Utility of positron emission tomography scans in mantle cell lymphoma
advertisement

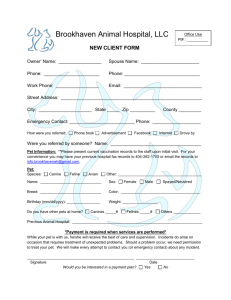
Research Article Utility of positron emission tomography scans in mantle cell lymphoma Peter J. Hosein,1 Vitor H. Pastorini,1 Fabio M. Paes,2 Daryl Eber,2 Jennifer R. Chapman,3 Aldo N. Serafini,2 Ash A. Alizadeh,4 and Izidore S. Lossos1,5 Positron emission tomography (PET) scans are widely used in patients with lymphoma but little is known about their utility in mantle cell lymphoma (MCL). MCL patients were included from two prospective trials and one observational study at our institution. A total of 276 PET scans were performed among 52 patients. After a median follow-up of 37.5 months, the 3-year event-free survival (EFS) and overall survival (OS) were 73% (95% confidence interval [CI]: 61–85%) and 92% (95% CI 85–100%), respectively. There were 34 pretreatment PET scans, 26 interim, 28 end-of-treatment, 162 surveillance, and 26 scans at relapse or beyond. Pretreatment PETs were positive in 94%. A negative interim or end-of-therapy PET scan was not significantly associated with better EFS or OS, but no deaths were observed in patients who had a negative interim or end-of-therapy PET. Surveillance PET scans had a high false positive rate (35%) and low positive predictive value (8%). PET scans contributed to an earlier diagnosis of relapse in only two out of the 18 patients (11%) who relapsed. PET scans did not meaningfully contribute to staging or surveillance of MCL patients in this study. There was a trend toward improved survival in patients who had a negative end-of-therapy PET scan. C 2011 Wiley-Liss, Inc. Am. J. Hematol. 86:841–845, 2011. V Introduction Mantle cell lymphoma (MCL) is a distinct subtype of nonHodgkin lymphoma (NHL) accounting for 6–8% of the estimated 65,540 new NHL cases in the United States annually [1]. MCL was previously considered to be an indolent incurable lymphoma, but the elucidation of some key molecular features of this disease has led to a better understanding of its biology and consequently a more refined approach to treatment. The molecular hallmark of MCL is the t(11;14) translocation, which results in cyclin D1 overexpression and consequently increased cell proliferation [2– 4]. The high proliferation rate of MCL cells may contribute to disease aggressiveness and inferior clinical outcomes [5,6]. Indeed, many investigators have now adopted very aggressive treatment paradigms including intensive chemoimmunotherapy [7,8] as well as upfront myeloablative therapy and autologous stem cell transplant [9–11] in an attempt to improve survival outcomes. Although these approaches have led to better outcomes [12], relapses are still common, necessitating further research into innovative management approaches. Moreover, there appears to be a subset of MCL patients who follow a more indolent course [13] and better identification of these patients may help to streamline management algorithms. The propensity of MCL to exhibit a pattern of continuous relapses over time implies that after frontline therapy, patients have residual disease that is below the level of detection of conventional diagnostic tools. It is not uncommon to find subcentimeter lymph nodes on a computed tomography (CT) scan at the end of treatment for lymphoma and these would not be considered significant by CT size criteria. Functional or metabolic imaging with 18Fluorine-fluorodeoxyglucose positron emission tomography (18F-FDG PET) scanning can potentially identify lesions that contain residual disease that would not be diagnosed by conventional imaging. Based on data supporting this premise, PET scans are now routinely recommended as part of the post-therapy evaluation of patients with HL and aggressive NHL such as diffuse large B-cell lymphoma (DLBCL) [14,15]. The incorporation of PET scans into the clinical management of MCL has not been studied systematically. The initial reports describing the FDG-avidity of NHLs focused mainly on the more common aggressive subtypes such as DLBCL and only included a handful of MCL patients [16–18], with the largest reported NHL PET series of 766 patients containing only 14 MCL patients [19]. Recently, there have been a few retrospective series of MCL patients who underwent PET scanning throughout their disease course [20–23]. One consistent theme through these reports is that MCL appears to be almost uniformly FDG-avid before treatment but PET scans are not sufficiently sensitive to pick up disease in the gastrointestinal tract or the bone marrow, both of which are common sites of involvement for MCL. Because of the paucity of available data, we undertook this study to evaluate the clinical utility of PET scans in MCL Patients and Methods Study design. Patients were eligible for inclusion in this study if they were enrolled in one of the prospective MCL trials at the University of Miami Sylvester Comprehensive Cancer Center or Jackson Memorial Hospital, both in Miami, FL. Patients were also included from an observational NHL study database that stores clinical, pathological, and outcome data for patients treated off-protocol at the same institutions listed above. One of the prospective therapeutic trials, the UM-MCL1 (registered at www.clinicaltrials.gov with the national clinical trial [NCT] identifier NCT00450801) accrued between 2004 and 2008 and has been published,8 and the other UM-MCL2 is ongoing (NCT00878254). 1 Department of Medicine, Division of Hematology/Oncology, University of Miami Miller School of Medicine, Sylvester Comprehensive Cancer Center, Miami, Florida; 2Department of Radiology, Division of Nuclear Medicine, University of Miami Miller School of Medicine, Sylvester Comprehensive Cancer Center, Miami, Florida; 3Department of Pathology, University of Miami Miller School of Medicine, Sylvester Comprehensive Cancer Center, Miami, Florida; 4Department of Medicine, Divisions of Oncology and of Hematology, Stanford University School of Medicine, Stanford, California; 5Department of Molecular and Cellular Pharmacology, University of Miami Miller School of Medicine, Sylvester Comprehensive Cancer Center, Miami, Florida Conflict of interest: Nothing to report. Contract grant sponsor: National Institutes of Health; Contract grant numbers: CA109335, CA122105. Contract grant sponsors: Fidelity Foundation and the Dwoskin Family Foundation (to I.S.L.). *Correspondence to: Izidore S. Lossos, Sylvester Comprehensive Cancer Center, 1475 NW 12th Avenue (D8-4), Miami, FL 33136. E-mail: Ilossos@med.miami.edu Received for publication 10 May 2011; Revised 22 June 2011; Accepted 24 June 2011 Am. J. Hematol. 86:841–845, 2011. Published online 8 July 2011 in Wiley Online Library (wileyonlinelibrary.com). DOI: 10.1002/ajh.22126 C 2011 Wiley-Liss, Inc. V American Journal of Hematology 841 http://wileyonlinelibrary.com/cgi-bin/jhome/35105 research article The eligibility criteria for both of these studies were identical and have been described elsewhere [8]. In brief, untreated patients with a confirmed histological diagnosis of MCL underwent baseline evaluation with laboratory tests, CT and PET (or combined PET/CT), esophagogastroduodenoscopy, colonoscopy, and bone marrow biopsy. When possible, immunostaining with an antibody to Ki-67 (DAKO, Carpinteria, CA) was quantified in the diagnostic specimens. Treatment consisted of two cycles of intensive chemoimmunotherapy and then patients underwent interim reimaging with CT and PET (or combined PET/CT). Regardless of the result of the interim restaging, patients underwent two more cycles of intensive chemoimmunotherapy and then had endof-therapy reimaging with CT and PET (or combined PET/CT). PET scans were optional in the UM-MCL1 study but were required in the UM-MCL2 study. Patients with bone marrow and/or gastrointestinal involvement at baseline were required to have a repeat bone marrow examination and/or endoscopy, respectively, to evaluate response to treatment. Patients achieving a complete response (CR) to therapy then went on to receive maintenance therapy. During the maintenance phase, surveillance imaging with CT and PET (or combined PET/CT) was repeated every 6 months for 3 years, or sooner if clinically indicated. The UM-MCL1 trial tested thalidomide as the maintenance agent, and the UM-MCL2 trial is testing rituximab maintenance. Patients with a confirmed histological diagnosis of MCL who were not willing or eligible for participation in either of these two therapeutic trials were followed on an observational study looking at clinical and pathological predictors of outcome in patients with NHL. All these studies were conducted in compliance with the Declaration of Helsinki and the Guidelines of Good Clinical Practice. The University of Miami Institutional Review Board (IRB) approved each of the protocols and all patients participating in the therapeutic trials provided written informed consent; the requirement for written informed consent was waived by the IRB for patients on the observational study. PET Imaging. All patients enrolled prior to March 2005 at the University of Miami Sylvester Comprehensive Cancer Center were studied using the Philips C-PET System (n 5 6 scans); from March 2005 until March 2008, a Philips Gemini Power-16 PET/CT scanner (n 5 117); and after April 2008, Philips Gemini TF-16 and Philips Gemini TF-64 PET/CT scanners (n 5 131). Patients enrolled at the Jackson Memorial Hospital were studied using the Philips C-PET system (n 5 18), and GE Discovery LightSpeed system (n 5 4). Patients fasted for at least 6 hr before the 18F-FDG injection. The serum glucose level was determined at the time of 18F-FDG injection using a glucometer, and all the patients had to have glucose levels less than 130 mg/dl. Sixty to ninety minutes after intravenous administration of 18F-FDG (0.045 mCi/kg with a maximum of 6 mCi for C-PET unit and 0.14 mCi/kg with a maximum of 15 mCi for the PET/CT units), a PET or PET/CT imaging study from the skull base to the upper thigh was acquired. Images were reconstructed by iterative algorithm (ordered subset expectation maximization) with and without attenuation correction. A clinical report was issued at the time of performance of each scan. For the purposes of this study, all PET scan images and reports were reviewed again by one nuclear medicine specialist physician to ensure consistency of interpretation and reporting of results. Pretreatment PET scans were interpreted as being either negative or positive for disease activity. A positive scan was defined as one having higher FDG uptake relative to uptake in the mediastinal blood pool or surrounding background, with no similar activity seen on the contralateral side, or increased activity at any location incompatible with normal physiological distribution [24]. A negative scan was defined as having no abnormally increased FDG accumulation at any site. Metabolic activity within sites of pathological FDG uptake was semiquantitatively analyzed. A region of interest was manually positioned over the pathological focus with maximal standardized uptake value (SUVmax). The SUVmax was calculated using measured activity, decay-corrected injected dose, and patient body weight. For interim restaging or end-of-therapy scans, responses were determined according to the International Harmonization Project (IHP) criteria [14]. Interim response assessment by PET was performed at least 2 weeks after chemotherapy (4 weeks after the last dose of rituximab) and end-of-therapy PET scans, at least 3 weeks after chemotherapy (5 weeks after the last dose of rituximab). Statistical analysis. Event-free survival (EFS) was calculated from the date of the start of frontline therapy to the date of first appearance of progressive disease, relapse, or death from any cause. Patients, known to be alive and without progressive disease, were censored at the time of last contact. Overall survival (OS) was calculated from the date of the start of frontline therapy to the date of death from any cause or last contact. EFS and OS were estimated by the Kaplan-Meier 842 TABLE I. Patient Characteristics (N 5 52) Age Median (range) Sex Male Female ECOG performance status 0 1 2 Extranodal sites Bone marrow or leukemic phase Gastrointestinal tract Spleen Lung or pleura Orbital, ocular, or central nervous system Other Ann Arbor stage II III IVA IVB Histology Diffuse Blastic Beta-2 microglobulin <3 mg/dl 3 mg/dl Missing Ki-67 staining 10% 11–29% 30% Missing Mantle Cell International Prognostic Index Low (<5.7) Intermediate (5.7 and <6.2) High (6.2) Missing Frontline treatment Ritxumab 1 MACLO-IVAM Rituximab 1 CHOP Rituximab 1 Hyper-CVAD/MA Rituximab 1 Bendamustine Other Best response to frontline treatment Complete response Partial response Stable disease Progression or death Missing Number of PET scans performed Pretreatment/baseline Interim during frontline treatment End of frontline treatment Surveillance At first relapse or beyond Total 58 years (39–92) 40 (77%) 12 (23%) 31 (60%) 18 (35%) 3 (6%) 42 16 12 9 3 13 (81%) (31%) (23%) (17%) (6%) (25%) 2 8 27 15 (4%) (15%) (52%) (29%) 44 (85%) 8 (15%) 20 (38%) 20 (38%) 12 (23%) 5 12 18 17 (10%) (23%) (35%) (33%) 19 18 7 8 (37%) (35%) (13%) (15%) 29 12 3 2 5 (56%) (23%) (6%) (4%) (10%) 36 8 1 3 4 (69%) (15%) (2%) (6%) (8%) 34 26 28 162 26 276 Abbreviations—CHOP: cyclophosphamide, doxorubicin, vincristine, prednisone; Hyper-CVAD/MA: hyperfractionated cyclcophosphamide, vincristine, doxorubicin, dexamethasone alternating with methotrexate and cytarabine; MACLO-IVAM: methotrexate, leucovorin, doxorubicin, cyclophosphophamide, vincristine alternating with ifosphamide, mesna, etoposide, and cytarabine. method with corresponding two-sided 95% confidence interval (CIs) for survival proportions based on Greenwood’s variance and the log-transform method [25]. The statistical software package PASW Statistics 18 (IBM Corporation, New York, NY) was used for these analyses. Results Between November 2004 and March 2011, 52 patients with MCL were treated at our institutions and had a total of 276 PET or combined PET/CT scans performed (median 4, range 1–15). Among these patients, 22 were treated on the UM-MCL1 protocol (between 2004 and 2008), seven on the UM-MCL2 protocol (between 2008 and 2011), and 23 were enrolled on the observational NHL study (between 2004 and 2011). Among the patients on the observational study, only two had initial ‘‘watchful waiting’’ for 6 months and 9 years, respectively, and the remainder had treatment American Journal of Hematology research article Figure 1. Kaplan-Meier survival plots showing EFS (panel A) and OS (panel B) stratified by the MIPI group (low, intermediate, and high) in all 52 patients. started soon after the initial diagnosis. The median followup for all patients was 37.5 months (range 0.1–173.7 months). The median follow-up for the patients on the UMMCL1 and UM-MCL-2 protocols was 51.1 months (range 0.5–81) and 12.9 months (range 4.6–21.7), respectively. All 29 of these patients had longitudinal follow-up from the time of their initial diagnosis until death or March 2011. The baseline characteristics of the patients are shown in Table I. Patients who were treated on the study protocols had a significantly longer EFS compared with those treated offprotocol (median 54.1 vs. 35.6 months, log rank P 5 0.022). The OS was not significantly different for patients treated on-protocol versus off-protocol (median not reached vs. 64.2 months, log rank P 5 0.15), likely due to the small number of deaths in both groups. The baseline MCL International Prognostic Index (MIPI) score [26] was predictive of OS but not EFS in the entire study population (log rank P for a difference between MIPI groups 5 0.013 and 0.078, respectively), as shown in Fig. 1. Pretreatment PET scans PET scans prior to administration of any therapy were available in 34 patients and demonstrated abnormal signal in 32 (94%; exact 95% CI 80–99%) patients. In the initial staging workup, 26 of 34 patients had stage IV disease by virtue of a positive bone marrow biopsy and three of these 26 patients had significant FDG accumulation in the bone marrow, giving a sensitivity of PET of 12% (95% CI 2–30%) for the detection of bone marrow involvement. Within this subgroup of 34 patients with pretreatment PET scans available, 10 had biopsy-proven gastrointestinal tract involvement by MCL. Only two of these patients had abnormal FDG accumulation in the gastrointestinal tract, giving a sensitivity of 20% (95% CI 3–56%) for the detection of gastrointestinal involvement. Among the patients with stage I–III disease by conventional staging, PET scanning upstaged one patient with previously unsuspected splenic involvement, increasing the stage from III to IIIs by the Ann Arbor system. Therefore, PET upstaged 4% (95% CI 0–20%) of patients in this study. A comparison of negative versus positive baseline PET scans was not done as only two out of these 34 patients had completely negative pretreatment PET scans. Interim PET scans PET scans during the course of frontline therapy were available in 26 patients. Most of these patients (69%) were enrolled on the UM-MCL1 or UM-MCL2 trials and had the interim scan done after two cycles of therapy. There was no significant difference in survival between patients who had a negative interim PET scan (i.e., CR by the IHP criteria) compared to those with a positive interim PET scan, as shown in Table II. End-of-therapy PET scans PET scans at the end of frontline therapy were available in 28 patients, with 14 being positive and among these, further workup confirmed persistence of lymphoma in only one case. In the remaining 13 patients, five were later proven to have relapsed lymphoma after a median disease-free interval of 9 months (range 6.3–48.8 months). There was a trend toward better survival for patients who had a negative end-oftherapy PET (i.e., CR by the IHP criteria) compared to those with a positive PET but the difference was not statistically significant, as shown in Table II and Fig. 2. Surveillance PET scans A total of 162 surveillance PET scans were performed among 34 patients who were in remission and asymptomatic from a disease standpoint at the time of the scans. These scans yielded five true positive results, 56 false positives, one false negative, and 100 true negatives. Among TABLE II. Survival by Interim and End-of-treatment PET Scan Resulta All patients (N 5 52) Interim PET (N 5 26) Negative (N 5 15) Positive (N 5 11) End-of-treatment PET (N 5 28) Negative (N 5 15) Positive (N 5 13) 3-year EFS (95% CI) 3-year OS (95% CI) Median follow-up (range) 73% (61–85%) 92% (85–100%) 37.5 months (0.1–173.7) 80% (60–100%) 82% (59–100%) p 5 0.73 100% (94–100%) 91% (74–100%) p 5 0.19 32.5 months (4.1–76.7) 87% (69–100%) 69% (44–94%) p 5 0.16 100% (94–100%) 85% (65–100%) p 5 0.07 44.2 months (4.6–76.7) CI: confidence interval; EFS: event-free survival; OS: overall survival; PET: positron emission tomography. a Statistics not calculated for pretreatment PET scans as there were only two negative scans among 34 patients. American Journal of Hematology 843 research article Figure 2. Kaplan-Meier survival plots showing EFS (panel A) and overall survival (OS, panel B) stratified by the end-of-treatment positron emission tomography scan. the 56 false positive scans, three were serial scans done for the same patient who was later diagnosed with thyroid cancer in the FDG-avid site, two were serial scans in the same patient who was later diagnosed with lung cancer at the FDG-avid site, and one represented renal cancer. The most frequent sites of false-positive FDG update were cervical lymph nodes (63%), mediastinal lymph nodes (34%), abdominal lymph nodes (20%), and bone (14%). The two patients with negative pretreatment PET scans were not included in the interim or end-of-therapy analyses. They were included in the surveillance analysis where they contributed 11 of the 162 PET scans (7%) analyzed. Among these 11 scans, there was one true positive and 10 true negatives. The sensitivity (Sens), specificity (Spec), positive predictive value (PPV), and negative predictive value (NPV) for surveillance PET scans for the detection of relapsed MCL were 83% (95% CI 36–100%), 64% (95% CI 56– 72%), 8% (95% CI 3–18%), and 99% (95% CI 95–100%), respectively. For detection of any malignancy (including MCL), the Sens, Spec, PPV, and NPV were 91% (95% CI 59–100%), 66% (95% CI 58–74%), 16% (95% CI 8–28%) and 99% (95% CI 95–100%), respectively. None of the patients with false positive PET scans during surveillance were in the cohort of patients who were treated with rituximab maintenance. PET scans at relapse There were 18 patients in the study who achieved a CR with frontline therapy but then went on to have a biopsyproven relapse. These 18 cases were examined to determine whether PET scans contributed to the diagnosis of relapse. In 12 of these patients, relapse was suspected by a new symptom or physical examination finding, most commonly being the development of a new enlarged lymph node mass. The remaining six patients were clinically asymptomatic and abnormal surveillance PET/CT scans raised the suspicion for relapse. In three of the six cases, an abnormality was detected on both the PET and CT portions of the study; in the fourth case, there was an abnormality on CT but not PET; in the fifth case, increased FDG accumulation at the site of relapse preceded the appearance of enlarged lymph nodes by 3 months; and in the last case, increased FDG accumulation in the duodenum (with no CT abnormality) prompted a biopsy leading to the diagnosis of relapse. Therefore, abnormal FDG accumulation was the exclusive first sign of relapse in only two out of the 18 patients (11%, 95% CI 1–35%) who relapsed. 844 Discussion PET scans are increasingly being used in oncology and especially in lymphoma. A recent analysis of Medicare beneficiaries in the US showed a 39% increase in the use of PET scans in lymphoma between 1999 and 2006 [27]. Consensus guidelines now include recommendations for initial and post-treatment PET scans in aggressive NHL [14], and risk-adapted strategies based on interim PET scan results are currently being tested [15]. MCL is a relatively uncommon subtype of NHL and no specific guidelines exist for the use of PET in MCL. Our study represents one of the largest series examining the utility of PET scans in MCL patients. For pretreatment PET scans, our data are consistent with other published series in that MCL is almost always FDG-avid at presentation [21]. Our finding that pretreatment PET scans had a low sensitivity (12%) to detect bone marrow involvement is also consistent with the reports by Bodet-Milin et al. and Brepoels et al. who reported sensitivities of 12% and 13%, respectively [21,22]. Similarly, we found a sensitivity of 20% for gastrointestinal tract involvement in our study, which was not markedly different to the sensitivity of 11% reported by Bodet-Milin et al. [22]. As most patients had positive scans at the time of the diagnosis, we could not stratify patients by a categorical positive versus negative PET scan and therefore we considered using a continuous variable such as SUVmax. Other investigators have reported that a higher SUVmax at baseline is associated with worse survival [22,23]. In these reports, the cutoff SUVmax values that stratified patients into high risk versus low risk groups were 5 and 6, respectively. This variation may be due to differences in the study populations as well as different types of scanners and image acquisition techniques. In our study, the scans were performed on five different machines over a 6-year period. It has been well described that several technical, biological, and physical factors affect the reproducibility of FDG quantification [28]. Therefore, we could not reliably analyze SUVmax as a prognostic variable in our study. Recently, there have been efforts to standardize SUV measurements to reduce variability and allow comparisons across different machines [29]. We plan to use these techniques prospectively to further study SUVmax as a prognostic variable in MCL. With regards to PET for response assessment, a CR on an interim PET did not correlate with better survival in our study. The evidence for interim PET scanning as a predictive tool in NHL is inconsistent, and a recent review reported a sensitivity of interim PET for DLBCL of 33–100% and a American Journal of Hematology research article specificity of 53–100% [15]. This wide range for the sensitivity and specificity was due to a lack of uniformity in the timing of the scans, interpretation of the scans, and study endpoints. In recent reports, the PPV of PET in studies using rituximab has fallen to as low as 42% in one series [30], and this has been hypothesized to be due to inflammatory changes associated with the recruitment of immune cells to the tumor by rituximab [31]. For end-of-therapy assessment, we found that a posttreatment CR defined by the IHP criteria (which includes a negative PET), did not predict for better survival in our study, although there was a trend in that direction. In a similar analysis, Bodet-Milin et al. [22] reported a statistically significant survival advantage for patients with a CR (i.e., negative PET) compared to those without a CR. This discrepancy between Bodet-Milin’s results and ours may have been due to a lower statistical power in our study (28 vs. 36 patients) or the higher number of events in our study due to a longer median follow-up (44 vs. 21 months). A consistent finding in that study and ours was that a negative end-of-therapy PET scan had a high NPV for relapse (100% and 87%, respectively) and death (100% in both studies). Of note in our study, a positive end-of-therapy PET scan was only acted on in one patient with proven persistent lymphoma. The others with positive end-of-therapy scans were followed until relapse was proven before any further treatment was given. The majority of PET scans analyzed in this study (59%) were performed for routine surveillance of asymptomatic patients who were in remission from MCL. A total of 35% of these scans yielded false positive results, giving a PPV of only 8%. None of these false positives occurred in patients who were receiving rituximab maintenance. An examination of the patients who relapsed revealed that among the 34 patients who had at least one surveillance PET scan, only two (6%) had an abnormality on PET that was the exclusive first sign of relapse. Therefore, almost all the relapses could have been diagnosed by history, physical examination, and CT scans. These data argue against the use of PET scans for surveillance of asymptomatic patients who are in remission from MCL. El-Galaly et al. recently reported their experience with surveillance PET/CT scans in patients with aggressive NHL, showing that the impact of PET/CT was limited by the high number of false positives, and was significantly more costly than CT surveillance [32]. Although we did not gather minimal residual disease data in our study, there is emerging evidence that this may be a more promising tool for surveillance in MCL [33]. In summary, this study does not support routine use of PET scans in MCL for staging or surveillance. There appears to be consistent data that a CR by the IHP response criteria, which includes a negative PET scan, is a good prognostic factor and this can form the basis of future studies testing risk-adapted approaches after front-line therapy. References 1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277–300. 2. Fernàndez V, Hartmann E, Ott G, et al. Pathogenesis of mantle-cell lymphoma: All oncogenic roads lead to dysregulation of cell cycle and DNA damage response pathways. J Clin Oncol 2005;23:6364–6369. 3. Leonard JP, Schattner EJ, Coleman M. Biology and management of mantle cell lymphoma. Curr Opin Oncol 2001;13:342–347. 4. Determann O, Hoster E, Ott G, et al. Ki-67 predicts outcome in advancedstage mantle cell lymphoma patients treated with anti-CD20 immunochemotherapy: Results from randomized trials of the European MCL Network and the German Low Grade Lymphoma Study Group. Blood 2008;111:2385–2387. 5. Garcia M, Romaguera JE, Inamdar KV, et al. Proliferation predicts failure-free survival in mantle cell lymphoma patients treated with rituximab plus hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with rituximab plus high-dose methotrexate and cytarabine. Cancer 2009;115:1041–1048. American Journal of Hematology 6. Rosenwald A, Wright G, Wiestner A, et al. The proliferation gene expression signature is a quantitative integrator of oncogenic events that predicts survival in mantle cell lymphoma. Cancer Cell 2003;3:185–197. 7. Romaguera JE, Fayad L, Rodriguez MA, et al. High rate of durable remissions after treatment of newly diagnosed aggressive mantle-cell lymphoma with rituximab plus hyper-CVAD alternating with rituximab plus high-dose methotrexate and cytarabine. J Clin Oncol 2005;23:7013–7023. 8. Lossos IS, Hosein PJ, Morgensztern D, et al. High rate and prolonged duration of complete remissions induced by rituximab, methotrexate, doxorubicin, cyclophosphamide, vincristine, ifosfamide, etoposide, cytarabine, and thalidomide (R-MACLO-IVAM-T), a modification of the National Cancer Institute 89C-41 regimen, in patients with newly diagnosed mantle cell lymphoma. Leuk Lymphoma 2010;51:406–414. 9. Tam CS, Bassett R, Ledesma C, et al. Mature results of the M. D. Anderson Cancer Center risk-adapted transplantation strategy in mantle cell lymphoma. Blood 2009;113:4144–4152. 10. Dreyling M, Lenz G, Hoster E, et al. Early consolidation by myeloablative radiochemotherapy followed by autologous stem cell transplantation in first remission significantly prolongs event-free survival in mantle-cell lymphoma: Results of a prospective randomized trial of the European MCL Network. Blood 2005;105:2677–2684. 11. Geisler C, Kolstad A, Laurell A, et al. Long-term progression-free survival of mantle cell lymphoma after intensive front-line immunochemotherapy with in-vivo purged stem cell rescue: A non-randomized phase-2 multicenter study by the Nordic Lymphoma Group. Blood 2008;112:2687–2693. 12. Herrmann A, Hoster E, Zwingers T, et al. Improvement of overall survival in advanced stage mantle cell lymphoma. J Clin Oncol 2009;27:511–518. 13. Martin P, Chadburn A, Christos P, et al. Outcome of deferred initial therapy in mantle-cell lymphoma. J Clin Oncol 2009;27:1209–1213. 14. Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol 2007;25:579–586. 15. Hosein PJ, Lossos IS. The evolving role of 18F-FDG PET scans in patients with aggressive non-Hodgkin’s lymphoma. Eur J Clin Med Oncol 2009;2:131–138. 16. Elstrom R, Guan L, Baker G, et al. Utility of FDG-PET scanning in lymphoma by WHO classification. Blood 2003;101:3875–3876. 17. Han HS, Escalón MP, Hsiao B, et al. High incidence of false-positive PET scans in patients with aggressive non-Hodgkin’s lymphoma treated with rituximab-containing regimens. Ann Oncol 2009;20:309–318. 18. Tsukamoto N, Kojima M, Hasegawa M, et al. The usefulness of (18)F-fluorodeoxyglucose positron emission tomography ((18)F-FDG-PET) and a comparison of (18)F-FDG-pet with (67)gallium scintigraphy in the evaluation of lymphoma: Relation to histologic subtypes based on the World Health Organization classification. Cancer 2007;110:652–659. 19. Weiler-Sagie M, Bushelev O, Epelbaum R, et al. (18)F-FDG avidity in lymphoma readdressed: A study of 766 patients. J Nucl Med 2010;51:25–30. 20. Gill S, Wolf M, Prince HM, et al. [18F]Fluorodeoxyglucose positron emission tomography scanning for staging, response assessment, and disease surveillance in patients with mantle cell lymphoma. Clin Lymphoma Myeloma 2008;8:159–165. 21. Brepoels L, Stroobants S, De Wever W, et al. Positron emission tomography in mantle cell lymphoma. Leuk Lymphoma 2008;49:1693–1701. 22. Bodet-Milin C, Touzeau C, Leux C, et al. Prognostic impact of 18F-fluorodeoxyglucose positron emission tomography in untreated mantle cell lymphoma: A retrospective study from the GOELAMS group. Eur J Nucl Med Mol Imaging 2010;37:1633–1642. 23. Karam M, Ata A, Irish K, Feustel PJ, et al. FDG positron emission tomography/computed tomography scan may identify mantle cell lymphoma patients with unusually favorable outcome. Nucl Med Commun 2009;30:770–778. 24. Juweid ME, Stroobants S, Hoekstra OS, et al. Use of positron emission tomography for response assessment of lymphoma: Consensus of the imaging subcommittee of international harmonization project in lymphoma. J Clin Oncol 2007;25:571–578. 25. Collett D. Modelling Survival Data in Medical Research. London: Chapman & Hall; 1994. p 26. 26. Hoster E, Dreyling M, Klapper W, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood 2008;111:558–565. 27. Dinan MA, Curtis LH, Hammill BG, et al. Changes in the use and costs of diagnostic imaging among medicare beneficiaries with cancer, 1999–2006. JAMA 2010;303:1625–1631. 28. Boellaard ,R. Standards for PET Image acquisition and quantitative data analysis. J Nucl Med 2009;50:11s–20s. 29. Lockhart CM, MacDonald LR, Alessio AM, et al. Quantifying and reducing the effect of calibration error on variability of PET/CT standardized uptake value measurements. J Nucl Med 2011;52:218–224. 30. Cashen AF, Dehdashti F, Luo J, et al. 18F-FDG PET/CT for early response assessment in diffuse large B-cell lymphoma: Poor predictive value of international harmonization project interpretation. J Nucl Med 2011;52:386–392. 31. Spaepen K, Stroobants S, Dupont P et al. [(18)F]FDG PET monitoring of tumour response to chemotherapy: Does [(18)F]FDG uptake correlate with the viable tumour cell fraction? Eur J Nucl Med Mol Imaging 2003;30:682–688. 32. El-Galaly T, Prakash V, Christiansen I, et al. Efficacy of routine surveillance with positron emission tomography/computed tomography in aggressive nonHodgkin lymphoma in complete remission: Status in a single center. Leuk Lymphoma 2011;52:597–603. 33. Pott C, Hoster E, Delfau-Larue MH, et al. Molecular remission is an independent predictor of clinical outcome in patients with mantle cell lymphoma after combined immunochemotherapy: A European MCL Intergroup Study. Blood 2010;115:3215–3223. 845