Insights into the physiologic significance of the mitral inflow velocity
advertisement

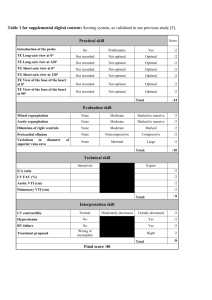
1718 JACC Vol. 14, No. 7 December 1989:171&20 Editorial Comment Insights Into the Physiologic Significance of the Mitral Inflow Velocity Pattern* ROBERT A. LEVINE, JAMES D. THOMAS, Boston, MD, FACC, MD, FACC Massachusetts The ability to measure mitral inflow velocities by Doppler echocardiography has allowed us to examine left ventricular filling noninvasively (1,2). Initially, the availability of this information generated great enthusiasm for extracting intrinsic diastolic properties of the left ventricle from a simple analysis of these velocities, in particular, the early and late diastolic filling velocities (the E and A waves) and their ratio. This initial enthusiasm has been tempered by the growing realization that inflow patterns result from a complex amalgam of ventricular, atria1 and mitral valve properties and are profoundly influenced by superimposed loading conditions (3-5). Because of these multiple determinants, similar mitral inflow patterns could appear in different clinical settings if the time course of the transmitral pressure gradient is similar in those conditions. The hypertrophic pattern versus decreased preload. One of the earliest characteristic abnormal patterns described (6-8) was the diminished early filling (E) wave and decreased E/A wave ratio in patients with hypertrophic cardiomyopathy. These findings were explained by delayed ventricular relaxation causing relatively high early diastolic left ventricular pressures and, therefore, a relatively low early diastolic gradient across the mitral valve. More recently, however, a similar pattern has been reproduced simply by decreasing left-sided filling pressures without intrinsic myocardial changes, for example, by nitroglycerin infusion: the de- *Editorials published in Journal of the American College of Cardiolog reflect the views of the authors and do not necessarily represent the views of JACC or the American College of Cardiology. From the Noninvasive Cardiac Laboratory, Massachusetts General Hospital, Department of Medicine, Harvard Medical School, Boston, Massachusetts. Dr. Levine is a Clinician-Scientist of the American Heart Association, with funds contributed by its Massachusetts Affiliate. This study was supported in part by Grant-in-Aid 13-532-867 from the American Heart Association, Massachusetts Affiliate, Inc., Boston, Massachusetts (Dr. Thomas); by Grant HL-38176from the National Institutes of Health, Bethesda, Maryland; and grants from the Whitaker Foundation, Mechanicsburg, Pennsylvania and the American Heart Association, Dallas, Texas (Dr. Levine). Address for renrints: Robert A. Levine, MD, Cardiac Ultrasound Laboratory, Phillips House 8, Massachusetts General Hospital, Boston, Massachusetts 02114. 01989 by the American College of Cardiology Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 creased left atria1 pressure lowers the early diastolic gradient and the corresponding E wave velocity (29-12). Conversely, the classic pattern in hypertrophic cardiomyopathy can be masked by associated mitral regurgitation, which raises left atria1 pressure (7). The restrictive pattern. Another distinctive filling pattern has been observed in restrictive cardiomyopathy (13-15). The early filling wave rapidly decelerates from its peak as left ventricular pressure rises rapidly in early diastole, and the late filling (A) wave is variably reduced, presumably by the high diastolic ventricular pressures. The E/A wave ratio is consequently increased, and the elevated ventricular pressures cause late diastolic mitral regurgitation in some patients. The effect of severe aortic regurgitation. This restrictive pattern is mimicked by that now described by Oh et al. (16) in this issue of the Journal in severe aortic insufficiency of relatively acute onset. In 11 patients with this condition, the early filling velocity was higher than in matched normal control subjects and decelerated more rapidly from its peak; the late filling wave tended to be smaller, and the E/A wave ratio was abnormally high-changes that could be reversed by surgical repair. Late diastolic mitral regurgitation also occurred in 8 of the 11 patients. Understanding these results in aortic regurgitation. Our understanding of these findings is improved by relating them to the fundamental determinants of transmitral flow. We have described (3,4) a mathematical model of ventricular filling that uses atria1 compliance, ventricular compliance and relaxation, and mitral valve morphology to predict the time course of atria1 and ventricular pressure and mitral velocity. The effect of aortic regurgitation can be studied by including aortic pressure and regurgitant orifice area in this model (giving five coupled nonlinear differential equations that must be solved simultaneously). The advantage of such analysis is that it allows us to isolate primary causes from secondary effects on the transmitral velocity pattern. For instance, Figure 1A shows the isolated effect of increasing aortic regurgitant orifice area with all other parameters held at roughly physiologic values (mitral area = 4 cm2, exponential pressure-volume curves for the atrium and ventricle, ventricular relaxation time constant = 40 ms, initial left atria1 pressure = 10 mm Hg, aortic pressure = 100 mm Hg). As the aortic regurgitant orifice area increases from 0 to 0.6 cm2, the early filling wave undergoes profound changes, with peak velocity falling from 71 to 43 cm/s and deceleration time shortening from 124 to 66 ms. These changes reflect the rising ventricular pressure, which decreases the pressure gradient across the mitral valve. The filling volume for this portion of diastole falls from 37.4 to 15.7 cm’. Thus, the isolated effect of worsening aortic regurgitation 0735.1097/89/$3.50 LEVlNE AND THOMAS EDITORIAL COMMENT JACC Vol. 14. No. 7 December lY89:1718-XI Figure 1. Competing effects of worsening aortic regurgitation (AR) and left atrial (LA) pressure on the configuration of the early mitral filling wave. A, Enlarging the aortic regurgitant orifice area (AROA) decreases peak E wave velocity (E) and shortens deceleration time (DT). B, For a 0.6 cm’ aortic regurgitant orifice area, increasing left atrial pressure (LAP) at the mitral valve opening raises peak velocity dramatically (137%) with a relatively minor (24%) increase in deceleration time. Note that the smallest curves in the two graphs display the same data (AROA = 0.6 cm’. LAP = IO mm Hg). AT = acceleration time (ms): FV = filling volume (trammitral flow during E wave. cm’). A ,20_+xi~y_ (cm/secl Effect 100 - 80. A ";?A ‘1”,’ 71 E 104 &T 124 LT 37.4 E_V 0.2 ;g % 10 62 53 43 100 96 90 26.9 21.6 15.7 200 300 Time (msec) time (as noted by Oh et al. [161) and also to decrease peak velocity (in contrast to their findings). However, the natural physiologic compensation for this fall in filling volume is to raise left atria1 pressure to preserve forward output (though at the expense of pulmonary congestion), the effect of which is shown in Figure IB. All curves are for an aortic regurgitant orifice area of 0.6 cm2 with atria1 pressures of 10 to 25 mm Hg. Peak velocity rises from 43 to 102 cm/s and filling volume from 15.7 back to the original 37.5 cm3. The deceleration time remains short at 82 ms. Thus, this model of severe aortic regurgitation with compensatory rise in atria1 pressure reproduces precisely the findings of Oh et al. (16) concerning the E wave. Of course, E wave velocities could also be increased by mitral regurgitation, which was present in systole in at least one patient (Fig. 2 of that paper [16]) and just before systole in eight. The late diastolic of A wave is not modeled here because the atria1 systolic fitnction are incompletely However. we expect the A wave to depend on both preload (atria1 pressure at the time of the A wave) and afterload (ventricular pressure and compliance). High left atria1 pressure should cause a more forceful contraction and (if atria1 afterload is held constant) a larger A wave; in contrast, a stiff ventricle should limit atria1 transmitral flow for the same force of atria1 contraction. In the case of severe aortic regurgitation, therefore, we can conclude that the profoundly elevated end-diastolic ventricular pressures more than offset any enhanced contractility from elevated atrial pressures. The net result is thus to see tall, narrow E waves and blunted A waves. Clinical implications. As in the case of the mitral inflow pattern seen in hypertrophic disease, these findings illustrate that different clinical entities can generate similar alterations in selected measures of the mitral inflow pattern, such as the deceleration time of the E wave and the E/A wave ratio. Therefore. these features of the inflow pattern must be understood. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016 .__ of Increasincl AR is to shorten deceleration determintrnts 1719 100 60 66 200 300 Time (msecl interpreted in the context of atrial and ventricular loading conditions. The pattern described by Oh et al. (16), along with findings such as proximal jet width (17,18) and the deceleration half-time of the aortic regurgitant jet (19). can serve as corroborative evidence of severe aortic regurgitation. It must be recognized that this mitral inflow velocity pattern, like the aortic regurgitant half-time, depends on left ventricular compliance, and is therefore most applicable with regurgitation of acute onset, as in the patients studied. Over time and with increasing compliance, diastolic ventricular pressures should fall, causing mitral inflow velocities to assume a more normal pattern. Similarly, Downes et al. (20) described diastolic mitral regurgitation in a series of patients with acute severe aortic regurgitation but not in a group with chronic insufficiency, also severe. Further, as Oh et al. (16) note. their findings were described in a group of patients known to have severe aortic regurgitation by clinical assessment and correlative tests; broader application of these findings will require further prospective study. Finally. their results emphasize the need to study the effects of aortic insufficiency and left ventricular compliance on the Doppler pressure half-time method for assessing stenotic mitral valve area. The dependence of the half-time on factors other than mitral valve area has already been demonstrated by the inaccuracies in this method immediately after percutaneous mitral valvotomy (2 I). The potential of aortic insufficiency for decreasing the pressure half-time and causing mitral valve area to be overestimated requires further study as a function of the chronicity of the regurgitant lesion and ventricular compliance. in view of the variable initial clinical results (22-25). Conclusions. Similar Doppler mitral inflow velocity patterns can be produced by different conditions causing similar changes in the time course of the transmitral pressure difference. Nevertheless. informed interpretation of these 1720 LEVINE AND THOMAS EDITORIAL COMMENT patterns guided by the results of computational models and in vitro simulations can allow us to extract meaningful pathophysiologic insights from them. We thank Arthur E. Weyman, MD for review of the manuscript. References 1. Rokey R, Kuo LC, Zoghbi WA, Limacher MC, Quinones MA. Determination of parameters of left ventricular diastolic filling with pulsed Doppler echocardiography: comparison with cineangiography. Circulation 1985;71:543-50. 2 Choong CY, Herrmann HC, Weyman AE, Fifer MA. Preload dependence of Doppler-derived indexes of left ventricular diastolic function in humans. J Am Coil Cardiol 1987;10:800-8. 3. Thomas JD, Wilkins CT. Choong CYP, Levine RA, Weyman AE. A fluid dynamics model of mitral valve flow: description with initial in vitro and clinical validation. In: Computers in Cardiology 1987.Long Beach, CA: IEEE Computer Society, 1988:211-4. 4. Thomas JD, Weyman AE. A fluid dynamics model of mitral valve Row: description with in vitro validation. J Am Coil Cardiol 1989:13:221-33. 5. Nishimura RA, Abel MD, Matte LK, Tajik AJ. Assessment of diastolic function of the heart: background and current applications of Doppler echocardiography. Part II. Clinical studies. Mayo Clin Proc 1989:64:ISI204. 6. Maron BJ, Spirit0 P. Green KJ, Wesely YE, Bonow RO, Arce J. Noninvasive assessment of left ventricular diastolic function by pulsed Doppler echocardiography in patients with hypertrophic cardiomyopathy. J Am Coil Cardiol 1987:10:743-7. 7. Takenaka K, Dabestani A, Gardin JM, et al. Left ventricular filling in hypertrophic cardiomyopathy: a pulsed Doppler echocardiographic study. J Am Coil Cardiol 1986;7:1263-71. 8. Gidding SS, Snider R, Rocchini AP, Peters J, Farnsworth R. Left ventricular diastolic fillingin children with hypertrophic cardiomyopathy: assessment with pulsed Doppler echocardiography. J Am Coil Cardiol 1986:8:310-6. 9. Choong CY, Abascal VM, Thomas JD, Guerrero JL, McGlew S. Weyman AE. Combined inthrence of ventricular loading and relaxation on the transmitral flow velocity profile in dogs measured by Doppler echocardiography. Circulation 1988:78:672-83. JACC Vol. 14, No. 7 December 1989:17lIUO 12 Nishimura RA, Abel MD, Housmans PR, Warnes CA, Tajik AJ. Mitral flow velocity curves as a function of different loading conditions: evaluation by intraoperative transesophageal Doppler echocardiography. J Am Sot Echo 1989;2:79-87. 13. Appleton CP, Hatle LK, Popp RL. Demonstration of restrictive ventricular physiology by Doppler echocardiography. J Am Coil Cardiol 1988; 11:757-68. 14. Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Colt Cardiol 1988:12:426-40. 15. Klein AL. Hatle LK, Burstow DJ, et al. Doppler characterization of left ventricular diastolic function in cardiac amyloidosis. J Am Coll Cardiol 1989:13:1017-26. 16. Oh JK, Hatle LK, Sinak LJ. Seward JB, Tajik AJ. Characteristic Doppler echocardiographic pattern of mitral inflow velocity in severe aortic regurgitation. J Am Coll Cardiol 1989;14:1712-7. 17. Perry GJ, Helmcke F. Nanda NC, Byard C, Soto B. Evaluation of aortic insufficiency by Doppler color flow mapping. J Am Coil Cardiol 1987;9: 952-9. 18. Switzer DF. Yoganathan AP, Nanda NC, Woo YR, Ridgway AJ. Calibration of color Doppler flow mapping during extreme hemodynamic conditions in vitro: a foundation for reliable quantitative grading system for aortic incompetence. Circulation 1987;75:837-46. 19. Teague SM, Heinsimer JA, Anderson JL, et al. Quantification of aortic regurgitation utilizing continuous wave Doppler ultrasound. J Am Coll Cardiol 1986:8:592-9. 20. Downes TR. Nomeir AM, Hackshaw BT, Kellam LJ, Watts LE, Little WC. Diastolic mitral regurgitation in acute but not chronic aortic regurgitation: implications regarding the mechanism or mitral closure. Am Heart J 1989:117:1106-12. 21. Thomas JD, Wilkins GT, Choong CYP, et al. Inaccuracy of mitral pressure half-time immediately after percutaneous mitral valvotomy: dependence on transmitral gradient and left atria1and ventricular compliantes. Circulation 1988;78:98C-93. 22. Gillam LD, Choong CY, Wilkins GT, Marshall JE. The effect of aortic insufficiency on Doppler pressure half-time calculations of mitral valve area in mitral stenosis (abstr). Circulation 1986;74(supplII):II-217. 23. Moro E. Nicolosi GL, D’Angelo G, Burelli C, Zanuttini D, Roelandt J. Aortic regurgitation in patients with mitral stenosis: influence on determination of pressure half-time for mitral valve area calculation (abstr). Circulation 1986;74(supplII):Il-231. IO. Courtois M, Vered Z, Barzilai B, Ricciotti NA, Perez JE, Ludbrook PA. The transmitral pressure-flow velocity relation: effect of abrupt preload reduction. Circulation 1988;78:1459-68. 24. Nakatani S, Masuyama T, Kodama K, Kitabatake A, Fujii K, Kamada T. Value and limitations of Doppler echocardiography in the quantification of stenotic mitral valve area: comparison of the pressure half-time and the continuity equation methods. Circulation 1988;77:78-85. 11. Stoddard MF. Pearson AC, Kern MJ, Ratcliff J, Mrosek DG, Labovitz AJ. Influence of alteration in preload on the pattern of left ventricular diastolic filling as assessed by Doppler echocardiography in humans. Circulation 1989:79:1226-36. 25. Frayburn PA, Smith MD, Gurley JC, Booth DC, DeMaria AN. Effect of aortic regurgitation on the assessment of mitral valve orifice area by Doppler pressure half-time in mitral stenosis. Am J Cardiol 1987; 60:3226. Downloaded From: https://content.onlinejacc.org/ on 10/01/2016