The Effects of the Femoral Component on Cortical Bone Shape
advertisement

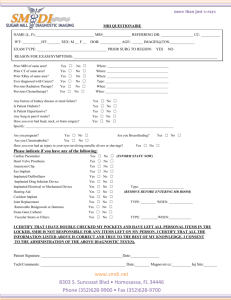
The Effects of the Femoral Component on Cortical Bone Shape Following Total Hip Arthroplasty +Rosenbaum, T G; +Ashrafi, S; +Lester, K; +**Bloebaum, R D +Bone and Joint Research Lab, SLC VA Health Care System, **Dept of Orthopedics, University of Utah, Salt Lake City, UT INTRODUCTION: Femoral components may affect the magnitude and direction of loads placed on the proximal femur. Altered loads may result in stress-shielding, which can lead to bone resorption and mechanical implant loosening. Previously, finite element analysis models have qualitatively predicted in vivo cortical bone shape changes such as stress shielding and point effect1, 2, and quantitively predicted bone density changes due to the femoral component3. Bilateral human femur studies have also quantified bone mineral changes between the implanted and unimplanted femurs4, 5 but only qualitatively describe changes in cortical bone shape5. To improve predictions based on implant design, studies should demonstrate the bone response due to the presence of the implant. After an extensive literature review, this study appears to be the first to quantify cortical bone shape differences between unimplanted and implanted human femur pairs from the same donors. Since the bilateral femurs experienced similar in situ conditions, cortical bone shape represented how the bone adapted to the magnitude and direction of the loads6. The objective of this study was to quantify cortical bone shape differences in order to deduce how the bone responded to the implant in an IRB approved protocol. Shape differences were quantified by comparing area, centroid, polar moment of area, principal moments of area, location of the principal axes (Imax, Imin), and inner/outer cortical diameter along Imax and Imin. The null hypothesis tested was that there would be no significant difference in the parameters of geometric shape between matched femoral pairs. METHODS: The five femur pairs (implant in situ time, 59 ± 46 months) were embedded in PMMA and sectioned at 25% (most proximal), 45%, 65%, and 85% (referred to as levels 1-4, respectively) along the length of the femoral component (Alloclassic design). The unimplanted femur was sectioned at the same levels. The 3-mm thick sections were oriented according to anatomical regions. Microradiographs were taken and digitally scanned. Cortical bone measurements and calibrations were performed in Scion Image (NIH). A macro was used that calculated area, centroid (x, y), polar moment of area (Ip), maximum and minimum second moments of area (Imax, Imin), and location of principal axes (Phi1, Phi2). Phi1 was the location of Imax (minor axis), and Phi2 was the location of Imin (major axis). Moments of area provide information on the cross-section’s resistance to bending or torsional loads. Polar moment of area (J) was calculated from Imax and Imin (J = Imax + Imin). Inner and outer cortical bone diameter was measured along Imax/Imin in Scion Image. The position of the Imax and Imin on the implanted femur was the axes selected for measuring both unimplanted and implanted cortical bone diameters. Statistical analysis included a two-way repeated measures analysis of variance (ANOVA) with Huynh-Feldt corrected degrees of freedom, with level (1, 2, 3, 4) as one repeated measurement and content (unimplanted or implant) as another repeated measurement. A significance of α ≤ 0.05 (p-value ≤ 0.05) and β ≤ 0.20 (Power =1-β, Power ≥ 0.80) was established. RESULTS: The mean area for the implanted specimens (293 + 158)mm2 was significantly less than the unimplanted specimens (424 + 108)mm2 (p = 0.016). Three patients (3, 4, and 5) had larger decreases in cortical area for the implanted femur (Table 1). Activity score (function, deformity, and motion) from the Harris Hip Score (HHS) was inversely correlated (r2 = 0.82, p = 0.034) to bone loss (Table 1). Pain, the other HHS element, was 44 for all the patients. No correlations (r2 < 0.2) existed between % bone loss and implant in situ time or patient weight. Table 1 – Percent bone loss between the cortical bone area (mm2) of the unimplanted (Unimpl) and implanted (Impl) femur of each patient. As the activity score decreased, % bone loss increased. Patient # Unimpl Impl % Bone Loss Activity 1 450 + 38 410 + 73 9% 56 2 591 + 20 500 + 79 15% 56 3 394 + 61 233 + 43 41% 37 4 281 + 16 148 + 43 47% 46 5 370 + 28 137 + 29 63% 18 Centroid x was not significantly affected by the implant (p = 0.061). In centroid y, trends were observed between levels. Ip and Imin means were higher in the unimplanted than the implanted (p < 0.05), but not Imax (p = 0.096). The location of the principal axes varied between patients and between levels. The outer diameter along Imax did not significantly change between unimplanted and implanted (p = 0.998); however, the Imax inner diameter of the implanted is significantly larger than the unimplanted (p = 0.030). Along Imin, the outer diameter (p = 0.005) and inner diameter (p = 0.003) significantly increased in the implanted as compared to the unimplanted (Table 2 and Figure 1). The mean percent differences between the unimplanted and implanted were larger for the inner diameter along Imax (20%) than the inner diameter along Imin (16%) showing net resorption along Imax. Table 2 – Cortical bone inner and outer diameters of the unimplanted and implanted along Imax and Imin of implanted femur (mean + std). P values and % differences are between unimplanted and implanted of each diameter measurement. Dia. (mm) Unimplanted Implanted p value % Diff Imax(outer) 29.8 + 4.8 29.8 + 3.9 0.998 0% Imax(inner) 19.1 + 6.1 23.8 + 6.6 0.030 20% Imin(outer) 31.8 + 6.8 33.4 + 7.2 0.005 5% Imin(inner) 20.3 + 8.7 24.1 + 9.6 0.003 16% Figure 1 – Cortical bone of patient 5 (level 4) showing principal axes. Anterior Anterior Imin Imax Imin Medial Unimplanted (Left) Imax Medial Implanted (Right) DISCUSSION: The reduction in cortical area observed in the implanted femur has usually been attributed to stress-shielding2. Resorption in the implanted femur agrees with Wolff’s Law and Frost’s Mechanostat Theory6 in that bone adapted to lower strains in the implanted femur because the minimum effective strain was not maintained. Decreased activity scores correlated to increased bone loss between femur pairs; therefore, bone loss cannot be attributed to implant design alone. This relationship requires further investigation. Although the direction and amount the principal axes rotated between unimplanted and implanted was variable, resorption along the Imax and cortical expansion along the Imin were the mechanisms for the Imax shifts between unimplanted and implanted. This is because Imax can only shift if bone resorbs/deposits or diameter expands/erodes in a new location. Since the mean % differences between the unimplanted and implanted were larger for the inner diameter along Imax (20%) than the inner diameter along Imin (16%), resorption concentrated around the Imax axis. The data also showed cortical expansion along Imin contributed to Imax shifts. However, the level of contribution of resorption versus cortical expansion requires further investigation. By understanding why the cortical bone changed in the implanted femur, we may equate the relationship of bone adaptation, implant design, and patient activity to methods of maintaining bone stock. REFERENCES: 1Doblare M. and Garcia J.M. J Biomech. 35, 1 (2001). 2Weinen H. et al. J Biomech 33, 809 (2000). 3Kerner et al. J Biomech. 32, 695 (1999). 4Sychterz C. et al. Clin Orthop, 389, 218 (2001). 5Bugbee W., Sychterz C., and Engh C. South Med J. 89, 1036 (1996). 6Frost H. M. Anat Rec. 219, 1 (1987) 50th Annual Meeting of the Orthopaedic Research Society Poster No: 1337