Conservative approach in the treatment of the biliary tract`s
advertisement
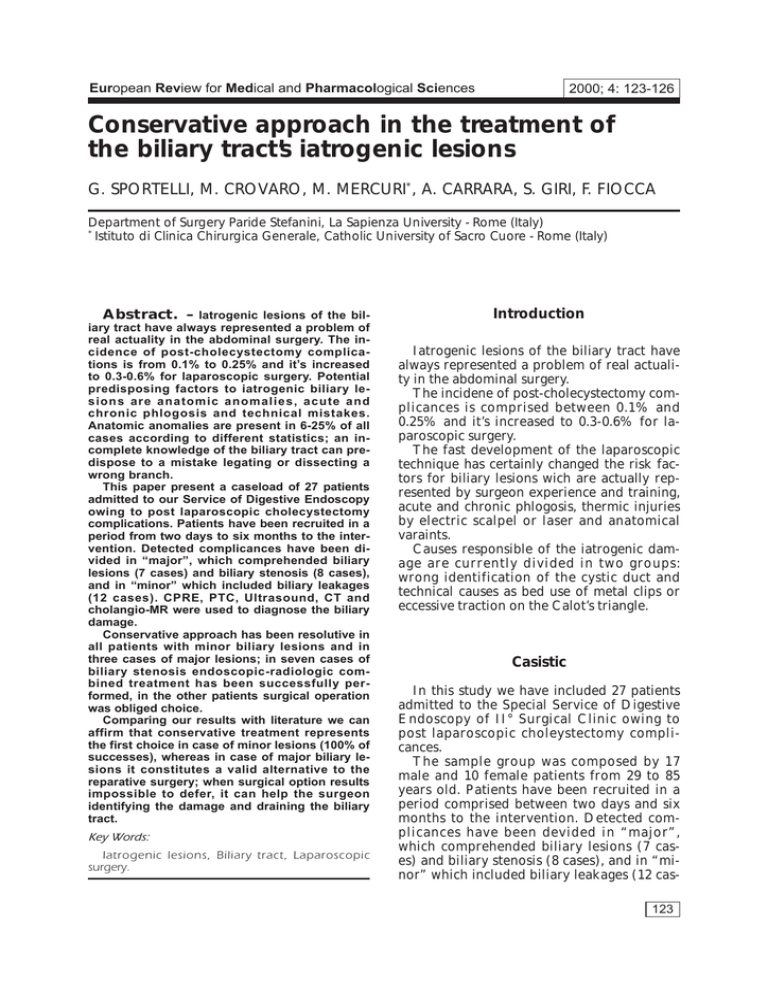
European Review for Medical and Pharmacological Sciences 2000; 4: 123-126 Conservative approach in the treatment of the biliary tract’s iatrogenic lesions G. SPORTELLI, M. CROVARO, M. MERCURI*, A. CARRARA, S. GIRI, F. FIOCCA Department of Surgery Paride Stefanini, La Sapienza University - Rome (Italy) * Istituto di Clinica Chirurgica Generale, Catholic University of Sacro Cuore - Rome (Italy) Abstract. – Iatrogenic lesions of the biliary tract have always represented a problem of real actuality in the abdominal surgery. The incidence of post-cholecystectomy complications is from 0.1% to 0.25% and it’s increased to 0.3-0.6% for laparoscopic surgery. Potential predisposing factors to iatrogenic biliary lesions are anatomic anomalies, acute and chronic phlogosis and technical mistakes. Anatomic anomalies are present in 6-25% of all cases according to different statistics; an incomplete knowledge of the biliary tract can predispose to a mistake legating or dissecting a wrong branch. This paper present a caseload of 27 patients admitted to our Service of Digestive Endoscopy owing to post laparoscopic cholecystectomy complications. Patients have been recruited in a period from two days to six months to the intervention. Detected complicances have been divided in “major”, which comprehended biliary lesions (7 cases) and biliary stenosis (8 cases), and in “minor” which included biliary leakages (12 cases). CPRE, PTC, Ultrasound, CT and cholangio-MR were used to diagnose the biliary damage. Conservative approach has been resolutive in all patients with minor biliary lesions and in three cases of major lesions; in seven cases of biliary stenosis endoscopic-radiologic combined treatment has been successfully performed, in the other patients surgical operation was obliged choice. Comparing our results with literature we can affirm that conservative treatment represents the first choice in case of minor lesions (100% of successes), whereas in case of major biliary lesions it constitutes a valid alternative to the reparative surgery; when surgical option results impossible to defer, it can help the surgeon identifying the damage and draining the biliary tract. Key Words: Iatrogenic lesions, Biliary tract, Laparoscopic surgery. Introduction Iatrogenic lesions of the biliary tract have always represented a problem of real actuality in the abdominal surgery. The incidene of post-cholecystectomy complicances is comprised between 0.1% and 0.25% and it’s increased to 0.3-0.6% for laparoscopic surgery. The fast development of the laparoscopic technique has certainly changed the risk factors for biliary lesions wich are actually represented by surgeon experience and training, acute and chronic phlogosis, thermic injuries by electric scalpel or laser and anatomical varaints. Causes responsible of the iatrogenic damage are currently divided in two groups: wrong identification of the cystic duct and technical causes as bed use of metal clips or eccessive traction on the Calot’s triangle. Casistic In this study we have included 27 patients admitted to the Special Service of Digestive Endoscopy of II° Surgical Clinic owing to post laparoscopic choleystectomy complicances. The sample group was composed by 17 male and 10 female patients from 29 to 85 years old. Patients have been recruited in a period comprised between two days and six months to the intervention. Detected complicances have been devided in “major”, which comprehended biliary lesions (7 cases) and biliary stenosis (8 cases), and in “minor” which included biliary leakages (12 cas123 G. Sportelli, M. Crovaro, M. Mercuri, A. Carrara, S. Giri, F. Fiocca es). Patients with biliary fistula referred manifestations attributable to choleperitoneum; patients with biliary stenosis presented symptoms of cholestatic jaundice more or less intense. CPRE, PTC, US, TC and cholangio RMN were used to diagnose the biliary damage. Results Conservative approach has been resolutive in all patients with minor biliary lesions: all leakages from cystic duct were resolved by endoscopic sphincterectomy and by positioning an endoscopic drainage; follow up of these patients in one year has demonstrate the complete solution of the case. Endoscopic-radiologic combined treatment has been used in seven cases of biliary stenosis; in one case of biliary costriction we have recurred to surgical intervention to remove a wrong positioned endoloop. Four of these cases have been definitely resolved, the other ones are still continuing the treatment by periodical substitutions of the stents. In major lesions endoscopic treatment of the damage has been performed only in three cases; in the other ones surgical operation was obliged choice. Anastomotic stenosis occurred in one patient submitted to surgery who required pneumatic dilatations by percutaneous transhepatic access. Follow up of these cases from tree months to three years have demonstrate the full welfare of six patients. Our results show that 22 of 27 patients have been treated with a non-invasive method; in patients with tight stenosis and biliary lesions of III° and IV° type according to Bismuth (four cases in total) the prolonged treatment raises perplexities about the opportunity either of a continuation of the conservative therapy or of an adequate surgical correction. Discussion Surgical complicances secundary to laparoscopic cholecystectomy represent a topic of real interest because of the rapid develop124 ment of this method which about in ten years has almost replaced the traditional surgery. Incidence of specific complications is about 0.5-5% according to different statistics, two or three times more than the “open surgery”, and represents concretely a problem not easy to solve. Potential predisposing factors to iatrogenic biliary lesions are anatomic anomalies, acute and chronic phlogosis, technical mistakes due to improper use of laparoscopic instruments, thermic or mechanic injuries, insufficient exposition of the Calots’ triangles structures. Anatomic anomalies are present in 6-25% of all cases according to different statistics; an incomplete knowledge of the biliary tract can predispose to a mistake ligating or dissecting a wrong branch. Therefore when the laparoscopic thecnique results difficult to perform because of phlogosis or adherences or when a lesion is suspected, an intraoperative cholangiograpy should be executed to value the biliary anatomy, to define the type and the location of possible lesions and to start an immediate therapy. Treatment results of tardive discovered lesions are worse than those of cases submitted to an immediate treatment. In spite of controversial advices it’s clear that an intraoperative cholangiography well performed can show the presence of residual biliary stones or anatomic anomalies and can reveal damages which could be repared immediately. All patients included in our study were submitted to CPRE associated to PTC in case of serried stenosis with incomplete images of the biliary tract. Bile walled off in abdomen (10 patients) were drained by percutaneous puncture. In ten patients with leakage from cystic duct and in one patient with patency of the Lushkas’ duct endoscopic spincterotomy and positioning of a trans papillar drainage have resolved the damage. In the patient with biliary overflow from an anomalous right duct we recurred to a combined treatment endoscopic-radiologic to have an exact definition of the hepatic parenchyma drained by the duct and of the lesions’ location. All patient with biliary stenosis were submitted to CPRE, in two cases of stenosis of the hepatics’ confluence (Bismuth III and IV) a PTC was necessary to define the stenosis grade and the number of included ductal stenosis; more- Conservative approach in the treatment of the biliary tract’s iatrogenic lesions over combined treatment permitted the positioning two internal external drainages after pneumatic dilatations of the stenosis. One patient with stenosis due to endoloop was submitted to a CPRE and successively to surgical operation to remove the loop. Two patients of those with biliary lesions and overflow (4 patients) were treated successfully using CPRE; the other two ones were operated after unlucky combined attemps to resolve the fistula. Therefore we assume that mini-invasive treatment should be the first approach to biliary complicances because also in case of total transection of the common bile duct it can bring the patient to surgical intervent in optimal conditions draining and decompressing the biliary tract; in this case the surgical treatment can be managed in a steryl aphlogistic field with minor conseguent complicances. The same mini-invasive approach appear less standardizable when a lesion or a stenosis of the common bile duct is present. In conclusions, laparoscopic cholecystectomy is certaienly the best treatment in terms of comfort and social coasts; higher elevate incidence of complicances represent the only blind point of a real valid intervention. Its routinary use associated to an instrumentarium improvment and a standardization of this technique will probably obtain a decrease of complicances in few years. The exact exposition of the Calots’ triangles’ structures (common bile duct, cystic duct, cystic artery), an anatomic dissection of the gallbladder bed and finally an adequate use of the electrocoagulation and of the metal clips seem to be primary assumptions for a correct laparoscopic cholecystectomy. All this must be supported by a perfect knowledge of the biliary anatomy; therefore the intraoperative cholangiography become a point of extreme importance to recognize prospective anatomic anomalies and expecially to spot the location of a prospective biliary lesion. Comparing our results with licterature we can assert that conservative treatment represents the first choice in case of minor lesions (100% of success), whereas in case of major biliary lesions it constitutes a valid alternative to the reparative surgery; when surgical operation results impossible to refer it can help the surgeon identifying the damage and draining the biliary tract. References 1) MIRZA DF, NARSIMHAN KL, FERRAZ NETO BH, MAYER AD, MCMASTER P, BUCKELS JAC. Bile duct injury following laparoscopic cholecystectomy: referral pattern and management. Br J Surg 1997; 84: 786-790. 2) TARGARONA EM, MARCO C, BALAGUÈ C, RODRIGUEZ J, C UGAT E, H OYUELA C, V ELOSO E, T RIAS M. How, when, and why bile duct iniury occurs. Surg End 1998, 12: 322-326. 3) MACFAYDEN BV, VECCHIO R. RICARDO A, MATHIS CR. Bile duct injury after laparoscopic. cholecystectomy. Surg End 1998; 12: 315-321. 4) Adamsen S, Hansen OH, Funch-Jensen P, Schulze S, Stage JG, Wara P. Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg 1997 June, 184: 571-578. 5) WOODS MS, TRAVERSO LW, KOZAREK RA, DONOHUE JH, F LETCHER DR, H UNTER JG et al. Biliary tract complication of laparoscopic cholecystectomy are detected more frequently with routine intraoperative cholangiography. Surg Endosc 1995: 9: 1076-1080. 6) LATTERI S. VECCHIO R, ANGILELLO A. Lesioni e stenosi biliari iatrogeniche. Giorn Chir 1997; 18: 61-64. 7) DUMONCEAU JM, DEVIÈRE J, DELHAYE M, BAIZE M, CREMER M. Plastic and metal -stents for postoperative benign bile duct strictures: the best and the worst. Castr Endosc 1998; 47: 8-17. 8) BEZZI M, SILECCHIA G, ORSI F, MATERIA A, SALVATORI FM, F I O C C A F, F A N T I N I A, B A S S O N, R O S S I P. Complications after laparoscopic cholecystectomy. Surg Endosc 1995; 9: 29-36. 9) BALSARA KP, DUBASH C, SHAH CR. Pseudoaneurysm of the hepatic artery along with common bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 1998: 12: 276-277. 10) STRASBERG SM, HERTL M, SOPER NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995; 180: 101-124. 11) BERCI G. Biliary ductal anatomy and anomalies. Surg Clin North Am 1992; 72: 1069-1075. 12) KOZAREK RA, BALL TJ, PATTERSON DJ, BRANDABUR JJ, RALTZ S, TRAVERSO W. Endoscopic treatment of biliary injury in the era of laparoscopic cholecystectomy. Gastr Endosc 1994; 40: 10-16. 13) W O O D S MS, T R A V E R S O W, K O Z A R E K RA. Charateristics of biliary tract complications during laparoscopic cholecystectomy: A multi-institutional study. Am J Surg 1994; 167: 27-32. 14) M ORGENSTERN L. M C G RATH MR, C ARROL BJ, PAZ PARTLOW M, BERCI G. Continuous hazards of the learning curve in laparoscopic cholecystectomy Am Surg 1995; 61: 914-918. 15) HANAZAKI K, SODEYAMA H, SODE Y et al. Endoscopic nasobiliary drainage for bile duct injury after laparoscopic cholecystectomy. Surg Endosc. 1997; 11: 1123-1125. 125 G. Sportelli, M. Crovaro, M. Mercuri, A. Carrara, S. Giri, F. Fiocca 16) DAVIDOFF AM, PAPPAS TN, MURRAY EA, HILLAREN DJ et al. Mechanism of major biliary injury during laparoscopic cholecystectomy. Ann Surg 1992; 215: 196-202. 23) C OX M, W ILSON T, J EAN P, PATBURY R, T OOULI J. Minimizing the risk of bile duct injury at laparoscopic cholecystectomy. World J Surg 1994, 18: 422-427. 17) Moossa AR, Easter DW, VANSONNERBERG E, CDSOLA G, D’AGOSTINO H. Laparoscopic injures to the bile duct. Ann Surg 1992; 215: 203-208. 24) A N D R É N -S A N D B E R G A, A L I N D E R G, B E N G M A R K S. Accidental lesions of the common bile duct at cholecystectomy. Ann Surg 1985; vol. 201, 3: 328-332. 18) T REROTOLA SO, S AVADER SJ, L UND G, V ENBRUX A, SOSTRE S, LILLEMOE K, CAMERON J, OSTERMAN F. Biliary tract complications following laparoscopic cholecystectomy: imaging and intervention. Radiology 1992; 184: 195-200. 19) BRANUM G, SCHIMTT C, BAILLIE J, SUHOKKI P et al. Management of major biliary complications after laparoscopic cholecystectomy. Ann Surg 1993; 217: 532-541. 20) R O C C A E, A I D A L A S, P L A C I D A G, C O S E N T I N I A, MORGIONE G, ROMEO G, TOMMASINI O, BAVA D. Il ruolo della laparoscopia nel determinismo e nella riparazione delle lesioni della via biliare extraepatica. Atti 98° Congresso Società Italiana Chirurgia Vol 2. 21) NUZZO G, MURAZIO M, GIULIANTE F. Inquadramento nosologico delle lesioni iatrogene della via biliare. Atti 980 Congresso Società Italiana Chirurgia. Vol. 2 22) DC B ROOKS , B ECKER J, C ONNORS P, C ARR -L OCKE . Management of bile leaks following laparoscopic cholecystectomy. Surg Endosc. 1993, 7: 292295. 126 25) MCMAHON AJ, FULLARTON G, BAXTER JN, O’DWYER PJ. Bileduct injury and bile leakage in laparoscopic cholecystectomy. Brit J Surg 1995; 82: 307-313. 26) RANDLE VOYLES C, SANDERS D, HOGAN R. Common bile duct evaluation in the era of laparoscopic cholecystectomy. Ann Surg 1994; 219: 744-752. 27) PITT H, KAUFMAN S, COLEMAN J, WHITE R, CAMERON J. Benign postoperative biliary strictures. Ann Surg 1989, 210: 417-425. 28) RUSSEL J, WALSH S, MATTLE A, LYNCH J. Bile duct injures, 1989-1993. Arch Surg 1996; 131: 382-387. 29) R A N T I S P, G R E E N L E H, P I C K E M A N J, P R I N Z R. Laparoscopic cholecystectomy bile duct injures. Am Surg 1993; 59: 534-540. 30) PETERS J, OLLILA D et al. Diagnosis and management of bile leaks following laparoscopic cholecystectomy. Surg Lapar Endosc 1994; 4: 163170. 31) MORGENSTERN L, WONG L, BERCI G. Twelve hundred open cholecystectomy before the laparoscopic era. Arch Surg 1992; 127:400-403.