G Model
PEC-4423; No. of Pages 7
Patient Education and Counseling xxx (2012) xxx–xxx
Contents lists available at SciVerse ScienceDirect
Patient Education and Counseling
journal homepage: www.elsevier.com/locate/pateducou
Medical Decision Making
Combining deliberation and intuition in patient decision support
Marieke de Vries a,b,1,*, Angela Fagerlin c,d,e, Holly O. Witteman e,f,g, Laura D. Scherer c,e,h,1
a
Tilburg Institute for Behavioral Economics Research (TIBER), Department of Social Psychology, Tilburg University, Tilburg, The Netherlands
Department of Medical Decision Making, Leiden University Medical Center, Leiden, The Netherlands
c
VA Ann Arbor Center for Clinical Management Research, Ann Arbor, USA
d
Division of General Internal Medicine and Department of Psychology, University of Michigan, Ann Arbor, USA
e
Center for Bioethics and Social Sciences in Medicine, University of Michigan, Ann Arbor, USA
f
Vice-décanat à la pédagogie et au développement professionnel continu, Faculté de médecine, Université Laval, Quebec City, Canada
g
Département de médecine familiale et de médecine d’urgence, Faculté de médecine, Université Laval, Quebec City, Canada
h
University of Missouri, Department of Psychological Sciences, USA
b
A R T I C L E I N F O
A B S T R A C T
Article history:
Received 11 July 2012
Received in revised form 31 October 2012
Accepted 24 November 2012
Objective: To review the strengths and weaknesses of deliberative and intuitive processes in the context
of patient decision support and to discuss implications for decision aid (DA) design.
Methods: Conceptual review of the strengths and weaknesses of intuitive and analytical decision making
and applying these findings to the practice of DA design.
Results: DAs combine several important goals: providing information, helping to clarify treatment
related values, supporting preference construction processes, and facilitating more active engagement in
decision making. Many DAs encourage patients to approach a decision analytically, without solid
theoretical or empirical grounding for this approach. Existing research in other domains suggests that
both intuition and deliberation may support decision making. We discuss implications for patient
decision support and challenge researchers to determine when combining these processes leads to
better outcomes.
Conclusions: Intuitive and analytical decision processes may have complementary effects in achieving
the desired outcomes of patient decision support.
Practice implications: DA developers should be aware that tools solely targeted at supporting
deliberation may limit DA effectiveness and harm preference construction processes. Patients may
be better served by combined strategies that draw on the strengths and minimize the weaknesses of both
deliberative and intuitive processes.
ß 2012 Elsevier Ireland Ltd. All rights reserved.
Keywords:
Patient decision aids (DAs)
Values clarification methods (VCMs)
Preference construction
Decision making
Intuition
Deliberation
1. Introduction
1.1. Supporting patient decisions: current practices
In health care, individual treatment and screening decisions are
often preference sensitive, involving important trade-offs. For
example, available options can be equivalent in terms of medical
efficacy, but involve trade-offs between length and quality of life or
between comfort and efficacy of procedures. By taking individual
patient values into account, treatment and screening decisions can
be made so that they best fit an individual, with his/her unique
* Corresponding author at: Decision Psychologist, Tilburg Institute for Behavioral
Economics Research (TIBER), Department of Social Psychology, Tilburg University,
P.O. Box 90153, 5000 LE Tilburg, The Netherlands. Tel.: +31 13 466 8394;
fax: +31 13 466 2067.
E-mail address: MariekedeVries@TilburgUniversity.edu (M. de Vries).
1
Equal contribution.
situation, needs and desires [1–6]. However, putting this ideal into
practice is challenging. First, clinicians have been found to be
inaccurate at estimating patients’ values for health states [7] and
treatment options [8,9]. Moreover, in the novel, unanticipated, and
emotionally charged situations that many patients face, their
values and preferences are often labile or non-existent and need to
be clarified [10–12]. This clarification process can be complicated,
because potential outcomes and risks can be hard to verbalize and
imagine, and available options often involve trade-offs that make
them incommensurable [1,2].
In order to help patients make informed medical decisions that
reflect their personal values and circumstances, patient decision
aids (DAs) have become an increasingly common tool [5,6,13–17].
DAs combine several important goals, such as informing patients
about options, helping clarify patient values, supporting patients’
preference construction process, and enabling patients to more
actively engage in shared decision making with their health care
providers. DAs can, among other positive effects, enhance patients’
0738-3991/$ – see front matter ß 2012 Elsevier Ireland Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.pec.2012.11.016
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
2
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
involvement in medical decisions [3,5,6], and increase patients’
knowledge and contentment with the decision-making process
[4,5]. Yet the effects of DAs on decision quality and process
measures (e.g., decisional conflict, feeling clear about one’s values)
are not consistent [5].
DAs often incorporate values clarification methods (VCMs) to
help elicit patients’ treatment values and help patients make
decisions. Many VCMs encourage patients to follow deliberative,
analytical processes in comparing available choice options,
suggesting an assumption on the part of developers that
deliberation is the preferable strategy for making medical
decisions [18]. This assumption has strong historical precedent,
but lacks a solid theoretical or empirical grounding, and is in
conflict with what we know about natural human reasoning and
action, which are not purely analytical and depend strongly on
intuition [19–30].
In the present article we argue that the effectiveness of DAs, and
of VCMs in particular, may be enhanced by drawing on the
strengths and minimizing the weaknesses of both deliberative as
well as intuitive decision processes. For the purposes of the present
article, deliberative decision processes are defined as effortful,
conscious and analytical and include decision strategies such as
making lists of pros and cons, as well as explicitly rating and
weighting these pros and cons. By contrast, intuitive processes are
defined as less effortful and less conscious processes. For example,
implicit and apparently effortless integration of available information can give rise to affective responses and gut feelings on which
intuitive decisions can be based. Such affectively-based decisions
are an important subset of intuitive decisions, but there are other
types of intuitive decision processes, such as the reliance on fastand-frugal heuristics, as we will discuss in more detail later [4,31–
33]. Whereas deliberative and intuitive processes are not always
entirely distinct, they clearly have been shown to have different
effects on decision making [4,33,34].
1.2. Intuition and deliberation in patient decision making
Evidence from psychological literatures suggests that at least in
some contexts, deliberation may interfere with decision making,
and intuitive decision strategies sometimes result in better
outcomes [19,21,34]. As we will outline in more detail below,
encouraging patients to extensively deliberate about their
personal preferences may have some unintended, potentially
harmful implications. Yet encouraging patients to deliberate also
serves important goals, such as supporting patients in taking a
more active role in the decision-making process with their health
care providers.
In order to understand how to design DAs and VCMs so that
they result in the intended outcomes, we underscore the need to
better understand the nature of intuitive and deliberative decision
processes that are involved in patient decision making, and that are
likely to be affected by the design of DAs and VCMs [1,5,16,18,35].
In the present article we aim to (a) provide an in-depth treatment
of this issue, as well as (b) clarify how existing research findings
can serve as a framework for developing hypotheses about how
these decision tools may influence outcomes.
2. Strengths and pitfalls of intuition and deliberation in patient
decision support
Throughout western intellectual history, the dominant view
has been that decisions are best made via analytical reasoning, and
that feelings interfere with good, rational decision making [36].
Indeed, ample evidence has shown that reliance on heuristic
processing or initial emotional reactions (e.g., fear, panic, anger)
can cause bias and error [37–39]. However, an influential body of
research also suggests that intuitions may be surprisingly accurate,
because they can be based on an implicit integration of a large
amount of information [4,19–24,32–34,40]. In fact, when it comes
to making important personal decisions, rational reasoning seems
to strongly depend on intuitive processes [19–24]. In the following
sections, we will review literature that illuminates both these
strengths and weaknesses of intuitive and deliberative decision
making strategies.
2.1. Deliberative decision making: taxonomy of strengths and pitfalls
2.1.1. Strengths of deliberation
Deliberation serves several important goals in decision
making. First, deliberation is likely to help people articulate their
preferences. Deliberation may empower patients by enhancing
their ability to engage in the shared decision-making process, and
communicate what they want to physicians [6]. Moreover,
deliberation may help decision-makers articulate reasons for
their preferences, which may reduce uncertainty and decisional
conflict, and help patients communicate why they have certain
preferences [5].
A second advantage of deliberation is that after people
analyze reasons for the values they find important, they act more
value-congruently. For example, when people are asked to
analyze their reasons for why they find the value ‘‘helpfulness’’
important, they later behave in a more helpful manner [41]. In
the context of patient decision support, this could cause patients
to make decisions that are more consistent with earlier-stated
preferences and values. However, as we will discuss in more
detail later on, the preferences that people report after
deliberative reasoning may systematically underweight attributes that are difficult to articulate, but that may nonetheless be
important to the decision at hand.
A third benefit of deliberation is that it may fit patients’
expectations about how health decisions should be made. When a
person feels good about how a decision is made, this can affect how
the person feels about the quality of the decision itself [33,42,43].
For example, when people believe that mental effort is required to
get the best decision outcome, they may interpret their exertion of
mental effort as a signal that an optimal decision has been achieved
[43]. This suggests that if a patient believes that deliberation is the
optimal strategy for the decision at hand, then deliberative
decisions will be viewed more favorably than intuitive decisions,
irrespective of the actual benefit of either strategy.
Finally, DAs are explicitly designed to encourage patients to
follow the logic of utilitarian decision-making, based on the
assumption that this will help patients to make decisions that
maximize utility. Hence, a fourth potential strength of encouraging
patients to deliberate in a DA is that this encourages them to
explicitly consider the likelihood of different outcomes and the
values they attach to these outcomes, and to decide based on a
logical integration of these. However, as outlined below, explicitly
considering and integrating likelihoods and values associated with
different outcomes is a complex and error-prone process that may
not only help, but also harm decision making.
2.1.2. Pitfalls of deliberation
A growing body of evidence shows that deliberation also has
several important limitations, and may even be harmful to
preference construction. First, in the choices patients face, some
choice attributes evoke strong immediate emotions, such as
feelings of anxiety or depression. When experiencing negative
emotions, subsequent thinking will be likely to be emotioncongruent, sustaining and possibly even intensifying these initial
negative emotional reactions [44,45]. For example, prolonged
elaborative processing when experiencing feelings of depression
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
can exacerbate depression, as this ruminative response allows
depressed feelings to bias thinking in an emotion-congruent way
[44]. Hence, a VCM that encourages patients to deliberate about
emotion-evoking information immediately after being exposed to
it may result in emotion-congruent thoughts, which may then
sustain or intensify the initial emotional response. Immediate
deliberation may thus overshadow other potentially important
choice attributes, such as the likelihoods of risks and benefits.
Interestingly, follow-up research has shown that distraction after
exposure to emotion-evoking stimuli can attenuate negative
feelings [46]. Later, we will discuss these findings’ potential
usefulness for DA design.
A second disadvantage of deliberation is that people are often
unaware of factors that influence their choices [19]. As a
consequence, when probed for reasons why they favor or disfavor
various options, patients may invent reasons that seem plausible,
but that are not correct. Moreover, people frequently fail to identify
the factors that actually do influence their choices. In one classic
psychological experiment [47] participants were asked to choose
from an array of identical stockings. Most people had a bias toward
choosing one of the right-most stockings. However, when asked
why they chose that particular stocking, none of the participants
realized that the position influenced their choice, and instead they
invented other reasons (e.g. ‘‘This one was the softest’’). This
phenomenon—given the apt title ‘‘Telling more than we can
know’’—is particularly relevant for patient decision making,
because it raises questions about patients’ ability to accurately
articulate the reasons for their preferences. If decision makers
cannot articulate the reasons for their preferences after a decision
is made, then asking patients to do so as part of the decision
making process could lead them to a decision they might not
otherwise make.
A third drawback of deliberation is that the act of verbalization
of reasons for one’s preferences can decrease decision satisfaction
and agreement between people’s judgments and expert opinions
[48–51]. Deliberation tends to cause people to focus on just a select
few reasons for choosing one option over another. Because of
failures of introspection, these reasons may not actually be the
most important, or even the real reasons for one’s preferences.
Instead, they are likely to be the reasons that are easiest to
articulate. As a result, deliberative reasoning can temporarily alter
one’s perception of which option is the best. This phenomenon has
been shown across a range of judgments, ranging from choices
between decorative posters to ratings of Olympic dives [48–51].
For example, in one experiment [48], students were brought into a
research laboratory and asked to view five posters and select one to
take home. Half of the students simply chose a poster, the rest were
instructed to list what they liked and disliked about each poster
prior to making their choice. Weeks later, the researchers
contacted the students and asked them whether the poster was
still on their wall. Students who chose the poster based on their
intuition were happier with their choice, and were more likely to
have it on their wall, than students who made lists. The
deliberative decision-makers chose posters on the basis of the
attributes that appeared on their lists, and these lists mostly
included attributes that were easy to articulate. Hence, participants’ lists biased them toward choosing the posters on the basis of
a particular attribute (e.g. humor) that was not related to longterm liking. This research suggests that deliberation can cause
people to disproportionally focus on attributes that are obvious,
accessible, and easy to articulate, but that are not necessarily most
important [4,19].
One corollary finding involving deliberation is that more
thought, and less reliance on emotive cues, leads to less stability
in preferences across time. That is, people tend to change their
mind more often when they deliberate [52,53]. Hence, when it
3
comes to preference-based decisions, deliberative strategies often
fail to arrive at judgments that consistently maximize utility.
2.1.3. Summary of the strengths and pitfalls of deliberative decision
making
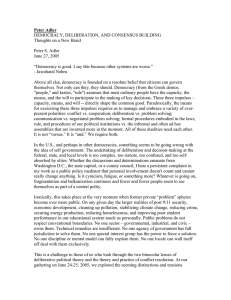
The second column of Table 1 represents an overview of the
above mentioned strengths and pitfalls of deliberation. In sum,
deliberation is likely to have several beneficial effects on decision
making: (1) it may help patients verbalize and articulate their
preferences and generate reasons for those preferences, (2) it may
help patients make decisions that are more congruent with their
stated preferences, (3) deliberation may help patients feel better
about how the decision was made, because it fits their expectations
about how such decisions ought to be made, and (4) it encourages
patients to explicitly consider the likelihood of different outcomes
and the values they attach to these outcomes, and to decide based
on a presumably logical integration of these. However, deliberative
strategies also possess a number of disadvantages, which together
suggest that deliberation does not always lead to a rational
integration of factual knowledge: (1) deliberative strategies may
cause emotion-congruent thoughts that intensify, rather than
abate, negative emotions, (2) they may cause patients to generate
reasons for their preferences that are inaccurate, and (3) they may
cause patients to focus on just a few salient treatment attributes,
and under-weight attributes that may be equally important but
more difficult to articulate.
2.2. Intuitive decision making: taxonomy of strengths and pitfalls
2.2.1. Strengths of intuition
Just like deliberation, intuitive processes also serve several
important goals in decision making, with some potentially
important implications for patient decision support. In particular,
over the past 20 years psychological evidence has shown that
compared to deliberative decision strategies, intuitive strategies
often result in better judgments and decisions, are more in line
with expert opinion, are more accurate, or result in higher
satisfaction [4,19,21,22].
The first advantage of intuitive decision making is that it is more
likely than deliberation to rely on automatic and/or unconscious
cognitive processes. Many of our mental processes take place
automatically, and in our everyday behavior we are largely
dependent on these automatic processes [20]. Importantly, these
processes are thought to be less limited in capacity than
deliberation, and therefore to be able to integrate larger amounts
of information [23,24,54–57]. Implicit integration of information
thereby results in a feeling toward various options that can reflect
the optimal choice with remarkable accuracy [23,24,41,55,57,58].
To illustrate this phenomenon, one study [40] asked participants to
view advertisements for an upcoming memory test. While viewing
the advertisements, information about stocks ran at the bottom of
a computer screen (stock information was irrelevant to the main
task). At the end of the experiment, participants were not able to
report which stock had the highest value, but when asked how
they felt toward each stock, their ratings accurately reflected the
actual stock value [40]. Such findings suggest that automatic
integration of information can result in feelings that do not
necessarily have a consciously accessible explanation but that are
nonetheless accurate [23,24,40,47,55].
Second, intuition may also provide an advantage in decision
making because compared to deliberation it is more sensitive to–
and better able to incorporate–feelings and affective cues in the
process of preference construction. That is, intuitive processing not
only results in feelings towards choice options in the form of
overall impressions of decision options, but it may also rely more
strongly on affective cues that can be of vital importance in
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
4
Table 1
Overview of decision maker goals, strengths and pitfalls of intuition and deliberation in preference construction and shared decision making and their implications for the
design of decision aids. Note: Goals, strengths, pitfalls and their implications are horizontally aligned.
Goals for decision making
Strengths and pitfalls of deliberation
Feeling good about decision
making process
Strength: fits expectations about
how medical decisions ought to be
made
Strength: may help to take all
relevant information into account
Acquiring all relevant information
Making decision congruent
with stated preferences, avoiding
heuristics and biases
Being able to explain preferences
and decision to others
Strength: facilitates decisions that
are congruent with stated
preferences (note that stated
preferences may not be accurate
due to faulty explicit reasoning)
Strength: facilitates verbalization
of preferences and reasons for
preferences
Incorporating all relevant attributes
into decision . . .
Pitfall: may focus attention on just
a few salient treatment attributes,
and under-weight attributes that
are difficult to articulate
. . . even if they are difficult to explain.
Pitfall: may cause patients to
generate inaccurate reasons for
their preferences
Avoiding making decisions in the
grip of strong emotions like fear
and panic.
Pitfall: intensification of negative
emotions
preference construction processes. Indeed, there is growing
acknowledgement that feelings and emotions are critical sources
of information for decision making [1,4,23,24]. As a classic
example, patients who have damage to the ventromedial
prefrontal cortex of the brain show impaired decision making,
in spite of having intact intellect and moral reasoning [58].
According to the ‘‘somatic marker hypothesis,’’ these patients have
deficits in emotional processing, and this emotion-specific deficit
makes it impossible to decide which option should be chosen, or
which course of action is best [24].
To illustrate this point empirically, researchers developed a
gambling task in which participants draw from four decks of
cards. On each draw, participants either lose or gain play money.
Two of the decks are stacked so that there are large gains, but also
large losses (the risky decks), resulting in a net loss of money. The
other two decks are stacked so that the gains are initially smaller
than those of the risky decks, but over time there is a net gain of
money, as losses are also smaller in these decks. Findings
consistently show that healthy participants learn to avoid the
risky decks, and show physiological signs of anxiety (e.g.
sweating) before drawing from that deck, even before they can
explicitly articulate why they prefer one deck over the other.
However, patients with damage to the prefrontal cortex do not
learn to avoid the risky decks, and show no physiological signs of
emotional distress when drawing from those decks. These
findings suggest that emotional cues, so called ‘‘somatic
markers’’ (e.g., sweating), can serve as an important signal for
making effective decisions [23,24]. Consistent with the idea that
affective cues can guide decision-making, it has recently been
proposed that affect may help patients make trade-offs between
options that are difficult to compare, such as choosing between
the quality versus quantity of life. In these situations, our
intuitive feelings help by serving as the ‘‘common currency’’
between logically incommensurable options [2].
Strengths and pitfalls of intuition
Potential implications for patient decision making support
Incorporate deliberative steps in
decision making support
Pitfall: may lead to uninformed
decisions when applied to early
stages of decision making, such as
information accrual
Pitfall: vulnerable to heuristics and
biases (but this may also be true of
deliberative strategies)
Encourage patients to become
informed and learn about each option
before making a decision
Pitfall: lacks logical-sounding
reasons and face validity that could
help to convince self and others
that decision is good
Strength: may rely on affective cues
that are based on larger amounts of
information and that weigh
information accurately, in spite of
lack of articulable reasons for those
feelings
Strength: may allow people to
compare options that are difficult
to compare using analytical
reasoning (i.e. provides a common
currency)
Encourage patients to articulate their
preferences for the purpose of
communicating to others
Present information so that heuristics
and biases are less likely to occur. Use
debiasing tools and strategies
Encourage patients to postpone
judgments, and instead form overall
impressions of all options first
Encourage patients to consider and
articulate their feelings, even if they
cannot provide reasons for those
feelings
Introduce distraction/delay to let
strong emotions abate prior to
deliberation
It is important to note that intuition serves as an umbrella
term, referring to the implicit and apparently effortless integration of information [4]. One example of automatic processing has
been widely influential—yet also highly controversial—in promoting intuition as an advantageous decision strategy. This
research suggests that after exposure to a decision problem, a brief
period of distraction can result in improved judgments and
decisions [59–62]. For example, in one experiment, participants
were asked to consider four hypothetical apartments, each of
which was described by twelve attributes [59]. One of the
apartments was an objectively better choice than the others, but
this best choice was not obvious, due to the large amount of
information presented. Participants who performed a distracting
task for a few minutes prior to their choice were more likely to
choose the objectively better apartment than participants who
deliberated and participants who decided immediately. This
effect has been labeled the Unconscious Thought Effect (UTE),
because it is assumed that the distracting task allows the
unconscious mind to integrate and weigh the relevant information. Yet a recent meta-analysis of 92 studies concluded that
distraction does not universally lead to better decisions. Instead,
distraction is most likely to lead to better decisions when the
decision is complex, when verbal and pictorial information
formats are combined, and when the information is ordered by
choice option rather than by attributes [62].
2.2.2. Pitfalls of intuition
Despite the importance of intuitive processes in decision
making, there are also some critical pitfalls associated with
reliance on intuition. First, decades of research have shown that
reliance on heuristic strategies and on strong, immediate
emotional reactions can cause bias and error in decision making
[38,39,63]. At this point there are countless biases that have been
documented in human judgment (e.g. recognition, framing,
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
anchoring, availability, conjunction fallacy, contrast effects), and
many of these biases have been attributed to failures of human
intuition. Consistent with this idea, research has shown that
the activation of deliberative processing can indeed reduce the
prevalence of various biases and heuristics [64]. However, some
heuristics (e.g. recognition) are actually more likely when
judgments are made deliberatively rather than intuitively [65].
Furthermore, although individuals who habitually use rational/
analytic processing are less likely to succumb to some types of
biases, they are equally—if not more—susceptible to other biases
[66–68]. In fact, recent evidence suggests that individuals who are
high in both rational and intuitive thinking styles are less
susceptible to heuristic biases than individuals who are highly
rational but not intuitive [69]. Hence, heuristics and biases are
indeed a disadvantage of intuition, but it appears that some biases
are not specific to intuition and rather are errors of human
judgment more generally.
A second disadvantage of intuitive decision strategies is that
they may make it difficult for patients to articulate the reasons for
their preferences. When patients lack plausible-sounding reasons
for their decisions, it may invite skepticism from health care
professionals, family and friends, or cause patients to feel
uncertain themselves.
Third, intuitive strategies may be more or less appropriate at
different stages of the decision making process. Recently, Pieterse
and De Vries [4] provided an analysis of the suitability of fast-andfrugal heuristics in the patient decision support context,
concluding that heuristics can be detrimental when they
encourage patient decision-makers to focus only on a subset of
the information provided in the DA. In other words, when fast,
intuitive strategies cause people to fail to acquire relevant
information, this can result in uninformed, poor decisions.
2.2.3. Summary of the strengths and pitfalls of intuitive decision
making
In this section, we reviewed theorizing and research addressing the strengths and pitfalls of intuition in preference
construction and decision making (see Table 1, third column,
for an overview). In sum, intuitive strategies have at least two
powerful advantages: (1) intuitive decisions are often based on
implicit information integration, which can integrate large
amounts of information and result in feelings that are surprisingly
accurate, and (2) intuitive decision making may be relatively more
influenced by, and dependent on, the presence of lower-order,
subtle affective cues. Indeed, the human mind seems to be wired
so that higher-order processes cannot function properly without
being grounded in lower-order, intuitive processes. However,
intuitive strategies also have a number of drawbacks: (1) they can
be influenced by heuristics and biases (but this may also be true of
deliberative strategies), (2) they lack logical-sounding reasons
that could help to convince others (and possibly also oneself) that
the decision is good, and (3) when intuitive strategies are applied
to early stages of decision making, such as information accrual,
they may lead to uninformed decisions.
3. Discussion and conclusion
3.1. Discussion: targeting intuition and deliberation in patient
decision support
A long-held assumption in patient decision making research is
that careful thought and reflection about medical choices should
lead to more positive outcomes, greater choice satisfaction, less
uncertainty, and less anxiety. Yet, our review of the decision
literature reveals a more nuanced picture. The evidence reviewed
in this paper suggests that deliberation may have intended
5
beneficial effects on facilitation of patient engagement. It also
encourages patients to become well-informed and follow the logic
of utilitarian decision-making. Patients may believe that deliberation is more appropriate than intuition, and therefore deliberation
may be viewed more favorably regardless of its actual effect on
decisions. However, deliberation can also produce biases and error
of its own: In particular, it can cause people to generate erroneous
reasoning which may negatively affect their preferences and
decisions, as well as cause people to focus on a few accessible
attributes that are not actually the most important. Our review of
the strengths and pitfalls of intuitive decision processes complements this picture. It indicates that, while heuristic processing and
reliance on strong, immediate emotional reactions can cause bias
and error, more sophisticated intuitive processes play a crucial role
in preference construction. Intuitive processes may allow people to
integrate larger amounts of information and to better use accurate
affective cues, thereby helping patients make difficult trade-offs
between dimensions that are hard to compare (e.g. the quality vs.
quantity of life; 1, 2, 4).
Some of the findings reviewed in this manuscript stem from
other research areas such as basic psychology and consumer
research. One objection to applying these findings to medical
decision making is that the decisions studied in basic research are
mostly simple and inconsequential consumer choices. Decision
processes in a consumer context may in some respects be
inherently different from choosing between medical options. For
example, medical decisions are sometimes made under distressing
conditions and can evoke strong emotions. Due to these strong
emotions these decisions are often avoided or approached in a
defensive manner. Even less dramatic medical decisions often
involve qualitatively different options than decisions made in a
consumer context. That is, unlike consumer choices where
decisions are being made about gains (i.e., goods or services a
consumer wishes to acquire), medical decisions typically involve
zero-gain or loss-minimizing options.
However, findings from other research areas nevertheless
illustrate important features of the architecture of the human
mind, such as how faulty reasoning can influence preference
construction, and how deliberation can focus attention on just a
few salient attributes. The existence of these psychological
processes calls into question the assumption that deliberative
thought necessarily renders optimal preferences and utilitymaximizing judgments. Moreover, these literatures suggest that
there are a number of counterintuitive ways in which intuitive
and deliberative thought modes influence decision making,
which are not yet fully realized in theoretical approaches to
decision aids. Even though medical decisions may indeed often
be more emotional than decisions that have been studied in other
contexts and involve zero-gain or loss-minimizing instead of
gain-maximizing options, we would still expect many of these
psychological phenomena to apply. For example, so long as the
less important decision attributes are easier to articulate than
the more important attributes, then we might expect that
deliberation can bias decision making. In fact, if anything, these
effects might be stronger when the situation is more emotionally
evocative, as deliberation may cause emotion-congruent
thoughts that intensify these emotions. Yet clearly future
research should investigate whether the same basic psychological mechanisms, for example, cause patients to disproportionally
focus on attributes that are emotionally evocative, salient, or
easy to articulate, overshadowing other important attributes to
the detriment of their eventual decision. The challenge,
therefore, is to gain a more fundamental understanding of
how we can support patients to be more engaged and informed
decision-makers, without causing unintended side-effects that
may harm their preference construction processes.
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
6
Together, the literatures that we reviewed suggest that both
intuition and deliberation are critical components in patient
decision making, but serve different goals in the patient decision
support context. Indeed, these processes might work best when
working together. Recently there has been evidence for precisely
this idea, insofar as experimental tests of the effects of intuitive
and deliberative decision strategies have shown that a combination of both resulted in the best decision outcomes [70]. It
could very well be the case that decision support is most
effective when it targets deliberative as well as intuitive
processes.
How can we combine the best of both intuition and
deliberation in patient decision making? In the right column
of Table 1, we provide an overview of potential implications for
patient decision support based on the identified strengths and
pitfalls of deliberation and intuition. The first two recommendations that follow from our analysis are already being implemented by DA developers: First, as many DA developers already
know, it is important to explicitly encourage patients to become
informed and learn about each option before making a decision.
This is because decision heuristics that are applied before
patients are informed are quite error-prone. Second, care should
be taken so that information is presented in such a way that
heuristics and biases are minimized. For example, people
generally have more favorable impressions of a treatment if
they learn it has a 90% survival rate rather than a 10% death rate
[71]. Hence, numerical information should be presented in both
formats (survival and death rates) in order to prevent this bias
from occurring.
Yet there are a number of additional and unique insights that
follow from the preceding review. First, although it may indeed be
helpful to encourage patients to articulate their preferences and
the reasons they have for their preferences, this exercise may be
better placed late in the decision process. This is because reasoning
about preferences early in the decision process (e.g. right after
exposure to new information) may be harmful to preference
construction, as it can focus attention away from decision
attributes that are relatively difficult to verbalize.
Second, when introduced too early, reasoning may cause bias
through the intensification of strong emotions evoked by the
content of the DA. Hence, patients could be encouraged (through
instructions in the DA) to delay making a decision and instead to
allow themselves to form more nuanced feelings and general
impressions of each of the options. Patients could benefit from
being encouraged to consider these overall impressions and
feelings about choice options, even if they cannot provide reasons
for them.
A third and related implication of this review is that a
distraction or delay could be useful after information has been
provided, because it could allow strong emotions to abate prior to
deliberation. This way, strong emotions that are linked to only a
part of the picture (e.g., fear for a potential outcome) would be less
likely to overshadow the rest of the decision.
3.2. Conclusion
The available findings reviewed here suggest that intuitive
and analytical decision processes have complementary effects in
achieving the desired outcomes of patient decision support. It is
our hope that this analysis of the strengths and weaknesses of
intuitive and deliberative decision processes, and their potential
implications for DA design, will contribute to the understanding
of how DAs—and VCMs in particular—can be designed and
evaluated. The ultimate goal is that DAs fit more closely with
how the human mind is naturally wired, resulting in increased
effectiveness.
3.3. Practice implications
DA developers should be aware that the current common
practice to encourage patients to extensively analyze available
choice options, typically immediately after information exposure,
lacks solid theoretical and empirical grounding. This practice may
limit potential DA effectiveness in supporting patient decision
making, and may even have some harmful side effects to
preference construction processes. Therefore, developers should
be encouraged to target, and evaluate the strengths and weaknesses of, both deliberative and intuitive decision processes, so
that future DAs and VCMs make the best use of all of patients’
decision making capabilities.
Conflict of interest
None.
Acknowledgements and funding
This work has been supported by an EASP Seedcorn Grant to
Marieke de Vries and Informed Medical Decisions Foundation
George Bennett Postdoctoral Grants to Laura Scherer and Holly
Witteman.
References
[1] Epstein RM, Peters E. Beyond information: exploring patients’ preferences. J
Am Med Assoc 2009;302:195–7.
[2] Kerstholt JH, van der Zwaard F, Bart H, Cremers A. Construction of health
preferences: a comparison of direct value assessment and personal narratives.
Med Decis Making 2009;29:513–20.
[3] Power TE, Swartzman LC, Robinson JW. Cognitive-emotional decision making
(CEDM): a framework of patient medical decision making. Patient Educ Couns
2010;83:163–9.
[4] Pieterse AH, De Vries M. On the suitability of fast and frugal heuristics for
designing values clarification methods in patient decision aids: a critical
analysis.
Health
Expect
2011.
http://dx.doi.org/10.1111/j.13697625.2011.00720.x.
[5] Stacey D, Bennett CL, Barry MJ, Col NF, Eden KB, Holmes-Rovner M, et al.
Decision aids for people facing health treatment or screening decisions (Review). Cochrane Collaboration 2011.
[6] Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Légaré F, Montori
VM, et al. Shared decision making: really putting patients at the centre of
healthcare. Brit Med J 2012;344. http://dx.doi.org/10.1136/bmj.e256 [published 27 January 2012].
[7] Cotler SJ, Patil R, McNutt RA, Speroff T, Banaad-Omiotek G, Ganger DR, et al.
Patients’ values for health states associated with hepatitis C and physicians’
estimates of those values. Am J Gastroenterol 2001;96:2730–6.
[8] Brothers TE, Cox MH, Robison JG, Elliott BM, Nietert P. Prospective decision
analysis modelling indicates that clinical decisions in vascular surgery often
fail to maximize patient expected utility. J Surg Res 2004;120:278–87.
[9] Fraenkel L, Bogardus ST, Concato J, Wittink DR. Treatment options in knee
osteoarthritis: the patient perspective. Arch Int Med 2004;164:1299–304.
[10] Fischhoff B. Value elicitation: is there anything in there? Am Psychol
1991;46:835–47.
[11] Simon D, Krawczyk DC, Bleicher A, Holyoak KJ. The transience of constructed
preferences. J Behav Decis Making 2008;21:1–14.
[12] Slovic P. The Construction of Preference. Am Psychol 1995;50:364–71.
[13] Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, et al. Developing a
quality criteria framework for patient decision aids: online international
Delphi consensus process. Brit Med J 2006;333:417–21.
[14] Molenaar S, Sprangers MAG, Postma-Schuit FCE, Rutgers EJTh, Noorlander J,
Hendriks J, et al. Feasibility and effects of decision aids. Med Decis Making
2000;20:112–27.
[15] Bekker HL. The loss of reason in patient decision aid research: do checklists
damage the quality of informed choice interventions? Patient Educ Couns
2010;78:357–64.
[16] Duggan PS, Geller G, Cooper LA, Beach MC. The moral nature of patientcenteredness: is it ‘‘just the right thing to do’’? Patient Educ Couns
2006;62:271–6.
[17] Waljee JF, Rogers MAM, Alderman AK. Decision aids and breast cancer: do they
influence choice for surgery and knowledge of treatment options? J Clin Oncol
2007;25:1067–73.
[18] Nelson WL, Han PK, Fagerlin A, Stefanek M, Ubel PA. Rethinking the objectives
of decision aids: a call for conceptual clarity. Med Decis Making 2007;27:609–
18.
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016
G Model
PEC-4423; No. of Pages 7
M. de Vries et al. / Patient Education and Counseling xxx (2012) xxx–xxx
[19] Wilson TD. Strangers to ourselves: discovering the adaptive unconscious.
Cambridge, MA: Harvard University Press; 2002.
[20] Bargh JA. The automaticity of everyday life. In: Wyer SR, editor. Advances in
social cognition, vol. 10. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 1997.
p. 1–61.
[21] Klein G. Intuition at work: why developing your gut instincts will make you
better at what you do. New York: Doubleday; 2003.
[22] Sadler-Smith E. Inside intuition. London: Routledge; 2008.
[23] Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before
knowing the advantageous strategy. Science 1997;275:1293–5.
[24] Damasio AR. Descartes’ error: emotion, reason, and the human brain. London:
Macmillan; 1994.
[25] Kahneman D. A perspective on judgment and choice: mapping bounded
rationality. Am Psychol 2003;58:697–720.
[26] Lee L, Amir O, Ariely D. In search of homo economicus: cognitive noise and the
role of emotion in preference consistency. J Consum Res 2009;36:173–87.
[27] Schwarz N, Clore GL. Feelings and phenomenal experiences. In: Higgins ET,
Kruglanski A, editors. Social psychology: handbook of basic principles. 2nd ed.,
New York: Guilford Press; 2007. p. 385–407.
[28] Zajonc RB. Feeling and thinking: preferences need no inferences. Am Psychol
1980;35:151–75.
[29] Damasio AR. Self comes to mind: constructing the conscious brain. New York:
Pantheon; 2010.
[30] Aarts H, Custers R, Marien H. Preparing and motivating behaviour outside of
awareness. Science 2008;319:1639.
[31] Betsch T. The nature of intuition and its neglect in research on judgment and
decision making. In: Plessner H, Betsch C, Betsch T, editors. Intuition in
judgment and decision making. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 2008. p. 3–22.
[32] Glöckner A, Betsch T. Multiple-reason decision making based on automatic
processing. J Exp Psychol Learn Mem Cogn 2008;34(5):1055–75.
[33] De Vries M, Holland RW, Witteman CLM. Fitting decisions: mood and intuitive
versus deliberative decision strategies. Cogn Emotion 2008;22(5):931–43.
[34] Hogarth RM. Deciding analytically or trusting your intuition? The advantages
and disadvantages of analytic and intuitive thought. In: Haberstroh S, Betsch
T, editors. The routines of decision making. Mahwah, NJ: Lawrence Erlbaum
Associates, Inc; 2005.
[35] Charles C, Gafni A, Whelan T, O’Brien MA. Treatment decision aids: conceptual
issues and future directions. Health Expect 2005;8:114–25.
[36] Von Neuman J, Morgenstern O. Theories of games and economic behavior.
Princeton, NJ: Princeton University Press; 1947.
[37] Tversky A, Kahneman D. Judgment under uncertainty – heuristics and biases.
Science 1974;185:1124–31.
[38] Kahneman D, Tversky A. Prospect theory – analysis of decision under risk.
Econometrica 1979;47:263–91.
[39] Loewenstein G. Out of control: visceral influences on behaviour. Organ Behav
Hum Decis Process 1996;65:272–92.
[40] Betsch T, Plessner H, Schwieren C, Gutig R. I like it but I don’t know why: a
value-account approach to implicit attitude formation. Pers Soc Psychol B
2001;27:242–53.
[41] Maio GR, Olson JM, Allen L, Bernard MM. Addressing discrepancies between
values and behaviour: the motivating effects of reasons. J Exp Soc Psychol
2001;37:104–17.
[42] Higgins ET, Idson LC, Freitas AL, Spiegel S, Molden DC. Transfer of value from
fit. J Person Soc Psychol 2003;75:617–38.
[43] Labroo AA, Kim S. The ‘‘Instrumentality’’ heuristic: why metacognitive difficulty is desirable during goal pursuit. Psychol Sci 2009;20:127–34.
[44] Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. J Abnorm Psychol 1993;102:20–8.
[45] Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can’t shake that
feeling: assessment of sustained event-related fMRI amygdala activity in
[46]
[47]
[48]
[49]
[50]
[51]
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
[71]
7
response to emotional information in depressed individuals. Biol Psychiat
2002;51:693–707.
Van Dillen L, Koole SL. Clearing the mind: a working memory model of
distraction from negative mood. Emotion 2007;7:715–23.
Nisbett RE, Wilson TD. Telling more than we can know: verbal reports on
mental processes. Psychol Rev 1977;84:231–59.
Wilson TD, Schooler JW. Thinking too much: introspection can reduce the
quality of preferences and decisions. J Pers Soc Psychol 1991;60:181–92.
Halberstadt J, Green J. Carryover effects of analytic thought on preference
quality. J Exp Soc Psychol 2008;44:1199–203.
Wilson TD, Dunn DS. Effects of introspection on attitude – behavior consistency: analyzing reasons versus focusing on feelings. J Exp Soc Psychol
1986;22:249–63.
Wilson TD, Hodges SD, LaFleur SJ. Effects of introspecting about reasons:
inferring attitudes from accessible thoughts. J Pers Soc Psychol 1995;69:16–
28.
Lee L, Amir O, Ariely D. In search of homo economicus: cognitive noise and the
role or emotion in preference consistency. J Cons Res 2009;36:173–87.
Nordgren LF. The devil is in the deliberation: thinking too much reduces
preference consistency. J Cons Res 2009;36:39–46.
Nørretranders T. The user illusion: cutting consciousness down to size. New
York: Viking; 1998.
Dijksterhuis A, Nordgren LF. A theory of unconscious thought. Psychol Sci
2006;1:95–109.
Lewicki P, Hill T, Bizot E. Acquisition of procedural knowledge about a pattern
of stimuli that cannot be articulated. Cogn Psychol 1988;20:24–37.
Betsch T, Glöckner A. Intuition in judgment and decision making: extensive
thinking without effort. Psychol Inq 2010;21:279–94.
Damasio AR. Emotion and reason in the future of human life. In: Cartledge B,
editor. Mind, brain, and the environment: the Linacre Lectures 1995-6. New
York, NY, US: Oxford University Press; 1998. p. 57–71.
Dijksterhuis A. Think different: the merits of unconscious thought in preference development and decision making. J Person Soc Psychol 2004;87:586–98.
Dijksterhuis A, Bos MW, Nordgren LF, Van Baaren RB. On making the right
choice: the deliberation-without-attention effect. Science 2006;311:1005–7.
De Vries M, Witteman CLM, Holland RW, Dijksterhuis A. The unconscious
thought effect in clinical decision making: an example in diagnosis. Med Decis
Making 2010;30:578–81.
Strick M, Dijksterhuis A, Bos MW, Sjoerdsma A, van Baaren RB, Nordgren LF. A
meta-analysis on unconscious thought effects. Soc Cogn 2011;29:738–62.
Kahneman D. Thinking fast and slow. New York, NY: US, Farrar, Straus &
Giroux; 2011.
Alter AL, Oppenheimer DM, Epley N, Eyre RN. Overcoming intuition: metacognitive difficulty activates analytic reasoning. J Exp Psychol Gen
2007;136:569–76.
Hilberg BE, Scholl SG, Pohl RF. Think or blink – is the recognition heuristic an
‘‘intuitive’’ strategy? Judg Decis Making 2010;5:300–9.
Shiloh S, Salton E, Sharabi D. Individual differences in rational and intuitive
thinking styles as predictors of heuristic responses and framing effects. Pers
Indiv Differ 2002;32:415–27.
Stanovich KE, West RF. Individual differences in rational thought. J Exp Psychol
Gen 2008;127:161–88.
West RF, Meserve RJ, Stanovich KE. Cognitive sophistication does not attenuate the bias blind spot. J Pers Soc Psychol 2012. http://dx.doi.org/10.1037/
a0028857 [advance online publication].
Ayal S, Hochman G, Zakay D. Two sides of the same coin: Information
processing style and reverse biases. Judg Decis Making 2011;6:295–306.
Nordgren LF, Bos MW, Dijsterhuis A. The best of both worlds: integrating
conscious and unconscious thought best solves complex decisions. J Exp Soc
Psychol 2011;47:509–11.
McNeil BJ, Pauker SG, Sox HC, Tversky A. On the elicitation of preferences for
alternative therapies. N Engl J Med 1982;306:1259–62.
Please cite this article in press as: de Vries M, et al. Combining deliberation and intuition in patient decision support. Patient Educ Couns
(2012), http://dx.doi.org/10.1016/j.pec.2012.11.016