MR Imaging Differentiation of Soft
advertisement

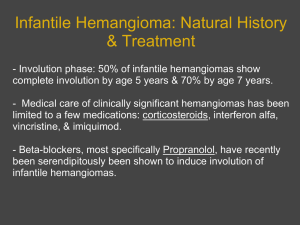
MR Imaging Differentiation of SoftTissue Hemangiomas from Malignant Soft-Tissue Masses Eu-Leong H. J. Teo 1,2 Peter J. Strouse 1 Ramiro J. Hernandez 1 OBJECTIVE. The purpose of this study was to determine whether MR imaging features can reliably distinguish hemangiomas from malignant soft-tissue masses. MATERIALS AND METHODS. We retrospectively reviewed MR imaging studies of 22 patients with soft-tissue hemangiomas and 22 patients with malignant soft-tissue masses. Images were reviewed and agreement reached by a consensus interpretation of two observers and by an independent observer. Masses were evaluated for signal intensity on T1- and T2-weighted images, for enhancement with gadolinium administration, and for morphology (lobulation, septation, central low-intensity dots). Lesion T2 signal and lesion enhancement with gadolinium administration were also objectively measured using regions of interest and comparison with skeletal muscle. RESULTS. Signal intensity on T1-weighted imaging of hemangiomas and malignant soft-tissue masses was similar. Subjective analysis showed greater T2 signal and gadolinium enhancement in hemangiomas; however, the differences were not statistically significant on objective analysis. Lobulation, septation, and central low-signal-intensity dots were all more common in hemangiomas, with statistical significance achieved; the combination of all three findings was specific for hemangioma. CONCLUSION. Although no single MR imaging feature was diagnostic in this study, analysis of lesion morphology, signal intensity, and enhancement with gadolinium allowed MR imaging differentiation of hemangiomas from malignant soft-tissue masses. H Received July 20, 1999; accepted after revision November 3, 1999. Presented at the annual meeting of the American Roentgen Ray Society, Boston, May 1997. 1 Section of Pediatric Radiology, Department of Radiology, C. S. Mott Children’s Hospital, University of Michigan Health Centers, Ann Arbor, MI 48109-0252. Address correspondence to R. J. Hernandez. 2 Present address: 26 Leedon Rd., Singapore 1026. AJR 2000;174:1623–1628 0361–803X/00/1746–1623 © American Roentgen Ray Society AJR:174, June 2000 emangiomas are common neoplasms that account for 7% of all benign soft-tissue tumors [1]. Although the biologic classification of vascular anomalies proposed by Mulliken and Glowacki [2] separates hemangioma of infancy from vascular malformations, the term “hemangioma” is used in this article to generically encompass hemangiomas and vascular malformations. Most patients with deep-seated hemangiomas present with either pain or intermittent swelling. Patients occasionally describe a poorly delineated mass that becomes larger or smaller from time to time. Deep-seated hemangiomas cannot be distinguished from malignant soft-tissue tumors without imaging studies. When imaging can distinguish hemangiomas from malignant soft-tissue tumors, patient management is affected regarding the need for further imaging or biopsy and the choice of therapy. Other researchers have described the MR imaging features of hemangiomas [1, 3–5]. Some studies have indicated that hemangiomas may be correctly diagnosed and distin- guished from malignant soft-tissue masses by their characteristic MR appearances [6–8]. Our objective in this study was to compare the MR imaging features of hemangiomas with those of malignant soft-tissue masses and to determine the combination of features that would allow hemangiomas to be distinguished from malignant soft-tissue masses. Materials and Methods The MR images of 22 patients with peripheral hemangiomas and 22 patients with primary malignant soft-tissue masses were retrospectively reviewed. The patients were consecutively imaged at our institution between 1992 and 1997 for hemangiomas and between 1995 and 1997 for the malignant soft-tissue masses. All patients were imaged before biopsy or surgery, when performed. The age range of the patients with hemangiomas was 2–43 years (median, 12 years) and with malignant soft-tissue masses was 3 months to 87 years (median, 53 years). Of the 22 hemangiomas, the diagnosis (three arterial venous malformations, two venous malformations, one benign vascular mal- 1623 Teo et al. formation, one cavernous hemangioma, three hemangiomas) was made histologically in 10 patients, on angiography in six, and by the characteristic clinical findings and follow-up in the remaining six patients. Malignant soft-tissue masses were confirmed histologically in all 22 patients. The soft-tissue masses were seven malignant fibrous histiocytomas, five rhabdomyosarcomas, two neurofibrosarcomas, two primitive neuroectodermal tumors, and six other soft-tissue sarcomas. All patients were imaged using a Signa 1.5-T scanner (General Electric Medical Systems, Milwaukee, WI). T1- and T2-weighted images were acquired in all patients. Eleven hemangiomas and 21 malignant soft-tissue masses were imaged after IV gadolinium administration (gadopentetate dimeglumine, 0.1 mmol/kg) using T1-weighted images with fat saturation. Gadolinium-enhanced images were obtained with a short delay after administration. The images were interpreted without knowledge of the final diagnosis of the soft-tissue mass or patient age. Two radiologists reviewed the images and arrived at a consensus interpretation of the imaging features. A third radiologist reviewed the images independently after being educated with regard to the imaging definitions. The purpose of the third reader was to provide a reliability measure for the imaging criteria used. The masses were evaluated for the signal intensity of the lesions on unenhanced T1weighted images, gadolinium-enhanced T1-weighted images, and T2-weighted images and for the morphologic features of the lesions: lobulation, septation, and the presence of central low-signal-intensity dots on T2-weighted images. Signal intensity was characterized as isointense or mildly, moderately, or TABLE 1 markedly hyperintense compared with the signal intensity of skeletal muscle. A lesion was considered lobulated if it showed internal septations resulting in a grapelike configuration (Figs. 1 and 2). It was considered septate if internal divisions or septa subdivided it into several smaller compartments (Fig. 3). The central low-signal-intensity dot sign on T2weighted images was deemed to be present if at least three or more punctate central low-signal-intensity dots were present in the center of the lobulation (Fig. 2). To obtain objective evaluation of the signal intensities of the lesions, measurements of regions of interest of representative portions of the lesions were compared with similar sized regions of interest in adjacent skeletal muscle. A ratio between the two signal intensities was calculated for each lesion seen on both gadolinium-enhanced T1weighted images and unenhanced T2-weighted images. The T2 relaxation time of the lesions was calculated for 18 hemangiomas and eight malignant soft-tissue masses in which dual-echo imaging was performed. T2 was calculated using the formula: T2 = (TE2 – TE1) / (Ln [ROI1 / ROI2]), where TE1 = time to first echo (msec), TE2 = time to second echo (msec), Ln = natural logarithm, ROI1 = signal intensity of region of interest on first echo, and ROI2 = signal of intensity of region of interest on second echo. Statistical analysis was performed using the chi-square test for categoric data and the independent t test for continuous data. The agreement between the consensus and the independent readings was assessed using the kappa statistic. Statistical significance was set at the 0.05 level. Frequency of Lobulations, Septations, and Central Low-Signal-Intensity Dots in Hemangiomas and Malignant Soft-Tissue Masses on T2-Weighted Imaging Lobulation Central Low-SignalIntensity Dots Septation Feature Imaged Hemangiomas (n = 22) Malignant soft-tissue masses (n = 22) A B A B A B 21 5 19 8 22 15 19 2 21 0 18 2 Note.—A = consensus interpretation by two radiologists, B = interpretation by one radiologist. TABLE 2 Frequency of Combined Lobulations, Septations, and Central Low-Signal-Intensity Dots in Hemangiomas and Malignant Soft-Tissue Masses on T2-Weighted Imaging Fig. 1.—Diagram shows septations and lobulations. In a septate mass, septa do not form lobulations. 1624 Characteristics on T1-Weighted Images T1-weighted images showed no reliable distinguishing features. Both hemangiomas and soft-tissue tumors were low in signal intensity. Characteristics on T2-Weighted Images The frequency of lobulation, septation, and central low-intensity dots on T2-weighted images was much higher for hemangiomas than for malignant soft-tissue tumors (Table 1). This difference was statistically significant for the consensus and independent readings. Masses with all three imaging characteristics (lobulations, septations, and central low-intensity dots) present were exclusively hemangiomas, independent of whether the consensus or independent readings were used (Table 2). Hemangiomas frequently had a lobulated appearance and central low-intensity dot. On the other hand, malignant soft-tissue tumors occasionally had septations and rarely had a central low-intensity dot. The T2 signal intensities of hemangiomas were generally higher than those of malignant soft-tissue masses (Table 3). Although subjective, this difference was found to be statistically significant for both the consensus and independent readings. Although the quantitative analysis revealed higher values of signal intensity ratios for hemangiomas than for malignant soft-tissue masses (Fig. 4), no statistical significance was observed. Characteristics on Gadolinium-Enhanced T1-Weighted Images In general, hemangiomas were judged to enhance markedly compared with malignant soft-tissue tumors (Table 4). This difference was statistically significant for both the consensus and independent readings. Although the median of the signal-intensity ratios for hemangiomas was higher than the median for malignant soft-tissue masses (Fig. 5), the difference was not statistically significant. Calculated T2 Relaxation Times Present Absent A B A B In general, hemangiomas had a higher T2 relaxation time than malignant soft-tissue masses (Fig. 6); however, the difference in calculated T2 relaxation times between hemangiomas and malignant soft-tissue masses was not statistically significant. 20 0 16 0 2 22 6 22 Consensus Versus Independent Readings Feature Imaged Hemangiomas (n = 22) MSTM (n = 22) Results Note.—A = consensus interpretation by two radiologists, B = interpretation by one radiologist, MSTM = malignant softtissue masses. Substantial agreement occurred between the two readings for the assessment of lobulations and central-low intensity dots (κ = 0.62–0.68), AJR:174, June 2000 MR Imaging of Soft-Tissue Hemangiomas B A Fig. 2.—10-year-old boy with hemangioma of lower extremity. A, Axial T1-weighted MR image (TR/TE, 500/16) shows low signal intensity of tumor (arrows) with interspersed areas of high signal intensity representing fat. B, Axial T2-weighted MR image (4000/85) shows lobulated high-signal-intensity lesion. Note several central low-signal-intensity dots (arrows). C, Gadolinium-enhanced T1-weighted MR image (500/16) shows marked enhancement of lesion. Central low-intensity dots seen on B are not seen after contrast administration, suggesting vascular nature. C TABLE 3 Subjective Evaluation of T2 Signal Intensity of Hemangiomas and Malignant Soft-Tissue Masses Compared with Skeletal Muscle Isointense Mild Moderate Marked Feature Imaged Hemangiomas (n = 22) MSTM (n = 22) A B A B A B A B 0 1 0 1 1 8 0 6 0 8 0 6 21 5 22 9 Note.—A = consensus interpretation by two radiologists, B = interpretation by one radiologist, MSTM = malignant soft-tissue masses. moderate agreement for the signal characteristic on T2-weighted images and the degree of enhancement after gadolinium (κ = 0.5–0.53), and fair agreement for the assessment of septation (κ = 0.3). AJR:174, June 2000 Discusson This study shows that hemangiomas have characteristic MR imaging features that enable their differentiation from malignant soft-tissue masses without the need for biopsy. Specifi- cally, these features are the lobulated and septate appearance of hemangiomas compared with malignant soft-tissue masses; the central low-intensity dot sign on T2-weighted imaging characteristically seen in hemangiomas; marked enhancement of hemangiomas after gadolinium administration on T1-weighted imaging; and the high T2 signal of hemangiomas compared with that of malignant soft-tissue masses. It is the summation of all these features, rather than any one particular feature taken in isolation, that will help the radiologist make a diagnosis of hemangioma. Although hemangiomas and vascular malformations constitute a continuum of pathologic abnormality, our study suggests that these le- 1625 Teo et al. distinction; however, it highlights the importance of distinguishing benign from malignant soft-tissue masses. In this paper, we have therefore used the generic term “hemangioma” to encompass sions may as a group manifest MR imaging characteristics that distinguish them from malignant soft-tissue masses. Admittedly, the grouping of a continuum of lesions blurs their TABLE 4 Evaluation of Degree of Gadolinium Enhancement of Hemangiomas and Malignant Soft-Tissue Masses No Enhancement Mild Moderate Marked Feature Imaged Hemangiomas (n = 11) MSTM (n = 21) A B A B A B A B 0 1 0 0 4 11 1 6 2 8 2 9 5 1 8 6 Note.—A = consensus interpretation by two radiologists, B = interpretation by one radiologist, MSTM = malignant soft-tissue masses. all hemangiomatous lesions and vascular malformations, although pathologic and imaging distinctions exist [2, 9]. Histologically, hemangiomas are vascular lesions containing nonvascular elements such as fat, fibrous and myxoid tissue, smooth muscle, thrombus, and even bone [10]. The MR imaging appearance of deep peripheral hemangiomas has been well described in the literature [1, 3–5, 11, 12]. Characteristics on T2-Weighted Imaging On T2-weighted images, hemangiomas have been described as having a multilobulated high-signal-intensity configuration interspersed B A Fig. 3.—7-year-old girl with malignant sarcoma of lower extremity. A, Axial T2-weighted MR image (TR/TE, 4500/90) shows high-signal-intensity mass posterior to femur. Note septations within mass, giving mass slightly lobulated appearance. Also note low-signal-intensity dots within mass (arrows); however, dots are not centrally located in a lobulation. B, T1-weighted image (500/8) shows marked enhancement. Low-signal-intensity dots (arrow ) in mass remain visible. Fig. 4.—Box plot shows signal-intensity ratios between tumor and muscle on T2-weighted MR imaging. Note that signal-intensity ratios are higher for hemangiomas than for malignant tumors. Upper margin of each box represents 75th percentile; lower margin represents 25th percentile. Line in middle of box represents median. Stars indicate outside values. 4 1626 5 Fig. 5.—Box plot shows signal intensity ratio between tumor and muscle on T1-weighted imaging after gadolinium administration. Note that enhancement with contrast material was higher for hemangiomas than for malignant soft-tissue tumors. Upper margin of box represents 75th percentile; lower margin represents 25th percentile. Line in middle of box represents median. Star indicates outside values. AJR:174, June 2000 MR Imaging of Soft-Tissue Hemangiomas Fig. 6.—Box plot shows calculated T2weighted MR imaging of hemangiomas and malignant soft-tissue tumors. Note higher values for hemangiomas. Upper margin of box represents 75th percentile; lower margin represents 25th percentile. Line in middle of box represents median. Circle indicates faroutside value. with linear and lacelike areas of low or intermediate signal intensity [1, 3, 4, 12]. This morphologic appearance is supported by our study. These findings were also shown by Cohen et al. [13], who suggested that the distinctive septate–lobulated appearance on T2-weighted imaging correlated with fibrous and fatty septa (low signal) between endothelial-lined vascular channels (high signal) identified on histologic examination. Our study suggests that the T2 signal intensity of hemangiomas is greater than that of malignant soft-tissue masses, although the quantitative assessment was not shown to be statistically significant. The lack of statistical significance was probably caused by the small sample in which this quantitative analysis was performed. The T2 signal intensity of lesions is a reflection of their T2 relaxation times. Hemangiomas have high T2 values, which may reflect pooling of the blood within cavernous spaces and slow flow within dilated venous channels [5]. Buetow et al. [3] suggested that the high T2 signal intensity of hemangiomas appeared to be related to increased free water in stagnant blood pooled in the larger vessels of lesions. The calculated T2 was not significantly different between hemangiomas and malignant soft-tissue masses in our study. However, the small numbers of malignant soft-tissue masses for which the T2 value could be calculated may have contributed to the lack of statistical significance. The central low-intensity dot sign on T2weighted imaging in hemangiomas has been previously described [1]. Our study has shown that this sign is highly specific for hemangiomas compared with malignant soft-tissue masses. These rounded foci of low signal intensity seen in hemangiomas may represent fibrofatty septa seen in cross section, or hyalinized or thrombosed vascular channels AJR:174, June 2000 [4]. Hawnaur et al. [11] have also suggested that smooth muscle components, fast flow within blood vessels, calcification, or ossification may give rise to this appearance. The central low-intensity dots are not likely to represent phleboliths because they were not recognizable on the T1-weighted images or on conventional radiographs. Fast flow in blood vessels is a likely cause in some cases because the central low-intensity dots disappear after gadolinium administration (Fig. 2C). This central low-intensity dot has also been described in benign neurofibromas, where it produces a so-called targetlike appearance [14, 15]. The pattern of enhancement is helpful in distinguishing between neurofibromas and hemangiomas. Because the central low-intensity dot in benign neurofibromas is caused by dense collagen, it is not likely to exhibit enhancement with gadolinium as hemangiomas do [15]. Characteristics on T1-Weighted Gadolinium-Enhanced Images Qualitative assessment revealed that hemangiomas showed a greater degree of enhancement with gadolinium than did malignant soft-tissue masses. Quantitative assessment of enhancement with gadolinium showed that the median of the region-of-interest ratios of hemangiomas was greater than that of malignant soft-tissue masses; however, the difference was not statistically significant. The small sample of hemangiomas in which gadolinium had been given may have contributed to the lack of statistical significance. Intense enhancement, therefore, is supportive of the diagnosis of hemangioma but should be used in corroboration of other findings to reach the diagnosis. We did not specifically analyze whether the presence of fat or its distribution in the lesion was a feature distinguishing hemangiomas from malignant soft-tissue masses. Fatcontaining malignant soft-tissue masses are rare in children. Although intercalated fat is a feature of hemangiomas, other fat-containing soft-tissue masses, most notably lipoblastoma, do occur in children [16, 17]. A possible limitation of this study is the small number of patients in both lesion groups in whom the quantitative parameters could be evaluated. This may have contributed to the lack of statistical significance in the differences in the T2 signal intensities, T2 relaxation times, and lesion enhancement with gadolinium in the objective parts of the study. A second limitation was the difference in the age ranges of the two patient populations. The group of patients with hemangiomas had an age range that was substantially lower than the age range of patients with malignant softtissue masses. The difference in age in our study between the two patient populations was necessitated by the relatively small number of malignant soft-tissue masses imaged with MR in pediatric patients. The difference in age range is not thought to be critical because the morphology of malignant soft-tissue masses on MR imaging is unlikely to be affected by the age of patients. The age of the patient in itself should not be overlooked as valuable information in helping to distinguish hemangiomas from malignant soft-tissue masses. Other clinical factors, such as chronicity of the mass and a rapid increase in its size, are also helpful. A third limitation of this study is the subjective assessment of imaging features such as septation, lobulation, and the degree of enhancement after gadolinium administration. Different observers may develop different thresholds, which is reflected by some degree of discrepancy in the assessment of septations and lesion enhancement between the consensus reading and the independent reader in our study. However, despite this variability and regardless of whether the consensus or independent readings are used, the combination of imaging findings (lobulation, septation, and central low-intensity dot) has predictive value. Last, this investigation is limited by the relatively small number of patients studied. It was not possible to include all types of malignant soft-tissue tumors in this analysis. Boon et al. [18] reported two cases of congenital fibrosarcoma mimicking congenital hemangioma. No case of this tumor was included in our study. Although it is possible that application of our criteria allowed the 1627 Teo et al. correct diagnosis, further analysis of a larger number of patients with a wider spectrum of malignant soft-tissue masses is warranted. In summary, this study suggests that hemangiomas can be distinguished from malignant soft-tissue masses on MR imaging by using a combination of morphologic features, the degree of enhancement after the administration of gadolinium, and the T2 signal intensity, potentially obviating biopsy in many cases. References 1. Suh JS, Hwang G, Hahn SB. Soft-tissue hemangiomas: MR manifestations in 23 patients. Skeletal Radiol 1994;23:621–625 2. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412–420 3. Buetow DC, Kransdorf MJ, Moser RP Jr, Jelink JS, Berrey BH. Radiological appearance of intramuscular hemangioma with emphasis on MR imaging. AJR 1990;154:563–567 4. Kaplan PA, Williams SM. Mucocutaneous and peripheral soft-tissue hemangiomas: MR imaging. Radiology 1987;163:163–166 1628 5. Jenner G, Soderlund V, Bauer HFC, Brosjo O. MR imaging of skeletal muscle hemangiomas. Acta Radiol 1996;37:140–144 6. Berquist TH, Ehman RL, King BF, Hodgman CG, Ilstrup DM. Value of MR imaging in differentiating benign from malignant soft-tissue masses: study of 95 lesions. AJR 1990;155:1251–1255 7. Crim JR, Seeger LL, Yao L, Chadnani V, Eckhardt JJ. Diagnosis of soft-tissue masses with MR imaging: can benign masses be differentiated from malignant ones? Radiology 1992;185:581–586 8. Moulton JS, Blebea JS, Dunco DM, Braley SE, Bisset GS III, Emery KH. MR imaging of softtissue masses: diagnostic efficacy and value of distinguishing between benign and malignant lesions. AJR 1995;164:1191–1199 9. Meyer JS, Hoffer FA, Barnes PD, Mulliken JB. Biological classification of soft-tissue vascular anomalies: MR correlation. AJR 1991;157:559–564 10. Allen PW, Enzinger FM. Hemangioma of the skeletal muscle: an analysis of 89 cases. Cancer 1972;29:8–22 11. Hawnaur JM, Whitehouse RW, Jenkins JPR, Isherwood I. Musculoskeletal haemangiomas: comparison of MRI with CT. Skeletal Radiol 1990;19: 251–258 12. Greenspan A, McGahan JP, Vogelsang P, Szabo RM. Imaging strategies in the evaluation of soft- 13. 14. 15. 16. 17. 18. tissue hemangiomas of the extremities: correlation of the findings of plain radiography, angiography, CT, MRI and ultrasonography in 12 histologically proven cases. Skeletal Radiol 1992; 21:11–18 Cohen EK, Kressel HY, Perosio T, et al. MR imaging of soft-tissue hemangiomas: correlation with pathologic findings. AJR 1988;150:1079–1081 Suh JS, Abenoza P, Galloway HR, Everson LI, Griffiths HJ. Peripheral [extracranial] nerve tumors: correlation of MR imaging and histologic findings. Radiology 1992;183:341–346 Bhargava R, Parha DM, Lasater OE, Chari RS, Chen G, Fletcher BS. MR imaging differentiation of benign and malignant peripheral nerve sheath tumors: use of the target sign. Pediatr Radiol 1997;27:124–129 Murphey MD, Fairbairn KJ, Parman LM, Baxter KG, Parsa MB, Smith WS. Musculoskeletal angiomatous lesions: radiologic-pathologic correlation. RadioGraphics 1995;15:893–917 Reiseter T, Nordshus T, Borthne A, Roald B, Naess P, Schistad O. Lipoblastoma: MRI appearances of rare paediatric soft tissue tumour. Pediatr Radiol 1999;29:542–545 Boon LM, Fishman SJ, Lund DP, Mulliken JB. Congenital fibrosarcoma masquerading as congenital hemangioma: report of two cases. J Pediatr Surg 1995;30:1378–1381 AJR:174, June 2000