Some folded issues related to over
advertisement

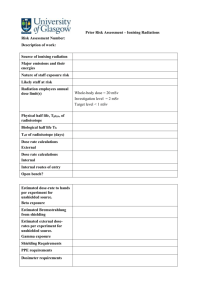
Journal of the Korean Physical Society, Vol. 67, No. 3, August 2015, pp. 599∼607 Some Folded Issues Related to Over-shielded and Unplanned Rooms for Medical Linear Accelerators - A Case Study Wazir Muhammad and Asad Ullah Health Physics Division, Pakisntan Institute of Nuclear Science & Technology (PINSTECH), Islamabad 45650, Pakistan Amjad Hussain Department of Oncology, Aga Khan University Hospital, Karachi 74800, Pakistan Nawab Ali Physics Division, Pakisntan Institute of Nuclear Science & Technology (PINSTECH), Islamabad 45650, Pakistan Khan Alam Department of Physics, University of Peshawar 25000, Khyber Pakhtunkhwa, Pakistan Gulzar Khan Department of Physics, Abul Wali Khan University, Mardan 23200, Khyber Pakhtunkhwa, Pakistan Matiullah Directorate of System & Services, Pakisntan Institute of Nuclear Science & Technology (PINSTECH), Islamabad 45650, Pakistan Seongjin Maeng and Sang Hoon Lee∗ School of Architectural, Civil, Environmental and Energy Engineering, Kyungpook National University, Daegu 702-701, Korea (Received 7 April 2015, in final form 27 May 2015) A medical linear accelerator (LINAC) room must be properly shielded to limit the outside radiation exposure to an acceptable safe level defined by individual state and international regulations. However, along with this prime objective, some additional issues are also important. The current case-study was designed to unfold the issues related to over-shielded and unplanned treatment rooms for LINACs. In this connection, an apparently unplanned and over-shielded treatment room of 610 × 610 cm2 in size was compared with a properly designed treatment room of 762 × 762 cm2 in size (i.e., by following the procedures and recommendations of the IAEA Safety Reports Series No. 47 and NCRP 151). Evaluation of the unplanned room indicated that it was over-shielded and that its size was not suitable for total body irradiation (TBI), although the license for such a treatment facility had been acquired for the installed machine. An overall 14.96% reduction in the total shielding volume (i.e., concrete) for an optimally planned room as compared to a non-planned room was estimated. Furthermore, the inner room’s dimensions were increased by 25%, in order to accommodate TBI patients. These results show that planning and design of the treatment rooms are imperative to avoid extra financial burden to the hospitals and to provide enough space for easy and safe handling of the patients. A spacious room is ideal for storing treatment accessories and facilitates TBI treatment. PACS numbers: 87.52.-g, 87.52.Ga, 87.65.-v Keywords: Radiation shielding, Medical linear accelerator (LINAC), Room design DOI: 10.3938/jkps.67.599 ∗ E-mail: lee@knu.ac.kr -599- -600- Journal of the Korean Physical Society, Vol. 67, No. 3, August 2015 I. INTRODUCTION Time, distance and shielding are the three important parameters that influence external radiation exposure. In other words, the radiation dose received by an individual is directly proportional to the spent time in the radiation field and inversely proportional to the square of distance from the source. The dose is also reduced if a shielding material is introduced [1,2]. In special circumstances, when the first two parameters (i.e., time and distance) cannot be compromised, radiation shielding plays an important role in reducing the individual exposure. The primary purpose of radiation shielding is to limit radiation exposure to the general public and employees of the radiation facilities to an acceptable level recommended by the International Atomic Energy Agency (IAEA) [3] or by an individual state regulatory body. Two types of radiation barriers or shielding, known as primary and secondary barriers, are considered to reduce radiation exposures from high-energy medical linear accelerators (LINACs) to within safe limits [1,2,4]. The primary barrier of the treatment room is irradiated directly by the radiation produced by the LINAC while the secondary barrier receives radiation scattered by the patient and by the different surfaces of the room, as well as leakage radiation from the machine’s head. The maximum beam size of the LINAC is used to determine the characteristics of the primary barrier. On the other hand, secondary radiations are, emitted in all directions and are therefore, considered for the entire treatment room [1,2]. Neutrons are produced at high-energy X-rays and electron beams (energies > 10 MV) through X-ray-neutron (x, n) and electron-neutron (e, n) reactions [1, 2, 4–12, 12, 14]. The X-ray target, primary collimators, beam flattening filters, collimator jaws, and X-ray beam accessories are the main sources of neutron contamination [1, 2,10]. The cross section for the (x, n) reaction is at least an order of magnitude larger than for the (e, n) reaction at the high energies of LINACs [2, 15]. The neutrons produced during the X-ray mode are of primary concern. Some elements, such as 15 O (t1/2 : 2 minutes) and 13 N (t1/2 : 10 minutes), inside the LINAC’s treatment room may also become radioactive with short half-lives (i.e., t1/2 ∼ seconds to a few minutes) by direct activation due to (x, n) reactions or by activation of secondary neutrons. The radiation produced by these radioactive elements contributes to the radiation exposure to the radiotherapy staff, who enter the treatment room after a high-energy photon-beam treatment [2,15]. Both the primary and the secondary barriers are designed to protect against expected photon and contamination neutron doses. The primary barrier of the treatment room is responsible for providing protection against primary/direct X-ray beams. On the other hand, secondary barriers are designed to provide protection against scattered and leakage photons and neutrons. These also attenuate the neutron-capture γ-rays [1]. A specially designed maze and door are essential to reduce the scattered and the leakage radiation fields along the maze [2]. For the design of a maze or duct, a strong knowledge of the scattering characteristics of X-rays is required [4]. Efficient room ventilation is an effective method for removing the radioactivity and will reduce the exposure to the radiotherapy staff who enter the treatment room after a high-energy photon-beam treatment [2]. The treatment room should be designed on the lowest floor of the building to avoid huge shielding loads on the floor [1,2]. The area around the treatment room is usually classified into two subtypes, controlled and uncontrolled, on the basis of the access, occupancy and working conditions. The former has limited-access immediate areas where radiation is used and where the occupational exposure to the radiation workers is under the supervision of an individual in charge of radiation protection [2,3]. Examples are treatment rooms, control consoles, and other areas that require control of access, occupancy and working conditions for radiation protection purposes. The latter are those occupied by the general public (i.e., patients, visitors) and workers not involved in any radiation related task [1,2]. The factors used in shielding calculations are as follows: • The occupancy factor (T) is the fraction of time that a particular area (i.e., controlled/uncontrolled) is occupied by radiation/nonradiation workers, patients or the general public. The choice of an appropriate T ensures the protection of the occupationally exposed (i.e., radiation workers), non-radiation workers, and members of the general public who may be exposed to radiation in these areas. The typical values of T are 1, 0.25 and 0.125 for offices, corridors and waiting rooms, respectively [1,2]. The first and main feature in the design of a LINAC’s treatment room is to surround it with areas having a zero or low value of T while keeping the heavily-occupied areas as far away as possible. The other feature of the LINAC’s treatment room is that it should be large enough that the movements of equipment during installation/service and of gurnies containing the patients for treatments are easy. • The workload (W) is expressed in Gy/week or Gy/year and is used to provide an indication of the amount of radiation produced in a week by Xray or γ-ray sources. It depends upon the dose per fraction, the expected number of patients treated per day, the number of work days per year and other uses such as physics quality assurance, blood irradiation and maintenance services [4]. A workload of 1000 Gy/week based on a dose of 4 Gy at 1 m per patient and a 5 day week for photon energies up to 10 MV is suggested in NCRP Reports # 49 Some Folded Issues Related to Over-shielded and Unplanned Rooms · · · – Wazir Muhammad et al. -601- & 151 [1,16]. For high-energy beams in dual energy LINACs, a workload of 500 Gy/week is estimated in NCRP Report 51 [4,17]. • The use factor (U) is the fraction of the beam’s on time for the primary beam in a particular direction. For primary beams, typical values of U are 1 for the floor and 0.25 each for the walls and ceiling. For secondary radiation, U is always equal to 1 because scatter is present always and everywhere [1, 2, 16, 18]. The main goal of the shielding is to reduce the dose equivalent (H) to minimum acceptable levels for radiation/non-radiation workers and members of the public. The dose levels used for the shielding calculation and for the evaluation of the radiation barriers are normally termed as the shielding design goals (P). There are different recommendations on the values of P for controlled and uncontrolled areas [1, 2, 16, 18]. At present, the IAEA recommended dose limits for controlled and uncontrolled areas are 20 mSv/year (i.e., averaged over 5 consecutive years and 50 mSv in any single year) and 1 mSv/year, respectively [3]. In the USA, for controlled and uncontrolled areas, doses are limited to 10 mSv/year (cumulative dose of age × 10 mSv, and 50 mSv in any single year) and 1 mSv/year (infrequently, 5 mSv annually), respectively [4,19]. According to NCRP Rep. 151, the recommended P values for controlled areas and uncontrolled areas are 0.1 mSv/week (5 mSv/year) and 0.02 mSv/week (1 mSv/year), respectively [1]. Normally, the consequences of under-shielded area are well known. However, an over-shielded unplanned area may have other associated financial and physical issues. A thorough literature survey was conducted to properly address optimal structural shielding & design requirements [1,2,4,17,20–22]. In light of the recommendations and technical information, issues associated with overshielded and unplanned LINAC exposure areas are identified to provide the reader with a better understanding of the factors involved in designing exposure areas for medical linear accelerators. The study is intended to be useful for medical/health physicists and other radiation protection professionals in the planning and designing of new exposure areas and in the assessment of existing facilities. II. MATERIALS AND METHODS 1. Calculational Methods A new room was designed for a LINAC producing multiple-energy photons (i.e., low & high with a maximum energy of 20 MV) with a maximum field size of 40 × 40 cm2 for intensity modulated radiation therapy (IMRT) and total-body irradiation by adopting the Fig. 1. (Color online) (a) Simplified schematic diagram and (b) side view of the treatment room for a 20-MV LINAC. guidelines recommended in the IAEA Safety Reports Series No. 47 and NCRP 151 [1, 4]. A workload of 1000 Gy/week based on a 4 Gy per treatment fraction at 1 meter for 5 days a week, as suggested in the NCRP Reports # 49 & 151, was used [1,16,17]. Regarding the permissible dose limits, the guidelines of the IAEA and ICRP Publication 33 were followed (i.e., 20 mSv/year and 1 mSv/year for controlled and uncontrolled populations, respectively) [2,3,23]. In accordance with the recommendations of the local regulatory authority, lower P values of 0.04 mSv/week and 0.002 mSv/week for controlled (radiation workers) and uncontrolled (non-radiation workers & member of the general public) populations, respectively, were used. All the distances, areas and values of T for the calculations were estimated from a scaled diagram of the new optimally-designed facility (Fig. 1). Concrete with a of density 2350 kg/m3 is assumed for shielding purposes. For concrete of this density, the documented values of the first tenth-value layer (TVL1) and the equilibrium tenth-value layer (TVLe ) are 0.46 m and 0.44 m, respectively, for the primary beam. For the scattered beam, a single value of 0.343 m is adopted for 20-MV photons [4,24]. The width of the primary barrier (WP B ) in meters is -602- Journal of the Korean Physical Society, Vol. 67, No. 3, August 2015 estimated as follows [1,2,4,16]: WP B = (F × X + 0.60)m, (1) where F is the diagonal of the maximum radiation field size (i.e., 0.56 m for a field size of 0.40 m × 0.40 m), X is the distance from the target to the wall-ceiling junction in meters, and 0.60 is an additional margin (i.e., 0.30 m on each side of the primary barrier) [1,16]. The barrier transmission factor (B) is the fraction of the incident beam’s air kerma in air transmitted through a given thickness of shielding material [1, 4, 16]. The Bpri corresponds to the primary radiation barrier and is calculated as below [1,4,16]: Bpri = P × (dpri )2 /(W × U × T ), (2) where dpri (m) is the distance from the source to the point protected outside the primary barrier. The number of TVLs based on the maximum energy of the beam (i.e., 20 MV) and the type of shielding material was calculated by using the following equation [1,4]: n = −T V L × log10 (B). (3) Hence, the required thickness of barrier in meters (m) is given by [1] S = T V L1 + (n − 1)T V Le . (4) The first (i.e., TVL1 ) and the equilibrium (i.e., TVLe), TVLs are used to account for the spectral changes as the radiation penetrates the barrier [1]. For designing secondary barriers, scattered (from the patient and surfaces) and leakage radiations were computed separately and compared in order to arrive at the final recommended thickness [1]. The required barrier transmission (Bs ) to shield against radiation scattered by the patient was computed as follows [1,4]: Bs = P d2sec d2sca 400 , aW T F (5) where dsca is the distance from the radiation source to the patient, (i.e., 1 m for LINACs), dsec is the distance from the patient to the point of interest, and ‘a’ is the scatter fraction defined at dsca. The primary scatter ratio ‘a’ depends on the energy of the X-ray beam and the scattering angle, and F is the area of the field incident on the patient (i.e., for LINACs with a maximum field size of 40 × 40 cm2 , F = 1600 cm2 ) [4]. Similarly, the barrier transmission factor (Bw ) that is needed to shield against scattered radiation when the primary beam strikes a wall is given by the following equation [1,4]: Bw = P d2w d2r . aAW T U (6) Here, dw and dr are the distances from the radiation source to the scattering surface (wall) and the distance from the scattering surface (wall) to the point of interest, respectively, α is the reflection coefficient for the barrier material, which depends on the wall’s material, the scattering angle, and the beam’s energy, and A is the beam’s area at first reflection. Finally, the required attenuation (Bl ) to shield against leakage radiation was calculated as follows [1,4]: Bl = P d2l 10−s W T (7) where dl is the distance from iso-center to the point of interest. Equations (3) and (4) were used to calculate the number of TVLs for the barrier thickness necessary to shield against the head leakage radiation and the radiation scattered from the patient and the surfaces. If the differences between the shielding thicknesses necessary to shield against head leakage and scatter from patient and from surfaces are less than three half-value layers, then to be on safe side, one half-value layer (HVL) of concrete is added to the larger thickness; otherwise, the larger shielding is enough for the required attenuation [4]. These techniques were used to design the primary and the secondary barriers of the walls and the roof of the room. For a gantry rotation axis perpendicular to the maze axis, the total dose at the maze entrance Dd (Gy/week) can be calculated by using the following relation [1]: Dd = ΣG DP + ΣG f × DwT + ΣG DL + ΣG DT , (8) where Dd is the dose due to radiation scattered from the patient, f is the primary radiation transmitted through the patient, DwT is the primary radiation scattered by the wall into the maze, DL is the leakage radiation scattered down the maze, and DT is the leakage radiation transmitted through the maze wall. In the NCRP-151 formalism, the first scatterer is taken to be the wall, but a better approximation is obtained if the patient is taken to be the first scatterer [1,16,17]. All the factors in Eq. (8) were calculated individually according to the guidelines provided in NCRP-151, and Dd (Gy/week) was finally calculated by using Eq. (8) [1,4,16, 17]. The calculated Dd was 1.14 × 10−4 Gy/week. This dose was added to the capture gamma and neutron doses at the maze entrance, which was calculated as below: The capture gamma dose in the maze Dϕ depends on the maze length d2 and the total neutron fluence ϕA = ϕd + ϕsc + ϕth at the inner maze point ‘A’, as shown in Fig. 1(a) [1, 4]. Here, ϕd , ϕsc and ϕth are the fluencies due to direct neutrons from the head of the accelerator and due to scattered and thermal neutrons, respectively. ‘A’ indicates the point of intersection of the center line of the maze and the line joining the iso-center and the end of the maze wall. The total neutron fluence was calculated as follows [4,11,12,25]: ϕA = (QN /4πd21 )+(5.4QN /2πS)+(1.26QN /2πS), (9) Some Folded Issues Related to Over-shielded and Unplanned Rooms · · · – Wazir Muhammad et al. -603- Table 1. The widths of the primary barriers, the distances from the source to the point protected outside the primary barrier (i.e., dpri ), the occupancy factor (T) and the shielding design goal (P) for each barrier, the calculated transmission factor (Bpri ), the number of TVLs (n), the thickness of the primary barriers (S), and the final recommended shielding thickness against the primary radiation of a LINAC having a maximum photon energy of 20 MV. Wall B D Width (cm) 450 450 dpri (cm) 748 748 Ceiling 450 590 T 0.063 0.063 0.025 0.063 P (Sv/w) 2E-6 2E-6 2E-6 4E-5 Bpri 7.16E-6 7.16E-6 1.11E-5 8.91E-5 n 5.15 5.15 4.95 4.05 Calculated S (cm) 237 237 228 186 Final Thickness (cm) 240 240 230 190∗ ∗ If a chiller room is designed above the treatment room, the chiller room will have limited occupancy and access may be restricted, thus allowing a greater design dose limit. where d1 is the distance from the source to the point of interest, and QN is the apparent neutron source strength in number of neutrons emitted from the shielded accelerator head per unit dose of photon delivered to the isocenter. QN is related to the neutron source strength Q [4]. The values of the Q are available in the published literature for LINACs with energies in the range of 10 − 25 MV [4, 21, 26]. S is the surface area of the treatment room, excluding the maze area, in m2 . The surface area S is the sum of all wall areas visible from the isocenter. Once the total neutron fluence ϕA at the inner maze point is determined, the capture gamma dose Dϕ is determined for the maze length d2 as follows [4,26]: d2 Dϕ = 5.7 × 10−16 ϕA × 10− 6.2 . (10) The weekly dose equivalent due to the capture gamma dose (in Sv/week) is calculated as follows: Dc = W × Dϕ . (11) The neutron dose at any point in the maze is calculated on basis of the distance from the inner maze point A to the iso-center (d1 ), the surface area S of the treatment room, the cross-sectional area of the inner entrance to the maze (Ar ) and the cross-sectional area of the maze (S1 ). These quantities are calculated from a scaled diagram of the room, as shown in Fig. 1(a). The neutron dose is also a function of the energy, the gantry angle and the field size of the photon beam. With the Kersey’s method to measure the neutron dose equivalent at the maze entrance, Dn in Sv per X-ray·Gy at the iso-center is given as follows [4,27,28]: Dn = 2.4 × 10−15 × ϕA × Ar /S1 d2 −( d2 ) × [1.64 × 10−( 1.9 ) + 10 TN ] (12) √ where TN = 2.06 × S1 , Ar and S1 are the crosssectional areas in m2 of the inner entrance to the maze and the maze, respectively, d1 and d2 are the distances in m from the iso-center to the inner maze point A as defined above and from the inner maze point A to the outer entrance of the maze, respectively. The weekly dose due to neutrons is calculated as follows [1,4,16]: DE = W × Dn (13) By using the above formalism (i.e., Eqs. 1 − 13) and professional guidelines, we performed optimized shielding calculations to design the treatment room for a LINAC with a maximum photon energy of 20 MV. 2. Evaluation and Comparison The newly-designed room was compared with an already constructed LINAC treatment room (610 × 610 cm2 ). A Varian’s CLINAC 2100C LINAC with dual mode (photons & electrons) and dual photon energy (i.e., 6 MV and 15 MV) for IMRT and total body irradiation (TBI) was installed in the room [29–33]. The total shielding requirements (i.e., concrete volume in m3 ) and the inner treatment room sizes were calculated and compared with the values for an optimally-planned and an already-constructed room. III. RESULTS AND DISCUSSION The widths of the primary barriers, the distances from the source to the point protected outside the primary barrier (dpri ), the occupancy (T) factor for each barrier, the calculated transmission factor of the primary barrier (Bpri ), the number of TVLs, the calculated thicknesses of the primary barriers (S) on the basis of Bpri , and the final recommended shielding thickness against the primary radiation (20 MV energy) are listed in Table 1. The calculated thicknesses were increased 2 − 4 cm to compensate for any human errors in the final construction of the walls. Similarly, the calculated values of the transmission factors and the corresponding number of TVLs and thicknesses of the barriers against radiation scattered by the patient, head leakage radiation and radiation scattered from surfaces, respectively, -604- Journal of the Korean Physical Society, Vol. 67, No. 3, August 2015 Table 2. The occupancy factor (T) and the shielding design goal (P) for each barrier, the distances from the patient to the point of interest (i.e., dsec ), the scatter fraction defined at dsca (a), the calculated transmission factor (Bp ), the number of TVLs (n) and the thickness of barriers (Sp ) against radiation scattered by the patient. Wall A B C D Ceiling P (Sv/w) 2E-6 2E-6 4E-5 2E-6 2E-6 T 1.000 0.063 1.000 0.063 0.025 a 0.000386 0.006320 0.000386 0.006320 0.006320 dsec (m) 5.70 6.48 8.50 6.48 4.50 Bp 4.21E-5 5.32E-5 1.87E-3 5.32E-5 6.41E-5 n 4.38 4.27 2.73 4.27 4.19 Sp (cm) 150 146 94 146 144 Table 3. The occupancy factor (T) and the shielding design goal (P) for each barrier, the distance from the iso-center to the point of interest (i.e., dsec ), the calculated transmission factor (Bl ), the number of TVLs (n) and the thickness of barriers (Sl ) against head leakage. Wall A B C D Ceiling P (Sv/w) 2E-6 2E-6 4E-5 2E-6 2E-6 T 1.000 0.063 1.000 0.063 0.025 dsec (m) 5.70 6.48 8.50 6.48 4.50 Bl n 6.50E-5 1.34E-3 2.89E-3 1.34E-3 1.62E-3 4.19 2.87 2.54 2.87 2.79 Sl (cm) 144 98 87 98 96 Table 4. The occupancy factor (T) and the shielding design goal (P) for each barrier, the distances from the radiation source to the scattering surface (wall) (i.e., dsca ) and from the scattering surface (wall) to the point of interest (i.e., dsec ), the calculated transmission factor (Bs ), the number of TVLs (n) and the thickness of barriers (Ss ) against surface scatterer. Wall A B C D Ceiling P (Sv/w) 2E-6 2E-6 4E-5 2E-6 2E-6 T 1.000 0.063 1.000 0.063 0.025 dsca (m) 3.81 4.81 3.81 4.81 3.35 dsec (m) 5.70 6.48 8.50 6.48 4.50 Bs n 4.64E-5 1.53E-3 2.06E-3 1.53E-3 8.94E-3 4.33 2.82 2.69 2.82 3.05 Ss (cm) 149 97 92 97 105 are summarized in Tables 2 − 4. The secondary barrier thicknesses against radiation scattered by the patient, head leakage radiation and radiation scattered from surfaces were computed separately due to the fact that each type of radiation has a different energy. The computed value for each secondary barrier thickness against radiation scattered by the patient, head leakage radiation and radiation scattered from surfaces were compared for the Fig. 2. (a) Neutron- and photon-shielded door for the outer maze entrance (20 MV) and (b) the ducts wrap technique for HVAC openings. final recommended secondary barrier thicknesses. Based on the above shielding calculation, we presented the final schematic diagram of the new radiation facility in Fig. 1(a); Fig. 1(b) shows a side view. Figure 1(a) and (b) display complete information on the occupancy of the surroundings areas and on the various distances and areas used in the above calculations, as well as the thicknesses and the lengths of both the primary and the secondary barriers. The calculated values of DP , Dw , DL , DT and Dd were 4.01 × 10−5 Gy/week, 4.02 × 10−6 Gy/week, 1.67 × 10−6 Gy/week, 8.67 × 10−8 Gy/week and 1.14 × 10−4 Gy/week, respectively, for a gantry rotation axis perpendicular to the maze axis. These doses were added Some Folded Issues Related to Over-shielded and Unplanned Rooms · · · – Wazir Muhammad et al. -605- Table 5. Comparison of the optimized shielded LINAC treatment room to the non-optimized shielded LINAC treatment room. Here, PB represents the primary barrier while SB represents the secondary barrier. Walls A PB SB B C PB SB D E Ceiling Total PB SB Optimized shielded LINAC room Size: 762 × 762 cm2 Length Width Height ) Volume (cm) (cm) (cm) (m3 ) 1242 165 365 74.8 450 240 365 39.4 312 150 365 17.1 1242 110 365 49.9 450 240 365 39.4 1099 150 365 60.2 817 122 365 36.4 1242 450 190 106.2 1242 924 150 172.1 595.5 to the capture gamma and neutron doses, especially for the maze door. The calculated value of Dϕ was 3.71 × 10−7 Gy per iso-centre X-ray·Gy based on the computed value of ϕA at the inner maze point (i.e., 1.53 × 1010 n·m−2 per X-ray·Gy at 1 m). Therefore, the value of P due to capture gammas was 4 × 10−5 Sv/week. To reduce this dose to 2 × 10−5 Sv/week (P = 4 × 10−5 Sv/week by considering that half of the dose at the door is due to photons plus capture γ-rays and half is due to neutrons), we take the number of required TVLs to be 1.38 and the total calculated thickness of lead to be 8.3 mm (i.e., 1 TVL of lead = 6 mm). Similarly, the calculated Dn at the maze entrance and the weekly dose due to neutrons (DE ) based on A were 2.01 × 10−6 Sv per X-ray·Gy at the iso-center and 2.01 × 10−3 in Sv/week, respectively. The required number of TVLs to reduce the neutron dose of 2.01 × 10−3 Sv/week to 2 × 10−5 (P/2) Sv/week was 2.00. By using a TVL of 45 mm of BPE (borated (5%) polyethylene) [4] for neutrons, we found the required thickness to be 90 mm. The HVAC duct opening was approximately 4 × 12 cm2 in cross section above the room and 1.22 meter down the maze. One cm of lead and 2.54 cm of polyethylene were used to enclose the duct for proper shielding. The final design of the neutron- and photon-shielded door for the outer entrance to the maze and of the HVAC duct for a highenergy LINAC (i.e., 20 MV) are shown in Figs. 2(a) and (b), respectively. Figure 3(a) shows the final approved sketch of the nonplanned LINAC facility while Fig. 3(b) presents the final approved design of a properly planned and optimized shielded room based on the above calculations. The term unplanned and non-optimized was used due to the fact that all the walls and the ceiling, except the maze and the wall next to it, were built as primary barriers. Figure Non-optimized shielded LINAC room Size: 610 × 610 cm2 Length Width Height Volume (cm) (cm) (cm) (m3 ) 663 244 366 98.1 610 244 366 54.5 442 122 366 49.0 915 244 366 81.7 377 122 366 30.0 1281 1098 264 371.3 684.6 Fig. 3. (Color online) Final approved designs for (a) a nonplanned and non-optimized (over) shielded LINAC treatment room and (b) a pproperly planned and optimized shielded LINAC treatment room based on Fig. 1. 3(a) indicates that the primary and the secondary barriers are of the same thickness. The maze and the outer parallel wall of the maze are about equal to the secondary barriers of the planned LINAC facility and are, therefore, regarded as secondary barriers. The inner dimensions of the unplanned room, excluding the maze area, is 610 × 610 cm2 . The volume of required shielding for each portion of the wall, the total shielding volume for both the planned and the existing volumes of each portion of the wall, and finally the total shielding volume for the unplanned LINAC facility were calculated and are listed in Table 5. A total of 595.5 m3 of concrete were required for the planned room whereas 684.6 m3 were estimated for the existing unplanned room (see Table 5). Figure 4(a) shows a comparison of the volumes of the walls and the ceiling, as well as total volumes for the planned and the unplanned facilities, while Fig. 4(b) shows the percent reduction in the required volume of -606- Journal of the Korean Physical Society, Vol. 67, No. 3, August 2015 and shielding calculation. IV. CONCLUSION A careful plan for a radiation room is imperative to avoid an extra financial burden on the hospital. This will also ensure optimal utilization of the available space for providing special radiotherapy procedures (i.e., TBI) and storage of various treatment accessories and/or immobilization devices. In doing so, a balance between safety & cost-effectiveness must be achieved. ACKNOWLEDGMENTS This research was financially supported by the Ministry of Education, Science Technology (MEST) and the National Research Foundation of Korea (NRF) through the Human Resource Training Project for Regional Innovation (2012H1B8A2026280) and by the Kyungpook National University Research Fund (2014). REFERENCES Fig. 4. (a) Comparison of an optimized shielded LINAC treatment room having a size of 762 × 762 cm2 with a nonoptimized shielded LINAC treatment room having a size of 610 × 610 cm2 . (b) Percent reduction in the volume of the shielding requirements for the planned LINAC treatment room as compared to that for the non-planned LINAC treatment room. shielding. The results show a 14.96% reduction in the required total shielding volume for the optimally-planned facility, but the inner dimensions were increased from 610 × 610 cm2 to 762 × 762 cm2 . The reduction in required shielding means that the total construction cost for the facility may reduce by up to 14.96%. A 14.96% decrease in construction cost is a significant figure for a developing country. The treatment room size is enough to fulfill the requirements for total body irradiation (TBI) at an extended SSD (∼ 400 − 500 cm) and for translational bed TBI [34–37]. An evaluation of the unplanned LINAC facility points out that the room cannot be used as a TBI facility for patients, even though the machine installed inside could not only be used for TBI but also had a license. The facility, to be cost-effective, must be optimally designed by consulting experts in radiation safety [1] J. A. Deye et al., Structural Shielding Design and Evaluation for Megavoltage X- and Gamma-Ray Radiotherapy Facilities (National Council on Radiation Protection and Measurements (NCRP), Bethesda, MD, 2005), NCRP REPORT No. 151. [2] G. R. P. Ortiz López and E. B. Podgorsak, Radiation Protection and Safety in Radiotherapy, in Radiation Oncology Physics: A Handbook for Teachers and Students (International Atomic Energy Agency (IAEA), Vienna, Austria, 2005), p. 549. [3] IAEA, International basic safety standards for protection against ionizing radiations and for the safety of radiation sources (IAEA, Vienna, Austria,1996). [4] IAEA, Radiation Protection in the Design of Radiotherapy Facilities (IAEA, Vienna, Austria, 2006). [5] O. Chibani and C. M. Ma, Med. Phys. 30, 1990 (2003). [6] F. d’Errico, M. Luszik-Bhadra, R. Nath, B. R. Siebert and U. Wolf, Health Phys. 80, 4 (2001). [7] F. d’Errico, R. Nath, L. Tana, G. Curzio and W. G. Alberts, Med. Phys. 25, 1717 (1998). [8] A. Facure, R. C. Falcão, A. X. Silva, V. R. Crispim and J. C. Vitorelli, Appl. Rad. Isotop. 62, 69 (2005). [9] D. S. Followill, M. S. Stovall, S. F. Kry and G. S. Ibbott, J. Appl. Clin. Med. Phys. 4, 189 (2003). [10] S. M. Hashemi, B. Hashemi-Malayeri, G. Raisali, P. Shokrani, A. A. Sharafi and F. Torkzadeh, J. Radiat. Res. 49, 279 (2008). [11] R. McCall, Neutron radiation from medical electron accelerators (Stanford Linear Accelerator Center, CA, USA, 1983). [12] R. C. McCall, Neutron yield of medical electron accelerators. in the proceedings of the 7th International Congress Some Folded Issues Related to Over-shielded and Unplanned Rooms · · · – Wazir Muhammad et al. [13] [14] [15] [16] [17] [18] [19] [20] [21] [22] on International Radiation Protection Association (Sydney, Australia, 1987). NCRP, Neutron contamination from medical accelerators (National Council on Radiation Protection and Measurements (NCRP), Washington, DC, USA, 1984). V. Vylet and J. C. Liu, Radiat. Prot. Dosimetry 96, 333 (2001). J. A. Kalef-Ezra, Radiat. Prot. Dosimetry 147, 281 (2011). R. O. G. John, P. Kelley, A. Raventos, D. Keasey and R. Wu, Structural Shielding Design and Evaluation for Medical Use of X-rays and Gamma-rays of Energies up to 10 MeV (National Council on Radiation Protection and Measurements (NCRP), Washington, DC, USA, 1976). NCRP, Radiation protection design guidelines for 0.1100 MeV particle accelerator facilities: recommendations of the National Council on Radiation Protection and Measurements (National Council on Radiation Protection and Measurements (NCRP), Washington, DC, USA, 1977). J. A. Devanney, IEEE Trans. Nucl. Scien. 30, 1583 (1983). S. A. Charles, B. Meinhold, S. J. Adelstein, W. J. Bair, J. D. Boice, Jr., R . J. M. Fry, E. J. Hall, E. W. Webster and W. K. Sinclair, Limitation of Exposure to Ionising Radiation (National Council on Radiation Protection and Measurements (NCRP), Bethesda, MD, USA, 1993). ICRP, Recommendations of the International Commission on Radiological Protection (International Commission on Radiological Protection (ICRP), Ann. ICRP 21, 1991). P. H. McGinley, Shielding Techniques for Radiation Oncology Facilities (Medical Physics Publishing, Madison, WI, 2002). W. Muhammad, S. Lee and A. Hussain, Med. Phys. 39, 3765 (2012). -607- [23] ICRP, Protection Against Ionizing Radiation from External Sources Used in Medicine (International Commission on Radiological Protection (ICRP), Ann. ICRP 9, 1982) [24] W. R. Nelson and P. D. LaRiviere, Health Phys. 47, 811 (1984). [25] R. C. McCall, P. H. McGinley and K. E. Huffman, Med. Phys. 26, 206 (1999). [26] R. K. Wu and P. H. McGinley, J Appl. Clin. Med. Phys. 4, 162 (2003). [27] R. W. Kersey, Medicamundi 24, 151 (1979). [28] P. H. McGinley and E. K. Butker, Med. Phys. 18, 279 (1991). [29] I. Ahmad, W. Muhammad, M. B. Kakakhail, A. Sbilal, A. Khwaja and A. Khushnaseeb, Iranian J. Cancer Prevention 4, 10 (2011). [30] M. Ahmad, A. Hussain, W. Muhammad and S. Q. A. Rizvi, J. med. phys./ Assoc. Med. Phys. India. 35, 33 (2010). [31] W. Muhammad, L. S. Hoon, K. Alam, M. Maqbool and G. Khan, Nucl. Tech. Radiat. Prot. 27, 368 (2012). [32] W. Muhammad, M. Maqbool and M. Shahid, Rep. Pract. Oncol. Radiother. 14, 214 (2009). [33] W. Muhammad, M. Maqbool, M. Shahid, A. Hussain, S. Tahir, G. Rooh, T. Ahmad and S. H. Lee, Physica Medica 27, 135 (2011). [34] A. Bulent, Total Body Irradiation and IntensityModulated Total Marrow Irradiation, in Quality and Safety in Radiotherapy (Taylor & Francis, Boca Raton, FL, USA, 2010) p. 541. [35] A. Hussain, P. Dunscombe, J. E. Villarreal-Barajas and D. Brown, J. Appl. Clin. Med. Phys. 13, 3767 (2012). [36] A. Hussain, E. Villarreal-Barajas, D. Brown and P. Dunscombe, J. Appl. Clinical Med. Phy. 11, 3213 (2010). [37] A. Hussain, J. E. Villarreal-Barajas, P. Dunscombe and D. W. Brown, Med. phys. 38, 932 (2011).