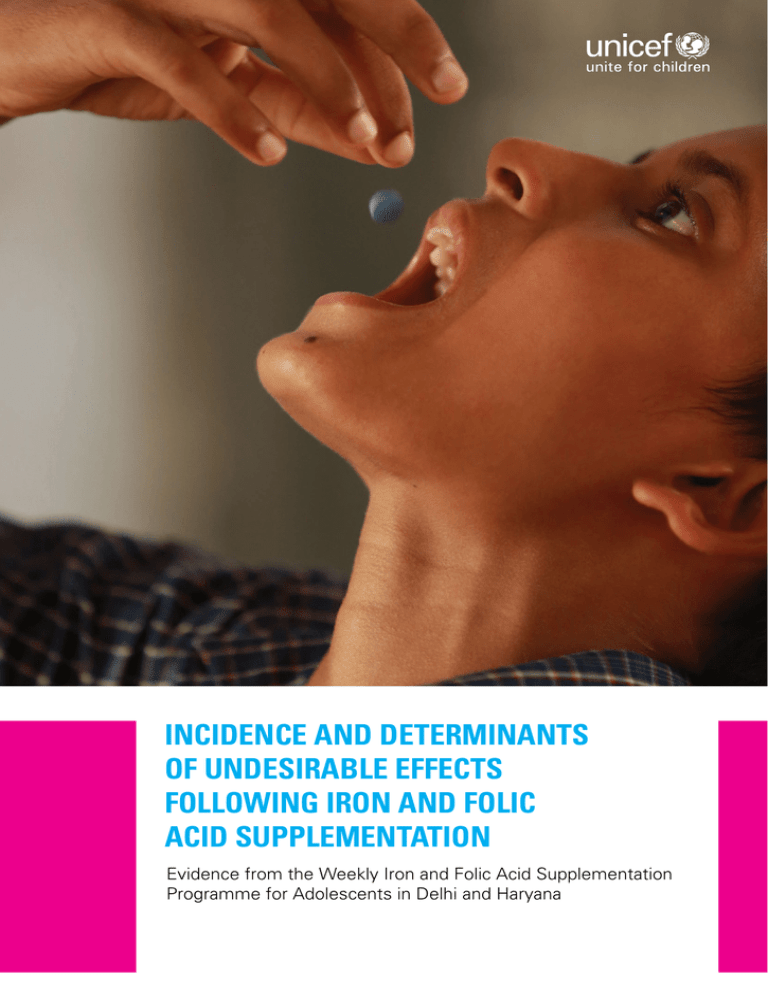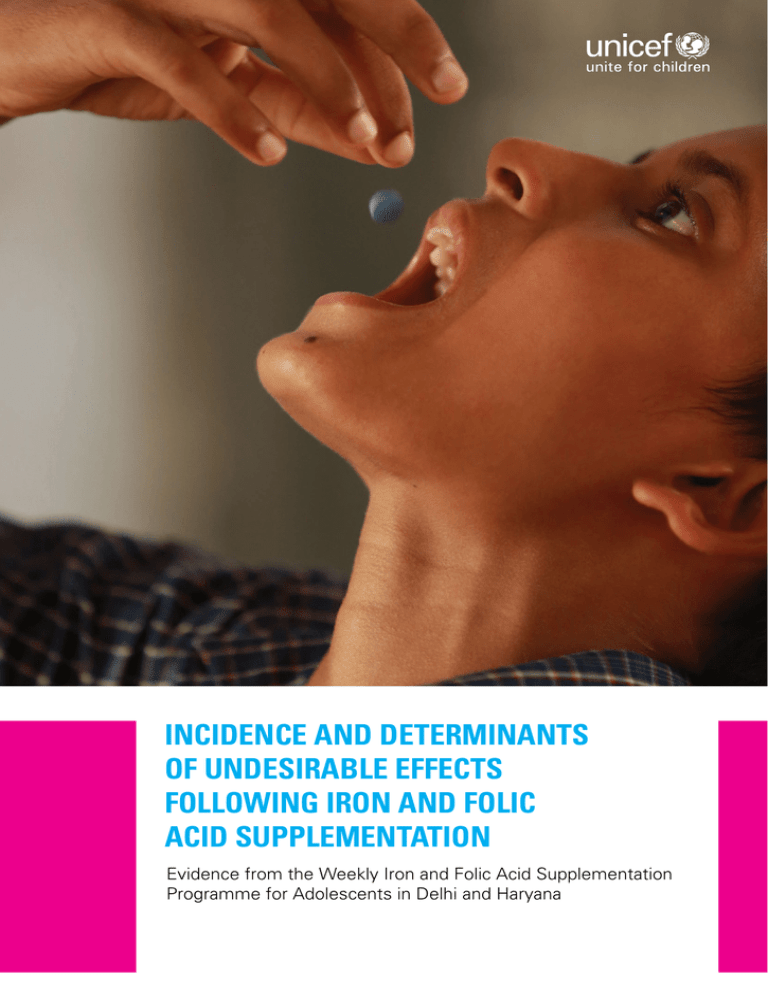
INCIDENCE AND DETERMINANTS
OF UNDESIRABLE EFFECTS
FOLLOWING IRON AND FOLIC
ACID SUPPLEMENTATION
Evidence from the Weekly Iron and Folic Acid Supplementation
Programme for Adolescents in Delhi and Haryana
United Nations Children´s Fund
India Country Office
UNICEF House
73, Lodi Estate
New Delhi 110003
Telephone: +91 11 24690401
www.unicef.in
All rights reserved
©United Nations Children’s Fund (UNICEF)
2014
Cover photo: ©UNICEF India/Divakar Mani
Suggested citation: United Nations Children’s Fund (UNICEF). Incidence and determinants
of undesirable effects following iron and folic acid supplementation. Evidence from the
Weekly Iron and Folic Acid Supplementation Programme for adolescents in Delhi and
Haryana. Nutrition Reports, Issue 3, 2014. New Delhi: UNICEF, 2014.
INCIDENCE AND DETERMINANTS
OF UNDESIRABLE EFFECTS
FOLLOWING IRON AND FOLIC
ACID SUPPLEMENTATION
Evidence from the Weekly Iron and Folic Acid Supplementation
Programme for Adolescents in Delhi and Haryana
Nutrition Reports, Issue 3, 2014
Notice: This discussion paper is a part of the UNICEF India nutrition discussion paper series containing
preliminary material and research results. The nutrition discussion papers have been internally reviewed, but have not been subject to a formal external review. They are circulated in order to stimulate
discussion and critical comment. This discussion paper has been shared with the Adolescent Health
Division, Ministry of Health and Family Welfare, Government of India, on 7 February 2014.
CONTENTS
SUMMARY.................................................................. 5
Introduction.................................................................. 6
Methods....................................................................... 6
Results......................................................................... 7
Conclusion.................................................................... 8
REPORT...................................................................... 11
Introduction................................................................ 12
Methods..................................................................... 12
Results....................................................................... 16
Discussion.................................................................. 21
Conclusion.................................................................. 23
Literature cited........................................................... 25
STATISTICAL TABLES.............................................. 27
ANNEXES.................................................................. 45
ACKNOWLEDGEMENTS......................................................50
©UNICEF India/Divakar Mani
SUMMARY
INTRODUCTION
METHODS
In January 2013, the Ministry of Health and
Family Welfare (MHFW), Government of India,
launched the nationwide Weekly Iron and Folic Acid Supplementation (WIFS) programme.
The WIFS programme includes adolescent boys
and girls of Class VI–XII in government, government-aided and municipal schools. It also covers
out-of-school adolescent girls through the Integrated Child Development Services platform of
the Ministry of Women and Child Development.
The study was cross-sectional and conducted
across government schools in three districts
each in Delhi and Haryana that reported the
highest incidence of undesirable effects in May
2013 (Haryana) and July 2013 (Delhi). Thirty
schools from each state were selected utilizing
30-cluster Probability Proportional to Size (PPS)
methodology. In total, 4,183 adolescents (1,980
boys and 2,203 girls) from 60 schools were covered. Respondents were adolescent boys and
girls from Class VI-XII. However, as only Class
VI-VIII were covered in the WIFS programme in
Delhi, only these classes were covered in the
Delhi sample. Additionally, 49 nodal teachers
and 29 health providers were interviewed.
When WIFS roll-out began at state level, many
states reported that adolescents were complaining about undesirable effects after consuming iron folic acid tablets (IFA) and this
was hampering the programme significantly
through negative peer-to-peer pressure, mass
hysteria and media reports. The latter brought
the WIFS programme in Delhi and Haryana to
near standstill after the administration of the
first dose of WIFS in Haryana (in May 2013)
and in Delhi (in July 2013).
Upon the re-launch of WIFS in September 2013
in the two aforesaid states, upon request of
the MHFW, UNICEF India was commissioned
a study to answer the following four research
questions:
1. What is the incidence of undesirable effects
among school-going adolescent boys and
girls in Delhi and Haryana?
2. Do the adolescent boys and girls who experience an undesirable effect vs. those
who do not differ socio-demographically
and nutritionally?
3. Are schools and health providers prepared
to avert and manage undesirable effects?
4.What are the programme lapses that
can be avoided to improve WIFS programme performance?
6
Summary
The data collection period was 15-30 September 2013 in Haryana and 15-30 October 2013
in Delhi. Areas of enquiry included socio-demographic characteristics, consumption of iron folic
acid (IFA) tablets, protocol followed and undesirable effects on first consumption and in last
two consumptions. Nutritional status was ascertained through anthropometry – height, weight
and mid-upper arm circumference (MUAC),
and height-for-age (HAZ) and body mass index
(BMI)-for-age z-scores were calculated using
World Health Organization Anthroplus software.
BMI-for-age z-score <-3SD was taken as severe
thinness and BMI-for-age z-score <-2SD as thinness. Similarly, HAZ score <-3SD was taken as
severe stunting and <-2SD as stunting. MUAC
cut-off of <16 cm and <18.5 cm were considered severely thin and thin respectively.
Dietary diversity was ascertained using a
seven-day qualitative food frequency questionnaire. Information on perceived gaps in IFA administration and suggestions to bridge the gaps
were collected from nodal teachers and medical
officers. Appropriate analysis was done using
STATA 12 (STATA Corporation, College Station,
TX, USA). P values <0.05 were considered statistically significant. Tests of diagnostic accuracy were conducted to assess sensitivity and
specificity of MUAC compared to BMI-for-age
as the gold standard.
RESULTS
A total of 4,183 adolescents (1,980 boys and
2,203 girls) aged 10-19 years formed the analytical sample. The most important findings from
the study are summarized in this section.
RESEARCH QUESTION 1
What is the incidence of undesirable
effects among school-going adolescents
in Delhi and Haryana?
The incidence of undesirable effects following
IFA in the three weeks of WIFS administration
(week 1: first consumption; week 2 and 3: two
most recent consumptions) is discussed here.
In week 1, out of 4,183 adolescents who were
given IFA, 3,568 (85%) consumed IFA. Out of
the 3,568 adolescents who consumed an IFA
tablet, 907 (25%) reported that they faced an
undesirable effect. Importantly, 410 out of the
907 adolescents (45%) who faced an undesirable effect in week 1 did not consume IFA in the
subsequent week (week 2). Interestingly, 694
out of the 2,661 adolescents (26%) who did not
face any undesirable effect in week 1 did not
take IFA in week 2.
In week 2, again when IFA was administered to
all 4,183 adolescents, 2,630 (63%) reported that
they consumed IFA – a drop of 18 percentage
points in IFA consumption compared to 85% in
week 1. But out of those who consumed IFA
(n: 2,630), 7% reported an undesirable effect.
Again, 80 out of 194 (41%) adolescents who
faced an undesirable effect in week 2 did not
consume IFA in week 3. Also, 685 of the 2,435
adolescents (28%) who did not face an undesirable effect did not consume IFA in week 3.
In week 3 i.e., most recent consumption, again
IFA was administered to all 4,183 adolescents.
Out of these, 2,181 (52%) reported consuming
IFA – a drop of 24 percentage points from week
2, although an overall reported incidence of undesirable effects was 5%.
Thus, the incidence of undesirable effects
in week 1, 2 and 3 was 25%, 7% and 5%,
respectively. But the proportion of adoles-
cents consuming IFA gradually decreased
each subsequent week from 85% to 63% to
52% in week 1, 2 and 3, respectively. Importantly, 354 out of the 907 adolescents (39%)
who faced an undesirable effect on first consumption discontinued IFA. Taking all three
weeks, 1,050 adolescents faced an undesirable effect: 88% faced it only once, 8% twice
and only 4% faced an undesirable effect on
all three consumptions.
The types of undesirable effects were abdominal pain (80%), nausea (10%), dizziness (8%)
and fever (2%). Of the adolescents who reported undesirable effects two or more times –
90% had consumed the IFA tablet on an empty
stomach, 72% had chewed the tablet and 85%
had not had it with water. It is important to note
that 18% adolescents in the two states did not
eat anything before coming to school. Majority
of the adolescents (85% boys and 87% girls)
walked to school daily. The mean travel distance
to school was 1.7 km.
RESEARCH QUESTION 2
Do the adolescent boys and girls
who experience an undesirable effect
vs. those who do not differ sociodemographically and nutritionally?
The prevalence of thinness i.e., BMI-for-age
z-score <-2SD was 30% among boys and 23%
among girls. One quarter of adolescent boys
and girls were stunted (HAZ <-2SD). Multinomial regression analysis showed that the risk
of undesirable effects was higher in girls, in
lower classes (Class VI-VIII), and in urban residents, where parents, teachers and peers did
not encourage IFA consumption, and when IFA
was not consumed according to protocol. Having a BMI-for-age z-score <-2SD or HAZ <-2SD
or coming from a poorer family were not significantly associated with facing undesirable
effects. Adjusted binary logistic regression
showed that positive pressure from parents,
teachers and peers increased the odds of
full compliance (of IFA) by nearly twofold,
irrespective of the occurrence of an undesirable effect.
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
7
CONCLUSION
RESEARCH QUESTION 3
Are schools and health providers
prepared to avert and manage
undesirable effects?
In conclusion, undesirable effects significantly
hamper the WIFS programme but are not influenced by poverty or nutritional status. Particular
attention is to be paid to:
No. Half of the teachers interviewed in Haryana
and 5% teachers in Delhi did not receive training
before roll-out of the WIFS programme. On the
day of supplementation, only 43% teachers
discussed the protocol on how to consume
the tablet. In case of undesirable effects, 20%
schools did not have any designated official/
team to handle the undesirable effects. As a preparedness exercise to manage undesirable effects, 37% of schools had provision of common
medicines, in 29% schools the nodal teacher
had contact details of the Emergency Response
System team, and 20% teachers were aware
of the WIFS emergency toll free helpline
number, but none used it.
1. Constant positive reinforcement through
multiple channels and preparedness to
handle undesirable effects. Regular counselling by teachers and health providers to
parents and peers can improve IFA compliance. At school, information on benefits and
correct protocol should be disseminated
through loud speakers, posters and visually attractive educational sessions (possibly
through engagement of those who consume
IFA regularly and can advocate its benefits).
RESEARCH QUESTION 4
What are the programme lapses that
can be avoided to improve WIFS
programme performance?
Programmatic lapses identified in performance
of the WIFS programme as perceived by teachers and medical officers were: (i) suboptimal
training of teachers, (ii) teachers themselves
not being convinced of benefits of IFA administration, (iii) schools lacking ownership of the
programme, feeling it is the job of the Department of Health, (iv) ineffective convergence between Departments of Health and Education,
(v) inadequate positive media publicity and engaging with media only when an undesirable effect takes place, (vi) adolescents not liking the
taste (and taking it mostly because teachers
have asked them to), (vii) too much focus on
IFA rather than addressing anaemia, (viii) long
meal gaps for most adolescents, who mostly
came from deprived families (did not eat anything before coming to school and had a diet
which was poor in diversity), (ix) negative publicity by parents and peers after occurrence of
the undesirable effect, and (x) panic in schools
to manage undesirable effects.
8
Summary
At community level, informative television or
radio spots and positive messages through
youth icons may be considered for reaching out to adolescents and their families.
Use of mobile communication may also be
considered. Information to raise awareness
of helpline numbers, medicines and ‘WHAT
TO DO’ when there are reported undesirable effects should be displayed in schools,
and one day prior to IFA administration, all
arrangements for emergency response
should be re-checked by the emergency response team.
2.
Following WIFS protocol matters.
Majority of the adolescents who faced
undesirable effects were those who did not
follow the protocol. Hence, reinforcing the
protocol is important. Although nutritional
and socio-economic status did not influence
the occurrence of undesirable effects, given
that a large proportion of adolescents came
from deprived families, walked to school
and had a poor diet, provision of a nutrientdense snack to all adolescents may be
considered so that no adolescent consumes
IFA on an empty stomach. A nutrient-dense
snack will also bridge the calorie-protein
gap. Importantly, no adolescent should be
missed from WIFS if they are not covered
under the mid-day meal programme.
3. Convergence between Departments of
Health and Education needs strengthening. Inter-sectoral collaboration and
accountability mechanisms need to be
strengthened. Presently, a large proportion
of teachers have not received training on the
WIFS programme. If they have, they are not
equipped to manage undesirable effects and
do not own the programme.
4.Test alternative iron supplementation
methods. Compliance of IFA supplementation decreased each subsequent week
from 85% in week 1 to 52% in week 3. This
means that despite all effects, 48% of adolescents were not consuming the tablet in
week 3. These findings suggest the need for
experimenting more likeable energy dense
iron-rich food supplements, which not only
provide iron, but also bridge the gap in dietary macronutrient intake.
5. Ideally all schools should have World
Health Organization BMI-for-age charts
to assess progress on nutritional status.
Until then, MUAC appears as a reasonable
field alternative, subject to more diagnostic
accuracy studies in other settings.
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
9
©UNICEF India/Divakar Mani
REPORT
INTRODUCTION
Adolescent anaemia is a public health problem
in India. Every second adolescent girl and every
third adolescent boy is anaemic in India1. Given
the adverse consequences of adolescent anaemia on growth, resistance to infections, cognitive
development and work productivity, preventing
adolescent anaemia is a high priority agenda for
the Indian government2.
After 13 years of evidence generation by UNICEF
on the use of weekly iron and folic acid supplementation to address anaemia in adolescent girls
in different Indian states, the Ministry of Health
and Family Welfare (MHFW), Government of
India, launched a nationwide Weekly Iron and
Folic Acid Supplementation (WIFS) programme
in January 2013. The WIFS programme includes
both adolescent boys and girls enrolled in Class
VI–XII in government, government-aided and
municipal schools. It also covers ‘out-of-school’
adolescent girls through the Integrated Child Development Services platform of the Ministry of
Women and Child Development3.
The WIFS programme has four components:
1. Supervised WIFS comprising 100 mg of elemental iron and 500 mcg of folic acid (IFA).
2. Screening for moderate/severe anaemia and
referral to nearest health facility.
3. Deworming prophylaxis (400 mg albendazole) six months apart for the prevention of
helminthic infestations.
4.Monthly nutrition and health education
(NHE) to encourage consumption of locally
available iron-rich foods and prevent helminthic infestations.
Global research shows that there are unintended but expected mild undesirable effects
following IFA consumption. These include
gastrointestinal discomfort (stomach ache
and nausea) and change in the colour of stool.
Studies show that the proportion of adolescent girls who experience undesirable effects
following IFA consumption varies from 5% to
20%4. When the universal WIFS programme
roll-out began in various Indian states, state
programme managers in charge of the roll-out
12
Report
in many states reported that adolescents were
complaining about undesirable effects after
consuming iron and folic acid tablets and this
was hampering the programme significantly
through negative peer-to-peer pressure, mass
hysteria and media reports. The latter brought
the WIFS programme in the states of Delhi and
Haryana to near standstill after the administration of the first dose of IFA in May 2013 in Haryana and July 2013 in Delhi.
Questions arose among state programme managers whether adolescents who are weak socio-economically and nutritionally are more likely
to experience undesirable effects and should
the IFA dose be reduced for them. Upon the relaunch of WIFS in September 2013 in the two
aforesaid states, and upon request of the MHFW,
UNICEF India was commissioned a study to answer the following four research questions:
1. What is the incidence of undesirable effects among school-going adolescent boys
and girls?
2. Do the adolescent boys and girls who experience an undesirable effect vs. those
who do not differ socio-demographically
and nutritionally?
3. Are schools and health providers prepared to
avert and manage undesirable effects?
4. What are the programme lapses that can
be avoided to improve WIFS programme
performance?
METHODS
The present study was school-based, crosssectional and followed 30-cluster Probability
Proportional to Size (PPS) methodology.
Setting
States: The geographical scope of the study
was the National Capital Territory of Delhi and
Haryana – home to 5.3 million and 3.3 million
adolescent boys and girls, respectively5. Delhi
and Haryana were selected as they reported
the highest number of undesirable effects following administration of the first dose of IFA
after the launch of the WIFS programme in
these states (May 2013 in Haryana and July
2013 in Delhi).
institutions. The team was trained on the tools
and techniques used for data collection by the
UNICEF lead focal point for the study. The tools
were pre-tested on 5% of the sample in a school
in West Delhi.
Districts: In consultation with state governments and the national and state programme
teams of the WIFS programme, the top three
districts where the WIFS programme was operational in September 2013 and from where
the maximum number of undesirable effects
following the first dose of IFA supplementation
were reported in May 2013 (Haryana) and July
2013 (Delhi) were selected. In Delhi, the three
districts were West A, West B and South West
B. In Haryana, Hissar, Jind and Jhajjar districts
were chosen.
Respondents and sample size: A sample size
of 2,049 was calculated for each state using
maximum reported incidence of undesirable
effects of 20%3, relative precision of 15%,
95% confidence interval and design effect of
3 (see Annex 4). The respondents were adolescent boys and girls from Class VI-XII covered under the WIFS programme. Only Class
VI-VIII were included in the Delhi survey as
only these classes were covered in the WIFS
programme here. From each school (which is
considered as a cluster in the present study),
at least 70 adolescents were included. An attempt was made to include at least five boys
and girls from each class. Adolescents were
selected randomly from each class to complete minimum sample size.
Schools: The study was restricted to government schools, which fall under the jurisdiction
of the state government’s Directorate of Education, as majority of the undesirable effects were
reported from government schools. The list of
schools was obtained by the state Department
of Health and Family Welfare from the Directorate of Education. All the schools were enlisted
with their respective populations.
Thirty schools from each state were selected
utilizing the 30-cluster PPS method. The details of the 30-cluster PPS method are given
in Annex 1. The list of the 30 schools selected
from the two states is given in Annexes 2 and
3. Survey weeks were decided in consultation with district medical officers, the school
health programme division and school principal. However, the exact date was not told to
the school administration until the eve of data
collection to ensure accuracy in the collection.
Written consent from the school authorities
was taken prior to the survey.
Data collection
The nodal teacher of the WIFS programme from
each school and at least one primary health medical officer responsible for the Emergency Response System (ERS) for the block in which the
school was situated were also interviewed. In
total, 4,183 adolescents (1,980 boys and 2,203
girls) from 60 schools, 49 nodal teachers and 29
health providers formed the sample. The graphical presentation of research design is shown in
Figure 1. The data collection period was 15-30
September 2013 in Haryana and 15-30 October
2013 in Delhi.
Information
and
assessments:
Two
methods were used for collection of data
from the adolescents – interview method and
assessment of nutritional status using dietary
and anthropometric methods. Nodal teachers
and medical officers were interviewed using a
structured interview schedule and verbal consent
was taken from all the respondents.
The team: A team was formed comprising two
doctoral researchers trained in nutrition epidemiology and 15 postgraduate nutrition students
from the nutrition department of two academic
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
13
Information gathered from and
assessments conducted on adolescent
boys and girls
i. Adolescent characteristics: The information gathered included class, age (in completed years), residence (urban/rural), mode,
distance and time taken to reach the school,
and whether any form of employed work
(paid or unpaid) is carried out by the adolescent before/after coming to school. From adolescent girls, information on onset of menses, availability and use of sanitary pads,
availability of free sanitary pads in schools
(which were provided free of cost in Delhi)
and use of cotton/cloth during menses was
also collected.
ii. Family characteristics: The study included
information on the number of siblings, family size, education level and occupation of
mother and father. Household characteristics were also enquired and included source
of drinking water and toilet facility, material
of flooring and roof (as per definitions used
in India’s National Family Health Survey 31),
number of persons per sleeping room, availability of communication media like radio,
television, mobiles and computers, type
of cooking fuel used and availability of ration card.
iii.Anthropometry measurements6: Three
types of anthropometric measurements
– height, weight and mid-upper arm circumference (MUAC) were done on all the
adolescents.
Height was measured to nearest 0.1 cm
using a wall-mounted microtoise, nailed
on a wall with no or minimum skirting.
Adolescents stood barefoot on a flat floor
with heels together, calves, buttocks,
shoulder and head in one straight vertical
line touching the wall. They were asked to
keep legs straight and shoulders relaxed.
The head was comfortably positioned in
Frankfurt plane, that is, lower body of the
orbit of the eye in same horizontal plane
as the external canal of the ear and arms
hanging loosely on the sides. The head-
14
Report
piece of the microtoise was gently lowered and slight pressure was applied,
making contact with top of head to record
the height.
Weight was recorded to nearest 0.1 kg using an electronic weighing balance (TANITA
scale model no. H0358). Weight was taken
barefoot with minimal clothing while standing
straight on the weighing scale without any
support. Weighing scales were calibrated daily using standard weight of 1 and 5 kg before
taking the first observation.
Mid-upper arm circumference was
measured to nearest 0.1 cm using a nonstretchable standard MUAC tape (provided
by UNICEF). The left arm of the adolescent
was bent at the elbow at 90-degree angle,
with upper arm held parallel to the side
of the body. The distance between tip
of acromion and olecranon process was
measured and mid-point was marked. The
adolescent was then asked to let the arm
loose and the upper arm at the mid-point
was measured, making sure the tape was
not tight.
iv. Dietary assessment: A seven-day qualitative food frequency questionnaire was administered to assess consumption of foods
from different food groups, especially ironrich foods. The food frequency questionnaire
included nine food groups, namely, cereals
(including roots and tubers), dark green leafy
vegetables (DGLV), vitamin-C rich fruits, organ meats, meats, eggs, pulses and milk.
Each food group was assigned 1 score to
calculate the dietary diversity score (scores
were in the range of 0-9)7. Respondents
were enquired about the meal consumed
before coming to school on survey day.
v. IFA consumption, undesirable effects and
receipt of other services of the WIFS programme: Respondents were asked to recall
IFA administration of three weeks to determine the consumption pattern of IFA. Three
weeks included first consumption when the
programme was first initiated (May 2013 for
Haryana and July 2013 for Delhi) and last
Figure 1
Research design
States with highest prevalence of
undesirable effects
Delhi
Haryana
3 districts
West A
West B
South West B
3 districts
Hissar
Jind
Jhajjar
Maximum cases of
undesirable side effects
30 schools
Boys
(N=1,063)
Girls
(N=1,070)
30 schools
Boys
(N=917)
Teachers (N=22)
MO (N=13)
Girls
(N=1,133)
Teachers (N=27)
MO (N=16)
Interview with adolescents:
Socio-demographic profile, nutritional assessment, consumption pattern of IFA, incidence of
undesirable effects and benefits of IFA consumption.
Interview with MOs and teachers:
Emergency response system on occurrence of undesirable effects.
Data analysis
MS Excel (Office 10), WHO Anthroplus version 1.0.4,
SPSS version 16.0
Report writing
MO = medical officer
two consumptions from the day of enquiry
(September 2013 in Haryana and October
2013 in Delhi). Information on the WIFS protocol being followed, that is, IFA intake on
full stomach, swallowed with full glass of
water and supervised administration by the
nodal teacher was also collected.
The following information was collected on experience of undesirable effects after each of the
three IFA consumptions: type of undesirable effects and perceived reasons. Information was
also asked on reasons for consuming or not con-
suming the IFA tablet. Information was also collected about receipt of two other services under
the WIFS programme – receipt of biannual dose
of albendazole and monthly nutrition and health
education in school.
Interview with nodal teachers and
health providers
The nodal teacher responsible for IFA administration in each school (n: 49) and the medical
officer of the nearest Primary Health Centre/
Dispensary (n: 29) to the school responsible for
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
15
emergency response were interviewed. Data on
training received for IFA administration (teachers
only), protocol for IFA administration, reporting
of undesirable effects, preparedness for adverse effects and actions taken in case of undesirable effects were collected from teachers and
medical officers. Information on perceived gaps
in IFA administration and suggestions to bridge
those gaps were also collected.
(state, sex, residence and deprivation index), anthropometry (BMI-for-age z-score, HAZ, MUAC
less than 16 cm and 18.5 cm), dietary profile
(not eating anything before coming to school
and dietary diversity score), enabling factors for
IFA consumption (peer, parents’ and teachers’
influence), self-efficacy and protocols followed
for IFA consumption (supervised IFA consumption, full stomach, with water and swallowed).
Statistical analysis
The statistical significance of the bivariate association was assessed using chi-square test. The
net association of undesirable effects with significant variables was examined in a step-wise
multinomial logistic regression. Associations
of compliance (intake of at least two IFA) with
socio-demographic characteristics, undesirable
effects and promoters of IFA consumption were
also studied using chi-square for bivariate and
multivariate logistic regression analysis. P values
<0.05 were considered statistically significant.
The collected data were consolidated in Microsoft Excel (2007). The consolidated data were
rechecked for completeness and accuracy.
Height was used to calculate height-for-age
z-score (HAZ) and body mass index (BMI)-for-age
z-score was calculated using height and weight
measurements. World Health Organization Anthroplus (version 1.0.4)8 software was used for
calculating z-scores. BMI-for-age z-score cut-off
point of <-3SD was taken as severe thinness and
<-2SD as thinness (which included severe thinness). Similarly, HAZ cut-off point of <-3SD was
taken as severe stunting and <-2SD as stunting
(which included severe stunting). MUAC cut-off
of <16 cm and <18.5 cm were considered severely thin and thin, respectively9.
A multidimensional index of deprivation was
used to determine deprivation (proxy: for poverty). It included seven components – adolescent BMI-for-age z-score <-2SD, non-improved
drinking water facility, no toilet facility at home,
no access to health facility, illiteracy or less than
primary literacy among adolescents, ≥3 household members living in one room and no exposure to media, that is, non-availability of newspapers, radio, television, computers or mobiles
at home. Deprivation threshold score of 2-3 indicates moderate poverty and 4-7 indicates severe deprivation. Such a multidimensional index
of deprivation has been used elsewhere10.
Analysis was done using STATA 12 (STATA
Corporation, College Station, TX, USA). First,
standard univariate descriptive statistics were
calculated. Then, bivariate associations of undesirable effects (no undesirable effects, undesirable effects faced once and faced two or more
times) was done with adolescent characteristics
16
Report
To estimate the diagnostic accuracy between
BMI-for-age z-scores and MUAC, BMI-for-age
was considered as the gold standard and sensitivity, specificity, positive and negative predictive values and likelihood ratios were calculated.
To compare agreement between the two methods, kappa statistic was calculated. Association
between the absolute values of BMI-for-age
z-scores and MUAC was determined by Pearson
correlation (r) method11.
RESULTS
All the 4,183 adolescents in Class VI to XII in the
study were included in the analysis. Of these,
1,980 were adolescent boys and 2,203 were
adolescent girls. In Delhi, the sampled adolescents were from Class VI-VIII, given that only
beneficiaries of the mid-day meal scheme were
given an IFA tablet. In Haryana, IFA was being
provided to adolescents in Class VI-XII.
1. What were the background
characteristics of the adolescents?
Table 1 describes the profile of the sampled
adolescents. Over 90% of the Haryana sam-
Figure 2
Mean BMI-for-age z-scores
10-12
13-15
16-19
Mean BMI-for-age z-score
-1.05
-1.1
-1.15
-1.2
n=2094
-1.25
-1.3
n=1632
-1.35
-1.4
n=457
Age range (in completed years)
ple resided in rural areas and nearly 90% of the
Delhi sample resided in urban areas. The majority of the adolescents (85% boys and 87%
girls) walked to school daily in both states.
The mean travel distance to school was 1.7 km.
Out of 4,183 adolescents, 88 (2%) also worked
in a job along with regular schooling. Of these
88 adolescents who worked, 56 (64%) worked
without pay.
Among adolescent girls, 41% had started menstruating (31% in Delhi and 50% in Haryana).
Out of the girls who started menstruating,
76% girls used sanitary napkins (96% in Delhi
and 64% in Haryana). In Delhi, 85% of the girls
were using sanitary napkins as they were available free of cost from school, under the School
Health Programme; no such programme was
operational in Haryana. In Haryana, 64% of
the girls used sanitary pads, while 36% used
cotton/cloth.
2. What were the socio-economic
characteristics of the adolescents?
About 50% of the mothers of the sampled
adolescents were illiterate and at least three
quarters of them were not engaged in working
outside the home. In contrast, most (≈60%) fa-
thers of the sample adolescents had received
education up to middle and higher level schooling and were engaged in skilled work. Homes
from where the adolescents came from were
mostly pucca or made of high quality (≈80%).
However, this proportion was lower in Haryana
(≈66%) compared to Delhi (≈90%). According
to the multidimensional index of deprivation, in
both states, three quarters adolescents were
from moderately deprived and 13% were from
severely deprived families (see Table 2).
3. What was the nutritional status of
the adolescents?
Thinness: The prevalence of thinness i.e.,
BMI-for-age z-score <-2SD was 30% among
boys and 23% among girls (see Table 3). The
sex-wise differences were starker in Delhi
(boys: 29% vs. girls: 19%) compared to Haryana (boys: 31% vs. girls: 26%). Over 9% boys
and 6% girls were severely thin i.e., BMI-forage z-score <-3SD. As age increased, mean
BMI-for-age z- score worsened (see Figure 2).
The prevalence of thinness and severe thinness also increased with increasing age (see
Table 4). As household deprivation increased,
mean BMI-for-age z-score also worsened
(see Figure 3).
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
17
Stunting: One quarter of adolescent boys
and girls were stunted (HAZ <-2SD) (see
Table 3). Proportion of severely stunted adolescents i.e., HAZ <-3SD was 6%. Stunting increased steeply from 9% in age of 10
years to 32% in age group of 18-19 years in
boys. Among girls, stunting was highest in the
age group of 11-12 years and 14 years (see
Table 4).
Identifying at-risk adolescents using MUAC:
Almost one third (29%) adolescent boys and
26% adolescent girls had a MUAC less than
18.5 cm. Proportion of adolescent boys and
girls with MUAC less than 16 cm was 7% and
6%, respectively.
Dietary pattern: Almost one fifth (18%)
adolescents in the two states did not eat
anything before coming to school (see Table
3). This proportion was higher in Haryana in
comparison to Delhi (21% vs. 16%) and higher
in girls compared to boys (23% vs. 13%). Not
even half of the sampled adolescents consumed
iron-rich foods twice a week. Diet diversity was
low, as 49% of the adolescents were consuming
fewer than three food groups in a day.
Consumption of eggs and meat twice a week
was also low (<15%). Meals chiefly comprised
a cereal and pulse/vegetable. Consumption of
DGLVs and vitamin C rich fruits at least twice a
week was 42% and 31%, respectively.
Diagnostic accuracy of MUAC compared to
BMI-for-age z-score (as gold standard): There
was agreement in 3,246 out of 4,183 (78%) observations of MUAC < 18.5 cm with BMI-forage z-score <-2SD. Kappa value of 0.34 (95% CI
0.31-0.38) showed a moderate agreement between the two tests. With BMI-for-age z-score
<-2SD as the gold standard, sensitivity and
specificity by MUAC <18.5 cm to correctly identify thinness (true-positive) and non-thinness
(true negative) was 73% and 79%, respectively
(see Table 5).
When MUAC <16 cm was compared with BMIfor-age z-score <-3SD (as gold standard), there
was agreement in 3,959 out of 4,183 (95%) observations, kappa value was 0.38 (95% CI 0.310.38) but sensitivity and specificity of MUAC
18
Report
<16 cm method to correctly identify severely
thinness (true-positive) and non-severely thinness (true negative) was 63% and 97% (see
Table 5). Taking absolute value of MUAC (in cm)
and BMI-for-age z-score, the power of association between MUAC and BMI-for-age z-score
was strong (r value of 0.68 (p<0.001)).
4. What was the IFA consumption and
compliance to protocol?
Table 6 describes the consumption pattern of IFA
during the first week of WIFS administration i.e.,
in May 2013 (Haryana) and July 2013 (Delhi) and
the last two weeks preceding the survey, a total
of three consumptions. The proportion of adolescents who consumed IFA only once, twice
and all three times were 23%, 26% and 42%,
respectively (see Table 6). The protocol for IFA
consumption is that it is to be supervised, after
a meal, with water and swallowed (not chewed).
Overall 43% adolescents reported supervised
IFA consumption (67% in Haryana and 47% in
Delhi). Percentage of adolescents consuming
IFA on an empty stomach was low, but higher
in Haryana compared to Delhi, and few but yet
more adolescents in Haryana chewed IFA than
in Delhi (see Table 6). Since the universal rollout of the WIFS programme, albendazole had
been given once in both states, and it was consumed by two thirds of the adolescents. One
third of adolescent girls mentioned receiving at
least one nutrition and health education session.
Attendance in NHE was higher in Haryana compared to Delhi (37% vs. 27%) and higher in girls
compared to boys (34% vs. 29%).
5. What was the incidence of
undesirable effects following
IFA consumption?
The incidence of undesirable effects in each of
the three weeks of WIFS administration (week
1: first consumption, week 2 and week 3 i.e.,
two most recent consumptions) is presented in
Table 7.
In week 1, out of 4,183 adolescents who were
given IFA, 3,568 (85%) consumed IFA. Out of
the 3,568 adolescents who consumed an IFA
Figure 3
Association of BMI-for-age z-score with multidimensional index of poverty
Non-poor
Moderately poor
Severely poor
Mean BMI-for-age z-score
0
-0.5
-0.6
-1
-1.2
-1.5
-2
-2.1
-2.5
Multidimensional index of poverty
tablet, 907 (25%) reported that they faced an
undesirable effect. Interestingly, 410 out of
the 907 adolescents (45%) who faced an undesirable effect in week 1 did not consume
IFA in the subsequent week (week 2). Also,
694 out of 2,661 adolescents (26%) who did
not even face any undesirable effect in week
1 did not take IFA in week 2, on influence of
their peers.
In week 2, again when IFA was administered to
all 4,183 adolescents, 2,630 (63%) reported that
they consumed IFA – a drop of 18 percentage
points in IFA consumption compared to 85% in
week 1. But out of those who consumed IFA
(n: 2,630), 7% reported to have faced an undesirable effect. Again, 80 out of 194 (41%) of
adolescents who faced an undesirable effect in
week 2 did not consume IFA in week 3. Also,
685 of the 2,435 adolescents (28%) who did not
face an undesirable effect did not consume IFA
in week 3.
In week 3 i.e., most recent consumption, again
IFA was administered to all 4,183 adolescents.
Out of these, 2,181 (52%) reported consuming
IFA – a drop of 24 percentage points from week
2, although the overall reported prevalence of
undesirable effects was only 5%.
Thus, incidence of undesirable effects in
week 1, 2 and 3 was 25%, 7% and 5%, respectively. But the proportion of adolescents
consuming IFA gradually decreased each subsequent week from 85% to 63% to 52% in
week 1, 2 and 3, respectively. Importantly, 410
out of the 907 adolescents (45%) who faced an
undesirable effect in week 1 did not consume
IFA in the subsequent week (week 2) and 354
of the 410 did not have IFA in week 3.
This means that 354 out of the 907 adolescents (39%) who faced an undesirable
effect on first consumption discontinued
taking IFA tablets. Taking all three weeks,
1,050 adolescents faced an undesirable effect: 88% faced it only once, 8% twice and
only 4% faced an undesirable effect on all
three consumptions.
The types of undesirable effects were abdominal pain (80%), nausea (10%), dizziness (8%)
and fever (2%). When the 1,050 adolescents
who faced an undesirable effect were asked
the perceived reasons for it (see Table 7), 37%
said because the body had not adjusted to the
tablet, 16% mentioned because they did not
follow the protocol and 2% mentioned that it
was due to menses.
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
19
6. What factors affected full compliance
of IFA?
Table 8 describes the characteristics of the
adolescents who demonstrated full IFA compliance (i.e., consumed IFA in all three weeks)
compared to those who consumed IFA either in
week 1 or 2. Full compliance was significantly
higher in Haryana compared to Delhi (53% vs.
47%, p<0.001), in girls compared to boys (54%
vs. 46%, p=0.04) and in rural compared to urban
adolescents (60% vs. 43%, p=0.001).
Adjusted binary logistic regression showed that
a high self-efficacy and positive pressure from
parents, teachers and peers increased the odds
of full compliance by 1.4-2.0-fold (see Table 8), irrespective of the occurrence of the undesirable
effect. High self-efficacy meant that the adolescents themselves felt that the tablet is beneficial
to them. Most commonly perceived benefits
were that they felt healthier (28%), felt energetic
(16%), and did not fall sick (17%) (see Table 9).
7. Did the adolescents who experienced
an undesirable effect vs. those who
did not differ socio-demographically
and nutritionally?
Table 10 shows the proportion of adolescents
who faced undesirable effects at least twice
significantly differed by state (2% in Delhi vs.
4% in Haryana, p=0.001), gender (32% in males
vs. 69% in females, p=0.001) and class (58% in
Class VI-VIII vs. 42% in Class IX-XII, p=0.001).
Having a BMI-for-age z-score <-2SD or HAZ
<-2SD or coming from a poorer family were
not significantly associated with facing undesirable effects two or more times. Regression analysis (see Table 12) confirmed that risk
of facing undesirable effects was twofold higher
in girls, in lower classes (Class VI-VIII), urban residents, where peers and parents did not encourage IFA consumption, and when IFA was not
consumed according to protocol.
8. Were teachers prepared to avert and
manage undesirable effects?
More than half of the teachers interviewed in
Haryana and 5% teachers in Delhi did not re-
20
Report
ceive training before roll-out of the WIFS programme (see Table 13). Twelve per cent of the
schools did not have a teacher designated as a
nodal teacher in-charge of the WIFS programme.
On the day of supplementation, only 43%
teachers discussed the protocol on how to
consume the tablet. In case of undesirable effects, 20% schools did not have any designated
official/team to handle the undesirable effects.
As a preparedness exercise to manage undesirable effects, 37% of schools had provision of
common medicines, in 29% schools the nodal
teacher had contact details of the ERS team,
and 20% teachers were aware of the WIFS
emergency toll free helpline number, but
none used it. In Haryana, there was no helpline
number.
9. Were health providers prepared
and equipped to manage
undesirable effects?
Approximately two thirds (66%) health providers interviewed reported that contact details of
hospitals and an ERS team were made available
to schools and common medicines were also
at the schools’ disposal (see Table 14). At least
80% of medical officers interviewed reported
that an ambulance was available on the day of
IFA administration in the health facility. The main
causes of undesirable effects amongst adolescents reported by medical officers were not following protocol (62%) and domino effect (48%).
Surprisingly, 59% of them felt that adolescents
who are undernourished or anaemic are more
likely to face an undesirable effect.
10.Which programme lapses could
have been avoided to improve
WIFS programme performance?
Programmatic lapses identified in the performance of the WIFS programme as perceived by
teachers and medical officers were:
i. suboptimal training of teachers;
ii. teachers themselves not being convinced of
benefits of IFA administration;
iii.schools lacking ownership of the programme, feeling it is the job of the Department of Health;
iv. ineffective convergence between Departments of Health and Education;
v. inadequate positive media publicity and engaging with media only when an undesirable effect takes place;
vi.adolescents not liking the taste (and taking it mostly because teachers have asked
them to rather than willingness to have
the tablet);
vii. too much focus on the IFA tablet instead of
raising awareness on the harms of anaemia and the role IFA consumption plays in
preventing anaemia.
viii. long meal gaps for most adolescents, who
mostly came from deprived families (did not
eat anything before coming to school and
had diet which was poor in diet diversity);
ix. negative publicity by parents and peers after occurrence of undesirable effects; and
x. lack of preparedness and panic in schools to
manage undesirable effects.
DISCUSSION
The 10 most important findings that emerged
from this study are discussed in this section.
1. In Delhi, adolescents in Class IX-XII
were not receiving WIFS.
After the re-launch of the WIFS programme in
September 2013, Delhi schools administrated
IFA to only Class VI-VIII (younger adolescents)
after the mid-day meal. IFA was not being distributed to adolescents in Class IX-XII, as it was
felt that older adolescents reported more undesirable effects and were more likely to take the
tablet on an empty stomach.
Programme implication:
According to NFHS-3, 56% girls and 30% boys
aged 15-19 years are anaemic in India1. Nonadministration of IFA in Class IX-XII misses a
large number of anaemic girls aged 15-19 years,
who should be provided WIFS.
2. Nearly one fifth of adolescents (23%
girls and 13% boys) did not eat
anything before coming to school
and 85% adolescents walked at least
1.5 km to school.
Nearly one fifth of adolescents came to school
on an empty stomach. In any case, the diets
consumed by the adolescents were sub-optimal
in diet diversity and low in iron-rich foods. Adolescents who reported not consuming anything
before coming to school were 1.2 times more
likely to report facing undesirable effects (OR
1.3, 95% CI 1.0-1.5). Also, 90% of adolescents
who reported experiencing undesirable effects
two or more times consumed the tablet on an
empty stomach.
Programme implication:
There is a need to sensitize adolescents on the
importance of eating before going to school.
Provision of a nutrient-dense snack to all adolescents may be considered so that no adolescent consumes IFA on an empty stomach. The
school assembly platform should be tapped to
spread awareness on the harms of anaemia and
benefits of IFA.
3. Incidence of undesirable effects
reduced gradually but adversely
affected compliance.
In the first consumption, 25% adolescents
faced an undesirable effect, which reduced to
7% and 5% in subsequent consumptions. The
most common undesirable effect was stomach
ache. However, the overall consumption of IFA
reduced from 85% in week 1 to 52% in week 3
due to negative media publicity, negative parental and peer pressure (which was more in urban
areas and among girls) and ill preparedness of
schools to manage undesirable effects. Importantly, 40% of adolescents who faced an undesirable effect in week 1 did not have IFA in week
2 and week 3.
Programme implication:
Regular IFA consumption reduces incidence
of undesirable effects as among those adolescents who consumed IFA and faced undesirable
effects, 88% faced them only once. However,
mass hysteria adversely affected WIFS in both
states and reduced the motivation among teachers and health providers who administer the tab-
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
21
lets. Focus on positive media publicity, and positive engagement of parents and peers needs to
be accelerated in the WIFS programme.
4. Reported undesirable effects were
higher among girls and urbanites.
The reported odds of undesirable effects were
twofold higher in girls compared to boys (adjusted OR = 2.2, 95% CI 1.5 to 3.3). Adolescents in rural areas were less likely to report
undesirable effects (adjusted OR 0.5, 95% CI
0.3-0.9).
Programme implication:
Adolescent girls who have benefited from IFA
should be encouraged to become peer monitors to motivate others. Positive video and audio communication materials may be played
through the school central speaker system and
through mass and mid media so that there is
a positive discussion and dialogue around addressing anaemia and the positive role of IFA
among peers, parents and providers.
5. Nutritional status was not a
predictor of undesirable effects.
One quarter of adolescents were stunted and
27% were thin (BMI-for-age z-score <-2SD).
Thinness, severe thinness and stunting were
not significantly associated with occurrence of
undesirable effects.
Programme implication:
Nutritional status of the adolescents does not affect the occurrence of undesirable effects. Thus,
there is no need to reduce the IFA dosage for
adolescents who are thin or stunted. However,
given that a large proportion of adolescents are
thin and stunted, there is a need to accelerate
measures for improving their nutritional status.
6. Socio-economic status was not a
predictor of undesirable effects.
According to the multidimensional deprivation
index, 87% school-going adolescents were
moderately/severely deprived. However, socioeconomic status did not emerge as a significant
predictor of undesirable effects.
22
Report
Programme implication:
Socio-economic status is not associated with
undesirable effects among adolescents. However, focus needs to be made on ensuring these
children receive a mid-morning snack as their dietary practices at home are poor.
7. Not following protocols was
a significant predictor of
undesirable effects.
Consumption of IFA without water (adjusted OR
16.4, CI 4.1-66.5), on an empty stomach (adjusted OR 50.3, CI 5.9-116.9) and chewing the
tablet (adjusted OR 4.03, CI 2.3-5.95) increased
the odds of facing undesirable effects.
Programme implication:
Not following WIFS protocols was a significant
predictor of undesirable effects. Worryingly,
in only 50% schools these protocols were reinforced on the day of administration of IFA.
Teachers should be instructed to repeat the protocols a day prior and on the day of administration of IFA. Provisions can be made to provide a
mid-day meal in case some adolescents forget
to bring lunch to school.
8. Schools were not prepared to avert
and manage undesirable effects.
One third of the teachers did not receive training before the roll-out of the WIFS programme.
Schools and teachers felt that the programme
was an added responsibility. More than half of
the schools did not reinforce the protocol while
administering IFA. Awareness of the helpline
number and its use, and disseminating important information about what do in the event of an
undesirable effect was very low.
Programme implications:
Collaboration with the Department of Education is essential to improve IFA administration, ensure nodal teachers are trained and
monitored to ensure undesirable effects are
averted and managed as well as ensure students are provided information on the types of
undesirable effects, counselled on what to do
and who to go to when such effects happen
to avoid panic.
CONCLUSION
9. Parental and peer pressure influenced
compliance and undesirable effects.
Negative parental and peer pressure increased
the odds of undesirable effects by at least threefold (OR 3.4, CI 2.3-5.1). Positive peer influence
increased compliance by 1.4 times (OR 1.4, CI
1.2-1.7) and also reduced the odds of reporting
undesirable effects (OR 0.6, CI 0.5-10). Both
these factors increased the self-efficacy of the
adolescent.
Programme implication:
Positive environment was identified as an important determinant for IFA consumption and
reducing undesirable effects. Parents and peers
should be made the focus of communication
strategies on IFA and informed about the benefits of IFA as well as possible undesirable effects
and their management.
10.MUAC appeared as a promising
field-based method for identifying
at-risk adolescents. More evidence is
needed on its use.
Kappa value of 0.34 (95% CI, 0.31-0.38) for
BMI-for-age z-score <-2SD and MUAC <18.5
cm and 0.38 (95% CI, 0.31-0.38) for BMI-forage z-score <-3SD and MUAC <16 cm showed
a moderate agreement between the two methods of assessing nutritional status, that is, BMI
(gold standard) and MUAC. Other studies comparing diagnostic accuracy of MUAC against
BMI also found that MUAC has a moderate to
good agreement with BMI12,13.
Programme implication:
In settings where weighing scales, height meters and BMI-for-age charts are not available,
simple methods such as MUAC may be used
to identify adolescents at risk and institute corrective measures for them. These may include
providing them an additional snack/supplement, enrolling them for extra diet and counselling sessions, which would include improving
dietary habits, confidence building and supplementary feeding.
In conclusion, undesirable effects significantly
hamper the WIFS programme but are not influenced by socio-economic or nutritional status.
Particular attention is to be paid to:
1. Positive reinforcement and preparedness
to handle undesirable effects matter.
Regular counselling by teachers and health
providers to parents and adolescents can
improve IFA compliance. At school, information should be disseminated through loud
speakers, posters and visually attractive
educational sessions (possibly through engagement of those who consume IFA regularly and can advocate its benefits).
At community level, informative television
or radio spots, through youth icons, may
be considered for reaching out to adolescents and their families. Information to raise
awareness on helpline numbers, medicines
and ‘WHAT TO DO’ when there are reported
undesirable effects should be displayed in
schools, and one day prior to IFA administration, all arrangements for emergency response should be re-checked by the emergency response team.
2. Following WIFS protocol matters. On the
day of IFA distribution, it is essential to ensure
that the adolescents have a meal before
consuming the IFA tablet. The availability
of safe water for swallowing IFA should be
ensured on school premises. Adolescents
should be informed about anaemia, the
positive benefits of IFA along with possible
undesirable effects, which may reduce with
subsequent IFA consumption.
Although nutritional status and socioeconomic status did not influence
undesirable effects, given that a large
proportion of adolescents came from
deprived families, walked to school and had
a poor diet, provision of a nutrient-dense
snack to all adolescents may be considered
so that no adolescent consumes IFA on an
empty stomach. There is a need to sensitize
adolescents on the importance of consuming
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
23
meals before going to school. All platforms
for promoting WIFS should also promote
improved dietary practices.
3.
Convergence between Departments
of Health and Education needs strengthening. Inter-sectoral collaboration and
accountability mechanisms need to be
strengthened at all levels. Presently a large
proportion of teachers have not received
training on WIFS. If they have, they are not
equipped to manage undesirable effects and
do not own the programme.
4.Test alternative iron supplementation
methods. Compliance of IFA supplementation decreased each subsequent week
from 85% in week 1 to 52% in week 3.
24
Report
This means that despite all effects, 48% of
adolescents were not consuming the tablet.
These findings suggest the need for experimenting to find more likeable energy dense
iron-rich food supplements, which not only
provide iron, but also supplement recommended macronutrients. Large-scale studies on efficacy, feasibility and effectiveness
of use of alternative food supplementation
products on haemoglobin levels are still to
be carried out.
5.Ideally all schools should have BMIfor-age charts to assess progress on
nutritional status. Until then, MUAC appears as a reasonable field alternative, subject to more diagnostic accuracy studies in
other settings.
LITERATURE CITED
1
International Institute for Population Sciences (IIPS) and Macro International. National Family Health
Survey (NFHS-3), 2005-06. Mumbai: International Institute for Population Sciences, 2007. http://www.
measuredhs.com/pubs/pdf/FRIND3/FRIND3-VOL2.pdf. Accessed 1 September 2013.
2
World Health Organization. Nutrition in adolescence – issues and challenges for the health sector.
Geneva: World Health Organization, 2005. http://whqlibdoc.who.int/publications/2005/9241593660_
eng.pdf. Accessed 14 January 2014.
3
Ministry of Health and Family Welfare. Operational framework: weekly iron folic acid supplementation
programme for adolescents. New Delhi: Government of India, 2012. http://tripuranrhm.gov.in/Guidlines/
WIFS.pdf. Accessed 1 September 2013.
4
World Health Organization. Weekly iron and folic acid supplementation programmes for women of
reproductive age. An analysis of best programme practices. Geneva: World Health Organization,
2011. http://www.wpro.who.int/publications/docs/FORwebPDFFullVersionWIFS.pdf. Accessed 12
September 2013.
5
Office of the Registrar General and Census Commissioner India 2011. Census of India 2011: Provisional
Population Totals, India series. New Delhi: Government of India, 2011.
6
World Health Organization. Physical status: the use and interpretation of anthropometry. Report WHO
Expert Committee. WHO Tech Rep Series 1995; 854: 1-452.
7
Food and Agriculture Organization. Guidelines for measuring household and individual dietary diversity.
Rome: FAO, 2011. http://www.fao.org/fileadmin/user_upload/wa_workshop/docs/FAO-guidelines-dietarydiversity2011.pdf. Accessed 2 September 2013.
8
World Health Organization. WHO anthroplus: software for assessing growth of the world’s children and
adolescents. Geneva: World Health Organization, 2009.
9
United Nations Standing Committee on Nutrition. Adults: assessment of nutritional status in emergencyaffected populations. Geneva: SCN, 2000.
10
United Nations. Expert group meeting on youth development indicators. Indicators of poverty and
hunger. New York: United Nations, 2005.
11
Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;
33: 159-174.
12
Dasgupta A, Butt A, Saha TK, Basu G, Chattopadhyay A, and Mukherjee A. Assessment of Malnutrition
Among Adolescents: Can BMI be Replaced by MUAC. Indian J Community Med. 2010 April; 35(2):
276–279.
13
Chakraborty R, Bose K, Koziel S. Use of mid-upper arm circumference in determining undernutrition
and illness in rural adult Oraon men of Gumla District, Jharkhand, India. Rural and Remote Health
2011: 1754.
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
25
©UNICEF India/Divakar Mani
STATISTICAL TABLES
Table 1
Sample population (column %)
Characteristics
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
TOTAL
(N=1,063)
(N=1,070)
(N=917)
(N=1,133)
(N=1,980)
(N=2,203)
(N=4,183)
Class
6-8
9-12
100 100 58.7 54.5 80.3 76.7 78.6
# # 41.3 45.5 19.7 23.3 21.4
Residence
Rural
11.7 18.1 93.5 91.3 45.4 39.0 42.2
Urban
88.3 81.9 6.5 8.7 54.6 61.0 57.8
Adolescent characteristics
Distance
between school
and home
Mean (SD)
1.9 (1.4) 1.8 (1.5) 1.5 (1.7) 1.5 (1.5) 1.7 (1.6) 1.6 (1.5) 1.6 (1.5)
<1 km
10.8 9.8 30.4 27.7 19.9 19.0 19.5
1-2 km
80.0 81.5 62.3 65.2 71.8 73.1 72.4
3 km or more
9.2 8.7 7.3 7.1 8.3 7.9 8.1
Children
walking to
school
81.7 80.9 89.4 93.5 85.3 87.4 86.4
Children
working (n=88)
0.8 1.1 3.7 2.9 2.1 2.0 2.0
Paid work
33.3 33.3 38.2 36.4 34.9 37.8 36.5
Unpaid work
77.7 77.7 61.8 63.6 65.1 62.2 63.5
- 31.1 - 49.9 - 40.8 40.8
Sanitary
napkins
- 95.5 - 63.6 - 76.2 76.2
Free from
school
- 85.0 - - - 32.7 32.7
Purchased
- 10.5 - 63.6 - 43.5 43.5
Cloth
- 36.4 - 23.8 23.8
Illiterate
45.7 43.0 55.2 51.4 50.4 47.4 48.9
Primary
13.7 15.5 22.0 18.2 17.5 16.9 17.2
Middle or higher
40.6 41.5 22.8 30.4 32.1 35.7 33.9
Unemployed
79.2 77.0 78.0 77.8 78.8 75.7 77.3
Unskilled work
10.4 12.2 11.1 11.3 10.8 13.4 12.1
10.4
10.8
10.9
10.9
10.4
10.9
10.6
Menses
among girls
Started
Material used
during menses
(n=932)
4.5
Parental characteristics
Mother’s
education
Mother’s
occupation1
Skilled work
28
Statistical tables
Table 1
(cont.)
Characteristics
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
TOTAL
(N=1,063)
(N=1,070)
(N=917)
(N=1,133)
(N=1,980)
(N=2,203)
(N=4,183)
Parental characteristics
Father’s
education
Illiterate
26.3 28.9 30.7 28.2 28.4 28.6 28.5
Primary
13.0 11.7 16.9 14.3 14.8 13.0 13.9
Middle or higher
60.7 59.4 52.4 57.5 56.8 58.4 57.6
Unemployed
6.1 9.8 10.4 9.6 7.9 9.6 8.8
Unskilled
work
34.1 33.1 42.6 39.0 38.0 36.1 37.0
Skilled work
59.8 57.1 47.7 51.4 54.1 60.4 57.2
Kaccha
9.0 7.1 34.5 30.3 20.8 19.0 19.9
Pucca
89.8 91.7 64.1 68.7 77.9 79.9 78.9
Semi-pucca
1.1 1.2 1.4 1.0 1.3 1.1 1.2
Father’s
occupation1
Housing
Housing
2
Adolescents of Class 9-12 were not receiving WIFS tablets in Delhi.
#
Derived from Kuppuswamy’s classification for occupation.
Houses made from mud, thatch, or other low quality materials are called kaccha houses, houses that use partly
low quality and partly high quality materials are called semi-pucca houses, and houses made with high quality
materials throughout, including the floor, roof and exterior walls, are called pucca houses.
1
2
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
29
Table 2
Multidimensional index of poverty1 (column %)
Household
characteristics
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
TOTAL
(N=1,063)
(N=1,070)
(N=917)
(N=1,133)
(N=1,980)
(N=2,203)
(N=4,183)
BMI-for-age
z-score <-2SD
29.2 19.1 31.4 26.1 30.2 22.7 26.4
Non-improved
drinking water
facility2
30.6 28.2 24.7 19.0 27.8 23.5 25.7
No toilet facility at home
15.8 14.4 29.6 22.9 22.2 18.8 20.5
No access to
health facility
0.0 0.0 0.0 0.0 0.0 0.0 0.0
≥3 people
residing in one
room
77.3 80.5 70.9 74.0 74.3 77.2 75.8
Illiteracy
among
adolescents
0.0 0.0 0.0 0.0 0.0 0.0 0.0
Radio
13.9 16.4 10.8 13.9 12.5 15.1 13.8
Television
95.8 98.2 73.3 76.9 85.3 85.6 85.5
Mobile
97.7 97.9 90.8 91.4 94.5 94.1 94.3
Newspaper
17.4 17.1 11.9 13.2 14.9 15.1 15.0
Computer
5.3 6.1 0.9 2.3 3.1 4.2 3.7
Non-poor (0-1) 12.0 11.3 12.5 13.4 12.3 12.4 12.4
Moderate (2-3) 73.9 77.2 72.3 76.3 73.1 76.7 74.9
Severe (4-7)
14.1 11.5 15.2 10.3 14.6 10.9 12.8
Exposure to
media
Multidimensional index
of poverty
Includes seven components – BMI-for-age z-score <-2SD, drinking water facility, toilet facility at home, access
to health facility, illiteracy or less than primary literacy among adolescents, ≥3 household members living in one
room and exposure to media (newspapers, radio, television, computers or mobiles at home). Poverty threshold
score of 2-3 indicates moderate poverty and 4-7 indicates severe poverty.
2
Non-improved drinking water facility included unprotected dug well, unprotected spring, tanker truck/cart with
small tank and surface water.
1
30
Statistical tables
Table 3
Anthropometry and dietary status of sample population (column %)
Characteristics
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
TOTAL
(N=1,063)
(N=1,070)
(N=917)
(N=1,133)
(N=1,980)
(N=2,203)
(N=4,183)
BMI-for-age
z-score
Thin <-2SD1
29.2 19.1 31.4 26.1 30.2 22.7 26.5
Severely thin
<-3SD
10.2 5.5 8.6 6.2 9.4 5.8 7.6
Over nourished >2SD
0.9 1.1 0.0 0.3 0.5 0.6 0.6
65.8 74.8 67.4 72.2 66.5 73.4 70.0
Moderately
thin
41.7 34.1 32.1 30.1 37.3 32.0 34.7
Severely thin2
<16 cm
9.0 6.3 7.2 6.6 8.2 6.4 7.3
25.3 31.1 23.4 22.0 24.4 26.4 25.4
Severely
stunted <-3SD
7.1 9.7 4.7 3.9 6.0 6.5 6.3
9.5 22.9 17.8 23.1 13.3 23.0 18.2
Pulses or
beans
90.5 90.5 69.3 66.1 80.7 77.9 79.3
Dark GLVs
56.4 50.6 28.8 28.9 43.6 39.4 41.5
Vitamin C rich
fruit
39.2 40.4 21.4 23.5 31.0 31.7 31.3
Eggs
23.7 19.7 3.5 0.5 14.3 9.9 12.1
Fish/chicken/
meat
15.5 12.9 0.4 0.4 8.5 6.5 7.5
<3 food groups 46.1 47.7 48.2 51.6 47.1 49.8 48.5
3-5 food
groups
53.6 51.6 51.8 48.4 52.8 49.9 51.4
6-9 food
groups
0.3 0.7 - - 0.1 0.3 0.2
Normal ≤2SD
& ≥-2SD
MUAC
Height-for-age
z-score
Stunted
<-2SD1
Ate nothing
before coming
to school on
survey day
Iron-rich food
consumed
twice weekly
Dietary
diversity3
Includes children who are below -3SD from the WHO international growth standard median.
Includes children who have values below 18.5 cm.
3
Nine food groups include consumption of cereals, dark green leafy vegetables (GLVs), vitamin A rich foods,
fruits, organ meats, meats, eggs, pulses and milk in past 24-hour recall.
1
2
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
31
Table 4
Distribution of the sample population by age and sex (row %)
Agewise
distribution
(completed years)
BMI-for-age
Height-for-age
z-score
z-score
N
<-2SD
<-3SD
<-2SD
<-3SD
MUAC
<18.5 cm
<16 cm
10
Boys
131
19.1
5.3
9.2
0.8
66.4
18.3
Girls
195
17.4
4.6
20.5
4.6
61.5
11.8
Boys
393
24.4
5.3
15.8
5.3
53.7
Girls
455
25.9
7.2
28.4
7.3
52.7
10.5
Boys
473
29.8
9.9
25.5
9.9
44.0
8.7
Girls
447
25.3
5.4
29.1
5.4
34.9
6.5
Boys
423
32.6
11.6
30.0
11.6
33.3
7.8
Girls
400
23.5
6.0
26.5
6.0
24.7
4.5
Boys
239
35.6
11.7
31.0
11.7
23.8
7.5
Girls
251
18.7
4.8
31.9
4.8
16.7
3.2
Boys
147
40.1
12.2
29.3
12.2
13.6
4.8
Girls
172
18.0
4.1
19.8
4.1
10.5
3.5
Boys
89
30.3
6.7
25.8
6.7
7.9
2.2
Girls
143
23.1
8.4
21.0
8.4
11.2
3.5
Boys
48
33.3
14.6
25.0
14.6
10.4
4.2
Girls
85
23.5
5.9
23.5
5.9
11.8
2.4
Boys
37
32.4
10.8
32.4
5.4
5.4
2.7
Girls
55
18.2
5.5
23.6
-
9.1
5.5
Boys
1,980
30.2
9.4
24.8
8.9
28.7
7.2
Girls
2,203
22.7
5.8
24.9
6.5
25.9
6.4
TOTAL
4,183
26.5
7.6
24.9
7.7
27.3
6.8
11
8.7
12
13
14
15
16
17
18-19
10-19
32
Statistical tables
Table 5
Diagnostic accuracy of MUAC in identifying thinness
BMI method
(Gold standard)
BMI <-2SD
Undernourished
BMI ≥-2 SD
Non-undernourished
Total
MUAC method
Prevalence
Sensitivity
= 26.2%
= 73.4%
Specificity
= 79.2%
Positive (<18.5 cm)
Undernourished
803 (True +ve)
641(False +ve)
1444
PV+
PV-
= 55.6%
= 89.4%
Negative (≥18.5 cm)
Non-undernourished
296 (False –ve)
2443 (True –ve)
2739
LR+
LR-
= 3.53
= 0.34 (95%
CI 0.31-0.38)
Total
1099
3084
BMI <-3SD
Undernourished
BMI ≥-3 SD
Non-undernourished
Total
Prevalence
Sensitivity
= 7.6%
= 62.6%
Specificity
= 97.3%
MUAC method
Positive (<16 cm)
Undernourished
198 (True +ve)
106 (False +ve)
304
PV+
PV-
= 63.2%
= 97%
Negative (≥16 cm)
Non-undernourished
118 (False –ve)
3761 (True –ve)
3879
LR+
LR-
= 33.9
= 0.38 (95%
CI 0.31-0.38)
Total
316
3867
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
33
Table 6
Consumption pattern of IFA in sample population of last three weeks from date of study (column %)
Characteristics
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
TOTAL
(N=1,063)
(N=1,070)
(N=917)
(N=1,133)
(N=1,980)
(N=2,203)
(N=4,183)
91.1 92.5 90.8 86.8 90.9 89.6 90.3
Never (0)
8.9 7.5 9.2 13.2 9.0 10.4 9.7
Once
24.9 17.9 20.5 26.0 22.9 22.1 22.5
Twice
32.1 30.7 21.3 17.7 27.1 24.1 25.6
All three times
34.1 43.9 49.0 43.1 41.0 43.4 42.2
Supervised IFA
consumption
43.8 50.4 69.8 65.4 44.1 41.9 43.0
NHE session in
past 2 weeks
23.5 30.2 34.9 37.8 28.8 34.1 31.5
Albendazole
consumption
65.2 65.5 63.4 62.3 64.4 63.9 64.2
IFA consumed at
least once
IFA Consumption
Protocol followed* N=488 N=637 N=502 N=554 N=990 N=1,191 N=2,181
Empty stomach
1.2 0.6 6.8 3.6 4.0 2.0 3.0
Without water
0.8 0.6 3.0 0.7 1.9 0.7 1.3
Chewed
3.5 2.5 8.4 8.3 6.5 5.2 5.8
* last consumption
NHE = nutrition and health education
34
Statistical tables
Table 7
Undesirable effects faced by sample population in past three weeks from the date of study
Characteristics
Delhi (N=2,133)
Haryana (N=2,050)
Pooled (N=4,183)
n
%
n
%
n
%
1828 85.7 1740 84.9 3568 85.3
Faced
378 20.7 529 30.4 907 25.4
IFA discontinued
161 42.6 249 47.0 410 45.2
IFA continued
217 57.4 280 53.0 497 54.8
1450 79.3 1211 69.6 2661 74.6
435 30.0 259 21.4 694 26.1
1015 70.0 952 78.6 1967 73.9
1337 62.7 1293 63.1 2630 62.9
66 4.9 129 10.0 195 7.4
Week 1 (First consumption)
IFA consumption
Undesirable effects
No undesirable effects
Not faced
IFA discontinued
IFA continued
Week 2
IFA consumption
Undesirable effects
Faced
IFA discontinued
29 43.9 51 39.5 80 41.0
IFA continued
37 56.1 78 60.5 115 59.0
1271 95.1 1164 90.0 2435 92.6
IFA discontinued
410 32.2 271 23.3 685 28.1
IFA continued
861 67.8 893 76.7 1750 71.9
1125 52.7 1054 51.4 2181 52.1
No undesirable effects
Not faced
Week 3 (Recent consumption)
IFA consumption
Undesirable effects
Faced
Not faced
44 3.9 65 3.2 109 5.0
1081 96.1 989 96.8 2072 95.0
Details of undesirable effects1
Delhi (N=425)
Pattern
Faced once
Haryana (N=625)
Pooled (N=1,050)
380 89.4 548 87.7 928 88.4
Faced twice
28 6.6 57 9.1 85 8.1
Faced on every consumption
17 4.0 20 3.2 37 3.5
Nausea
40 9.4 60 9.6 100 9.5
Dizziness
38 8.9 42 6.7 80 7.6
340 80.0 498 79.7 838 79.8
Type
Abdominal pain
Black stool
3 0.7 11 1.8 14 1.3
Allergy
3 0.7 10 1.6 13 1.2
8 1.8 16 2.6 24 2.3
16 3.8 72 11.5 88 8.4
158 37.2 226 36.2 384 36.6
19 4.5 44 7.0 63 6.0
9 2.1 12 1.9 21 2.0
16 3.8 4 0.6 20 1.9
Fever
Perceived causes
2
IFA eaten on empty stomach
Body takes time to adjust to IFA
Chewed/broken IFA
IFA taken without water
Consumed IFA during menses
1
2
Based on having undesirable effects at least once.
Multiple choice question.
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
35
Table 8
Characteristics of adolescents who consumed one or two IFA vs those who
consumed three IFA (N=3,775)
Independent variables
Compliance (column %)
Consumed 1 or 2 IFA
Consumed 3 IFA
(N=2,006)
(N=1,769)
P value
Adj. OR 95% CI1
Background
characteristics
of adolescents
State
Delhi
56.2 47.0 0.001 1.00
Haryana
43.8 53.0
Boys
49.3 45.9 0.037 Girls
50.7 54.1
1.1 [0.9,1.3]
6-8
78.3 77.2 0.419 -
9-12
21.7 22.8
Urban
52.2 43.1 0.001 Rural
47.8 59.9
0
68.9 75.9 0.001 1
28.9 19.6
0.3 [0.2,0.4]
2
2.2 4.5
0.4 [0.3,0.6]
Negative/none
37.4 22.0 0.001 1.00
Positive
62.6 78.0
Negative
26.6 38.8 0.001 Positive
73.4 61.2
Negative
40.6 28.4 0.001 Positive
59.4 71.6
Low
21.7 33.1 0.001 High
78.3 66.9
1.4 [1.1,1.7]**
Gender
1.00
Class
Residence
1.00
1.1 [0.9,1.4]
Undesirable effects
No. of times faced
1.00
Enabling environment
Parental pressure
1.9 [1.7, 2.3]***
Teachers’ pressure
1.00
1.7 [1.4,1.9]***
Peer pressure
1.00
1.4 [1.2,1.7]***
Self-efficacy
1
36
1.4[1.3,1.8]***
Adjusted for: state, gender, class, residence, number of times facing side effects, enabling environment –
parents, school teachers, friends, self-motivated.
OR (CI) = Odds Ratio (Confidence Interval)
Significant at **p<0.01 and ***p<0.001
Statistical tables
1.00
Table 9
Compliance, barriers and perceived benefits for consumption of IFA1 (column %)
Responses
Delhi
Haryana
Pooled
Boys
Girls
Boys
Girls
Boys
Girls
(N=703)
(N=798)
(N=645)
(N=689)
(N=1,348)
(N=1,487)
Reasons for compliance2
Positive influencers
Friends
18.6 20.0 35.5 36.4 26.6 27.5
Family
28.6 20.1 35.6 50.6 38.5 44.3
Teachers
38.5 28.8 62.4 62.3 49.7 48.2
Media
0.3 0.2 0.2 0.1 0.2 0.2
Self-motivated
59.1 59 75.3 70.9 48.5 64.5
Did not face
undesirable effect
15.2 24.8 13.1 12.2 22.8 19.7
Following school
norms
33.9 31.7 22.9 30.7 28.7 31.2
Perceived benefits
Felt healthier
35.7 34.6 23.4 19.7 29.8 27.7
Felt energetic
24.5 20.8 11.6 10.3 18.3 15.9
Better physical
capacity
3.7 2.7 1.4 1.0 5.1 2.0
Less pain during
menses
- 4.4 - 2.9 - 3.7
Do not fall sick
18.6 17.7 20.0 17.1 37.7 17.4
Increased blood
1.3 1.3 9.5 5.5 5.2 3.2
No benefit
25.5 27.9 22.6 25.7 24.1 26.9
N=488 N=637 N=502 N=554 News
2.3 1.6 5.4 6.9 3.8 4.0
Parents
4.9 9.9 22.7 33.8 13.9 21.0
Barriers for nonconsumption3
N=990 N=1,191
Negative influencers
School
1.6 2.8 11.6 13.2 6.7 7.6
Fell sick after
consuming
IFA previously
5.3 10.8 15.0 24.4 11.0 17.1
Fear consumption
6.6 9.4 19.9 27.8 13.3 18.0
IFA not available
at school
8.4 3.8 7.4 9.9 7.9 6.6
Suffering from long
term illness
3.5 1.6 0.6 0.7 2.0 1.2
Multiple answers. The total may not correspond to 100%.
Consuming IFA tablet at least twice out of three times was considered as compliance (n=2,835).
3
Consuming IFA tablet fewer than two times out of three was considered for barriers (n=2,181).
1
2
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
37
Table 10
Sample and household characteristics of adolescents facing undesirable effects once or
twice or more times vs. those who did not (N=3,775)
Independent variables
Undesirable effects (column %)
None
Once
Two or more
(N=2,725)
(N=926)
times (N=124)
Delhi
78.3
19.4
2.3
Haryana
65.6
30.1
4.3
P value
State
0.001
Gender
Boys
50.9
40.4
31.5
Girls
49.1
59.6
68.5
6-8
80.4
72.8
58.1
9-12
19.6
27.2
41.9
2.0
2.4
31.5
98.0
97.6
68.5
Yes
85.9
87.5
86.3
No
14.1
12.5
13.7
<-2SD
26.4
27.2
22.6
>=-2SD
73.6
72.8
77.4
<-2SD
26.1
24.8
25.0
>=-2SD
73.9
75.2
75.0
Non-poor (0-1)
12.6
11.3
11.3
Moderate (2-3)
75.3
73.5
74.2
Severe (4-7)
12.1
15.1
14.5
0.001
Class
0.001
Work status
Working
Not working
0.786
Child walk to school
0.505
BMI-for-age z-score
0.539
Height-for-age z-score
0.752
Poverty index
38
Statistical tables
0.171
Table 11
Protocol for IFA administration and enabling environment for consumption of adolescents
facing undesirable effects once or twice or more times vs. those who did not (N=3,775)
Independent variables
Undesirable effects (column %)
None
Once
Two or more
(N=2,725)
(N=926)
times (N=124)
100.0
13.2
15.3
Without water
0.0
86.8
84.7
Chewed
0.0
89.2
71.8
P value
Protocols for IFA
administration
With water
Swallowed
100.0
10.8
28.2
Empty stomach
100.0
83.9
90.3
0.0
15.0
9.7
Yes
85.2
78.3
79.8
No
16.8
21.7
20.2
Positive
77.6
50.0
46.0
Negative
22.4
50.0
54.0
Full stomach
0.001
0.001
0.001
Skip meal before school
0.003
Enabling environment
Parental pressure
0.001
Teachers’ pressure
Positive
69.2
63.5
63.7
Negative
30.8
36.5
36.3
Positive
70.1
52.3
51.6
Negative
29.9
47.7
48.4
High
13.3
36.3
37.1
Low
86.7
63.7
62.9
0.003
Peer pressure
0.001
Self-efficacy
0.001
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
39
Table 12
Association from stepwise multinomial logistic regression between adolescents and
household characteristics, enabling environment and protocols for IFA consumption,
controlling for all covariates
Independent variables
Delhi
Faced undesirable
effects once
Faced undesirable
effects at least twice
OR
95% CI
OR
95% CI
1.87***
[1.5,2.4]
2.77**
[1.5,5.3]
0.97
[0.7,1.3]
0.80
[0.4,1.7]
1.30
[1.0,1.8]
1.15
[0.5,2.4]
1.30
[0.8,1.6]
1.40
[0.6,3.5]
Moderate vs rich
0.907
[0.6,1.3]
1.668
[0.5,5.6]
Severe vs rich
1.289
[0.8,2.0]
4.90*
[1.3,18.9]
0.984
[0.8,1.3]
2.73***
[1.5,5.0]
3.477***
[2.7,4.5]
5.084***
[2.7,9.5]
1.296*
[1.0,1.7]
2.576**
[1.4,4.7]
0.655**
[0.2,0.5]
0.745
[0.4,1.4]
0.318***
[0.9,1.5]
2.402**
[1.3,4.3]
11.18**
[2.0,63.6]
3.524***
[1.5,8.4]
10.97*
[1.7,71.0]
Gender
Girls vs boys
Class
6-8 vs 9-12
BMI-for-age
<-2 vs ≥2SD
No eating before coming to school
Yes vs no
Residence
Urban vs rural
Poverty
Maternal literacy
Illiterate vs literate
Parental pressure
No vs yes
Teachers’ pressure
No vs yes
Positive peer pressure
Yes vs no
Self-efficacy
Low/middle vs high
Tablet consumed without water
Yes vs no
Tablet chewed
Yes vs no
Tablet consumed empty stomach
Yes vs no
State
Haryana vs Delhi
Observations
1,958
Significant at *p<0.1, **p<0.01 and ***p<0.001
40
Statistical tables
425
Haryana
Pooled
Faced undesirable
effects once
Faced undesirable
effects at least twice
Faced undesirable
effects once
Faced undesirable
effects at least twice
OR
95% CI
OR
95% CI
OR
95% CI
OR
95% CI
1.357**
[1.1,1.7]
1.935**
[1.2,3.2]
1.53***
[1.3,1.8]
2.218***
[1.5,3.3]
1.328*
[1.1,1.7]
2.310**
[1.4,3.9]
1.158
[0.9,1.4]
2.283***
[1.4,3.6]
0.706**
[0.6,0.9]
1.048
[0.6,1.9]
0.94
[0.8,1.5]
0.74
[0.5,2.0]
1.191
[0.9,1.5]
0.94
[0.5,1.7]
1.251*
[1.0,1.5]
1.008
[0.6,1.6]
1.39
[1.0,2.0]
2.49**
[0.5,1.7]
1.27
[1.0,1.6]
1.97*
[1.1,3.5]
1.223
[0.9,1.7]
1.097
[0.6,2.2]
1.086
[0.9,1.4]
1.192
[0.7,2.1]
1.505
[1.0,2.3]
0.675
[0.2,2.0]
1.449*
[1.1,1.6]
1.773
[0.8,3.7]
0.906
[0.7,1.1]
1.106
[0.7,1.8]
0.95
[0.8,1.1]
1.618*
[1.1,2.4]
2.344***
[1.9,2.9]
2.567***
[1.6,4.2]
2.759***
[2.3,3.3]
3.439***
[2.3,5.1]
1.313*
[1.1,1.6]
0.816
[0.5,1.4]
1.327***
[1.1,1.6]
1.297
[0.9,1.9]
0.682***
[0.5,0.9]
0.667
[0.4,1.1]
0.683***
[0.6,0.8]
0.696
[0.5,1.0]
1.302*
[1.1,1.6]
0.929
[0.6,1.5]
0.488***
[0.4,0.6]
0.955
[0.6,1.44]
22.42**
[2.2,230.4]
16.44**
[4.1,66.5]
4.033***
[2.2,7.3]
4.033***
[2.3, 5.95]
50.27**
[4.4,578.8]
50.27**
[5.9,115.8]
2.396**
[1.3,4.5]
2.043***
1,817
625
3,775
[1.6,2.6]
1,050
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
41
Table 13
Responses of teachers to the information requested regarding WIFS programme in
selected schools (column %)
Responses
Delhi
Haryana
Pooled
(N=22)
(N=27)
(N=49)
0
4.5
55.6
32.7
1
86.4
40.7
61.2
2
9.1
3.7
6.1
Number of trainings received
Nodal person for WIFS
Teachers
90.9
85.2
87.8
Health service providers
9.1
0.0
4.1
Students (class monitor)
0.0
14.8
8.2
Kamzor bachon mein hotein hai (“It happens
to children who are visibly undernourished”)
59.1
14.8
34.7
Sarkar ki dwai kharab hoti hai (“Government
supply is of bad quality”)
40.9
85.2
65.3
Regular NHE to children, parents and leaders
9.1
14.8
10.2
Decrease IFA dosage
9.1
22.2
14.3
27.2
7.4
16.3
54.6
55.6
59.2
Reasons for undesirable effects
Recommendations to address
undesirable effects
Others
1
None
Others include: Follow WIFS protocol, to be given in presence of the emergency response system team.
1
NHE = nutrition and health education
42
Statistical tables
Table 14
Responses of medical officers to the queries on IFA supply and protocol for administration
(column %)
Responses
Delhi
Haryana
Pooled
(N=13)
(N=16)
(N=29)
Domino effect
30.8
37.5
38.2
Parents and community leaders do not
allow distribution of IFA
23.1
12.5
17.2
23.1
18.8
20.7
Kuposhit aur anemic bachon ko hot
hai (“It happens to children who are
undernourished or anaemic”)
76.9
56.3
58.6
Children do not follow WIFS protocol2
54.3
84.2
62.1
Ek doosre ko dekh kar bimar hjatein hain
(“Domino effect”)
69.2
31.3
48.3
Regular NHE to children, parents and
local leaders
30.8
73.7
62.1
Collaboration with education department
46.2
43.8
44.8
Positive media publicity
23.1
12.5
17.2
0.0
12.5
6.9
Medicines3 at schools in case
of emergency
61.5
68.8
65.5
Toll-free helpline number to schools
84.6
0.0
37.9
Contact details of hospitals/ERS team
during emergency
84.6
50.0
65.5
Dedicated vehicle on the day of IFA
administration
92.3
75.0
82.7
NHE to the school on management
of undesirable effects
69.2
56.3
62.1
Perceived barriers in administration
Teachers do not take responsibility
Perceived reasons of undesirable effects
1
Recommendations to improve IFA
administration1
Positive peer to peer counselling
Components of ERS
Multiple responses.
Protocols: Swallow IFA tablet, take with 1 glass of water, consume after meal.
3
Medicines include paracetamol, citrizine, digene, Oral Rehydration Solution (ORS) and ciprofloxin.
1
2
ERS = emergency response system
NHE = nutrition and health education
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
43
©UNICEF India/Divakar Mani
ANNEXES
Annex 1
Population Proportionate to Size (PPS) methodology
The sample population was selected using PPS cluster sampling method, which was
as follows:
1. All the schools with a functional IFA supplementation programme under the Directorate of Education in Delhi and Haryana were enlisted. This information was
obtained from the School Health Programme-MHFW.
2. Against the name of each school the corresponding population was written.
3. The cumulative population was calculated. For instance, in Delhi the cumulative
population was 303,489.
4. The sampling interval was calculated using the formula:
Total cumulative population ÷ 30
= 303,489÷30
= 101,16.3 ≅ 10,116
Therefore sampling interval is ≅ 10,116
5. A random number was selected using random number tables between 1 and
10,116. The random number selected was 9,899.
6. The school in which the cumulative population was nearly equal or greater to the
random number (9,899) was selected as the first cluster. The first cluster was taken
from school number 7.
7. Cluster No. 2: 9,899 (cluster No. 1) + sampling interval (10,116) = 20,015. A cluster
having a cumulative population nearly equal to 20,015 was taken as the second
cluster. The cluster was thus taken from school number 15.
8. The remaining 28 clusters were identified in a similar manner.
46
Annexes
Annex 2
List of 30 clusters from Delhi selected for the study
S No. District
School Name
Population
Cluster No.
1.
West A
Khyala, No.2-SKV
1431
532
2.
West A
Hari Nagar, Block-L S(Co-ed)V
1408
539
3.
West A
Rajouri Garden Extn.-GBSSS
1462
548
4.
West A
Madipur, No.2-SKV
1303
557
5.
West A
Mansarovar Garden-SV
1467
565
6.
West A
Kirti Nagar-GGSSS
906
574
7.
West A
West Patel Nagar-SKV
2147
581
8.
West B
Nangloi, Kavita Colony-G(Co-ed)SSS
2469
586
9.
West B
Paschim Vihar, B 3-SKV
1172
593
10.
West B
Mundka Village-GBSSS
1684
599
11.
West B
Punjabi Basti-G(Co-ed)SSS
1771
605
12.
West B
Ambika Vihar-GGSSS
1922
610
13.
West B
Nangloi, J.J. Colony-GBSSS
3358
613
14.
West B
Vikas Puri, Block A-SBV
1919
622
15.
West B
Kakrola-SBV
2648
628
16.
West B
Kakrola-SKV
3212
635
17.
West B
Bindapur-GBSSS
1459
640
18.
West B
Mohan Garden-SKV
3552
644
19.
West B
GBSSS No.1, Mohan Garden
3056
649
20.
West B
Bindapur, Pocket-IV-G(Co-ed)SS
751
656
21.
South West B
Samalkha-GBSSS
2303
710
22.
South West B
Palam Village, No.2-SKV
1534
715
23.
South West B
Samalka-SKV
2258
720
24.
South West B
Dwarka, Sector II-G(Co-ed)SSS
2338
726
25.
South West B
Shahabad Mohammadpur-GBSSS
583
737
26.
South West B
Najafgarh-S(Co-ed)V
919
746
27.
South West B
Dhansa-SKV
447
765
28.
South West B
Malikpur-G(Co-ed)SSS
379
776
29.
South West B
Nangli Sakrawati Village-G(Co-ed)SS
794
786
30.
South West B
Najafgarh, Dharampura-GBSSS
1480
790
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
47
Annex 3
48
Annexes
List of 30 clusters from Haryana selected for the study
S No. District
School Name
Population
Cluster
No.
1.
Hisar
GGSSS, Adampur
1164
14
2.
Hisar
GSSSS, Kirtan
696
23
3.
Hisar
GSSS, Barwala
1677
58
4.
Hisar
GHS, Badhawar
579
75
5.
Hisar
GSSS, Nalwa
800
109
6.
Hisar
GHS, Bhaniamirpur
399
126
7.
Hisar
GHS, Mehjad
194
181
8.
Hisar
GHS, Sarangpur
292
213
9.
Hisar
GHS, Shekhpura
223
258
10.
Hisar
GMS, Puthimangal Khan
390
265
11.
Hisar
GSSS, Bhatol
288
276
12.
Hisar
GHS, Uklanamandi
2200
287
13.
Jind
GHS, Defence colony Jind urban
1400
319
14.
Jind
GSSS, Kharakramji
330
356
15.
Jind
GSSS, Pindara
250
360
16.
Jind
GGHS, Rajhana Kalan
156
403
17.
Jind
GSSS, Dhatrath
342
429
18.
Jind
GHS, Mohammad Kheri
234
430
19.
Jind
GMS, Ghagoria
350
492
20.
Jind
GMS, Amheri
440
511
21.
Jind
GMS, Ismailpur
67
534
22.
Jind
GMS, Koyal
168
567
23.
Jind
GSSS, Dumerkha Khurd
311
598
24.
Jind
GSSS, Uchana
235
611
25.
Jind
GHS, Loder
1587
622
26.
Jhajar
GSSS, Madana Kalan
249
662
27.
Jhajar
GSSS, Birohar
167
699
28.
Jhajar
GHS, Dehkora
151
745
29.
Jhajar
GSSS, Jasor Kheri
145
739
30.
Jhajar
GSSS, Dulhera
362
841
Annex 4
Sample size calculation
Minimum sample size per district:
Z 2 * (p) * (1-p) ______________________________ x 1.5
c2 ss =
Sample size = 1.96 x 1.96 * (0.2) * (0.8)
_______________________________ x 3 = 2049
0.03 x 0.03 Where:
Z = 1.96 for 95% confidence interval
p = 0.20
q = 0.80
c = 15% of 20 expressed as decimal = 0.03
Design effect = 3
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
49
ACKNOWLEDGEMENTS
Study design, data collection, analysis and writing
Dr. Vani Sethi
Ms. Palak Gupta
Ms. Radhika Sood
Nutrition Specialist, Child Development and Nutrition Programme,
UNICEF India Country Office, Delhi
PhD. scholar, Department of Foods and Nutrition,
Lady Irwin College, University of Delhi, Delhi
PhD. scholar, Department of Foods and Nutrition,
Lady Irwin College, University of Delhi, Delhi
Data collection
Postgraduate students with specialization in ‘Foods and Nutrition’ from academic institutions in
Delhi and Haryana:
Lady Irwin College, Delhi
Ms. Surbhi Aggarwal
Ms. Prachi Ahuja
Ms. Jagriti Jain
Ms. Shaivya Rani
Manav Rachna University, Haryana
Ms. Surbhi Gandhi
Ms. Tania Kar
Ms. Shalini Khetarpal
Ms. Mansi Rajput
Ms. Shreya Ratra
Ms. Rabia Saluja
Ms. Himani Sharma
Ms. Shivani Sharma
Ms. Shalini Thakur
Ms. Kavita Tiwari
Ms. Khushboo Verma
Ms. Kiran Yadav
Statistical advice
Dr. Dimple Kondal
Public Health Foundation of India, New Delhi
Study design and data collection facilitation
Adolescent Health Division, Ministry of Health and Family Welfare, Government of India
Dr. Sushma Dureja
Joint Commissioner, Adolescent Health
Dr. Sheetal Rahi
Medical Officer, Adolescent Health
Ms. Anshu Mohan
Programme Manager, Adolescent Health
50
Contributors
Department of Health and Family Welfare, Government of Haryana
Dr. Inoshi Sharma
Director, Adolescent Health Division
Dr. Deepika Gupta
Coordinator, School Health Scheme
State Consultant, Adolescent Health Division
Dr. Sadhna Agarwal
District School Health Officer, Jind
Dr. Anshu Dalal
Senior Medical Officer, Jhajhar
Dr. Kumud Sharma
Civil Surgeon, Hissar
Dr. AK Choudhary
Department of Health and Family Welfare, Delhi
Additional Director/Head, School Health Scheme
Dr. JP Kapoor
Coordinator, School Health Scheme
Ms. Swati Singh
District In-charge, South-West B
Dr. BK Jha
District In-charge, West B
Dr. Poonam Kishore
District In-charge, West A
Dr. Sangeeta Rani
UNICEF
Dr. Jee Hyun Rah
Nutrition Specialist, Child Development and Nutrition Programme,
UNICEF India Country Office, Delhi
Editor
Ms. Delice Gan
Funding
UNICEF
Design and pre-press production
Lopez Design
Incidence and Determinants of Undesirable Effects following Iron and Folic Acid Supplementation
51
NOTES
52
United Nations Children´s Fund
India Country Office
UNICEF House
73, Lodi Estate
New Delhi 110003
Telephone: +91 11 24690401
www.unicef.in
©UNICEF India, 2014