouth helps convince them that
it truly does bring relief and it won’t affect their daily lives in a
negative way. Author’s Bio
Anita McMillen graduated from the New Hampshire Technical Institute, Dental Hygiene Program and now works as a periodontal therapist in
Concord, New Hampshire. Her greatest passions are strong family bonds and providing the best possible care for her patients. Hygienetown
online participation has provided Anita with a wealth of knowledge and expertise. Anita can be reached at needardh@hotmail.com.
124
SEPTEMBER 2012 » dentaltown.com
FREE FACTS, circle 48 on card
hygiene and prevention
message board
Sleep Apnea and Sleep Disordered
Breathing Cause More than Hypoxemia
»
Hygienetown Message Board > Etiology and Diagnosis > Sleep Apnea/Snoring > Sleep Apnea and Sleep Disordered Breathing Cause More than Hypoxemia
Howard
Member Since: 03/28/00 Post: 1 of 18
Hygienists discuss the importance of sleep apnea care to a patients’ overall health, and their role in it.
A recent study in the Journal of the American Medical Association claims that aside from
diabetes, high blood pressure, heart attacks and strokes, sleep apnea might be one of the
causes of dementia. This sleep apnea and dementia link can be explained through
hypoxemia, which is a drop in oxygen levels in the blood, often caused by the obstruction
of breathing that is the main symptom of sleep apnea. In a sample size of 298 women,
approximately one-third reported sleep-disordered breathing, including 15 episodes of
hypoxemia (an occurrence of a drop in the level of oxygen in the blood). Over a period of
five years, almost 45 percent of that third of the original sample size developed mild
cognitive decline or dementia. The researchers concluded that the cognitive decline was
related to the hypoxemia experience. JUN 19 2012
Trisha O’Hehir Member Since: 05/22/03 Post: 5 of 18
Regarding obstructive sleep apnea (OSA), hygienists can begin by checking patients
for mouth breathing and tongue resting down and forward – not up on the palate
where it should be. For those taking sleep courses, add the Buteyko Breathing course –
it’s fascinating and you can help so many people before they develop sleep problems,
from kids to old folks. Anyone else taken the Buteyko Breathing course taught by Patrick
McKeown from Ireland? JUN 26 2012
Healthy Smiles Member Since: 10/25/11 Post: 6 of 18
We have our own home sleep screenings but we also work very closely with some sleep
centers and physicians. We had to make a separate business, I think due to insurance
payments. Seeing the patients after they get their appliance and hearing how great they feel
is amazing! I hope this spreads through the dental community because we really can catch it
early. There have been children as well that suffer from what they think is ADHD but we
refer to ENT to get tonsils and adenoids taken out, and like magic, they are off the meds! JUN 26 2012
batkinson Member Since: 06/01/12 Post: 8 of 18
We’re convinced that dental hygienists are the front line in the battle against OSA. No
other health-care professional has expertise in oral/soft palate anatomy and the access to
patients like the dental hygienist. Primary care has no financial incentive to screen for OSA
and most aren’t familiar with the subjective/objective screenings, or the anatomical signs.
(I’ve asked MDs about the Mallampati score and most have never heard of it.)
When we set up a practice to begin providing dental sleep services, we train the hygienists on the subjective screenings (Epworth, STOP-BANG, HRQOL) and anatomical signs
of OSA. It’s all captured on a Web-based tablet computer. The results are displayed
graphically for the patient. This two-minute screening might be the most powerful tool for
helping combat the OSA epidemic. I hope more hygienists take an interest in dental sleep.
We need more health-care providers like you to help us combat OSA. JUL 7 2012
126
SEPTEMBER 2012 » dentaltown.com
hygiene and prevention
message board
Interesting and timely topic. Earlier this year I took the Orofacial Myofunctional
Therapy (OMT) Course offered by Joy Moeller in San Francisco. There was discussion
about OSA and how OMT can be helpful in treating this disorder.
Roger Price, a respiratory physiologist, wrote a paper on “Sleep Apnea and Dysfunctional
Breathing” (2007) and is of the opinion that OSA is very frequently misdiagnosed in many
individuals. People who have “OSA” more likely have dysfunctional breathing in that they
are taking shallow breaths, often through the mouth, and are therefore required to breathe
many times per minute more than if one were deep breathing. His premise is that if a
person can be trained to breathe deeply and change their inhalation habits, the snorting and
gasping for air while sleeping will disappear, and he has a lot of research to back that up.
He also states that many asthma patients were successfully treated with breathing
therapies. It is not stated in the literature if he used Buteyko Breathing or not but that would
be my guess. Doris Waite, RDH, OMT
singtenor Member Since: 02/11/11 Post: 10 of 18
JUL 7 2012
search Sleep Apnea Hypoxemia
»
Find it online at: www.dentaltown.com
FREE FACTS, circle 43 on card
127
dentaltown.com « SEPTEMBER 2012
dentally incorrect
humor
At a towing company:
“We don’t charge an arm and a leg. We want tows.”
On a septic tank truck sign:
On an electrician’s truck:
“We're #1 in the #2 business.”
At a proctologist’s door:
“To expedite your visit, please back in.”
On a plumber’s truck:
“We repair what your husband fixed.”
“Let us remove your shorts.”
At an optometrist’s office:
“If you don’t see what you're looking for,
you’ve come to the right place.”
Outside a muffler shop:
“No appointment necessary. We hear you coming.”
At a tire shop in Milwaukee:
“Invite us to your next blowout.”
In a veterinarian’s waiting room:
“Be back in five minutes. Sit! Stay!”
On a maternity room door:
“Push. Push. Push.”
In the front yard of a funeral home:
“Drive carefully. We’ll wait…”
Sign over a gynecologist’s office:
“Dr. Jones, at your cervix.”
At a Chicago radiator shop:
“Best place in town to take a leak.”
On a plastic surgeon’s office door:
n
“Hello. Can we pick your nose?”
FREE FACTS, circle 18 on card
128
SEPTEMBER 2012 » dentaltown.com
CREDIT CARD PROCESSING PROGRAM
7)2%,%33s2%4!),s).4%2.%4s-!),/2$%2s$)!,0!9
MAJOR NEWS!
WHOLESALE RATES GO AS LOW AS
05
%
.
EXAMPLE:
PROCESSING $10,000 = $5 in fees!
Process Credit
Cards with your
Smart Phone & Tablet
We Will Give You
$
500
If We Can’t Beat Your Current
Credit Card Processing Rate*
*
,Ê/, "*/" ,
/, Ê
EÊ* Ê*
UÊ ,Ê*>ViiÌ]Ê
Ài`ÌÊ
>À`Ê/iÀ>
Wireless/Land Line / High Speed / Dial-Up
UÊ
UÊ
UÊ
UÊ
UÊ
>ÃÞÊ-iÌÕ«ÊÊ+ÕVÊ««ÀÛ>
Ìi}À>ÌiÊÜÌ
ÊÞÕÀÊVÕÀÀiÌÊ*"ÀiiÊ*>«iÀ
ÊÃiÌÕ«Êvii
iVÊ-iÀÛViÃÊÛ>>Li
Ê>ÀÞÊ/iÀ>ÌÊiiÊ
with your current processor? NAB will
reimburse your business up to $295*
,
7,-/, FREE FACTS, circle 7 on card
www.nynab.com
ENROLL NOW - CALL A SPECIALIST TODAY!
866-481-4604
* some restrictions apply. Contact a NAB representative for Details. North America Bancard is a registered Independent Sales Organization/Merchant Service Provider
for HSBC Bank USA, National Association, Buffalo, NY and Wells Fargo Bank, N.A.,Walnut Creek, CA. American Express and Discover require separate approval.
FREE FACTS, circle 41 on card
Special Supplement to Dentaltown Magazine
An Excerpt From:
Guided Implantology Made Easy:
CEREC Integration
by Dr. August de Oliveira, page 20
What’s on Your Implant Tray?
page 6
1
.5
CE Credits
See Page 26
Tired of Price Increases on
Over-Priced Implants?
It’s Time for a Reality Check. Choose Implant Direct for...
Innovative Products. Great Value. Highest Customer Satisfaction1
Legacy™3 Implant
All-in-1 Packaging includes implant, abutment,
transfer, cover screw & healing collar
$175 vs $6212 from Zimmer Dental
Reality Check
Zimmer Customers
Save $446 with Legacy3
SwishPlant™ Implant
All-in-1 Packaging includes implant, straight
abutment/transfer, cover screw & healing collar
$200 vs $7053 from Straumann®
Reality Check
Straumann Customers
Save $505 with SwishPlant
ReActive™ Implant
All-in-1 Packaging includes implant,
abutment, transfer & cover screw
$200 vs $6944 from Nobel Biocare™
Reality Check
Nobel Customers
Save $494 with ReActive
Implant Direct’s New Las Vegas Training Center
Implant Direct offers an extensive list of educational opportunities at its Las
Vegas Training Center with computers at each desk for Image Guided Surgical
Training, models/mannequins for hands-on training and a four chair dental office
for live surgical demonstrations.
Next Courses: September 13-15 | November 30-December 2
For information on courses and dates, both in Las Vegas and
throughout the US, visit Implant Direct's website or use your smart
phone to link directly to our Educational Section.
EARN 2 CE CREDITS FREE: View Online Lecture with 3D Graphic Videos & Answer 13 Test Questions
The Changing Reality of Implant Dentistry
Presented by Dr. Gerald Niznick
Technological advances and economic factors have shifted
the implant industry toward affordable care.
Continuing education credits may not apply toward license renewal in all states.
It is the responsibility of each participant to verify the requirement of his/her states licensing board(s).
Price comparisons based upon US list prices as of February 2012. All trademarks are property of their respective companies.
1Satisfied among Current and Former Users, by Company US Q211 Millenium Research Group A Decision Research, Inc. Company
2US list price for Tapered Screw-Vent with micro grooves, healing collar & straight abutment
3US list price for SLActive Tapered Effect implant, closure screw, healing abutment, solid abutment, transfer and comfort cap.
4US list price for NobelActive with cover screw, impression coping & abutment
Live surgical demonstrations not available at all courses
www.implantdirect.com | 888-649-6425
FREE FACTS, circle 57 on card
contents
special supplement
In 2009, The New York Times featured
an in-depth piece on how dental implants are “the new bridge” as
a long-term solution to irreplaceably damaged teeth. Today, that
analysis has never been truer. There is a reason, according to a
recent Dentaltown.com poll, nearly 50 percent of dentists now
place implants in their practice. And that reason is increased
demand. More and more patients are requesting implants over
bridges and removable partial or full dentures, and they are seeking out doctors who provide that service. And as an aesthetically
pleasing, natural-feeling, highly functional solution to lost teeth,
it’s no wonder. In this special supplement to Dentaltown
Magazine, we bring together some of the leading voices in
implant dentistry in order to provide you up-to-date information
on the growing field – information you can use to help bolster
your practice and standard of care.
Whether you are a pioneer in implant dentistry or still hesitant about integrating it into your practice, we hope you find
value in this exclusive implant supplement and encourage you
to jump onto Dentaltown.com to discuss your reactions with
your colleagues.
2
Howard Speaks
Dental Implants and the Law of
Unintended Consequences
6
What’s on Your Tray
What’s on Your Implant Tray?
10
Message Board
Congenitally Missing Laterals
14
Message Board
Implant Microsurgery:
Narrow Diameter Implants
15
Message Board
RPD Support Using BSB One Stage 3.3
and Rhein83 Sphero Block
17
Implants
Small Diameter Implants – An Aesthetic
Option to Replace Missing Maxillary Laterals
by Dr. Paresh B. Patel
20
Book Excerpt
Guided Implantology Made Easy
by Dr. August de Oliveira
26
Continuing Education
Top Implantology Breakthroughs for the GP
by Dr. Brady Frank with a special contribution by
Dr. Ryan Swain
1
dentaltown.com « SPECIAL SUPPLEMENT
howard speaks
column
»
Dental Implants and the Law
of Unintended Consequences
by Howard Farran, DDS, MBA, Publisher, Dentaltown Magazine
Ten years ago my oldest sister told me if you
study all the major religions, they don’t share a common name of a person, city or place; there is nothing that overlaps all major religions except for one
tenet, which we all familiarly know as “the Golden
Rule” (Check out Figure 1 on page 4). This single
most pervasive rule in the history of religion, in its
varying forms, has been a guide for thousands of
years, and has even been applied to professional
codes like the Hippocratic Oath. It’s the one rule
upon which we all seem to agree.
As doctors we try to do the best for our patients.
We’re supposed to. It’s our job, isn’t it?
Are you doing enough to encourage your
patients to get implants rather than a bridge? Bridges
are always the easy way out when patients want the
“what-the-insurance-covers” option, but are you
informing them of the long-term cost? Maybe you
should think about it this way: remove the financial
incentives. Is doing a bridge instead of a titanium
implant the way you think this patient needs to be
treated if insurance didn’t cover either? No. When
you prepare the adjacent teeth for a crown, you
know that in five years one of those two teeth might
need a root canal. If you’re going to do a root canal,
10 years later that same tooth might need to be
extracted. Your patient can’t brush or floss around a
bridge very well – so she won’t.
You also know that if this patient goes to a
nursing home some day, root surface decay
will completely wipe out everything we’ve
done to repair her teeth in about 18
months. She’s on medication that causes
xerostomia, she eats a diet of sweet and soft
food, and she might have terrible arthritis
and/or dementia so she won’t be able
to physically brush her own teeth. The
luckiest people in nursing homes are
those who have dental implants,
removable dentures or partials. There’s virtually no
oral health care in these
nursing homes. The
best you might get is
a candy striper who has to brush the teeth of 25
unruly octogenarians from time to time.
Are you really doing to others as you would have
done to yourself by placing a bridge? Sure your
patient’s insurance will pay for half of the work, but
in seven years it’s all going to be in a landfill. And
instead of replacing one tooth, you’re sentencing its
two adjacent teeth to death. It’s time to take a good
look at yourself in the mirror, doc, and stop the
madness. Unless the neighboring teeth are already
slated for crowns, a bridge is nowhere near as good
as an implant. You know this.
“We’re all creatures of habit, and
it’s your habits that can get you
into a rut. The easiest way to
break a habit is to force yourself
out and try something new.”
If you’re more concerned about your patient’s
pocketbook, you’re not thinking about their longterm dental health. There are at least 10 other countries that place more implants per 10,000 people
than the United States does. If you’re concerned that
it takes too much training, think about this: there
are more implants being placed in Brazil than here
– and their economy is a scant fraction of ours!
When I graduated from dental school in 1987, I
first learned how to place implants with Dr. Carl
Misch – and placing implants more than 20 years ago
was tough. All we had were 2D X-rays or panos.
Compared to the technology we have at our disposal
today, we were basically placing implants blind. You’d
take a look at a pano and see that you had an inch of
mandible, so you’d go ahead, numb up the area,
reflect back the tissue and you’d find you had only a
knife’s-edge worth. Today, 3D cone beam computed
tomography (CBCT) has changed the game for
implant placement. Anyone who has gone the CBCT
route has never turned back. A 2D X-ray doesn’t
find a periapical radioluncency until it’s about 3mm
continued on page 4
2
SPECIAL SUPPLEMENT » dentaltown.com
FREE FACTS, circle 58 on card
howard speaks
column
Find us on Facebook
continued from page 2
www.facebook.com/dentaltown
FIG. 1
RELIGION
FOUNDED
MEMBERSHIP
“GOLDEN RULE”
JUDAISM
2000 BC
13,866,000
“What is hateful to you, do not to your fellow man. That is the
entire Law, all the rest is commentary.” – The Talmud, Shab 31A
HINDUISM
1500 BC
793,075,000
“This is the sum of all the true righteousness: deal with the
others as thou wouldst thyself be dealt by.” – The Mahabharata
BUDDHISM
500 BC
325,275,000
“Hurt not others in ways that you yourself would find hurtful.”
– Undanavarqua:518
CONFUCIANISM
500 BC
5,086,000
“Surely it is the maxim of loving kindness: Do not unto others that
you would have not have them do unto you.” – Analects
CHRISTIANITY
0
1,955,229,000
“Do unto others as you would have done unto you.” – Luke 6:31
ISLAM
500 AD
1,126,325,000
“No one of you is a believer until he desired for his brother that
which he desires for himself.” – Sunnah
large, but on CBCT machines, they’re finding dead
teeth with a 1mm radiolucency – so not only are docs
better prepared to place an implant, their endodontic
diagnoses have shot up an amazing 20 percent!
What’s more amazing is there are CBCT software programs that will actually tell you the precise
implant that will fit. It will tell you that you can
only go 4mm in diameter and 18mm deep. There’s
no guesswork involved. Placing an implant in 2012
is three times easier than placing one in 1990.
It’s time to start telling your patients about the
decisions you and they are going to make when
you’re putting a treatment plan together. Do they
want something that’s going to stay with them for a
long time? Do they want something that is easier to
maintain but costs more, or do they want something
cheaper that they’ll have to throw away along with
other teeth and end up spending more money repairing in a few years? It’s time to start educating your
patients about the benefits of dental implants, and it’s
time to take money out of the equation. Who cares if
insurance pays for half of the bridge?! What if insurance paid half of a castration but nothing on a vasectomy? Would you recommend the castration to your
patient because Delta covers half of it?
Right now many of you are in this state of mind
where you’re trying to analyze whether or not you
should place implants, and I’m here to say it will be
one of the best professional decisions you could ever
make, and not even just for the reasons you think.
The law of unintended consequences comes into play
when you make the decision to start placing implants
4
SPECIAL SUPPLEMENT » dentaltown.com
and begin taking courses on Dentaltown.com. All of
a sudden you start going to seminars at dental meetings, and then you start traveling and taking hands-on
courses. And you start meeting people. And you start
chitchatting with doctors you’ve seen at a couple of
these seminars. And you start coordinating your travel
schedule with your new implant buddies. You go out
to lunch with them and you discuss implants and
start motivating each other. You learn how they run
their practices. You learn how their marketing plans
are performing. Your new buddy tells you what he’s
tracking with his practice management software,
which you have and had no idea it could do that! And
your whole professional life starts flourishing.
When I stepped out of my rut to learn about
implants I ended up meeting Dr. Jerome Smith,
who, when he places an implant today is like watching Beethoven compose a symphony. Through
Jerome Smith, I got turned onto missionary dentistry and through missionary dentistry I’ve learned
more about the meaning of life than through just
about anything I’ve ever done.
We’re all creatures of habit, and it’s your habits
that can get you into a rut. The easiest way to break
a habit is to force yourself out and try something
new. Stop hanging out with the same friends in the
same town you’ve been in since you were born. Get
out of the practice and get on Dentaltown.com, too.
Learn something you’ve never learned and implement it into your practice. Get out of your daily
grind. Take implant courses and become proficient.
Get a little mojo going! ■
FREE FACTS, circle 59 on card
what’s on your tray
feature
August de Oliveira, DDS
Encino, California
August de Oliveira is the author of “Implants Made Easy,” a book geared toward starting your first implant. He has just
released, “Guided Implantology Made Easy,” a book on the basics of guided implant surgery. Dr. de Oliveira has lectured
nationally on cone beam technology, dental implants and CAD/CAM technology. He has been a software beta tester for
Sirona, Blue Sky Bio, Anatomage and Implant Direct. He is currently a moderator and regular contributor to
Dentaltown.com’s Implantology and Mini Implants Forum. Dr. de Oliveira practices general dentistry in Encino, California.
To find out more about implants and Guided Surgery, go to www.implantsmadeeasy.com.
Implant Direct Complete Kit
Sirona CEREC
Guided Implant kit
Tissue Punches by Salvin
Sirona CEREC Guide Block
What’s on Your Implant Tray?
As clinicians, we’re always trying out new products and equipment. And before we buy, we will almost always
gauge what to purchase based on what colleagues and key opinion leaders use. Unfortunately, it isn’t very often we
actually get to see other dentists’ or specialists’ tray set ups. Here, we make it easy for you. In this installment of
“What’s On Your Tray?” Dentaltown Magazine takes a close-up look at two of your colleagues’ implant tray set ups
– these include the tools they love, the instruments they can’t practice without and the brands they prefer.
continued on page 8
6
SPECIAL SUPPLEMENT » dentaltown.com
FREE FACTS, circle 55 on card
what’s on your tray
feature
continued from page 6
Dan Holtzclaw, DDS, MS
Lone Star Periodontics & Dental Implants • Austin, Texas
Dr. Dan Holtzclaw is a native Texan, raised in Humble and Midland, Texas. After attending Texas A&M University, he graduated with honors from the University of Texas Health Science Center at San Antonio and was commissioned as an officer in
the United States Navy. While in the Navy, Dr. Holtzclaw attained the rank of Lieutenant Commander during 12 years of service at duty stations all over the world. During this time, Dr. Holtzclaw completed a one-year General Practice Residency (GPR)
at Naval Medical Center Portsmouth, Virginia and an additional three-year residency in periodontics at the National Naval
Medical Center (“The President’s Hospital”) in Bethesda, Maryland. Dr. Holtzclaw finished his naval career as the periodontist for the world famous U.S. Navy Blue Angels flight demonstration team.
Gauze, 4x4 and 2x2
Emesis basin with sterile saline
Monoject syringe
Glass dappen dish
Mouth prop
Anesthetic syringe
MIS implant kit
MIS bone compression kit
Wieder retractor
Minnesota retractor
Straight scissors
Russian forceps
Cotton forceps
Mirror
Explorer/UNC 15 probe
15c blade round handled scalpel
12b blade round handled scalpel
Orban gingivectomy knife
Buser periosteal elevator
Pritchard retractor
Corne forceps
Iris scissors
Hemostat
Castroviejo Needle Driver
Wiedelstadt chisel
Rhodes back action chisel
Sugarman file
Alveloplasty file
Tunnelling instrument
Curettes: 17, 11/12, 13/14, 7/8
Thank you to everyone who submitted your tray setups for our implants category!
If you’d like the chance to be featured in our What’s on Your Tray series, send us your photos and lists of the
items on your trays in the category below by the following date:
Temporary Crown Tray Setup:
Due October 8
Please send your photos and item lists to: ben@dentaltown.com.
8
SPECIAL SUPPLEMENT » dentaltown.com
FREE FACTS, circle 60 on card
implants
message board
Congenitally Missing Laterals
»
Dentaltown Message Boards > Implantology > Implantology > Congenitally Missing Laterals
drjscott
Member Since: 11/20/08
Post: 1 of 30
sunburstlespaul Member Since: 07/04/07 Post: 2 of 30
Patient refuses to complete ortho and wants a quick fix. But a lot of these Townies say ortho is the only option for the
sought-after results.
I’m getting a surgical stent made for this case (tooth #7) and was wondering how you
guys would treat to get the best aesthetic outcome since she has a high lip line. Flapless?
Ridge augmentation? Connective tissue graft? My thoughts are to place a CT graft from the
palate and do it flapless to preserve the bone height and thickness. What length would you
use? I was thinking longer is better if I do an immediate temp.
Fig. 1: Looks like good width
F ig. 1
F ig. 2
for a 3.7mm x 15 or 17.
Fig. 2: Definitely shows this
on the full smile. Patient had
braces but wanted to take them
off and have some minimal prep
veneers placed. Thoughts? Just a couple questions so I can understand better.
1. Are you saying patient wanted braces off mid-treatment and just wanted to do
no-prep veneers?
2. Is that a congenital lateral on the patient’s left side? Maybe it’s just the pictures, but
the space for the laterals looks huge! Almost as big as the centrals?
3. Occlusion looks like it might be an issue, and again, back to if ortho was finished
like this? MAY 17 2012
drjscott Member Since: 11/20/08 Post: 3 of 30
Yes, the patient wanted braces off. She had worn them for six months and had moved
and did not want to complete ortho. I tried to convince her to do six-month smiles and she
said no. We then did a wax-up for some minimum/no-prep veneers and she really wants to
go this route.
10
SPECIAL SUPPLEMENT » dentaltown.com
implants
message board
The #10 is a peg lateral. I can take a picture of the wax-up if you’d like to see it. We are
splitting the difference in the space between the lateral and the canine. It makes the teeth on
that side look quite wide from the side, but she likes it. MAY 17 2012
Hey Justin, would you mind posting the wax-up and maybe articulated with opposing
model? How does it look with that bite? It’s tough when a patient refuses to do things, as not
finishing ortho definitely compromises this case. sunburstlespaul Member Since: 07/04/07 Post: 4 of 30
MAY 18 2012
Jrod:dds Are you planning on recontouring the gingiva, too?
MAY 18 2012
Beyond the facts that without ortho this never will look wonderful and that given the
health, or lack thereof, of her tissue, there’s the problem of the 90 percent overbite and lack
of interocclusal space for the implant-supported crown. Looks to me that if you get any
occlusal contact on the implant-supported crown it’ll be traumatic, and to keep contact off
the crown it’ll have to be almost concave on the lingual surface, and what design will you
use on the abutment to get that accomplished? I’d proceed very cautiously. What happens to
you when, because of the space limitations, something happens like fractured porcelain or
one of her friends says her new tooth looks funny? Sometimes when patients are controlling
how we proceed (refusing ortho, ignoring their periodontal health) they place impossible
restrictions on us, while simultaneously their expectations are of a “magazine smile.” I’ll bet
you John Nosti wouldn’t touch this case as is. Best of luck. Tom
Member Since: 06/26/09 Post: 5 of 30 twmdds Member Since: 02/16/04 Post: 6 of 30
MAY 18 2012
No thanks for me on this one as well. Sometimes when a patient places too many
limitations that are in conflict with their goals, the best plan is to embrace the power
of the two-year-old. Say “No” – repeat as needed.
Honestly? “Jane, I know you are looking for a great looking smile. The options you are
looking at and the limitations you are placing on how we get there are not going to
get you there. Given that, I am much more comfortable with doing nothing rather than
anything that we have discussed.” See what she says… Michael Melkers Member Since: 09/09/00 Post: 7 of 30
MAY 18 2012
I just told that to a consult today. “The more you put limitations on what I can do, the
less predictable the outcome becomes.” Schnazbot Member Since: 02/19/09 VPost: 8 of 30
MAY 18 2012
CT grafts around anterior implants are definitely a benefit to plump up tissue.
I think there are some docs on here who do it for every anterior case even with good
tissue already present.
Justin, do you have photos of the wax-up? I agree with others, it just looks so tight in
that spot for an implant. I would be careful here and make sure you can pull it off before
getting out the scalpel or the handpiece. sunburstlespaul Member Since: 07/04/07 Post: 17 of 30
MAY 19 2012
continued on page 12
11
dentaltown.com « SPECIAL SUPPLEMENT
implants
message board
continued from page 11
Wade Pilling Member Since: 03/26/03
Post: 19 of 30
I don’t think a CT graft is needed with the implant. But that’s a side note to this case.
Basically tell her that you can give her a gorgeous smile but you need ortho to do it. I’m not
sure this is a six-month braces case. More of a comprehensive ortho case. MAY 20 2012
drjscott Member Since: 11/20/08 Post: 20 of 30
Yeah I’m definitely taking my time before I do this one. That’s why I posted it. I can’t
find the lower model to articulate so I will have to get my assistant to help me find it and
get that later this week.
I got the lab to do a wax-up and I didn’t specify that they were to be veneers and they
sent me back a wax-up with full coverage crowns.
So I sent it back and
kindly asked to do a veneer
wax-up instead (except for the
implant) and this is what
I got…
I actually like the full coverage wax-up better from the front but I wouldn’t want to
be so aggressive with the preps. The question here is if the patient refuses to do ortho
(patient made the orthodontist take them off ), then do you just tell her no? I get that it
is compromised from what it could be but I believe that it is an improvement. Now I
understand that it is possible that this just won’t work due to functional issues, but just
wondering what options we have if she refuses ortho. I could try to convince her to do
ortho but I’m certain she will refuse. MAY 19 2012
Wade Pilling Member Since: 03/26/03 Post: 21 of 30
I find that if your patients trust you and you educate them enough they’ll do what you
say. It’s very rare, if ever, that I find someone who refuses ortho. There are cases that can
be done without ortho and the results won’t be as good, but still acceptable. I don’t fight
too hard on those ones. But there are some cases I won’t do without ortho. This looks like
one of them. Partly because an implant can’t be moved once it’s done. So I tell the patient
that if we are doing an implant, I want it to be done for life, so let’s set it up right. After
seeing the wax-up, I’d say it can’t be done. Look at those interproximal contours. Either
you are super sub g to get emergence or you get funky emergence that is not hygienic.
So I would just tell her no. Flat out no. It seems like you really want to do this case.
But leaving her as-is is the best choice here. MAY 19 2012
drjscott Member Since: 11/20/08 Post: 22 of 30 Well I would like to, but not if it isn’t going to work. So ortho to correct the overbite
is my only treatment option for her you think? I don’t imagine this could be done with
short-term ortho. MAY 20 2012
12
SPECIAL SUPPLEMENT » dentaltown.com
implants
message board
DrHarry This is a difficult case. I would like to see a full face and a full face smile shot along with
a couple of profile shots to help with the diagnosis. I think doing the lateral without ortho
would be a disaster. Make her a flipper and tell her to come back when she is ready to resolve
her problem. Member Since: 03/14/12 Post: 23 of 30
MAY 20 2012
sunburstlespaul Well the wax-up doesn’t look terrible, it’s not bad. But the laterals and canines are quite
big. As someone else said, you are going to have to prep quite deep to get some good smooth
emergence on the lateral and canines.
Man, that is tight for the implant. You just have no room there. I would try and get the
patient on board with ortho again. Six to 18 months (depending on ortho duration) is so
worth it for a long-term, and far superior treatment. You have to find a way to communicate the benefit to the patient. Member Since: 07/04/07 Post: 25 of 30 MAY 20 2012
search Missing Laterals
»
Find it online at: www.dentaltown.com
Register Now for Early Bird Pricing
www.towniemeeting.com
13
dentaltown.com « SPECIAL SUPPLEMENT
implants
message board
»
Implant Microsurgery:
Narrow Diameter Implants
Dentaltown Message Boards > Implantology > Implantology > Implant Microsurgery: Narrow Diameter Implants
jkwan Member Since: 07/15/08 Post: 1 of 8
A Townie shares insights into a favorite narrow-diameter implant system.
Narrow diameter implants like Implant Direct’s Legacy 3 system allow us to predictably
restore smaller sites. MAY 8 2012
Implant Depot Member Since: 12/02/09 Post: 3 of 8
If you like narrow implants – the Logic 3.0 is compatible with
NobelActive.
The top of it is 3.2mmD and it takes the conical shape connection of the 3.5/NP to restore.
This enables existing NobelActive users to not have to purchase
all the 3.0 components to place and restore this implant. MAY 8 2012
greg moritz Member Since: 01/28/08 Post: 4 of 8
jkwan Member Since: 07/15/08 Post: 5 of 8
What does microsurgery mean? Is it with a microscope? MAY 9 2012
All my videos are recorded through a beam-splitter interface on the Global microscope. Hence, I am labeling this “microsurgery.” Obviously you do not need a microscope to
do these procedures. I do, because my level of precision is enhanced.
Those who don’t use a microscope, don’t because either they don’t feel the need or because
they don’t know what they don’t know. This world of microsurgery is amazing and it has
allowed me to do and record, and therefore teach what is happening in our practice. MAY 15 2012
gxm321 Member Since: 05/11/03 Post: 6 of 8
glennvanas Member Since: 04/08/02 Post: 7 of 8
MAY 15 2012
John: As a fellow microscope enthusiast, also learning to place more implants, I find
that the scope helps me a lot of times in implant placement. Visual acuity helps in
most disciplines in dentistry. I enjoy your posts so thank you for sharing this one with
Dentaltown!
Warmest regards. Find it online at: www.dentaltown.com
14
SPECIAL SUPPLEMENT » dentaltown.com
search Implant Microsurgery
»
Thank you, jkwan. I always look for your posts, and learn from them. MAY 16 2012
implants
message board
»
RPD Support Using BSB One Stage 3.3
and Rhein83 Sphero Block
Dentaltown Message Boards > Implantology > Implantology > RPD Support Using BSB One Stage 3.3 and Rhein83 Sphero Block
A Townie shares this implant case with Dentaltown peers for review and feedback.
shpinatlanta Patient presented with multiple decayed teeth and flaring of all upper teeth due to very
large tongue.
F ig. 1
Member Since: 02/19/06 Post: 1 of 6
F ig. 2
Fig. 1: Pre-op.
Fig. 2: Immediate post-ext and implant #11 (3.3 X 12 BSB one stage).
F ig. 3
F ig. 4
F ig. 5
Fig. 3: Two weeks post-op.
Fig. 4: Eight weeks post-op; not as much labial attached gingiva as desired. Decided to
do pedicle graft from palate.
Fig. 5: Immediate post-pedicle graft.
F ig. 6
F ig. 7
F ig. 8
Search the following message
boards to see additional
implant cases.
Variations on a Theme
Search: Implant Variations
Complex Implant Case Using
e.max & GC Gradia
Search: Complex Implant
Fig. 6: Two weeks post-pedicle graft.
Fig. 7: Seven weeks post-graft. Sphreo Block abutment placed today. Decided to use this
abutment due to its ability to allow for off-angle corrections. Have never used it before.
Seems to be working well so far.
Fig. 8: Facial view at one week post-delivery RPD.
continued on page 16
15
dentaltown.com « SPECIAL SUPPLEMENT
implants
message board
continued from page 15
F ig. 9
F ig. 10
F ig. 11
Fig. 9: The angle correction device for the abutment.
Fig. 10: RPD in place.
Fig. 11: Occlusal view; patient states he has eaten a hamburger and steak so far and is
extremely happy. Comments welcome. MAY 18 2012
Schnazbot Member Since: 02/19/09 Post: 2 of 6 Nice. Serious question, cause I don’t know: Do you get appreciably more retention with
one implant and RPD as opposed to just RPD? He’s got a molar back there to clasp. Do
you find that the single implant as an RPD abutment has a higher failure rate than
other implants? I guess the locator has some stress relieving, but the fixture is at the
canine. Thanks. MAY 18 2012
shpinatlanta Member Since: 02/19/06 Post: 3 of 6
Thanks for the comments. Although the implant does aid in retention, its main purpose
is to move, or remove, the fulcrum line between #7-15 that the partial would tend to rotate
on over time, thus causing more bone loss in this long edentulous area. The fulcrum line is
now from #7-11 or almost non-existent, making for a much more stable base/RPD. To date,
I haven’t had a higher failure rate using implants as partial abutments. MAY 19 2012
wesleypipes Member Since: 10/20/09 Post: 4 of 6
I think this is a great service. I see a lot of patients who could benefit from this type of
procedure. I’m glad you posted this as I have a few patients I can discuss this with as opposed
to a compete denture. It’s not going to break the bank. MAY 19 2012
Julio 1 Member Since: 10/18/02 Post: 5 of 6
Great surgeries, Steve. I don’t do many partials on implants or on teeth for that matter.
I noticed you still use the RPI concept, as I do. Are you aware that the Dawson group does
not believe in this anymore? If I remember correctly, they claim lateral and occlusal displacement are the only factors that need to be considered. Sheeeeeesh, things sure do change given
enough time. MAY 19 2012
shpinatlanta Member Since: 02/19/06 Post: 6 of 6
Find it online at: www.dentaltown.com
16
SPECIAL SUPPLEMENT » dentaltown.com
search RPD Support
»
Thanks, Julio. I do like to use I-bars when possible, but didn’t use any on this case. I do
way more partials than I’d like to after purchasing a geriatric practice from a friend who had
to quit due to health problems. Recently increased my fee for them significantly to offset my
dislike for doing them. I wasn’t aware of the Dawson group stance. Don’t keep up with them
that much. MAY 21 2012
implants
feature
by Paresh B. Patel, DDS
F ig. 1
F ig. 2
One of the most difficult restorative procedures to manage has always been how to
replace the missing anterior tooth. One of the most common in young adults happens
to be the congenitally missing lateral incisor (Fig. 1).1
Treatment options range from:
• A traditional three-unit bridge utilizing the canine and central incisor as abutments
• A resin-bonded bridge utilizing the canine and central incisor lingual surfaces
as retainers
• Orthodontic movement of the canine into the lateral position along with cosmetic
reshaping
• An implant to replace the missing maxillary lateral
If enough bone volume, soft tissue and mesial distal space is available, then a standard body implant can be considered. In cases where these dimensions are deficient, the
restorative dentist will have difficulty managing these violated parameters. Potential
1.
Graber JM. Anomalies in number of teeth. In: Graber TM, ed. Orthodontics: Principles and practice. 1966
continued on page 18
17
dentaltown.com « SPECIAL
SUPPLEMENT
implants
feature
continued from page 17
problems can be lack of restorative prosthetic space, implants too close to adjacent
roots, implant shows through or facial plate dehiscence.
A novel solution to solve these issues can be the use of a 3.0mm implant. The use of
a small-diameter implant such as this should be considered as most congenitally missing
maxillary lateral incisors have an edentulous space of around 5.5 to 6.5mm (Fig. 1). The
facial lingual dimension can also be compromised and usually has a dimension of 5mm
(insufficient to adequately place a standard body implant without bone manipulation).
In an area where only 6mm of space exists, the SDI allows for the placement of the
implant 1.5mm from the adjacent teeth. Other reasons to consider the use of a 3.0mm
SDI could be that most implants have abutments larger than the implant crestal dimension (including platform shifted abutments). This is usually done to enhance the emergence profile of the final prosthesis and creates the need for even more additional space.
The 3.0mm SDI is one piece in design and with no microgap crestal bone loss may also
be reduced or eliminated.2
F ig. 4
F ig. 3
F ig. 5
F ig. 6
F ig. 7
Clinical Case
F ig. 8a
A 17-year-old female presented to our office requesting replacement of her congenitally missing laterals. She had completed orthodontic treatment 12 months prior.
Clinical examination reveled lack of mesial-distal space (Fig. 2) as well as spacing
between the adjacent roots. Bone sounding confirmed limited facial-lingual width at
around 3.5mm (Fig. 3). The patient declined our suggestions to consider a bone graft
and soft tissue graft to add hard and soft volume to the edentulous areas. To confirm
our clinical findings the patient was sent for a CT scan (Gendex GB-500 iCAT). Cross
sectional slices demonstrate a facial lingual width of 3.8mm in the area of #7 and #10
(Fig. 4). Based off these results, it was readily assessed that a SDI would be necessary
to replace the missing teeth.
Surgical Procedure
F ig. 8b
F ig. 9
The placement protocol for SDI is similar to other endosteal implants. A pilot drill
was used in a flapless approach to puncture through the cortical plate. A 3mm tissue
punch (Zoll-Dental) was used to remove the overlying tissue and to visualize the boney
crest (Fig. 5). The flapless approach preserved as much blood supply as possible to the
compromised site. With the CT scan, our knowledge of the angle and topography of
the ridge was known prior to surgery and the need to make a flap was further reduced.
If at any time the need became apparent, a flap could and should be made. The pilot
bit was stopped short of full depth and the quality of bone was assessed clinically with
the blunt end of an endo probe. This was done to confirm what our CT scan showed
as D3 bone in Hounsfield units. A PA was exposed to confirm that the pilot bit was
aligned parallel between the adjacent tooth roots. Once confirmed a final drill of
2.4mm was taken to three-quarters depth of the implant length. This was done to follow our protocol that when in poor bone, the SDI will act as an osseotome and will
compress and expand the bone to create bone of a more dense nature.
A small diameter implant 3.0 x 13mm MILO (Intra-Lock) was selected for a few
important reasons (Fig. 6). Its Ossean surface is impregnated with calcium phosphate
at the molecular level, allowing the implant to bypass the catabolic phase of bone
remodeling. With that the implant can begin its osseointegration weeks ahead than
without this nano-textured surface; a huge advantage when we are talking about one
piece implants that require some sort of immediate restoration.
2.
18
SPECIAL SUPPLEMENT » dentaltown.com
Misch CE. Early bone loss etiology and its effect on treatment planning. Dent today June 1996
implants
feature
Cement over abutments for this system were also planned to be used to convert the
O-ball into a crown form (Fig. 7 on previous page). It allows for any laboratory to make
a well-fitting crown on SDIs. The implant was introduced into the osteotomy via an
implant handpiece (Aseptico AEU-7000). I prefer to place implants with a handpiece
to minimize off axis vector forces. The SDI was gently rotated to its full seating depth
at 30RPM and achieved a final torque of 45ncm (Figs. 8a & 8b on previous page). A
final PA and CT scan was taken to ensure the one piece 3.0mm SDI was fully seated in
bone with no threads above the crestal margin nor penetrated out of the facial or lingual plates (Fig. 9 on previous page).
A plastic comfort cap was snapped over the O-ball and square portion of the one
piece SDI. This would allow the soft tissue to be sculpted as healing occurred and would
keep the gum tissue from covering the square platform of the implant (Fig. 10).
Composite was added to the comfort caps to fashion an immediate non-loaded temporary. Impressions were taken (Capture Glidewell Direct) and sent to the lab for custom
temporaries (DuraTemp Burbank Laboratories) (Fig. 12).
With the use of the DuraTemps, the tissue could continue to be formed for an ideal
aesthetic result while function and phonetics could be verified (Fig. 13).
To ensure an elegant prosthetic solution, it was decided to utilize cement over abutments (Intra-Lock). This abutment converts the standard O-ball portion of the SDI
into a tapered crown form and can be modified on the working model (Fig.11). By
using the cement over abutments the laboratory can fabricate the implant-supported
prosthesis with standard crown and bridge techniques and create a “true fit” SDI crown
within the confines of a smaller prosthetic space.
Discussion
SDI does have certain limitations. The foremost being reduced surface area. A
3.0mm SDI has about 33 percent less surface area than a 4mm standard body implant.
In this case, due to the constricted mesial distal width, the use of an SDI is appropriate.
Occlusal forces will be manageable due to the small prosthetic size of the laterals and
the implant can be fully encased in bone without the fear of fenestration along the buccal aspect. The one-piece design provides a micro-gap-free design and good crestal bone
maintenance as well as no chance for screw loosening.
Another limitation of SDI is the need for immediate restoration (not necessarily
immediate function). The implant, due to its design, will have its abutment supragingival at the time of placement. This puts SDI at risk of being loaded during the healing
phase by any oral habits.
F ig. 10
F ig. 11
F ig. 12
F ig. 13
F ig. 14
F ig. 15
Conclusion
The prosthetic replacement of a missing tooth has been a challenge for clinicians for
years. This is compounded when dealing with a constricted aesthetic site. This case
report demonstrates the novel use of SDI as part of a practitioners’ implant armamentarium. When considering the use of an SDI, it is prudent to select one that offers the
best features to allow quick osseointegration. ■
Author’s Bio
Dr. Paresh Patel is a graduate of UNC-CH School of Dentistry and the MCG/AAID MaxiCourse. He is the co-founder of the American Academy of
Small Diameter Implants and is a clinical instructor at the Reconstructive Dentistry Institute. Dr. Patel has placed more than 2,500 mini implants
and has worked as a lecturer and clinical consultant on mini implants for various companies. He can be reached at pareshpateldds2@gmail.com
or online at www.dentalminiimplant.com.
19
dentaltown.com « SPECIAL
SUPPLEMENT
book
excerpt
by August de Oliveira, DDS
The field of implant dentistry is growing and adapting to the digital world at an extraordinary pace. Dr. August de Oliveira’s recently
released second book Guided Implantology Made Easy – a follow up to
Implants Made Easy – provides general dentists a comprehensive
overview of the process of placing implants via guided surgery. In this
book excerpt, de Oliveira discusses the use of CEREC to generate a
simple crown proposal.
CEREC Integration
I think that there is a misconception that you need to use CEREC
in order to get Guides from SiCAT. By utilizing Guide Sleeves in the
posterior, you can get a pretty good idea of where to place your implant.
However, I can say from not only using Galileos, but many other
Guided Surgery systems, that having access to CEREC greatly increases
the safety and predictability of guided surgery.
There are many uses restoratively for CEREC when it comes to
implants. You can not only mill the final restoration, but temporaries and abutments. Unlike Implants Made Easy, this is not a book
on implant restoration so I won’t go into restoring your implant
with CEREC.
In my office I use CEREC with Galileos in five ways:
1. To generate a simple crown proposal to aid in the placement of
the implant.
2. To decrease the effect of noise and increase the resolution of the
teeth and soft tissue by importing a stone model.
3. To import a model of a duplicate denture.
4. To use the Opti Guide system by importing a full arch image of
the patient’s respective arch.
5. To mill out a CEREC Guide.
20
SPECIAL SUPPLEMENT » dentaltown.com
book
excerpt
Generating a Simple Crown Proposal
The difference between perfect implant placement, from a
restorative point of view, and “acceptable” is only a matter of a
few degrees. This is especially true in the anterior where the size
of the tooth root and the size of the implant are not that different. In the posterior we can get away with more as the average
implant diameter is 5mm and the average root 10mm (Fig. 2).
In the example below (Figs. 3&4) an implant was planned using
a simple Guide Sleeve. The one on the lower right was planned with
CEREC. I think you can see that in both examples it is pretty easy
to get a good result when one has a mesial and distal neighbor.
When one lines up the Guide Sleeve with the adjacent teeth’s central grooves, you can feel pretty confident that the final restoration
Fig. 2
Fig. 5
Fig. 7
will be in harmony with the adjacent teeth. Although much nicer to
look at, the CEREC restoration more or less does the same thing.
The following example (Figs. 5&6) really shows the benefit
of having a simple crown proposal. In the example below an
implant was planned looking at the adjacent teeth and the available bone. The Guide Sleeve is lingual to the ridge and should
yield a crown with a screw access hole in the cingulum.
The image below (Fig. 7) shows the case with the CEREC
proposal entered. As you can see, I thought I planned this case
well. If this implant was placed in that orientation I would either
need an angled abutment and could not do a screw retained
restoration or if a screw retained restoration was planned the screw
hole would be on the incisal edge. In the next picture (Fig. 8) I
Fig. 3
Fig. 4
Fig. 6
Fig. 8
continued on page 22
21
dentaltown.com « SPECIAL
SUPPLEMENT
book
excerpt
continued from page 21
repositioned the implant, leaving the apex where it was but
rotated the platform to the lingual.
Like the anterior, another area where CEREC really shines is
when you have a distal end case. When you have a mesial and a
distal neighbor, you have a lot of references to plan your
implant. However things get complicated when no distal tooth
is present. Also there is a tendency to place second molar
implants too far to the distal. This may lead to a large mesial
cantilever. Due to high occlusal forces in this area, that can lead
to screw loosening or breakage, or bone loss around the implant
(Figs. 9-11).
The images on this page (Figs. 12-15) clearly demonstrate
the benefits of this crown proposal. The Cross Sectional image
on the upper left demonstrates that there is no clear indication
of where to place the implant. However, it’s very obvious when
superimposing the CEREC data. In the lower you can see that
by having that crown form in the image, one can place the
implant in a position that avoids the distal root of the first
molar, while still placing the Guide Sleeve, and the eventual
screw hole, in the ideal restorative position.
Fig. 9
For two or less adjacent teeth proposals I typically use
Biogeneric Individual in the CEREC software. You would start
as you would normally for designing a restoration. Select the
tooth or teeth in the Administration screen and select Biogeneric
Individual (Figs. 16&17). If you have a wax up or were smart
enough to either take a scan or model of the tooth before it was
extracted, you can use Biogeneric Copy.
There is no right or wrong way to take a scan. At the very
least you would want to get the adjacent teeth as well as a good
amount of the soft tissue buccal and lingual to the edentulous
space. The more scans I do, I like to get at least the whole quadrant if not the whole arch (Fig. 18). By getting the whole arch
you can compare your CEREC proposal to the contralateral
tooth. That way if you have problems getting a decent proposal,
you can toggle the proposal off in Galileos and just look at the
contralateral side (Fig. 19).
When designing a restoration in CEREC we are used to
using the automatic margin finding feature. In designing
a proposal to be imported in Galileos we want to turn that
off and go to manual. The automatic margin finder will flop
Fig. 11
Fig. 10
Fig. 12
Fig. 13
22
SPECIAL SUPPLEMENT » dentaltown.com
Fig. 14
Fig. 15
book
excerpt
Fig. 16
Fig. 17
Fig. 19
Fig. 20
Fig. 18
Fig. 21
around looking for a margin and you won’t be able to get
anything decent. Trace around where you want the emergence profile of the crown to be, not the eventual margin.
In essence you are tracing out where the tooth socket was
(Figs. 20&21).
Turn your model to the buccal and lingual and trace out the
margin (Figs. 22&23). Mimic the cervical areas of the adjacent
teeth in essence mimicking what a ridge lap pontic would do.
If you do not do this you will end up with a small or distorted
proposal. Design the crown as you would normally. I don’t
spend too much time on occlusion or working out my marginal
ridge heights. Just make sure that the crown looks like it fits in
the arch.
Fig. 22
Fig. 23
continued on page 24
23
dentaltown.com « SPECIAL
SUPPLEMENT
book
excerpt
continued from page 23
In either 3.85 or in 4.0, get to the mill preview (Figs.
24&25). Inspect the crown and just make sure it can be
exported. Look for any artifacts that may give you an error in the
exporting process.
If you are using 3.85 you will need a dongle like the one pictured below (Fig. 26). In 4.0 there is a license manager that can
be accessed by using the “top menu.” You will need an internet
connection so that the license (Fig. 27) can be verified.
Fig. 24
Fig. 25
Fig. 27
Fig. 26
Fig. 28
Fig. 30
Fig. 29
24
SPECIAL SUPPLEMENT » dentaltown.com
Export the file as a .ssi file (Fig. 28). Sometimes it takes
the computer awhile to pull this up, so if you don’t see the
.ssi option, close the export menu and open it up again.
If you have networked your CEREC, export the file to
the appropriate drive and then export to the Galileos
Acquisition PC (Fig. 29). If not, simply export to a USB
drive. In Galileos, click the CAD/CAM menu and open the
appropriate drive.
book
excerpt
After selecting the appropriate .ssi file, a model like
the one below will pop up (Fig. 30). Continue on to the
next window where you will select teeth on the model
(Fig. 31) and teeth on the Pan (Fig. 32). For a full arch
model I look for the teeth with the least distortion, usually teeth without restorations. For me, more is better, so
I may use up to 4 different points scattered throughout
the mouth. For a simple quadrant I usually just select
two teeth.
In the confirmation screen look at the yellow outline
of the model in the Pan (Fig. 33). If it is off you will see
it readily here. If it does not match up, no big deal. Just
click the “back” button. Usually this does not happen,
but it can. You should have a nice model that you can
plan on (Fig. 34). Fig. 32
Fig. 31
Fig. 33
Author’s Bio
Fig. 34
Dr. August de Oliveira is the
author of Implants Made Easy, a
book geared toward starting
your first implant. He just released Guided
Implantology Made Easy. Dr. de Oliveira has
lectured nationally on cone beam technology, dental implants and CAD/CAM technology. He has been a software beta tester
for Sirona, Blue Sky Bio, Anatomage and
Implant Direct. He is currently a moderator
and regular contributor to Dentaltown.com’s
Implantology and Mini Implants Forum.
Dr. de Oliveira practices general dentistry
in Encino California. To find out more
about implants and Guided Surgery, go to
www.implantsmadeeasy.com.
25
dentaltown.com « SPECIAL
SUPPLEMENT
continuing education
feature
by Brady Frank, DDS,
with a special contribution by Ryan Swain, DDS
Abstract
This course is designed to load the general practitioners arsenal
with multiple minimally invasive techniques that can be implemented
immediately. Not only do the techniques increase the level of patient
care but add significant increase to the productivity of the general
practitioner. Multiple case studies are used to demonstrate no-drill
implants, the five-minute implant, abutment and crown and the top
five flapless techniques used by GPs in today’s implant-geared practice.
Educational Objectives
At the end of this program participants will be able to:
1. Identify the suitable clinical situations for and learn to complete the five flapless/sutureless soft-tissue surgical implant
access procedures (to include the direct, high-speed handpiece,
tissue punch and mini-envelope procedures).
2. Identify situations that lend themselves to the clinical application of the “no-drill” implant procedure.
3. Be able to identify clinical situations where an implant can be
predictably placed into the site of a freshly extracted tooth
without the use of a drill.
4. List several implant final prosthetic techniques that reduce the
overall number of appointments necessary and minimize rework.
5. Define specific marketing medium and specific ads to place in
that medium to vastly increase new patient flow and ultimately
place more implants.
6. Understand why short-term orthodontics is an ideal accompaniment to efficient implants in the GP practice.
This written self-instructional program is designated for 1.5 hours of CE credit by
Farran Media. Participants will receive verification shortly after Farran Media receives
the completed post-test. See instructions on page 32.
26
SPECIAL SUPPLEMENT » dentaltown.com
Approved PACE Program Provider
FAGD/MAGD Credit
Approval does not imply acceptance
by a state or provincial board of
dentistry or AGD endorsement.
12/01/2004 to 12/31/2012
continuing education
feature
Garrett Gunderson recently stated in a lecture to general
dentists, “leveraging hot topics in your practice is one of the top
ways to build business equity.” I think that we would all agree
that implants, particularly minimally invasive/efficient techniques, are at the pinnacle today. This article is an exploration of
the ever-increasing arsenal of implant efficiency techniques
available to the general practitioner. The most popular protocols
are demonstrated through the selection of several case studies.
Case Study: Four maxillary implants and a fixeddetachable hybrid bridge with mandibular
implants site #19 and #30
Dental implant techniques and technology have been
evolving at a similar rate to what has been witnessed in the PC
and smartphone market over the last few years. Dental
implants have become much less invasive and more efficient
causing this procedure to be the most talked about and hottest
topic in dentistry from both a patients’ and clinicians’ perspective. This case study will highlight multiple efficiency techniques that you will be able to incorporate into your practice
right away. If you add these techniques to your practice you
will recognize great value from both a time savings and overall
patient comfort perspective.
The patient presented with an ill-fitting maxillary denture and
a mandibular distal-extension partial that had not been worn in
months due to discomfort (Figs. 1 & 2a). The patient had a moderate gag reflex, which prevented the upper denture from being
worn comfortably. The distal third of the palate had been removed
in an attempt to relieve the gag reflex. The patient elected for a
treatment plan, which involved replacement of the upper denture
with a fixed-detachable hybrid bridge to be screw-retained and supported by four maxillary implants. The lower treatment plan
involved replacing the existing partial with implants, teeth numbers
19 and 30. All implant procedures and final prosthetic impressions
were completed in a 90-minute appointment.
Efficiency Technique Highlight: Sizing and angling the
implant to utilize available bone rather than manipulating
the bone through grafting procedures to accommodate a certain sized implant. Recent advances in implant stability at the
time of insertion have allowed implantologists to chose an
implant size in relation to available bone rather than manipulating the bone via grafting procedures.5 (In fact, a recent study
of 14,722 placed between the years 1980 and 2009 demonstrated that “There was no statistically significant difference
between the failure rates of short dental implants and standard
implants or between those placed in a single stage and those
placed in two stages (multivariate analysis).” So basically they
found that implants shorter than 10mms placed in a one-stage
approach show no difference in success rate. This allows a clinician to confidently place a maxillary 8mm implant in an area
of 8-9mms of bone height rather than a sinus lift and bone graft
to accommodate a longer implant. This has allowed implant
Fig. 1
Fig. 1: Pre-op pano.
Fig. 2a: Post-op pano immediately after implant placement.
Fig. 2b: Two appointment implant, abutment and crown.
Fig. 2a
Fig. 2b
dentistry to be minimally invasive and achieve new levels of
efficiency within the general dentistry practice. In this particular case there is very shallow bone height just inferior to the
maxillary sinus as demonstrated on the PAN. There is more
than sufficient bone just medial of the inferior wall of the sinus.
An implant placement following the angle of the wall of the
sinus will allow for enough bone to place 4.7 X 13 implants.
This saves both the clinician and patient additional appointments needed to recover from more invasive sinus grafting surgery, thus, greater efficiency. On the mandible, 4.7mm X
10mm length implants were selected. Even as little as 8mm of
available bone height (to accommodate an 8mm implant) has
been demonstrated in numerous studies to be sufficient to
maintain a 97 percent success rate. A 2009 study published by
the Journal of Oral and Maxilofacial Surgery concluded:
“Placement of short dental implants is a predictable treatment
method for patients with decreased posterior mandibular bone
height.”1 To demonstrate the efficacy of short implants on the
maxillary arch (Fig. 2b) is a post pan of implant, abutments and
crowns #13, #14 and #15. The distal abutment, #15, on a
bridge spanning #13-#15, is lost due to a combination of secondary decay and periodontal issues. Not long ago the preferred
treatment for most would have been extraction of #15 and a
sinus lift/bone graft procedure to create enough vertical bone
for 10-13mm implants to be placed. A simplified approach
1.
5.
J Oral Maxillofac Surg. 2009 Apr;67(4):713-7. Outcomes of placing short dental implants in the posterior mandible: a retrospective study of 124 cases.
Int J Oral Maxillofac Implants. http://www.ncbi.nlm.nih.gov/pubmed/21841992# 2011 JulAug;26(4):816-25. Failure rates of short () 10 mm) dental implants and factors influencing their failure:
a systematic review. Sun HL, Huang C, Wu YR, Shi B
continued on page 28
27
dentaltown.com « SPECIAL SUPPLEMENT
continuing education
feature
continued from page 27
involves 5.7mm wide by 8mm long implants to avoid more
extensive, expensive and uncomfortable sinus bone grafting
procedures for the patient.
Most applications of “short implants” in the 8mm range
include the maxillary and mandibular posterior areas where the
sinus and mandibular nerve come into play. Armed with studies
proving the efficacy of “short” implants, a general dentist does
not need to flirt with anatomical structures to provide great, predictable patient care.5 Always staying 3-4mm away from the
mandibular nerve and keeping the apex of the implant embedded in the cortical plate of the sinus are great protocols to avoid
anxiety. In fact, I often speak of the 6mm rule when the
mandibular nerve is in the same sentence. Human error can be
up to 3mm so if you follow the 6mm rule and always try to stay
that distance from the nerve then if human error occurs you
have at least a 3mm safety zone.
Efficiency Technique Highlight: High-speed drill gingival access and initial pilot hole. Referencing the initial case
study, the maxillary ridge was palpated to assimilate the alveolar
ridge anatomy. This allowed for accurate entry points into the
tissue to be determined. After deciding on the ideal entry points,
a high-speed handpiece was used with a special long surgical bur
(Fig. 3). Small circular movements were used to enlarge a hole
through the keretinized tissue using the surgical high-speed bur
and simultaneously creating a 5-6mm pilot hole in the bone to
initiate the osteotomy. After all four tissue accesses were opened,
a 2.3mm drill was used to create the initial full length
osteotomy. The drill was buried to the length of 16mm to compensate for 2-3mm of gingival tissue. A pan was taken with the
drill inserted to length to verify correct angulation and to ensure
that the sinus cavity was not being encroached upon. After verifying correct position, the final osteotomies were created one
drill short of the final drill to allow for greater bone compression
and thus greater torque/primary stability. A 3.8mm drill is one
short of the final 4.4mm, which is used for a 4.7mm diameter
implant. All four upper implants were torqued to 40-60N/Cms
(Fig. 4a). This technique is much less invasive
than an approach involving a full thickness
flap and also requires fewer appointments,
thus, more efficiency. Please scan the following
QR code with your smartphone or visit
www.frankimplantprocedures.com/video1 to
view a video.
Efficiency Technique Highlight: Creating a custom
bar/framework template in mouth immediately after
implant insertion with final bite, midline and inter-pupillary smile-line. Oftentimes at this stage in the procedure the
clinician will place cover screws or healing caps over the
implants and wait for several months. This efficiency technique
involves initiation of the prosthetic process immediately after
implant insertion. This technique is recommended when the
implants can be torqued to a level of around 60N/cms. After
insertion of the implants the transfers were removed and 18-
28
SPECIAL SUPPLEMENT » dentaltown.com
degree-angle correction multi-unit abutments were placed. The
angled abutments were approximated to create a certain degree
of parallelism but additionally to allow for the prosthetic screw
to be accessed from the lingual of the anterior teeth and
occlusally in the posterior. The multi-unit abutments used are
able to accommodate an angle differentiation of up to 20
degrees. After achieving an acceptable angulation of the multiunit abutments, castable copings that are generally used by the
lab in fabricating the framework were screwed into the abutments (Figs. 4a & b). The castable copings were then adjusted
using a high-speed to approximate the vertical dimension. After
establishing the vertical, two strips of Triad light-cured custom
tray material were cut from a sheet using a Barred Parker blade.
The strips were approximately 5mm wide. The strips were then
formed around the cast-able copings, one on the lingual and
one on the facial/buccal. The material was palpated into the
rough bar location based on visualization of the ideal position
of the maxillary teeth. After light curing the material in the
mouth, a blue-mouse was taken to relate the correct bite and
vertical. A cotton swab was embedded into the blue-mouse to
correlate the inter-pupillary smile line and the midline was
marked. The screws were then removed from the cast-able copings and a pick-up impression was taken. This efficiency technique has saved both the patient and clinician several steps and
created a more exact communication with the lab. In the past,
frameworks and bars necessitated sectioning and oftentimes
new impressions due to minute discrepancies in the final
impression with implant analogs. Not so with this technique as
Fig. 3
Fig. 4a
Fig. 4b
Fig. 3 Implant tray setup.
Fig. 4a: Implants in place with transfers.
Fig. 4b: Implants with abutments and lab castable copings immediately after
implant placement.
continuing education
feature
all four implants are a fixed unit via the rigid light-cured acrylic
(Fig. 5e).
Efficiency Technique Highlight: Utilizing a mini-envelope incision (flapless approach). After completing the upper
final impression, the initial soft-tissue entry for implants site #30
and #19 was initiated. Due to a slight deficiency of keritinized
tissue on the buccal aspect of the implant sites, a mini-envelope
incision was chosen. This is basically a small slit made at the crest
of the ridge to reflect a 4mm wide portion of keretinized tissue
to the buccal. This will allow for a nice cuff of keritinized tissue
around the implant. I use a sharp instrument commonly used for
sculpting composite resin (Fig. 3). It works well for releasing the
tissue from the bone and creating a small envelope. Next, a surgical bur in the high-speed handpiece was used to create a 45mm pilot hole in the cortical plate of the bone. Using this hole
the osteotomies were initiated and completed to a length of
13mm from the gingival height. This allowed for 3mm of tissue,
which accommodates a 4.7 X 10mm implant. Implants were
placed and a final impression was taken for the prosthetic portion of the procedure (cemented porcelain fused to metal restorations). No sutures or flap saves both clinical time and an
appointment as the final impression was taken immediately after
implant insertion (Figs. 5a & b). In 2002 the Journal of Oral and
Maxilofacial Implants published a study that concluded: “Flapless
implant surgery is a predictable procedure if patient selection
and surgical technique are appropriate.”2
Figure 7 is a picture of mandibular posterior implants immediately after placement
utilizing the mini-envelope incision. Note
the ideal conditions for a final impression
without bleeding or sutures. Please scan the
following QR code with your smartphone
Fig. 5a
Fig. 6a
or visit www.frankimplantprocedures.com/video2 to view
a video.
Efficiency Technique Highlight: Utilizing a 3-in-1 implant
system. Several implant companies now provide the option of
3-in-1 systems to their customers (Fig. 3). This basically means
that the implant body, a customizable abutment and a transfer all
come attached to one another in the same package. This provides
efficiency because the clinician does not need to track down
numerous small parts. Also, the impression for final prosthetics
can be taken seamlessly immediately after implant insertion with
a very accurate closed-tray impression technique. As the implant
is being inserted it is very easy to visualize the ideal placement of
the margin of the final abutment. Simply screw down the implant
until ideal margin in relation to the tissue is achieved. Not only is
this technique efficient, but also is very overhead friendly.
Efficiency Technique Highlight: Taking the final prosthetic impression and bite immediately after implant placement during the same appointment.
As has been mentioned, the final prosthetic impressions for
both arches were taken at the end of the surgical stages for both
arches. The next appointment is the final seat appointment for
both the upper and lower restorations in 30 to 90 days (Figs. 6a
& 6b). Is early loading OK? In 2007 the Journal of Oral
Maxilofacial Implants published a study that concluded: “Early
loading of endosseous dental implants placed in healed ridges
offers select benefits to clinicians and their patients.”3 Final
restorations seated approximately one month after implant
placement showed a 97 percent success rate as long as a torque
greater than 40N/cm was achieved. In the case pictured of an
2.
Int J Oral Maxillofac Implants. 2002 Mar-Apr;17(2):271-6. Flapless implant surgery: a 10-year clinical retrospective analysis. Campelo LD, Camara JR.
Fig. 5c
Fig. 5b
Fig. 6b
Figs. 5a-e: Chairside pre-lab prosthetic procedures.
Fig. 5e
Fig. 5d
Fig. 7
Fig. 6c
Figs. 6a & b: Wax try-in of maxiliary full arch.
continued on page 30
29
dentaltown.com « SPECIAL SUPPLEMENT
continuing education
feature
continued from page 29
upper left quadrant bridge (Figs. 8a-d), the final impression was
taken immediately after implant placement and was seated three
weeks later. The stock abutments that come with the implant
were actually prepped and used as final, customized abutments.
I have found it is much more efficient and accurate to customize
your own abutments chairside with a diamond bur rather that utilizing lab fabricated
customized abutments. Please scan the following QR code with your smartphone or visit
www.frankimplantprocedures.com/video3 to
view a video.
Case Study:
No-Drill Implants with an Osteoconverter
Efficiency Technique Highlight: Immediate placement of an
implant into a fresh extraction site, particularly no-drill
implants. This involves the extraction of a compromised tooth and
the immediate placement of an implant without the use of a drill.
The procedure is atraumatic and predictable. Why is this procedure
preferred to using a drill in the fresh extraction site? The drilling
action can fracture fragile bone around the extraction site or remove
thin buccal/facial bone, which would ideally be retained around the
implant. The Osteoconverter acts to expand the extraction site
while keeping wanted bone intact. The Osteoconverter also scores
the internal aspects of the extraction site in roughly 1mm increments, which increases blood flow to the implant interface. This
improves osseointegration and provides bone expansion, which converts the irregular root circumference into a shape that is accommodating to the implant. The Osteoconverter has a flat end much like
an osteotomb so in areas just inferior to the maxillary sinus, it gently converts the socket site without damaging the fragile sinus floor
(Fig. 9a). The Osteoconverter also serves as a measuring device; once
the socket site has been converted, a simple measurement is made in
order to select the correct size implant (Figs. 10a-c).
Fig. 8a
Fig. 8b
Fig. 9
Fig. 9: OsteoConverters by OsteoCore Dental Implants.
30
SPECIAL SUPPLEMENT » dentaltown.com
Fig. 8c
Fig. 10a
It certainly sounds nice to avoid picking up a drill when placing implants, but what are some contraindications to this procedure? Perhaps the most common is acute infection around the
apex of the tooth. Experienced implantologists often clean out
the infected area and place the implant directly into the area that
had infection. In fact, the Journal of Periodontology published a
study in 2001 with the following conclusion: “The present study
shows that when a screw-type dental implant is placed without
the use of barrier membranes or other regenerative materials into
a fresh extraction socket with a bone-to-implant gap of 2mm or
less, the clinical outcome and degree of osteointegration does not
differ from implants placed in healed, mature bone.”4 Therefore
the use of bone grafting materials or membranes is not necessary
for superior outcomes. Interestingly the majority of the teeth had
long-term infection associated with the tooth. It has been found
that implants are very resistant to infection in socket sites due to
the fact that bacteria cannot feed on titanium so once the source
of the infection is gone, the tooth, the area is quickly exterminated of remaining bacteria by killer T-cells and lymphocytes.
What if the root is too short to place what you think to be an
ideal-sized implant? Drilling beyond the apex for a sufficient
length with the pilot drill will solve that issue. In these cases it is
prudent to underprepare (use one size smaller drill) beyond the
apex and use the Osteoconverter to convert the site. This will
assure primary stability and an excellent success rate. If the apex
of the socket site is right against the floor of the sinus, like many
are, the Osteoconverter will gently push against the sinus floor
and allow for the apex of the implant to be even with the floor
3.
4.
Int J Oral Maxillofac Implants. 2007 Sep-Oct;22(5):791-800. Three-year evaluation of single-tooth
implants restored 3 weeks after 1-stage surgery. Cooper LF, Ellner S, Moriarty J, Felton DA, Paquette D,
Molina A, Chaffee N, Asplund P, Smith R, Hostner C.
Immediate Implantation in Fresh Extraction Sockets. A Controlled Clinical and Histological Study in
Man: Dr. Michele Paolantonio, Marco Dolci, Antonio Scarano, Domenico D’Archivio, Giacinto Di
Placido, Vincenzo Tumini, Adriano Piattelli, Journal of Periodontology Vol. 72, No. 11, 15601571(Volume publication date: November 2001) DOI: 10.1902/jop.2001.72.11.1560
Fig. 8d
Fig. 10b
Fig. 10c
Figs. 10.a-c: Atraumatic extraction of #27 and immediate placement of implant.
continuing education
feature
of the sinus or less than 2mm. The cells between the sinus membrane and bone on the sinus floor are highly bone-forming. This
will provide for bone at the apex of the implant. This pano of full
maxillary extractions and four implants with locator abutments
to retain an upper prosthesis was placed without the use of a drill
(Figs. 11a & b). OsteoCore implants may be inserted without
the use of an Osteoconverter.
Case Study
Efficiency Technique Highlight: Short-term ortho and
implants. The recent expansion and availability of short-term
orthodontics in the GP practice has opened up a great deal of
opportunity from an implant standpoint. Just five years ago the
average length of time needed to complete an ortho/implant
comprehensive case was two to three years. Today, with proper
education on short-term ortho and efficient 3-in-1 implant systems, ortho/implant cases can be completed in as few as seven
months. The referenced case study to demonstrate this point is
contributed by Dr. Ryan Swain. The dual objective in this case
was to efficiently correct anterior spacing and additionally create
an ideal amount of room to restore congenitally missing #24
and #25 with implants, abutments and crowns. The orthodontic phase of treatment was completed in six months (Figs. 12a &
b). A minimally invasive approach to the implant surgery
involves mini-envelope incisions, one-drill (narrow-body)
implants and a final impression for the crowns immediately after
implant placement. One huge advantage to the short-term
ortho approach as it relates to implants is that the bone does not
have time to resorb after a tooth is dragged through the area via
bodily movement. Thus, implant surgery is idealized with more
available bone width.
The similar case below demonstrates the placement and
restoration of implants in an anterior area of partial edentulism.
In figures 13a-d, you’ll see the high-speed handpiece soft-tissue
approach and initial pilot hole. Just prior to this bone sounding
was performed with an anesthetic needle and a perio probe. Final
drill was used and implants were placed to bone level. After
placement, abutments were customized chairside and Expasyl
retraction was used just prior to a final impression being taken.
In this case, crowns were permanently cemented in 30 days.
This approach and most of the others were simply not
options to the implantologist just three to five years ago. This is
a huge benefit to patients and clinicians alike as treatment times
are vastly reduced and clinical success rates are increased. Join
the growing trend of general dentists today who have embraced
implant efficiency and watched their practices reach new levels
both financially and from a professional satisfaction standpoint.
If you would like more information about the topics covered
in this article or would like to view upcoming Implant
Efficiency Institute training programs, please call 541-8640312, go to www.osteocoredentalimplants.com or e-mail
info@osteocoredentalimplants.com. Fig. 11a
Fig. 11b
Fig. 12a
Fig. 12b
Fig. 13a
Fig. 13b
Fig. 13c
Fig. 13d
Figs. 11a & b: Four extractions and four implants placed using the No-Drill
Implant Procedure
Figs. 12a & b: Pre- and post-short-term ortho treatment to set up for implants
Figs. 13a-d: One appointment implant, abutment, and crown impression
Author’s Bio
Over the last 10 years, Dr. Brady Frank has owned and managed multiple practices. Dr. Frank has addressed thousands of dentists at popular seminars throughout the country including Excellence in Dentistry, Phasing-Out Seminars (over 20 presentations delivered), and
Schein/Camlog Seminars. Dr. Frank’s topics include Implantology, Dental Transitions and Entrepreneurial Satellite Practice Ownership.
continued on page 32
31
dentaltown.com « SPECIAL SUPPLEMENT
continuing education
feature
continued from page 31
Post-test
Claim Your CE Credits
Answer the test in the Continuing Education Answer Sheet and submit it by mail or fax with a processing fee of $36. We invite you to view all of our CE
courses online by going to http://www.dentaltown.com/onlinece and clicking the View All Courses button. Please note: If you are not already
registered on www.dentaltown.com, you will be prompted to do so. Registration is fast, easy and of course, free.
1. Which length of implant has shown in recent studies to have
the greatest long-term success rate?
a. 8mm
b. 10mm
c. 13mm
d. All lengths have demonstrated similar, very high success
rates in recent clinical studies.
7. The 6mm rule basically means that the clinician maintains a
6mm buffer zone in relation to the:
a. Hamular notch.
b. Mandibular nerve or mental foramen.
c. Incisive papilla.
2. As the field of implantology has developed over the years, we
have, as a profession, found that bone grafting procedures
are ___ needed than in the past.
a. More
b. Less
8. Flapless procedures are considered by some to be preferred
to a flap because:
a. There is less of an opportunity for oral microflora to
invade the site.
b. Patients experience much less post-operative discomfort.
c. They are more efficient.
d. All of the above.
3. Using a high-speed handpiece for the initial soft-tissue access
hole and start to osteotomy:
a. May cause osteonecrosis.
b. Is inaccurate for the general dentist.
c. Causes excess tissue trauma.
d. Is generally the most exacting and least traumatic for the
patient.
9. Which of the procedures is included in the top five flapless
procedures used by general practitioners in the U.S.?
a. Direct
b. High-speed handpiece
c. Mini-envelope
d. Tissue punch
e. All of the above
4. The use of a mini-envelope incision is:
a. Used primarily to aid in the retention of keritinized tissue
around the implant.
b. Used in conjunction with a full-thickness flap.
c. Used with mucosal tissue.
10. A no-drill implant involves the placement of an implant
directly into a fresh extraction site without using the implant
drill.
a. True
b. False
5. Implants that are manufactured to include both the straight
abutment, which is attached directly to a transfer allow for
fewer patient appointments and a more minimally invasive
nature and are generally called:
a. One-piece implants.
b. Mini-implants.
c. 3-in-1 implants.
*Some answers to questions may be found in embedded videos.
6.
Due to the fact that implants are such a hot topic among
the general public, implant marketing tends to receive
____results than that of other general dentistry procedures.
a. Much more favorable
b. Less favorable
32
SPECIAL SUPPLEMENT » dentaltown.com
Legal Disclaimer: The CE provider uses reasonable care in selecting and providing content
that is accurate. The CE provider, however, does not independently verify the content or
materials. The CE provider does not represent that the instructional materials are error-free
or that the content or materials are comprehensive. Any opinions expressed in the materials are those of the author of the materials and not the CE provider. Completing one or
more continuing education courses does not provide sufficient information to qualify participant as an expert in the field related to the course topic or in any specific technique or
procedure. The instructional materials are intended to supplement, but are not a substitute
for, the knowledge, expertise, skill and judgment of a trained healthcare professional. You
may be contacted by the sponsor of this course.
Licensure: Continuing education credits issued for completion of online CE courses may
not apply toward license renewal in all licensing jurisdictions. It is the responsibility of each
registrant to verify the CE requirements of his/her licensing or regulatory agency.
continuing education
feature
Continuing Education Answer Sheet
Instructions: To receive credit, complete the answer sheet and mail it, along with a check or credit card payment of $36 to:
Dentaltown.com, Inc., 9633 S. 48th Street, Suite 200, Phoenix, AZ 85044. You may also fax this form to 480-598-3450. You will
need a minimum score of 70 percent to receive your credits. Please print clearly. This course is available to be taken for credit
September 1, 2012 through its expiration on September 1, 2015. Your certificate will be e-mailed to you within 3-4 weeks.
Top Implantology Breakthroughs for the GP
by Brady Frank, DDS, with a special contribution by Ryan Swain, DDS
License Number ______ ______ ______ ______ ______ ______ ______ ______ ______ _______
CE Post-test
Please circle your answers.
AGD# _____________________________________________________________________________________
1.
a
b
2.
a
b
3.
a
4.
c
d
b
c
d
a
b
c
5.
a
b
c
6.
a
b
7.
a
b
c
8.
a
b
c
d
9.
a
b
c
d
10.
a
b
Name _____________________________________________________________________________________
Address ___________________________________________________________________________________
City___________________________________________ State __________ ZIP _________________________
Daytime phone_____________________________________________________________________________
E-mail (required for certificate) _________________________________________________________________
Check (payable to Dentaltown.com, Inc.)
e
Credit Card (please complete the information below and sign; we accept Visa, MasterCard and American Express.)
Card Number _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____ _____
Expiration Date – Month / Year ______ ______ / ______ ______ ______ ______
Signature ________________________________________________________________________________________ Date ____________________
Yes, I would like to continue receiving Denaltown Magazine free of charge
(Signature required for subscription - free to U.S. only)
Field of practice (optional)
No, thank you.
Program Evaluation (required)
Please evaluate this program by circling the corresponding numbers: (3 = Excellent to 1 = Poor)
1. Course objectives were consistent with the course as advertised
3
2
1
2. Course material was up-to-date, well-organized and presented in sufficient depth
3
2
1
3. Instructor demonstrated a comprehensive knowledge of the subject
3
2
1
4. Overall, I would rate this course
3
2
1
5. Overall, I would rate this instructor
3
2
1
For questions, contact Director of Continuing Education Howard Goldstein at hogo@dentaltown.com
General Dentist
Anesthesiology
Consultant
Cosmetic Dentistry
Dental Assistant
Dental Company Rep.
Dental Education
Dental Lab Tech
Dental Student
Dental Hygiene Student
Endodontics
Endodontic Resident
Front Office
Hygienist
Implantology
Oral & Maxillofacial Surgeon
OMS Resident
Oral Pathology
Orthodontics
Orthodontic Resident
Pediatric Dentistry
Pediatric Resident
Periodontics
Periodontic Resident
Prosthodontics
Public Health
Radiology
Speaker
TMD Specialist
Other
33
dentaltown.com « SPECIAL SUPPLEMENT
FREE FACTS, circle 56 on card