2501
Relation Between Shock-Related Myocardial
Injury and Defibrillation Efficacy of Monophasic
and Biphasic Shocks in a Canine Model
Stefan Osswald, MD; Thomas G. Trouton, MD; Sean S. O'Nunain, MD; Hartley B. Holden;
Jeremy N. Ruskin, MD; Hasan Garan, MD
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Background Certain biphasic waveforms with specific time
ratios of positive and negative components require less energy
for successful defibrillation of the fibrillating ventricles than
monophasic waveforms. However, if more efficient waveforms
were also to be associated with more injurious effects on
myocardial function, they might not provide a true biological
advantage. This study investigates the relation between defibrillation efficacy and potential toxicity of monophasic and
asymmetric, single capacitor, biphasic waveforms with equal
durations of positive and negative components.
Methods and Results The myocardial lactate extraction rate
(LER) was used to measure the injurious effects on myocardial
oxidative metabolism of two synchronized 35 -J shocks in sinus
rhythm. LER, mean arterial pressure (MAP) and, in a subset
of experiments, cardiac output (CO) and coronary blood flow
(CBF) were measured at baseline, 30 seconds, 60 seconds, 90
seconds, 150 seconds, 300 seconds, and 600 seconds after the
shocks. In 12 dogs, three different waveforms (M 10:
monophasic 10 milliseconds; BI 10: biphasic 10 milliseconds;
BI 20: biphasic 20 milliseconds) were tested as series of two
consecutive shocks (60 seconds apart) resulting in a total of 36
sets of data. At baseline, LER was 25 ± 11%. After monophasic
shocks, LER decreased significantly more than after biphasic
W tith the introduction of nonthoracotomy lead
x
(NTL) systems and the decrease in morbidity and mortality of device implantation,1'2
the implantable cardioverter-defibrillator (ICD) has
increasingly been used in patients with severe left
ventricular dysfunction. Generally, NTL configurations
require higher energy for defibrillation than epicardial
lead systems.3-6 Defibrillation energy requirements,
however, have been shown to decrease by using specific
biphasic shocks with equal duration of positive followed
by negative components (5- and 5-millisecond biphasic
shocks) in experimental models, whereas other ratios
may result in even more superior or actually less efficient shocks.7 Recent clinical availability of biphasic
shock capability with its higher defibrillation efficacy
allows the successful implantation of NTL systems in
more than 90% of patients.28 Clinically, the higher
defibrillation efficacy of certain biphasic waveforms has
Received April 20, 1994; revision accepted May 23, 1994.
From the Cardiac Unit, Massachusetts General Hospital, Harvard Medical School, Boston, Mass.
Correspondence to Hasan Garan, MD, Cardiac Unit, Massachusetts General Hospital 32 Fruit St, Boston, MA 02114.
© 1994 American Heart Association, Inc.
shocks (LER at 150 seconds: M 10: -6+31% versus BI 10:
21±15% versus BI 20: 21±16%; M 10 versus BI 10 and M 10
versus BI 20, P<.05) and showed also a slower recovery (LER
at 300 seconds: M 10: 1±24% versus BI 10: 20±11% versus BI
20:20±15%; M 10 versus BI 10 and M 10 versus BI 20, P<.05).
The maximal decrease in LER was 41±27% for M 10 compared with 18±15% for BI 10 and 15±11% for BI 20 (both, M
10 versus BI 10 and M 10 versus BI 20, P<.05). There was a
similar decrease in CO and MAP, with the lowest MAP after
monophasic shocks. The maximal decrease in MAP was significantly greater after M 10 compared with BI 20 (-29±15
mm Hg versus -13±11 mm Hg, P<.05). The defibrillation
threshold was 18.6±8 J for M 10 compared with 11.5±4.0 J for
BI 10 (P<.05) and 15.0±6.1 J for BI 20, respectively (P=NS).
Conclusions Our results suggest that these specific biphasic
waveforms are associated with less injurious effects on myocardial oxidative metabolism and hemodynamic performance.
Given their higher defibrillation efficacy as well, biphasic
waveforms may provide important long-term benefits in patients receiving frequent shocks from implantable cardioverter-defibrillators. (Circulation. 1994;90:2501-2509.)
Key Words * shock * myocardium * defibrillation
been reported in several studies.8-16 Extensive studies
performed in cultured chick embryo myocardial cells
have shown that not only defibrillation efficacy but also
adverse effects such as postcountershock mechanical
dysfunction and arrhythmias depend largely on the
waveforms used.14'16-19 This relation between defibrillation efficacy and potential toxicity is less well studied in
in vivo models and clinically, and it remains to be shown
whether the potential advantage of the higher efficacy of
currently clinically used biphasic waveforms may be
outweighed by more injurious effects on myocardial
function and therefore provide no true biological benefit. This might become an important safety issue in
patients with critical left ventricular dysfunction.
Electrical myocardial injury, ranging from reversible
myocardial depression with arterial hypotension and
intermittent heart block to irreversible myocardial necrosis, is a well-recognized complication of high-energy
transthoracic defibrillation.20-23 Experimental studies
have identified impaired mitochondrial function with
transient suppression of oxidative metabolism and the
generation of free intracellular radicals as possible
mechanisms underlying high-energy transthoracic defibrillation injury.24-26 These injurious effects on cell
2502
Circulation Vol 90, No 5 November 1994
metabolism, together with their indirect effects on intracellular ion homeostasis, lead to cell membrane
disruption and disintegration of normal cell structures.27
It is not known whether such injurious effects may also
result from repetitive internal ICD countershocks, and
only limited data about shock-induced deterioration in
cardiac function have been reported in the literature.29,30 Using hemodynamic and metabolic monitoring
techniques, the present study investigates the relation
between electrical shock-related myocardial injury and
defibrillation efficacy of monophasic and biphasic
shocks delivered during sinus rhythm.
Methods
Experimental Preparation
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
The protocol was approved by the Massachusetts General
Hospital Committee on Research and the Subcommittee on
Research Animal Care, and all procedures were conducted in
compliance with the guidelines from the NIH Guide for Care
and Use of Laboratory Animals.
Twelve mongrel dogs (weight, 35 +6.7 kg; range, 27 to 46 kg)
were anesthetized with methohexital (15 mg/kg) and pentobarbital (20 mg/kg) and ventilated with oxygen (2 L/min) and
room air. Deeper anesthesia for operative procedures was
achieved with additional halothane (1.0% to 2.0%), which was
later discontinued to avoid anesthesia-related myocardial depression during the study protocol. To reduce shock-induced
skeletal muscle contractions with uncontrolled lactate release
into the systemic circulation, muscle relaxation was induced by
intravenous administration of metocurine iodide (0.05 to 0.10
mg/kg). Under general anesthesia, the heart was exposed via a
left lateral thoracotomy through the fourth intercostal space.
After the pericardium was opened, two defibrillation patch
electrodes (Ventritex Inc) with a surface area of 8 cm2 were
positioned over the right ventricular outflow tract and the left
ventricular inferior wall and sutured to the epicardial surface
to ensure proper contact of the patch electrodes with the
myocardium. Then the pericardium was closed. At the end of
the implantation procedure, a single synchronized 10-millisecond monophasic test shock of 500 V was delivered for determination of the lead resistance, which was later used for
estimation of the first shock energy. After externalization of
the leads, the chest was closed in layered fashion, and intrathoracic air was evacuated via suction over a chest tube.
Under fluoroscopy, a coronary sinus NIH 7F catheter with
two side holes (USCI) was placed in the coronary sinus via the
right external jugular vein. A standard quadripolar 7F EP
catheter (Webster Laboratories Inc) was inserted through the
right femoral vein and positioned at the right ventricular apex
(RVA) for later pacing and sensing purposes. Heart rate
(HR), intracardiac electrograms (IECG), surface ECG, and
the mean arterial pressure (MAP) were monitored continuously. Arterial blood samples were analyzed at regular intervals to keep the arterial blood gas values in the physiological
range (Sao2>95%; Pco2, 38 to 44 mm Hg; pH, 7.36 to 7.44).
Defibrillation Protocol
The externalized defibrillation electrodes (RV-patch=positive
polarity, LV-patch=negative polarity) and the right ventricular
pacing and sensing electrode catheter were connected to an
HVS-02 pulse generator (Ventritex), which has the capability to
deliver synchronized monophasic and single capacitor (150-,uF)
biphasic high-energy shocks with truncated exponential waveforms of programmable voltage (50 to 990 V) and pulse duration
(0.5 to 20 milliseconds). The study protocol required the delivery
of two synchronized 35-J shocks during sinus rhythm with an
interpulse duration of 60 seconds. The stored voltage for the first
35-J shock was estimated based on the resistance and measured
0
L ium
---
A
-----------
It"!"
1-
iumlin
me-
0
W)
Monophasc 10 me Blphasic 10 me
Blphasic 20 me
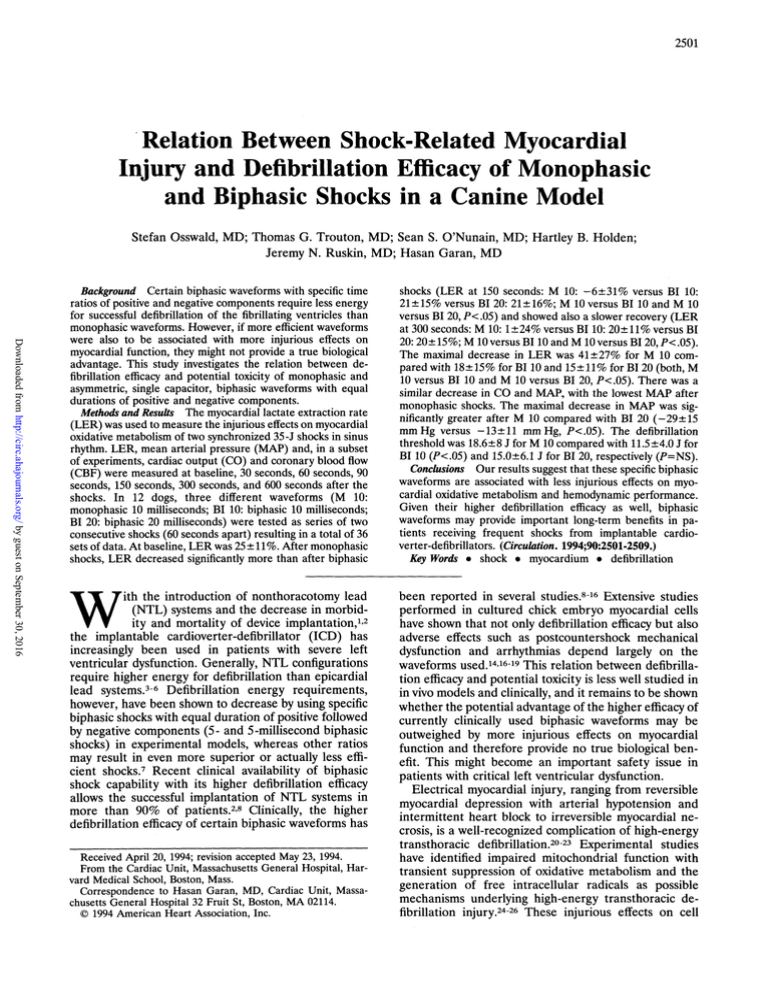
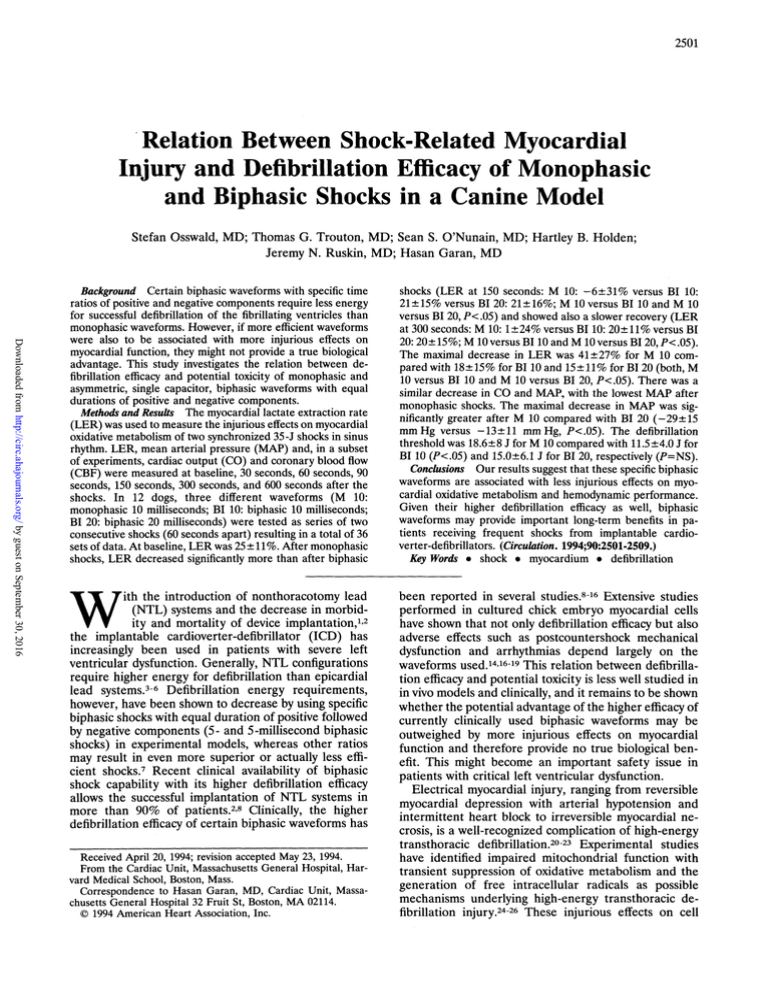
FIG 1. The three different waveforms tested are shown. A
truncated monophasic waveform of 10 milliseconds was compared with two truncated asymmetrical biphasic waveforms of
1 0-millisecond and 20-millisecond duration. All waveforms were
delivered from a Ventritex HVS 02 generator with a single
capacitor of 150 1JF. To keep the delivered energy constant (35
J), the stored voltage was adjusted for each waveform.
energy of the test shock at the end of the implantation procedure.
If the delivered first shock energy differed by more than ± 1.5 J
from the estimated energy (35 J), adjustments were made for the
second shock based on the actual measurements of the first
shock. Lead impedance (R), delivered energy (E), and stored
voltage (V) were recorded for each shock.
Two different biphasic waveforms (Fig 1) with a 50:50 phase
duration (BI 10: 5- to 5-millisecond biphasic pulse, total pulse
duration 10 milliseconds, first component positive, and BI 20:
10- to 10-millisecond biphasic pulse, total pulse duration 20
milliseconds, first component positive) were compared with a
single monophasic pulse wave (M 10: monophasic pulse wave,
10-millisecond pulse duration). In random order, each waveform (M 10, BI 10, BI 20) was tested as two consecutive 35-J
shocks delivered during sinus rhythm, which allowed us to
study metabolic and hemodynamic changes unrelated to myocardial ischemia superimposed by the induction of ventricular
fibrillation (VF). Since the 50:50 ratio was never altered
throughout the study, "biphasic" will mean biphasic with a
50:50 phase ratio (5 and 5 milliseconds biphasic or 10 and 10
milliseconds biphasic) for the rest of this study.
Metabolic and Hemodynamic Monitoring
The lactate concentration was simultaneously measured in
the arterial and the coronary sinus (CS) blood at baseline (t 0),
30 seconds (t 30), 60 seconds (t 60), 90 seconds (t 90), 150
seconds (t 150), 300 seconds (t 300), and 600 seconds (t 600)
after delivery of the first synchronized shock. The first shock
was delivered immediately after baseline measurements
(LERbaseline, MAPbaseline) and the second in a similar fashion
immediately after the measurements at elapsed time 60 seconds (LER60, MAP60).
Immediate deprotonization of the blood with 0.6N perchloric acid (incubated tubes) and storage on ice ensured that the
blood lactate was not further metabolized in vitro and that the
measured lactate concentration was accurate. The lactatepyruvate-dehydrogenase method (enzymatic assay with photospectrometric measurement of NADH production) was used
for lactate measurements. For standardization of the assay, a
standard curve using a Sigma 735-11 standard series was
obtained. The lactate extraction rate (LER) was derived from
the arteriovenous difference of the lactate concentration in the
arterial (art) and CS blood and expressed as a percentage
(LER = ([lactate]a - [lactate]cs)/[lactate]an x100). The minimal
LER (LERm.n) was defined as the lowest LER measured at any
point after delivery of the first shock, and the maximal
decrease in LER was derived by comparing LERmIn with
LERbaselne. Similarly, the lowest MAP (MAPmin) after shocks
was used to calculate the maximal decrease in MAP. To enable
the metabolic and hemodynamic changes to return to baseline,
Osswald et al Defibrillation and Myocardial Electrical Injury
a recovery period of at least 15 minutes was provided after
completion of each shock series.
Continuous hemodynamic monitoring (HR, MAP) was obtained in all experiments (36 of 36). Metabolic monitoring
(LER) was obtained in only 34 of 36 experiments; in one
experiment (BI 10), the coronary sinus catheter was displaced
and could not be repositioned. In another experiment (BI 20),
the catheter was occluded and did not allow further blood
sampling after the shocks. Serial cardiac outputs (CO) measured by the thermodilution technique (7F Swan Ganz catheter, 2095A Cardiac Output Computer, Edwards Laboratories),
continuous pulmonary artery (PA) and right atrial (RA)
pressures, as well as continuous coronary blood flow (CBF)
measurements using a Doppler flow probe (2R probe, HT
101D, Transonic Systems Inc) over the exposed left anterior
descending artery were additionally obtained in 8 of 36
experiments. Vascular resistance in response to high-energy
shocks was calculated for the systemic arterial and coronary
arterial circulation (R=[P1-P2]/flow).
Defibrillation Threshold Measurements
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
After acquisition of hemodynamic and metabolic data for
the three different shock wave series, the defibrillation efficacy
was assessed for each waveform (M 10, BI 10, and BI 20) by
determining the defibrillation threshold (DFT) using the same
electrode configuration and polarity as before. For DFT
estimation, VF was repeatedly induced by burst pacing (output, 10 V; pulse duration, 1.5 milliseconds; cycle length, 20 to
50 milliseconds) at the RVA. After a 10-second period of VF,
a high-energy shock at a selected energy was delivered for VF
termination, followed by a first rescue shock of 25 J and a
second of 40 J if VF was not successfully terminated. A
3-minute recovery period was allowed between each VF
induction. An "up-and-down" algorithm was used for determination of the DFT.31 With this algorithm, the actually tested
shock energy is determined by the success of the preceding
shock. Starting at 15 J, the energy was decreased by 1.0-J steps
after each successful shock until failure to defibrillate was
encountered. After a nonsuccessful shock, a rescue shock was
delivered, and the energy was increased by 1.0 J for the
subsequent defibrillation attempt. Depending on the result of
this latter defibrillation attempt, we either further increased
the energy for the subsequent shock or decreased it again. This
algorithm was carried out until a triplicate confirmation of the
lowest successful shock energy was found, which was defined
as the DFT. This DFT estimation is comparable to the ED50
derived from sigmoidal dose-response curves.30,31 If a rescue
shock was required, a recovery of 5 minutes was allowed to let
the hemodynamic parameters return to baseline and ensure
stability of the preparation throughout the study. Leadingedge voltage, delivered energy, and measured resistance were
recorded for each single defibrillation shock.
Statistical Analysis
are given as mean±1 SD. Continuous variables
compared (baseline versus values at specific time intervals) using two-sided paired Student's t test (Figs 2 and 3).
ANOVA with repeated measures was used to compare serial
measurements between different groups to detect global differences among the different shock waves. Because it was also
desirable to determine at which time interval a significant
difference from baseline occurred, the ANOVA was performed with factorial analysis using a Scheff6's F test (Figs 4
through 7). A value of P<.05 was considered to indicate a
All values
were
significant difference.
Results
A total of 36 series consisting of two synchronized
35 -J
shocks
during sinus rhythm were given
in
12
2503
Test Shock Wave Characteristics
Monophasic
10 ms
Biphasic
10 ms
Biphasic
20 ms
First shock (t 0)
Energy, J
36.8+2.4
38.3+2.1
35.5+2.0
Voltage, V
795±38
864±28
736±19
Resistance, fl
76±9
66±7
71±11
Second shock (t 60)
Energy, J
35.8±1.2
34.4±2.1
35.7±2.2
Voltage, V
791±39
827±26
739±25
75±11
69+8
71±11
Resistance, Q
Average shock
Energy, J
36.3±1.4
36.4±1.3
35.6±1.9
Voltage, V
793±35*
845±21*
737±20*
Resistance, fl
76±10
68±7
71±11
Each waveform was delivered as a series of two consecutive
shocks with an energy of 35 J during sinus rhythm with a
60-second recovery between the shocks. Stored voltage, delivered energy, and resistance for the first and second shock and
their average values for each shock series are given.
*P<.05.
animals. In random order, a series of two monophasic
shocks of 10-millisecond duration (M 10) separated by a
60-second period was compared with a series of two
similarly spaced biphasic shocks of 10-millisecond duration (BI 10) and another series of two biphasic shocks
of 20-millisecond duration (BI 20) in each animal. All
72 shocks were confirmed to be synchronized to the
IECG signal recorded at the RVA, and none of them
induced VF. However, in some experiments the shocks
induced brief runs of accelerated junctional or idioventricular rhythm, which uniformly terminated spontaneously within a few seconds. Thirty-four of 36 series of
lactate sampling (M 10: n=12; BI 10: n=11; BI 20:
n=11) were successfully completed and therefore included in this analysis. The DFT for each waveform was
determined after completion of the lactate sampling
protocol in all 36 experiments.
Metabolic and Hemodynamic Response to
High-Energy Shocks in Sinus Rhythm
The mean delivered energy, resistance, and leadingedge voltage are listed separately for each waveform in
the Table. Biphasic waveforms of 10-millisecond duration (BI 10) required a significantly higher voltage for
delivery of a 35-J shock than monophasic shocks of 10
milliseconds (M 10), whereas biphasic shocks of 20
milliseconds (BI 20) were characterized by the lowest
voltage of all tested waveforms (P<.001 by ANOVA).
The mean LER at baseline was 25+11% (range, 5%
to 48%) for all configurations tested, indicating that
lactate was extracted and metabolized by the myocardium (positive values). Fig 2 depicts the overall changes
of LER in response to two consecutive 35 -J shocks
during sinus rhythm (n=34 experiments). LER decreased significantly from 25 ± 11% (LERbaseline) to
17+19% after the first shock (LER,60) and to 11+25%
after the second shock (LER1P50). After 10 minutes of
Circulation Vol 90, No 5 November 1994
2504
35 J
p
L
40
**
0.05
p
35J
50
L
*
0.001
~~~~~~~~~p
** p<0.0
p
p 0O.0001
p, 0.0001
50
-c
140a
40
30
E 120.
. 110
Cu 100
20
0
10
0
30.
20
-10
0
t
-20
c
W
-J
10
ca
130|
I
Baseline 30
60
90
150
300
-30
0)
Baseline
-10
50
40J
.40
600 sec.
70
60
LER m
MAPIR~
Baseline
FIG 3. Plots show maximal changes in lactate extraction and
mean arterial pressure compared with their baseline values for
all experiments (two-sided paired t test). The minimal lactate
extraction rate (LERmin) and the minimal arterial blood pressure
(MAPmin) were defined as the lowest values observed at any time
after the shocks. Mean values + 1 SD are depicted.
120
E 110
100
CL
t- 70.80
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
e 6070_
2l_
Baseline 30
L
60
l_
90
150
I
l_
300
600 sec.
FIG 2. Bar graphs show metabolic and hemodynamic changes
after two consecutive 35-J shocks in sinus rhythm for all experiments (n=36). The first shock was delivered immediately after
completion of the baseline measurements and the second was
delivered 60 seconds apart (dashed lines). Top, Overall response of the lactate extraction rate in 34 of 36 experiments (M
10: 12 of 12 series of monophasic shocks of 10 milliseconds; BI
10: 1 1 of 12 series of biphasic shocks of 10 milliseconds; BI 20:
11 of 12 series of biphasic shocks of 20 milliseconds of pulse
duration). Bottom, Changes in mean arterial pressure are shown
at the same time intervals after shocks. Values are given as
mean+SD. Changes after shocks are compared with baseline
using a two-sided paired t test.
recovery, LER was still significantly depressed compared with baseline (24.8±11.1% versus 20.2+14.5%;
LERbaseline versus LER1600; P<.05 by paired t test).
The MAP showed a parallel decrease after shocks
(Fig 2, bottom). Although the recovery of MAP was
faster than that of LER, it was incomplete, with the
pressures remaining slightly depressed after 10 minutes
compared with baseline (94±16 versus 90±17 mm Hg,
MAPbaseline versus MAP1600; P<.05 by paired t test).
Since the time course of decrease in LER manifested
marked individual variations, the lowest LER measurement (LERmin) at any point after the shocks was compared with the corresponding baseline value (LERbaseline).
By this analysis, a maximal decrease in LER (LERImi,.=
[LERbaseline>-[LERmin]) of 25±+-22% was observed
(P<.0001 by paired t test). Fig 3 compares LER at
baseline with the lowest values for each experiment
individually. Myocardial lactate production, as indicated
by negative LER values, occurred in 13 of 34 experiments
(38%). Similarly, there was a comparable maximal decrease in MAP of 22±15 mm Hg, if the lowest MAP
(MAPrmin) was compared with the corresponding baseline
value (MAPbaseline) in each series (Fig 3, right). For the
following analysis, both the maximal decrease in LER
(LERAmax) and MAP (MAPAma,x) as well as their absolute
changes over time were used for quantitative comparison
of defibrillation injury caused by the three different
shock waves (M 10, BI 10, BI 20).
Shock-Related Myocardial Injury of Monophasic
and Biphasic Shocks
Fig 4 depicts the serial changes in LER after delivery
of monophasic and biphasic shock waves. During late
recovery, LER15O and LER300 were markedly lower after
two monophasic shocks than after two biphasic shocks
(M 10 versus BI 10 and M 10 versus BI 20, both P<.05
by ANOVA with factorial analysis), whereas no significant difference between the two biphasic shock waves
was found. In 7 of 12 series (58%) of monophasic
shocks, lactate production occurred after the shocks,
accounting for a negative mean LER for the whole
group at 150 seconds of elapsed time (LER1So
-6±31%). In contrast, lactate production was observed
in only 6 of 22 series (27%) with biphasic shocks
(P=.15). There was also a greater decrease in MAP
after monophasic shocks, but statistically the difference
between M 10 and BI 20 was only borderline significant
(Fig 5).
501
O
401
@ 30
X 20
o 10
o
0
E ox -10 X
W
o -20
(U
X 0-30.
_X(C -40.
to
*
-50
0
-a
M1o
-*-*
B510
B 20
p 0.05
60 120 180 240 300 360 420 480 540 600
*
Time (seconds)
FIG 4. Plot shows changes in the lactate extraction rate over
time separated by shock waveform. During sinus rhythm, the first
35-J shock (dashed line) was given immediately after the baseline measurements and the second after a 60-second recovery
period. After monophasic shocks, the LER turned negative
(lactate production) at 150 seconds of elapsed time and was
significantly lower compared with biphasic shocks after 150 and
300 seconds (P<.05 by ANOVA with factorial analysis). M 10
indicates monophasic shock wave of 10-millisecond pulse duration; BI 10, biphasic shock wave of 10 milliseconds; and BI 20,
biphasic shock wave of 20-millisecond pulse duration. Values
are shown as mean+1 SD.
Osswald et al Defibrillation and Myocardial Electrical Injury
Cardiac Output
35J 35J
z
22505
120
E
110
E
100
0
90
0
80
3.0
E 2.5
-J
2.0
1.5
-
Systemic Vascular Resistance
60
70
60
0
s0
k;;'E
|
.1
;.;
201
Coronary Blood Flow (LAD)
Time (seconds)
FIG 5. Similar to Fig 4, plot shows the mean arterial blood
pressure response to two consecutive 35-J shocks in sinus
rhythm depicted for each shock waveform. Although there was a
trend toward a more marked hypotension after monophasic
compared with biphasic shocks, statistically the difference was
only borderline significant between M 10 and B 20 at 90 seconds
(P=.10). Abbreviations as in Fig 4.
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
When the maximal decrease in LER and MAP were
compared (Fig 6), the differences between monophasic
and biphasic shocks became even more evident, with the
monophasic group showing a decrease in LER by
41±27% compared with 18±15% (BI 10) and 15+11%
(BI 20) in the groups with biphasic shocks (P<.05). The
difference between the two biphasic shocks did not
reach statistical significance. Similarly, the maximal
decrease in MAP (MAPAma,) was greater after monophasic shocks (28± 15 mm Hg versus 21±15 mm Hg versus
14± 11 mm Hg; M 10 versus BI 10 versus BI 20), but this
difference was only significant between the groups with
monophasic shocks of 10-millisecond and biphasic shocks
of 20-millisecond duration (P<.05). Neither voltage nor
pulse duration showed a significant correlation with the
maximal decrease in LER or MAP, although there was a
trend toward a greater maximal decrease in LER with
higher leading-edge voltages after monophasic shocks
(r2=.35). However, since the delivered energy was kept
constant (35 J), our protocol did not generate sufficient
data to define a dose-response curve.
CD
m
E
-c
E
._
(0
ca
0
.E
0
0
E
x
E
0
0
pc 0.05
Baseline
MAP51n
Baseline
LER min
in
maximal
decrease
show
FIG 6. Similar to Fig 3, bar graphs
the lactate extraction rate (LER) (left) and mean arterial pressure
(right) used for quantitative comparison of the three different
shock waveforms (statistical comparison by ANOVA by factorial
analysis). The maximal decrease in LER was significantly greater
after monophasic shocks than after biphasic shocks. The maximal decrease in MAP, however, was only significantly different
between M 10 and BI 20. Abbreviations as in Fig 4. Values are
given as mean+1 SD.
40
E 30
20
Coronary Vascular Resistance
5.0
4.0 K*i.. .
----
2.0
__
_
_
Baseline 30
_
_
60
_
_
90
_
.
..
_
_
150
_
_
300
_
_
600 sec.
FIG 7. Graphs show changes in cardiac output (CO) and systemic
vascular resistance as well as coronary blood flow (CBF) and
coronary vascular resistance measured over the left anterior descending artery in a subset of eight experiments. A significant
decrease in cardiac output compared with baseline (P<.001 by
two-sided paired ttest) was observed after the second shock (t 60),
followed by a prolonged recovery. CBF was intermittently increased after the first shock (P=NS compared with baseline) but
stabilized within a narrow range of its baseline value during late
recovery when the CO was still reduced. Moreover, at the time
when the greatest decrease in LER (t 150 and t 300) was observed,
coronary perfusion was normal, suggesting that the changes in
LER were not CBF-related but reflected a direct depression of
myocardial oxidative metabolism.
Influence of High-Energy Shocks on Coronary Flow
and Cardiac Output
In the present study, a decreased LER (or a reduced
arteriovenous difference between the arterial and coronary sinus lactate concentration) was used as an indicator of depressed myocardial oxidative metabolism.
However, to confirm that the increased lactate concentration after shocks measured in the coronary sinus
blood was related to a depressed myocardial lactate
extraction and did not result from ischemia or an
increased lactate supply to the heart as a consequence
of elevated coronary perfusion, CO and continuous
CBF were additionally measured in eight experiments.
The blood pressure response in this subset was comparable to that of the whole study group (Fig 2). In all
eight experiments, MAP and CO decreased significantly
after the shocks with a prolonged and incomplete
recovery after 10 minutes in all measured parameters
(Fig 7). After an initial decrease, the peripheral vascular
resistance increased in response to the markedly depressed CO and MAP after the second shock and
returned to baseline after 10 minutes despite persistently reduced CO (Fig 7). In three of eight experiments, an early increase in CBF up to 230% was
observed after the first shock, whereas in the remaining
five of eight experiments, only minimal changes within a
10% to 20% range were found. However, 90 seconds
after the first shock, CBF was only mildly decreased and
Circulation Vol 90, No 5 November 1994
2506
N.S
N.S.
N.S.
P
30
C 0.05
N.S.
25CD
25
W
M
N.S.
700
N.S.
600.
~~~~~~~500
>
M20
0
Cu400.
15.
0
0
10
~~~~~~~~~200
0.
0
M 1O
B610
20
M10
10
20
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
FIG 8. Bar graphs show defibrillation efficacy compared between the three different shock waveforms. Using an 'up-anddown" algorithm (see "Methods"), we defined the defibrillation
threshold (DFT) as a triplicate confirmation of the lowest shock
energy that successfully terminated ventricular fibrillation. Biphasic shock waves of 10 milliseconds in duration were characterized by significantly lower DFTs in terms of delivered energy
(left). However, if the DFT was compared by the stored capacitor
voltage, there was only a nonsignificant trend toward lower
voltage requirements for biphasic shocks (right). Values are
given as mean+1 SD. Abbreviations as in Fig 4.
remained within a 5% to 10% range of the baseline
value beyond 90 seconds of recovery in eight of eight
experiments. Moreover, at the time when the maximal
decrease in LER was documented (LER,150, LERt300),
CBF had returned to baseline. Maintenance of CBF
during markedly reduced CO and arterial hypotension
after the shocks (t 60, t 90) was related to a decrease in
coronary resistance with selective coronary vasodilation
at a time when systemic vascular resistance was increased. Pulmonary vascular resistance increased only
moderately, and the PA pressures remained stable
despite a significant reduction in CO after the shocks.
Thus, the decrease in LER found in our study appears
to be related to a suppression of the myocardial oxidative metabolism and is not related to changes in coronary perfusion.
Defibrillation Efficacy of Monophasic and
Biphasic Shocks
For each waveform, the DFT was assessed after
completion of the study protocol. As shown in Fig 8
(left), the energy requirements for reliable defibrillation
were significantly higher for monophasic 10-millisecond
shock waves compared with biphasic 10-millisecond
waveforms (18.6±8.6 J versus 11.5±4.0 J; M 10 versus
BI 10; P<.05). The DFT for biphasic 20-millisecond
waveforms (BI 20: 15.0±6.1 J) did not significantly
differ from the other two waveforms. If the lowest
voltage required for successful defibrillation was compared (Fig 8, right), there was no significant difference
among the three groups, although there was a trend
toward a lower leading-edge voltage for biphasic shock
waves (540+117 V versus 475+79 V versus 470+97 V;
M 10 versus BI 10 versus BI 20, respectively; P=NS).
Discussion
Although serious adverse effects including death have
been observed after high-energy transthoracic defibril-
lation,20,21,32,33 little is known about the adverse effects
of repeated internal defibrillation shocks. In the present
study, we have demonstrated that internal defibrillation
suppresses myocardial oxidative metabolism and cardiac function for at least several minutes after shock
delivery. After two 35-J shocks in sinus rhythm, myocardial lactate extraction and hemodynamic performance assessed by CO and arterial blood pressure were
substantially impaired and did not fully recover after 10
minutes of recovery. Biphasic shocks were less injurious
on myocardial oxidative metabolism compared with
monophasic shocks of the same energy and were also
associated with less systemic hypotension. In terms of
defibrillation efficacy, biphasic shocks required less energy for defibrillation as reflected in lower DFTs. Given
the higher defibrillation efficacy and the less injurious
effects on myocardial oxidative metabolism and hemodynamic function, the safety margin between efficacy
and toxicity, or the "therapeutic range" of biphasic is
better than monophasic shock waves, which might provide an important long-term benefit in patients with
frequent ICD discharges.
Mechanisms of Myocardial Defibrillation Injury by
High-Energy Shocks
Since the clinical introduction of direct-current transthoracic defibrillation by Lown et al,33 serious doubts
about adverse outcome after repeated transthoracic
countershocks with high-energy direct current have
been raised.23 Complete heart block,21 severe hypotension resulting in death, as well as myocardial necrosis
have previously been reported as complications of highenergy transthoracic defibrillation.21,33 However, despite the widespread clinical use of ICDs, there are only
a few reports in the literature that suggest that repetitive defibrillation shocks may have serious adverse effects on myocardial function in patients with preexisting
left ventricular dysfunction.28,29
Experimental studies have documented myocardial
necrosis34 and acute death after high-energy transthoracic shocks.26 Severe depression of myocardial lactate
and free fatty acid extraction as well as an increase in
coronary sinus oxygen saturation after defibrillation
offer strong evidence for a shock-induced dysfunction of
cell respiration and oxidative metabolism.24,25 Membrane breakdown,27 in addition to functional33-36 and
morphological mitochondrial changes'8,34 after highenergy shocks, suggests that an uncoupling effect on the
electron transport chain of the mitochondrial membrane may be the primary mechanism of defibrillation
injury. However, a recent study in which isolated mitochondria were exposed to high-energy shocks did not
find such an uncoupling effect, and the measured lactate
extraction in this cell-free mitochondria preparation
remained unaffected.37 Therefore, it was speculated
that the in vivo documented suppression of oxidative
metabolism might be related to an increased transmembrane permeability and intracellular accumulation of
toxic mediators (eg, free intracellular calcium overload
or formation of free radicals). This theory is supported
by the finding that defibrillation-related myocardial
necrosis is reduced by pretreatment with calcium channel blockers but not with f3-adrenoceptor blocking
agents.38
Osswald et al Defibrillation and Myocardial Electrical Injury
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Quantitative Assessment of Myocardial
Defibrillation Injury
For the purposes of our study, myocardial LER was
chosen as a quantitative marker of defibrillation injury.
Although the LER after shocks manifests great interindividual variability, no significant increase in LER was
observed after shocks in any of our experiments (Fig 3).
The finding that LER recovered more slowly after
monophasic shocks than after biphasic shocks suggests
that biphasic shocks are less injurious on myocardial
oxidative metabolism than monophasic shocks of the
same energy. Similar to the metabolic changes was also
a trend toward greater systemic hypotension after
monophasic shocks (Fig 5). On the basis of our results it
appears that metabolic and, to a lesser degree, hemodynamic monitoring are valuable tools for the quantitative comparison of defibrillation injury caused by different shock waves.
In a previous study using a similar defibrillation protocol with two damped cine wave 30-J shocks delivered
during sinus rhythm, the investigators reported a maximal decrease in LER from 37% to -20% (lactate
production) 2.5 minutes after the first shock.25 This more
marked decrease in LER compared with our study may
be related in part to the use of paddles with a greater
contact area (19.6 cm2 compared with our 8-cm2 patches)
and also to differences between the shock waves used.
However, the shock-related decrease in MAP was comparable with our findings. In that study, relative myocardial ischemia as a potential source of lactate production
was excluded by 'Tc pyrophosphate perfusion scintigraphy. In our study, continuous CBF measurements over
the left anterior descending coronary artery were used
for monitoring coronary perfusion. In fact, by this technique an early increase in CBF immediately after the
shocks with return to baseline by 90 seconds was observed. Our results and findings from other studies39
suggest that this early coronary vasodilation (when the
CO is still unchanged) might be directly induced by
electrical shocks, whereas the decrease in coronary vascular resistance during late recovery probably occurs as
an autoregulative response to the depressed CO. However, at the time when the maximal decrease in LER
(LER1so and LER3,) was documented, CBF was constant
compared with its baseline value. This finding suggests
that the rise in CS lactate concentration seen in this study
represents a true suppression of myocardial oxidative
metabolism rather than an ischemia-related increase in
lactate production or an increased lactate supply due to
increased coronary flow.
Currently, there are no data in the literature comparing the adverse effects of monophasic and biphasic
internal high-energy defibrillation shocks by other
quantitative techniques. Indirect evidence that biphasic
shocks may be less injurious compared with monophasic
shocks can be found in the work of Zhou et al,40 who
documented less prolongation of the stimulated postshock action potential (MAP) duration after biphasic
shocks. This direct effect on repolarization may result in
a decreased inhomogeneity of myocardial refractoriness, which in turn may explain the lower propensity for
postshock arrhythmias of biphasic waveforms. Although
it is difficult to explain metabolic changes by invoking
2507
such a mechanism, the two phenomena may share
common features such as an intracellular electrolyte
imbalance due to a changed membrane and ion-channel
permeability. Tovar and Tung41 demonstrated that both
monophasic and biphasic shock waves of the same
voltage have the potential to induce cell membrane
leakage to a variable degree. Although there was a trend
toward a faster recovery after biphasic shocks, the
difference between monophasic and biphasic shocks was
not significant.41 This shock-induced membrane leakage
with alterations in the intracellular ionic composition
with the secondary potential to arrhythmias and dysfunction of the contractile apparatus was documented
over a time course of seconds to minutes after the
shocks and was even irreversible in some preparations.4'
Therapeutic Range of Monophasic and Biphasic
Defibrillation Shocks
On the basis of the above observations, it appears
that monophasic and biphasic shock waves have different effects on cellular membranes, resulting in a differing potential to cause intracellular electrolyte changes
that secondarily affect cellular metabolism and electrophysiological properties. These effects may account in
part for the differences in defibrillation energy requirements between monophasic and biphasic shocks, but at
the same time, they may also be responsible for a
different susceptibility to electrical myocardial injury.
The concept of a waveform specific safety ratio dates
back to the work of Jones and Jones.16,17 These investigators used cultured chick embryo myocardial cells to
investigate in vitro postcountershock myocardial dysfunction and arrhythmias and demonstrated that biphasic waveforms had larger safety factors than truncated
or rectified waveforms.1617 Recent work from the same
investigators demonstrated less injurious effects on
myocardial function with triphasic waveforms as measured by postshock contractility of cultured myocardial
cells.19
In our study, biphasic shocks of 10-millisecond duration were characterized by significantly lower DFTs
than monophasic shocks, whereas biphasic shocks of
20-millisecond duration did not differ significantly from
either form (Fig 8). If the DFT was defined as the lowest
voltage required for successful defibrillation, biphasic
waveforms provided only a marginal advantage, which
did not reach statistical significance. However, if the less
injurious effects of biphasic waveforms are taken into
account, the safety margin, or "therapeutic range,"
appears to be better for biphasic waveforms.
Limitations
A major limitation of our study is the lack of a "gold
standard" for the quantitative assessment of defibrillation injury in vivo. Hemodynamic changes are not
accurate enough to detect subtle differences between
different shock waves, whereas metabolic monitoring
with the method of LER is limited by a considerable
interindividual variability. Although compared with histopathological studies, LER monitoring provides the
important advantage that different shock waves can be
compared in the same animal, it introduces another
limitation, namely, that irreversible changes incurred
from a preceding series of shocks may influence the
2508
Circulation Vol 90, No 5 November 1994
results of the subsequent series. To attempt to over-
problem, our protocol provided a long recovery period of at least 15 minutes between the shock
series. For the same reason, only two shocks per series
were delivered, and to avoid irreversible injury incurred
from extensive DFT testing, the DFTs were obtained
after completion of the study protocol. Therefore, the
shock waves had to be compared at fixed rather than
individualized energy levels (eg, twice DFT energy for a
given heart), which biologically might have been more
come this
relevant.
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Although relatively large animals were used for this
study, and the average heart size was comparable to that
of a human heart, energy requirements and resulting
voltage gradients across the myocardium are likely to be
different in humans. Furthermore, in our experiments
the patch electrode size was relatively small compared
with those commonly used for clinical epicardial implantation. Therefore, the results of our study should be
extrapolated to the clinical setting with appropriate
caution.
Clinical Implications and Conclusions
The results of the present study suggest that biphasic
shocks are more efficient at defibrillation and are also
associated with less injurious effects on myocardial oxidative metabolism and cardiac function. Therefore, the
use of biphasic waveforms should not necessarily be
limited to patients with high DFTs, since the better
therapeutic range may provide an important long-term
benefit in patients with frequent ICD discharges and
patients with severe left ventricular dysfunction. Future
research should focus not only on defibrillation efficacy
but also on defibrillation injury and ways of minimizing it.
Acknowledgments
Stefan Osswald is the recipient of a research fellowship
granted by the Lichtenstein Foundation, Switzerland. We
express our gratitude to Louis Guerrero for his technical
assistance and to Gus J. Vlahakes, director of the cardiac
surgical research laboratory, for the use of the laboratory
facilities.
References
Bardy GH, Hofer B, Johnson G, Kudenchuk PJ, Poole JE, Dolack
GL, Gleva M, Mitchell R, Kelso D. Implantable transvenous
cardioverter-defibrillators. Circulation. 1993;87:1152-1168.
2. Bardy GH, Johnson G, Poole JE, Dolack GL, Kudenchuk PJ, Kelso
D, Mitchell R, Mehra R, Hofer B. A simplified, single-lead unipolar
1.
transvenous cardioversion-defibrillation system. Circulation.
543-547.
3.
1993;88:
Bardy GH, Troutman C, Johnson G, Mehra R, Poole JE, Dolack
GL, Kudenchuk PJ, Gartman DM. Electrode system influence on
biphasic waveform defibrillation efficacy in humans. Circulation.
1991;84:665-671.
4. Yee R, Klein GJ, Leitch JW, Guiraudon GM, Guiraudon CM,
Jones DL, Norris C. A permanent transvenous lead system for an
5.
implantable pacemaker cardioverter-defibrillator: nonthoracotomy
approach to implantation. Circulation. 1992;85:196-204.
Saksena S, Luceri R, Krol RB, Brownstein S, Burkhardt E, Accorti
P, Brewer G, Scott S, Callaghan F, Livingston A. Endocardial
pacing, cardioversion and defibrillation using a braided
endocardial lead system. Am J Cardiol. 1993;71:834-841.
Bardy GH, Allen MD, Mehra R, Johnson G. An effective and
adaptable transvenous defibrillation system using the coronary
sinus in humans. JAm Coll Cardiol. 1990;16:887-895.
7. Dixon EG, Tang ASL, Wolf PD, Meador JT, Fine MJ, Calfee RV,
Ideker RE. Improved defibrillation thresholds with large con6.
toured epicardial electrodes and biphasic waveforms. Circulation.
1987;76:1176-1184.
8. Saksena S, An H, Mehra R, DeGroot P, Krol RB, Burkhardt E,
Mehta D, John T. Prospective comparison of biphasic and
monophasic shocks for implantable cardioverter-defibrillators
using endocardial leads. Am J Cardiol. 1992;70:304-310.
9. Chapman PD, Vetter JW. Souza JJ, Troup PJ, Wetherbee JN,
Hoffmann RG. Comparative efficacy of monophasic and biphasic
truncated exponential shocks for nonthoracotomy internal defibrillation in dogs. JAm Coll Cardiol. 1988;12:739-745.
10. Fain ES, Sweeney MB, Franz MR. Improved internal defibrillation
efficacy with a biphasic waveform. Am Heart J. 1989;117:358-364.
11. Flaker GC, Schuder JC, McDaniel WC, Stoeckle H, Dbeis M.
Superiority of biphasic shocks in the defibrillation of dogs by
epicardial patches and catheter electrodes. Am Heart J. 1989;118:
288 -29 1.
12. Jones DL, Klein GJ, Guiraudon GM, Yee R. Biphasic versus
sequential pulse defibrillation: a direct comparison in humans. Am
Heart J. 1993;125:405 -409.
13. Holley LK, McCulloch RM. Comparison of biphasic and monophasic
defibrillation waveforms in an isolated rabbit heart preparation. Cardiovasc Res. 1991;25:979-983.
14. Jones JL, Jones RE, Balasky G. Improved cardiac cell excitation
with symmetrical biphasic defibrillator waveforms. Am J Physiol.
1987;253:H1418-H1424.
15. Winkle RA, Mead RH, Ruder MA, Guadiani V, Buch WS, Pless
B, Sweeney M, Schmidt P. Improved low energy defibrillation
efficacy in man with the use of a biphasic truncated exponential
waveform. Am Heart J. 1989;117:122-127.
16. Jones JL, Jones RE. Determinants of safety factor for defibrillator
waveforms in cultured heart cells. Am J Physiol. 1982;242:
H662-H670.
17. Jones JL, Jones RE. Improved defibrillator waveform safety factor
with biphasic waveforms. Am J Physiol. 1983;245:H60-H65.
18. Jones JL, Proskauer CC, Paul WK, Lepeschkin E, Jones RE.
Ultrastructural injury to chick myocardial cells in vitro following
'electric countershock.' Circ Res. 1980;46:387-394.
19. Jones JL, Jones RE. Improved safety factor for triphasic
defibrillator waveforms. Circ Res. 1989;64:1172-1177.
20. Weaver WD, Cobb LA, Copass MK, Hallstrom AP. Ventricular
defibrillation-a comparative trial using 175-J and 320-J shocks.
N Engl J Med. 1982;307:1101-1106.
21. Dahl CF, Ewy GA, Warner ED, Thomas ED. Myocardial necrosis
from direct current countershock: effect of paddle electrode size
and time interval between discharges. Circulation. 1974;50:
956-961.
22. Tacker WAJ, Van VJF, Geddes LA. Electrocardiographic and
serum enzymic alterations associated with cardiac alterations
induced in dogs by single transthoracic damped sinusoidal
defibrillator shocks of various strengths. Am Heart J. 1979;98:
185-193.
23. Resnekov L, McDonald L. Complications in 220 patients with
cardiac dysrhythmias treated by phased direct current shock, and
indications for electroconversion. Br Heart J. 1967;29:926-936.
24. Gaba DM, Maxwell MS, Merlone S, Smith C. Internal countershock produces myocardial damage and lactate production
without myocardial ischemia in anesthetized dogs. Anesthesiology.
1987;66:477-482.
25. Trouton TG, Allen JD, Adgey AA. Oxidative metabolism and
myocardial blood flow changes after transthoracic DC countershocks in dogs. Eur Heart J. 1992;13:1431-1440.
26. Trouton TG, Allen JD, Yong LK, Rooney JJ, Adgey AA. Metabolic
changes and mitochondrial dysfunction early following transthoracic
countershock in dogs. PACE Pacing Clin Electrophysiol. 1989;12:
1827-1834.
27. Tovar 0, Tung L. Electroporation and recovery of cardiac cell
membrane with rectangular voltage pulses. Am J Physiol. 1992;
263:H1128-H1136.
28. Grimm W, Flores BF, Marchlinski FE. Complications of implantable
cardioverter defibrillator therapy: follow-up of 241 patients. PACE
Pacing Clin Electrophysiol. 1993;16:218-222.
29. Frame R, Brodman R, Furman S, Kim SG, Roth J, Ferrick K,
Hollinger I, Gross J, Fisher JD. Clinical evaluation of the safety of
repetitive intraoperative defibrillation threshold testing. PACE
Pacing Clin Electrophysiol. 1992;15:870-877.
30. Jones DL, Irish WD, Klein GJ. Defibrillation efficacy: comparison
of defibrillation threshold versus dose-response curve determination. Circ Res. 1991;69:45-51.
Osswald et al Defibrillation and Myocardial Electrical Injury
31. Fujimura 0, Jones DL, Klein GJ. The defibrillation threshold:
how many measurements are enough? Am Heart J. 1989;117:
977-979.
32. Lown B, Neuman J, Amarasingham R, Berkovitz BV. Comparison
of alternating current with direct current electroshock across the
closed chest. Am J Cardiol. 1962;10:223-227.
33. Warner ED, Dahl C, Ewy GA. Myocardial injury from transthoracic defibrillator countershock. Arch PathoL 1975;99:55-60.
34. Koning G, Veefkind AH, Schneider H. Cardiac damage caused by
direct application of defibrillator shocks to isolated Langendorffperfused rabbit heart. Am Heart J. 1980;100:473-482.
35. Abood LG, Gerard RW, Ochs S. Electrical stimulation of metabolism
of homogenates and particulates. Am J Physiol. 1952;171:134-139.
36. Narayanaswami A, McIlwain H. Electrical pulses and the
metabolism of cell-free preparations. Biochem J. 1954;57:
663-666.
2509
37. Trouton TG, Barry JJ, Allen JD, Adgey AA. Failure of countershock-type pulses in vitro to adversely alter mitochondrial oxidative
phosphorylation. Ann Emerg Med. 1992;21:132-136.
38. Patton JN, Allen DJ, Pantridge FJ. The effects of shock energy,
propranolol, and verapamil on cardiac damage caused by transthoracic countershock. Circulation. 1984;69:357-368.
39. Kerber RE, Martins JB, Gascho JA, Marcus ML, Grayzel J. Effect of
direct-current countershocks on regional myocardial contractility and
perfusion: experimental studies. Circulation. 1981;63:323-332.
40. Zhou XH, Knisley SB, Wolf PD, Rollins DL, Smith WM, Ideker
RE. Prolongation of repolarization time by electric field stimulation with monophasic and biphasic shocks in open-chest dogs.
Circ Res. 1991;68:1761-1767.
41. Tovar 0, Tung L. Electroporation of cardiac cell membranes with
monophasic or biphasic rectangular pulses. PACE Pacing Clin Electrophysiol. 1991;1887-1892.
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Relation between shock-related myocardial injury and defibrillation efficacy of
monophasic and biphasic shocks in a canine model.
S Osswald, T G Trouton, S S O'Nunain, H B Holden, J N Ruskin and H Garan
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Circulation. 1994;90:2501-2509
doi: 10.1161/01.CIR.90.5.2501
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1994 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/90/5/2501
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/